Abstract
Granulosa cell tumors constitute less than 5 % of all ovarian tumors. Unlike epithelial ovarian tumors, they occur in a younger age group, are usually detected in an early stage and often have features of hyperestrogenism. The presenting symptoms are usually nonspecific with abdominal pain or distension. They follow an indolent course and are characterized by a long natural history. Mutation of FOXL2 (402C->G) seen in 97 % of adult GCT may be pathognomonic for adult GCT. Only stage of the disease has been consistently shown in various studies to affect survival of patients with GCT. The initial management of patients, for whom fertility is not an issue, is total abdominal hysterectomy, bilateral salpingo-oophorectomy and removal of all gross disease. Nodal dissection is not a significant factor for survival and is not recommended in surgical staging of GCT. Fertility preserving surgery with unilateral salpingo-oophorectomy is feasible in young patients with stage Ia GCT. Patients with early stage disease (stage I and II) have a very good prognosis with 5 year DFS and OS of 89 % and 99 % respectively and these groups of patients usually don’t require any postoperative treatment. Patients with stage Ic disease associated with poor prognostic factors like large tumor size or high mitotic index and stage II, have a higher chance of relapse, and may benefit with postoperative treatment but role of chemotherapy is still debatable. In advanced stage disease (stage III and IV) the 5 year DFS and OS disease was 72 % and 80 % respectively hence the option of postoperative treatment with 6 cycles of BEP should be considered in this group. Recently paclitaxel is being investigated as an effective tool in GCT. The efficacy of radiation in GCT is not well defined but in optimally debulked cases postoperative radiation is a viable option. Due to high chance of recurrence even years after apparent clinical cure of the primary tumor, lifelong follow up with clinical examination and tumor markers like inhibin B is recommended. About 25 % GCT develop recurrence and the median time to recur is usually 4–5 years. Most recurrences are intraperitoneal and usually a complete debulking of the disease is feasible even in the recurrent setting. Postoperative chemotherapy (platinum based) is usually given after surgery more so in cases with widespread disease or after suboptimal cytoreduction. Recurrent chemoresistant, progressive non-responding GCT or patients with high surgical risk are ideal candidates for targeted therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Granulosa cells are the somatic cells of the sex cords of the ovary which are closely associated with the developing oocyte. Granulosa cells differentiate from either the coelomic epithelium or mesenchymal precursors (the embryological origin is still disputed). The major functions of granulosa cells include the production of sex steroids and various peptides required for folliculogenesis and ovulation.
Granulosa cell tumors (GCT) are derived from the granulosa cells. They constitute less than 5 % of the ovarian tumors and more than 70 % of the sex cord-stromal tumors. There are two distinct histological types—adult GCT (AGCT) and juvenile GCT (JGCT) which display different clinical and histopathological features. AGCTs are more common and are usually seen in perimenopausal and postmenopausal women, with a peak incidence at 50–55 years. JGCTs are rare tumors, representing 5 % of all GCTs and occurring in premenarchal girls and young women.
What makes them different from the epithelial ovarian cancers is the nature of presentation and clinical behaviour. They occur in a younger age group, are usually detected in an early stage and often have features of hyperestrogenism. They are more readily cured by surgery alone. Generally they have a better prognosis than epithelial ovarian tumors and follow an indolent course. They are characterized by a long natural history and 25 % may recur years after apparent clinical cure of the primary tumour. There has been a lot of interest in the molecular pathogenesis of these tumors and due to their origin from the granulosa cells, they are potential targets for hormonal and targeted therapy.
Etiology and Risk Factors
The age standardized incidence of GCT varies from 0.58 to 1.6/100,000 women per year [1–3]. GCT are seen in the premenopausal or early postmenopausal age group and the median age of diagnosis is 51 years, in the range of 9–93 years [4]. Lee et al. showed that 9.7 % of GCT in their series were juvenile GCT (JGCT) with the mean age at diagnosis of 20 years (range 8–45 years). More than 50 % were diagnosed before 20 years and 45.5 % were premenarchal [5].
Chromosomal abnormalities have also been recently evaluated in granulosa cell tumors. Detected abnormalities include trisomy 12, monosomy 22, and deletion of chromosome 6. Among juvenile granulosa cell tumors, cytogenetic studies have identified trisomy 12 and a deletion in chromosome 6q. BRCA1 and BRCA 2 mutations are not associated with an increased risk of GCT.
Few tumor predisposition syndromes associated with GCT are Peutz Jeghers syndrome and Potters syndrome. Ollier disease and Maffucci disease are associated with juvenile GCT.
Continuous exposure to ovulation induction drugs like selective estrogen receptor modulators (SERM), clomiphene citrate, gonadotropins may increase the risk of GCT.
The Molecular Genetics of GCT
FOXL2 gene encodes the transcription factor required for the normal development of the granulosa cell. Shah et al. detected a somatic missense muation in FOXL2 (c.402C- > G; p.C134W) in GCT. This mutation was seen in 86 of 89 (97 %) adult GCT, 1 of 10 (10 %) juvenile GCT and 3 of 14 (21 %) thecomas. The high frequency of mutation suggests this mutation may be pathognomic for AGCT, and the absence of this mutation in JGCT shows that JGCT may be an entirely different tumor [6].
Granulosa cell proliferation is dependent on different signalling pathways and any alteration of these pathways leads to uncontrolled proliferation of these cells and the formation of GCT. Understanding the role of these pathways involved in the pathogenesis of GCT helps in the use of novel drugs to treat GCT especially in the recurrent scenario [7].
-
1.
Adenyl cyclase/cAMP/protein kinase A (PKA) pathway is stimulated by action of follicle stimulating hormone (FSH) on FSH receptors. Hence hormonal therapies that decrease gonadotropins can be effective in GCT [7].
-
2.
MAPK and phosphatidyl innositol 3-kinase- PI3K/AKT pathway is stimulated by action of epidermal growth factor (EGF) related growth factors on tyrosine kinases receptors. Use of tyrosine kinase inhibitors like imatinib, geftinib, erlotinib and lapatinib can be tried in GCT [7, 8].
-
3.
Vascular endothelial growth factor (VEGF) and its receptors are involved in angiogenesis. Trials evaluating the role of sunitinib, pazopanib, bevacizumab are underway [9–11].
-
4.
Estrogen receptors activated with estrogen have a tumorigenic action. Estrogen can also act on the neighboring stromal tissue and via angiogenesis to promote tumor growth. Suppression of endogenous estrogen will provide an antiproliferative milieu which could be effective in treating GCT [12].
-
5.
Nuclear factor kB (NFkB). Certain studies show that the increased cell proliferation and escape from apoptosis seen in GCT is mediated by NFkB. Bortezomib, a proteasome inhibitor targets NFkB to inhibit cell proliferation and viability while stimulating apoptosis [13].
-
6.
