Key summary points
To explore the longitudinal association between body mass index categories and falls risks in community-dwelling men and women aged ≥ 50 years in the cross-national Survey of Health, Ageing and Retirement in Europe (SHARE).
AbstractSection FindingsUnderweight and obese participants had a higher falls risk, compared to those with normal weight. These associations were independent of age, self-rated health, previous falls, comorbidities and medications.
AbstractSection MessageThe relationship between body mass index and falls risk in adults is U-shaped; both underweight and obesity are associated with increased falls risk, compared to normal weight.
Abstract
Purpose
To investigate the longitudinal associations between body mass index (BMI) categories and falls risk in men and women.
Methods
Prospective cohort study using data from 50,041 community-dwelling adults aged ≥ 50 years assessed in Wave 6 and 7 in the cross-national Survey of Health, Ageing and Retirement in Europe (SHARE). Socio-demographic and clinical factors were assessed at baseline (Wave 6). Functional impairment was defined by any limitations in activities of daily living (ADL) or instrumental ADL (IADL). Participants were classified as underweight, normal weight, overweight or obese at baseline. At 2-year follow-up (Wave 7), falls in the previous six months were recorded. The longitudinal associations between BMI categories and falls were analysed by binary logistic regression models; odds ratios (OR) and 95% confidence intervals (CI) were calculated. All analyses were adjusted for socio-demographic and clinical factors. Furthermore, analyses were stratified by sex, age and functional impairment.
Results
Mean age was 67.0 years (range 50–102); 28,132 participants were women; 4057 (8.1%) participants reported falls at follow-up. Participants had an increased falls risk [OR (95% CI)] if they were underweight [1.41 (1.06–1.88), p = 0.017] or obese [1.20 (1.09–1.32), p < 0.001] compared to those with normal weight. The association of underweight and obesity with increased falls risk was consistent in participants aged ≥ 65 years. In participants with functional impairment, underweight was associated with higher falls risk [1.61 (1.09–2.40), p = 0.018], while obesity was not.
Conclusion
A U-shaped relationship between BMI and falls risk was found in community-dwelling adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Controversy persists on the association between body mass index (BMI) categories—underweight, normal weight, overweight and obesity—and falls risk in adults [1,2,3,4,5,6,7,8,9]. Previous literature has yielded conflicting results, with some studies suggesting no consistent association [1,2,3], or an association between overweight or obesity and increased risk [4,5,6,7] or a U-shaped association, with both underweight and obesity being associated with increased risk [8, 9]. Furthermore, the U-shaped association was reported only by cross-sectional studies; it is also unknown whether functional status may modulate it.
Falls in adults are a serious public health issue [10,11,12,13]. About one in three community-dwelling adults older than 65 years fall each year [10, 11] and one in ten falls results in a major injury [12]; women may be at higher risk for falls and injurious falls, compared to men [9, 14,15,16]. Even non-injurious falls can lead to fear of falling, reduced quality of life, loss of confidence and independence [17]. Falls are associated with increased morbidity, mortality and healthcare costs [18, 19]. Therefore, preventing falls by identifying their potentially reversible risk factors is crucial. Moreover, targeting risk factors that are commonly present among the general population may be of benefit for many adults. Indeed, obesity is highly prevalent among adults worldwide [20]; one in three adults in the US and one in five adults in Europe is obese [21, 22]. Both underweight and obesity can be effectively treated in older adults, through lifestyle changes, diet, pharmacological or other treatment [23, 24].
This study aims to explore the longitudinal associations between BMI categories and falls in community-dwelling middle-aged and older men and women in the cross-disciplinary longitudinal Survey of Health, Ageing and Retirement in Europe (SHARE). It also aims to explore whether these associations may be modulated by sex, age and functional status.
Methods
Study design and population
This was a prospective study based on data from the Survey of Health, Ageing and Retirement in Europe (SHARE). SHARE is a multidisciplinary and cross-national panel database of micro data on health, socio-economic status and social and family networks of individuals aged 50 years and older in European countries and Israel [25]. SHARE started in 2004 and comprises eight biennial survey waves. In the present study, we used data from Wave 6 (fieldwork in 2015) and 7 (fieldwork mainly in 2017).
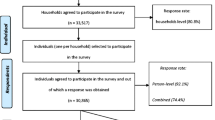
Figure 1 presents the flow-chart of this study inclusion criteria. A total of 68,186 participants had a main interview at Wave 6 (baseline); of these, 64,660 participants were aged 50 years and older and had complete data of interest at baseline. We further excluded participants who did not have a main interview (n = 14,315) or data on falls (n = 304) at Wave 7 (follow-up). Therefore, the final sample included 50,041 community-dwelling participants, aged 50 years or older at baseline, who participated to both Wave 6 and 7 and with complete data of interest. These participants resided in 18 countries. We have arbitrarily classified these countries into three regions: Western and Northern Europe: Austria, Belgium, Denmark, France, Germany, Luxembourg, Sweden and Switzerland; Southern Europe: Greece, Israel, Italy, Portugal and Spain; Eastern Europe: Croatia, Czech Republic, Estonia, Poland and Slovenia.
