Abstract
Purpose
Uretero-pelvic junction obstruction is the most common cause of prenatal hydronephrosis. It can be intrinsic, extrinsic due to crossing vessel (CV) or mixed. This paper aims to present the surgical outcome in a single pediatric third-level center.
Methods
A retrospective analysis of all children operated between 2011 and 2018 was conducted. Demographic information, pre-operative pelvic antero-posterior diameter (APD), intra-operative parameters, hospital stay and follow-up were considered. Re-do operations and success rate for Vascular Hitch (VH), open and laparoscopic pyeloplasties were recorded.
Results
128 patients were included. The mean pre-operative APD was 30 mm. The etiology was intrinsic in 71.9%, extrinsic in 25.0% and mixed in 3.1%. The median age between intrinsic and extrinsic groups was statistically different. Thirty-one VH, 88 dismembered and 9 non-dismembered pyeloplasties were performed. The median hospital stay was 2 days for VH and 6 for pyeloplasties. The median hospital stay was statistically longer in open pyeloplasties compared to laparoscopic. The mean post-operative APD was 14 mm. The success rate after VH was 90.3%, after open pyeloplasties 97.9% and after mini-invasive pyeloplasties 91.8%.
Conclusions
VH could be a good option in the treatment of hydronephrosis due to CV, laparoscopic pyeloplasties have equivalent success rate and shorter hospital stay than open pyeloplasties.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hydronephrosis is the impairment of urinary flow from the renal pelvis to the ureter. Most cases are caused by intrinsic factors, such as an aperistaltic ureteral segment, infoldings of the ureteral wall or true strictures [1]. Extrinsic forms of uretero-pelvic junction obstruction (UPJO) include the presence of an aberrant crossing vessel (CV), kinkings or fibrous bands over the uretero-pelvic junction (UPJ) [2, 3]. Intrinsic UPJO is one of the most frequent urological diseases affecting the pediatric population, and it is the most common pathological cause of prenatal dilation of pelvis and calices and neonatal hydronephrosis with an overall incidence of 1:1500 [4, 5]. 50–75% of the prenatal hydronephrosis stabilizes or resolves spontaneously with the growth of the child [6,7,8]. In the remaining cases, surgical correction is recommended to avoid a progressive and irreversible deterioration of renal function due to chronic pelvic obstruction [9].
The surgical gold standard for patients with hydronephrosis has always been dismembered pyeloplasty (DP) as described by Anderson and Hynes in 1949 [10, 11]. Another surgical technique which can be a valid alternative to DP in case of aberrant CV is the vascular hitch (VH), first described by Hellstrom in 1949. It consists in displacing and fixing the UPJ in a more distal position [12,13,14]. This technique was later modified by Chapman, who proposed moving the CV more cranially within a wrap of the anterior wall of the redundant pelvis, without vascular adventitial sutures [15]. According to Schneider et al. the only situation in which a VH has to be performed is when the vessels are under the UPJ, resulting in ureteral kinking (defined as a ureteral curl or bend around the polar vessels similar to a swan-neck ureter) [16]. Some authors reported good results also by performing a non-dismembered pyeloplasty (Y–V Foley) (NDP), especially in those patients with a small-sized renal pelvis, a long narrow ureteric segment or a high insertion of the ureter [17]. Laparoscopic pyeloplasty for the management of UPJO provides operative times, total hospital costs, and success rates similar to those of open surgery, but at the same time patients treated laparoscopically benefit from the minimally invasive approach with reduced morbidity [18]. Minimally invasive surgery includes also the laparoscopic-robotic assisted approach. Long-term follow-up shows that robotic pyeloplasty is a safe method, with advantages compared to open pyeloplasty, and with the same success rate [19].
The aim of this study was to evaluate the outcome of UPJO surgery in a single pediatric third-level center, analyzing the long-term follow up of children who underwent laparoscopic VH, laparoscopic/open DP and NDP in a seven-years-period.
