Abstract
Purpose
In children, ureteropelvic junction obstruction (UPJO) is mostly caused by intrinsic factors (IUPJO); extrinsic UPJO are rare and often due to crossing vessels (CVs).
Methods
We retrospectively reviewed all data of children with UPJO that underwent surgery in our institution from 2004 to 2011. Analyses included age at surgery, gender, preoperative and postoperative results of ultrasound and renal scans [differential renal function (DRF); signs of obstruction], and pathology reports. Available histological specimens of cases with CV were compared to a random selection of intrinsic cases in a blinded fashion. After additional Masson’s trichrome staining, the specimens were scored for fibrosis, muscular hypertrophy, and chronic inflammation.
Results
Out of 139 patients with UPJO, 39 cases were associated with CV. Median age at surgery was 68 months (range 2–194) in the CV group and 11.5 months (range 0–188) in IUPJO group. Laparoscopic dismembered pyeloplasty (LDMP) was carried out in 134 and open DMP in five patients. Preoperative ultrasound identified 28/39 cases with CV. DRF below 40 % was more frequently seen in CV patients (p = 0.020). Histological analyses revealed no differences between the CV and IUPJO specimens in total. CV patients with higher grades of muscular hypertrophy had lower preoperative DRF, compared to those with higher preoperative DRF (p = 0.026). Functional recovery after (L)DMP was excellent in both groups.
Conclusion
We could not find any significant histological differences between CV and IUPJO in children. To obtain excellent functional recovery, surgical procedures with a definite correction of the UPJ should be preferred in paediatric patients with CV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
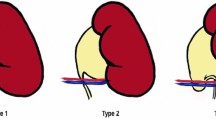
Most cases of ureteropelvic junction obstruction (UPJO) in children are caused by intrinsic factors (IUPJO), such as an aperistaltic ureteral segment, infoldings of the ureteral wall or true strictures. Differing histological changes in the constricted segment in relation to outcome and differential renal function (DRF) or degree of obstruction have been described [1–6]. The rare cases of extrinsic UPJO in children are due to fibrous bands or crossing vessels (CVs). These vessels may arise from the renal vessels, aorta, vena cava, or iliac vessels that supply the lower pole of the kidney. CVs are found in 20 % of adult patients with normal UPJ and in up to 38–71 % in patients with UPJO, whether causative or coincidental [7, 8]. Treatment of choice is surgery in case of flank pain, loss of DRF, or relevant obstruction in dynamic renal scans. The dismembered pyeloplasty (DMP) is the gold standard to successfully treat both intrinsic and extrinsic UPJO in children; recently published reports proved comparable results for laparoscopic, one trocar-assisted, or robotic-assisted dismembered pyeloplasty (LDMP, OTAP, RDMP), even in small infants [9, 10]. Furthermore, in adults, nondismembered pyeloplasty (YV-plasty) and DMP have gained advantage over laser pyelotomies in extrinsic UPJO [11].
However, in cases with crossing vessels, some authors promote vascular hitch procedures in order to avoid dissection and anastomosis of the ureteropelvic junction [12, 13]. Cases of failed vascular hitch and redo surgery with DMP or endopyelotomy have been described [14, 15]. The aim of this study was to compare clinical, functional, and histological aspects of IUPJO and UPJO–CV.
Methods
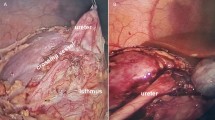
We retrospectively analysed all patients undergoing dismembered pyeloplasty (DMP) in our department between 2004 and 2011. Preoperative assessment consisted of colour Doppler ultrasound (US) and diuretic renal 99mTc-MAG3-scan (DRS). Indications for surgery were: significant impairment of differential renal function (DRF, below 40 %); more than 10 % loss of DRF in follow-up DRS; signs of obstruction in DRS with less than 50 % tracer clearance 20 min after furosemide application (TC20 min%); and half-time tracer clearance (½TC) over 20 min after furosemide application. LDMP was performed as previously described [16],
Postoperative follow-up included clinical evaluation once a year as well as DRS and colour Doppler ultrasound (US) after 3 months. Cases with IUPJO and UPJO–CV were compared regarding age, gender, pre- and postoperative courses, pre- and postoperative DRFs, TC20 min%, and reoperations.
