Abstract
Purpose
Bone fractures are the most common large organ injuries to humans, and critical situations can delay the consolidation process or even in nonunion fractures. In this context, many technologies for improving bone regeneration have been emerging, and including the use of biomaterials for bone tissue healing, once biomaterials are known by their osteogenic stimulus and capacity to produce tissue ingrowth associated with their biocompatibility and non-cytotoxicity.
Methods
This review of the literature investigated the effects of different biomaterials on the process of bone healing in animal experiments manufactured using the electrospinning technique.
Results
It is possible to highlight that a crucial aspect is combining different materials tailored to a specific and effective use. Additionally, the electrospinning method can be considered a great ally to overcome the challenges offered by manufacturing functional and compatible biomaterials for scaffolds production to be applied in the tissue healing process.
Conclusion
Scaffolds manufactured by electrospinning technique using biomaterials with different origins have a great potential to be used as bone grafts for bone healing stimulation since most material scaffolds are noncytotoxic, biocompatible, and have osteogenic properties.
Lay Summary
Many methods for improving bone regeneration have been studied by scientists worldwide, including the use of biomaterials for bone tissue healing, once biomaterials are known by their capacity to produce tissue ingrowth associated with their compatibility with our biological systems and low toxicity. The literature review investigated the effects of different materials manufactured by the electrospinning technique on bone healing in animal experiments. It is possible to highlight that scaffolds manufactured by electrospinning technique using biomaterials with different origins have a great potential to be used as bone grafts for bone healing stimulation.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bone fractures, either due to pathologies or traumas, are the most common large organ injuries to humans [1]. It is estimated that around 9 million fractures occur annually worldwide, representing a significant health problem in orthopedic clinics so far [1, 2]. Fortunately, bone is a dynamic and highly vascularized tissue, and most cases of fractures heal without any therapeutical intervention [3, 4]. However, in critical situations such as sizeable traumatic bone defects, insufficient blood supply, or even infections, the biological capacity of repair may be impaired, resulting in a delay of the consolidation process or even in nonunion fractures [2]. In this context, many technologies for improving and promoting bone regeneration have been emerging, including cell-based therapies [4], phototherapy (such as laser therapy) [5, 6], and biomaterial-based bone grafts [7].
Biomaterials are known by their osteogenic stimulus and capacity to produce tissue ingrowth in fractures and bone defects, associated with their biocompatibility and non-cytotoxicity [7]. Biomaterials are divided into many different categories, and one of the most common is bioceramics, which include hydroxyapatite, calcium phosphate, and bioactive glasses (BGs) [7, 8]. Bioceramics present high bioactivity index and their unique capacity to bond to bone tissue, forming a biologically active bone-like apatite layer and stimulating new bone deposition [7]. In addition, another class of biomaterials widely used for bone tissue engineering is polymers [9]. Biodegradable natural-based polymers (collagen, silk, alginate, chitosan, hyaluronic acid) and synthetic polymers (poly(lactic acid): PLA, poly(glycolic acid): PGA, poly(lactic-co-glycolide): PLGA, poly(ε-caprolactone): PCL, polyhydroxyalkanoates: PHA) have been widely applied for biomedical applications [10, 11].
The biomaterials on the process of bone regeneration have great importance, as well as the performance of bioceramics and polymers, the material presentation [7], since bone tissue is a natural nanocomposite consisted of collagen, proteoglycans, and hydroxyapatite (HA) crystals, all at the nanometer scale. In this context, it is highly desirable that biomaterials used to improve bone tissue regeneration also present nanoscale characteristics, resembling tissue aspects, which may enhance regeneration [12]. On the other hand, considering nanomaterials, more efficient biological behavior can be attributed to their closer surface-area-to-volume ratio, surface wettability, and mechanical properties, which are correlated with higher adsorption of proteins, and consequently favoring cell or tissue responses [13].
Two of the most used biomaterial-based bone grafts are the scaffold and membrane. The scaffold, known as a temporary foundation for cellular survival, must comprise not only strength and good cell-attachment properties to provide cell proliferation and functions but also porous structures to benefit the diffusion of oxygen, nutrients, and wastes [14]. The membrane is also used as a support for tissue regeneration and must have essential characteristics for its proper functioning, such as providing gas exchange, sustaining a humid environment avoiding maceration, and promoting drainage and absorption of exudates [15]. Besides, due to its larger surface area, it allows the addition of specific substances, such as antibiotics and active components [16, 17]. Considering the revised literature, it is possible to affirm that these forms can be applied alone or together according to each case and objective.
Despite the positive effects of biomaterials on bone healing, there is still a limited understanding of their biological interaction and the process of bone tissue stimulation. In this context, the purpose of this study was to review the literature investigating the effects of different materials on bone healing in animal experiments.
Preliminary Approach
A thorough literature search was conducted to detect studies that demonstrated the innovation and challenges of applying materials to produce scaffolds, mainly to improve bone tissue healing. A density visualization map was created from the most frequently used keywords. Figure 1 shows the more cited words and their interactions among the explored articles, wherein darker colors mean higher frequencies.
The different generated colors illustrate the clustering, showing a clear separation of the distinct frequency, as well as the relationship among the most frequently cited words. In the publication map, four central regions can be observed. The clusters comprise the words tissue regeneration, nanomaterial, recent advance, biomedical application, and hydrogel, showing consistent interest as a trend in innovative ways to explore nanotechnology to increment tissue regeneration. The second cluster comprised the terms bone, polymer, effect, bone regeneration, and property and the terms role, regeneration, nanotechnology, nanostructure, wound healing, and fabrication in other regions. Moreover, the last cluster comprised the words titanium, nano, and challenge.
The inclusion criteria of the defined articles were as follows: (1) articles published in English from 2000 to 2021 and (2) original articles and reviews on the selected themes. Independent studies published in scientific events, blogs, and other media, as well as in not indexed published material, were not considered as part of this review. From this, a database was created, recognizing the advances made in the field and what is still pending to improve our knowledge regarding scaffolds production and tissue healing using materials. The main articles consulted and used in the elaboration of the present work are shown in Table 1.
The search was conducted on Scopus databases to identify the literature regarding electrospinning, scaffolds, and nanomaterials. In this search, 1696 articles were found, and after a careful evaluation, 101 articles were used to elaborate the present work. Thus, the data obtained from the frequency of mention (Fig. 1) was used to guide the discussions and the construction of the following topics, highlighting the challenges and perspectives in each area.
Sources of Biomaterials
Numerous material types, manufactured from different sources (both natural and synthetic), with bioactivity and osteogenic properties, have been used to produce biomaterials and scaffolds [53]. For example, one of the most promising classes for material manufacturing is biopolymers, which can be obtained from natural (living organisms) or synthetic sources [53]. They are used for a broad range of biomedical applications due to their intrinsic biological characteristics like biocompatibility, biodegradation to nontoxic products, low antigenicity, and high bioactivity [53]. Among those, it can be highlighted the use of collagen/gelatin from bovine and porcine origins [29], chitosan from marine species (including shrimps) [48], cellulose from purified cotton [38], and poly(3-hydroxybutyrate-co-3-hydroxybutyrate) (PHBV) prepared by microbial fermentation [54]. Furthermore, synthetic biopolymers have also gained great prominence for medical applications due to a wide range of physical and chemical properties that can be achieved based on the monomer units, polymerization reaction, and formation of copolymers consisting of different components at adjustable concentrations [39]. In this regard, polyurethane [23] and polycaprolactone [24] can be highlighted.
Moreover, the metals class can also be mentioned as a tool to manufacture biomaterials. They are attractive for this purpose due to their unique mechanical strength, resistance to corrosion, oxidation, and non-reactiveness [55]. Notably, the metal gold (Au) has arisen as an option for many biotechnology applications such as drug delivery [19]. In addition, silver (Ag) has also been used as a biomaterial primarily due to its antibacterial effects. Marsich et al. [64] developed an antibacterial scaffold by introducing silver nanoparticles to alginate and hydroxyapatite for tissue engineering applications. In addition, in the study conducted by Eid et al. [40], the researchers explored the applications of platinum (Pt) nanoparticle-loaded calcium phosphate scaffolds that demonstrated anti-inflammatory properties, enhanced cell proliferation, and attached powerful tools for bone regeneration.