Material and methods
We retrospectively reviewed data of all children who underwent surgical treatment for hydronephrosis in the period from January 2011 to March 2018 in the Giannina Gaslini Children’s Hospital of Genoa. The indications for surgery were based on the following criteria: symptomatology (recurrent flank pain, urinary tract infection), increased renal pelvic antero-posterior diameter (APD) (with or without calicectasis), worsening of split renal function and poor drainage function after the administration of furosemide.
Demographic data, pre-operative and intra-operative parameters, and post-operative follow-up results were evaluated. The following descriptive items were considered: sex, side of the affected kidney, age at surgery and associated morphologic anomalies. Pre-operative pelvic APD had been evaluated with ultrasound (US) or with functional Magnetic Resonance Urography (fMRU), all the patients had an obstructing drainage curve detected at the dynamic renal scintigraphy before the operation.
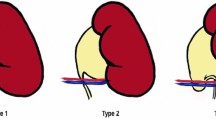
The descriptions of all surgical procedures were reviewed. The etiology of UPJO could be intrinsic, extrinsic due to a CV or mixed (Fig. 1). Patients underwent a classic Anderson Hynes DP when a pure intrinsic UPJO or a mixed etiology (intrinsic stenosis with aberrant CV) was detected. Children with CV without any associated intrinsic UPJO underwent Hellstrom VH. In patients with intraparechymal pelvis or with long stenotic tract a Foley NDP was preferred. The surgical approach was open, laparoscopic or robotic assisted. The robotic system was used only in a twelve-months-period in which it was available in our pediatric institution (Avril 2016–March 2017). The post-operative length of hospital stay (LHS) was recorded for all the children. The laparoscopic and robotic assisted operations were all performed by a single surgeon, while the open pyeloplasties were performed by 4 surgeons.
Success after the surgical procedure was defined as resolution of symptoms (urinary tract infections or pain) and improvement of hydronephrosis detected at US or fMRU with reduction of APD without tension and compression of the kidney parenchyma. The worsening of the hydronephrosis was defined as the augmentation of APD at US or fMRU with the persistence of kidney parenchyma compression and drainage curve with obstructing pattern detected with dynamic renal scintigraphy or fMRU. These patients were later re-operated. Redo operations and the APD after the re-operation were recorded to evaluate the success rate of the re-do surgical procedure.
Surgical details in laparoscopic and robotic surgery
The patient is usually positioned in a 60° lateral decubitus with the affected side elevated, over a soft roll. Transperitoneal laparoscopy (with or without the robotic assistance) is performed by placing a 12-mm umbilical camera port, followed by two 3–5-mm working ports (8 mm if robotic assisted) placed in the epigastrium and in the ipsilateral lower quadrant, respectively. Operating on the right side may require a fourth 3-mm port to retract the liver. Access to the renal pelvis and ureter is achieved by displacement of the colon, with the minimal opening of the parietocolic peritoneum. An anterior approach to the perinephric area is used to safely manage the vessels and the pelvis. When a CV is identified, the pelvis is mobilized and a Hellstrom VH is performed dislocating the UPJ more caudally (Fig. 2). During this phase the surgeon must be very careful to respect the aberrant CV, in fact in most cases it is an arterial vessel which supplies the lower pole of the kidney. Impairment of the aberrant artery can cause an ischemia of the lower renal pole. The hitch is usually performed by three single stitches with a 5/00 absorbable monofilament thread. When a crossing vessel is not present and/or a narrow UPJ is visualized during the dislocation of the pelvis, the surgeon usually decides to perform a pyeloplasty. In most cases, the Anderson-Hynes DP is preferred. The pelvis is suspended with a single traction stitch and the urinary continuity is completely interrupted in the stenotic UPJ. The anastomosis is performed with a 6/00 absorbable monofilament thread making an intermittent suture in the posterior wall and a continuous suture in the anterior one. During the procedure, a pelvi ureteric double J stent is positioned to protect the anastomosis and it is maintained for 30–45 days. When the pelvis is intraparechymal or the stenotic tract is too long, the surgeon could decide to perform a Foley NDP. The pelvis is suspended with a single traction stitch and the urinary continuity is partially interrupted at the stenotic UPJ. The anastomosis is performed with a 6/00 absorbable monofilament thread.