TNF-related apoptosis-inducing ligand (TRAIL; CD253) via its receptors TRAIL-R1/DR4 and TRAIL-R2/DR5 induce cell death in malignant cells with minimal damage to normal tissue. Recombinant human TRAIL (rhTRAIL) and DR4/DR5 specific monoclonal antibodies are under study in various phase II trials [14, 15].
Tumor Markers
Tumor markers are useful in early detection of recurrence. In GCT secreted hormones are used as tumor markers.
-
a)
17b- Estradiol (E2)
E2, the principle female sex hormone, is formed from androstenedione by the action of cytochrome P450 aromatase. Due to unregulated aromatase action, high estrogen level is seen in GCT. But the role of E2 as a tumor marker is limited as no corelation was noted between E2 levels and disease progression or recurrence in most cases. This may be due to lack of theca cells seen in 30 % cases of GCT. Thus E2 can be helpful in postoperative management of certain cases but is not sensitive enough to be used as a reliable tumor marker.
In androgen secreting GCT, testosterone or its precursors can be used as tumor markers.
-
b)
Inhibin
Inhibins are mainly formed in granulosa cells and are made of two subunits, an a subunit covalently bound to either bA or bB subunit forming inhibin A and inhibin B respectively. In the postmenopausal women, with depletion of ovarian follicles, inhibin levels become undetectable. But in GCT, inhibin levels are elevated, thus inhibin can be used as a marker for GCT in premenopausal and postmenopausal women. Lappohn et al. [16] first demonstrated the efficacy of inhibin as a marker for both primary and recurrent disease and showed a rise in inhibin levels preceeded clinical recurrence as early as 20 months. Newer studies using subunit specific ELISA showed inhibin B to be the major form secreted in GCT, and that inhibin B was more accurate than inhibin A in detecting GCT. Inhibins act as autocrine and paracrine granulosa cell growth factors and levels of inhibin reflect the tumor burden [17–19].
However not all tumors express inhibin and loss of inhibin expression may be associated with poor prognosis as these tumors are usually poorly differenciated tumors [20]. Epithelial ovarian tumors especially the mucinous variety may also secrete inhibin (82 % cases); showing inhibin is not specific for GCT. Inhibin levels fall to normal range around 1 week after tumor removal, suggesting inhibin could be secreted either by the tumor tissue or surrounding normal ovarian tissue [21].
-
c)
Mullerian InhibitingSubstance(MIS)/ Anti Mullerian Hormone (AMH)
MIS are formed in granulosa cells during reproductive life. MIS are cyclically elevated during the menstural cycle but are never more than 5 mcg/L. MIS becomes undetectable in postmenopausal women. An elevated level of MIS is highly specific for GCT. MIS parallel changes in inhibin levels in GCT and predate clinical recurrence as early as 11 months [21]. Several studies show MIS to be a reliable tumor marker with sensitivity between 76 % and 100 % [22, 23]. Anttonen et al. found reduced MIS expression in 87 % tumors more than 10 cm in size suggesting MIS may be less useful in advanced disease [24].
Further studies are required before deciding which among the tumor markers could be most reliable in detection and management of GCT. One retrospective study suggests MIS to be more sensitive and reliable than inhibin [25].
-
d)
Follicle Regulatory Protein (FRP)
FRP is secreted by granulosa cells and is detected in normally mensturating women. Regulation of secretion occurs with granulosa cell differenciation. Elevated levels of FRP have been noted in few cases of GCT but its clinical significance is yet to be confirmed [21].
Pathology
GCT usually appears as a large unilateral mass having a tan yellow color due to steroid production. It often has solid and cystic areas. They are usually >10 cm in size (73.5 %) but can vary from a small nonpalpable lesion to large masses (3–24 cm) [1]. JGCT average around 12.4 cm (5–26 cm) [5].
Granulosa cells are small round to oval pale cells with characteristic coffee- bean nuclei (longitudinal nuclear grooves). Well differentiated GCT have a microfollicular, macrofollicular, trabecular, insular, solid-tubular and hollow tubular patterns. Microfollicular patterns are the most common pattern seen and have the characteristic Call-Exner bodies which are small rings of granulosa cells surrounding shrunken nuclei or eosinoplilic fluid material. Call Exner bodies are seen in 30 % of cases [5]. The poorly differentiated forms (39 %) [4] appears as undulating parallel (watered-silk) or zigzag (gyriform) rows of granulosa cells in a single file and diffuse (sarcomatoid) pattern characterized by a monotonous appearance. GCT with a diffuse pattern can be mistaken for a poorly differentiated carcinoma in frozen section. The nuclear pattern can help in clinching the diagnosis. The nuclei of GCT are uniform and pale while undifferentiated carcinomas have hyperchromatic, ungrooved nuclei of unequal size and shape. Nuclear atypia and multiple mitotic figures are common in undifferentiated carcinomas unlike GCT [26].
In difficult cases immunohistochemistry can help clinch the diagnosis. GCT is alpha inhibin and calretinin positive [27]. Advanced stage disease has weaker expression of inhibin, demonstrating a lesser degree of normal cellular function [28]. These tumours on IHC are nonspecifically positive for CD99, CAM 5.2, AE1/AE3, CD10, S100, WT-1, smooth muscle actin and desmin. They are negative for CK7 and EMA [29].
Endometrial cancers, usually detected in the pathological specimens, are well differentiated early stage disease.
Testing for FOXL2 mutation can aid in detection of problematic cases as 97 % of adult GCT showed mutation of this gene [6].
On microscopic examination, two characteristics distinguish juvenile from adult granulosa cell tumors: the nuclei of juvenile granulosa cell tumors are rounded, hyperchromatic and ungrooved with moderate to abundant eosinophilic or vacuolated cytoplasm, and the theca cell component is luteinized [26].
Clinical Presentation and Diagnosis
Similar to epithelial ovarian cancers the presenting symptoms are usually nonspecific with abdominal pain (41.1 %) or distension (26.4 %) [1]. These patients present with a large palpable ovarian mass. In JGCT abdominal pain was seen in 28.3 % and abdominal mass in 45.5 % [5].
Symptoms related to hyperestrogenesim occur in all age groups. In prepubertal age group, precocious puberty with breast development increased pubic hair, vaginal bleeding (27.3 %) [5] and increased growth will be seen. In the reproductive age group, altered menstural patterns (32.8 %) [1] like menorrhagia, intermenstural bleeding or amenorrhoea may manifest. Postmenopausal bleeding is the most common finding in the postmenopausal age group.
Around 25–50 % cases are associated with endometrial hyperplasia and endometrial cancer is seen in 5–13 % cases. Endometrial cancers, usually detected in the pathological specimens, are well differentiated early stage disease and have a good prognosis. Primary uterine cancer with ovarian metastasis or synchronous endometroid ovarian and uterine cancer has to be excluded in cases of uterine adenocarcinoma with an ovarian mass. Breast enlargement and tenderness occurs secondary to estrogen action [26].
