Abstract
Adult ovarian granulosa cell tumor is one of the rare types of malignant tumor, which arises from the sex cord granulosa cell of the ovary. The tumor can arise from different type of gonadal sex cord cells like thecal cells, Sertoli cells, granulosa cells and stromal cells. The specific type of granulosa cell tumor is comprised of thecal cells and fibroblasts. In our case report, we are reporting a case of 63-year-old women with granulosa cell tumor of low-grade malignancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult ovarian granulosa cell tumor [GCT] is one of the rare types of malignant tumor, which arises from the sex cord granulosa cell of the ovary [1]. The tumor can arise from different type of gonadal sex cord cells like thecal cells, Sertoli cells, granulosa cells and stromal cells. The specific type of granulosa cell tumor is comprised of thecal cells and fibroblasts [2]. There are two types of granulosa cell tumors—adult and juvenile [3]. Adult type of tumor is comprised of about 95% while only 5% represent juvenile type which is most commonly seen in prepubertal girls and in younger women with less than 30 years of age [4, 5]. Adult type of cell tumor is the most common type and is usually unilateral, while only 1% of the cases are bilateral. This type of tumor is considered to be a hormone-producing tumor [1]. GCT is diagnosed by immunohistochemistry (IHC) presented with abdominal distension of 3–4, and it reports positive for inhibin, while negative for makers for epithelial types [6].
Case Report
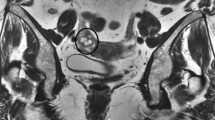
A 63-year-old post-menopausal woman was presented to the OPD of Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India. Patient with a history of hysterectomy done 9 years ago was complained of abdominal distension since 3–4 months. On examining, the patient was moderately thin, weighing 63 kgs. On abdominal ultrasound, a large heterogeneous cystic lesion measuring 26 × 15 × 30 cm with solid component seen in the pelvis extending into abdomen, which suggested to be likely an ovarian neoplasm. Further CT with contrast was done, which suggested multiloculated cystic lesion measuring 24 × 9.9 × 25 cm with evidence of thick septations and irregular eccentric solid components within. There was post-contrast enhancement of septations with no evidence of calcification or hemorrhage. Superiorly the lesion was extended up to epigastrium and laterally displacing the bowel loops with maintained fat plane between the lesion and bowel loops, anteriorly abutting the abdominal wall. It was also observed that small homogenously enhancing omental lymph node was measuring 10 × 6 mm. The large pelvic abdominal multiloculated cystic lesion in the left adnexa was described as malignancy, which was likely to be mucinous cystadenocarcinoma. Tumor markers such as CA 19.9, CA 125 reports were well within the normal limits.
Exploratory laparotomy was done with bilateral oophorectomy and appendectomy on July 8, 2022, under general anesthesia and epidural anesthesia. Peritoneal fluid, which was seen on opening the abdomen, was collected and sent for analysis. Abdominal mass of 24 × 25 cm was attached to the mesentery of sigmoid colon. Another mass measuring 20 × 18 cm was adherent to the omentum (Figs. 1 and 2). Cyst wall was thick; multiple loculi with thick and thin septa were seen, which was mostly filled with fluid. Left ovary, omentum and appendix were normal. Specimen was sent to histopathological evaluation. Frozen section impression was suggestive of mesenchymal neoplasm. Post-operative period was uneventful and was discharged on 7th post-operative day.
The peritoneal fluid collected suggested negative for malignancy. Histopathological reports suggested that both the masses were capsulated and intact. The tumor cells had characteristic feature of ovarian sex cord stromal tumor that is granulosa cell tumor of adult type. Occasionally call exner bodies was noted. FIGO stage was reported as IA. Immunohistochemistry reports were consistent with adult granulosa cell tumor. The IHC markers were negative for pan CK, while inhibin showed moderate and diffuse granular cytoplasmic staining of tumor cells and calretinin showed weak-to-moderate nuclear and cytoplasmic staining of tumor cells. On re-reviewing the slides, it was reported as: (1) adult granulosa cell tumor of right ovary. The capsule was intact in the sections studied. (2) Right-sided paratubal cyst was seen with unremarkable fallopian tube.
