Abstract
Congenital chylous ascites (CCA) is a rare condition where there is an accumulation of chyle in the peritoneal cavity. Primary CCA due to dysplastic lymphatics is the most common cause in children. CCA discovered on ventriculopertoneal (VP) shunt insertion following previous myelomeningocele repair has only been described in a single paper before with the authors recommending a VP shunt safe to be sited in the presence of CCA. In this paper, we present a case of CCA in a term neonate with a myelomeningocele and an imperforate anus who underwent the siting of a VP shunt with no adverse effect. We provide an alternative hypothesise suggesting the link between raised intra-abdominal pressure caused by the imperforate anus as the aetiological factor in CCA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital chylous ascites (CCA) is a rare disorder pertaining to the collection of chyle in the peritoneal cavity. The incidence of CCA is reported to be 1/20,000–1/187,000 live births [1]. Patient often present with vomiting, loss of appetite, increased abdominal circumference, respiratory compromise and signs of fluid in the peritoneal cavity such as genital oedema. CCA has been described as of primary or secondary aetiology. The primary disorder is thought to occur due to a dysplastic lymphatic systems leading to leakage of lymphatic fluid into the peritoneal cavity and is more common in children. Secondary causes are more common in adults but iatrogenic and non-accidental injury are the most common secondary causes in children. CCA can have serious effects to the new born including mechanical bowel disorder, immunological and nutritional deficit due to loss of proteins and lymphocytes and developmental delay. Both medical and surgical management options have been described with many favouring a staged approach [2].
Asymptomatic CCA discovered on opening of the peritoneal cavity for surgical procedures unrelated to gastrointestinal surgery is extremely rare. To date only three cases of CCA discovered upon opening of the peritoneum for a ventriculoperitoneal shunt (VP) have been described in literature.
Here we present a case of CCA in a term neonate with a myelomeningocele who underwent the siting of a VP shunt with no adverse effect.
Case Report
Baby AS was born to a 26-year-old Caucasian mother who was a non-smoker, did not drink any alcohol during pregnancy, and took folic acid supplementation during pregnancy. The mother had a gravidity of 6 and parity of 2 with no family history of spina-bifida. AS was delivered by planned caesarean section (CS) at a gestational age of 37+1 due to the known spina-bifida deformity from antenatal scans and weighed 2830 g. Routine new-born examination identified spontaneous upper limb movement. However the lower limbs were flexed with reduced spontaneous movements, but withdrawal from painful stimuli was noted. Further examination found a soft T11-L4 closed myelomeningocele of approximate 50 ml in volume with associated ventriculomegaly, an imperforate anus, a small muscular ventriculo-septal defect and an ectopic left kidney.
On day 2, with joint plastic surgery involvement, AS was taken to theatre and underwent the closure of the myelomeningocele in the standard fashion with a Z-plasty skin flap. The general surgical team also performed a colostomy following a failed primary anoplasty. AS made steady progress post-operatively but examination revealed flaccid lower limbs with no antigravity movement or response to pain. Over the next 12 days, there was progressive increase in the occipitofrontal circumference (OFC) with crossing over the 50th centile mark. AS was taken to theatre 11 days after his initial myelomeningocele closure for a VP shunt placement. Upon opening of the peritoneum, a yellow milky fluid discharge was noted. Approximately 20 ml leaked out the cavity and a further 30 ml remained in the peritoneal cavity. A mini-laparotomy was performed and examination revealed no bowel or gastric perforation. The distal shunt catheter was inserted, and the VP shunt placement was undertaken with an adjustable valve system. Cytological tests on the intra-abdominal fluid revealed no pus cells, and microbiological tests yielded no bacterial growth. Based on the appearance of the fluid together with the cytological and microbiological tests, it was thought that this fluid represented chylous ascites. Post-operatively the patient did well and was discharged from neurosurgery with planned outpatient follow-up.
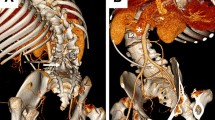
Over the next 12 months, the patients OFC remained static on the 50th centile mark. AS also had one presentation to neurosurgery at 3 months post-VP shunt insertion with anorexia and sunken fontanels. It was thought the shunt maybe over-draining, and the valve was adjusted accordingly with good clinical response. An MRI at 8 months showed a type 2 Chiari malformation, atrophy of the thoracic cord and dilatation of the central canal at C7-T3 that was being managed conservatively (Fig. 1).
