Abstract
Purpose of Review
Sleep plays a pivotal role in regulating numerous physiological functions, including cardiovascular activity, glucose regulation, lipid management, and hormone secretion. This review explores the impact of insufficient and irregular sleep, as well as specific sleep disorders, on cardiometabolic risk. We aim to illuminate the potential mechanisms underlying these associations.
Recent Findings
A substantial body of evidence links sleep duration (both short and long), sleep regularity, and disorders such as obstructive sleep apnea, insomnia, and restless leg syndrome with the development of obesity, hypertension, hyperlipidemia, inflammation, diabetes, cardiovascular complications, and related mortality.
Summary
Despite the significant volume of research highlighting the interplay between sleep disturbances and cardiometabolic disorders, our understanding of this intricate relationship remains somewhat incomplete. Future research is essential to deepen our understanding and identify therapeutic strategies and interventions that can mitigate the detrimental effects of sleep disorders on cardiometabolic health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep plays a major role in regulating and maintaining human body functions, including cardiovascular function, blood glucose, lipids, and hormone secretion [1••, 2•]. Therefore, much of the recent research has focused on the impact of sleep on the maintenance of cardiometabolic health since cardiometabolic disorders stand as the primary cause of morbidity and mortality on a global scale [3••]. Cardiometabolic risks (CMR) constitute a group of interlinked factors such as hypertension, high blood sugar, dyslipidemia, and obesity [4]. Recent research suggests that incorporating sleep health as an additional metric in cardiovascular health (CVH) scores can enhance the prediction of cardiovascular disease (CVD) risk in adults [5••]. Observational studies suggest that even minor sleep changes at a population level correlate with changes in CVD risk factors. In view of this evidence, sleep duration was added as an eighth metric to the definition of cardiovascular health [6••]. In 2022, the American Heart Association expanded its “Life’s Simple 7” prevention targets by adding sleep health, renaming it “Life’s Essential 8 [6].” This inclusion emphasizes the holistic approach to cardiovascular health, covering areas like diet, physical activity, and now sleep, to benefit individuals of all ages.
This review explores topics like the consequences of insufficient and irregular sleep and other sleep disorders, such as obstructive sleep apnea (OSA), insomnia, and restless leg syndrome, on cardiometabolic disorders.
Search Methodology
We undertook an exhaustive literature search using PubMed and Google Scholar, prioritizing studies from the last 5 years (until mid-October 2023). Key older studies were also considered for a holistic perspective. Keywords like “sleep duration,” “insomnia,” “obstructive sleep apnea,” and “cardiometabolic disorders” guided our search. Additionally, we manually checked references of pertinent articles to ensure comprehensive coverage. After identifying potential papers, we assessed titles and abstracts for relevance. Only those aligning with our focus were read in-depth and critically evaluated for final inclusion in our review.
Sleep Duration and Cardiometabolic Health
There is a U-shaped relationship between sleep duration and adverse cardiometabolic health outcomes, including mortality [7], with the lowest risk observed in individuals who maintain a sleep duration of 7 to 8 h and increased risk with deviation from that range [7, 8•, 9••].
The current literature suggests that sleep patterns, mainly those related to sleep duration, can disrupt circadian rhythms, which can cause metabolic and endocrine dysfunction, increasing cardiovascular risks [5••, 10•]. In a recent study by Cui et al., researchers found a J-shaped association between sleep duration and the onset of CVD, especially in those aged 50 and above [11••]. Specifically, individuals sleeping more than 9 h faced a higher risk of CVDs, with the association being most pronounced among those with chronic health conditions.
Reduced sleep duration might affect hemodynamic control and cardiovascular regulation in healthy individuals, possibly through increasing inflammation and changes in endothelial function, which play a major role CVD risk [5••, 10•]. Proinflammatory processes and markers that promote atherosclerotic plaque development, like TNFα, IL-1, IL-6, IL-17, CRP, cellular adhesion molecules, and visfatin, have demonstrated a possible link with sleep deprivation in laboratory studies [12•].
Impact of Sleep Duration on Obesity and Appetite Regulation
Recent data indicate that both short and long sleep durations have been associated with an increased risk of obesity [13••, 14, 15]. This can be explained by physiological changes, such as reduced energy expenditure, glucose regulation disruption, and changes in appetite-regulating hormones (Fig. 1) [16•, 17•, 18, 19]. Moreover, lifestyle choices can lead to increased calorie intake, since sleep-deprived individuals are more likely to indulge in unhealthy eating habits [18].
This figure illustrates the complex interplay between sleep duration, leptin and ghrelin secretion changes, increased calorie consumption, endothelial dysfunction, and circadian rhythm disruptions. These factors collectively contribute to an increased inflammatory response, highlighting the importance of adequate sleep for maintaining optimal cardiometabolic health
Laboratory studies have shown that sleep deprivation is associated with a decrease in the secretion of leptin, a hormone that suppresses hunger, and an increase in ghrelin, a hormone that stimulates appetite [2•, 20]. This was further supported by a recent meta-analysis conducted by Lin et al., which showed that individuals with short sleep duration have a 14% increase in ghrelin levels compared to those with normal sleep duration [17•]. This suggests that sleep deprivation could potentially lead to increased hunger and food intake, contributing to weight gain [17•]. Furthermore, a sleep laboratory cohort study assessed 1202 participants from the European NoHoW trial, exploring the connection between objective sleep duration and obesity, finding that sleeping less than 6 h was associated with increased BMI and fat mass [21].
Similarly, another recent systematic review showed that short sleep duration was associated with an increased risk of metabolic syndrome in cohort studies, while long sleep duration was not associated with new-onset metabolic syndrome. In cross-sectional studies, both short and long sleep durations were associated with a high prevalence of metabolic syndrome[22•].
Moreover, recent research underscores a significant relationship between sleep duration and obesity in children, with a trend indicating that shorter sleep durations are associated with an increased risk of obesity [23,24,25,26,27]. This correlation appears to be influenced by a variety of factors, including age, gender, and cultural background. Notably, studies conducted during the COVID-19 pandemic, as well as research involving children from diverse geographical regions around the world, have contributed to these findings [25,26,27]. Therefore, it is crucial to consider sleep duration and sleep habits when addressing childhood obesity and formulating interventions to promote healthy weight in children.
Sleep Duration and Lipids
CVDs are influenced by cholesterol levels, particularly low levels of high-density lipoprotein (HDL) and high levels of low-density lipoprotein (LDL), which can be affected by age and gender, reflecting the impact of sex hormones on cholesterol metabolism [28]. Recent studies have further explored the relationship between sleep duration and cholesterol levels.
A study on 5016 Chinese middle-aged and older adults from the China Health and Retirement Longitudinal Study showed varying temporal relationships between sleep duration and different cholesterol types over 4 years of follow-up; individuals with higher triglycerides tended to sleep longer, and those who slept more had lower LDL and total cholesterol levels [29]. The strength and direction of these relationships are potentially influenced by factors like age and BMI. Specifically, higher HDL was notably linked to more sleep in the future for people aged 60 and above or those with a BMI exceeding 25. This association was not present in younger individuals or those with a lower BMI [29]. This report is supported by data showing that the effect of sleep duration on cholesterol levels in adolescents appears to be less consistent [30, 31]. The underlying reasons for these patterns are yet to be determined.
Sleep Duration and Glucose Regulation
There is also a close connection between sleep duration and glucose homeostasis. Sleep deficiency can disrupt glucose regulation, leading to insulin resistance and increasing the risk of diabetes [13••, 32, 33]. Several studies have demonstrated that short sleep duration is associated with an increased incidence of diabetes [18, 34]. In a cohort study of 384 Mexican adolescents, Chen et al. observed that objectively documented shorter sleep duration and a later sleep midpoint were linked to increased insulin resistance, as indicated by higher HOMA-IR (Homeostatic Model Assessment of Insulin Resistance) levels [32]. Another recent large study from the cohort of the Korean Genome and Epidemiology data over a 16-year follow-up linked sleep deprivation to increased T2DM risk [35••]. Those sleeping ≤5 h/night had a 17% higher diabetes risk (HR, 1.17; 95% CI, 1.02 to 1.33). Notably, the risk varied with obesity: non-obese, men, and those under 60 faced higher risks with ≤5 h of sleep, while obese individuals had risks with >7 h of sleep.
Collectively, the above findings were confirmed by a recent systematic review and meta-analysis of 10 studies with 107,756 participants that examined the link between sleep duration and T2DM risk [3••]. It found both short (≤5–6 h/night) and long sleep (>8–9 h/night) increased T2DM risk, with relative risks of 1.28 and 1.48, respectively. This supports a U-shaped relationship between sleep length and diabetes risk.
Sleep Duration and CVD
Recent comprehensive studies have delved into the broader implications of sleep on CVD risks. A study analyzed data from a vast population and emphasized the significance of proper sleep duration in reducing CVD risks.
Sleep duration also has an important effect on blood pressure levels [3••, 36]. Numerous studies have demonstrated an important association between short sleep duration and the risk of developing hypertension [37,38,39]. A systematic review and meta-analysis of cohort studies showed that both short and long sleep durations are associated with a higher risk of developing hypertension [13••].
A study analyzed data from 67,250 women and 29,114 men and explored the link between sleep duration and CVD risk [40]. Findings revealed that adhering to a healthy lifestyle, including proper sleep duration, significantly reduced CVD, coronary artery disease (CAD), and stroke risks. Including sleep duration in the lifestyle score improved its predictive accuracy, emphasizing the importance of sleep in cardiovascular health [40].
Recently, Pan et al. conducted a comprehensive meta-analysis to explore the connection between sleep deprivation and the risk of CVD, using data from 18 cohort studies focused on adult participants [41]. Their findings revealed that individuals sleeping only ≤5 or ≤6 h a day faced a heightened likelihood of developing CVDs, with a relative risk of 1.09 [41]. Interestingly, the younger population, aged ≥18 years, showed a stronger association compared to their counterparts aged ≥40 years, emphasizing the significant link between shorter sleep durations and increased CVD risks, highlighting the potential cardiac advantages of ensuring 7–8 h of sleep daily [41].
Another recent systematic review involving 97,837 participants aged 18–92 studied the relationship between sleep and arterial stiffness, a vascular health marker [42]. Results indicated that while sleep duration did not generally affect arterial stiffness, durations over 8 h increased pulse wave velocity. Both extended sleep and poor quality were linked to arterial stiffness in adults.
Putting it together, sleep duration significantly influences cardiometabolic health. Ideally, adults should aim for 7–8 h of sleep, with deviations linked to increased health risks. Disturbed sleep can cause metabolic disruptions, increase cardiovascular risks, affect appetite regulation, and lead to obesity. Additionally, it impacts cholesterol metabolism and glucose homeostasis, elevating diabetes risk. Moreover, sleep duration correlates with blood pressure regulation. In summary, optimal sleep duration is vital for maintaining cardiometabolic balance.
Sleep Irregularity and Cardiometabolic Risk
Irregularities in both the duration and timing of sleep are emerging as novel risk factors for CVDs, irrespective of traditional CVD risk factors and sleep quantity/quality.