Patient was followed up after 3 months. An abdominal USG scan was done, which showed a small 2-cm growth in abdominal region. Presuming it to be recurrence or relapse, patient was suggested for contrast CT. Report suggested as multiloculated cystic lesion in the mesentery of the left lumbar region measuring approximately 36 × 37 × 35 mm (CC × AP × TR), which shows multiple nodular enhancing septations with no evidence of retroperitoneal or mesenteric lymphadenopathy. A patient was further followed up for every 3 months for clinical examination. In May 2023, when repeat USG was done a well-defined multiloculated cystic lesion measuring 6.9 × 2.9 cm with multiple thin septae on the left side of pelvis was observed. After 2 weeks, patients developed severe pain with cramps in the left side of abdomen and was taken for USG to note on the changes. Report suggested of complex solid and cystic mass lesion measuring 8.7 × 6.0 × 6.1 cms was noted in left lower abdomen, and vascularity could not be demonstrated.
PET CT was done, which was reported as large heterogeneously enhancing lobulated soft tissue lesion with solid components and areas of central necrosis with metabolic activity along its periphery, which was noted in the left lower abdomen measuring 6.5 × 6.3 × 5.7 cm. It also suggested of solid components within the lesion, and areas of internal bleed. FDG uptake was noted along the periphery [Max SUV 6.4]. There was a significant perilesional stranding. The lesion was closely abutting the transverse colon and part of small bowel loops with no significant infiltration. There were no features of obstruction, and the lesion was closely abutting the left lateral abdominal wall, with mild free fluid. They also reported that there was no FDG avid or enhancing lesion in peritoneum or in omentum with no significant enlarged retroperitoneal lymph nodes.
Considering this report, surgery was planned for the removal of lesion immediately. Midline laparotomy with cytoreduction surgery was done on June 23, 2023. Adhesiolysis, total omentectomy with omental mass, was excised. Findings during the surgery were—10 × 8 cm hematoma with underlying mass in greater omentum with adhesions to mesocolon was found (Fig. 3); rest of the omentum was normal. Liver, stomach, small and large bowel, mesentery was inspected in detail and was found to be normal. There was no free fluid. Specimen was sent to histopathological evaluation. Patients’ post-operative period was uneventful. Histopathology reports showed fibro fatty tissues with areas of hemorrhage surrounded by spindle cell fibroblast with capillary proliferation, with atypical cells. Features were suggestive of organizing hematoma.
Discussion
Granulosa cell tumor is considered to be a low-grade ovarian tumor, which is known to arise from granulosa cells of the sex cord. The peak incidence of this type of tumor is between the age group of 55 and above [7]. A case reported by Moustaide et al. has an age group ranging from 51 to 81 years [8]. Adult type of granulosa cell tumor is one of the rare type among all the other type of ovarian tumors. We have reported a case of 63 years old with unilateral adult-type granulosa cell tumor. As per the literature review, the granulosa cell tumor varies in their gross appearance, which can be major present as enlarged cystic and solid ovarian mass, while sometimes it can be similar to mucinous cystadenoma, which was similar to the report suggested in our CT report.
A report by S. Kayastha [9] and Miller [10] also had similar radiological findings where large pelvic mass measured up to 12 cm in diameter with solid and multicystic component. The size of mass correlates with the prognosis of the tumor. Inhibin is a usual tumor marker for both primary and recurrent diseases [11]. In our study, inhibin A and B was done postoperatively after the final histopathology report, which was due to low level of suspicion.
Treatment modalities depend on individual’s age, stage and future fertility plan. Laparoscopic management is controversial. Exploration of cases managed with laparoscopy is known to have peritoneal disease [12]. However, Nakayama et al. [13] have shown that laparoscopic outcome is reasonable with similar outcome as in laparotomy.