The 14,619 participants who dropped out between Wave 6 and 7 were older, more likely to be men, underweight and report previous falls compared to those 50,041participants who were included in the final sample (data not shown).
Demographic and clinical characteristics
At the baseline interview (Wave 6), the following variables were collected: age, self-rated health, self-reported co-morbidities and medications, previous falls and functional limitations.
Self-rated health was assessed by asking the participants: “Would you say your health is …”; options were: “excellent”, “very good”, “good”, “fair” or “poor”. We dichotomised self-rated health as good (“excellent” or “very good” or “good”) versus poor (“fair” or “poor”).
Co-morbidities were assessed by asking the participants: “Has a doctor ever told you that you had/do you currently have any of the conditions on this card?”; a show-card with multiple non-mutually exclusive options was presented to the participants. We focussed on these co-morbidities: heart attack, hypertension, high cholesterol, stroke, diabetes, chronic lung disease, cancer, Parkinson’s, hip fracture, other fractures, cognitive impairment, affective/emotional disorder, any arthritis (we grouped rheumatoid arthritis and osteoarthritis/other rheumatism).
Similarly, medications were assessed by asking: “Do you currently take drugs, at least once a week, for problems mentioned on this card?” and a list was shown. Based on previous literature [1, 6], we selected these medications: anti-hypertensives, drugs for pain (we grouped drugs for joint pain and those for other pain) and psychotropic drugs (we grouped drugs for sleep problems and those for anxiety or depression).
Previous falls were assessed by asking the participants: “For the past six months at least, have you been bothered by any of the health conditions on this card?'; options included: “falling down”.
Baseline functional limitations in activities of daily living (ADL) or instrumental activities of daily living (IADL) were assessed by asking the participants whether they had difficulties with one or more of six ADLs or with one or more of nine IADLs. ADLs were consistent with those developed by Katz [26] and included: dressing, walking across a room, bathing, eating, getting in or out of bed, using the toilet. IADLs were similar to those developed by Lawton [27] and included: using a map, preparing a meal, shopping for groceries, using the phone, taking medications, doing housework, managing money, using transport, doing personal laundry. We classified the participants as those with no functional impairment (no ADL or IADL limitations) versus those with functional impairment (one or more ADL and or IADL limitations).
BMI categories
At baseline, self-reported height and weight were collected. We computed the body mass index (BMI) as weight divided by squared height. We classified the participants into these categories: underweight (BMI < 18.5 kg/m2), normal weight (BMI ≥ 18.5 and < 25 kg/m2), overweight (BMI ≥ 25 and < 30 kg/m2) and obese (BMI ≥ 30 kg/m2).
Falls
At the follow-up interview at Wave 7, the participants were again asked the question: “For the past six months at least, have you been bothered by any of the health conditions on this card?”; options included: “falling down”. Our outcome of falls at follow-up was dichotomized as “no” (no falls) versus “yes” (one or more falls).
Statistical analyses
We plotted and visually inspected the distribution of BMI in our study population; BMI appeared to be normally distributed. We reported the characteristics of the participants at baseline as number (percentages) for categorical variables and as mean (standard deviation, SD) for age, which we used as a continuous variable. Sex-differences in characteristics at baseline were assessed using Pearson’s Chi-squared test for categorical variables and t test for age. Similarly, we tested for differences in baseline characteristics across BMI categories using Pearson’s chi-squared test for categorical variables and analysis of variance (ANOVA) for age.
Binary logistic regression models were used to assess the longitudinal association between BMI categories at baseline (determinant) and falls at follow-up (outcome). BMI categories were recoded so that the normal weight category was the reference. We performed our analyses in two steps. First, we adjusted our analyses for age and sex (Model 1). Finally, we adjusted for age, sex, self-rated health, co-morbidities, medications and previous falls (Model 2). We entered each co-morbidity and medication variable in Model 2, separately.
We repeated our analyses after restricting the sample to participants who were interviewed in 2017.
Sensitivity analyses were performed by stratifying the participants according to: (1) age groups (aged 50–64 years versus aged 65 years and older); (2) functional status (no functional impairment versus functional impairment) and (3) European region of residence (Western and Northern Europe; Southern Europe; Eastern Europe). All analyses were performed in the whole population and in men and women, separately. All analyses were performed using SPSS software (version 25).
Ethics
SHARE obtained institutional review board approval by the Ethics Committee of the University of Mannheim, during Waves 1–4, and by the Ethics Council of the Max Planck Society for Wave 4 and the continuation of the project.
Results
Characteristics at baseline
Baseline interviews were conducted from January to November 2015. Our study population included 21,909 men and 28,132 women aged 50 years and older at baseline. In our study population, mean age was 67.0 years (standard deviation 9.4 years; range 50–102 years). In particular, 21,726 (43.4%) participants were aged from 50 to 64 years, 28,315 (56.6%) were aged 65 years and older. Of note, 5596 (11.2%) participants were aged 80 years and older. 3314 (6.6%) participants reported previous falls (Table 1). Women were more likely to be underweight, report poor self-rated health, previous falls or functional limitations, compared to men (all p values < 0.001). Men were more likely to report ischaemic heart disease, stroke or diabetes, compared to women (all p values < 0.001).