Secondary to high inhibin levels patients can present with infertility. Androgen secreting GCT, which may have a sertoli- leydig cell component, can cause virilizing symptoms and hirsuitism. At times torsion ovary presents with acute abdominal pain. Because of the high vascularity, tumor rupture is seen in 10 % cases, and presents with acute abdominal pain, abdominal distension and hypotension due to hemoperitoneum [21].
Unlike epithelial tumors, GCT presents at early stage in 81 % cases (stage I-71 %, II-10 %) and at late stage in 19 % (III-11 %, IV-8 %) [4]. In advanced stages, the pelvis, intra-abdominal organs and peritoneum are involved. It’s unusual for patients to present with pulmonary and skeletal metastasis.
Radiologically GCT can appear either as a solid mass, a mass with haemorrhagic or fibrotic changes, a multilocular cyst or a completely cystic tumor. Unlike epithelial tumors GCT are usually confined to the ovary at diagnosis, don’t have intracystic papillary projections. The incidence of peritoneal spread is low and they are rarely bilateral. Enlarged uterus with a thickened endometrium is noted due to estrogenic action. Ascites is very rarely seen [30, 31].
Differential diagnosis of patients with adnexal mass and abnormal vaginal bleeding
-
1.
Primary uterine cancer with metastasis to the ovary.
-
2.
Primary ovarian cancer with metastasis to the endometrium.
-
3.
Synchronous ovarian and endometrial cancer
Prognostic Factors
The efficacy of prognostic factors in GCT has been taken from a number of retrospective studies. Various factors shown to have prognostic significance include age, tumor size, rupture of tumor, mitotic activity, nuclear atypia, aneuploidy (in 5–20 % GCT), p53 overexpression, high Ki-67 and stage of the disease [1–6, 32–38].
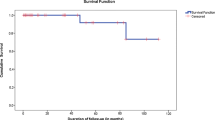
Only stage of the disease has been consistently shown in various studies to affect survival of patients with GCT. In a recent study by Park et al. [39] the 5 year DFS and OS rates in early stage (stage I and II) disease was 89 % and 99 % respectively while in advanced stage (stage III and IV) disease it was 72 % and 80 % respectively. The 10 year DFS and OS rates in early stage (stage I and II) disease was 89 % and 90 % respectively while in advanced stage (stage III and IV) disease it was 57 % and 67 % respectively (Table 1).
The overall 25 year survival rate ranges from 40 % to 60 %.
Complete surgical debulking of the disease is essential in GCT as the presence of postoperative residual lesions was shown to reduce survival from 82 % to 22 %. In the study by Ranganathan et al. [1] median survival of patients who underwent optimal cytoreduction was 60 months in contrast to 19 months for those who did not. In this study 76.5 % patients underwent primary optimal cytoreduction. All the patients who were unable to undergo optimal cytoreduction died of disease. Chan et al. [32] have shown that absence of residual disease is a predictor for improved survival.
The effect age plays on prognosis is controversial. A recent study by Lee et al. [5] has shown a high recurrence rate in patients less than 40 years. When comparing the survival of patients less than 40 years to those older than 40 years the 5 and 10 year disease free survival rates reduced from 93 % to 82 % and 84 % to 48 % respectively. However other studies have shown an improved prognosis in younger patients [4, 32, 33].
There are a number of conflicting reports on the efficacy of other prognostic factors. Few studies [2, 32] have shown that tumors more than 10 cm–15 cm have a higher chance of recurrence and poorer survival.
A study evaluating the significance of tumor rupture showed a decrease in 25 year survival from 86 % in patients with stage I a disease to 60 % in patients with stage I c. In a study of patients whose tumors had a mitotic index <4 /10 HPF the DFS at 80 months was 90 % compared to 25 % for patients with a higher mitotic index. In a study comparing the 25 year survival rate in patients with mild nuclear atypia to those with marked atypia a fall in survival from 80 % to 60 % was noted. Tumors with a follicular pattern supposedly had a better survival rate compared to tumors with a diffuse or insular histological pattern [21].
Grade I and II tumors had better survival compared to grade III tumors. The disease specific survival at 5 and 10 years for grade I and II tumors was 96 % and 86 % respectively while the disease specific survival at 5 and 10 years for grade III tumors was 64 % and 59 % respectively [4].
However other studies have not validated the significance of these prognostic factors.
GATA-4 promotes granulosa cell proliferation. Immunohistochemistry studies showed high GATA-4 activity in GCT which positively correlated to the clinical stage (Ic and above) and risk of recurrence. This can be used as an important tool to predict tumor aggressiveness [40].
Treatment and Disease Management
GCT are usually diagnosed from the pathology specimen although a preoperative diagnosis can be suspected based on presence of an adnexal mass with features of hyperestrogenism, thickened endometrium and elevated serum inhibin
Surgical Management
Surgical staging remains the initial management of a suspected case of GCT. The principles of surgery are similar to epithlial ovarian tumor with a vertical midline incision. Surgical staging includes exploration of peritoneal cavity, washings for cytology, multiple peritoneal biopsies and omentectomy. According to Thrall et al. [41] secondary surgical staging is necessary in unstaged cases of GCT as the stage was upstaged in 2 of 8 cases. Lee et al. [5] showed that 18.6 % had ascites of which 5.9 % had malignant cells. Peritoneal wash was positive in 11.8 % cases. 27.3 % of JGCT had ascites but none had malignant cells. Preoperative tumor rupture was seen in 17.6 % and 27.3 % cases of AGCT and JGCT respectively
Several studies [39, 41–43], Table 2, evaluating the role of lymph node dissection have shown that nodal dissection is not a significant factor for survival and is not recommended in surgical staging of GCT. Enlarged or suspicious nodes should be removed to allow evaluation and maximal cytoreduction. In the series by Brown et al. [42] none of the 58 patients who had nodal sampling had positive nodes.
Optimal cytoreduction to no residual disease was achieved in 98 % cases of AGCT and 99.9 % cases of JGCT. In Lees series of 11 JGCT, 81.8 % underwent unilateral salpingoovariotomy, one had cystectomy and one had total abdominal hysterectomy with bilateral salpingoovariotomy [5]. In a larger series of 106 cases Park et al. achieved 100 % optimal debulking even in cases of advanced stage [39] and none of the patients with early stage disease who underwent optimal debulking had tumor recurrence.
In patients where fertility is not an issue, a total abdominal hysterectomy and bilateral salpingo-oophorectomy with removal of all gross disease is the definite initial treatment. Fertility preserving surgery with unilateral salpingo-oophorectomy is feasible in young patients with stage Ia GCT. The results of various studies have shown that, there is not much difference with a conservative approach when compared to the radical surgery 97 % vs. 98 % respectively. The 5 and 10 year disease specific survival was 97 % and 94 % [4]. As the incidence of bilateral disease is low (2 %) [1] a wedge biopsy of the opposite ovary is controversial and must be done with caution. In the series by Lee et al. none of the JGCT were bilateral. He showed an incidence of 2 % for a co-existing uterine cancer (which should be ruled out with an endometrial biopsy). 9.8 %, 1.1 %, 2 % and 2.9 % had simple hyperplasia without atypia, simple hyperplasia with atypia, complex hyperplasia without atypia, complex hyperplasia with atypia respectively. After child bearing is complete, completion surgery with removal of the other ovary and hysterectomy is a reasonable but controversial option.
