Abstract
Objective
The aim of the study is to assess whether obesity affects balance in elderly patients with postural instability.
Study design
It is a case–control study, with cases defined by BMI ≥30 kg/m2, and developed in a third level university hospital.
Methods
We included 135 patients aged 65 years old or more who presented postural instability. Balance assessment was through the sensory organisation test (SOT), limits of stability (LOS) and rhythmic weight shift (RWS) of computerised dynamic posturography (CDP) and the modified timed up-and-go (TUG) test. The patients also completed the Dizziness Handicap Inventory and short Falls Efficacy Scale-International questionnaire.
Results
Patients with obesity took longer to perform the modified TUG and required more steps. Also these patients had poorer scores in the subjective tests. In the CDP there were no significant differences in the SOT nor the LOS, and only there was a statistical significant difference in the anterior-posterior directional control of the RWS. Obese patients have a higher risk of fallings compared to non-obese patients.
Conclusion
In essence, our results indicate that obesity interferes in the balance of elderly patients with postural instability, putting them at a greater risk of fallings, performing worse dynamic tasks and feeling more disabled. Although continued education on training balance may be useful in older population, since the obese group shows more rate of fallers, rehabilitation programmes focus on dynamic tasks in these patients could be useful to reduce their fall risk and improve their quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Balance becomes more precarious with age and balance disorders become more common. In the published studies, balance disorders among the elderly patients who require medical care, need pharmacological treatment or limit activity show a prevalence ranging from 4 to 29 % [1–3]. When considering the prevalence of balance disorders in elderly patients in general, it rises to 37–61 % [4, 5], and is greater among women [4].
Accidental falls, especially in such elderly patients, represent one of the main social-healthcare problems in ageing western societies [6]. Nearly a third of all people who fall three or more times a year are hospitalised, admitted to a residential facility or die in the following year [7]. Repeated falls are therefore a prognostic factor for greater morbidity-mortality.
With ageing several inputs of balance, especially the use of visual and vestibular information, are deteriorating [8]. This fact implies a worse postural control even in healthy patients. In addition balance function could be different according to gender [9, 10].
Also we know that excessive body weight is associated with postural instability [11, 12]. However it has been suggested that this may not be true in elderly, because in these patients an increased body weight tended to reduce the risk of falling and consequently the risk of hip fractures [13]. But these findings are not consistent with recent studies showing that obesity has been associated with an increased risk of falls among older people [14].
Several devices exist in order to facilitate an objective evaluation of balance. Computerised dynamic posturography (CDP) platform allows independent evaluation of the contributions of vestibular, visual and proprioceptive inputs to the maintenance of balance [15]. CDP has already proven useful for the evaluation of balance and fall risk of elderly patients [16]. In addition there are clinical tests to determine the risk of falls in elderly population, one of the most widely used is the timed up-and-go (TUG) test [17, 18].
The aim of the present study is to assess with clinical and instrumental examination whether obesity affects balance in elderly patients with postural instability, and if obesity increases risk of falling in this population.
Materials and methods
This study forms part of a research project funded by the National Institute of Health Carlos III (National R&D&I Plan, dossier PI11/01328) entitled “Reduction in falls by the elderly by the use of vestibular rehabilitation to improve balance”. It is cross-sectional and was conducted in a tertiary university hospital.
Study population: inclusion and exclusion criteria
The age of the study subjects was 65 years or more, and they presented balance disorders solely due to age. An otoneurological examination was performed to rule out other causes, including assessment for the absence of spontaneous or induced nystagmus with the head shake test, and the absence of saccades by the Halmagy test. The study was completed with videonystagmography or imaging tests when necessary. They also presented a high risk of falling, fulfilling at least one of the following inclusion criteria [19]:
-
Have fallen at least once in the last twelve months.
-
Taking more than 15 s, or needing support, in the modified timed up-and-go (TUG) test.
-
Obtaining a score of less than 68 in the average score of the sensory organisation test (SOT) of the computerised dynamic posturography (CDP).
-
Have fallen at least once during the SOT.
The study’s exclusion criteria were:
-
Cognitive decline that prevents the patient from understanding the examinations.
-
Balance disorders caused by conditions other than age (neurologic, vestibular, etc.).
-
Organic conditions that prevent standing, which is necessary for a complete postural assessment.
Sample
The study sample comprised 135 people aged 65 years or more, who met the above criteria and were seen because of balance disorders in the Neurotology Department of a third level hospital. 104 of the patients were women and 31 were men. Their mean age was 77.15 ± 6.72 years, their mean height was 154.46 ± 8.34 cm and their mean body mass index (BMI) was 30.32 ± 4.15 kg/m2.