Recent research demonstrates that irregular sleep duration or timing is associated with adverse metabolic outcomes such as increased blood pressure, abnormal lipid profile, and insulin resistance [43, 44], all of which can increase CVD risks, in addition to sleep regularity’s direct effect on the cardiovascular system integral rhythmicity.
Irregular sleep can disrupt the circadian rhythm, causing different sleep-wake disorders [45••]. Those circadian rhythm disruptions result in many pathophysiological changes, including autonomic nervous dysfunction [46], inflammation [47, 48•], and metabolic disorders [49], which can increase cardiovascular risks.
There are several measures used to assess sleep regularity [50]. Each measure reflects specific features of sleep regularity. Interdaily stability (IS) and intra-individual standard deviation (SD) reflect the variability of the overall sleep during the monitored period. Sleep regularity index (SRI) describes sleep variability between consecutive days. On the other hand, social jetlag (SJL) mainly measures sleep regularity throughout the week, and is insensitive to day-to-day sleep variability, and reflects the misalignment between the body’s internal clock and social schedule [50].
A recent study analyzed over 10 million hours of accelerometer data from 60,977 UK Biobank participants [51••], and showed that higher sleep regularity was associated with a 20–48% lower risk of all-cause mortality, a 16–39% lower risk of cancer mortality, and a 22–57% lower risk of cardiometabolic mortality across the top 4 Sleep Regularity Index (SRI) quintiles compared to the least regular quintile [51••]. Sleep regularity was found to be a stronger predictor of all-cause mortality than sleep duration. The findings suggest that sleep regularity is a vital predictor of mortality risk and may be another practical focus for enhancing health and longevity rather than just sleep duration.
The relation between sleep regularity and hypertension seems to vary according to the sleep regularity measure studied. Some studies have demonstrated a link between SRI, IS, and hypertension [44, 52]. On the other hand, the link between SJL, SD, and hypertension was less consistent [53,54,55,56,57]. These differences could be attributed to the different study designs used as well as to the sleep regularity measures studied with measures like SRI and IS, being more sensitive in covering all the sleep-wake information throughout the recording period [50].
Of the sleep regularity measures, SD and IS exhibit a more consistent association with glycated hemoglobin A1c (HbA1c) levels in individuals with diabetes compared to the general population [43, 52, 53, 58,59,60]. There is also a link between SRI and diabetes, glucose levels, and HbA1c [44, 61]. On the other hand, SJL effect on glucose metabolism varies according to age [50, 56, 57, 60, 62].
The relation between obesity and sleep regularity varies according to the specific measure used. For example, SRI demonstrated a significant association with obesity [44]. On the other hand, the relationship between IS and obesity seems less consistent [52]. As for the relationship between obesity and SJL, the results are mixed, with adults showing a stronger association between SJL and obesity when compared to children and adolescents [55,56,57, 63,64,65]. However, a recent study of 277 adolescents demonstrated that the association of visceral adiposity with MetS is worse among those with circadian misalignment, delayed sleep phase, an irregular sleep-wake cycle, or greater SJL [66•]. It also appears that SD of sleep duration has a stronger link to obesity and BMI compared to sleep timing [53, 58, 67, 68].
Evidence linking irregular sleep with CAD is limited, but two studies offer some insights into potential associations. In a study of almost 2000 participants, those with greater variability in sleep duration and onset were more likely to develop cardiovascular events [69•]. Another study involving 1978 adults found that participants with higher sleep irregularity exhibited a 10-year increased risk of cardiovascular disease [44].
Current research suggests that irregular sleep patterns, including variations in sleep duration and timing, are emerging as novel risk factors for cardiometabolic disorders. However, the evidence is less solid and varies depending on the specific measure used. Future research should focus on refining sleep regularity measures, investigating potential underlying mechanisms, and conducting longitudinal studies to establish causality. Additionally, potential confounding effects of other sleep disorders and lifestyle factors should be considered in future studies.
Obstructive Sleep Apnea and Cardiometabolic Risk
Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder (SDB), affecting approximately 34% of men and 17% of women aged 30 to 70 [70]. OSA is characterized by recurrent episodes of partial or complete upper airway collapse during sleep, causing cyclical episodes of hypoxemia, hypercapnia, and sleep fragmentations. This results in sleep disruption, fluctuations in intrathoracic pressure, and increased sympathetic nervous system activity [71]. Intermittent hypoxia also produces oxygen-free radicals, which lead to an enhanced inflammatory response. Over time, this can heighten the risk of cardiovascular diseases, including systemic hypertension, congestive heart failure, arrhythmias, atherosclerosis, stroke, and pulmonary hypertension [71, 72].
OSA and Cardiovascular Risks
OSA has been associated with various cardiovascular disorders. Recent findings have emphasized the role of hypoxia burden in predicting cardiovascular disease (CVD) outcomes in OSA patients [73]. This burden reflects the extent, depth, and duration of OSA-related low oxygen levels. It has been linked to increased CVD mortality and other adverse health impacts [74••, 75••]. Trzepizur et al. demonstrated that hypoxia burden and the percentage of sleep time with oxygen saturation <90% were significantly associated with the incidence of cardiovascular events in a clinical cohort of more than 5300 individuals with OSA [75••].
Furthermore, a recent cohort study from Hong Kong with 1860 participants examined the relationship between sleep parameters and major adverse cardiovascular events (MACEs) over a median of 8.3 years [76••]. The study found that the AHI was not a consistent predictor of MACEs. Instead, the duration of sleep with oxygen saturation below 90% (TST90) and both wake and nocturnal heart rate were more reliable indicators. This suggests that TST90 and mean heart rate are better predictors for MACE in OSA patients than AHI. However, a randomized controlled trial study indicated that OSA does not necessarily increase cardiovascular events in non-sleepy patients with ACS, and the use of CPAP does not significantly reduce this prevalence, highlighting the intricate relationship between OSA and cardiovascular risk [77•]. Therefore, future research endeavors should aim to uncover the underlying cardiometabolic complications in OSA and design personalized treatment strategies, while also validating these study results across diverse populations.
Moreover, OSA and CVD share common risk factors, such as obesity, insulin resistance, incident diabetes, and dyslipidemia [78, 79•, 80]. Recent epidemiological studies demonstrated that individuals with OSA are more likely to have MetS [81,82,83,84].
The American Heart Association (AHA) advocates for screening OSA in patients with certain cardiovascular conditions, such as resistant hypertension, pulmonary hypertension, and recurrent atrial fibrillation [85]. It also suggests considering sleep apnea evaluation in patients with tachy-brady syndrome, ventricular tachycardia, or those who have survived sudden cardiac arrest, especially if sleep apnea is suspected after a comprehensive sleep assessment.
As a sleep medicine specialist, understanding this connection is crucial in OSA patient care and risk evaluation. Continued research is vital to deepen our comprehension of this relationship and tailor treatments for OSA patients with higher cardiovascular risks.
Figure 2 illustrates the relationship between OSA and cardiovascular risks
It illustrates the relationship between obstructive sleep apnea (OSA) and cardiovascular risks. It shows how OSA, through mechanisms such as hypoxia, hypercapnia, arousals, and intrathoracic pressure fluctuations, can lead to increased sympathetic activity, oxidative stress, inflammatory response, and endothelial dysfunction, which in turn contribute to cardiovascular conditions like hypertension, heart failure, atherosclerosis, arrhythmias, and coronary heart disease
The Relationship Between OSA and Hypertension
Hypertension is common in OSA patients, with estimates suggesting that 30 to 50% of hypertensive patients have coexisting OSA. Conversely, half of OSA patients have comorbid hypertension [72]. Despite the shared risk factors between hypertension and OSA, such as obesity and metabolic syndrome, their relationship is independent [86]. Furthermore, the ESADA group’s recent study demonstrated the significance of monitoring bicarbonate levels to understand hypertension pathophysiology in OSA patients [87].
There is significant evidence to support using CPAP in hypertensive OSA patients. CPAP treatment leads to a drop of 2 to 2.5 mmHg in systolic blood pressure (SBP) and 1.5 to 2 mmHg in diastolic blood pressure (DBP); this response seems to be more pronounced in patients with resistant hypertension [88, 89]. Although this reduction may appear modest, research suggests that even a slight decrease can positively impact cardiovascular risk [90]. In a recent study of hypertensive OSA patients from the ESADA cohort with a follow-up of 2–36 months, the initiation of positive airway pressure (PAP) treatment led to significant reductions in systolic and diastolic blood pressure (BP). BP control showed marked improvement post-PAP treatment, especially for those on monotherapy [91•]. Notably, the improvement in BP dependent on antihypertensive treatment was found to be independent of any confounders [91•]. Moreover, a recent large clinical trial assessed the prolonged impacts of OSA and CPAP on BP in patients with ACS, and segregated patients into three groups based on OSA diagnosis and CPAP adherence [92••]. After an average of 41.2 months, there were no significant BP differences between OSA and non-OSA groups. However, a notable BP rise was observed in patients with AHI > 40 [92••]. Remarkably, persistent adherence to CPAP treatment led to a BP reduction after 18 months, especially in severe OSA patients, suggesting that consistent CPAP treatment can mitigate this rise.
OSA and Heart Failure
Heart failure (HF) is a significant cardiac outcome in OSA patients [93]. Among HF patients, the OSA prevalence ranges from 15 to 50% [94•]. Several mechanisms explain OSA’s effects on HF, including intrathoracic pressure changes during sleep and sympathetic nervous system activation from hypoxia [95].
Multiple mechanisms underlie the pathophysiological effects of OSA on HF. Apneic events during sleep cause intrathoracic pressure changes, increasing venous return and left ventricular afterload while decreasing stroke volume (SV) [95]. This, coupled with sympathetic nervous system activation from hypoxia and frequent arousals, results in tachycardia, vasoconstriction, and elevated myocardial oxygen consumption, thereby increasing myocardial infarction risk [95]. Hypoxia independently predicts ventricular dysfunction and impairs myocardial contractility, leading to oxidative stress, myocardial damage, and reduced left ventricular ejection fraction (LVEF) [96]. Furthermore, hypoxia-induced pulmonary hypertension amplifies right ventricular afterload, promoting HF onset [95].
CPAP treatment offers several benefits for HF patients, including reduced sympathetic activity, blood pressure, myocardial oxygen consumption, improved cardiac function, and fewer HF-related hospitalizations [97]. However, it does not consistently improve LVEF in OSA patients with stable systolic dysfunction [97], so its long-term advantages for HF patients remain under study.
OSA and Atrial Fibrillation
OSA is a standalone risk factor for atrial fibrillation (AF). Severe OSA patients have a four-fold higher AF incidence than non-OSA individuals, and there seems to be a potential dose-response relationship between OSA severity and the risk of AF [98]. The proposed mechanisms behind this involve a mix of acute atrial stimulation and long-term changes, such as chronic electrical and structural alterations [99]. Understanding these mechanisms can help develop new treatments and optimize current ones.
A recent study found that the AF incidence was 88% higher in OSA patients, with both age and hypertension reinforcing this association [100]. Additionally, AF-related OSA patients experience higher cardioversion recurrence rates and increased catheter ablation failures [99].
