Abstract
Summary
The association of BMI with falls differed between men and women in Korea. Obesity was associated with a greater risk of falls in women, whereas underweight seemed to increase the risk of falls compared with normal weight in men.
Purpose
This study examined the sex-specific association between body mass index (BMI) and falls in Korean adults using data from a large population-based survey.
Methods
We analyzed 113,805 men and women (age ≥ 50 years) who participated in the Korean Community Health Survey in 2013. Logistic regression was used to assess the relationship between BMI and falls.
Results
The mean (± standard deviation) age and BMI of all participants were 63.8 ± 9.6 years and 23.2 ± 2.9 kg/m2, respectively. Among the 113,805 subjects, 19.1% and 6.7% had histories of falls and recurrent falls, respectively. The association of BMI with recurrent falls differed between men and women. The multivariable-adjusted odd ratios (ORs) for recurrent falls were 0.98 (95% confidence interval [CI] 0.86–1.12), 1.23 (1.14–1.32), and 1.51 (1.26–1.81) in women with BMIs of < 18.5, 25–29.9, and ≥ 30 kg/m2, respectively, relative to those with BMIs of 18.5–24.9 kg/m2. The corresponding ORs for men were 1.20 (95% CI 1.01–1.42), 1.05 (0.96–1.14), and 0.97 (0.69–1.38), respectively. Older age and low economic level were associated independently with higher ORs of recurrent falls in men and women, respectively. In addition, comorbidities, including diabetes, stroke, arthritis, osteoporosis, and asthma, correlated significantly with an increased risk of recurrent falls (all p < 0.001).
Conclusions
Obesity was associated with a greater risk of recurrent falls in women, whereas underweight seemed to be associated with a greater risk of falls in men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falls are the leading cause of unintentional injury and a major public health problem in worldwide [1]. In the USA, one-third of community-dwelling people aged ≥ 65 years fall every year, and about 10% of these events result in major injuries, including fractures and severe soft-tissue injuries requiring medical attention [2]. Previous studies have identified clinical risk factors for falls, which include previous falls, gait and balance impairments, visual impairment, depression, and cognitive impairment [3]. In addition, polypharmacy, arrhythmia, and Parkinson’s disease are reported risk factors for falls [4, 5].
Obesity is also a public health concern worldwide. Although lower than in other populations, the prevalence of obesity is rapidly increasing in Asian populations and is a growing concern in Asia [6]. As aspects of balance control, such as postural stability, are altered in adults with obesity [7, 8], obesity has been suggested to increase the risk of falling. Few studies have assessed the relationship between obesity and falls, and the results have been contradictory. Some researchers have reported that obese adults have an increased risk of falls relative to those of normal weight [9, 10]. A longitudinal study conducted with older adults in the USA showed that centrally obese participants had an increased risk of falls (odds ratio [OR] 1.37), but that adults with obesity according to their body mass indices (BMIs; > 30 kg/m2) were not at greater risk than their counterparts [11].
We previously reported that the association of BMI with hip fracture differed according to sex, namely, that obesity was associated with an increased risk of hip fracture in women, but not in men [12]. Thus, we hypothesized that the association between BMI and falls may differ by sex. A limited number of studies have involved sex-specific analyses of the association between BMI and fall risk. A study conducted in Canada showed that obese men had a 33% greater risk of falls than did normal-weight men, but that obese women were not at greater risk [13].
No previous study has evaluated the relationship between BMI and falls according to sex in Asia. Thus, the objective of this study was to evaluate the sex-specific association between BMI and falls among Korean adults and to examine the clinical risk factors for falls.
Materials and methods
Study participants
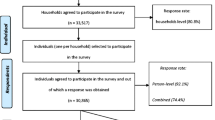
We used data from the 2013 Community Health Survey (CHS), a nationwide, cross-sectional interview-based health survey conducted by the Korea Centers for Disease Control and Prevention. The CHS has been conducted annually since 2008 with individuals aged ≥19 years in 253 regions around the country; two-stage systematic sampling methods are used to ensure that the samples are representative of the entire population [14]. Of the 228,781 participants, the following participants were excluded from this study: individuals who did not indicate their height or weight (n = 13,758); individuals who had incomplete data related to smoking, alcohol consumption history, exercise, and comorbidities (n = 39); and individuals aged < 50 years (n = 101,179).