In addition, the class of bioceramics is also used for material manufacturing [25]. Bioceramics are biocompatible with bioactive materials, and they also can interact with a bone when implanted into the tissue [65]. Silica, titanium dioxide (TiO2), zirconia (ZrO2), calcium phosphates (CaP), and bioactive glass [28] are examples of these materials.
As an example of the formulation and study of bioceramics as a promising biomaterial, Thakare et al. [41] demonstrated the inclusion of ZrO2 in the electrospun polycaprolactone nanofiber scaffolds exhibited an enhanced fibroblast proliferation and improved bioactivity of the scaffolds.
At the same time, osteoconductive properties at the scale, CaP materials such as synthetic hydroxyapatite, and β-tricalcium phosphate (β-TCP, Ca3(PO4)2) are well-known for their potential in bone tissue engineering [22] due to their similarity of the chemical structure of HA and TCP with the inorganic phase of bone [26]. Similarly, bioactive glasses, composed essentially of calcium, sodium, phosphate, and silicate, have been widely studied and used as potential bioactive materials for bone substitution and repair [49, 56].
Another option is to combine different materials with different biological and mechanical characteristics to manufacture composite materials. In this context, two or more different raw materials are frequently used, such as poly (L-lactic acid)/gelatin [30], polycaprolactone/type-1 collagen [66], poly (aspartic acid)/Zein [42], and oyster shell (OS) with poly (L-lactide) [43]. Mehrasa et al. [31] manufactured poly lactic-co-glycolic acid (PLGA) and PLGA/gelatin fibrous scaffolds embedded with mesoporous silica particles and found significant superior biological properties of the fibrous scaffolds in the stem cell proliferation.
Table 2 illustrates the variety of materials used for fabricating biomaterials that can be used for tissue engineering applications and the simulation of bone healing.
Methods to Produce Scaffolds: Electrospinning as a Well-established Protocol
Several techniques can be applied to produce scaffolds using biomaterials. In the last years, the electrospun process has been gaining attention to produce nanostructures in different industrial fields.
The electrospun method is a versatile technique that is highly recommended to produce nanostructures because of their close working system that permits simpler, faster, secure, and efficient work conditions. Above all, dismissing specific solutions and dangerous solvents, even extreme temperatures, so it is used under ambient temperature [32, 50]. During the last decade, the use of electrospun nanostructures, mainly to produce fibers (NFs), for bone tissue engineering scaffolds has enhanced, especially since their morphology is similar to the structure of the natural extracellular matrix, presenting high porosity and their large surface area that can promote cell adhesion, proliferation, increases solubility, and also allows more precise targeting of molecules in the body [54, 67, 99].
This technique utilizes the electrostatic property to charge a viscous polymer solution. A positive high-voltage source is applied at the tip of a syringe needle, and there is a potential gradient in the collector, so a strong electric field is generated between both. When a critical voltage is applied, mutual charge repulsion overcomes the surface tension of the polymer solution, and an electrically charged jet is ejected from the tip of a conical shape, known as the Taylor cone. In this process, the solvent is evaporated, resulting in the formation of solid nanofibers (electrospinning method) or nanoparticles (electrospraying method) deposited on the collector electrode as a nonwoven mat (Fig. 2) [20, 58, 68, 69].
Depending on the choice of materials and controllable parameters processes, such as voltage, feeding rate, and tip-to-collector distance, electrospun scaffolds could be molded according to the objective desired. The parameters range utilized by several authors analyzed ranged widely and, therefore, resulted in different results, for example, the tip-to-collector distance varied among 7.5 to 20 cm considering the studies conducted by Biazar et al. [68], Mathew et al. [24], and Wang et al. [25]. Similarly, considering the voltage applied for the electrospun processes, the authors Mathew et al. [24] and Schofer et al. [46] ranged this parameter from 9 to 30 kV. Besides, the feeding rate of the polymeric solution ejected from the syringe was varied from 14 µL/min to 5 mL/h by Schofer et al. [46] and Wang et al. [25]. It is essential to emphasize that although these process variables are of utmost importance, several studies omit this information. Likewise, the solutions containing one or more materials in a mixture are the most variable and must be adapted according to each objective, and the matrix is chosen. Additionally, different collectors are also available and infer significant changes in the final product. The process versatility and the practical apparatus allow the obtention of diversification in the manufactured structures, and as a result, it is possible to develop particles, fibers, and membranes.
The literature consulted showed a wide gamma of options to produce scaffolds. However, some studies obtained biomaterials and have been tested by in vitro conditions. Hence, it is worth mentioning that it is also applicable to use heat treatment after the electrospinning process [18, 47, 59] or to employ coaxial electrospinning method, which comprehends in two syringes with concentric needles that ejected the polymer and a bioactive substance simultaneously, avoiding adverse interactions [37, 57, 99]. Regarding all these works, it is possible to affirm that will always exist the best way to produce what is desired; clearly, much more is to come. However, it is essential to recognize that many opportunities could be created with an efficient method.
The choice of biomaterial combined with the method for scaffolds manufacturing is of utmost importance. The possibilities that rely on the design task of specific material applied on the electrospinning method can be considered a great ally to overcome the challenges offered by the obtention of functional and compatible biomaterials for scaffolds production to be used in the tissue healing process.
Biomaterials Manufactured Using the Electrospinning Technique for Bone Healing: In Vivo Studies
As widely known, in vivo studies are an important step for evaluating the safety and biological performance of new biomaterials, and many studies have been performed to assess the effects of materials on bone tissue regeneration [75]. Considering this fact, the literature shows several ways to evaluate the in vivo response to the application of the electrospinning scaffolds for bone tissue healing purposes, and some of them are presented as discussed in the following.
Hou et al. [33] designed a bioactive nanoparticle-gelatin composite scaffold and implanted it into bone defects in rats. The authors evaluated the tissue response after 4, 8, and 12 weeks of surgery. They observed new bone tissue in the medullary cavity in the bone defect area, evidencing that the composite scaffold displayed excellent biodegradability, bioactivity, and cytocompatibility. Moreover, the mechanical properties of the newly designed bioactive particle-gelatin composite scaffold and the 3-D structure of new bone tissue are comparable to the surrounding cancellous bones. The authors stated that the material constitutes a promising artificial bone graft. A schematic process describing electrospun fibers and 3D scaffolds is presented in Fig. 3.
Abazari et al. [27] explored the effects of an electrospun fibrous (789 ± 564 nm) polyvinyl alcohol, chitosan, and hydroxyapatite (PVA-chitosan-HA) composite enriched with platelet-rich plasma (PRP) as a bioactive substance and seeded with mesenchymal stem cells (MSCs) in the healing process of a critical-sized calvarial defect. The authors found that the proposed treatment was able to accelerate bone repair. In the same line of work, Biazar and Heidari Keshel [68] evaluated the effects of the implantation of fibrous poly(3-hydroxybutyrate-co-3-hydroxyvalerate) (PHBV) and nanohydroxyapatite (nano-HAp) composite scaffolds, seeded with stem cells (USSCs), in the process of healing using an experimental model of calvarial bone defect in rats. The authors found that both the pure PHBV and PHBV with nanoHA scaffolds showed a randomly interconnected and highly porous structure, with diameter size ranging from 100 to 324 nm (by the pure PHBV to the most concentrated scaffold), and, after 28 days after implantation, a significantly more significant amount of regenerated tissue in the treated animals, highlighting the positive osteogenic effect of scaffolds.
Zhong et al. [54] evaluated the potential of electrospun nanofibers of PHBV but with different adenosine concentrations for bone healing in a critical-size calvarial defect model in rabbits. The authors observed that the biomaterial could guide bone tissue ingrowth through the defect, promoting the complete filling after 12 weeks postimplantation. The variation of adenosine concentration did not exhibit differences in function and efficacy biocompatibility of the NFs.