CPAP therapy remains the primary and preferred treatment for OSA. Li et al.’s 2021 meta-analysis, encompassing nine studies with 14,812 participants, suggested that CPAP might decrease AF in patients not undergoing rhythm adjustment or direct cardioversion [101•]. Yet, a recent randomized controlled trial indicated that CPAP treatment did not significantly lower the likelihood of AF recurrence post-ablation for patients with paroxysmal AF and OSA [102].
These findings suggest the importance of considering this relationship for future AF prevention strategies.
OSA and Coronary Artery Disease
Repetitive low-oxygen cycles in OSA lead to chronic and acute changes like intermittent hypoxia, acidosis, sympathetic overactivation, inflammation, oxidative stress, insulin resistance, elevated lipids, and endothelial dysfunction, which can promote atherosclerosis and contribute to CAD development and plaque instability [103].
Current evidence indicates an increased risk of CAD in OSA patients [104]. More than 70% of patients with acute CAD have undiagnosed OSA [105•]. Additionally, OSA has been linked to an increased risk of nocturnal ischemic events [105•].
A post hoc examination of the OSA-ACS project, which sequentially enrolled ACS patients and performed overnight sleep studies from June 2015 to January 2020, explored the relationship between OSA and long-term cardiovascular risks in ACS patients revealed that ACS patients with hypertension, especially severe hypertension, had an elevated risk of major cardiovascular events due to OSA [106••]. However, this was not the case for ACS patients without hypertension, highlighting the importance of identifying OSA in ACS patients with hypertension.
In OSA patients with CAD comorbidity, CPAP therapy has shown reduced cardiovascular events and mortality [107].
CPAP Therapy and Cardiovascular Outcomes
Although CPAP therapy has been found to lessen systemic inflammation and is correlated with a tendency towards a lower risk of cardiovascular incidents, its influence on the risk of heart attacks and acute coronary syndrome (ACS) is still under discussion.
OSA, linked to elevated cardiovascular risks, has been studied for the potential benefits of CPAP treatment. While observational research supports CPAP’s positive effects [108,109,110], many recent RCTs have shown limited benefits, especially in non-sleepy patients with severe conditions. However, prior research has not fully addressed the diverse nature of OSA, which has multiple subtypes due to various factors like anatomy, inflammation, and obesity. This diversity leads to different physiological issues [111•, 112]. New studies have pinpointed markers related to OSA’s hypoxic burden and cardiac response as indicators of OSA’s impact on health and treatment outcomes, potentially aiding in CVD risk categorization [111•]. CVD risk linked to OSA varies based on factors like age, gender, symptoms, and OSA’s physiological effects, phenotypes, and endotypes [113•, 114]. Previous trials have not focused on patient subgroups most vulnerable to CVD or responsive to treatments, proposing specific apnea-related measures for risk and intervention targeting. The International Collaboration of Sleep Apnea Cardiovascular Trialists (INCOSACT initiative) emphasizes considering the individual differences in OSA and enhancing treatment adherence [115].
Surprisingly, in the cohort study from Hong Kong, the application of regular CPAP treatment did not reduce MACE occurrences in patients with moderate to severe OSA [76••]. Yet, a distinct subgroup, characterized by younger age, higher obesity, increased severity of OSA, and more cardiovascular risks, did exhibit a reduced risk of MACEs when subjected to regular CPAP treatment. Moreover, a recent cohort study with a follow-up period of 5 years reported that the presence/severity of OSA and its related PSG parameters were not associated with worse cardiovascular/mortality prognosis in patients with resistant hypertension [116]; however, the study showed that CPAP treatment might be protective in individuals with moderate/severe OSA. These findings emphasize the need for a tailored approach to treating OSA, particularly by identifying patients with specific clinical markers who are most likely to benefit from CPAP. Building upon this, a recent preliminary report of an IPD meta-analysis of RCTs, which evaluated 4186 patients, mostly hypertensive men with moderate OSA, found that while the initial risk of major cardiovascular events was similar regardless of CPAP use, consistent adherence to CPAP significantly reduced the risk [117]. While these findings are still preliminary, they highlight the critical role of CPAP adherence for secondary cardiovascular prevention in OSA patients, reinforcing the notion that consistent treatment is crucial, despite ongoing debates about the overall effectiveness of CPAP in reducing cardiovascular events.
In summary, it is vital to realize OSA’s multifaceted link with CVD, stressing the importance of recognizing OSA’s diversity in research and adherence to treatment. More robust trials are needed before dismissing CPAP for high-risk OSA patients. Enhanced collaboration among specialists and tailored risk assessments utilizing emerging biomarkers in CVD risk assessment are essential.
OSA Paradox and Hypoxia Preconditioning
Despite the understanding that OSA exacerbates CVD risk, a recent analysis from the Veterans Health Administration (1999–2020) offers a fresh perspective on OSA and CVD [118•, 119]. Of 72,036 veterans hospitalized for acute MI, obese veterans with OSA had the lowest in-hospital mortality. After adjustments, compared to non-obese patients without OSA, the mortality odds ratio was marginally higher for obese individuals without OSA, but notably lower for those with OSA, regardless of obesity [118•]. The data hints at a potential protective role of OSA in acute MI, especially for the obese, underscoring the intricate relationship between OSA, obesity, and CVD and emphasizing the need for further research.
Insomnia and Cardiometabolic Risk
Nearly 20–30% of the general population suffers from symptoms of insomnia, with 8–10% fulfilling the criteria for a chronic insomnia disorder [120]. There is substantial evidence linking acute and chronic insomnia to adverse long-term health outcomes and negatively impacting the quality of life [121].
Insomnia is characterized by cerebral excitability or hyperarousal state [122]. This hyperarousal stems from the elevated overall metabolic rate during both sleep and wakefulness [123]. The increase in systemic inflammation, the dysregulation of the HPA axis leading to increased cortisol secretion in the early stages of sleep, in addition to the abnormal modulation of the autonomic nervous system (ANS), causing increased sympathetic activity and reduced parasympathetic activity, which contributes to adverse cardiovascular outcomes [1••, 122, 124].
Recent research indicates that insomniac patients, particularly those with objective short sleep duration, are at increased risk for various CVDs [1••], including hypertension, CAD, AF, and HF [121, 125, 126]. In a 16-year cohort study examining younger veterans, insomnia was linked to a 32% increased risk of AF and an earlier onset of AF by up to 2 years [127]. This association remained consistent even after accounting for factors like OSA. Further research is needed to determine if treating insomnia can reduce AF risk.
There also appears to be a relation between insomnia and HTN [128], and in population-based studies based on self-reported data, there was a significant link between insomnia, whether defined as a symptom or a disorder, and HTN [129,130,131,132]. A study using a US medical claims database revealed that within a year, 40.9% of untreated insomnia patients had arterial hypertension, compared to 26.3% in the non-insomnia group [133•], and the annual occurrence rate of arterial hypertension was notably higher among those with insomnia, with a marked difference of 44.20 (95% CI 43.76, 44.60) [133•]. This underscores a significant link between untreated insomnia and increased hypertension risk, which is supported by an earlier meta-analysis of prospective cohort studies, which estimated the risk of developing HTN with insomnia to be 5 to 20% [134].
A more recent systematic review and meta-analysis found a notable link between insomnia and an elevated risk of hypertension, particularly in individuals struggling with maintaining sleep and early morning awakenings; however, this correlation was significant mainly in European populations [135]. These findings could be crucial for preventing hypertension in those experiencing insomnia symptoms.
A more recent systematic review analyzed 21 studies, including 388,906 insomnia patients and 2,194,211 healthy subjects [136••], with a follow-up duration ranging from 3 to 19.6 years, showed that risks for CV mortality and MI were significantly higher in patients with insomnia (Relative Risk (RR) 1.53, p < 0.01, and RR 1.48, p = 0.03, respectively). The risk for all-cause mortality and CV disease incidence was also significantly higher in insomnia patients (RR 1.14, p = 0.03, and RR 1.31, p < 0.01, respectively). Regarding CV disease incidence, the researchers found that CV events increased non-significantly up to 10 years (RR: 1.40, 95% CI [0.99–1.98], p-value = 0.06, I2 = 98%). However, consistent trends with the overall result were observed at 10–20 years, which revealed a significantly higher incidence of CV events among insomnia patients vs. those without insomnia.
Several cross-sectional and longitudinal studies have reported significant associations between insomnia symptoms and metabolic markers such as insulin resistance, high fasting glucose levels, and the presence of T2D [137,138,139]. A recent systematic review of 12 studies revealed that insomnia increases the risk of developing metabolic syndrome components: hypertension by 41%, hyperglycemia by 29%, and obesity by 31%. However, there was no identified conclusive link between insomnia and hyperlipidemia [140]. On the other hand, genetically predicted insomnia consistently showed associations with higher BMI, triglyceride levels, and lower levels of high-density lipoprotein cholesterol [141].
A recent study that analyzed data from 2861 patients, with 8954 observations, obtained from two prospective cohorts (PsyMetab and PsyClin) [142•] concluded that insomnia disorders were significantly associated with metabolic disorders and risk of death.
In light of the above discussion, it is evident that insomnia is intricately linked with heightened cardiometabolic risk. As we move forward, research efforts must be directed towards establishing the causal relationship between insomnia and cardiometabolic risk factors, scrutinizing the interplay between insomnia and sleep duration on cardiometabolic risk, probing into potential moderating factors such as age and baseline hypertension, evaluating the impact of different insomnia subtypes on cardiometabolic risk, and undertaking longitudinal and intervention studies. By filling these research voids, we can gain a more nuanced understanding of the complex interplay between insomnia and cardiometabolic risk, thereby paving the way for more effective prevention and treatment strategies for both insomnia and cardiometabolic diseases.
Restless Leg Syndrome And Cardiometabolic Risk
Restless leg syndrome (RLS) is a common sleep disorder affecting 3 to 10% of adults [143••]. It is characterized by an unpleasant sensation in the lower limbs, which is worse at rest and improves with movement [143••]. RLS symptoms have circadian patterns and are worse at night, causing sleep disruption, which affects sleep duration and quality [144]. Many studies have shown that RLS patients have a higher risk of developing CVDs and other chronic diseases [145, 146].
Although it is unclear how RLS could lead to CVDs, several mechanisms have been suggested. RLS causes sleep disruption and negatively impacts sleep quality, increasing inflammatory responses such as eosinophil, platelet, C-reactive protein-to-albumin ratio, neutrophil-to-lymphocyte ratio monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and monocyte-to-lymphocyte ratio [147]. These inflammatory markers are known to contribute to the development of CVDs and have been linked to elevated blood pressure, CHD, and cardiovascular mortality [148].
A recent study evaluated the levels of proteins KNG1 and A1AT in patients with high-severity RLS and healthy controls [149]. It found elevated KNG1 and reduced A1AT levels in High Severity-RLS patients, independent of factors like age or smoking. The results suggest that these proteins are potential biomarkers for CVD risk in HS-RLS patients.
Moreover, dopamine deficiency in RLS can result in loss of inhibition in the spinal cord somatosensory and sympathetic pathways. This may lead to increased sympathetic activation, potentially increasing the risk of hypertension, CVDs, and stroke [146]. Impairment in the arterial baroreflex and increased peripheral vascular resistance, possibly due to sympathetic activity increase, may also contribute to CVDs [150]. Furthermore, patients with RLS display nocturnal blood pressure irregularities and factors like endothelial dysfunction and hypoxia, and a significant increase in total cholesterol and low-density lipoprotein cholesterol, elevating their CVD risk [147, 151].