For histopathologic comparison, first, the histological reports were compared concerning mention of fibrosis, muscular hypertrophy, and signs of chronic infection. Furthermore, the available histological haematoxylin- and eosin (HE)-stained specimens of cases with CV (24 specimens) were compared to a randomly selected control group of IUPJO (26) specimens. Additionally, a Masson’s trichrome (MT) staining was realized for better assessment of fibrosis (Fig. 1). The specimens were graded for fibrosis, muscular hypertrophy, and inflammation from 0 to 3, as follows: grade 0: no alterations; grade 1: mild alterations; grade 2: moderate alterations; and grade 3: severe alterations. The stained sections were examined by light microscopy and rated independently by two observers blinded to patient information and to each other. To assess intraobserver variability, the same observers performed each method again without knowing the initial data. In case of incongruent results, specimens were rejected from the study. The project was approved by the Independent Ethics Committee (IEC, Project No. 566/2014R).
Statistical analysis was performed using SPSS version 22.0. Shapiro–Wilk test, and D’Agostino’s K-squared test was performed to proof for parametric distribution. Descriptive statistics show the median, interquartile range (IQR) of nonparametric data, and mean and standard deviation (SD) of parametric data. For nonparametric data differences between patient’ demographics and for correlation of DRF/TC20 min% with histological results, a two-sided Mann–Whitney U test was used. Contingency analyses were performed to calculate differences between histological aspects using a two-sided Fisher’s exact test. Significance was assumed for p below 5 % (*). Because the number of cases was not high enough, equivalence tests concerning the histological findings were not possible.
Results
From 2004 to 2011, 139 patients (102 males, 73.4 %) were operated on because of UPJO. In 83 cases (59.7 %), UPJO was located on the left side; in 4 cases, it was bilateral (2.9 %, CI 0.7–7.2). The clinical and disease-specific characteristics of our study population are listed in Table 1. The median follow-up period was 37 months (12–190). In 134 patients, a laparoscopic dismembered pyeloplasty (LDMP) was carried out, in three of them on both sides. In five patients, an open DMP was performed. These latter patients (median age 2.5 months, IQR 0–3 months, 1 case with CV) were operated on open during our early observation period (2005) when our experience in laparoscopy in small infants was still growing. During surgery, CVs were associated with obstruction in 39 cases (28.1 %). The remaining 100 patients had IUPJO. Preoperative ultrasound identified 28 cases of the 39 CV cases; in 11 cases, CV was not described in preoperative ultrasound reports. In the IUPJO cases, ultrasound reports described CV in 12 cases that were not verified intraoperatively. This means a sensitivity of 71 %, a specificity of 88 %, a positive predictive value of 70 %, a negative predictive value of 88 %, and an accuracy of 84 % of US for depicting CV in our institution. There was no significant difference between the groups concerning the median DRF before and after surgery. However, focusing on preoperative DRF below 40 %, there were significantly more patients in the group of CV (p = 0.020). Postoperatively, this difference was no longer evident. There was no difference between patients with CV and IUPJO regarding signs of obstruction as expressed in preoperative TC20 min%. However, in the CV group, the obstruction recovery was significantly higher than in the IUPJO group (p = 0.030). Reoperation (re-LDMP) for re-stenosis was necessary in three cases (2.1 %) after 5, 6, and 24 months, respectively. In two patients (LDMP, IUPJO), complete loss of renal function (patient 1, early postoperative peritonitis, sepsis, and renal tubular necrosis; patient 2, prolonged loss of renal function after 5 years) led to nephrectomy (1.4 %). There was no significant difference between CV and IUPJO cases.
Standard pathological results were available in 132 cases. In these, there was no difference between the groups (Table 1). Out of 39 cases with CV, 26 histopathologic specimens were available for evaluation. These were compared to a randomly picked cohort of 26 IUPJO specimens. Because of incongruent findings in two specimens of the CV group, these cases were excluded from further histological evaluation. The clinical and disease-specific characteristics of the subgroup are listed in Table 2. Grading of HE and MT-stained specimen for fibrosis, muscular hypertrophy, and chronic inflammation did not reveal any difference between CV and IUPJO (Table 2).
Differing between lower (0–1) and higher (2–3) grades of muscular hypertrophy, higher grades of muscular hypertrophy had significantly lower preoperative DRF in CV cases (p = 0.026) and significantly lower preoperative TC20 min% in IUPJO cases (p = 0.030). Details are shown in Table 3. In the postoperative analyses, there were no such differences.
Discussion
There is still an ongoing discussion whether CVs are even able to cause UPJO or whether they become trapped by an expanding renal pelvis in patients with intrinsic obstruction [17]. IUPJO is often diagnosed very early in live or even prenatally due to the widespread use of prenatal ultrasound. CV cases present at an older age [18]. Our findings confirm the late presentation of CV. Although the reliability of US has greatly improved with higher technical resolution, in our cohort the correlation between CV and preoperative US in intraoperative findings was not as good as described in other reports and the US reliability did not improve over the years [19].