Obese participants were more likely to report poor self-rated health, ischaemic heart disease, stroke, diabetes and arthritis; in contrast, underweight participants were more likely to report cancer, hip fracture or other fracture or cognitive impairment (Table 2). Further details on the distribution of baseline characteristics across BMI categories in men and women, respectively, can be found in Supplementary Tables 1 and 2.
Falls at follow-up
Follow-up interviews were conducted from February 2017 to January 2019. Follow-up interviews were conducted in Portugal in 2017, 2018 and 2019; in all other countries, only in 2017. Mean time interval between baseline and follow-up interview was 24.5 (SD 3.5) months. At the follow-up interview, 4057 (8.1%) participants—in particular, 1330 (6.1%) men and 2727 (9.7%) women—reported fall(s). In detail, 70 (13.9%) of underweight participants, 1284 (7.4%) of normal weight participants, 1527 (7.3%) of overweight participants and 1176 (10.4%) of obese participants reported falls at follow-up.
Covariates and falls risk
In the whole study population, older age, female sex (versus male), poor self-rated health (versus good), previous falls (versus no falls), taking drugs for pain and taking psychotropic drugs were each associated with increased falls risk, independently of all other covariates (Supplementary Table 3). Among co-morbidities, the following were independently associated with an increased falls risk: ischaemic heart disease, stroke, diabetes, chronic lung disease, Parkinson’s disease, hip fracture, other fracture, cognitive impairment, affective or emotional disorders, any arthritis (Supplementary Table 3).
BMI categories and falls risk
In the whole study population, the longitudinal association between BMI categories at baseline and falls risk at 2-year follow-up was U-shaped (Table 3).
In age- and sex-adjusted analyses, underweight and obese participants had an increased risk (OR) of falls of 1.71 (95% CI 1.31–2.23) and 1.61 (95% CI 1.48–1.75), respectively, compared to those with normal weight (both p values < 0.001). After full adjustment, underweight and obese participants had an increased risk of falls of 1.41 (95% 1.06–1.88) and 1.20 (95% CI 1.09–1.32), respectively, compared to those with normal weight (p values 0.017 and < 0.001).
In age-adjusted analyses, underweight and obese men had an increased falls risk compared to those with normal weight; these associations were no longer significant after full adjustment. In age-adjusted analyses, underweight, overweight and obese women had an increased falls risk compared to those with normal weight; after full adjustment, underweight and obese women had an increased risk of falls of 1.43 (95% CI 1.06–1.94) and1.27 (95% CI 1.13–1.42), respectively, compared to those with normal weight (p values 0.020 and < 0.001).
Our findings remained similar when restricting to participants who were interviewed in 2017 (n = 49,367, data not shown). Likewise, our results remained unchanged when restricting to participants without cognitive impairment (n = 49,323, data not shown).
Age-stratified results
The longitudinal associations between BMI categories and falls risk varied according to age group, after full adjustment (Table 4). In the age group from 50 to 64 years, obesity was associated with a higher falls risk, compared to normal weight (OR 1.23, 95% CI 1.03–1.47, p = 0.022), while underweight was not (Table 4). The association between obesity and increased falls risk remained consistent in women aged from 50 to 64 years, while not in men. In men aged from 50 to 64 years, overweight was associated with a lower falls risk, compared to normal weight (OR 0.74, 95% CI 0.55–0.99, p = 0.043).
In the age group 65 years and older, we observed again a U-shaped association between BMI categories and falls risk. Among participants 65 years and older, both underweight (OR 1.44, 95% CI 1.03–2.01, p = 0.032) and obesity (OR 1.20, 95% CI 1.07–1.34, p = 0.001) were associated with an increased risk of falls, compared to normal weight (Table 4). The association between obesity and increased falls risk remained significant in both women and men aged 65 years and older. A trend of association between underweight and higher falls risk was found for men and women aged 65 years and older, with ORs above the unit.
Functional status-stratified results
The longitudinal associations between BMI categories and falls risk varied according to functional status, after full adjustment (Table 5). Among participants without functional impairment, obesity was associated with an increased risk of falls of 1.18 (95% CI 1.04–1.34, p = 0.008); no association between underweight and falls risk was found (Table 5). The association between obesity and increased falls risk remained significant among women without functional impairment (Table 5).
Among participants with functional impairment, underweight was associated with an increased risk of falls of 1.61 (95% CI 1.09–2.40, p = 0.018), while obesity was not (Table 5). The association between underweight and increased falls risk was consistent among women with functional impairment (Table 5).
European region-stratified results
After full adjustment, obesity was longitudinally associated with an increased falls risk among adults from Western and Northern Europe and Southern Europe; in contrast, underweight was longitudinally associated with an increased falls risk among adults from Eastern Europe (Supplementary Table 4).