Nearly three-quarters of RLS patients have periodic limb movements, which has also been linked to a higher risk of CVDs [152, 153]. A study examined the prevalence of RLS and PLMS in the Multi-Ethnic Study of Atherosclerosis. Findings indicated that 7% of participants had both conditions, with variations based on age and ethnicity but not by sex or obesity [154].
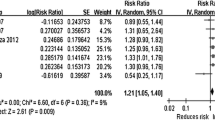
A 2017 systematic review of 18 cohorts by Kendzerska et al. examined the potential of RLS and PLMS as predictors for cardiovascular events (CVE) and overall mortality in adults [153]. The meta-analysis indicated a significant link between RLS and CVE, especially in severe and prolonged cases. However, the connection between RLS and overall mortality was less clear. On the other hand, all studies showed a positive correlation between PLMS and CVE/mortality, especially when accompanied by arousals [153]. The current evidence suggests that PLMS might be a significant prognostic factor for CVE and mortality. A 2023 systematic review and meta-analysis evaluated the association between PLMS and hypertension, including six observational studies, with 8949 participants demonstrating that the pooled risk ratio of hypertension in patients with PLMS was found to be 1.26 (95% CI, 1.12–1.41) [155••]. The results of this analysis indicate an increased risk of hypertension among patients with PLMS. However, prospective or interventional studies are needed to confirm this association. In a recent study, data were collected retrospectively from the Truven Health MarketScan Commercial Claims and Encounters database [156•]. The study examined 169,393 individuals, including 24,199 diagnosed with RLS who were then prospectively monitored for specific outcomes. Findings showed that RLS patients had an increased CVD risk, but treatment effectively lowered this threat. While untreated RLS patients had a higher adjusted hazard ratio for future CVD, all RLS treatments, except for ergot-dopamine, reduced the CVD risk [156•], suggesting that while RLS is associated with a higher future CVD risk, the treatment of RLS can significantly reduce this risk.
Recent evidence indicates that RLS patients are at a heightened risk for CVD and other chronic conditions. Given this, it is imperative for future studies to investigate the mechanisms linking RLS to these diseases and to pinpoint potential biomarkers indicating CVD risk among RLS sufferers. Therefore, examining the efficacy of different treatments in mitigating CVD risks and exploring non-drug solutions for RLS symptoms is crucial. By expanding on this knowledge, we aim to enhance the well-being of RLS patients and minimize their chances of severe health issues.
Conclusions
Sleep plays a major role in regulating and maintaining human body functions, including cardiovascular function, blood glucose, lipids, and hormone secretion. In this review, we explored recent data on the consequences of insufficient and irregular sleep and other common sleep disorders on cardiometabolic risk and attempted to understand the possible mechanisms behind this relationship. Sleep duration, sleep regularity, and disorders such as OSA, insomnia, and RLS have been associated with the development of obesity, hypertension, hyperlipidemia, inflammation, diabetes, CVDs, and cardiac disease-related mortality. Table 1 offers an overview of the main results presented in the paper, emphasizing the profound influence of sleep disorders on cardiometabolic well-being.
The current evidence suggests that sleep duration and regularity significantly influence cardiometabolic health. Optimal sleep is vital for maintaining cardiometabolic balance. Sleep disorders such as OSA, insomnia, and RLS have been linked to increased cardiometabolic risk, highlighting the need for further research to better understand these relationships and identify interventions to reduce risks caused by sleep disorders. By expanding our knowledge in this area, we aim to enhance the well-being of individuals with sleep disorders and minimize their chances of severe health issues.
Abbreviations
- AF:
-
atrial fibrillation
- AHI:
-
apnea-hypopnea index
- ANS:
-
autonomic nervous system
- BMI:
-
body mass index
- BP:
-
blood pressure
- CHD:
-
coronary heart disease
- CMR:
-
cardiometabolic risks
- CPAP:
-
continuous positive airway pressure
- CRP:
-
C-reactive protein
- CVD:
-
cardiovascular disease
- DBP:
-
diastolic blood pressure
- HbA1c:
-
hemoglobin A1c
- HDL:
-
high-density lipoprotein
- HF:
-
heart failure
- HTN:
-
hypertension
- HOMA-IR:
-
Homeostatic Model Assessment of Insulin Resistance
- HPA:
-
hypothalamus pituitary adrenal
- IL :
-
interleukin
- IS:
-
interdaily stability
- LDL :
-
low-density lipoprotein
- LVEF:
-
left ventricular ejection fraction
- MACEs:
-
major adverse cardiovascular events
- MetS:
-
metabolic syndrome
- MSLT:
-
multiple sleep latency test
- OSA:
-
obstructive sleep apnea
- RCTs:
-
randomized-controlled trials
- RLS:
-
restless leg syndrome
- SBD:
-
sleep-related breathing disorders
- SBP:
-
systolic blood pressure
- SD:
-
standard deviation
- SJL:
-
social jetlag
- SRI:
-
sleep regularity index
- SV:
-
stroke volume
- TNF:
-
tumor necrosis factor
- T2D:
-
type 2 diabetes
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Tobaldini E, Fiorelli EM, Solbiati M, Costantino G, Nobili L, Montano N. Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. Nat Rev Cardiol. 2019;16(4):213–24. https://doi.org/10.1038/s41569-018-0109-6. It explores the relationship between short sleep duration and cardiometabolic risk and the pathophysiology behind this association, providing clinical evidence to support the claim.
• Mosavat M, Mirsanjari M, Arabiat D, Smyth A, Whitehead L. The role of sleep curtailment on leptin levels in obesity and diabetes mellitus. Obes Facts. 2021;14(2):214–21. https://doi.org/10.1159/000514095. It discusses the impact of short sleep duration on the regulation of leptin, an adipocyte-derived peptide that regulates food intake and energy expenditure.
•• Dejenie TA, GM MT, Admasu FT, Adella GA, Enyew EF, Kifle ZD, et al. Impact of objectively-measured sleep duration on cardiometabolic health: a systematic review of recent evidence. Front Endocrinol (Lausanne). 2022;13:1064969. https://doi.org/10.3389/fendo.2022.1064969. It examines the association between objectively measured sleep duration and cardiometabolic profiles, including cardiovascular diseases, T2DM, and metabolic syndrome.
Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368–454. https://doi.org/10.1161/cir.0000000000001029.
•• Makarem N, Castro-Diehl C, St-Onge MP, Redline S, Shea S, Lloyd-Jones D, et al. Redefining cardiovascular health to include sleep: prospective associations with cardiovascular disease in the MESA Sleep Study. J Am Heart Assoc. 2022;11(21):e025252. https://doi.org/10.1161/JAHA.122.025252. It explores the relationship between sleep and cardiovascular health. It suggests that sleep parameters should be included in the definition of cardiovascular health, highlighting the prospective associations between sleep characteristics and the risk of cardiovascular disease.
•• Kumar M, Orkaby A, Tighe C, Villareal DT, Billingsley H, Nanna MG, et al. Life’s Essential 8: optimizing health in older adults. JACC Adv. 2023;2(7) https://doi.org/10.1016/j.jacadv.2023.100560. It proposes a comprehensive approach to optimizing health in older adults. It introduces the concept of “Life’s Essential 8”, a set of eight health domains that are crucial for maintaining health and well-being in older adults.
Wang W, Yang J, Wang K, Niu J, Wang J, Luo Z, et al. Assoication between self-reported sleep duration, physcial activity and the risk of all cause and cardiovascular diseases mortality from the NHANES database. BMC Cardiovasc Disord. 2023;23(1):467. https://doi.org/10.1186/s12872-023-03499-y.
• Yin J, Jin X, Shan Z, Li S, Huang H, Li P, et al. Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc. 2017;6(9) https://doi.org/10.1161/jaha.117.005947. The study suggests that both short and long sleep durations are associated with increased risk of all-cause mortality and cardiovascular events.
•• Yang L, Xi B, Zhao M, Magnussen CG. Association of sleep duration with all-cause and disease-specific mortality in US adults. J Epidemiol Community Health. 2021; https://doi.org/10.1136/jech-2020-215314. The study finds a U-shaped relationship, with both short and long sleep durations associated with increased mortality risk.
• AS BH, Alghannam AF, Aljaloud KS, Aljuraiban GS, MA AM, Dobia AM, et al. Joint consensus statement of the Saudi Public Health Authority on the recommended amount of physical activity, sedentary behavior, and sleep duration for healthy Saudis: background, methodology, and discussion. Ann Thorac Med. 2021;16(3):225–38. https://doi.org/10.4103/atm.atm_32_21. It The presents a consensus statement on the recommended amount of physical activity, sedentary behavior, and sleep duration for healthy of all age group. The paper provides a comprehensive review for the evidence on sleep duration and health and well-being.
•• Cui H, Xu R, Wan Y, Ling Y, Jiang Y, Wu Y, et al. Relationship of sleep duration with incident cardiovascular outcomes: a prospective study of 33,883 adults in a general population. BMC Public Health. 2023;23(1):124. https://doi.org/10.1186/s12889-023-15042-x. The study finds that both short and long sleep durations are associated with increased risk of cardiovascular outcomes.
• Barragan R, Zuraikat FM, Cheng B, Scaccia SE, Cochran J, Aggarwal B, et al. Paradoxical effects of prolonged insufficient sleep on lipid profile: a pooled analysis of 2 randomized trials. J Am Heart Assoc. 2023;12(20):e032078. https://doi.org/10.1161/JAHA.123.032078. Sleep restriction raised high-density lipoprotein cholesterol but lowered total and low-density lipoprotein cholesterol in premenopausal women.
•• Che T, Yan C, Tian D, Zhang X, Liu X, Wu Z. The association between sleep and metabolic syndrome: a systematic review and meta-analysis. Front Endocrinol (Lausanne). 2021;12:773646. https://doi.org/10.3389/fendo.2021.773646. The study found that both short and long sleep durations significantly increased the risk of metabolic syndrome. Also, short and long sleep increased the risk of obesity and high blood pressure. Short sleep was also found to potentially increase the risk of high blood sugar.
Saidi O, Rochette E, Del Sordo G, Doré É, Merlin É, Walrand S, et al. Eucaloric balanced diet improved objective sleep in adolescents with obesity. Nutrients. 2021;13(10) https://doi.org/10.3390/nu13103550.
Matricciani L, Dumuid D, Paquet C, Fraysse F, Wang Y, Baur LA, et al. Sleep and cardiometabolic health in children and adults: examining sleep as a component of the 24-h day. Sleep Med. 2021;78:63–74. https://doi.org/10.1016/j.sleep.2020.12.001.
• Zhu B, Shi C, Park CG, Zhao X, Reutrakul S. Effects of sleep restriction on metabolism-related parameters in healthy adults: a comprehensive review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2019;45:18–30. https://doi.org/10.1016/j.smrv.2019.02.002. It reviews the effects of sleep restriction on metabolism-related parameters in healthy adults, finding significant impacts on various metabolic outcomes.