Based on the fact that a CV exists from the beginning, but starts to present varying symptoms sometimes later in life, it is an important consideration of how the development of the ureteral wall is impaired by a pulsating and compressing CV. In theory, the alterations of the ureteropelvic segment caused by a CV are part of an individually ongoing process, depending on how long and how high the affecting pressure by the vessel is. One of our more recent cases with CV showed persistent signs of severe obstruction after a vascular hitch procedure. After secondary LDMP, the resected ureteral specimen showed histological signs of intrinsic stenosis (muscular hypertrophy and fibrosis). Comparable cases of failed vascular hitch and redo surgery have been previously described [14, 15]. In IUPJO, differing findings of histopathologic changes have been described: increased intermuscular and intramuscular connective tissue, or increased collagen that acts as an inelastic collar hampering ureteral peristalsis [1, 6]. Alterations of innervation [20, 21], muscular hypotrophy [2, 3], or hypertrophy have also been reported [4] as causative or resulting alterations of the ureteral wall. Surprisingly, in our reviewed CV specimens, we did not find any lower scores for the so-called intrinsic alterations such as muscular hypertrophy, fibrosis, and chronic inflammation. Only few other reports compared histomorphological aspects of ureteral segments in IUPJO with those of CV patients [22–25]. In most of them, significant differences between IUPJO and CV specimens have been described with fewer or even no intrinsic alterations of the ureteral wall in CV patients [23–25]. However, studies were limited because of very low numbers of analysed patients (four–nine patients) [23, 25] or did not deal with paediatric patients [23, 24]. Other limitations were the lack of grading the pathologic features [24]. One study observed findings similar to our results with muscular hypertrophy in two-thirds and muscle atrophy in one-third of all cases [22].
While the exact pathogenetical mechanisms of intrinsic obstruction remain unclear, some correlations of histopathologic findings with the grade of obstruction or renal impairment have been previously described: a lower collagen-to-muscle ratio was associated with a better renal function recovery after surgery [3]. Decreased preoperative DRF in children younger than 12 months was associated with higher grades of muscular hypertrophy and fibrosis; a postoperative significant recovery of DRF correlated with higher grades of inflammation [5]. We also found significantly lower preoperative DRF in CV patients with higher grades of muscular hypertrophy, respectively, lower preoperative TC20 min% in IUPJO patients in association with higher grades of fibrosis.
The findings of a higher amount in the CV patients with more severe impairment of preoperative DRF (below 40 %) and higher grades of muscular hypertrophy in CV patients with lower DRF should be of great interest in further studies.
Our study provides data of functional recovery concerning both DRF and obstruction not only 3 months but also 1 year after surgery. Whereas there are several reports, meta-analyses, and even one Cochrane review concerning the safeness and effectiveness of laparoscopic or robotic-assisted dismembered pyeloplasty in children [26], and the advantage of definitive procedure like NDMP and DMP over endopyelotomies in adults with extrinsic UPJO [11], only few reports about vascular hitch procedures in children are available (Table 4) [12, 27–33]. However, even in some of these reports, the analysed patient’ cohorts consisted of mixed ages—children and adults [12, 29, 30]. In most of these studies, functional recovery was defined as recovery of obstruction in renal scans. One study described the poorer outcome of CV patients compared to IUPJO after YV-plasty or retroperitoneal DMP [Subotic], but did not give information about DRF and obstruction recovery rates in detail. However, only one study mentioned the DRF recovery rate after vascular hitch with a rate of only 21 % [12]. We could show that LDMP offers an appropriate therapy in children with CV with high rates of functional recovery, especially DRF recovery of 87.7 %. Taking together reports on failed vascular hitch procedures [14, 15], missing information about DRF recovery after vascular hitch procedures in children, and our current findings of “intrinsic” histopathologic changes in CV patients, we favour pyeloplasty as standard procedure for both extrinsic and intrinsic UPJO in children.
In conclusion, our data revealed no significant differences between CV and IUPJO patients concerning the pathologic features of fibrosis, muscular hypertrophy, and inflammation in paediatric patients. Functional impairment is worse in cases with higher grades of fibrosis and muscular hypertrophy. Functional recovery after LDMP is excellent in both groups.