Frohbergh et al. [86] studied the osseointegration capability of a nanofibrous chitosan-hydroxyapatite-genipin (CTS-HA-GP) scaffold manufactured with the electrospinning technique in a murine model of critical-size calvarial defects by histology and micro-CT. After 3 months, CTS-HA-GP scaffolds with 334.7 ± 119.1 nm diameter size could induce a 38% increase for the new bone tissue area. Similarly, Nguyen et al. [87] created porous and nonporous PCL fiber-based fibrous scaffolds manufactured with the electrospinning technique and induced calcium phosphate (CaP) particles to coat on the fibers after immersion in simulated body fluid solution (SBF) during 2, 4, 8, and 12 h, and could observe, after 1 and 3 months of the implantation into the femoral plug defects of rabbits, a new bone formation in the case of porous PCL 12 h scaffold.
The incorporation of the antibiotic azithromycin in the calcium phosphate (CaP)-coated mPCL membrane was studied by Mathew et al. [24], ranging the antibiotic doses from 1 to 2.5 until 5 mg. Lower doses of entrapped azithromycin were limited to the upper surface of the membranes, and the higher dose (5 mg) caused a deep penetration; furthermore, between 1 and 8 weeks, the authors observed a better response of the sample with 5 mg to form new bone regeneration contralaterally in rodent calvarial defects, than to membrane without azithromycin.
Ma et al. [88] explored the effect of berberine (BBR), an active component extracted from herbs that have potential bone protection, with PCL and collagen. Their results showed this protection in critically sized cranial defects once the condition with BBR obtained higher bone mineral density. The BBR also provides clinical potential which was utilized to produce a 3D scaffold with a bilayer membrane. Zhang et al. [89] used mineralized collagen and chitosan to deliver the BBR into PCL/PVP nanofibers for this production and observed a positive result in the process of bone healing after the material application.
Considering bone healing and cell proliferation, a positive result was obtained by Hashemi et al. [90], who produced a scaffold containing PCL, PLA, and gelatin and added ascorbic acid in different concentrations (0.5, 1, 5, and 10%). The rats were kept with these scaffolds during 4 months in the calvarial defects, and then, the group with 5% showed higher new bone than others. Samadian et al. [91] added taurine into the same scaffold base mentioned above, following this research line. After 12 weeks, the condition with 10% of taurine showed the best bone regeneration.
A novel carrier to BMP-6 was tested by Toprak et al. [92]. ZIF-8, among zeolitic imidazole frameworks (ZIFs), a subclass of metal–organic frameworks (MOFs), possess high permanent porosity with intrinsic biodegradability. The authors fabricated PCL/ZIF-8 scaffolds for 8 weeks using the electrospinning technique, with and without BMP-6, and implanted them into rat cranial bone defects. They found that the degree of bone repair was expressively higher when the BMP-6 was applied than control and PCL/ZIF-8 scaffold groups. This positive result was also obtained by Xue et al. [76], who utilized the same material combination above with collagen into the scaffold fabrication.
Junka and Yu [76] utilized the PCL with osteoblast and endothelial decellularized extracellular matrix to test the osteoconductive activity in the rat femur. In all conditions evaluated, the authors found an improvement in the insertion and proliferation of osteoblast. Padalhin et al. [93] also obtained outstanding results when applying a similar scaffold to a rat’s skull defect. Additionally, Huang et al. [94] observed the same region almost totally regenerated when preparing a scaffold with super-active platelet lysate into gelatin/PCL/PLLA nanofibers.
Schofer et al. [46] explored the influence of electrospun PLLA fiber scaffolds and their use in combination with bone morphogenetic protein-2 (BMP-2) for the reconstruction of critical-size bone defect by cranial computed tomography (CCT), histology, histomorphometry, and immunohistochemistry. The PLLA/BMP-2 presence demonstrated a capability to increase bone formation and expression of osteocalcin after 12 weeks. Su et al. [48] investigated the effects of electrospinning membranes manufactured with nano chitosan for GBR in critical-sized calvarial defects. After 12 weeks, treated animals presented a significantly increased bone formation at the defect region and increased material resorption.
Hydroxyapatite was also used by Rainer et al. [21] to produce a functionalized PLLA scaffold. The results showed the dispersion of HA nanoparticles on the surface of PLLA fibers and an intrinsic porosity with an average pore size of approximately 100 nm, which contributes to their application, resulting in the complete repair of the sternum of rabbits in 21 days in comparison with control scaffolds. The same mixture was utilized by Koç et al. [95] using the same mix to produce a 3D nanofibrous to verify the presence of graft materials in the calvarial bone regeneration process for 20 weeks. The authors observed better results when these scaffolds were applied than control groups; however, autograft condition, considered the gold standard, was the best for bone regeneration in this case.
The electrospinning process may complement other procedures to include biocompounds to reinforce structures and improve the final product, as we can infer from several articles, for example, as presented by Anitha et al. [44]. The authors produced electrospun yarns using PLLA to develop the scaffolds with diameters ranging between 200 and 600 nm. To develop the scaffold, the authors incorporated the yarns into a gelatinous matrix containing silica-coated nanoHA at different weight ratios (5, 10, 15 wt%) and lengths (short and continuous), resulting in structures with porous geometry. The authors found that all conditions improved the femur defect regeneration at 2 or 4 months after the surgery in rats.
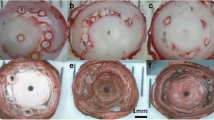
Ren et al. [45] utilized different collectors to produce PLLA/gelatin composite nanofibers. The results showed the production of random nanofibrous meshes using a steel plate as the collector and nestlike nanofibrous meshes using a copper wire grid. After 4 and 12 weeks from the surgery in the calvarium defects in rats, the authors observed an evident bone regeneration when both conditions of scaffolds were implanted than the control one. Furthermore, the nestlike nanofibrous showed a higher level of bone regeneration than the random NFs. Andalib et al. [96] used the combination PLLA/gelatin and added HA with and without MSCs to introduce this scaffold made with the electrospinning technique into a critical-sized rat calvarial defect for 8 weeks. In general, the authors observed a better response in respect to bone regeneration for both conditions than just PLLA nanofibers. Besides, when added with MSC, the growth was faster than without.
Schuttler et al. [77] observed that after 4 weeks of the scaffold implantation into rat skull defect, the blend with collagen did not show a significant difference in comparison with PLLA/MSCs scaffold. Composite hydrogel scaffolds are also a good end product of nanofibers integration. It was observed by Huang et al. [78], who introduced NFs loaded with pANG and pBMP-2 genes into gelatin methacryloyl (GelMA) and thiolated chitosan (TCS) composite hydrogel system, utilizing PLLA as the base for NFs, and evaluated the structure of fiber of the healing in the skull defect for 12 weeks. The authors found that in the presence of the NFs, the capacity of bone regeneration was better than without it.
Kutikov et al. [67] produced and compared two spiral-wrapped HA − PELA (poly(D, L-lactic acid)-co-poly(ethylene glycol)-co-poly(D, L-lactic acid)) scaffolds, one with mesenchymal stromal cells (MSCs) and another with BMP-2, utilizing post-spinning process, as 3D cylinders. Their results showed that the MSC scaffold obtained better adherence than BMP-2, and after 4 and 12 weeks into critical-size rat femoral segmental defects, both conditions and the control group showed bone regeneration; however, the scaffold with MSCs was identified with weak birefringence, while the scaffold with BMP-2 formed a strong birefringence.
Utilizing the coaxial electrospinning, Bhattarai et al. [97] produced nanofibers with PLA/BMP-2 and PLA/TUDCA (tauroursodeoxycholic acid) — a common bile acid— to experiment with rabbit calvarial defect for 8 weeks. The authors observed that both functional additives enhanced new blood vessels formation and bone regeneration compared to the PLA scaffold. Khoobi et al. [79] also utilized PLA in a mixture with carbon nanotube and human Wharton’s jelly mesenchymal stem cells to introduce critical-size bone defects and achieve positive results. The same polymer was utilized by Patel et al. [80] added with cellulose nanocrystal (CNC) to analyze its influence on the biocompatibility and osteoinductivity, which were confirmed after 3 weeks inserted in rat calvarial defect in comparison with the control group.