Intra-operative laparoscopic sequence of vascular hitch for extrinsic uretero-pelvic junction obstruction due to a crossing vessel. (1) A crossing vessel is visible over the uretero-pelvic junction; (2) dislocation of the uretero-pelvic junction among the vessel; (3) Beginning of the hitch that is usually performed by single stitches with a 5/00 absorbable monofilament thread; (4) performing of the first stitch of the vascular hitch; (5) no intrinsic narrowing are macroscopically visible and confirmed with the diuretic test; (6) end of the first stitch of the vascular hitch
Statistical analysis
Descriptive analysis of the entire cohort of patients had been performed first. Patients characteristics were provided: categorical data were summarised in terms of absolute frequencies and percentages, and quantitative variables were summarised in terms of mean, medians and range, as the data were not normally distributed. Fisher’s two-tailed exact test was used for dichotomous variables, the differences between groups about the age at surgery and hospital stay were calculated with the parametric t Student test. A p value < 0.05 was considered statistically significant.
Results
In the study period, 160 patients with hydronephrosis had been operated (98 males and 62 females). The affected side was right in 72 patients and left in 88 cases. Thirty-two patients were excluded because of incomplete data or because they were lost during the follow-up. The included patients were 128, of which 75 males and 53 females (ratio M:F = 1.58:1), 60 with right side affected and 68 left side. Three patients had a double collecting system, one patient had a horseshoe kidney. The mean pre-operative APD was 30 mm (median 30 mm, range 12–70 mm). In patients who later underwent VH the mean pre-operative APD was 32.8 mm (median 31), while in those who later underwent a pyeloplasty it was 29 mm (median 27).
The etiology of the obstruction was intrinsic in 92 patients (71.87%), extrinsic due to the presence of an obstructing CV in 32 (25.0%) and mixed in 4 cases (3.12%). The operation was open in 49 cases and laparoscopic in 79 cases (6 robotic-assisted). The Anderson Hynes DP had been performed in 88 children, a Foley NDP in 9 cases, while the Hellstrom VH in 31patients. Only one child with extrinsic UPJO due to a CV had undergone a DP because of the presence of multiple cicatricial adhesions due to a previous operation. Except one case, all the Hellstrom VH had been performed by mini-invasive surgery, while pyeloplasties had been performed by an open approach in 48 cases and by laparoscopic or robotic-assisted approach in 49 patients.
The median age at surgery of all patients was 20.27 months (mean age 52.52, range 5 days–240.87 months). The median age at surgery in patients with intrinsic stenosis was 12.27 months (mean 36.38, range 5 days–218 months), while in those with extrinsic etiology it was 102.18 months (mean 102.53 months, range 5–240 months). The median age between the two groups, calculated with Student’s t test, was statistically different (p = 0.0001).
The median post-operative LHS of all included patients was 5 days (mean 5.1, range 1–24). After a Hellstrom VH, the median hospital stay was 2 days (mean 2.16, range 1–7), while after a pyeloplasty it was 6 days (mean 6.25, range 2–24). Considering only pyeloplasties, the median hospital stay was statistically longer in open procedures compared to mini-invasive ones (p = 0.0430) (Table 1). The only case treated by open VH procedure had a LHS of 4 days.