-
Indications for preoperative endometrial biopsy
-
All women with abnormal uterine bleeding
-
All postmenopausal women with adnexal mass and thickened endometrium (>5 mm)
-
Suspected granulosa cell tumour and planning for fertility sparing surgery
Chemotherapy
Postoperative treatment with platinum based chemotherapy may be the treatment of choice due to ease of administration, wider accessibility and better tolerance. Postoperative radiation in GCT has not been widely used. Only 2.1 % received radiation in one of the largest series of GCT [4]. While around 30.4 % of AGCT and 32.3 % of JGCT received CT with BEP [5].
Patients with early stage disease (stage I and II) have a very good prognosis with 5 year DFS and OS of 89 % and 99 % respectively and these groups of patients usually don’t require any postoperative treatment. Few studies have shown that patients with stage Ic disease associated with poor prognostic factors like large tumor size or high mitotic index have a higher chance of relapse and may benefit with postoperative treatment [1–5, 32–38]. But due to the rarity of GCT, these data have been collected from retrospective studies and case reports and it’s impossible to conduct a randomized controlled trial to assess the efficacy of postoperative treatment in high risk patients. Thus we still don’t have the evidence showing postoperative treatment in the adjuvant setting can confer a survival benefit in high risk patients.
In advanced stage disease (stage III and IV) the 5 year DFS and OS disease was 72 % and 80 % respectively hence the option of postoperative treatment should be considered in this group. Park et al. [39] recommends optimal debulking followed by 6 cycles of BEP chemotherapy for advanced stage GCT. In this series none of the patients with advanced stage GCT who received at least 6 cycles of BEP had tumor recurrence. For patients with gross residual disease and stage IV disease chemotherapy is the mode of treatment.
Platinum based chemotherapy is often considered for GCT either alone or in combination with doxorubicin and cyclophosphamide (CAP) [45–47], vinblastine and bleomycin (PVB) [48–50], etoposide or etoposide and bleomycin (BEP) [51–53]. The response rates (RR) have varied from 60 to 93 % and duration of response 5–58 months (Table 3).
Gershenson et al. [45] reported an overall RR of 63 % among eight patients with metastatic stromal tumors. In another series, out of ten patients treated with CAP, five patients had a complete response (CR) and one had a partial response (PR) with a total response rate of 60 % [46].
Better response was noted with use of PVB. Colombo et al. [48] treated 11 patients with metastatic /recurrent GCT with PVB. Six patients had a CR and three patients had a PR with overall RR of 82 %. Other series have shown responses from 66 % to 93 %. But there was a high incidence of neutropenic sepsis and bleomycin induced pneumonitis.
To reduce the toxicity seen with PVB, vinblastin was replaced with etoposide. Gershenson [51] used BEP regimen for six cases with metastatic disease, two patients had a CR and three patients had PR with overall RR of 83 %. Median progression free survival was 14 months and median survival was 28 months. The largest study evaluating BEP as first line therapy in stromal tumors was by the Gynecologic Oncology Group [52]. 69 % of patients with advanced disease and 51 % with recurrent disease remained progression free over 3 years. Unfortunately etoposide is myelotoxic with a small risk of secondary acute myeloid leukemia; although it has less peripheral neuropathy compared to PVB.
Paclitaxel [54] alone or in combination with a platinum based agent is being investigated as an effective tool in GCT. Brown et al. compared the effects of BEP to taxanes. In newly diagnosed cases the RR was similar in the two groups (82 %). Median PFS was 46 months for BEP and >52 months for taxane and median OS was was 97 months for BEP and >52 months for taxane. For recurrent disease the RR (71 % vs 37 %) and median PFS (11 vs 7 months) for BEP vs taxane respectively were not statistically significant, although BEP may be a better tool in the recurrent setting.
Radiotherapy
The efficacy of radiation in GCT is not well defined. There are no prospective trials showing the benefit with radiation. Few studies have shown improved DFS in advanced and recurrent GCT, but this has not been validated in other studies.
Hauspy [28] treated 31 of 103 patients with adjuvant radiation. Eight patients received only pelvic radiation (41 Gy in 21 fractions) and 23 patients received whole abdominal radiation (23 Gy in 22 fractions) with a pelvic boost (45 Gy in 29 fractions). The median DFS was 251 months for patients given adjuvant radiation vs 112 months for patients who did not receive adjuvant radiation (HR, 0.4;95 % CI, 0.2–0.8, p = 0.02). Only 32 % cases recurred after radiation compared to 40 % who did not undergo radiation. Pelvic recurrence in radiated fields was only 10 % significantly lower than that in non radation cases (32 %, p = 0.03). In the upper abdomen the failure rate was similar in both groups (26 %). The DFS was prolonged by >10 years with radiation but the likelihood of recurrence was not altered. However they caution that as there was no survival advantage for adjuvant radiation and treatment at the time of recurrence may also be effective, radiation need only be offered when the tumor can’t be fully resected so as to avoid leaving behind microscopic residual disease.
Pankratz et al. [55] treated 48 of 61 cases of GCT with adjuvant radiation (20–30 Gy to abdomen and 30–50 Gy to the pelvis) and concluded radiation conferred an improved survival.
In the series by Savage et al. [56] 4 of 8 patients treated with radiation (for incompletely resected advanced disease) achieved a CR and three had DFI of at least 4 years.
Wolf et al. [57] in a study of 14 patients with advanced or recurrent disease showed that six patients had CR. Three patients remained in remission for 10–21 years while three patients relapsed by 4–5 years after radiation.
Hence the role of radiation in GCT is still debatable but in optimally debulked cases postoperative radiation is a viable option.
Recurrent GCT
GCT have a tendency for late recurrence. Once the tumor recurs it’s fatal in 80 % cases. In the study by Park et al. [39], none of the patients with early stage disease who underwent optimal debulking had tumor recurrence and of the patients with advanced stage GCT who received at least 6 cycles of BEP adjuvant chemotherapy none had tumor recurrence.
The longest reported time to recurrence is 40 years [58]. About 21 % develop recurrence and the median time to relapse was 57.6 months (2–166 months) as reported by Sun et al. [34].