References
Notley RG (1968) Electron microscopy of the upper ureter and the pelvi-ureteric junction. Br J Urol 40(1):37–52
Kaneto H, Orikasa S, Chiba T, Takahashi T (1991) Three-D muscular arrangement at the ureteropelvic junction and its changes in congenital hydronephrosis: a stereo-morphometric study. J Urol 146(3):909–914
Kim WJ, Yun SJ, Lee TS, Kim CW, Lee HM, Choi H (2000) Collagen-to-smooth muscle ratio helps prediction of prognosis after pyeloplasty. J Urol 163(4):1271–1275
Hosgor M, Karaca I, Ulukus C, Ozer E, Ozkara E, Sam B, Ucan B, Kurtulus S, Karkiner A, Temir G (2005) Structural changes of smooth muscle in congenital ureteropelvic junction obstruction. J Pediatr Surg 40(10):1632–1636. doi:10.1016/j.jpedsurg.2005.06.025
Kiratli PO, Orhan D, Gedik GK, Tekgul S (2008) Relation between radionuclide imaging and pathologic findings of ureteropelvic junction obstruction in neonatal hydronephrosis. Scand J Urol Nephrol 42(3):249–256. doi:10.1080/00365590701874967
Kaya C, Bogaert G, de Ridder D, Schwentner C, Fritsch H, Oswald J, Radmayr C (2010) Extracellular matrix degradation and reduced neural density in children with intrinsic ureteropelvic junction obstruction. Urology 76(1):185–189. doi:10.1016/j.urology.2009.09.097
Zeltser IS, Liu JB, Bagley DH (2004) The incidence of crossing vessels in patients with normal ureteropelvic junction examined with endoluminal ultrasound. J Urol 172(6 Pt 1):2304–2307
Boylu U, Oommen M, Lee BR, Thomas R (2009) Ureteropelvic junction obstruction secondary to crossing vessels-to transpose or not? The robotic experience. J Urol 181(4):1751–1755. doi:10.1016/j.juro.2008.11.114
Chang SJ, Hsu CK, Hsieh CH, Yang SS (2015) Comparing the efficacy and safety between robotic-assisted versus open pyeloplasty in children: a systemic review and meta-analysis. World J Urol. doi:10.1007/s00345-015-1526-3
Lima M, Ruggeri G, Messina P, Tursini S, Destro F, Mogiatti M (2015) One-trocar-assisted pyeloplasty in children: an 8-year single institution experience. Eur J Pediatric Surg 25(3):e1. doi:10.1055/s-0034-1394280
Rassweiler JJ, Subotic S, Feist-Schwenk M, Sugiono M, Schulze M, Teber D, Frede T (2007) Minimally invasive treatment of ureteropelvic junction obstruction: long-term experience with an algorithm for laser endopyelotomy and laparoscopic retroperitoneal pyeloplasty. J Urol 177(3):1000–1005. doi:10.1016/j.juro.2006.10.049
Pesce C, Campobasso P, Costa L, Battaglino F, Musi L (1999) Ureterovascular hydronephrosis in children: Is pyeloplasty always necessary? Eur Urol 36(1):71–74. doi:10.1159/000019930
Sakoda A, Cherian A, Mushtaq I (2011) Laparoscopic transposition of lower pole crossing vessels (‘vascular hitch’) in pure extrinsic pelvi-ureteric junction (PUJ) obstruction in children. BJU Int 108(8):1364–1368. doi:10.1111/j.1464-410X.2011.10657.x
Nerli RB, Jayanthi VR, Reddy M, Koura A (2009) Pelvi-ureteric junction obstruction with crossing renal vessels: a case report of failed laparoscopic vascular hitch. J Pediatr Urol 5(2):147–150. doi:10.1016/j.jpurol.2008.09.009
Janetschek G, Peschel R, Altarac S, Bartsch G (1996) Laparoscopic and retroperitoneoscopic repair of ureteropelvic junction obstruction. Urology 47(3):311–316. doi:10.1016/s0090-4295(99)80444-0
Fuchs J, Luithle T, Warmann SW, Haber P, Blumenstock G, Szavay P (2009) Laparoscopic surgery on upper urinary tract in children younger than 1 year: technical aspects and functional outcome. J Urol 182(4):1561–1568. doi:10.1016/j.juro.2009.06.063
Gupta M, Smith AD (1998) Crossing vessels. Endourologic implications. Urol Clin N Am 25(2):289–293
Dewan PA, Ng KP, Ashwood PJ (1998) The relationship of age to pathology in pelviureteric junction obstruction. J Paediatr Child Health 34(4):384–386
Veyrac C, Baud C, Lopez C, Couture A, Saguintaah M, Averous M (2003) The value of colour Doppler ultrasonography for identification of crossing vessels in children with pelvi-ureteric junction obstruction. Pediatr Radiol 33(11):745–751. doi:10.1007/s00247-003-1012-8