A membrane-reinforced 3D nanofibrous scaffold was fabricated by Yang et al. [81] by serially combining wet electrospinning and freeze-drying, utilizing silk fibroin (SF), HA with and without BMP-2. The authors evaluated these conditions into rat calvarial defects for 8 weeks. At the end of the time, they observed bone regeneration for all scaffolds, but when added with BMP-2, this process was faster. Similarly, silk fibroin was also utilized by Xiao et al. [34] to produce a 3D scaffold with PCL and obtained better skull bone regeneration in rats after 12 weeks of treatment. Hadisi et al. [98] utilized the same biomaterial and hardystonite with and without gentamicin, acting as bioactive/drug carrier and antibacterial, respectively, and implanted in the subcutaneous dorsum of rats. The analyses after 4 weeks revealed the formation of collagen fibers and new vessels.
Yao et al. [82] produced a 3D scaffold through coaxial electrospinning with polyethylene glycol (PEG), calcium phosphate cement (CPC), rhBMP-2, dexamethasone (DXM), SF, and PLGA to explore the influence of DXM and rhBMP-2 in the skull defects bone regeneration in rats during 8 weeks. According to their results, both substances demonstrated expressive difference and greater improvement than other conditions. Additionally, Cui et al. [83], using a green approach that did not involve organic solvents, produced a micro/nanofibrous scaffold of HA/poly(lactide-co-glycolide) (HA/PLGA) composite to treat a critical-size bone defect model in rabbits, observing a significant increase in the expression of osteointegration, collagen type 1/2, and BMP-2. The same was studied and found by Tsai et al. [35].
Regarding the wide adoption of 3D format, it is essential to emphasize that this conformation should be highly porous with aligned fibers to provide better compatibility with the region that will be inserted. In addition, the design and manufacturing process must be in mind, as they are fundamental for developing a desirable scaffold [84]. Furthermore, among the variety of techniques, electrospinning is precise concerning control over the final product’s design and micro/nanostructure [84, 85], enabling the formation of healing with properties similar to bone tissue. In addition, electrospun scaffolds provide a dense framework of fibers with pore sizes and fiber diameters that closely resemble the architecture of the native extracellular matrix. However, it generates limited three-dimensional structures of relevant physiological thicknesses. On the other hand, 3D printing allows the digitally controlled fabrication of three-dimensional single/multi-material constructs with precisely ordered fiber and pore architecture in a single build. Thus, the combination of both techniques allows the manufacturing of scaffolds that resemble the physiological thickness and a multiscale heterogeneous fibrous architecture of bone tissue [60].
In this context, based on the presented data, materials manufactured with the electrospinning technique with different compositions have an osteogenic effect, stimulating bone tissue regeneration in animal models. Many other mechanisms can be proposed, but authors affirm that nanobiomaterials can promote mesenchymal cell migration and differentiation in osteoblasts, increasing the expression of growth factors and proteins and accelerating newly formed bone deposition [33, 100].
Toxicity and Legislation
For bone tissue engineering proposals, biomaterial designed for biological uses should be easy to create, be biocompatible, biodegradable, noncytotoxic, and be chemically well-matched with physiological fluids [51].
A question that frequently can be overlooked by the researchers is that the source of the biomaterial has been proved nontoxic does not guarantee that the final bioproduct is safe. Since, when combined with other matrix and substances, a rearranging of the material is often achieved, the final product can present toxicity, even though the primary material is biocompatible and nontoxic. Therefore, the structures must always be carefully evaluated before commercialization and application.
Despite the myriad of properties of materials in tissue healing and scaffolds, the adoption of care and complete determinations so that the materials can be used safely requires adequate studies of their properties, interactions, and migration. Different conditions can influence the movement of structured components present scaffolds or other structures such as temperature, mechanical stress on the structure, the construction characteristics related to the polymer structure, viscosity, and pH. Thus, the particle migration can also be influenced by the tissue composition and contact time, the material concentration, particle size, molecular properties of structures, and the polymer’s weight, solubility, and diffusivity [52, 61].
One of the problems in determining the biological/toxicological effects is the diversity of physical and chemical properties presented by the scaffolds made by the electrospinning technique. Thus, it is mandatory to establish predictive toxicity methods to characterize the potential risks of the rapidly growing number of new particles available for tissue engineering applications. The expression of the toxicological activity involving technology about reference materials that have already been subjected to rigorous tests and were considered to be of low or very high toxicity has been discussed as one of the alternatives to solve the lack of information and data concerning toxicity. In this way, this procedure would classify scaffolds made by the electrospinning technique of unknown toxicity and, thus, provide necessary information to identify hazards. Other possibilities for determining the safety of these new scaffolds, with potential applications in bone healing, include the use of in vitro tests validated by in vivo tests [36, 62] and also the adoption of a hazard scale based on higher reactivity (or effect) per unit surface area [62].
Few data regarding the toxicity of scaffolds made by the electrospinning technique used in tissue healing and scaffolds are available in the literature. However, there is a consensus that the population should be aware and informed about the issues of functionality and possible dangers of this technology, as they have a significant impact on the development and implementation of emerging technologies, especially those employed in the biomedical sector. In addition, regardless of the application, it is known that the use of the scaffolds must present a high level of protection of public health and consumer safety, as well as protection of the environment.
The application of components in the biomedical field is governed by control measures to guarantee the safety and protection of consumers, workers, and the environment, also serving to control the actions of public or private companies and standardize the production process through consistent criteria and safer routines [63].
The adoption of regulations, especially regarding the implementation of new technologies, is critical, considering that every new material contains numerous uncertainties and properties that need to be understood before its effective implementation. Thus, considering the advances in the area of materials for medicinal purposes, and even so that society can benefit from these new applications, there is a great challenge in order to overcome barriers related to the development of regulatory frameworks and particular requirements of security, being indisputable that these are applied and developed together.
In this sense, despite the positive evidence presented about enhancing the mechanical, technological, and functional properties of nanostructures and their application in medical products, the survey of risks and functionality of these materials is still neglected by consumers, researchers, and producers, as well as legal frameworks.
In general, there is no consensus or global regulation of the sector, with few protocols to assess the environmental impact, as well as established exposure limits, as it exists for other ecological components, such as heavy metals and gases. There are few regulations for products that have scaffolds made by the electrospinning technique in their composition, even in countries that conduct most of the development and application of these materials. However, several challenges need to be overcome to ensure the effective regulation of medical applications using electrospinning techniques and promoting a standardized approach among countries, such as assessing the risk and safety of nanoparticles, terminologies, definitions, and traceability of these scaffolds.
Alphandéry [52] mentioned that despite the fast development in bone tissue engineering, the regimentation is slowly taking form. The author discusses several aspects, claiming the emergence of regulation. Most of the articles that exploited the toxicity aspects of scaffolds manufactured by electrospinning for tissue healing affirm that the materials are safe and present low toxicity [23, 27, 52, 70,71,72, 86].
Clausen and Hansen [51] gathered the annexes of the European Union’s chemical legislation concerning biomaterials. The documents provided more organization and transparency; however, they indicate that manufacturers, importers, and downstream users place considerable work into understanding the specific behavior aspects and guidelines. The chemical legislation comprises 17 annexes detailing many of the technical and scientific specifics of the legislation and the standards for registration and chemical safety assessment. The annex improvements, aiming to elucidate registration obligations for nano-sized materials, are derive from years of discussion among the European Commission, EU member states, and other stakeholders. Even if the document can help as a guide, many questions are still very generalized, making practical decisions regarding specific uses, such as tissue engineering, very difficult.
Trends and Gaps in Knowledge
The use of scaffolds obtained by electrospinning for bone tissue regeneration has been widely studied using in vivo animal model studies, and it has shown satisfactory results for bone healing, tissue repair, the porosity of structures, and the resorption of active materials. However, several gaps concerning legislation, as well as challenges in the production and morphology of scaffolds, should be approached by future research. Several studies have reported the use of natural polymers and biodegradable synthetic polymers to the output of these biomaterials. Many in vitro and in vivo studies have demonstrated the capacity for bone regeneration after the implantation of scaffolds. However, further investigations must be performed to verify the biocompatibility of these materials when used within the human body [73, 74].