Local pelvic recurrence is reported in 70 % cases, 9 % in pelvis and abdomen, 6 % retroperitoneum, 6 % pelvis and retroperitoneum and 3 % pelvis, abdomen and retroperitoneum (Abu-Rustum et al.) [44]. Most recurrences are intraperitoneal suggesting the possibility of missed peritoneal disease during primary surgery especially for early stage disease. According to a study by Fotopoulou et al. [43] the tumor dissemination patterns differed significantly between primary and recurrent patients, having significantly higher rates of diffuse peritoneal involvement and extraovarian tumor involvement of the middle and upper abdomen in the recurrent cases. Not surprisingly, only about 85 % of the relapsed patients could be operated without residual lesions compared to nearly 100 % in all primary patients. Multivisceral involvement with metastasis to liver, appendix and intestines are quite common. Metastases to lung, bone, vagina, adrenal, spleen, pancreas, gall bladder, rectus muscle are rarely reported.
Similarly nodal recurrence (cervical, axilla and inguinal nodes have been mentioned) is unusual; however Abu-Rustum et al. [44] reported an incidence of 15 % of first recurrence in the retroperitoneum. Brown et al. [42] found that nodal involvement was present in only 6 of 117 patients at the time of recurrence (5 %). Three of these six patients had no nodal involvement at the time of initial staging while the rest had no nodal evaluation. Hence nodal recurrence is unrelated to lymph node status at time of initial diagnosis. As five of the six patients had multiple sites of metastatic disease, nodal involvement may represent secondary spread of recurrent disease in other organs rather than primary spread from the initial disease (Table 4).
A combined modality of treatment, usually involving debulking of the disease followed by radiation or chemotherapy is the norm and may prolong the DFS. A complete debulking of the disease is feasible even in the recurrent setting especially with pelvic and intra-abdominal recurrence [59]. Lordan et al. [60] reported a case of recurrent GCT managed with palliative debulking hepatectomy.
In optimally debulked cases postoperative radiation (pelvic or whole abdominal) is a viable option. Radiotherapy has been used in a case with recurrent GCT in the mediastinum and showed CR 2 years after treatment [61]. In three cases with large recurrent lesions the tumor volume reduced by 85 %–90 % with responses lasting 5–21 months [62]. Radiotherapy can thus be useful for providing symptomatic relief. But with radiotherapy there exists a risk of abdominal recurrence in areas outside the radiotherapy portal, hence chemotherapy (platinum based) is usually given after surgery more so in cases with widespread disease or after suboptimal cytoreduction [45, 63, 64]. Taxols have also been tried in recurrent GCT but platinum based chemo is likely to be the first choice in the recurrent scenario [54].
Hormonal therapies are usually tried in advanced stage or recurrent GCT. Recurrent chemoresistant, progressive non- responding GCT or patients with high surgical risk are ideal candidates for hormone therapy. Estrogen stimulates proliferation of granulosa cells by increasing the cells responsiveness to FSH. In a study of 45 cases of GCT, Foutopoulou [43] reported that there was 43 %, 72 %, and 89 % expression of ER, PR and inhibin respectively while in the recurrent scenario this was 91 %, 91 %, and 65 % respectively. Hormonal manipulation of GCT arise from the surmise that suppression of endogenous estrogen will provide an antiproliferative milieu which could be effective in treating GCT. Several mechanisms have been suggested for how hormone manipulation may inhibit tumor growth in GCT. These can be categorized as indirect action on tumors via suppression of gonadotropins or endogenous steroids and direct effects on the tumor via a local mechanism mediated by specific receptors in the GCT.
Various drugs like medroxyprogestrone acetate, megestrol acetate, tamoxifen, aromatase inhibitors and GnRH agonists have been tried, but with varied success and the results are usually short lived (Table 5).
Progestins act as chemopreventive agents by inducing apoptosis pathway involving transforming growth factor (TGF-α) in ovarian epithelium, a plausible local mechanism for inhibiting tumor growth [75]. Malik et al. and Issacs et al. [65, 66] have documented prolonged remission (14–42 months) in patients having extensive disease treated with high doses of medroxyprogestrone acetate (100–300 mg thrice daily). Similarly Briasoulis et al. [67] reported partial response lasting 20 months after megestrol acetate (160 mg four times a day) was given to an elderly lady with lung metastasis.
ER antagonist tamoxifen was used by Schwartz et al. for disease stabilization [76].
Hardy et al. by alternating biweeky cycles of megestrol acetate (40 mg twice daily) with tamoxifen (10 mg twice daily) in a patient with recurrent ER negative PR positive GCT documented a CR at 22 months and a DFI of 5 years. Continuous progesterone exposure leads to depletion and down regulation of PRs in target tissues while tamoxifen increases PR concentration. Thus, sequential therapy may prolong the antiproliferative effects of progestin by allowing regeneration and stimulation of PRs [68].
Non steroidal aromatase inhibitors (anastrozole and letrozole) and steroidal aromatase inhibitors (exemestane) act by inhibiting the conversion of androstenediol to estriol and testosterone to estradiol. They cause upto 90 % reduction of aromatization of androgens and have few side effects. Freeman et al., Korach et al. and others [69–72] have reported the use of anastrozole (1 mg/day) and letrozole (2.5 mg/day) in recurrent GCT and have documented remissions ranging from 12 to 54 months. There was reduction in size of disease, few cases had complete response and fall in inhibin levels were seen. More ever there was an improvement in the performance status too.
GCTs express receptors for follicle stimulating hormone (FSH), which has been shown to support the growth of GCTs. Thus, hormonal therapies that can decrease gonadotropins may block the stimulatory effects on granulosa cells. Kim et al. [75] have described PR with monthly GnRH agonists (leuprolide acetate 3.75 mg IM) lasting 3–11 months. A few other studies have shown response to GnRH agonists [73, 74, 77] while others showed no response to agonists and GnRH antagonists [78, 79].
The vascular nature of GCT makes it succeptible to inhibition of angiogenesis [9–11]. VEGF expression and microvessel density are associated with poor outcome. Tao et al. evaluated eight patients treated with bevacizumab, a VEGF inhibitor. The overall response rate was 38 % and clinical benefit rate was 63 %. Although only one patient had a complete response the median PFS of 7.2 months was similar to the PFS of 6.8 months after taxanes and 11.2 months after BEP seen in patients with recurrent GCT [9].
Jakob et al. reported significant response in a 87 year patient with recurrent GCT, showing overexpression of mast/stem cell growth factor (KIT; CD117), with TKI imatinib [8]. Thus in selected cases of recurrent GCT, imatinib may be useful in controlling the disease.
Active NFkB molecules formed after proteasomal degradation cause increased cell proliferation and escape from apoptosis. Bortezomib a proteasome inhibitor may be effective to inhibit cell proliferation and viability while stimulating apoptosis [13, 80].
TNF-related apoptosis-inducing ligand (TRAIL; CD253) via its receptors TRAIL-R1/DR4 and TRAIL-R2/DR5 induce cell death in malignant cells with minimal damage to normal tissue. Recombinant human TRAIL (rhTRAIL) and DR4/DR5 specific monoclonal antibodies are under study in various phase II trials [14, 15].