Study variables
We collected data about age, gender, the number of falls referred by the patients and the numbers of admissions to hospital for fall-related injuries during the 12 months prior to inclusion in the study. The presence or absence of obesity was defined as BMI ≥30 kg/m2. Postural assessment was performed by the following tests:
-
CDP. We used the Neurocom® Smart Equitest platform to perform the following tests:
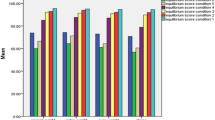
(A) Sensory organisation test (SOT). This posturograph consists of a moveable platform and screen, which can remain fixed or move in proportion to the force of the patient’s feet; the patient stands on the platform and attempts to maintain his or her balance in the Romberg position when sensorial conditions change [15]. The test assesses centre of gravity stability in 6 different sensorial conditions:
-
Condition 1: fixed surface and visual surround, eyes open.
-
Condition 2: fixed surface, eyes closed.
-
Condition 3: fixed surface, eyes open, moving surround.
-
Condition 4: moving surface, eyes open, fixed surround.
-
Condition 5: moving surface, eyes closed.
-
Condition 6: moving surface, eyes open, moving surround.
Each of these six conditions is repeated three times in order to calculate the average results obtained in each condition. The duration of each record is 20 s.
Analysing and comparing the responses to the different sensorial conditions, we can quantify the contribution of sensorial receptors to maintaining balance. The study analysed the following variables:
-
Average balance score, obtained by weighting the means scores of each sensorial condition.
-
Somatosensory input, which is the percentage value that results from the following formula: (mean score of condition 2/mean score of condition 1) × 100.
-
Visual input, calculated as the result of (mean score of condition 4/mean score of condition 1) × 100.
-
Vestibular input, calculated as (mean score of condition 5/mean score of condition 1) × 100.
-
Visual preference, calculated as [(mean scores of conditions 3 + 6)/(mean scores of conditions 2 + 5] × 100. It is a measure of the patient’s reliance of visual information, even when that information is incorrect.
(B) Stability limits: the patient’s ability to move his or her centre of gravity (CoG) to eight positions in a circle at a distance of 100 % of the theoretical greatest for the patient’s age of the space represented on the posturograph’s screen [15]. We analysed the following parameters:
-
Reaction time: time from signal movement to start of patient movement.
-
Mean velocity: mean speed of CoG movement as degrees per second.
-
Endpoint excursion: distance travelled by CoG in first attempt to attain the target.
-
Maximum excursion: longest distance travelled by CoG during the test. It can differ from the above if corrective movements are attempted because the first attempt fell short.
-
Directional control: comparison between quantity of movement in the object’s direction and the quantity of movement in another direction.
-
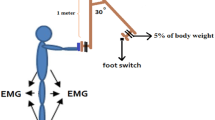
(C) Rhythmic weight shift (RWS): this test quantifies the patient’s ability to move their COG from left to right (lateral) and forward to backward (anterior/posterior) between two targets at three different speeds (slow, medium and fast). The test outcome variables were the mean speed of COG movement in the desired direction and the directional control.
-
Modified TUG. In the standard test [17], the subject rises from a chair (without arm support), walks 3 m towards a wall, turns around and returns to sit on the chair. In the modified test [20], when the patient returns to the chair, he or she has to walk around it once before sitting (an additional 180° turn). We analyse the time taken to perform the test and the number of steps required.
All the patients completed the following questionnaires:
-
The Spanish version of the DHI [21]. It assesses the disability induced by balance disorders in daily life activities. It comprises 25 questions divided into three groups (9 on the functional scale, 9 on the emotional scale and 7 on the physical scale), with three possible answers: yes (4 points), sometimes (2 points) and no (0 points). The highest score (representing the greatest disability) is therefore 100.
-
Short falls efficacy scale-international (FES-I) [22]. It is a shortened version to assess fear of falling during seven activities with four possible answers (we use a modification in the score): not at all concerned (0 points), somewhat concerned (1 point), fairly concerned (2 points) and very concerned (3 points). The highest score (severe concern about falling) is therefore 21.
Statistical analysis
The analysis was carried out performing Student’s t test or Mann–Whitney (data distribution was tested by Kolmogorov–Smirnoff test) to examine mean differences between obese and non-obese on continuous variables. Fisher’s exact test was used to assess associations between categorical variables (fallers vs. non-fallers, previous admissions to hospital for fall-related injuries vs. non-previous admissions, gender). Level of statistical significance in all the tests applied was p < 0.05. All analyses were carried out with SPSS version 22.0 (IBM, Armonk, NY) for Windows.
Ethical aspects
The study was conducted according to the Declaration of Helsinki and all the patients granted their consent to participate in the study in writing. The study protocol was approved by our regional committee on research ethics.
Results
The patients presented a mean of 8.16 ± 33.39 falls in the last 12 months (96 of them presented at least one or more falls in the period) and a mean of 0.40 ± 1.29 numbers of admissions to hospital for fall-related injuries (29 of them presented at least one or more in the period).