The mean follow-up was 24 months. The mean post-operative APD was 14 mm (median 11 mm, range 5–67 mm). After a pyeloplasty the mean post-operative APD was 13 mm (median 11, range 5–67), while after a VH it was 16 mm (median 13, range 7–50). The percentage of reduction of the APD was 46% after a pyeloplasty and 50% after a VH. During the follow-up, the reduction of APD without tension and compression of the kidney parenchyma was present in 120/128 patients. In 8/128 patients (6.25%) the hydronephrosis worsened after the operation. Re-do surgery was required in seven cases (3 after VH, 3 after DP and 1 after NDP), while in one patient the residual kidney function was absent and the affected side was considered lost. In the three cases of failed VH a laparoscopic DP was later performed; within the four laparoscopic pyeloplasties with bad evolution, two were re-operated on using the robotic system and two using the traditional laparoscopy.
The total pyeloplasty success rate was 94.8%, while for the VH it was 90.3%, without statistical differences (p = 0.4). No differences were detected about the number of re-do operations and success rate after open and mini-invasive pyeloplasties (0.362) (Table 1). After re-do pyeloplasty all the patients had an improvement of the hydronephrosis with reduction of pelvic APD without compression of the kidney parenchyma.
We had 6 early complications (4.7%). Three patients (2.3%) presented early complications that required second access to the operating room (grade 3b according to Clavien Dindo classification): one dehiscence of the uretero-pelvic anastomosis which required a stent placement at 4th post-operative day; one patient complaining about flank pain and worsening of US hydronephrosis after a VH required a stent placement at 4th post-operative day; and one had omental herniation from the drainage exit requiring its reduction in the operative room. These 3 early complications caused a longer length of stay: 19, 7 and 7 days, respectively. Three other patients (2.3%) presented postoperative urinary tract infection that required prolonged intravenous antibiotic therapy (grade 2 according to Clavien Dindo classification) and, therefore, a longer time of hospitalisation (12, 20 and 24 days, respectively).
Discussion
UPJO is the most common anatomical cause of prenatal hydronephrosis with an overall incidence of 1:1500 [4]. UPJO may also be diagnosed later during childhood due to symptoms such as flank pain or recurrent urological infections [19]. The etiology of the obstruction can be intrinsic, extrinsic or mixed. According to literature data, the presence of CV in patients with hydronephrosis ranges from 11 to 58% in different cohorts [20,21,22,23]. In our study, we found the presence of CVs in 25% of the children operated for hydronephrosis in a 7-year period. The incidence of CV has a direct correlation with the age of children, being low in neonates and infants who usually have prenatal diagnosis and very high in older children who usually present with intermittent symptoms of obstruction (pain, nausea, vomiting) [22]. Calisti et al. reported lower polar CV in six out of 54 (11%) prenatally detected cases with a mean age of 3.5 months compared with 12 out of 30 (40%) symptomatic patients who had a mean age of 6.4 years [23]. In our sample, we confirm that in children with CV the symptomatology appears later in life with intermittent lumbar pain, with a median age at surgery statistically higher compared to the group without CV (102.18 months vs. 12.27). No statistically significant differences were found about the sex of patients, with a higher incidence of hydronephrosis in males (M:F = 1.58:1), and about the side of the affected kidney, with a higher incidence in the left side, in agreement with literature data [4].
Open Anderson-Hynes DP has always been considered the gold standard both for intrinsic and extrinsic UPJO with success rates of more than 90% [10]. In the last decade, many authors have wondered whether Hellstrom VH can be considered a valid alternative to DP in presence of CV [12, 16, 24, 25], considering the advantages of this technique: surgical repair without opening the collecting system, leaving the UPJ intact, eliminating the risk of leakage or urinoma and preserving the pyelo-ureteral motility peristalsis. This procedure avoids the technical challenge of pelvi-ureteric anastomosis with a low complication rate and operative time [25, 26]. During the operation, if a CV is present, it can be difficult to determine whether it is an incidental finding or plays a significant role in the obstruction [25]. Evaluating if the crossing vessel is obstructing the UPJ or it is only located near it without any functional compression is not mathematically possible. During the operation, the dilatation of the UPJ due to liquid volume infusion, after the vascular dislocation, is the only confirmation. For this reason, we prefer an anterior trans-peritoneal approach [27, 28]. After a VH, the hospital stay is usually shorter compared to Anderson Hynes DP with a median length of 2 days [24, 25, 29]. In our sample, the hospital stay was shorter in patients who had undergone Hellstrom VH compared to those subjected to dismembered or non-dismembered pyeloplasty (respectively, 2 vs. 6 days). This difference is related to different surgical technique. In fact, the VH assures a repair without opening the collecting system, leaving the UPJ intact and eliminating the risk of postoperative leakage or urinoma. Furthermore, in case of pyeloplasty we usually placed a laminar drain which was removed after at least 48 h. On the contrary, in VH we never left a drain.