Discussion
Chylous ascites is a condition where there is a failure of the absorption of chyle into the lymphatic system. Various theories have been suggested as to the pathophysiology of this condition including primary and secondary causes. Primary chylous ascites is thought to occur as a result of de-novo abnormalities such as lymphagiectasia, mesenteric cysts or lymphatic hypoplasia/malformation as seen in conditions such as Turners syndrome, yellow nail syndrome and Klippel-Trenaunay syndrome and is more common in children. The presence of dysplastic lymphatic seen in genetic syndromes and in children of related parents also points to a genetic basis of the pathogenesis. Secondary causes are more common in adults and include malignancy, trauma, infection, heart or liver failure and iatrogenic causes [2].
Cases of chylous ascites following abdominal, retroperitoneal and cardiothoracic surgery have been described in literature, but incidental chylous ascites found following spinal procedures is very rare [3]. A single case series in the American Journal of Neurosurgery reported 3 cases where milky brown fluid was found upon opening of the peritoneum during insertion of VP shunts that was preceded by myelomeningocele repair 2–3 days previously [4]. The authors theorised that closure of the myelomeningocele caused raised intra-abdominal pressure, which may have led to the chylous ascites. Our case would support the findings of the report and support the causal linkage suggested between myelomeningocele repair and finding of chylous ascites. However we also noted that our patient had an imperforate anus, which undoubted would have led to gastrointestinal stasis and backpressure. One could theorise that this could also lead to raised intra-abdominal pressure causing venous hypertension and lymphatic flow obstruction and thus leading to leakage of lymphatic fluid into the peritoneal cavity causing CCA rather than the chylous ascites being a consequence of the myelomeningocele repair. This would be also be supported by reports of chylous ascites being the main manifestation of portal hypertension due to asymptomatic left ventricular failure and reports of spinal procedures causing chyloretroperitoneum rather than chylous ascites [5]. We do not know if the patients described in the report by Stubbs et al. had any congenital gastrointestinal malformations that could support our theory.
The authors also suggested that upon finding of chylous ascites, it is still appropriate to proceed and site a VP shunt. Our case also demonstrates that chylous ascites is not a contraindication to the placement of a VP shunt as we found that the presence of chylous ascites did not alter the functioning of the VP shunt nor did it increase the risk of infection.
Conclusion
CCA is a rare and not a contraindication to VP shunt placement. Knowledge of this is vital to prevent delay of shunt placement and multiple unnecessary procedures. The aetiology of CCA is multifactorial, and we present a hypothesis suggesting venous congestion secondary to anorectal abnormalities leading to raised intra-abdominal pressure as an aetiological factor for CCA.
References
Albaghdady A, El-Asmar KM, Moussa M, Abdelhay S. Surgical management of congenital chylous ascites. Ann Pediatr Surg. 2018;14(2):56–9.
Bhardwaj R, Vaziri H, Gautam A, Ballesteros E, Karimeddini D, Wu GY. Chylous Ascites: A review of pathogenesis, diagnosis and treatment. J Clin Translat Hepatol. 2018;6(1):105–13.
Göçmen A, Avcı ME, Şanlıkan F, Uçar MG. Four cases of chylous ascites following robotic gynecologic oncological surgery. Case Rep Obstet Gynecol. 2014;2014.
Tubbs RS, Tyler-Kabara EC, Wellons JC, Blount JP, Oakes WJ. Unusual findings during abdominal placement of a ventriculoperitoneal shunt: report of three cases. J Neurosurg Pediatr. 2005;102(4):423–5.
Su IC, Chen CM. Spontaneous healing of retroperitoneal chylous leakage following anterior lumbar spinal surgery: a case report and literature review. Eur Spine J. 2007;16(3):332–7.
Availability of data and material
Not applicable
Code availability
Not applicable
Funding
This work has not been funded by any bodies.
Author information
Authors and Affiliations
Contributions
All authors have contributed to this project and approve of the final version.
Corresponding author
Ethics declarations
Ethics approval
Not applicable
Consent for publication
The next of kin/guardian has given written informed consent to the submission of the case report for publication.
Patient Consent
The next of kin/guardian has consented to the submission of the case report for submission to the journal.
Conflict of Interest
The authors declare that there is no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery
Rights and permissions
About this article
Cite this article
Shumon, S., Reehal, R., ElGhamry, A. et al. A case report: Ventriculo-peritoneal Shunt in the Presence of Chylous Ascites—Is It Safe?. SN Compr. Clin. Med. 3, 1682–1684 (2021). https://doi.org/10.1007/s42399-021-00907-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00907-2