Discussion
In our large, European prospective study, we found that both underweight and obesity were longitudinally associated with higher falls risk, at 2-year follow-up, in community-dwelling adults aged 50 years and older, independently of socio-demographic and clinical variables. Moreover, the association between underweight and falls risk is more pronounced in women with functional impairment, while that between obesity and falls risk is consistent among women with no functional impairment.
The novelty of our longitudinal study is to show a U-shaped relationship between BMI and falls risk in adults. A similar U-shaped relationship has been suggested by cross-sectional studies. In a large Canadian survey of adults aged 65 years and older, underweight and obese men were more likely to report falls in the previous 12 months, compared to normal weight men, while this association was less pronounced in women [9]; in contrast, in our longitudinal study, the U-shaped association between BMI and falls risk remained consistent in women, but not in men, after full adjustment. Similarly, in a large Korean study, underweight and obesity were associated with falls in the previous 12 months in adults; the association between obesity and falls remained consistent in older adults [8].
Moreover, longitudinal studies showed that obesity was a predictor of falls in adults. In the Women’s Health Initiative (WHI), obesity predicted falls among postmenopausal women, aged 50–79, of non-Hispanic white and Hispanic ethnicity [5]. In the Osteoporotic Fractures in Men (MrOS) study, obesity predicted falls in men aged 65–80 years [6]; similarly, in our study, obesity was consistently associated with a greater falls risk in men aged 65 years and older. In the Women’s Health and Aging Study I, overweight predicted recurrent falls among disabled older women with diabetes [7]; in contrast, underweight, compared with normal weight, was correlated with an increased falls risk among women with functional impairment in our study. In the Health and Retirement Study, obesity predicted falls in adults aged 65 years and older [4].
Our finding that underweight is associated with a higher falls risk in adults conflicts with those of a systematic review and meta-analysis, showing that low BMI was not associated with falls risk in community-dwelling older adults [1]. However, low BMI was defined by cutpoints of 20 or 25 kg/m2 [1]; in our study, underweight was defined as BMI < 18.5 kg/m2. A Swedish report showed that underweight was longitudinally associated with risk of injurious falls among women aged 60 years and older [28], while in our study, underweight was associated with falls only in women with functional impairment. Discrepancies among studies may result from differences in the definition of underweight, or in the age- and sex-composition of the study population or, possibly, in the proportion of adults with functional impairment. Indeed, another novelty of our secondary analyses of the SHARE database is to suggest that the relationship between BMI and falls risk may vary by functional status, while previous studies did not explore this [8, 9] or explored it only among disabled women [7]. Our analyses were stratified by sex, as sex-differences may be observed in the incidence of falls and in the influence of risk factors on falls [9, 14,15,16]. Our findings in the age group 50–64 years—obesity was associated with an increased risk for falls in women but not in men—may reflect sex-differences in the influence of BMI on falls risk. However, we did not formally test for sex-differences as our study is likely underpowered for this.
The prevalence of underweight and obesity—1% and 22.7%, respectively—in our population is in line with the WHO estimates for adults in the European region [29]. The rate of falls in our study—about 8% within 6 months prior to the follow-up interview—is consistent with previous literature reporting rates of about 20% within 12 months, among community-dwelling adults [9, 15]. In line with previous reports, female sex was a risk factor for falls, independently of covariates [9, 14,15,16].
Different factors may mediate the association between obesity and increased falls risk. Obesity has been associated with poor gait and postural balance [30,31,32,33]. Furthermore, obesity—in particular, abdominal visceral fat—has been associated with chronic inflammation [34, 35], which, in turn, may promote sarcopenia—the loss of muscle mass and muscle strength [36, 37]. Sarcopenia is a key component of frailty, and frailty and falls are intertwined [38]. Indeed, a recent report suggested a U-shaped relationship between BMI and frailty in older adults, with increased levels of frailty among those with low and very high BMI [39]. Another study has shown an association between obesity and frailty in older women [40]. Finally, obesity has been associated with comorbidities (including diabetes) and medications (including psychotropic drugs and drugs for pain), which have been correlated with increased falls risk [1]. However, our finding of an association between obesity and falls risk remained consistent, after adjusting for these, showing that obesity is independently associated with increased risk of falls.
Different factors may explain the association between underweight and increased falls risk. Weight loss has traditionally been viewed as a marker of frailty [41]. Yet, in a systematic review and meta-analysis, low BMI was not associated with falls risk in community-dwelling older adults [1]. Of note, in our study, underweight was associated with falls risk in those adults (men and women combined) aged 65 years and older and in those with functional impairment, while not in those aged from 50 to 64 years or without functional impairment. We hypothesize that there may be two types of participants with low BMI: those older and frail and those younger and fit. In the former, low BMI is related to a disproportionate loss of muscle mass (i.e. sarcopenia); in the latter, low BMI is related to loss of adipose tissue.
In our study, overweight participants had the same falls risk as normal weight participants; this is consistent with a Canadian report showing the lowest prevalence of falls around a BMI of 25 kg/m2, for both sexes [9]. It also parallels previous reports suggesting that the optimal BMI could be around 25 kg/m2 in older adults; indeed, slight overweight may be beneficial for survival in older adults [42,43,44].