In addition, scaffolds must present not only a chemical structure that integrates with the tissues but also adequate porosity and specific properties to facilitate cell adhesion to the scaffold surface. The electrospinning technique allows the manufacturing of scaffolds with uniform fiber orientation and excellent mechanical properties [72, 74].
Although electrospun scaffolds have made great progress in bone repair, some issues remain to be resolved. First of all, it is important to check if the various materials with for manufacturing can be uniformly embedded and if some of the characteristics are still kept, such as biocompatibility, mechanical properties, and the rate of degradability. Due to these limitations, the practical applications of electrospun scaffolds have so far been relatively limited to in vitro and in vivo works in animal models, especially small-sized ones, studies with large animals were not found, and it was not studied in clinical trials, which are a crucial step towards the application of these bone tissue healing in practice.
An additional difficulty in the electrospinning process to produce the scaffolds is the use of some pure polymers, such as alginate and chitosan, due to their high molecular weight and low solubility mainly. In this case, the polymeric solution must be prepared with another polymer, forming a composite with carrier polymers as polyethylene oxide. Moreover, surfactants and solvents can be used to increase the content of these polymers in nanofibrous mats [73, 74].
Another aspect that the sector should face will be the regulation of the use of scaffolds made by electrospinning techniques in the biological system. There is a lack of answers regarding the criteria for choosing the characterization and quality control methods for these biomaterials, mainly related to toxicity, in addition to defining specific conditions for scaling production since it can lead to significant changes in the properties of the nanomaterials. Due to this, the need to establish regulations aimed at this type of application is fundamental for expanding the use of scaffolds [52].
Conclusion
In conclusion, the present work demonstrated that scaffolds made by electrospinning technique, with different origins such as metals, polymers, or ceramics, have a great potential to be used as bone grafts for bone healing stimulation. It was demonstrated that most of the scaffolds are noncytotoxic, biocompatible, and with osteogenic properties. Although all the positive evidence of the effects of the scaffolds on bone healing, there is still a lack of consensus about the more optimized method of manufacturing the scaffolds. Further studies are required to investigate the more appropriate technique for sample production, including electrospinning.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Ensrud KE. Fracture Risk in CKD. Clin J Am Soc Nephrol. 2013;8:1282–3. Available from: http://cjasn.asnjournals.org/lookup/doi/10.2215/CJN.06300613
Caplan AI. MSCs as Therapeutics. Mesenchymal Stromal Cells. New York: Springer New York; 2013 [cited 2020 Jun 20]. p. 79–90. Available from: https://springerlink.bibliotecabuap.elogim.com/chapter/10.1007/978-1-4614-5711-4_5
Dash BC, Thomas D, Monaghan M, Carroll O, Chen X, Woodhouse K, et al. An injectable elastin-based gene delivery platform for dose-dependent modulation of angiogenesis and inflammation for critical limb ischemia. Biomaterials. 2015;65:126–39. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0142961215005517
Gibot L, Chabaud S, Bouhout S, Bolduc S, Auger FA, Moulin VJ. Anticancer properties of chitosan on human melanoma are cell line dependent. Int J Biol Macromol. 2015;72:370–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0141813014005777
Karu T. Is it time to consider photobiomodulation as a drug equivalent? Photomed Laser Surg. 2013;31:189–91. Available from: https://www.liebertpub.com/doi/10.1089/pho.2013.3510
Kargozar S, Mozafari M, Hashemian SJ, Brouki Milan P, Hamzehlou S, Soleimani M, et al. Osteogenic potential of stem cells-seeded bioactive nanocomposite scaffolds: a comparative study between human mesenchymal stem cells derived from bone, umbilical cord Wharton’s jelly, and adipose tissue. J Biomed Mater Res B: Appl Biomater. 2018;106:61–72. Available from: http://doi.wiley.com/10.1002/jbm.b.33814
Hench LL, Jones JR. Bioactive glasses: frontiers and challenges. Front Bioeng Biotechnol. Frontiers Media S.A.; 2015 [cited 2020 Jun 20];3:194. Available from: http://journal.frontiersin.org/Article/10.3389/fbioe.2015.00194/abstract
Wojtowicz AM, Shekaran A, Oest ME, Dupont KM, Templeman KL, Hutmacher DW, et al. Coating of biomaterial scaffolds with the collagen-mimetic peptide GFOGER for bone defect repair. Biomaterials. Elsevier Ltd; 2010;31:2574–82. Available from: https://doi.org/10.1016/j.biomaterials.2009.12.008
Lei B, Guo B, Rambhia KJ, Ma PX. Hybrid polymer biomaterials for bone tissue regeneration. Front Med. 2019;13:189–201. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s11684-018-0664-6
Igwe JC, Mikael PE, Nukavarapu SP. Design, fabrication and in vitro evaluation of a novel polymer-hydrogel hybrid scaffold for bone tissue engineering. J Tissue Eng Regen Med. 2014;8:131–42. Available from: http://doi.wiley.com/10.1002/term.1506
Venkatesan J, Bhatnagar I, Manivasagan P, Kang KH, Kim SK. Alginate composites for bone tissue engineering: a review. Int J Biol Macromol. Elsevier B.V.; 2015;72:269–81. Available from: https://doi.org/10.1016/j.ijbiomac.2014.07.008
Jeevanandam J, Barhoum A, Chan YS, Dufresne A, Danquah MK. Review on nanoparticles and nanostructured materials: history, sources, toxicity and regulations. Beilstein J Nanotechnol. 2018;9:1050–74. Available from: https://www.beilstein-journals.org/bjnano/articles/9/98
Mi L, Zhang X, Yang W, Wang L, Huang Q, Fan C, et al. Artificial nano-bio-complexes: effects of nanomaterials on biomolecular reactions and applications in biosensing and detection. J Nanosci Nanotechnol. 2009;9:2247–55. Available from: http://openurl.ingenta.com/content/xref?genre=article&issn=1533-4880&volume=9&issue=4&spage=2247
Wen F, Chang S, Toh YC, Teoh SH, Yu H. Development of poly (lactic-co-glycolic acid)-collagen scaffolds for tissue engineering. Mater Sci Eng, C. 2007;27:285–92.
Cai EZ, Teo EY, Jing L, Koh YP, Qian TS, Wen F, et al. Bio-conjugated polycaprolactone membranes: a novel wound dressing. Arch Plast Surg. 2014;41:638.
Mathew A, Vaquette C, Hashimi S, Rathnayake I, Huygens F, Hutmacher DW, et al. Antimicrobial and immunomodulatory surface-functionalized electrospun membranes for bone regeneration. Adv Healthcare Mater. 2017;6:1601345.
Ma L, Yu Y, Liu H, Sun W, Lin Z, Liu C, et al. Berberine-releasing electrospun scaffold induces osteogenic differentiation of DPSCs and accelerates bone repair. Sci Rep. 2021;11:1027.