In literature, the success rate of VH has been reported in a range of 92–100% [24, 25, 29], even if a careful pre-operative and intra-operative functional and anatomical assessment is crucial to guide the choice between VH and DP [24]. Schneider and colleagues identified three different types of intraoperative anatomical relationship between the lower pole CV, the renal pelvis, the PUJ, and the ureter and only Schneider type 3situation with ureteral kinking and normal junction should be proposed for VH [16]. In our experience, the laparoscopic VH success rate was 90.3% and we agree with other authors that VH may be a safe, feasible, and attractive alternative to treat obstructed hydronephrosis due to polar CV [16, 24, 25, 29].
In the last two decades, the open technique for DP has gradually been replaced by laparoscopic and, more recently, by robotic-assisted repair with comparable results [19, 30]. Mini-invasive approach for the treatment of UPJO has the advantage of reconstruction under magnified vision with low morbidity regarding the postoperative pain, the shorter hospital stay and smaller incision scar [31]. In our sample, 48 pyeloplasties were performed with open technique and 49 with mini-invasive approach. The open pyeloplasties had been performed in the first years of the study when only one surgeon had mini-invasive surgery skills or in small infants with low weight, while from 2014 the laparoscopic approach became the preferred technique. The LHS was significantly shorter in patients operated on with mini-invasive surgery pyeloplasties than with open technique. No statistically significant differences were present between the two groups about the number of re-operation and, consequently, the success rate. Considering the comparable success rate and shorter LHS, we agree with other authors that mini-invasive pyeloplasty has some advantages compared to traditional open methods. In our experience, the robotic surgery was used only in 6 patients. The use of robotic surgery was related to the fact that in our institution we had the possibility to use the Da Vinci system for a 12-months-period. Robotic surgery in paediatric urology has been gained popularity since its introduction almost two decades ago, as it allows three-dimensional imaging, reduces surgeon’s tremor and involuntary movements and consents a more ergonomic position for the surgeon. As reported by several studies, robotic-assisted pyeloplasty is the most common procedure performed in paediatric urology [32, 33].
Our study does have some limitations. First of all, it has been conducted in a retrospective way with all the limits that a retrospective analysis can have, especially the lack of complete data. Moreover, we recognize that the comparison of 1 vs. 4 surgeons respectively for laparoscopic and open pyeloplasties may limit our results. Finally, we evaluated the success rate after operation only measuring the pelvic APD, without functional techniques. This limit depends on the fact that if the APD is clearly reduced after the operation we usually follow-up patients with serial ultrasound evaluations, while scintigraphy or fMRU are usually used in the doubt of persisting obstruction.
Conclusions
In hydronephrosis with CV, the Hellstrom VH could be considered a good surgical option, but only if the pre-operative and post-operative anatomical and functional assessments have been well studied. Mini-invasive and open pyeloplasties in the pediatric population have comparable success rate, with a significant difference about the length of hospital stay. In our opinion, the laparoscopic and robotic-assisted surgeries should be preferred.