Assessment of falls
All participants were asked whether and how many times they had fallen in the previous 12 months. We defined a history of falls as any experience of falling in the past year and recurrent falls as the occurrence of two or more falls in the past year. Also, all participants were asked if they experienced a fear or “severe fear” of falling.
Socioeconomic and demographic factors
Participants were asked to report their current height and weight, and their BMIs (kg/m2) were calculated. The questionnaire also solicited data on participants’ smoking histories, alcohol use, and physical activity. Smoking status was divided into three groups: non-smoker, past smoker, and current smoker. Current smokers included individuals who had quit smoking for < 1 year. Alcohol consumption was categorized according to alcohol use frequency (none, < 4 times/month, 2 or 3 times/week, ≥ 4 times/week). Physical activity was classified using three items about the usual time (min) participants spent (1) walking, (2) engaging in moderate-intensity activity (e.g., slow swimming, doubles tennis, badminton, table tennis), and (3) engaging in vigorous-intensity activity (e.g., jogging or running, brisk bicycling, swimming, soccer) for at least 10 min. Metabolic equivalent of task (MET) ratings of 2.9, 4.0, and 7.0 were assigned for walking, moderate-intensity, and vigorous-intensity activities, respectively. Physical activity–related energy expenditure (MET min/week) was calculated by summing the product of frequency, intensity, and duration. The METs for physical activity were categorized into quartiles. Participants who had ever received National Basic Living Security were categorized as having low socioeconomic status. All participants were asked about their histories of comorbidities, including diabetes, hypertension, stroke, myocardial infarction, arthritis, osteoporosis, and asthma. Those who reported being diagnosed by a medical doctor with any of these diseases were recorded as having positive comorbidity histories.
Statistical analysis
Because fall and recurrent fall experiences differed significantly between men and women, all analyses were stratified by sex. BMIs were categorized into four groups (< 18.5, 18.5–24.9, 25–29.9, and ≥ 30 kg/m2) using cut-off points suggested by the World Health Organization. ORs were calculated for outcomes related to falls using logit regression models after adjustment for age at baseline (continuous variable within each age group), smoking status (current smoker, former smoker, never smoker), alcohol consumption frequency (none, < 4 times/month, 2 or 3 times/week, ≥ 4 times/week), physical activity (MET quartiles), and income status (history of National Basic Living Security receipt). The sensitivity analysis was adjusted further for comorbidities (physician diagnoses, including diabetes, stroke, myocardial infarction, arthritis, osteoporosis, and asthma). We also performed stratified analyses by sex and age group (50–59, 60–69, and ≥ 70 years). Subgroup analyses were used to test the sensitivity of the results. All p values are two-sided. All analyses were conducted using SAS software (ver. 9.4; SAS Institute, Cary, NC, USA).
Results
Characteristics of the study population
Tables 1 and 2 show the clinical characteristics of the study population. The mean age and BMI of all participants were 63.8 ± 9.6 years and 23.2 ± 2.9 kg/m2, respectively. Of the 113,805 subjects, 4.6% were underweight, 23.0% were overweight, and 1.7% were obese. The percentage of current smokers was highest in the underweight group and decreased with increasing BMI. The prevalence of diabetes and hypertension increased with increasing BMI in men and women, respectively. As expected, the prevalence of osteoporosis was greatest in the underweight group. In men, the prevalence of asthma was greatest in the underweight group; in women, it was greatest in the obese group.