Obesity is a growing epidemic worldwide [20], affecting one in three adults in the US and one in five adults in Europe [21, 22]. Based on our findings, we hypothesize that body weight reduction programmes targeting obese adults with no functional impairment could prevent falls. Treating obesity may be beneficial for many health outcomes [20]. In contrast, nutritional supplements could be considered for underweight, sarcopenic adults; indeed, evidence from randomized, controlled trials suggests that protein or amino acid supplementation may improve physical performance in older adults [45]. However, current international guidelines do not recommend protein or amino acid supplementation for preventing falls or improving physical performance; this type of supplements may be indicated for sarcopenia, which was not assessed in our study [46].
A major strength of this study is that it is population-based and has a longitudinal design, with the BMI categorisation of the participants preceding the ascertainment of falls in the follow-up. Further strengths are the use of standardized methods for data collection and data from nationally representative samples of community-dwelling adults aged 50 years and older from 18 countries. Our large sample size included both men and women, while other studies focussed on only men [6] or women [2, 5, 7]. Furthermore, we included adults aged 50–64 years, while many studies on falls focussed only on those aged 65 years and older [3, 4, 6, 7, 9,10,11,12]. By providing sensitivity analyses in those aged 65 years and older, our study can be compared to others on older ages, though not necessarily to studies in the oldest old, since only 11.2% of our participants was aged 80 years or older. Furthermore, we were able to explore the relationship of all BMI categories with falls risk, while other studies had too few participants in the underweight category to explore this [6].
This study also has some limitations. Height and weight were self-reported; as height tends to be overestimated and weight underestimated [47], this could lead to an underestimation of BMI and misclassification of participants towards lower categories of BMI. A further limitation is the use of BMI categories, based on the WHO classification; this classification does not provide age-specific categories, despite evidence suggesting that overweight may be beneficial for survival in older adults [42,43,44]. The WHO definition of underweight also differs from that of malnutrition in adults proposed by Global Leadership Initiative on Malnutrition (GLIM) [48]. Furthermore, falls were retrospectively self-reported and this could imply a recall bias; falls, particularly non-injurious falls, may be underreported [49]. Moreover, the study collected information only on falls in the six months prior to the interview at 2-year follow-up; in this way, falls that occurred in the months immediately following the first interview may have been missed; this study did not capture the association between BMI and falls in the very short-term follow-up. In addition, we could not distinguish participants who fell indoors or outdoors, or those who fell only once or more frequently. We deem it unlikely that participants may have reported coming to the ground due to external forces—including violence or accidents—as falls; although the SHARE questionnaire did not specify to exclude falls due to external forces, the question on falling was among others related to physical symptoms and not accidents; moreover, the words used for “falling” in many translated questionnaires uniquely identified falls that are not related to external forces. Furthermore, we lacked information on other potential risk factors for falls such as use of neuroleptics or anticonvulsants, orthostatic hypotension, dizziness, anaemia and balance disturbances and could not adjust our analyses for these. Moreover, the participants who dropped out between Wave 6 and 7 were older, more likely to be underweight and report previous falls at baseline; as a result, the association between falls and underweight might have been underestimated. However, we could retain a high proportion of participants across all BMI categories at follow-up (ranging from 67.4% among underweight participants to 78.7% among obese participants) and we could show associations between underweight and falls. Finally, our study included only community-dwelling adults and excluded those who were institutionalized and likely at a higher risk for falls. However, the relative importance of risk factors for falls may differ in community-dwelling and institutionalized adults [1, 50]; thus, restricting our study to community-dwelling adults made our sample more homogeneous. Yet, we acknowledge that our findings may not be generalizable to institutionalized populations.
In conclusion, our study showed a U-shaped relationship between BMI and falls risk in community-dwelling men and women aged 50 years and older. This association may be modulated by age and functional impairment. Underweight was consistently associated with falls in the oldest and functionally impaired, while obesity was consistently associated with falls in those without functional impairment. Further studies are needed to elucidate the influence of sex on the relationship between BMI and falls risk.
Availability of data and material
Data are available upon request from the SHARE website (see http://www.share-project.org/data-access/user-registration.html).
Code availability
Not applicable.