Chakraborty PK, Adhikari J, Saha P. Facile fabrication of electrospun regenerated cellulose nanofiber scaffold for potential bone-tissue engineering application. Int J Biol Macromol. Elsevier B.V.; 2019;122:644–52. Available from: https://doi.org/10.1016/j.ijbiomac.2018.10.216
Vieira S, Vial S, Reis RL, Oliveira JM. Nanoparticles for bone tissue engineering. Biotechnol Prog. 2017;33:590–611. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/btpr.2469
Alehosseini A, Ghorani B, Sarabi-Jamab M, Tucker N. Principles of electrospraying: a new approach in protection of bioactive compounds in foods. Crit Rev Food Sci Nutr. 2018;58:2346–63. Available from: https://www2.scopus.com/inward/record.uri?eid=2-s2.0-85059061807&doi=10.1080%2F10408398.2017.1323723&partnerID=40&md5=7ee4980a1d00b75c68afe0c276377f70
Rainer A, Spadaccio C, Sedati P, de Marco F, Carotti S, Lusini M, et al. Electrospun hydroxyapatite-functionalized PLLA scaffold: potential applications in sternal bone healing. Ann Biomed Eng. 2011;39:1882–90. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s10439-011-0289-2
Mouthuy P-A, Crossley A, Ye H. Fabrication of calcium phosphate fibres through electrospinning and sintering of hydroxyapatite nanoparticles. Mater Lett. 2013;106:145–50. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0167577X13006393
Jaganathan SK, Mani MP, Palaniappan SK, Rathanasamy R. Fabrication and characterisation of nanofibrous polyurethane scaffold incorporated with corn and neem oil using single stage electrospinning technique for bone tissue engineering applications. J Polym Res; 2018;25:146. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s10965-018-1543-1
Mathew A, Vaquette C, Hashimi S, Rathnayake I, Huygens F, Hutmacher DW, et al. Antimicrobial and immunomodulatory surface-functionalized electrospun membranes for bone regeneration. Adv Healthcare Mater. 2017;6:1601345. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28240815
Wang J, Wang M, Chen F, Wei Y, Chen X, Zhou Y, et al. Nano-hydroxyapatite coating promotes porous calcium phosphate ceramic-induced osteogenesis via BMP/Smad signaling pathway. Int J Nanomed. 2019;14:7987–8000. Available from: https://www.dovepress.com/nano-hydroxyapatite-coating-promotes-porous-calcium-phosphate-ceramic--peer-reviewed-article-IJN
Salimi E. Functionally graded calcium phosphate bioceramics: an overview of preparation and properties. Ceram Int. 2020;46:19664–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0272884220313651
Abazari MF, Nejati F, Nasiri N, Khazeni ZAS, Nazari B, Enderami SE, et al. Platelet-rich plasma incorporated electrospun PVA-chitosan-HA nanofibers accelerates osteogenic differentiation and bone reconstruction. Gene. Elsevier; 2019;720:144096. Available from: https://doi.org/10.1016/j.gene.2019.144096
Gul H, Khan M, Khan AS. Bioceramics. Handbook of Ionic Substituted Hydroxyapatites. Elsevier; 2020. p. 53–83. Available from: https://linkinghub.elsevier.com/retrieve/pii/B9780081028346000033
Jha BS, Ayres CE, Bowman JR, Telemeco TA, Sell SA, Bowlin GL, et al. Electrospun collagen: a tissue engineering scaffold with unique functional properties in a wide variety of applications. J Nanomater. 2011;2011:1–15. Available from: https://www.hindawi.com/journals/jnm/2011/348268/
Jaiswal AK, Chandra V, Bhonde RR, Soni VP, Bellare JR. Mineralization of nanohydroxyapatite on electrospun poly( <scp>l</scp> -lactic acid)/gelatin by an alternate soaking process: a biomimetic scaffold for bone regeneration. J Bioact Compat Polym. 2012;27:356–74. Available from: http://journals.sagepub.com/doi/10.1177/0883911512447211
Mehrasa M, Asadollahi MA, Ghaedi K, Salehi H, Arpanaei A. Electrospun aligned PLGA and PLGA/gelatin nanofibers embedded with silica nanoparticles for tissue engineering. Int J Biol Macromol. 2015;79:687–95. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0141813015003918
Yang H, Wen P, Feng K, Zong MH, Lou WY, Wu H. Encapsulation of fish oil in a coaxial electrospun nanofibrous mat and its properties. RSC Adv Royal Society of Chemistry. 2017;7:14939–46.
Hou G, Zhou F, Guo Y, Yang Z, Li A, Wang C, et al. In vivo study of a bioactive nanoparticle-gelatin composite scaffold for bone defect repair in rabbits. J Mater Sci: Mater Med. 2017;28:181. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s10856-017-5991-7
Xiao L, Wu M, Yan F, Xie Y, Liu Z, Huang H, et al. A radial 3D polycaprolactone nanofiber scaffold modified by biomineralization and silk fibroin coating promote bone regeneration in vivo. Int J Biol Macromol. 2021;172:19–29.
Tsai S, Ting Y. Synthesize of alginate/chitosan bilayer nanocarrier by CCD-RSM guided co-axial electrospray: a novel and versatile approach. Food Res Int. 2019;116:1163–72. Available from: https://www2.scopus.com/inward/record.uri?eid=2-s2.0-85057821508&doi=10.1016%2Fj.foodres.2018.11.047&partnerID=40&md5=a817089f084a185c56cc2c6cc3c7234e
Ranganathan S, Balagangadharan K, Selvamurugan N. Chitosan and gelatin-based electrospun fibers for bone tissue engineering. Int J Biol Macromol. Elsevier B.V.; 2019;133:354–64. Available from: https://doi.org/10.1016/j.ijbiomac.2019.04.115
Yuan X, Zhang M, Wang Y, Zhao H, Sun D. Using co-axial electrospray deposition to eliminate burst release of simvastatin from microparticles and to enhance induced osteogenesis. J Biomater Sci Polym Ed. Taylor & Francis; 2019;30:355–75. Available from: https://doi.org/10.1080/09205063.2018.1559978
Zhang X, Wang C, Liao M, Dai L, Tang Y, Zhang H, et al. Aligned electrospun cellulose scaffolds coated with rhBMP-2 for both in vitro and in vivo bone tissue engineering. Carbohydr Polym. Elsevier; 2019;213:27–38. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0144861719301808
Maitz MF. Applications of synthetic polymers in clinical medicine. Biosurf Biotribol. 2015;1:161–76. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2405451815000434
Eid K, Eldesouky A, Fahmy A, Shahat A, AbdElaal R. Calcium phosphate scaffold loaded with platinum nanoparticles for bone allograft. Am J Biomed Sci. 2013;5:242–9. Available from: http://www.nwpii.com/ajbms/papers/AJBMS_2013_4_03.pdf
Thakare VG, Joshi PA, Godse RR, Bhatkar VB, Wadegaokar PA, Omanwar SK. Fabrication of polycaprolactone/zirconia nanofiber scaffolds using electrospinning technique. J Polym Res. 2017;24:232. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s10965-017-1388-z
Liu Y, Miao Y-L, Qin F, Cao C, Yu X-L, Wu Y-H, et al. Electrospun poly (aspartic acid)-modified zein nanofibers for promoting bone regeneration. Int J Nanomed. 2019;14:9497–512. Available from: https://www.dovepress.com/electrospun-poly-aspartic-acid-modified-zein-nanofibers-for-promoting--peer-reviewed-article-IJN
Didekhani R, Sohrabi MR, Seyedjafari E, Soleimani M, Hanaee-Ahvaz H. Electrospun composite PLLA/oyster shell scaffold enhances proliferation and osteogenic differentiation of stem cells. Biologicals. 2018;54:33–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1045105618301155
Anitha A, Joseph J, Menon D, Nair S v., Nair MB. Electrospun yarn reinforced NanoHA composite matrix as a potential bone substitute for enhanced regeneration of segmental defects. Tissue Eng Part A. 2017;23:345–58. Available from: https://www.liebertpub.com/doi/10.1089/ten.tea.2016.0337
Ren Z, Ma S, Jin L, Liu Z, Liu D, Zhang X, et al. Repairing a bone defect with a three-dimensional cellular construct composed of a multi-layered cell sheet on electrospun mesh. Biofabrication. IOP Publishing; 2017;9:025036. Available from: https://iopscience.iop.org/article/10.1088/1758-5090/aa747f
Schofer MD, Roessler PP, Schaefer J, Theisen C, Schlimme S, Heverhagen JT, et al. Electrospun PLLA nanofiber scaffolds and their use in combination with BMP-2 for reconstruction of bone defects. Neves NM, editor. PLoS ONE. 2011;6:e25462. Available from: https://dx.plos.org/10.1371/journal.pone.0025462