Association between BMI and falls
Of the 113,805 subjects, 19.1% and 6.7% had histories of falls and recurrent falls, respectively. There were 446, 5126, 1823, and 176 cases of recurrent falls among those with BMIs of < 18.5, 18.5–24.9, 25–29.9, and ≥ 30 kg/m2, respectively. The patterns of recurrent fall experiences across BMI categories differed between men and women. The ORs for recurrent falls among women with BMIs of < 18.5, 25–29.9, and ≥ 30 kg/m2 were 0.98, 1.23, and 1.51, respectively (p < 0.05 for BMI categories > 25 kg/m2), relative to that for women with BMIs of 18.5–24.9 kg/m2 after adjustment for age, smoking, alcohol use, exercise, and income status (Table 3). After further adjustment for comorbidity, the ORs for recurrent falls among women with BMIs of 25–29.9 and ≥ 30 kg/m2 remained significantly higher than those for women in the reference BMI category (Table 2). Among women with BMIs ≥ 30 kg/m2, the OR was highest in the 50–59-year age group and decreased gradually with age (Pinteraction = 0.252). The ORs were 1.78 (95% confidence interval [CI] 1.30–2.43) in the 50–59-year age group, 1.48 (95% CI 1.08–2.03) in the 60–69-year age group, and 1.26 (95% CI 0.93–1.72) in those aged ≥ 70 years (Supplementary Table S1). For men, the ORs for recurrent falls associated with BMIs of < 18.5, 25–29.9, and ≥ 30 kg/m2 were 1.20, 1.05, and 0.97, respectively (p < 0.05 for BMI categories < 18.5 kg/m2) relative to those in the reference BMI category (Table 2). After further adjustment for comorbidity, the risk of recurrent falls in men with BMIs < 18.5 kg/m2 was not significantly higher than that in men with normal BMIs. Among men with BMIs < 18.5 kg/m2, the OR was highest (1.84) in the young age group and decreased gradually with age (Supplementary Table S1).
Association between BMI and fear of falling
The percentages of all participants with fear and severe fear of falling were 45.7% and 13.1%, respectively. Among women, the risks of fear and severe fear of falling were greater in participants with BMIs of 25–29.9 and ≥ 30 kg/m2 than in those with reference BMIs (Table 4). The OR for the severe fear of falling was significantly higher in underweight women (< 18.5 kg/m2) than in those with reference BMIs, although these women did not have higher ORs for recurrent falls. Among men, the underweight group had higher ORs for fear of falling (OR 1.41, 95% CI 1.28–1.55) and severe fear of falling (OR 1.52, 95% CI 1.34–1.73) compared with the normal-weight group (Table 4). These results are consistent with the recurrent fall experience across BMI groups.
Clinical factors associated with recurrent falls
In the multivariable-adjusted models, older age and low economic level were associated with an increased risk of recurrent fall history in men and women, respectively (Table 5). Some risk factors were sex-specific. Men in the highest quartile of exercise had an increased risk for recurrent falls, whereas women in the lower three quartiles of exercise were at lesser risk for recurrent falls than were those who did not exercise. As expected, diabetes, stroke, arthritis, osteoporosis, and asthma were associated significantly with recurrent falls among men and women (Table 5).
Discussion
Major findings
Our study showed that the association between BMI and recurrent falls among community-dwelling Koreans aged ≥ 50 years differed according to sex. Women with BMIs of 25–29.9 and ≥ 30 kg/m2 had an increased risk of recurrent falls than did those with reference BMIs (18.5–24.9 kg/m2) after adjustment for multiple confounders, including comorbidities. Low BMI was associated with a greater prevalence of recurrent falls among men, although this association was not significant after adjustment for comorbidity.
Association between BMI and falls
Several researchers have reported on the correlation between BMI and falls, but findings have been inconsistent. Many studies have shown a positive correlation between obesity and falls, but some studies have not. Himes et al. [9] conducted a longitudinal population-based survey to examine the effects of obesity on falls and fall-related injuries among 10,755 adults aged ≥ 65 years. They noted that obesity was associated significantly with fall risk, and that this risk increased with the BMI (obesity class 1, OR 1.17; obesity class 2, OR 1.26; obesity class 3, OR 1.50). Mitchell et al. [10] also found that older obese people had a 31% greater risk of falls than did normal-weight persons. Cho et al. [11] analyzed the US Health and Retirement Study data from community-dwelling adults aged ≥ 65 years. They showed that adults with central obesity were more likely to experience a fall (OR 1.37, 95% CI 1.01–1.85), whereas obese adults did not have a greater risk of falls. The mechanisms of increased fall risk in obese adults have not been explained fully. Generally, aspects of balance control, such as postural stability, are altered in obese adults. In particular, centrally obese people have higher centers of gravity and more pronounced lumbar lordosis, which are correlated with poor postural stability.