References
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E (2010) Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 21(5):658–668. https://doi.org/10.1097/EDE.0b013e3181e89905 (PMID: 20585256)
Rosenblatt NJ, Grabiner MD (2012) Relationship between obesity and falls by middle-aged and older women. Arch Phys Med Rehabil 93(4):718–722. https://doi.org/10.1016/j.apmr.2011.08.038 (Epub 2012 Jan 2 PMID: 22218136)
Qin Z, Baccaglini L (2016) Distribution, determinants, and prevention of falls among the elderly in the 2011–2012 California Health Interview Survey. Public Health Rep 131(2):331–339. https://doi.org/10.1177/003335491613100217 (PMID: 26957668; PMCID: PMC476598)
Himes CL, Reynolds SL (2012) Effect of obesity on falls, injury, and disability. J Am Geriatr Soc 60(1):124–129. https://doi.org/10.1111/j.1532-5415.2011.03767.x (Epub 2011 Dec 8 PMID: 22150343)
Follis S, Cook A, Bea JW, Going SB, Laddu D, Cauley JA, Shadyab AH, Stefanick ML, Chen Z (2018) Association between sarcopenic obesity and falls in a multiethnic cohort of postmenopausal women. J Am Geriatr Soc 66(12):2314–2320. https://doi.org/10.1111/jgs.15613 (Epub 2018 Oct 30, PMID: 30375641; PMCID: PMC6289680)
Hooker ER, Shrestha S, Lee CG, Cawthon PM, Abrahamson M, Ensrud K, Stefanick ML, Dam TT, Marshall LM, Orwoll ES, Nielson CM, Osteoporotic Fractures in Men (MrOS) Study (2017) Obesity and falls in a prospective study of older men: the osteoporotic fractures in men study. J Aging Health 29(7):1235–1250. https://doi.org/10.1177/0898264316660412 (Epub 2016 Jul 27, PMID: 27469600; PMCID: PMC5773405)
Volpato S, Leveille SG, Blaum C, Fried LP, Guralnik JM (2005) Risk factors for falls in older disabled women with diabetes: the women’s health and aging study. J Gerontol A Biol Sci Med Sci 60(12):1539–1545. https://doi.org/10.1093/gerona/60.12.1539 (PMID: 16424285; PMCID: PMC2366043)
Kim SY, Kim MS, Sim S, Park B, Choi HG (2016) Association between obesity and falls among Korean adults: a population-based cross-sectional study. Medicine (Baltimore) 95(12):e3130. https://doi.org/10.1097/MD.0000000000003130 (PMID: 27015190; PMCID: PMC4998385)
Handrigan GA, Maltais N, Gagné M, Lamontagne P, Hamel D, Teasdale N, Hue O, Corbeil P, Brown JP, Jean S (2017) Sex-specific association between obesity and self-reported falls and injuries among community-dwelling Canadians aged 65 years and older. Osteoporos Int 28(2):483–494. https://doi.org/10.1007/s00198-016-3745-x (Epub 2016 Aug 25 PMID: 27562568)
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly persons living in the community. N Engl J Med 319(26):1701–1707. https://doi.org/10.1056/NEJM198812293192604 (PMID: 3205267)
O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S (1993) Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 137(3):342–354. https://doi.org/10.1093/oxfordjournals.aje.a116681 (PMID: 8452142)
Tinetti ME, Doucette J, Claus E, Marottoli R (1995) Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc 43(11):1214–1221. https://doi.org/10.1111/j.1532-5415.1995.tb07396.x (PMID: 7594154)
Tinetti ME, Kumar C (2010) The patient who falls: “It’s always a trade-off.” JAMA 303(3):258–266. https://doi.org/10.1001/jama.2009.2024 (PMID:20085954; PMCID:PMC3740370)
Stevens JA, Sogolow ED (2005) Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev 11(2):115–119. https://doi.org/10.1136/ip.2004.005835 (PMID:15805442; PMCID:PMC1730193)
Chang VC, Do MT (2015) Risk factors for falls among seniors: implications of gender. Am J Epidemiol 181(7):521–531. https://doi.org/10.1093/aje/kwu268 (Epub 2015 Feb 19 PMID: 25700887)
Gale CR, Cooper C, Aihie Sayer A (2016) Prevalence and risk factors for falls in older men and women: the English Longitudinal Study of Ageing. Age Ageing. 45(6):789–794. https://doi.org/10.1093/ageing/afw129 (PMID: 27496938; PMCID: PMC5105823)
Nevitt MC, Cummings SR, Kidd S, Black D (1989) Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 261(18):2663–2668 (PMID: 2709546)
Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C (2018) Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 66(4):693–698. https://doi.org/10.1111/jgs.15304 (Epub 2018 Mar 7, PMID: 29512120; PMCID: PMC6089380)
Hartholt KA, van Beeck EF, Polinder S, van der Velde N, van Lieshout EM, Panneman MJ, van der Cammen TJ, Patka P (2011) Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma 71(3):748–753. https://doi.org/10.1097/TA.0b013e3181f6f5e5 (PMID: 21045738)
GBD 2019 Risk Factors Collaborators (2020) Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2 (PMID: 33069327; PMCID: PMC7566194)
Ogden CL, Carroll MD, Kit BK, Flegal KM (2014) Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 311(8):806–814. https://doi.org/10.1001/jama.2014.732 (PMID:24570244; PMCID:PMC4770258)