It’s unlikely that any one agent alone may be effective, so a combination of drugs targeting multiple pathways leading to better efficacy, less toxicity and use of lower doses may eventually emerge victorious in the long battle against this indolent tumor.
Conclusion
Due to high chance of recurrence even years after apparent clinical cure of the primary tumor, lifelong follow up with clinical examination and tumor markers like inhibin B is recommended. Other than stage of the disease, the other prognostic factors like age, tumor size, rupture of tumor, mitotic activity are not able to predict recurrences accurately. Thus the identification of prognostic and predictive factors for tumor recurrence is of paramount importance. Although it has been determined that FOXL2 (402C->G) mutation is characteristic of AGCT, the implications of this finding is yet to be elucidated. Further research in the molecular pathogenesis of GCT can shed light on various prognostic factors and therapeutic agents which can be effective in the adjuvant and palliative setting. Due to the rarity of this disease, multicentric RCT’s would be needed to determine the role of newer therapeutic agents in GCT’s. Subsequently drugs like tyrosine kinase inhibitors, bortezomib, bevacizumab may play a greater role in the control of GCT.
References
Ranganath R, Sridevi V, Shirley SS, Shantha V (2008) Clinical and pathologic prognostic factors in adult granulose cell tumors of the ovary. Int J Gynecol Cancer 18:929–933
Vimla N, Kumar L, Kumar S, Vijayaraghavan M, Bhatla N, Roopa H (2005) Granulosa cell tumors of the ovary: factors affecting prognosis. Indian J Med Pediatr Oncol 26:12–20
Mehta H, Trivedi P, Parikh B, Shukla K (2005) Clinicopathological prognostic factors of adult granulosa cell tumors of the ovary—a study of 37 cases. Indian J Pathol Microbiol 48:439–443
Zhang M, Cheung MK, Shin JY, Kapp DS, Husain A, Teng NN, Berek JS, Osann K, Chan JK (2007) Prognostic factors responsible for survival in sex cord stromal tumors of the ovary: an analysis of 376 women. Gynecol Oncol 104:396–400
Lee IH, Choi CH, Hong DG, Song JY, Kim YJ, Kim KT (2011) Clinicopathologic characteristics of granulosa cell tumors of the ovary: a multicenter retrospective study. J Gynecol Oncol 22:188–195
Shah SP, Köbel M, Senz J, Morin RD, Clarke BA, Wiegand KC, Leung G, Zayed A, Mehl E, Kalloger SE, Sun M, Giuliany R, Yorida E, Jones S, Varhol R, Swenerton KD, Miller D, Clement PB, Crane C, Madore J, Provencher D, Leung P, DeFazio A, Khattra J, Turashvili G et al (2009) Mutation of FOXL2 in granulosa-cell tumors of the ovary. N Engl J Med 360:2719–2729
Jamieson S, Fuller PJ (2012) Molecular pathogenesis of granulosa cell tumors of the ovary. Endocr Rev 33:109–144
Jakob A, Geiger R, Hirsch FW (2002) Successful treatment of a patient with a granulosa/theca cell tumor of the ovary with STI571 (Gleevec). Proc Am Soc Clin Oncol 21:24b, Abstract 1904
Tao X, Sood AK, Deavers MT, Schmeler KM, Nick AM, Coleman RL, Milojevic L, Gershenson DM, Brown J (2009) Anti-angiogenesis therapy with bevacizumab for patients with ovarian granulosa cell tumors. Gynecol Oncol 114:431–436
Kesterson JP, Mhawech-Fauceglia P, Lele S (2008) The use of bevacizumab in refractory ovarian granulosa-cell carcinoma with symptomatic relief of ascites: a case report. Gynecol Oncol 111:527–529
Barrena Medel NI, Herzog TJ, Wright JD, Lewin SN (2010) Neoadjuvant bevacizumab in a granulosa cell tumor of the ovary: a case report. Anticancer Res 30:4767–4768
Farinola MA, Gown AM, Judson K, Ronnett BM, Barry TS, Movahedi-Lankarani S, Vang R (2007) Estrogen receptor and progesterone receptor expression in ovarian adult granulosa cell tumors and Sertoli-Leydig cell tumors. Int J Gynecol Pathol 26:375–382
Chu S, Alexiadis M, Fuller PJ (2009) Proteasome inhibition by bortezomib decreases proliferation and increases apoptosis in ovarian granulosa cell tumors. Reprod Sci 16:397–407
Kruyt FA (2008) TRAIL and cancer therapy. Cancer Lett 263:14–25
Woods DC, Liu HK, Nishi Y, Yanase T, Johnson AL (2008) Inhibition of proteasome activity sensitizes human granulose tumor cells to TRAIL-induced cell death. Cancer Lett 260:20–27
Lappöhn RE, Burger HG, Bouma J, Bangah M, Krans M, de Bruijn HW (1989) Inhibin as a marker for granulosa-cell tumors. N Engl J Med 321:790–793
Petraglia F, Luisi S, Pautier P, Sabourin JC, Rey R, Lhomme C, Bidart JM (1998) Inhibin B is the major form of inhibin/activin family secreted by granulosa cell tumors. J Clin Endocrinol Metab 83:1029–1032
Mom CH, Engelen MJ, Willemse PH, Gietema JA, ten Hoor KA, de Vries EG, van der Zee AG (2007) Granulosa cell tumors of the ovary: the clinical value of serum inhibin A and B levels in a large single center cohort. Gynecol Oncol 105:365–372
Healy DL, Burger HG, Mamers P, Jobling T, Bangah M, Quinn M, Grant P, Day AJ, Rome R, Campbell JJ (1993) Elevated serum inhibin concentrations in postmenopausal women with ovarian tumors. N Engl J Med 329:1539–1542
Ala-Fossi SL, Aine R, Punnonen R, Mäenpää J (2000) Is potential to produce inhibins related to prognosis in ovarian granulosa cell tumors? Eur J Gynaecol Oncol 21:187–189
Koukourakis GV, Kouloulias VE, Koukourakis MJ, Zacharias GA, Papadimitriou C, Mystakidou K et al (2008) Granulosa cell tumor of the ovary: tumor review. Integr Cancer Ther 7:204–215
Long WQ, Ranchin V, Pautier P, Belville C, Denizot P, Cailla H, Lhommé C, Picard JY, Bidart JM, Rey R (2000) Detection of minimal levels of serum anti-Mullerian hormone during follow-up of patients with ovarian granulose cell tumor by means of a highly sensitive enzyme-linked immunosorbent assay. J Clin Endocrinol Metab 85:540–544