To date, few studies have investigated the relationship between BMI and falls in men and women separately, and the results have been inconsistent [13]. In a Canadian study, obesity was associated with a 33% greater risk of falls in men, but not women [13]. The prevalence of recurrent falls was greater among overweight and obese women than among normal-weight women (ORs 1.23 and 1.51, respectively) and a high BMI was not associated with recurrent falls among the men of our study. However, it remains unclear whether the association differs between the sexes. No clear explanation for any such difference is apparent. However, ethnic variation in body composition and sites of fat accumulation may partially explain the differences between the findings of the Canadian study and ours. Generally, white men accumulate fat around the trunk and abdomen and white women fat around the hips and thighs. Asian women have more abdominal and visceral fat, but less leg and hip fat, than do white women of similar overall adiposity [15]. This may explain the increased risk of falls and hip fracture in obese Asian women [12].
Underweight men had a 20% greater risk of recurrent falls than did normal-weight men after adjustment for age, smoking, alcohol use, exercise, and income status. However, after further adjustment for several comorbidities, the risk of recurrent falls decreased slightly (OR 1.18, P = 0.057). We also noted that asthma and osteoporosis were more prevalent among underweight men than among men in other BMI categories. This finding suggests that the correlation of low BMI with recurrent falls is due mainly to comorbidities, such as asthma and osteoporosis, although a low BMI itself could contribute to the increased risk of falls. Being underweight, which is associated with low muscle mass and increased frailty, could induce falls.
Association between BMI and fear of falling
As expected, the association between BMI and fear of falling was similar to that between BMI and recurrent falls in men and women. Additionally, the ORs for severe fear of falling were higher than those for recurrent falls in the same BMI categories, suggesting that fall experience may induce a more severe fear of falling. For example, women with BMIs > 30 kg/m2 had a 51% more experience of recurrent falls, but 117% more experience of severe fear of falling than did those with reference BMIs. Interestingly, we found that underweight women had a more severe fear of falling than did those with reference BMIs (OR 1.17, 95% CI 1.08–1.28), although they did not have an increased risk of falls or recurrent falls. Conversely, more women with low BMIs had a fear of falling, which may influence the prevalence of falls by reducing exercise or efforts to prevent falling. The occurrence or prevalence of fear or severe fear of falling was much higher than the fall number or recurrent fall experience in our study. Many studies have confirmed that a previous history of falls is a risk factor for the fear of falling [16]; in one study, however, the fear of falling at baseline was a predictor of fall occurrence during a 24-month follow-up period [17].
Clinical risk factors for falls
In this study, several comorbidities were associated with the increased prevalence of recurrent falls. For example, the prevalence of recurrent falls was greater in men and women with diabetes after adjustment for other confounders, including BMI, economic status, age, and physical activity. Among several comorbidities, asthma, stroke, and arthritis correlated strongly with recurrent fall risk after adjustment for other confounding factors (OR > 2.0 for all diseases in men and OR 1.75–1.9 in women).
Study strengths and limitations
The strengths of this study included the large numbers of participants and recurrent fall cases, which increased the statistical power. Our study also had some limitations. It was a cross-sectional survey, and the results for various variables are based on self-reports. We used self-reported height and weight, which likely introduced misclassification bias. Also, we lacked information on frailty and fall-related injuries, including fractures.
Conclusions
In conclusion, we found that obesity was associated with a greater risk of recurrent falls in women, whereas men with low BMIs had an increased prevalence of recurrent falls.
Data availability
There were some restrictions to accessing the raw data. The data are available from the Community Health Survey (CHS) conducted by the Korea Centers for Disease Control and Prevention, but access to confidential data is limited to researchers who meet the necessary criteria; basically, any researchers who propose a study subjects and plans with standardized proposal form, and being approved.