World Health Organization Regional Officer for Europe. Health topics. Non communicable diseases. Obesity: Data and statistics.https://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/data-and-statistics. Accessed 7 Dec 2020
Alibhai SM, Greenwood C, Payette H (2005) An approach to the management of unintentional weight loss in elderly people. CMAJ 172(6):773–780. https://doi.org/10.1503/cmaj.1031527 (PMID:15767612; PMCID:PMC552892)
Villareal DT, Apovian CM, Kushner RF, Klein S (2005) Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res 13(11):1849–1863. https://doi.org/10.1038/oby.2005.228 (PMID: 16339115)
Borsch-Supan A, Brandt M, Hunkler C et al (2013) SHARE Central Coordination Team Data. Resource Profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol 42:992–1001
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914–919. https://doi.org/10.1001/jama.1963.03060120024016 (PMID: 14044222)
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9(3):179–186 (PMID: 5349366)
Ek S, Rizzuto D, Fratiglioni L, Calderón-Larrañaga A, Johnell K, Sjöberg L, Xu W, Welmer AK (2019) Risk factors for injurious falls in older adults: the role of sex and length of follow-up. J Am Geriatr Soc 67(2):246–253. https://doi.org/10.1111/jgs.15657 (Epub 2018 Nov 29, PMID: 30496601; PMCID: PMC7379536)
World Health Organization. The Global Health Observatory (GHO). World Health Data Platform. Body mass index (BMI). https://www.who.int/data/gho/data/themes/theme-details/GHO/body-mass-index-(bmi). Accessed 23 Nov 2020
Hue O, Simoneau M, Marcotte J, Berrigan F, Doré J, Marceau P, Marceau S, Tremblay A, Teasdale N (2007) Body weight is a strong predictor of postural stability. Gait Posture 26(1):32–38. https://doi.org/10.1016/j.gaitpost.2006.07.005 (Epub 2006 Aug 22 PMID: 16931018)
Dutil M, Handrigan GA, Corbeil P, Cantin V, Simoneau M, Teasdale N, Hue O (2013) The impact of obesity on balance control in community-dwelling older women. Age (Dordr) 35(3):883–890. https://doi.org/10.1007/s11357-012-9386-x (Epub 2012 Feb 10, PMID: 22318311; PMCID: PMC3636380)
Rossi-Izquierdo M, Santos-Pérez S, Faraldo-García A, Vaamonde-Sánchez-Andrade I, Gayoso-Diz P, Del-Río-Valeiras M, Lirola-Delgado A, Soto-Varela A (2016) Impact of obesity in elderly patients with postural instability. Aging Clin Exp Res 28(3):423–428. https://doi.org/10.1007/s40520-015-0414-4 (Epub 2015 Jul 18 PMID: 26187012)
Lee JJ, Hong DW, Lee SA, Soh Y, Yang M, Choi KM, Won CW, Chon J (2020) Relationship between obesity and balance in the community-dwelling elderly population: a cross-sectional analysis. Am J Phys Med Rehabil 99(1):65–70. https://doi.org/10.1097/PHM.0000000000001292 (PMID: 31464747)
Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y (2017) Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci 13(4):851–863. https://doi.org/10.5114/aoms.2016.58928 (PMID: 28721154; PMCID: PMC5507106)
Schrager MA, Metter EJ, Simonsick E, Ble A, Bandinelli S, Lauretani F, Ferrucci L (2007) Sarcopenic obesity and inflammation in the InCHIANTI study. J Appl Physiol 102(3):919–925. https://doi.org/10.1152/japplphysiol.00627.2006 (Epub 2006 Nov 9, PMID: 17095641; PMCID: PMC2645665)
Schaap LA, Pluijm SM, Deeg DJ, Visser M (2006) Inflammatory markers and loss of muscle mass (sarcopenia) and strength. Am J Med 119(6):526.e9–17. https://doi.org/10.1016/j.amjmed.2005.10.049 (PMID: 16750969)
Stenholm S, Harris TB, Rantanen T, Visser M, Kritchevsky SB, Ferrucci L (2008) Sarcopenic obesity: definition, cause and consequences. Curr Opin Clin Nutr Metab Care 11(6):693–700. https://doi.org/10.1097/MCO.0b013e328312c37d (PMID:18827572; PMCID:PMC2633408)
Nowak A, Hubbard RE (2009) Falls and frailty: lessons from complex systems. J R Soc Med 102(3):98–102. https://doi.org/10.1258/jrsm.2009.080274 (PMID:19297650; PMCID:PMC2746842)
Hubbard RE, Lang IA, Llewellyn DJ, Rockwood K (2010) Frailty, body mass index, and abdominal obesity in older people. J Gerontol A Biol Sci Med Sci 65(4):377–381. https://doi.org/10.1093/gerona/glp186 (Epub 2009 Nov 25 PMID: 19942592)
Blaum CS, Xue QL, Michelon E, Semba RD, Fried LP (2005) The association between obesity and the frailty syndrome in older women: the Women’s Health and Aging Studies. J Am Geriatr Soc 53(6):927–934. https://doi.org/10.1111/j.1532-5415.2005.53300.x (PMID: 15935013)
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56(3):M146–M156. https://doi.org/10.1093/gerona/56.3.m146 (PMID: 11253156)
Flicker L, McCaul KA, Hankey GJ, Jamrozik K, Brown WJ, Byles JE, Almeida OP (2010) Body mass index and survival in men and women aged 70 to 75. J Am Geriatr Soc 58(2):234–241. https://doi.org/10.1111/j.1532-5415.2009.02677.x (PMID: 20370857)