Chang HL, Pahlavan N, Halpern EF, MacLaughlin DT (2009) Serum Mullerian inhibiting substance/anti-Mullerian hormone levels in patients with adult granulosa cell tumors directly correlate with aggregate tumor mass as determined by pathology or radiology. Gynecol Oncol 114:57–60
Anttonen M, Unkila-Kallio L, Leminen A, Butzow R, Heikinheimo M (2005) High GATA-4 expression associates with aggressive behavior, whereas low anti-Mullerian hormone expression associates with growth potential of ovarian granulosa cell tumors. J Clin Endocrinol Metab 90:6529–6535
Geerts I, Vergote I, Neven P, Billen J (2009) The role of inhibins B and antimullerian hormone for diagnosis and follow-up of granulosa cell tumors. Int J Gynecol Cancer 19:847–855
Schumer ST, Cannistra SA (2003) Granulosa cell tumor of the ovary. J Clin Oncol 21:1180–1189
Zhao C, Vinh TN, McManus K, Dabbs D, Barner R, Vang R (2009) Identification of the most sensitive and robust immunohistochemical markers in different categories of ovarian sex cord-stromal tumors. Am J Surg Pathol 33:354–356
Hauspy J, Beiner ME, Harley I, Rosen B, Murphy J, Chapman W, Le LW, Fyles A, Levin W (2011) Role of adjuvant radiotherapy in granulosa cell tumors of the ovary. Int J Radiat Oncol Biol Phys 79:770–774
Van der Vorst MJ, Bleeker MC, Boven E (2010) Unusual presentation of Granulosa cell tumour of the ovary. J Clin Oncol 28:e554–e556
Ko SF, Wan YL, Ng SH, Lee TY, Lin JW, Chen WJ, Kung FT, Tsai CC (1999) Adult ovarian granulosa cell tumors: spectrum of sonographic and CT findings with pathologic correlation. AJR Am J Roentgenol 72:1227–1233
Kim SH, Kim SH (2002) Granulosa cell tumor of the ovary: common findings and unusual appearances on CT and MR. J Comput Assist Tomogr 26:756–761
Chan JK, Zhang M, Kaleb V, Loizzi V, Benjamin J, Vasilev S, Osann K, DiSaia PJ (2005) Prognostic factors responsible for survival in sex cord stromal tumors of the ovary—a multivariate analysis. Gynecol Oncol 96:204–209
Ayhan A, Salman MC, Velipasaoglu M, Sakinci M, Yuce K (2009) Prognostic factors in adult granulosa cell tumors of the ovary: a retrospective analysis of 80 cases. J Gynecol Oncol 20:158–163
Sun HD, Lin H, Jao MS, Wang KL, Liou WS, Hung YC, Chiang YC, Lu CH, Lai HC, Yu MH (2012) A long-term follow-up study of 176 cases with adult-type ovarian granulosa cell tumors. Gynecol Oncol 24:244–249
Auranen A, Sundström J, Ijäs J, Grénman S (2007) Prognostic factors of ovarian granulosa cell tumor: a study of 35 patients and review of the literature. Int J Gynecol Cancer 17:1011–1018
Pectasides D, Papaxoinis G, Fountzilas G, Aravantinos G, Pectasides E, Mouratidou D et al (2008) Adult granulosa cell tumors of the ovary: a clinicopathological study of 34 patients by the Hellenic Cooperative Oncology Group (HeCOG). Anticancer Res 28:1421–1428
Sehouli J, Drescher FS, Mustea A, Elling D, Friedmann W, Kühn W, Nehmzow M, Opri F, Klare P, Dietel M, Lichtenegger W (2004) Granulosa cell tumor of the ovary: 10 years follow-up data of 65 patients. Anticancer Res 24:1223–1229
Uygun K, Aydiner A, Saip P, Basaran M, Tas F, Kocak Z, Dincer M, Topuz E (2003) Granulosa cell tumor of the ovary retrospective analysis of 45 Cases. Am J Clin Oncol 26:517–521
Park JY, Jin KL, Kim DY, Kim JH, Kim YM, Kim KR, Kim YT, Nam JH (2012) Surgical staging and adjuvant chemotherapy in the management of patients with adult granulosa cell tumors of the ovary. Gynecol Oncol 125:80–86
Kyrönlahti A, Rämö M, Tamminen M, Unkila-Kallio L, Butzow R, Leminen A, Nemer M, Rahman N, Huhtaniemi I, Heikinheimo M, Anttonen M (2008) GATA-4 regulates Bcl-2 expression in ovarian granulosa cell tumors. Endocrinology 149:5635–5642
Thrall MM, Paley P, Pizer E, Garcia R, Goff BA (2011) Patterns of spread and recurrence of sex cord—stromal tumors of the ovary. Gynecol Oncol 122:242–245
Brown J, Sood AK, Deavers MT, Milojevic L, Gershenson DM (2009) Gynecol Oncol 113:86–90
Fotopolou C, Savvatis K, Braicu EI, Brink-Spalink V, Darb-Esfahani S (2010) Adult granulosa cell tumors of the ovary: tumor dissemination patern at primary and recurrent situation, surgical outcome. Gynecol Oncol 119:285–290
Abu-Rustum NR, Restivo A, Ivy J, Soslow R, Sabbatini P, Sonoda Y, Barakat RR, Chi DS (2006) Retroperitoneal nodal metastasis in primary and recurrent granulosa cell tumors of the ovary. Gynecol Oncol 103:31–34
Gershenson DM, Copeland LJ, Kavanagh JJ, Stringer CA, Saul PB, Wharton JT (1987) Treatment of metastatic stromal tumors of the ovary with cisplatin, doxorubicin, and cyclophosphamide. Obstet Gynecol 70:765–769
Pectasides D, Alevizakos N, Athanassiou AE (1992) Cisplatin-containing regimen in advanced or recurrent granulosa cell tumours of the ovary. Ann Oncol 3:316–318
Uygun K, Aydiner A, Saip P, Kocak Z, Basaran M, Dincer M, Topuz E (2003) Clinical parameters and treatment results in recurrent granulosa cell tumor of the ovary. Gynecol Oncol 88:400–403
Colombo N, Sessa C, Landoni F, Sartori E, Pecorelli S, Mangioni C (1986) Cisplatin, vinblastine, and bleomycin combination chemotherapy in metastatic granulosa cell tumor of the ovary. Obstet Gynecol 67:265–268
Zambetti M, Escobedo A, Pilotti S, De Palo G (1990) cisplatinum/vinblastine/bleomycin combination chemotherapy in advanced or recurrent granulosa cell tumors of the ovary. Gynecol Oncol 36:317–320
Pecorelli S, Wagenaar HC, Vergote IB, Curran D, Beex LVA, Witshaw E et al (1999) Cisplatin (P), vinblastine (V) and bleomycin (B) combination chemotherapy in recurrent or advanced granulosa (-theca) cell tumours of the ovary. An EORTC Gynaecological Cancer Cooperative Group Study. Eur J Cancer 35:1331–1337
Gershenson DM, Morris M, Burke TW, Levenback C, Matthews CM, Wharton JT (1996) Treatment of poor prognosis sex cord-stromal tumors of the ovary with the combination of bleomycin, etoposide, and cisplatin. Obstet Gynecol 87:527–531