Abbreviations
- UPJO:
-
Ureteropelvic junction obstruction
- UPJ:
-
Ureteropelvic junction
- CV:
-
Crossing vessel
- DP:
-
Dismembered pyeloplasty
- NDP:
-
Non dismembered pyeloplasty
- APD:
-
Antero-posterior diameter
- US:
-
Ultrasound
- fMRU:
-
Functional magnetic resonance urography
References
Ellerkamp V, Kurth RR, Schmid E, Zundel S, Warmann SW, Fuchs J (2016) Differences between intrinsic and extrinsic ureteropelvic junction obstruction related to crossing vessels: histology and functional analyses. World J Urol 34(4):577–583
Zhang PL, Peters CA, Rosen S (2000) Uretero-pelvic junction obstruction: morphological and clinical studies. PediatrNephrol 14:820–826
Stephens FD (1982) Uretero-vascular hydronephrosis and the aberrant renal vessel. J Urol 128:984e7
Tekgül S, Dogan HS, Erdem E, Hoebeke P, Ko˘cvara R, Nijman JM, Radmayr C, Silay MS, Stein R, Undre S (2016) Guidelines on pediatric urology. https://uroweb.org/wp-content/uploads/23-Paediatric-Urology_LR_full.pdf Accessed 19 Aug 2016
Capello SA et al (2005) Prenatal ultrasound has led to earlier detection and repair of ureteropelvic junction obstruction. J Urol 174(4 Pt 1):1425–1428
Sanna-Cherchi S, Ravani P, Corbani V et al (2009) Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int 76:528–533
Nef S, Neuhaus T, Spartà G et al (2016) Outcome after prenatal diagnosis of congenital anomalies of the kidney and urinary tract. Eur J Pediatr 175:667–676
Thomas DFM (2008) Prenatally diagnosed urinary tract abnormalities: long term outcome. Semin Fetal Neonatal Med 13:189–195
Uy N, Reidy K (2016) Developmental genetics and congenital anomalies of the kidney and urinary tract. J Pediatr Genet 5:51–60
Anderson JC, Hynes W (1949) Retrocaval ureter; a case diagnosed pre-operatively and treated successfully by a plastic operation. Br J Urol 21(3):209–214
Mei H, Pu J, Yang C, Zhang H, Zheng L, Tong Q (2011) Laparoscopic versus open pyeloplasty for ureteropelvic junction obstruction in children: a systematic review and meta-analysis. J Endourol 25(5):727–736
Hellström J, Giertz G, Lindblom K (1949) Pathogenesis and treatment of hydronephrosis. In: Presentedat VIII Congreso de la Sociedad International de Urologia, Paris, France
Chiarenza SF, Bleve C, Fasoli L, Battaglino F, Bucci V, Novek S, Zolpi E (2016) Ureteropelvic junctionobstruction in children by polarvessels. Is laparoscopic vascular hitching procedure a good solution? Single center experience on 35 consecutive patients. J Pediatr Surg 51(2):310–314
Madec FX, Faraj S, Villemagne T, Fourcade L, Lardy H, Leclair MD (2016) Laparoscopic transposition of lower-pole crossing vessels: long-term follow-up of 33 patients at puberty. J Pediatr Urol 12(4):226.e1-6
Chapman TL (1959) Urology in outline. Churchill Livingstone, Edimburgh, London, p 82
Schneider A, Ferreira CG, Delay C, Lacreuse I, Moog R, Becmeur F (2013) Lower pole vessels in children with pelviureteric junction obstruction: laparoscopic vascular hitch or dismembered pyeloplasty? J Pediatr Urol 9(4):419–423
Nerli RB, Reddy MN, Jali SM, Hiremath MB (2014) Preliminary experience with laparoscopic Foley's YV plasty for ureteropelvic junction obstruction in children. J Minim Access Surg 10(2):72–75
Baldwin DD, Dunbar JA, Wells N, McDougall EM (2003) Single-center comparison of laparoscopic pyeloplasty, acuciseendopyelotomy, and open pyeloplasty. J Endourol 17(3):155–160
Salö M, Sjöberg Altemani T, Anderberg M (2016) Pyeloplasty in children: perioperative results and long-term outcomes of robotic-assisted laparoscopic surgery compared to open surgery. PediatrSurg Int 32(6):599–607