In the histopathological report, the stromal cell showed areas of atheromatous stroma, hemorrhage and scattered lymphoplasmacytic infiltrate. While second surgery showed fibro fatty tissues with areas of hemorrhage and suggested hematoma. As this case being on the lower grade of tumor, no further chemotherapy was suggested. Regular clinical follow-up was suggested along serum inhibin levels were advised every 3 months, which was normal and once in 6 months contrast CT.
Conclusion
Surgery is considered to be the mainstay in the treatment, while chemotherapy is advised only in advanced stages. Serum inhibin is considered to be the tumor marker, which need to be done post-surgery to correlate with the histopathological report. Hence, frequent and long-term follow-up is required as granulosa cell tumor is considered as late recurring tumor.
References
Kaur K, Kaur M, Singla N, Kaur A. Bilateral ovarian adult granulosa cell tumor: a rare case presentation. Int J Curr Res. 2018;10(10):74591–2.
Joshi R, Baral G, Malla K. Ovarian adult granulosa cell tumor: a rare case report. Nepal J Obstet Gynaecol. 2018;13(1):57–60.
Agius T, Gatt M, Falzon D, Babic D. A complex case of a granulosa cell tumour. BMJ Case Rep CP. 2021;14(12):e242224.
Classification of tumors of the ovary. In: kurman RJ, Carcangiu ML, Herringtom CS, Younf RH, editors. WHO classifiaction of tumors. 4th edition. Lyon. IARC; 2014
Ray-Coquard I, Morice P, Lorusso D, Prat J, Oaknin A, Pautier P, et al. Non epithelial ovarian cancer. ESMO clinicla practice guidelines for diagnosis, treatment and follow up. Ann oncol. 2018;29:1–18.
Movahedi-Lankarani S, Kurman RJ. Calretinin, a more sensitive but less specific marker than α-inhibin for ovarian sex cord-stromal neoplasms: an immunohistochemical study of 215 cases. Am J Surg Pathol. 2002;26(11):1477–83.
Kottarathil VD, Antony MA, Nair IR, Pavithran K. Recent advances in granulosa cell tumor ovary: a review. Indian J Surg Oncol. 2013;4(1):37–47.
Moustaide H, Taheri H, Benkirane S, Saadi H, Mimouni A. Ovarian adult granulosa cell tumor: report of 3 cases. J Clin Case Rep. 2017;7:2.
Kayastha S, Chitrathara K, Sigdel B, Sanam P, Anupama S, Remi A, Augustine T, Peter BC. Adult granulosa cell tumor of ovary: clinical study of 10 cases. Indian J Gynecol Oncol. 2020;18:2.
Miller BE, Barron BA, Wan JY. Prognostic factors in adult granulosa cell tumor of the ovary. Cancer. 1997;79:1951–5.
Lappöhn RE, Burger HG, Bouma J, Bangah M, Krans M, De Bruijn HW. Inhibin as a marker for granulosa-cell tumors. N Engl J Med. 1989;12:790–3.
Salani R, Goodrich K, Song C, Grumbine FC. Three case reports of laparoscopic management of granulosa cell tumor with intraoperative rupture and subsequent upstaging. J Minim Invasive Gynecol. 2008;15:511–3.
Nakayama J, Saks E, Pelkofski E, Edwards J, Stine JE, Secord AA, Gehrig PA, Duska L. Laparoscopy compared to laparotomy in the management of granulosa cell tumors of the ovary. Gynecol Oncol. 2015;137:168.
Acknowledgements
We the authors thank our pathology team for their efforts and suggestions. We extend our gratitude to Dr. Suraj Manjunath and Dr. Elvis Peter Joseph who were helpful in suggesting the case scenario. We thank patient for providing us with the case details.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dwajani, S., Rajeev, N., Shreya, M.S. et al. Extra Ovarian Adult Granulosa Cell Tumor: A Rare Clinical Case Report. Indian J Gynecol Oncolog 22, 22 (2024). https://doi.org/10.1007/s40944-023-00776-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-023-00776-8