References
James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, Hamilton EB, Henry NJ, Krohn KJ, Liu Z, McCracken D, Nixon MR, Roberts NLS, Sylte DO, Adsuar JC, Arora A, Briggs AM, Collado-Mateo D, Cooper C, Dandona L, Dandona R, Ellingsen CL, Fereshtehnejad SM, Gill TK, Haagsma JA, Hendrie D, Jürisson M, Kumar GA, Lopez AD, Miazgowski T, Miller TR, Mini GK, Mirrakhimov EM, Mohamadi E, Olivares PR, Rahim F, Riera LS, Villafaina S, Yano Y, Hay SI, Lim SS, Mokdad AH, Naghavi M, Murray CJL (2020) The global burden of falls: global, regional and national estimates of morbidity and mortality from the global burden of disease study 2017. Inj Prev 26:i3–i11. https://doi.org/10.1136/injuryprev-2019-043286
Painter JA, Allison L, Dhingra J, Painter JA, Allison L, Dhingra P, Daughtery J, Cogdill K, Trujillo LG (2012) Fear of falling and its relationship with anxiety, depression and activity engagement among community-dwelling older adults. Am J Occup Ther 66:169–176
Maki BE, Holliday PJ, Topper AK (1994) A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol Med Sci 49:M72–M84
Kojima T, Akishita M, Nakamura T, Nomura K, Ogawa S, Iijima K, Eto M, Ouchi Y (2012) Polypharmacy as a risk for fall occurrence in geriatric outpatients. Geriatr Gerontol Int 12:425–430
Sanders NA, Ganguly JA, Jetter TL, Daccarett M, Wasmund SL, Brignole M, Hamdan MH (2012) Atrial fibrillation: an independent risk factor for nonaccidental falls in older patients. Pacing Clin Electrophysiol 35:973–979
Ramachandran A, Snehalatha C (2010) Rising burden of obesity in Asia. J obes. 2010:868573
Handrigan GA, Corbeil P, Simoneau M, Teasdale N (2010) Balance control is altered in obese individuals. J Biomech 43:383–384
Dutil M, Handrigan GA, Corbeil P, Cantin V, Simoneau M, Teasdale N, Heu O (2013) The impact of obesity on balance control in community-dwelling older women. Age 35:883–890
Himes CL, Reynolds SL (2012) Effect of obesity on falls, injury, and disability. J Am Geriatr Soc 61:124–129
Mitchell RJ, Lord SR, Harvey LA, Close JC (2014) Associations between obesity and overweight and fall risk, health status and quality of life in older people. Aust N Z J Public Health 38:13–18
Cho BY, Seo DC, Lin HC, Lohrmann DK, Chomistek AK (2018) BMI and central obesity with falls among community-dwelling older adults. Am J Prev Med 54:e50–e66
Kim SH, Yi SW, Yi JJ, Kim YM, Won YJ (2018) Association between body mass index and the risk of hip fracture by sex and age: a prospective cohort study. J Bone Miner Res 33:1603–1611
Handrigan GA, Maltais N, Gagne M, Lamontagne P, Hamel D, Teasdale N, Hue O, Corbeil P, Brown JP, Jean S (2017) Sex-specific association between obesity and self-reported falls and injuries among community-dwelling Canadians aged 65 years and older. Osteoporos Int 28:483–494
Rim H, Kim H, Lee K, Chang S, Hovell MF, Kim YT, Kim Y, Kang G, Tak Y, Im J (2011) Validity of self-reported healthcare utilization data in the Community Health Survey in Korea. J Korean Med Sci 26:1409–1414
Lim U, Ernst T, Buchthal SD, Latch M, Albright CL, Wilkens LR, Kolonel LN, Murphy SP, Chang L, Novotny R, le Marchand L (2011) Asian women have greater abdominal and visceral adiposity than Caucasian women with similar body mass index. Nutr Diabetes 1:e6
Hughes CC, Kneebone II, Jones F, Brady B (2015) A theoretical and empirical review of psychological factors associated with falls-related psychological concerns in community-dwelling older people. Int Psychogeriatr 27:1071–1087
Lavedán A, Viladrosa M, Jürschik P, Botigué T, Nuín C, Masot O, Lavedán R (2018) Fear of falling in community-dwelling older adults: A cause of falls, a consequence, or both? PLoS One 13:e0194967
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 27 kb)
Rights and permissions
About this article
Cite this article
Yi, SW., Kim, Y., Won, Y. et al. Association between body mass index and the risk of falls: a nationwide population-based study. Osteoporos Int 32, 1071–1078 (2021). https://doi.org/10.1007/s00198-020-05725-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05725-1