• Lin J, Jiang Y, Wang G, Meng M, Zhu Q, Mei H, et al. Associations of short sleep duration with appetite-regulating hormones and adipokines: a systematic review and meta-analysis. Obes Rev. 2020;21(11):e13051. https://doi.org/10.1111/obr.13051. It investigates the associations between short sleep duration and appetite-regulating hormones and adipokines, finding significant relationships.
Antza C, Kostopoulos G, Mostafa S, Nirantharakumar K, Tahrani A. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. 2021;252(2):125–41. https://doi.org/10.1530/joe-21-0155.
Smiley A, King D, Bidulescu A. The association between sleep duration and metabolic syndrome: the NHANES 2013/2014. Nutrients. 2019;11(11) https://doi.org/10.3390/nu11112582.
van Egmond LT, Meth EMS, Engstrom J, Ilemosoglou M, Keller JA, Vogel H, et al. Effects of acute sleep loss on leptin, ghrelin, and adiponectin in adults with healthy weight and obesity: a laboratory study. Obesity (Silver Spring). 2023;31(3):635–41. https://doi.org/10.1002/oby.23616.
Larsen SC, Horgan G, Mikkelsen MK, Palmeira AL, Scott S, Duarte C, et al. Association between objectively measured sleep duration, adiposity and weight loss history. Int J Obes (Lond). 2020;44(7):1577–85. https://doi.org/10.1038/s41366-020-0537-3.
• Hua J, Jiang H, Wang H, Fang Q. Sleep duration and the risk of metabolic syndrome in adults: a systematic review and meta-analysis. Front Neurol. 2021;12:635564. https://doi.org/10.3389/fneur.2021.635564. It examines the relationship between sleep duration and the risk of metabolic syndrome in adults, providing a comprehensive analysis of the available evidence.
Dunn J, Singh K, Armstrong S, Wagner B, Counts J, Skinner A, et al. Physical activity and sleep changes among children with obesity during a period of school closures related to the COVID-19 pandemic. Res Sq [Preprint]. 2023. https://doi.org/10.21203/rs.3.rs-3293474/v1.
Fair M, Decker J, Fiks AG, Mayne S, Morales KH, Williamson AA, et al. Optimizing intervention components for sleep promotion in children in the context of obesity prevention: the SLEEPY 2.0 study protocol. Front Sleep. 2023:2. https://doi.org/10.3389/frsle.2023.1264532.
Gavela-Pérez T, Parra-Rodríguez A, Vales-Villamarín C, Pérez-Segura P, Mejorado-Molano FJ, Garcés C, et al. Relationship between eating habits, sleep patterns and physical activity and the degree of obesity in children and adolescents. Endocrinol Diabetes Nutr (Engl Ed). 2023;70(Suppl 3):10–7. https://doi.org/10.1016/j.endien.2023.08.001.
Duncan MJ, Mitchell J, Riazi NA, Belita E, Vanderloo LM, Carsley S, et al. Sleep duration change among adolescents in Canada: examining the impact of COVID-19 in worsening inequity. SSM Popul Health. 2023;23:101477. https://doi.org/10.1016/j.ssmph.2023.101477.
Roberto DMT, Pereira LJ, Vieira FGK, Di Pietro PF, de Assis MAA, Hinnig PF. Association between sleep timing, being overweight and meal and snack consumption in children and adolescents in southern Brazil. Int J Environ Res Public Health. 2023;20(18) https://doi.org/10.3390/ijerph20186791.
Robinson GA, Peng J, Peckham H, Radziszewska A, Butler G, Pineda-Torra I, et al. Sex hormones drive changes in lipoprotein metabolism. iScience. 2021;24(11):103257. https://doi.org/10.1016/j.isci.2021.103257.
Chen Z, Zhang X, Duan Y, Mo T, Liu W, Ma Y, et al. The relationship between sleep duration and blood lipids among chinese middle-aged and older adults: cross-lagged path analysis from CHARLS. Front Public Health. 2022;10:868059. https://doi.org/10.3389/fpubh.2022.868059.
Confortin SC, Aristizábal LYG, da Silva Magalhães EI, Barbosa AR, Ribeiro CCC, Batista RFL, et al. Association between sleep duration and cardiometabolic factors in adolescents. BMC Public Health. 2022;22(1):686. https://doi.org/10.1186/s12889-022-13119-7.
Sung V, Beebe DW, Vandyke R, Fenchel MC, Crimmins NA, Kirk S, et al. Does sleep duration predict metabolic risk in obese adolescents attending tertiary services? A cross-sectional study. Sleep. 2011;34(7):891–8. https://doi.org/10.5665/sleep.1122.
Chen P, Baylin A, Lee J, Dunietz GL, Cantoral A, Tellez Rojo MM, et al. The association between sleep duration and sleep timing and insulin resistance among adolescents in Mexico City. J Adolesc Health. 2021;69(1):57–63. https://doi.org/10.1016/j.jadohealth.2020.10.012.
Bawadi H, Al Sada A, Al Mansoori N, Al Mannai S, Hamdan A, Shi Z, et al. Sleeping duration, napping and snoring in association with diabetes control among patients with diabetes in Qatar. Int J Environ Res Public Health. 2021;18(8) https://doi.org/10.3390/ijerph18084017.
Tinajero MG, Malik VS. An update on the epidemiology of type 2 diabetes: a global perspective. Endocrinol Metab Clin North Am. 2021;50(3):337–55. https://doi.org/10.1016/j.ecl.2021.05.013.
•• Lee DY, Jung I, Park SY, Yu JH, Seo JA, Kim KJ, et al. Sleep duration and the risk of type 2 diabetes: a community-based cohort study with a 16-year follow-up. Endocrinol Metab (Seoul). 2023;38(1):146–55. https://doi.org/10.3803/EnM.2022.1582. Sleep deprivation was linked to an increased risk of T2DM, particularly among non-obese, younger individuals, and men. A significant interaction between sleep duration and obesity was also observed.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37–55. https://doi.org/10.1016/s0140-6736(16)31919-5.
Bock JM, Vungarala S, Covassin N, Somers VK. Sleep duration and hypertension: epidemiological evidence and underlying mechanisms. Am J Hypertens. 2022;35(1):3–11. https://doi.org/10.1093/ajh/hpab146.
Chang X, Chen X, Ji JS, Luo G, Chen X, Sun Q, et al. Association between sleep duration and hypertension in southwest China: a population-based cross-sectional study. BMJ Open. 2022;12(6):e052193. https://doi.org/10.1136/bmjopen-2021-052193.
Altman NG, Izci-Balserak B, Schopfer E, Jackson N, Rattanaumpawan P, Gehrman PR, et al. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med. 2012;13(10):1261–70. https://doi.org/10.1016/j.sleep.2012.08.005.
Guasch-Ferre M, Li Y, Bhupathiraju SN, Huang T, Drouin-Chartier JP, Manson JE, et al. Healthy lifestyle score including sleep duration and cardiovascular disease risk. Am J Prev Med. 2022;63(1):33–42. https://doi.org/10.1016/j.amepre.2022.01.027.
Pan Y, Zhou Y, Shi X, He S, Lai W. The association between sleep deprivation and the risk of cardiovascular diseases: a systematic meta-analysis. Biomed Rep. 2023;19(5):78. https://doi.org/10.3892/br.2023.1660.
Saz-Lara A, Luceron-Lucas-Torres M, Mesas AE, Notario-Pacheco B, Lopez-Gil JF, Cavero-Redondo I. Association between sleep duration and sleep quality with arterial stiffness: a systematic review and meta-analysis. Sleep Health. 2022;8(6):663–70. https://doi.org/10.1016/j.sleh.2022.07.001.
Huang T, Redline S. Cross-sectional and prospective associations of actigraphy-assessed sleep regularity with metabolic abnormalities: the multi-ethnic study of atherosclerosis. Diabetes Care. 2019;42(8):1422–9. https://doi.org/10.2337/dc19-0596.
Lunsford-Avery JR, Engelhard MM, Navar AM, Kollins SH. Validation of the sleep regularity index in older adults and associations with cardiometabolic risk. Sci Rep. 2018;8(1):14158. https://doi.org/10.1038/s41598-018-32402-5.
•• BaHammam AS, Pirzada A. Timing matters: the interplay between early mealtime, circadian rhythms, gene expression, circadian hormones, and metabolism—a narrative review. Clocks Sleep. 2023;5(3):507–35. https://doi.org/10.3390/clockssleep5030034. A recent comprehensive evidence-based review, highlighting that misalignments between the body’s natural clocks and eating patterns may increase the risk of metabolic disorders.
Gilbey MP. Special issue, “Circadian rhythms: autonomic & endocrine function in health and disease”. Auton Neurosci. 2019;220:102562. https://doi.org/10.1016/j.autneu.2019.102562.
Slavish DC, Taylor DJ, Dietch JR, Wardle-Pinkston S, Messman B, Ruggero CJ, et al. Intraindividual variability in sleep and levels of systemic inflammation in nurses. Psychosom Med. 2020;82(7):678–88. https://doi.org/10.1097/psy.0000000000000843.
• Girtman KL, Baylin A, O'Brien LM, Jansen EC. Later sleep timing and social jetlag are related to increased inflammation in a population with a high proportion of OSA: findings from the Cleveland Family Study. J Clin Sleep Med. 2022;18(9):2179–87. https://doi.org/10.5664/jcsm.10078. Later sleep schedules were correlated with elevated IL-6, while more pronounced social jetlag was tied to increased IL-1 levels, even after adjusting for OSA severity.
Bei B, Seeman TE, Carroll JE, Wiley JF. Sleep and physiological dysregulation: a closer look at sleep intraindividual variability. Sleep. 2017;40(9) https://doi.org/10.1093/sleep/zsx109.
Zhang C, Qin G. Irregular sleep and cardiometabolic risk: clinical evidence and mechanisms. Front Cardiovasc Med. 2023;10:1059257. https://doi.org/10.3389/fcvm.2023.1059257.
•• Windred DP, Burns AC, Lane JM, Saxena R, Rutter MK, Cain SW, et al. Sleep regularity is a stronger predictor of mortality risk than sleep duration: a prospective cohort study. Sleep. 2023; https://doi.org/10.1093/sleep/zsad253. A prospective cohort study using data from over 60,000 UK Biobank participants found that sleep regularity is a more potent predictor of mortality risk than sleep duration, linking higher sleep regularity with significantly lower risks of all-cause, cancer, and cardiometabolic mortality.
Abbott SM, Weng J, Reid KJ, Daviglus ML, Gallo LC, Loredo JS, et al. Sleep timing, stability, and BP in the Sueño Ancillary Study of the Hispanic Community Health Study/Study of Latinos. Chest. 2019;155(1):60–8. https://doi.org/10.1016/j.chest.2018.09.018.
Häusler N, Marques-Vidal P, Haba-Rubio J, Heinzer R. Association between actigraphy-based sleep duration variability and cardiovascular risk factors — results of a population-based study. Sleep Med. 2020;66:286–90. https://doi.org/10.1016/j.sleep.2019.02.008.
Mota MC, Silva CM, Balieiro LCT, Fahmy WM, Marqueze EC, Moreno CRC, et al. Social jetlag is associated with impaired metabolic control during a 1-year follow-up. Front Physiol. 2021;12:702769. https://doi.org/10.3389/fphys.2021.702769.