69 of the patients were included in the obese group (≥30 kg/m2) and 66 in the non-obese group (BMI < 30 kg/m2). The obese group comprised 56 females and 13 males with a mean age of 76.57 ± 5.62 years. The non-obese group was made up of 48 females and 18 males with a mean age of 77.76 ± 7.05 years. There were no statistical differences between the groups by gender (Fisher’s exact test) or age (Student’s t test).
Results of clinical assessment are summarised in Table 1. Patients with obesity took longer to perform the modified TUG and required more steps. Also these patients had poorer scores in the subjective tests (unless physical scale of DHI).
In the CDP there were no significant differences in the SOT nor the LOS, only there was a statistical significant difference in the antero-posterior directional control of the RWS (Table 2).
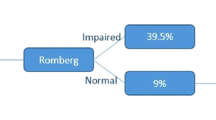
Figure 1 shows the number of fallers in each group, there was a statistically significant difference between the groups (p = 0.013, Fisher’s exact test). In the obese group 16 of the 69 patients presented at least one or more admissions to hospital for fall-related injuries in the last 12 months and in the non-obese group 13 of the 66 patients; there was not a statistical significant difference (p > 0.05, Fisher’s exact test).
Discussion
Our present study shows that obesity interferes in the balance of elderly patients with postural instability putting them at a greater risk of fallings compared to non-obese patients. However, there is no significant difference in the proportion of patients who required hospital admission for fall-related injuries. Previous research has shown inconsistent findings for the association between obesity and falls [13, 14, 23], and not necessarily a higher risk of fall-related injury [14, 23, 24]. One of these studies also highlighted sedentary behaviour, chronic health conditions and medication as mediators for the association between obesity and falls in community living older people [14].
CDP is a promising study to assess postural instability in elderly patients [16]. Previous work had hypothesise that obese individuals could rely more on visual and vestibular to control their balance [25], but we have found that integration of relevant sensory information that contributes to postural control is not affected in obese patients. SOT has the disadvantage that it only measures the ability to perform volitional, quiet stance during a series of six specific conditions. On the other hand, the ability to voluntarily move the COG to positions within the LOS is crucial to mobility tasks such as reaching for objects. Our obese patients have not reduced limits of body stability so they are not more likely to fall as a result of their diminished base of support. Only there is a difference in the anterior-posterior directional control (between the amounts of movement in the intended direction to the amount of extraneous movement) of the RWS. A previous study [26] has found an anterior displacement of the centre mass and a significantly greater ankle torque required to stabilise the body in these patients, so this fact may interfere their directional control too. Functional consequences of an impaired RWS include an inability to meet the timing demands of the environment, such as crossing the street, stepping onto elevators/escalators, and so on. Instability may result when performing activities that require rapid movement speeds, variability in speeds, or changing directions.
Compared with non-obese patients, elderly patients with obesity exhibit slower walking velocity and required a higher numbers of steps. These slower response may be used in an effort to facilitate dynamic postural stability. It is known that a longer TUG time implies greater risk of falling in impaired elderly patients [27] and also a higher number of steps [28].
Obese patients also feel more disabled in performing their daily-activities (specifically in functional and emotional tasks) and their fear of falling is higher.
These findings could be related to the fact that this group has a higher proportion of fallers, and previous studies have shown that falls are associated with significant social and psychological consequences, because patients lose confidence in themselves and thus restrict their physical activity [29].
In essence, our results indicate that obesity interferes in the balance of elderly patients with postural instability, putting them at a greater risk of fallings, performing worse dynamic tasks and feeling more disabled. Although continued education on training balance may be useful in older population, since the obese group shows more rate of fallers, rehabilitation programmes focus on dynamic tasks in these patients could be useful to reduce their fall risk and improve their quality of life.