Samadian H, Mobasheri H, Hasanpour S, Ai J, Azamie M, Faridi-Majidi R. Electro-conductive carbon nanofibers as the promising interfacial biomaterials for bone tissue engineering. J Mol Liq. Elsevier B.V.; 2020;298:112021. Available from: https://doi.org/10.1016/j.molliq.2019.112021
Su H, Liu K-Y, Karydis A, Abebe DG, Wu C, Anderson KM, et al. In vitro and in vivo evaluations of a novel post-electrospinning treatment to improve the fibrous structure of chitosan membranes for guided bone regeneration. Biomed Mater. IOP Publishing; 2016;12:015003. Available from: https://iopscience.iop.org/article/10.1088/1748-605X/12/1/015003
Foroughi MR, Karbasi S, Khoroushi M, Khademi AA. Polyhydroxybutyrate/chitosan/bioglass nanocomposite as a novel electrospun scaffold: fabrication and characterization. J Porous Mater. 2017;24:1447–60. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s10934-017-0385-2
Giaconia MA, Ramos S dos P, Pereira CF, Lemes AC, de Rosso VV, Braga ARC. Overcoming restrictions of bioactive compounds biological effects in food using nanometer-sized structures. Food Hydrocoll. Elsevier Ltd; 2020;107:105939. Available from: https://doi.org/10.1016/j.foodhyd.2020.105939
Clausen LPW, Hansen SF. The ten decrees of nanomaterials regulations. Nat Nanotechnol. Springer US; 2018;13:766–8. Available from: https://doi.org/10.1038/s41565-018-0256-2
Alphandéry E. A discussion on existing nanomedicine regulation: progress and pitfalls. Appl Mater Today. Elsevier Ltd; 2019;17:193–205. Available from: https://doi.org/10.1016/j.apmt.2019.07.005
Yadav P. Biomedical biopolymers, their origin and evolution in biomedical sciences: a systematic review. J Clin Diagn Res. 2015;9:21–5. Available from: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2015&volume=9&issue=9&page=ZE21&issn=0973-709x&id=6565
Zhong L, Hu D, Qu Y, Peng J, Huang K, Lei M, et al. Preparation of adenosine-loaded electrospun nanofibers and their application in bone regeneration. J Biomed Nanotechnol. 2019;15:857–77. Available from: https://www.ingentaconnect.com/content/10.1166/jbn.2019.2761
Tan H-L, Teow S-Y, Pushpamalar J. Application of metal nanoparticle–hydrogel composites in tissue regeneration. Bioengineering. 2019;6:17. Available from: http://www.mdpi.com/2306-5354/6/1/17
Li X, Wang J, Joiner A, Chang J. The remineralisation of enamel: a review of the literature. J Dent. 2014;42:S12–20. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0300571214500036
Yin L, Yang S, He M, Chang Y, Wang K, Zhu Y, et al. Physicochemical and biological characteristics of BMP-2/IGF-1-loaded three-dimensional coaxial electrospun fibrous membranes for bone defect repair. J Mater Sci: Mater Med. Springer US; 2017;28:94. Available from: https://doi.org/10.1007/s10856-017-5898-3
Ramos SP dos P, Giaconia MA, Assis M, Jimenez PC, Mazzo TM, Longo E, et al. Uniaxial and coaxial electrospinning for tailoring jussara pulp nanofibers. Molecules. 2021;26:1206.
Cardenas Turner J, Collins G, Blaber EA, Almeida EAC, Arinzeh TL. Evaluating the cytocompatibility and differentiation of bone progenitors on electrospun zein scaffolds. J Tissue Eng Regen Med. 2020;14:173–85. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/term.2984
Mellor LF, Huebner P, Cai S, Mohiti-Asli M, Taylor MA, Spang J, et al. Fabrication and evaluation of electrospun, 3D-bioplotted, and combination of electrospun/3D-bioplotted scaffolds for tissue engineering applications. BioMed Res Int. 2017;2017:1–9.
Chen G, Lv Y. Immobilization and application of electrospun nanofiber scaffold-based growth factor in bone tissue engineering. Curr Pharm Des. 2015;21:1967–78. Available from: http://www.eurekaselect.com/openurl/content.php?genre=article&issn=1381-6128&volume=21&issue=15&spage=1967
Watcharajittanont N, Putson C, Pripatnanont P, Meesane J. Layer-by-layer electrospun membranes of polyurethane/silk fibroin based on mimicking of oral soft tissue for guided bone regeneration. Biomed Mater. IOP Publishing; 2019;14:055011. Available from: https://iopscience.iop.org/article/10.1088/1748-605X/ab3502
Christy PN, Basha SK, Kumari VS, Bashir AKHKH, Maaza M, Kaviyarasu K, et al. Biopolymeric nanocomposite scaffolds for bone tissue engineering applications – a review. J Drug Deliv Sci Technol. Elsevier; 2020;55:101452. Available from: https://doi.org/10.1016/j.jddst.2019.101452
Marsich E, Bellomo F, Turco G, Travan A, Donati I, Paoletti S. Nano-composite scaffolds for bone tissue engineering containing silver nanoparticles: preparation, characterization and biological properties. J Mater Sci: Mater Med. 2013;24:1799–807. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s10856-013-4923-4
Hench LL. Third-generation biomedical materials. Science. 2002;295:1014–7. Available from: https://www.sciencemag.org/lookup/doi/10.1126/science.1067404
Chen X, Fu X, Shi J, Wang H. Regulation of the osteogenesis of pre-osteoblasts by spatial arrangement of electrospun nanofibers in two- and three-dimensional environments. Nanomed: Nanotechnol, Biol Med. Elsevier Inc.; 2013;9:1283–92. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1549963413001871
Kutikov AB, Skelly JD, Ayers DC, Song J. Templated repair of long bone defects in rats with bioactive spiral-wrapped electrospun amphiphilic polymer/hydroxyapatite scaffolds. ACS Appl Mater Interfaces. 2015;7:4890–901. Available from: https://pubs.acs.org/doi/10.1021/am508984y
Biazar E, Heidari Keshel S. Electrospun poly (3-hydroxybutyrate-co-3-hydroxyvalerate)/hydroxyapatite scaffold with unrestricted somatic stem cells for bone regeneration. ASAIO J. 2015;61:357–65. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002480-201505000-00019
Ramos SdP, Giaconia MA, Do Marco JT, Paiva RdS, De Rosso Vv, Lemes AC, Egea MB, Assis M, Mazzo TM, Longo E, Braga ARC. Development and characterization of electrospun nanostructures using polyethylene oxide: potential means for incorporation of bioactive compounds. Colloids and Interfaces. 2020;4(2):14. https://doi.org/10.3390/colloids4020014
Farokhi M, Jonidi Shariatzadeh F, Solouk A, Mirzadeh H. Alginate based scaffolds for cartilage tissue engineering: a review. Int J Polym Mater Polym Biomater. Taylor & Francis; 2020;69:230–47. Available from: https://doi.org/10.1080/00914037.2018.1562924
Lin W, Chen M, Qu T, Li J, Man Y. Three-dimensional electrospun nanofibrous scaffolds for bone tissue engineering. J Biomed Mater Res - Part B Appl Biomater. 2020;108:1311–21.
Bharadwaz A, Jayasuriya AC. Recent trends in the application of widely used natural and synthetic polymer nanocomposites in bone tissue regeneration. Mater Sci Eng C. Elsevier; 2020;110:110698. Available from: https://doi.org/10.1016/j.msec.2020.110698
Sedghi R, Shaabani A, Sayyari N. Electrospun triazole-based chitosan nanofibers as a novel scaffolds for bone tissue repair and regeneration. Carbohydr Polym. Elsevier; 2020;230:115707. Available from: https://doi.org/10.1016/j.carbpol.2019.115707
Taemeh MA, Shiravandi A, Korayem MA, Daemi H. Fabrication challenges and trends in biomedical applications of alginate electrospun nanofibers. Carbohydr Polym. Elsevier; 2020;228:115419. Available from: https://doi.org/10.1016/j.carbpol.2019.115419
MacNeill SR, Cobb CM, Rapley JW, Glaros AG, Spencer P. In vivo comparison of synthetic osseous graft materials. A preliminary study. J Clin Periodontol. 1999;26:239–45. Available from: http://doi.wiley.com/10.1034/j.1600-051X.1999.260407.x
Xue Y, Zhu Z, Zhang X, Chen J, Yang X, Gao X, et al. Accelerated bone regeneration by MOF modified multifunctional membranes through enhancement of osteogenic and angiogenic performance. Adv Healthcare Mater. 2021;10(6):2001369.