Mokhlesi B, Temple KA, Tjaden AH, Edelstein SL, Utzschneider KM, Nadeau KJ, et al. Association of self-reported sleep and circadian measures with glycemia in adults with prediabetes or recently diagnosed untreated type 2 diabetes. Diabetes Care. 2019;42(7):1326–32. https://doi.org/10.2337/dc19-0298.
Cespedes Feliciano EM, Rifas-Shiman SL, Quante M, Redline S, Oken E, Taveras EM. Chronotype, social jet lag, and cardiometabolic risk factors in early adolescence. JAMA Pediatr. 2019;173(11):1049–57. https://doi.org/10.1001/jamapediatrics.2019.3089.
Johnson DA, Reid M, Vu TT, Gallo LC, Daviglus ML, Isasi CR, et al. Associations of sleep duration and social jetlag with cardiometabolic risk factors in the study of Latino youth. Sleep Health. 2020;6(5):563–9. https://doi.org/10.1016/j.sleh.2020.02.017.
Rosique-Esteban N, Papandreou C, Romaguera D, Warnberg J, Corella D, Martínez-González M, et al. Cross-sectional associations of objectively-measured sleep characteristics with obesity and type 2 diabetes in the PREDIMED-Plus trial. Sleep. 2018;41(12) https://doi.org/10.1093/sleep/zsy190.
Soltero EG, Navabi N, Vander Wyst KB, Hernandez E, Castro FG, Ayers SL, et al. Examining 24-hour activity and sleep behaviors and related determinants in Latino adolescents and young adults with obesity. Health Educ Behav. 2022;49(2):291–303. https://doi.org/10.1177/10901981211054789.
Kelly RM, Healy U, Sreenan S, McDermott J, Coogan AN. An exploratory study of associations between sleep timing variability and cardiometabolic health in middle-aged adults with type 2 diabetes mellitus. Chronobiol Int. 2022;39(4):569–78. https://doi.org/10.1080/07420528.2021.2005083.
Fritz J, Phillips AJK, Hunt LC, Imam A, Reid KJ, Perreira KM, et al. Cross-sectional and prospective associations between sleep regularity and metabolic health in the Hispanic Community Health Study/Study of Latinos. Sleep. 2021;44(4) https://doi.org/10.1093/sleep/zsaa218.
Saylor J, Ji X, Calamaro CJ, Davey A. Does sleep duration, napping, and social jetlag predict hemoglobin A1c among college students with type 1 diabetes mellitus? Diabetes Res Clin Pract. 2019;148:102–9. https://doi.org/10.1016/j.diabres.2019.01.007.
Kim JH, Lyu YS, Kim SY. Impact of social jetlag on weight change in adults: Korean National Health and Nutrition Examination Survey 2016–2017. Int J Environ Res Public Health. 2020;17(12) https://doi.org/10.3390/ijerph17124383.
Hawkins MS, Levine MD, Buysse DJ, Abebe KZ, Hsiao WH, McTigue KM, et al. Sleep health characteristics among adults who attempted weight loss in the past year: NHANES 2017–2018. Int J Environ Res Public Health. 2021;18(19) https://doi.org/10.3390/ijerph181910170.
LeMay-Russell S, Schvey NA, Kelly NR, Parker MN, Ramirez E, Shank LM, et al. Longitudinal associations between facets of sleep and adiposity in youth. Obesity (Silver Spring). 2021;29(11):1760–9. https://doi.org/10.1002/oby.23281.
• Morales-Ghinaglia N, He F, Calhoun SL, Vgontzas AN, Liao J, Liao D, et al. Circadian misalignment impacts the association of visceral adiposity with metabolic syndrome burden in adolescents. Sleep. 2023; https://doi.org/10.1093/sleep/zsad262. The study emphasizes that circadian misalignment amplifies the effects of visceral obesity on cardiometabolic health, highlighting the importance of targeting it in preventative strategies for adolescents.
Papandreou C, Bulló M, Díaz-López A, Martínez-González MA, Corella D, Castañer O, et al. High sleep variability predicts a blunted weight loss response and short sleep duration a reduced decrease in waist circumference in the PREDIMED-Plus Trial. Int J Obes (Lond). 2020;44(2):330–9. https://doi.org/10.1038/s41366-019-0401-5.
Bowman MA, Brindle RC, Joffe H, Kline CE, Buysse DJ, Appelhans BM, et al. Multidimensional sleep health is not cross-sectionally or longitudinally associated with adiposity in the Study of Women’s Health Across the Nation (SWAN). Sleep Health. 2020;6(6):790–6. https://doi.org/10.1016/j.sleh.2020.04.014.
• Huang T, Mariani S, Redline S. Sleep irregularity and risk of cardiovascular events: the multi-ethnic study of atherosclerosis. J Am Coll Cardiol. 2020;75(9):991–9. https://doi.org/10.1016/j.jacc.2019.12.054. The findings from this study emphasize the potential cardiovascular implications of inconsistent sleep schedules.
Arredondo E, Udeani G, Panahi L, Taweesedt PT, Surani S. Obstructive sleep apnea in adults: what primary care physicians need to know. Cureus. 2021;13(9):e17843. https://doi.org/10.7759/cureus.17843.
André S, Andreozzi F, Van Overstraeten C, Ben Youssef S, Bold I, Carlier S, et al. Cardiometabolic comorbidities in obstructive sleep apnea patients are related to disease severity, nocturnal hypoxemia, and decreased sleep quality. Respir Res. 2020;21(1):35. https://doi.org/10.1186/s12931-020-1284-7.
Tietjens JR, Claman D, Kezirian EJ, De Marco T, Mirzayan A, Sadroonri B, et al. Obstructive sleep apnea in cardiovascular disease: a review of the literature and proposed multidisciplinary clinical management strategy. J Am Heart Assoc. 2019;8(1):e010440. https://doi.org/10.1161/jaha.118.010440.
Martinez-Garcia MA, Sanchez-de-la-Torre M, White DP, Azarbarzin A. Hypoxic burden in obstructive sleep apnea: present and future. Arch Bronconeumol. 2023;59(1):36–43. https://doi.org/10.1016/j.arbres.2022.08.005.
•• Azarbarzin A, Sands SA, Stone KL, Taranto-Montemurro L, Messineo L, Terrill PI, et al. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study. Eur Heart J. 2019;40(14):1149–57. https://doi.org/10.1093/eurheartj/ehy624. ‘Hypoxic burden’, a measure derived from overnight sleep studies, is a strong predictor of CVD mortality across populations, suggesting that the depth and duration of sleep-related upper airway obstructions are important characteristics of the disease.
•• Trzepizur W, Blanchard M, Ganem T, Balusson F, Feuilloy M, Girault JM, et al. Sleep apnea-specific hypoxic burden, symptom subtypes, and risk of cardiovascular events and all-cause mortality. Am J Respir Crit Care Med. 2022;205(1):108–17. https://doi.org/10.1164/rccm.202105-1274OC. Patients with elevated OSA-specific HB are at higher risk of a cardiovascular event and all-cause mortality.
•• Xu PH, Fong DYT, Lui MMS, Lam DCL, Ip MSM. Cardiovascular outcomes in obstructive sleep apnoea and implications of clinical phenotyping on effect of CPAP treatment. Thorax. 2023;78(1):76–84. https://doi.org/10.1136/thoraxjnl-2021-217714. The study found that sleep time with TST90 and mean heart rate, but not the AHI, were robust predictors of MACEs.
• Sanchez-de-la-Torre M, Sanchez-de-la-Torre A, Bertran S, Abad J, Duran-Cantolla J, Cabriada V, et al. Effect of obstructive sleep apnoea and its treatment with continuous positive airway pressure on the prevalence of cardiovascular events in patients with acute coronary syndrome (ISAACC study): a randomised controlled trial. Lancet Respir Med. 2020;8(4):359–67. https://doi.org/10.1016/S2213-2600(19)30271-1. Among non-sleepy patients with acute coronary syndrome, the presence of OSA was not associated with an increased prevalence of cardiovascular events, and treatment with CPAP did not significantly reduce this prevalence.
Siddiquee AT, Kim S, Thomas RJ, Lee MH, Ku Lee S, Shin C. Obstructive sleep apnoea and long-term risk of incident diabetes in the middle-aged and older general population. ERJ Open Res. 2023;9(2) https://doi.org/10.1183/23120541.00401-2022.
• Bajpai J, Pradhan A, Bajaj D, Verma AK, Kant S, Pandey AK, et al. Prevalence of dyslipidaemia in OSA patients at a tertiary care center. Am J Cardiovasc Dis. 2023;13(1):1–9. Patients with OSA had a higher prevalence of dyslipidemia, with lipid abnormalities increasing with OSA severity.
Xu PH, Hui CKM, Lui MMS, Lam DCL, Fong DYT, Ip MSM. Incident type 2 diabetes in OSA and effect of CPAP treatment: a retrospective clinic cohort study. Chest. 2019;156(4):743–53. https://doi.org/10.1016/j.chest.2019.04.130.
Gaines J, Vgontzas AN, Fernandez-Mendoza J, Bixler EO. Obstructive sleep apnea and the metabolic syndrome: the road to clinically-meaningful phenotyping, improved prognosis, and personalized treatment. Sleep Med Rev. 2018;42:211–9. https://doi.org/10.1016/j.smrv.2018.08.009.
Liu L, Su X, Zhao Z, Han J, Li J, Xu W, et al. Association of metabolic syndrome with long-term cardiovascular risks and all-cause mortality in elderly patients with obstructive sleep apnea. Front Cardiovasc Med. 2021;8:813280. https://doi.org/10.3389/fcvm.2021.813280.
Song SO, He K, Narla RR, Kang HG, Ryu HU, Boyko EJ. Metabolic consequences of obstructive sleep apnea especially pertaining to diabetes mellitus and insulin sensitivity. Diabetes Metab J. 2019;43(2):144–55. https://doi.org/10.4093/dmj.2018.0256.
Kim DH, Kim B, Han K, Kim SW. The relationship between metabolic syndrome and obstructive sleep apnea syndrome: a nationwide population-based study. Sci Rep. 2021;11(1):8751. https://doi.org/10.1038/s41598-021-88233-4.
Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N, et al. Obstructive sleep apnea and cardiovascular disease: a scientific statement From the American Heart Association. Circulation. 2021;144(3):e56–67. https://doi.org/10.1161/cir.0000000000000988.
Patel AR, Patel AR, Singh S, Singh S, Khawaja I. The association of obstructive sleep apnea and hypertension. Cureus. 2019;11(6):e4858. https://doi.org/10.7759/cureus.4858.
Zou D, Grote L, Basoglu OK, Verbraecken J, Schiza S, Sliwinski P, et al. Arterial bicarbonate is associated with hypoxic burden and uncontrolled hypertension in obstructive sleep apnea — the ESADA cohort. Sleep Med. 2023;102:39–45. https://doi.org/10.1016/j.sleep.2022.11.041.