References
Boult C, Murphy J, Sloane P et al (1991) The relation of dizziness to functional decline. J Am Geriatr Soc 39:858–861
Hale HE, Perkins LL, May FE et al (1986) Sympton prevalence in the elderly. An evaluation of age, sex, disease and medication use. J Am Geriatr Soc 34(5):333–341
Lin HW, Bhattacharyya N (2012) Balance disorders in the elderly: epidemiology and functional impact. Laryngoscope 122(8):1858–1861
Arellano B, Camacho RR (2003) Patología vestibular en el anciano. In: Camacho RR (ed) Trastornos del equilibrio. Un abordaje multidisciplinario. McGraw-Hill Interamericana, Madrid, pp 307–310
Neuhauser HK, von Brevern M, Radtke A et al (2005) Epidemiology of vestibular vertigo. A neurotologic survey of the general population. Neurology 65(6):898–904
Padilla Ruiz F, Bueno Cavanillas A, Peinado Alonso C et al (1998) Frecuencia, características y consecuencias de las caídas en una cohorte de ancianos institucionalizados. Aten Primaria 21(7):437–445
Lord SR, McLean D, Strathers G (1992) Physiological factors associated with injorius falls in older people living in the community. Gerontology 38:338–346
Faraldo-García A, Santos-Pérez S, Crujeiras-Casais R et al (2012) Influence of age and gender in the sensory analysis of balance control. Eur Arch Otorhinolaryngol 269(2):673–677
Basta D, Rossi-Izquierdo M, Soto-Varela A et al (2013) Mobile posturography: posturographic analysis of daily-life mobility. Otol Neurotol 34(2):288–297
Faraldo-García A, Santos-Pérez S, Labella-Caballero T et al (2011) Influence of gender on the sensory organisation test and the limits of stability in healthy subjects. Acta Otorrinolaringol Esp 62(5):333–338
Hue O, Simoneau M, Marcotte J et al (2007) Body weight is a strong predictor of postural stability. Gait Posture 26(1):32–38
Błaszczyk JW, Cieślinska-Swider J, Plewa M et al (2009) Effects of excessive body weight on postural control. J Biomech 42(9):1295–1300
Young Y, Myers AH, Provenzano G (2001) Factors associated with time to first hip fracture. J Aging Health 13:511–526
Mitchell RJ, Lord SR, Harvey LA et al (2015) Obesity and falls in older people: mediating effects of disease, sedentary behavior, mood, pain and medication use. Arch Gerontol Geriatr 60(1):52–58
Nashner LM (2011) Computerize dynamic posturography. In: Goebel JA (ed) Practical management of the dizzy patient. Lippincott Williams & Wilkins, Philadelphia, pp 143–170
Girardi M, Konrad HR, Amin M et al (2001) Predicting fall risks in an elderly population: computer dynamic posturography versus electronystagmography test results. Laryngoscope 111(9):1528–1532
Podsiadlo D, Richardson S (1991) The timed ‘up and go’ test. J Am Geriatr Soc 39:142–148
Ashburn A, Stack E, Pickering RM et al (2001) A community-dwelling sample of people with Parkinson’s disease: characteristics of fallers and non-fallers. Age Ageing 30:47–52
Soto-Varela A, Gayoso-Diz P, Rossi-Izquierdo M et al (2015) Reduction of falls in older people by improving balance with vestibular rehabilitation (ReFOVeRe study): design and methods. Aging Clin Exp Res (In press). doi:10.1007/s40520-015-0362-z
Rossi M, Soto A, Santos S et al (2009) A prospective study of alteration of balance among patients with Parkinson’s disease: protocol of the postural evaluation. Eur Neurol 61(3):171–176
Pérez N, Garmendia I, Martín E et al (2000) Adaptación cultural de dos cuestionarios de medida de la salud en pacientes con vértigo. Acta Otorrinolaringol Esp 51(7):572–580
Kempen GI, Yardley L, van Haastregt JC et al (2008) The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 37(1):45–50
Lin HW, Bhattacharyya N (2014) Impact of dizziness and obesity on the prevalence of falls and fall-related injuries. Laryngoscope 124:2797–2801
Himes CL, Reynolds SL (2012) Effect of obesity on falls, injury, and disability. J Am Geriatr Soc 60(1):124–129
Simoneau M, Teasdale N (2015) Balance control impairment in obese individuals is caused by larger balance motor commands variability. Gait Posture 41(1):203–208
Corbeil P, Simoneau M, Rancourt D et al (2001) Increased risk of falling associated with obesity: mathematical modeling of postural control. IEEE Trans Neural Syst Rehabil Eng 9:126–136
Schoene D, Wu SM, Mikolaizak AS et al (2013) Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc 61(2):202–208
Rossi-Izquierdo M, Basta D, Rubio-Rodríguez JP et al (2014) Is posturography able to identify fallers in patients with Parkinson’s disease? Gait Posture 40(1):53–57
Tinneti ME (2003) Clinical practice, preventing falls in elderly persons. N Engl J Med 348:42–49
Acknowledgments
This study was supported by a grant of the National Institute of Health Carlos III (National R&D&I Plan, dossier PI11/01328).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Human and Animal Rights
The experimental protocol was designed in accordance with the Declaration of Helsinki (1964) and was approved by the Independent Ethics Committee of Galicia (protocol 2010/139).
Informed consent
All study participants provided informed consent.
Rights and permissions
About this article
Cite this article
Rossi-Izquierdo, M., Santos-Pérez, S., Faraldo-García, A. et al. Impact of obesity in elderly patients with postural instability. Aging Clin Exp Res 28, 423–428 (2016). https://doi.org/10.1007/s40520-015-0414-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0414-4