Weiss DA, Kadakia S, Kurzweil R, Srinivasan AK, Darge K, Shukla AR (2015) Detection of crossing vessels in pediatric ureteropelvic junction obstruction: clinical patterns and imaging findings. J Pediatr Urol 11(4):173.e1-5
Cancian M, Pareek G, Caldamone A, Aguiar L, Wang H, Amin A (2017) Histopathology in ureteropelvic junction obstruction with and without crossing vessels. Urology 107:209–213
Rooks VJ, Lebowitz RL (2001) Extrinsic ureteropelvic junction obstruction from a crossing renal vessel: demography and imaging. Pediatr Radiol 31(2):120–124
Calisti A, Perrotta ML, Oriolo L, Patti G, Marrocco G, Miele V (2003) Functional outcome after pyeloplasty in children: impact of the cause of obstruction and of the mode of presentation. Eur Urol 43(6):706–710
Chiarenza SF, Bleve C, Caione P, Escolino M, Nappo SG, Perretta R, La Manna A, Esposito C (2017) Minimally invasive treatment of pediatric extrinsic ureteropelvic junction obstruction by crossing polar vessels: is vascular hitching a definitive solution? report of a multicenter survey. J Laparoendosc Adv Surg Tech A 27(9):965–971
Villemagne T, Fourcade L, Camby C, Szwarc C, Lardy H, Leclair MD (2015) Long-term results with the laparoscopic transposition of renal lower pole crossing vessels. J Pediatr Urol 11(4):174.e1–7
Miranda ML, Pereira LH, Cavalaro MA, Pegolo PC, de Oliveira-Filho AG, Bustorff-Silva JM (2015) Laparoscopic transposition of lower pole crossing vessels (Vascular Hitch) in children with pelviureteric junction obstruction: how to be sure of the success of the procedure? J Laparoendosc Adv Surg Tech A 25(10):847–851
Mattioli G, Avanzini S, Pio L, Costanzo S, Faticato MG, Montobbio G, Disma N, Buffa P (2015) Transperitoneal laparoscopic approach to the perinephric area in children: technical report and lessons learned. J Laparoendosc Adv Surg Tech A 25(10):841–846
Rehman J, Landman J, Sundaram C, Clayman RV (2001) Missed anterior crossing vessels during open retroperitoneal pyeloplasty: laparoscopic transperitoneal discovery and repair. J Urol 166:593–596
Godbole P, Mushtaq I, Wilcox DT, Duffy PG (2006) Laparoscopic transposition of lower pole vessels–the 'vascular hitch': an alternative to dismembered pyeloplasty for pelvi-ureteric junction obstruction in children. J Pediatr Urol 2(4):285–289
Gatti JM, Amstutz SP, Bowlin PR, Stephany HA, Murphy JP (2017) Laparoscopic vs open pyeloplasty in children: results of a randomized, prospective. Controlled Trial J Urol 197(3 Pt 1):792–797
Gadelmoula M, Abdel-Kader MS, Shalaby M, Abdelrazek M, Moeen AM, Zarzour MA, Mohammed N, Fornara P (2018) Laparoscopic versus open pyeloplasty: a multi-institutional prospective study. Cent Eur J Urol 71(3):342–345
Andolfi C, Adamic B, Oommen J et al (2019) Robot-assisted laparoscopic pyeloplasty in infants and children: is it superior to conventional laparoscopy? World J Urol. https://doi.org/10.1007/s00345-019-02943-z
Morales-López RA, Pérez-Marchán M, Pérez BM (2019) Current concepts in pediatric robotic assisted pyeloplasty. Front Pediatr 7:4
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wong, M.C.Y., Palo, F., Fiorenza, V. et al. Uretero-pelvic junction obstruction with and without crossing vessels: surgical outcome in a single center experience. J Ped Endosc Surg 2, 103–109 (2020). https://doi.org/10.1007/s42804-020-00055-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42804-020-00055-9