Liu L, Cao Q, Guo Z, Dai Q. Continuous positive airway pressure in patients with obstructive sleep apnea and resistant hypertension: a meta-analysis of randomized controlled trials. J Clin Hypertens (Greenwich). 2016;18(2):153–8. https://doi.org/10.1111/jch.12639.
Ou YH, Tan A, Lee CH. Management of hypertension in obstructive sleep apnea. Am J Prev Cardiol. 2023;13:100475. https://doi.org/10.1016/j.ajpc.2023.100475.
Li YE, Ren J. Association between obstructive sleep apnea and cardiovascular diseases. Acta Biochim Biophys Sin (Shanghai). 2022;54(7):882–92. https://doi.org/10.3724/abbs.2022084.
• Svedmyr S, Hedner J, Bonsignore MR, Lombardi C, Parati G, Ludka O, et al. Hypertension treatment in patients with sleep apnea from the European Sleep Apnea Database (ESADA) cohort — towards precision medicine. J Sleep Res. 2023;32(4):e13811. https://doi.org/10.1111/jsr.13811. The study suggests that specific clinical characteristics and the type of antihypertensive medication influence the degree of blood pressure control in hypertensive OSA patients.
•• Sanchez-de-la-Torre M, Gracia-Lavedan E, Benitez ID, Zapater A, Torres G, Sanchez-de-la-Torre A, et al. Long-term effect of obstructive sleep apnea and continuous positive airway pressure treatment on blood pressure in patients with acute coronary syndrome: a clinical trial. Ann Am Thorac Soc. 2022;19(10):1750–9. https://doi.org/10.1513/AnnalsATS.202203-260OC. In patients with ACS, severe OSA is associated with a long-term increase in blood pressure. However, this increase can be reduced by good adherence to CPAP treatment.
Bandi PS, Panigrahy PK, Hajeebu S, Ngembus NJ, Heindl SE. Pathophysiological mechanisms to review association of atrial fibrillation in heart failure with obstructive sleep apnea. Cureus. 2021;13(7):e16086. https://doi.org/10.7759/cureus.16086.
• Polecka A, Olszewska N, Danielski Ł, Olszewska E. Association between obstructive sleep apnea and heart failure in adults—a systematic review. J Clin Med. 2023;12(19) https://doi.org/10.3390/jcm12196139. It explores the prevalence of OSA in heart failure patients, the role of positive airway pressure in these patients, and the impact of new medications in heart failure pharmacotherapy on sleep-disordered breathing patients.
Varghese MJ, Sharma G, Shukla G, Seth S, Mishra S, Gupta A, et al. Longitudinal ventricular systolic dysfunction in patients with very severe obstructive sleep apnea: a case control study using speckle tracking imaging. Indian Heart J. 2017;69(3):305–10. https://doi.org/10.1016/j.ihj.2016.12.011.
Chen L, Zadi ZH, Zhang J, Scharf SM, Pae EK. Intermittent hypoxia in utero damages postnatal growth and cardiovascular function in rats. J Appl Physiol (1985). 2018;124(4):821–30. https://doi.org/10.1152/japplphysiol.01066.2016.
Holt A, Bjerre J, Zareini B, Koch H, Tønnesen P, Gislason GH, et al. Sleep Apnea, the risk of developing heart failure, and potential benefits of continuous positive airway pressure (CPAP) Therapy. J Am Heart Assoc. 2018;7(13) https://doi.org/10.1161/jaha.118.008684.
Zhang D, Ma Y, Xu J, Yi F. Association between obstructive sleep apnea (OSA) and atrial fibrillation (AF): a dose-response meta-analysis. Medicine (Baltimore). 2022;101(30):e29443. https://doi.org/10.1097/md.0000000000029443.
Saleeb-Mousa J, Nathanael D, Coney AM, Kalla M, Brain KL, Holmes AP. Mechanisms of atrial fibrillation in obstructive sleep apnoea. Cells. 2023;12(12) https://doi.org/10.3390/cells12121661.
Moula AI, Parrini I, Tetta C, Luca F, Parise G, Rao CM, et al. Obstructive sleep apnea and atrial fibrillation. J Clin Med. 2022;11(5) https://doi.org/10.3390/jcm11051242.
• Li X, Zhou X, Xu X, Dai J, Chen C, Ma L, et al. Effects of continuous positive airway pressure treatment in obstructive sleep apnea patients with atrial fibrillation: a meta-analysis. Medicine (Baltimore). 2021;100(15):e25438. https://doi.org/10.1097/MD.0000000000025438. It demonstrates that the recurrence of AF in OSA patients who were treated with CPAP was lower than in those who did not receive CPAP treatment.
Hunt TE, Traaen GM, Aakeroy L, Bendz C, Overland B, Akre H, et al. Effect of continuous positive airway pressure therapy on recurrence of atrial fibrillation after pulmonary vein isolation in patients with obstructive sleep apnea: a randomized controlled trial. Heart Rhythm. 2022;19(9):1433–41. https://doi.org/10.1016/j.hrthm.2022.06.016.
Kosacka M, Brzecka A. Endothelin-1 and LOX-1 as markers of endothelial dysfunction in obstructive sleep apnea patients. Int J Environ Res Public Health. 2021;18(3) https://doi.org/10.3390/ijerph18031319.
O’Donnell C, O’Mahony AM, McNicholas WT, Ryan S. Cardiovascular manifestations in obstructive sleep apnea: current evidence and potential mechanisms. Pol. Arch Intern Med. 2021;131(6):550–60. https://doi.org/10.20452/pamw.16041.
• Peker Y, Akdeniz B, Altay S, Balcan B, Başaran Ö, Baysal E, et al. Obstructive sleep apnea and cardiovascular disease: where do we stand? Anatol J Cardiol. 2023;27(7):375–89. https://doi.org/10.14744/AnatolJCardiol.2023.3307. A a comprehensive review of the current understanding of the relationship between OSA and CVD, discussing the underlying mechanisms, clinical implications, and potential treatment strategies.
•• Wang G, Miao H, Hao W, Zhao G, Yan Y, Gong W, et al. Association of obstructive sleep apnoea with long-term cardiovascular events in patients with acute coronary syndrome with or without hypertension: insight from the OSA-ACS project. BMJ Open Respir Res. 2023;10(1) https://doi.org/10.1136/bmjresp-2023-001662. OSA was associated with an increased risk of major adverse cardiovascular and cerebrovascular events in patients with ACS and hypertension, particularly in those with pre-existing severe hypertension.
Peker Y, Glantz H, Eulenburg C, Wegscheider K, Herlitz J, Thunström E. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The RICCADSA Randomized Controlled Trial. Am J Respir Crit Care Med. 2016;194(5):613–20. https://doi.org/10.1164/rccm.201601-0088OC.
Chetan IM, Maierean AD, Domokos Gergely B, Cabau G, Tomoaia R, Chis AF, et al. A prospective study of CPAP therapy in relation to cardiovascular outcome in a cohort of romanian obstructive sleep apnea patients. J Pers Med. 2021;11(10) https://doi.org/10.3390/jpm11101001.
Navarro-Soriano C, Martinez-Garcia MA, Torres G, Barbe F, Sanchez-de-la-Torre M, Caballero-Eraso C, et al. Long-term effect of CPAP treatment on cardiovascular events in patients with resistant hypertension and sleep apnea. Data from the HIPARCO-2 Study. Arch Bronconeumol (Engl Ed). 2021;57(3):165–71. https://doi.org/10.1016/j.arbres.2019.12.006.
Wang X, Zhang Y, Dong Z, Fan J, Nie S, Wei Y. Effect of continuous positive airway pressure on long-term cardiovascular outcomes in patients with coronary artery disease and obstructive sleep apnea: a systematic review and meta-analysis. Respir Res. 2018;19(1):61. https://doi.org/10.1186/s12931-018-0761-8.
• Redline S, Azarbarzin A, Peker Y. Obstructive sleep apnoea heterogeneity and cardiovascular disease. Nat Rev Cardiol. 2023;20(8):560–73. https://doi.org/10.1038/s41569-023-00846-6. A comprehensive review that emphasizes the heterogeneity of OSA, discussing the varied mechanistic pathways that result in CVD across different subgroups of OSA, and highlights the potential role of new biomarkers for CVD risk stratification.
Bahammam AS, Pandi-Perumal SR, Spence DW, Moscovitch A, Streiner DL. The SAVE trial: has the importance of CPAP for preventing cardiovascular events been discounted? Sleep Vigil. 2017;1(1):47–8. https://doi.org/10.1007/s41782-017-0003-z.
• Pirzada AR, AS BH. Rapid eye movement predominant obstructive sleep apnoea: prognostic relevance and clinical approach. Curr Opin Pulm Med. 2021;27(6):514–22. https://doi.org/10.1097/MCP.0000000000000817. It highlights that REM-OSA is independently associated with cardiometabolic complications, particularly hypertension, metabolic complications such as insulin resistance, and metabolic syndrome. However, there is currently no consensus on the accepted diagnostic criteria for REM-OSA.
BaHammam AS, Alshahrani M, Aleissi SA, Olaish AH, Alhassoon MH, Shukr A. Blood pressure dipping during REM and non-REM sleep in patients with moderate to severe obstructive sleep apnea. Sci Rep. 2021;11(1):7990. https://doi.org/10.1038/s41598-021-87200-3.
Drager LF, McEvoy RD, Barbe F, Lorenzi-Filho G, Redline S, Initiative I. Sleep apnea and cardiovascular disease: lessons from recent trials and need for team science. Circulation. 2017;136(19):1840–50. https://doi.org/10.1161/CIRCULATIONAHA.117.029400.
Cardoso CRL, Salles GF. Prognostic importance of obstructive sleep apnea and CPAP treatment for cardiovascular and mortality outcomes in patients with resistant hypertension: a prospective cohort study. Hypertens Res. 2023;46(4):1020–30. https://doi.org/10.1038/s41440-023-01193-2.
Manuel Sanchez De La T, Esther G-L, Ivan DB, Alicia S-D-L-T, Anna M-M, Gerard T, et al. Adherence to CPAP treatment is associated with a decrease in the incidence of cardiovascular events: an individual participant data meta-analysis. European Respiratory Journal. 2023;62(suppl 67):OA3292. https://doi.org/10.1183/13993003.congress-2023.OA3292.
• Sharafkhaneh A, Agrawal R, Nambi V, BaHammam A, Razjouyan J. Obesity paradox or hypoxia preconditioning: how obstructive sleep apnea modifies the obesity-MI relationship. Sleep Med. 2023;110:132–6. https://doi.org/10.1016/j.sleep.2023.07.035. It suggests that the association between obesity and improved survival in acute MI is largely driven by the presence of OSA.
Agrawal R, Sharafkhaneh A, Nambi V, BaHammam A, Razjouyan J. Obstructive sleep apnea modulates clinical outcomes post-acute myocardial infarction: a large longitudinal veterans’ dataset report. Respir Med. 2023;211:107214. https://doi.org/10.1016/j.rmed.2023.107214.
Kalmbach DA, Anderson JR, Drake CL. The impact of stress on sleep: pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res. 2018;27(6):e12710. https://doi.org/10.1111/jsr.12710.
Jarrin DC, Alvaro PK, Bouchard MA, Jarrin SD, Drake CL, Morin CM. Insomnia and hypertension: a systematic review. Sleep Med Rev. 2018;41:3–38. https://doi.org/10.1016/j.smrv.2018.02.003.