Auyeung TW, Lee JS, Leung J, Kwok T, Leung PC, Woo J (2010) Survival in older men may benefit from being slightly overweight and centrally obese—a 5-year follow-up study in 4,000 older adults using DXA. J Gerontol A Biol Sci Med Sci 65(1):99–104. https://doi.org/10.1093/gerona/glp099 (Epub 2009 Jul 23. PMID: 19628635; PMCID: PMC2796879)
de Hollander EL, Van Zutphen M, Bogers RP, Bemelmans WJ, De Groot LC (2012) The impact of body mass index in old age on cause-specific mortality. J Nutr Health Aging 16(1):100–106. https://doi.org/10.1007/s12603-011-0077-6 (PMID: 22238008)
Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, Phillips S, Sieber C, Stehle P, Teta D, Visvanathan R, Volpi E, Boirie Y (2013) Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc 14(8):542–559. https://doi.org/10.1016/j.jamda.2013.05.021 (Epub 2013 Jul 16 PMID: 23867520)
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M, Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2 (2019) Sarcopenia: revised European consensus on definition and diagn0osis. Age Ageing 48(1):16–31. https://doi.org/10.1093/ageing/afy169 (Erratum in: Age Ageing. 2019 Jul 1;48(4):601. PMID: 30312372; PMCID: PMC6322506)
ConnorGorber S, Tremblay M, Moher D, Gorber B (2007) A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev 8(4):307–326. https://doi.org/10.1111/j.1467-789X.2007.00347.x (PMID: 17578381)
Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, Baptista G, Barazzoni R, Blaauw R, Coats AJS, Crivelli AN, Evans DC, Gramlich L, Fuchs-Tarlovsky V, Keller H, Llido L, Malone A, Mogensen KM, Morley JE, Muscaritoli M, Nyulasi I, Pirlich M, Pisprasert V, de van der Schueren MAE, Siltharm S, Singer P, Tappenden K, Velasco N, Waitzberg D, Yamwong P, Yu J, Van Gossum A, Compher C, GLIM Core Leadership Committee, GLIM Working Group (2019) GLIM criteria for the diagnosis of malnutrition—a consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle 10(1):207–217. https://doi.org/10.1002/jcsm.12383 (PMID: 30920778; PMCID: PMC6438340)
Hoffman GJ, Ha J, Alexander NB, Langa KM, Tinetti M, Min LC (2018) Underreporting of fall injuries of older adults: implications for wellness visit fall risk screening. J Am Geriatr Soc 66(6):1195–1200. https://doi.org/10.1111/jgs.15360 (Epub 2018 Apr 17, PMID: 29665016; PMCID: PMC6105546)
Deandrea S, Bravi F, Turati F, Lucenteforte E, La Vecchia C, Negri E (2013) Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta-analysis. Arch Gerontol Geriatr 56(3):407–415. https://doi.org/10.1016/j.archger.2012.12.006 (Epub 2013 Jan 5, PMID: 23294998)
Acknowledgements
Dr. Giulia Ogliari was supported by Grant APP2380/N7359 (N7359 Osteoporosis and Falls Research for ‘Improving Quality of Life In Older Patients’) by Nottingham Hospitals Charity, Nottingham, UK. This paper uses data from SHARE Wave 6 and 7, release 7.1.0, as of 16 June 2020. The SHARE data collection has been primarily funded by the European Commission through the fifth framework programme (project QLK6-CT-2001–00 360 in the thematic programme Quality of Life), through the sixth framework programme (projects SHARE-I3, RII-CT- 2006–0 62 193; COMPARE, CIT5-CT-2005–0 28 857; and SHARELIFE, CIT4-CT-2006–0 28 812) and through the seventh framework programme (SHARE-PREP, 2 11 909 and SHARE- LEAP, 227822). Additional funding from the US National Institute on Ageing (U01 AG09740-13S2, P01 AG005842, P01 AG08291, P30 AG12815, Y1-AG-4553–01 and OGHA 04–064, IAG BSR06-11, R21 AG025169) as well as from various national sources is gratefully acknowledged (see http://www.share-project.org/contact-organisation/funding.html for a full list of funding institutions).
Funding
Dr. Giulia Ogliari was supported by Grant APP2380/N7359 (OSTEOPOROSIS and FALLS RESEARCH) by Nottingham Hospitals Charity.
Author information
Authors and Affiliations
Contributions
GO: study concept, data analysis, drafting the manuscript. JR, KAR, LLSH and TM: study concept, critical revision of manuscript for intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics approval
Institutional review board at University of Mannheim and Ethics Council of the Max Planck Society.
Consent to participate
This article uses anonymised data.
Consent for publication
Not applicable. Personal data were not identifiable during the analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ogliari, G., Ryg, J., Andersen-Ranberg, K. et al. Association between body mass index and falls in community-dwelling men and women: a prospective, multinational study in the Survey of Health, Ageing and Retirement in Europe (SHARE). Eur Geriatr Med 12, 837–849 (2021). https://doi.org/10.1007/s41999-021-00485-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00485-5