Schüttler KF, Bauhofer MW, Ketter V, Giese K, Eschbach DA, Yenigün M, et al. Direct incorporation of mesenchymal stem cells into a nanofiber scaffold – in vitro and in vivo analysis. Sci Rep. 2020;10(1):9557. https://doi.org/10.1038/s41598-020-66281-6
Huang L, Zhang Z, Guo M, Pan C, Huang Z, Jin J, et al. Biomimetic hydrogels loaded with nanofibers mediate sustained release of pDNA and promote in situ bone regeneration. Macromol Biosci. 2021;21(4):2000393.
Khoobi MM, Naddaf H, Hoveizi E, Mohammadi T. Silymarin effect on experimental bone defect repair in rat following implantation of the electrospun PLA / carbon nanotubes scaffold associated with Wharton’s jelly mesenchymal stem cells. J Biomed Mater Res Part A. 2020;108(9):1944–54.
Patel DK, Dutta SD, Hexiu J, Ganguly K, Lim K-T. Bioactive electrospun nanocomposite scaffolds of poly(lactic acid)/cellulose nanocrystals for bone tissue engineering. Int J Biol Macromol. 2020;162:1429–41.
Yang SY, Hwang TH, Che L, Oh JS, Ha Y, Ryu W. Membrane-reinforced three-dimensional electrospun silk fibroin scaffolds for bone tissue engineering. Biomed Mater. IOP Publishing; 2015;10:035011. Available from: https://iopscience.iop.org/article/10.1088/1748-6041/10/3/035011
Yao J, Liu Z, Ma W, Dong W, Wang Y, Zhang H, et al. Three-dimensional coating of SF/PLGA coaxial nanofiber membranes on surfaces of calcium phosphate cement for enhanced bone regeneration. ACS Biomater Sci Eng. 2020;6(5):2970–84.
Cui L, Zhang N, Cui W, Zhang P, Chen X. A novel nano/micro-fibrous scaffold by melt-spinning method for bone tissue engineering. J Bionic Eng. Jilin University; 2015;12:117–28. Available from: https://doi.org/10.1016/S1672-6529(14)60106-2
Bigham A, Foroughi F, Rezvani Ghomi E, Rafienia M, Neisiany RE, Ramakrishna S. The journey of multifunctional bone scaffolds fabricated from traditional toward modern techniques. Bio-Des Manuf. 2020;3(4):281–306.
Tamay DG, Dursun Usal T, Alagoz AS, Yucel D, Hasirci N, Hasirci V. 3D and 4D printing of polymers for tissue engineering applications. Front Bioeng Biotechnol. 2019;7(9). https://doi.org/10.3389/fbioe.2019.00164
Frohbergh ME, Katsman A, Mondrinos MJ, Stabler CT, Hankenson KD, Oristaglio JT, et al. Osseointegrative properties of electrospun hydroxyapatite-containing nanofibrous chitosan scaffolds. Tissue Eng Part A. 2015;21:970–81. Available from: https://www.liebertpub.com/doi/10.1089/ten.tea.2013.0789
Nguyen AT-B, Winckler P, Loison P, Wache Y, Chambin O. Physico-chemical state influences in vitro release profile of curcumin from pectin beads. Colloids Surf B: Biointerfaces. 2014;121:290–298.
Ma L, Yu Y, Liu H, Sun W, Lin Z, Liu C, et al. Berberine-releasing electrospun scaffold induces osteogenic differentiation of DPSCs and accelerates bone repair. Sci Rep. 2021;11(1):1027. https://doi.org/10.1038/s41598-020-79734-9
Zhang Y, Wang T, Li J, Cui X, Jiang M, Zhang M, et al. Bilayer membrane composed of mineralized collagen and chitosan cast film coated with berberine-loaded PCL/PVP electrospun nanofiber promotes bone regeneration. Front Bioeng Biotechnol. 2021;9:19. https://doi.org/10.3389/fbioe.2021.684335
Hashemi SF, Mehrabi M, Ehterami A, Gharravi AM, Bitaraf FS, Salehi M. In-vitro and in-vivo studies of PLA / PCL / gelatin composite scaffold containing ascorbic acid for bone regeneration. J Drug Deliv Sci Technol. 2021;61:102077.
Samadian H, Khastar H, Ehterami A, Salehi M. Bioengineered 3D nanocomposite based on gold nanoparticles and gelatin nanofibers for bone regeneration: in vitro and in vivo study. Sci Rep. 2021;11(1):13877. https://doi.org/10.1038/s41598-021-93367-6
Toprak Ö, Topuz B, Monsef YA, Oto Ç, Orhan K, Karakeçili A. BMP-6 carrying metal organic framework-embedded in bioresorbable electrospun fibers for enhanced bone regeneration. Mater Sci Eng: C. 2021;120:111738.
Padalhin A, Ventura R, Kim B, Sultana T, Park CM, Lee B-T. Boosting osteogenic potential and bone regeneration by co-cultured cell derived extracellular matrix incorporated porous electrospun scaffold. J Biomater Sci Polym Ed. 2021;32(6):779–98.
Huang Z, Wang W, Wang Q, Hojnacki T, Wang Y, Fu Y, et al. Coaxial nanofiber scaffold with super-active platelet lysate to accelerate the repair of bone defects. RSC Adv. 2020;10(59):35776–86.
Koç S, Çakmak S, Gümüşderelioğlu M, Ertekin TS, Çalış M, Yılmaz MM, et al. Three dimensional nanofibrous and compressible poly(L-lactic acid) bone grafts loaded with platelet-rich plasma. Biomed Mater. 2021;16(4):045012.
Andalib N, Kehtari M, Seyedjafari E, Motamed N, Matin MM. In vivo bone regeneration using a bioactive nanocomposite scaffold and human mesenchymal stem cells. Cell Tissue Bank. 2021;22(3):467–77.
Bhattarai DP, Kim MH, Park H, Park WH, Kim BS, Kim CS. Coaxially fabricated polylactic acid electrospun nanofibrous scaffold for sequential release of tauroursodeoxycholic acid and bone morphogenic protein2 to stimulate angiogenesis and bone regeneration. Chem Eng J. 2020;389:123470.
Hadisi Z, Bakhsheshi-Rad HR, Walsh T, Dehghan MM, Farzad-Mohajeri S, Gholami H, et al. In vitro and in vivo evaluation of silk fibroin-hardystonite-gentamicin nanofibrous scaffold for tissue engineering applications. Polym Test. 2020;91:106698.
Baudequin T, Gaut L, Mueller M, Huepkes A, Glasmacher B, Duprez D, et al. The osteogenic and tenogenic differentiation potential of C3H10T1/2 (mesenchymal stem cell model) cultured on PCL/PLA electrospun scaffolds in the absence of specific differentiation medium. Materials. 2017;10:1387. Available from: http://www.mdpi.com/1996-1944/10/12/1387
Dini F, Barsotti G, Puppi D, Coli A, Briganti A, Giannessi E, et al. Tailored star poly (ε-caprolactone) wet-spun scaffolds for in vivo regeneration of long bone critical size defects. J Bioact Compat Polym. 2016;31:15–30. Available from: http://journals.sagepub.com/doi/10.1177/0883911515597928
Funding
The authors acknowledge the financial support of the National Council for Scientific and Technological Development (CNPq), Coordination for the Improvement of Higher Education Personnel (CAPES) (001), and of the São Paulo Research Foundation (FAPESP) (process n° 2020/07046–0, 2020/03560–0, and 2020/06732–7).
Author information
Authors and Affiliations
Contributions
MAG: data curation, writing—original draft preparation, and editing. SdPR: data curation, writing—original draft preparation, and editing. TAA: data curation, writing—original draft, and editing. MdAC: writing—original draft and editing. ACR: data curation, writing—reviewing, methodology, and editing. ARCB: conceptualization, methodology, visualization, investigation, and writing—reviewing and editing.
Corresponding authors
Ethics declarations
Conflicts of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giaconia, M.A., dos Passos Ramos, S., Araújo, T.A. et al. Scaffold Production and Bone Tissue Healing Using Electrospinning: Trends and Gap of Knowledge. Regen. Eng. Transl. Med. 8, 506–522 (2022). https://doi.org/10.1007/s40883-022-00260-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-022-00260-3