Patel D, Steinberg J, Patel P. Insomnia in the elderly: a review. J Clin Sleep Med. 2018;14(6):1017–24. https://doi.org/10.5664/jcsm.7172.
Chapman JL, Comas M, Hoyos CM, Bartlett DJ, Grunstein RR, Gordon CJ. Is metabolic rate increased in insomnia disorder? A systematic review. Front Endocrinol (Lausanne). 2018;9:374. https://doi.org/10.3389/fendo.2018.00374.
Javaheri S, Redline S. Insomnia and risk of cardiovascular disease. Chest. 2017;152(2):435–44. https://doi.org/10.1016/j.chest.2017.01.026.
Jansen PR, Watanabe K, Stringer S, Skene N, Bryois J, Hammerschlag AR, et al. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nat Genet. 2019;51(3):394–403. https://doi.org/10.1038/s41588-018-0333-3.
Liao LZ, Li WD, Liu Y, Li JP, Zhuang XD, Liao XX. Causal assessment of sleep on coronary heart disease. Sleep Med. 2020;67:232–6. https://doi.org/10.1016/j.sleep.2019.08.014.
Gaffey AE, Rosman L, Lampert R, Yaggi HK, Haskell SG, Brandt CA, et al. Insomnia and early incident atrial fibrillation: a 16-year cohort study of younger men and women veterans. J Am Heart Assoc. 2023;12(20):e030331. https://doi.org/10.1161/jaha.123.030331.
Thomas SJ, Calhoun D. Sleep, insomnia, and hypertension: current findings and future directions. J Am Soc Hypertens. 2017;11(2):122–9. https://doi.org/10.1016/j.jash.2016.11.008.
Shivashankar R, Kondal D, Ali MK, Gupta R, Pradeepa R, Mohan V, et al. Associations of sleep duration and disturbances with hypertension in metropolitan cities of Delhi, Chennai, and Karachi in South Asia: cross-sectional analysis of the CARRS study. Sleep. 2017;40(9) https://doi.org/10.1093/sleep/zsx119.
Wang YM, Song M, Wang R, Shi L, He J, Fan TT, et al. Insomnia and multimorbidity in the community elderly in China. J Clin Sleep Med. 2017;13(4):591–7. https://doi.org/10.5664/jcsm.6550.
Clark AJ, Salo P, Lange T, Jennum P, Virtanen M, Pentti J, et al. Onset of impaired sleep and cardiovascular disease risk factors: a longitudinal study. Sleep. 2016;39(9):1709–18. https://doi.org/10.5665/sleep.6098.
Lin CL, Liu TC, Lin FH, Chung CH, Chien WC. Association between sleep disorders and hypertension in Taiwan: a nationwide population-based retrospective cohort study. J Hum Hypertens. 2017;31(3):220–4. https://doi.org/10.1038/jhh.2016.55.
• Grandner M, Olivieri A, Ahuja A, Busser A, Freidank M, McCall WV. The burden of untreated insomnia disorder in a sample of 1 million adults: a cohort study. BMC Public Health. 2023;23(1):1481. https://doi.org/10.1186/s12889-023-16329-9. The findings confirm the substantial burden of insomnia disorder on patients, with significant daytime impairment and numerous comorbidities, reinforcing the need for timely insomnia disorder diagnosis and treatments that improve both sleep and daytime functioning.
Meng L, Zheng Y, Hui R. The relationship of sleep duration and insomnia to risk of hypertension incidence: a meta-analysis of prospective cohort studies. Hypertens Res. 2013;36(11):985–95. https://doi.org/10.1038/hr.2013.70.
Li L, Gan Y, Zhou X, Jiang H, Zhao Y, Tian Q, et al. Insomnia and the risk of hypertension: a meta-analysis of prospective cohort studies. Sleep Med Rev. 2021;56:101403. https://doi.org/10.1016/j.smrv.2020.101403.
•• Ali E, Shaikh A, Yasmin F, Sughra F, Sheikh A, Owais R, et al. Incidence of adverse cardiovascular events in patients with insomnia: a systematic review and meta-analysis of real-world data. PLoS One. 2023;18(9):e0291859. https://doi.org/10.1371/journal.pone.0291859. It reveals that individuals with insomnia have a higher risk of long-term mortality, myocardial infarction, and incidence of cardiovascular disease.
Kalmbach DA, Pillai V, Arnedt JT, Drake CL. DSM-5 insomnia and short sleep: comorbidity landscape and racial disparities. Sleep. 2016;39(12):2101–11. https://doi.org/10.5665/sleep.6306.
Anothaisintawee T, Reutrakul S, Van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for diabetes development: systematic review and meta-analysis. Sleep Med Rev. 2016;30:11–24. https://doi.org/10.1016/j.smrv.2015.10.002.
Cespedes EM, Dudley KA, Sotres-Alvarez D, Zee PC, Daviglus ML, Shah NA, et al. Joint associations of insomnia and sleep duration with prevalent diabetes: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). J Diabetes. 2016;8(3):387–97. https://doi.org/10.1111/1753-0407.12308.
Zhang Y, Jiang X, Liu J, Lang Y, Liu Y. The association between insomnia and the risk of metabolic syndrome: a systematic review and meta-analysis. J Clin Neurosci. 2021;89:430–6. https://doi.org/10.1016/j.jocn.2021.05.039.
Liu X, Li C, Sun X, Yu Y, Si S, Hou L, et al. Genetically predicted insomnia in relation to 14 cardiovascular conditions and 17 cardiometabolic risk factors: a Mendelian randomization study. J Am Heart Assoc. 2021;10(15):e020187. https://doi.org/10.1161/jaha.120.020187.
•• Laaboub N, Dubath C, Ranjbar S, Sibailly G, Grosu C, Piras M, et al. Insomnia disorders are associated with increased cardiometabolic disturbances and death risks from cardiovascular diseases in psychiatric patients treated with weight-gain-inducing psychotropic drugs: results from a Swiss cohort. BMC Psychiatry. 2022;22(1):342. https://doi.org/10.1186/s12888-022-03983-3. Insomnia disorders are significantly associated with metabolic worsening and an increased risk of death from cardiovascular diseases in psychiatric patients treated with weight-gain-inducing psychotropic drugs.
•• Brostrom A, Alimoradi Z, Lind J, Ulander M, Lundin F, Pakpour A. Worldwide estimation of restless legs syndrome: a systematic review and meta-analysis of prevalence in the general adult population. J Sleep Res. 2023;32(3):e13783. https://doi.org/10.1111/jsr.13783. A comprehensive worldwide assessment of the prevalence of restless legs syndrome (RLS) in the general adult population, finding a corrected overall pooled prevalence of 3%.
Tang M, Sun Q, Zhang Y, Li H, Wang D, Wang Y, et al. Circadian rhythm in restless legs syndrome. Front Neurol. 2023;14:1105463. https://doi.org/10.3389/fneur.2023.1105463.
Trenkwalder C, Allen R, Högl B, Paulus W, Winkelmann J. Restless legs syndrome associated with major diseases: a systematic review and new concept. Neurology. 2016;86(14):1336–43. https://doi.org/10.1212/wnl.0000000000002542.
De Berardis D, Ricci V, Mazza M, Ullah I, Amerio A, Martinotti G. Commentary: increased risk of cardiovascular disease in restless legs syndrome patients: a call to action. Alpha Psychiatry. 2023;24(3):100–1. https://doi.org/10.5152/alphapsychiatry.2023.160523.
Abuş S, Kapıcı Y, Ayhan S, Arık A. Elevated cardiovascular disease risk in patients with restless legs syndrome. Alpha Psychiatry. 2023;24(3):95–9. https://doi.org/10.5152/alphapsychiatry.2023.221043.
Katsanos AH, Kosmidou M, Konitsiotis S, Tsivgoulis G, Fiolaki A, Kyritsis AP, et al. Restless legs syndrome and cerebrovascular/cardiovascular events: systematic review and meta-analysis. Acta Neurol Scand. 2018;137(1):142–8. https://doi.org/10.1111/ane.12848.
Bellei E, Bergamini S, Monari E, Tomasi A, Koseoglu M, Topaloglu Tuac S, et al. Evaluation of potential cardiovascular risk protein biomarkers in high severity restless legs syndrome. J Neural Transm (Vienna). 2019;126(10):1313–20. https://doi.org/10.1007/s00702-019-02051-7.
Bertisch SM, Muresan C, Schoerning L, Winkelman JW, Taylor JA. Impact of restless legs syndrome on cardiovascular autonomic control. Sleep. 2016;39(3):565–71. https://doi.org/10.5665/sleep.5528.
Li Y, Li Y, Winkelman JW, Walters AS, Han J, Hu FB, et al. Prospective study of restless legs syndrome and total and cardiovascular mortality among women. Neurology. 2018;90(2):e135–e41. https://doi.org/10.1212/wnl.0000000000004814.
Winkelman JW, Blackwell T, Stone K, Ancoli-Israel S, Redline S. Associations of incident cardiovascular events with restless legs syndrome and periodic leg movements of sleep in older men, for the outcomes of sleep disorders in older men study (MrOS Sleep Study). Sleep. 2017;40(4) https://doi.org/10.1093/sleep/zsx023.
Kendzerska T, Kamra M, Murray BJ, Boulos MI. Incident cardiovascular events and death in individuals with restless legs syndrome or periodic limb movements in sleep: a systematic review. Sleep. 2017;40(3) https://doi.org/10.1093/sleep/zsx013.
Doan TT, Koo BB, Ogilvie RP, Redline S, Lutsey PL. Restless legs syndrome and periodic limb movements during sleep in the Multi-Ethnic Study of Atherosclerosis. Sleep. 2018;41(8) https://doi.org/10.1093/sleep/zsy106.
•• Srivali N, Thongprayoon C, Tangpanithandee S, Krisanapan P, Mao MA, Zinchuk A, et al. Periodic limb movements during sleep and risk of hypertension: a systematic review. Sleep Med. 2023;102:173–9. https://doi.org/10.1016/j.sleep.2023.01.008. The pooled risk ratio of hypertension in patients with PLMS was 1.26, indicating an increased risk of hypertension among patients with PLMS.
• Gao X, Ba DM, Bagai K, Liu G, Ma C, Walters AS. Treating restless legs syndrome was associated with low risk of cardiovascular disease: a cohort study with 3.4 years of follow-up. J Am Heart Assoc. 2021;10(4):e018674. https://doi.org/10.1161/jaha.120.018674. RLS was associated with a higher future CVD risk, RLS patients who received treatment had a statistically significantly lower future cardiovascular risk than those without treatment.
Funding
Support was provided by The Strategic Technologies Program of the National Plan for Sciences and Technology and Innovation in the Kingdom of Saudi Arabia (MED511-02-08).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Shaden O. Qasrawi and Ahmed S. BaHammam declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qasrawi, S.O., BaHammam, A.S. Role of Sleep and Sleep Disorders in Cardiometabolic Risk: a Review and Update. Curr Sleep Medicine Rep 10, 34–50 (2024). https://doi.org/10.1007/s40675-024-00276-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-024-00276-x