Wang Y, Puri P, Hassan J, Miyakita H, Reen DJ (1995) Abnormal innervation and altered nerve growth factor messenger ribonucleic acid expression in ureteropelvic junction obstruction. J Urol 154(2 Pt 2):679–683
Harish J, Joshi K, Rao KL, Narasimhan KL, Samujh R, Choudhary SK, Mahajan JK (2003) Pelviureteric junction obstruction: how much is the extent of the upper ureter with defective innervation needing resection? J Pediatr Surg 38(8):1194–1198
Foote JW, Blennerhassett JB, Wiglesworth FW, Mackinnon KJ (1970) Observations on the ureteropelvic junction. J Urol 104(2):252–257
Murakumo M, Nonomura K, Yamashita T, Ushiki T, Abe K, Koyanagi T (1997) Structural changes of collagen components and diminution of nerves in congenital ureteropelvic junction obstruction. J Urol 157(5):1963–1968
Richstone L, Seideman CA, Reggio E, Bluebond-Langner R, Pinto PA, Trock B, Kavoussi LR (2009) Pathologic findings in patients with ureteropelvic junction obstruction and crossing vessels. Urology 73(4):716–719. doi:10.1016/j.urology.2008.10.069 (discussion 719)
Yiee JH, Johnson-Welch S, Baker LA, Wilcox DT (2010) Histologic differences between extrinsic and intrinsic ureteropelvic junction obstruction. Urology 76(1):181–184. doi:10.1016/j.urology.2010.02.007
Mei H, Pu J, Yang C, Zhang H, Zheng L, Tong Q (2011) Laparoscopic versus open pyeloplasty for ureteropelvic junction obstruction in children: a systematic review and meta-analysis. J Endourol 25(5):727–736 (Provisional abstract)
El-Ghoneimi A, Farhat W, Bolduc S, Bagli D, McLorie G, Aigrain Y, Khoury A (2003) Laparoscopic dismembered pyeloplasty by a retroperitoneal approach in children. BJU Int 92(1):104–108 (discussion 108)
Godbole P, Mushtaq I, Wilcox DT, Duffy PG (2006) Laparoscopic transposition of lower pole vessels—the ‘vascular hitch’: an alternative to dismembered pyeloplasty for pelvi-ureteric junction obstruction in children. J Pediatr Urol 2(4):285–289. doi:10.1016/j.jpurol.2005.11.017
Gundeti MS, Reynolds WS, Duffy PG, Mushtaq I (2008) Further experience with the vascular hitch (laparoscopic transposition of lower pole crossing vessels): an alternate treatment for pediatric ureterovascular ureteropelvic junction obstruction. J Urol 180(4 Suppl):1832–1836. doi:10.1016/j.juro.2008.05.055 (discussion 1836)
Nouralizadeh A, Simforoosh N, Basiri A, Tabibi A, Soltani MH, Kilani H (2010) Laparoscopic management of ureteropelvic junction obstruction by division of the aberrant vein and cephalad relocation of the crossing artery: a long-term follow-up of 42 cases. J Endourol 24(6):987–991. doi:10.1089/end.2009.0524
Schneider A, Ferreira CG, Delay C, Lacreuse I, Moog R, Becmeur F (2013) Lower pole vessels in children with pelviureteric junction obstruction: laparoscopic vascular hitch or dismembered pyeloplasty? J Pediatr Urol 9(4):419–423. doi:10.1016/j.jpurol.2012.07.005
Singh RR, Govindarajan KK, Chandran H (2010) Laparoscopic vascular relocation: alternative treatment for renovascular hydronephrosis in children. Pediatr Surg Int 26(7):717–720. doi:10.1007/s00383-010-2623-4
Subotic S, Weiss H, Wyler S, Rentsch CA, Rassweiler J, Bachmann A, Teber D (2013) Dismembered and non-dismembered retroperitoneoscopic pyeloplasty for the treatment of ureteropelvic junction obstruction in children. World J Urol 31(3):689–695. doi:10.1007/s00345-012-0887-0
Author contribution
V. Ellerkamp, J. Fuchs: Protocol/project development; V. Ellerkamp, R.R. Kurth S. Zundel: Data collection or management; V. Ellerkamp, R. R. Kurth, E. Schmid: Data analysis; V. Ellerkamp, S. W. Warmann, E. Schmid: Manuscript writing/editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The project was approved by the Independent Ethics Committee (IRB-Votum, IEC, Project No. 566/2014R).
Rights and permissions
About this article
Cite this article
Ellerkamp, V., Kurth, R.R., Schmid, E. et al. Differences between intrinsic and extrinsic ureteropelvic junction obstruction related to crossing vessels: histology and functional analyses. World J Urol 34, 577–583 (2016). https://doi.org/10.1007/s00345-015-1645-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1645-x