Homesley HD, Bundy BN, Hurteau JA, Roth LM (1999) Bleomycin, etoposide, and cisplatin combination therapy of ovarian granulosa cell tumors and other stromal malignancies: a Gynecologic Oncology Group study. Gynecol Oncol 72:131–137
Pautier P, Gutierrez-Bonnaire M, Rey A, Sillet-Bach I, Chevreau C, Kerbrat P, Morice P, Duvillard P, Lhommé C (2008) Combination of bleomycin, etoposide, and cisplatin for the treatment of advanced ovarian granulosa cell tumors. Int J Gynecol Cancer 18:446–452
Brown J, Shvartsman HS, Deavers MT et al (2003) The activity of taxanes compared with bleomycin, etoposide and cisplatin in the treatment of sex cord-stromal ovarian tumors. Gynecol Oncol 97:489–496
Pankratz E, Boyes DA, White GW, Galliford BW, Fairey RN, Benedet JL (1978) Granulosa cell tumors. A clinical review of 61 cases. Obstet Gynecol 52:718–723
Savage P, Constenla D, Fisher C, Shepherd JH, Barton DP, Blake P, Gore ME (1998) Granulosa cell tumours of the ovary: demographics, survival and the management of advanced disease. Clin Oncol (R Coll Radiol) 10:242–245
Wolf JK, Mullen J, Eifel PJ et al (1999) Radiation treatment of advanced or recurrent granulosa cell tumor of the ovary. Gynecol Oncol 73:35–41
East N, Alobaid A, Goffin F, Ouallouche K, Gauthier P (2005) Granulosa cell tumour: a recurrence 40 years after initial diagnosis. J Obstet Gynaecol Cancer 27:363–364
Crew KD, Cohen MH, Smith DH, Tiersten AD, Feirt NM, Hershman DL (2005) Long natural history of recurrent granulosa cell tumor of the ovary 23 years after initial diagnosis: a case report and review of the literature. Gynecol Oncol 96:235–240
Lordan JT, Jones RL, Karanjia ND, Butler-Manuel S (2007) Debulking hepatectomy for an unusual case of a grade 1 stage 1 granulosa cell tumour of the ovary with late metastases. Oncology 72:143–144
Lee IW, Levin W, Chapman W, Goldberg RE, Murphy KJ, Milosevic M (1999) Radiotherapy for the treatment of metastatic granulosa cell tumor in the mediastinum: a case report. Gynecol Oncol 73:455–460
Choan E, Samant R, Fung M, Fung K, Le T, Hopkins L, Senterman M (2006) Palliative radiotherapy for recurrent granulosa cell tumor of the ovary: a report of 3 cases with radiological evidence of response. Gynecol Oncol 102:406–410
Lee YK, Park NH, Kim JW, Song YS, Kang SB, Lee HP (2008) Characteristics of recurrence in adult-type granulose cell tumor. Int J Gynecol Cancer 18:642–647
Tresukosol D, Kudelka AP, Edwards CL, Charnsangavej C, Narboni N, Kavanagh JJ (1995) Recurrent ovarian granulosa cell tumor: a case report of a dramatic response to Taxol. Int J Gynecol Oncol 5:156–159
Malik ST, Slevin ML (1991) Medroxyprogesterone acetate (MPA) in advanced granulosa cell tumours of the ovary: a new therapeutic approach? Br J Cancer 63:410–411
Isaacs R, Forgeson G, Allan S (1992) Progestagens for granulosa cell tumours of the ovary. Br J Cancer 65:140
Briasoulis E, Karavasilis V, Pavlidis N (1997) Megestrol activity in recurrent adult type granulosa cell tumour of the ovary. Ann Oncol 8:811–812
Hardy RD, Bell JG, Nicely CJ, Reid GC (2005) Hormonal treatment of a recurrent granulosa cell tumor of the ovary: case report and review of the literature. Gynecol Oncol 96:865–869
Freeman SA, Modesitt SC (2006) Anastrozole therapy in recurrent ovarian adult granulosa cell tumors: a report of 2 cases. Gynecol Oncol 103:755–758
Abdul Munem A, Al-Bahrani B, Mehdi I, Kamona A, Nadas AM (2012) Aromatase inhibitors—a viable option for recurrent granulose cell tumour of ovary: overview and case report. J Pak Med Assoc 62:505–507
Korach J, Perri T, Beiner M, Davidzon T, Fridman E, Ben-Baruch G (2009) Promising effect of aromatase inhibitors on recurrent granulosa cell tumors. Int J Gynecol Cancer 19:830–833
AlHilli MM, Long HJ, Podratz KC, Bakkum-Gamez JN (2012) Aromatase inhibitors in the treatment of recurrent ovarian granulosa cell tumors: brief report and review of the literature. J Obstet Gynaecol Res 38:340–344
Martikainen H, Penttinen J, Huhtaniemi I, Kauppila A (1989) Gonadotropin-releasing hormone agonist analog therapy effective in ovarian granulosa cell malignancy. Gynecol Oncol 35:406–408
Fishman A, Kudelka AP, Tresukosol D, Edwards CL, Freedman RS, Kaplan AL, Girtanner RE, Kavanagh JJ (1996) Leuprolide acetate for treating refractory or persistent ovarian granulosa cell tumor. J Reprod Med 41:393–396
Kim HJ, Lee S-C, Bae SB, Kwon KW, Kim CK, Lee NS et al (2009) GnRH agonist therapy in a patient with recurrent ovarian granulosa cell tumors. J Korean Med Sci 24:535–538
Schwartz PE, MacLusky N, Sakamoto H, Eisenfeld A (1983) Steroid receptor proteins in nonepithelial malignancies of the ovary. Gynecol Oncol 15:305–315
Kauppila A, Bangah M, Burger H, Martikainen H (1992) GnRHagonist analog therapy in advanced/recurrent granulose cell tumors: further evidence of a role of inhibin in monitoring response to treatment. Gynecol Endocrinol 6:271–274
Maxwell GL, Soisson AP, Miles P (1994) Failure of gonadotropin releasing hormone therapy in patients with metastatic ovarian sex cord stromal tumors. Oncology 51:356–359
Ameryckx L, Fatemi HM, De Sutter P, Amy JJ (2005) GnRH antagonist in the adjuvant treatment of a recurrent ovarian granulosa cell tumor: a case report. Gynecol Oncol 99:764–766
Adams J (2004) The proteasome: a suitable antineoplastic target. Nat Rev Cancer 4:349–360
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kottarathil, V.D., Antony, M.A., Nair, I.R. et al. Recent Advances in Granulosa Cell Tumor Ovary: A Review. Indian J Surg Oncol 4, 37–47 (2013). https://doi.org/10.1007/s13193-012-0201-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-012-0201-z