Abstract
Restless legs syndrome (RLS) is a common sensorimotor disorder that, in case of severe symptoms, can be very distressing and negatively interfere with quality of life. Moreover, increasing evidences associate RLS with higher risk of cerebrovascular and cardiovascular disease (CVD). The purpose of this study was to quantify two proteins, previously identified by proteomics and potentially linked with CVD risk, namely kininogen-1 (KNG1) and alpha-1-antitrypsin (A1AT), in primary RLS patients at high severity grade (HS-RLS) in comparison to healthy control subjects. Proteins were quantified through enzyme-linked immunosorbent assay (ELISA) in plasma samples from 14 HS-RLS patients and 15 control individuals. The two groups were closely matched for age and gender. The expression level of KNG1 resulted significantly higher (p < 0.001), while A1AT was significantly decreased (p < 0.05) in HS-RLS patients compared to controls, confirming the relationship between these proteins and the disease severity. Furthermore, in patients group the association between the protein concentrations and the following parameters was further evaluated: age, disease onset and diagnosis, scores obtained from the RLS rating scales (Epworth Sleepiness Scale, Pittsburgh Sleep Quality Index, Beck Depression Inventory) and smoking habit. All the considered variables resulted independent of protein levels, so the disease can be reasonably considered the main cause of protein changes. As emerged from the literature, high levels of KNG1 and low amounts of A1AT seem to be related with a highest probability to develop CVD. Consequently, these proteins may be reliable candidate biomarkers of CVD risk in patients with RLS at high severity grade.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restless legs syndrome (RLS), also known as Willis-Ekbom disease (WED), is a neurological disorder that causes an uncontrollable necessity to move the legs, and occasionally the arms, usually accompanied by unpleasant and uncomfortable sensations without any apparent sensory stimulation. Generally, it begins during periods of rest or inactivity, often worse in the evening or night and can be partially or totally relieved by movement (Benes et al. 2007). Moreover, affected patients may also suffer from serious sleep disturbances, such as insomnia (Bogan 2006), with consequent negative effects on daily activities and productivity, impaired memory and cognitive functioning, depressive and anxious symptoms, resulting in reduced quality of life (Sevim et al. 2004).
RLS was once thought to be a rare disorder, but nowadays it is considered a common condition, with substantial clinical variability (Picchietti et al. 2017). Its phenotypes include an early onset form, usually idiopathic and with a familial history, and a late onset type, frequently secondary to other somatic conditions considered typical causative factors, such as iron-deficiency anemia (Allen et al. 2013), pregnancy, uremia, peripheral polyneuropathy and chronic renal failure (Guo et al. 2017). In addition, a positive association with cardiovascular disease (CVD), including coronary heart disease and stroke, has also been found (Gottlieb et al. 2017; Winkelman et al. 2017). Nevertheless, to date the pathophysiology of primary RLS is only partially understood; genetic mechanisms, alterations of iron homeostasis and dopaminergic neurotransmission dysfunctions are the most accepted involved pathways (Guo et al. 2017).
To extend the knowledge of RLS condition, we performed a previous mass spectrometry-based proteomic study on plasma samples from RLS patients in comparison to healthy control subjects, in the search of diagnostic biomarkers associated with the disease severity (Bellei et al. 2018). We detected several differentially expressed proteins in RLS, mainly linked to inflammatory and immune response. Notably, two proteins identified as kininogen-1 (KNG1) and alpha-1-antitrypsin (A1AT), seem to be associated with cardiovascular disorders. The role of KNG1 gene in vascular disease has been broadly explored, providing interesting results. To date, 17 genes including KNG1 have strongly demonstrated to have genetic variations associated with venous thrombosis, the pathologic expression of a blood clot formation (i.e., thrombus) which can further obstruct venous circulation or embolize (Morange et al. 2015). In addition, researches conducted in animal models show that KNG1 inhibition could prevents ischemic neurodegeneration and CVD (such as myocardial infarction) by combined antithrombotic and anti-inflammatory mechanisms (Langhauser et al. 2012). Regarding A1AT, a recent study pointed the attention on a possible causal link between genetic A1AT deficiency and increased cardiovascular risk (Curjuric et al. 2018). Deficiency of A1AT may results in the arterial wall degradation through inadequate protection against the proteolytic effect of elastase and collagenase, as observed in spontaneous cervical artery dissection (Vila et al. 2003). Since it has become increasingly evident a close relationship between RLS and CVD (Katsi et al. 2014; Fang et al. 2015; Li et al. 2018; Varim et al. 2019), although sometimes questionable and nebulous (Budhiraja 2013), the aim of the present work was to deepen the study of these proteins, first by their quantification through enzyme-linked immunosorbent assay (ELISA test). Moreover, it was evaluated the correlation between the protein levels and the patients age, the time of RLS onset and diagnosis, the scores obtained from the RLS rating scales and the cigarette smoking habit.
Materials and methods
Patients and controls recruitment
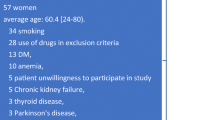
RLS patients, afferent to the sleep disorders outpatient clinic at the Neurology Department of Bakirkoy Psychiatry and Neurology Research and Training Hospital Sleep Disorders Center (Istanbul, Turkey), were enrolled in the study between May 2016 and December 2016. During this period, most of the screened subjects (about 90%) were excluded due to the presence of one or more of the following exclusion criteria: (1) chronic systemic diseases, such as diabetes mellitus, malignancies, chronic renal failure and uremia (2) neurologic diseases, comprising CVD and cerebrovascular disease, multiple sclerosis, Parkinson’s disease, inflammatory rheumatologic disease and polyneuropathy (excluded through anamnesis and neurologic examination) (3) other diagnosed sleep disorders detected by anamnesis or laboratory test (insomnia, central disorders of hypersomnolence, sleep-related breathing disorders, circadian rhythm sleep–wake disorders, parasomnias) and snoring or nocturnal witnessed apneas reported by the individuals or their partners (4) anemia, iron deficiency, low ferritin levels (< 45 ng/mL) (5) pregnancy (6) obesity (7) use of antidepressants, antipsychotics and mood stabilizers (8) excessive alcohol intake (considered as > 14 drinks/week for men and > 7 drinks/week for women). Smoking habit was considered in both groups (Table 1). Ultimately, 34 patients with primary RLS (face-to-face interviewed), diagnosed according to the International Classification of Sleep Disorders diagnostic criteria (American Academy of Sleep Medicine 2014; Sateia 2014), were selected for a previous proteomic study (Bellei et al. 2018). In this work, the patients were divided in two subgroups based on disease severity, evaluated according to the 10-item International Restless Legs Syndrome Study Group (IRLSSG) rating scale (by physician-administered questionnaire) (Allen et al. 2014): mild-moderate severity degree group (n = 17) and high severity group (n = 17). The control group (n = 17) was composed of healthy individuals from the medical staff, closely matched for age and gender with RLS patients. The analysis revealed a significantly different expression of KNG1 and A1AT proteins only in patients with high severity degree compared to controls. For this reason, in the present work were considered only those patients with severe and very severe score grades (IRLS scores 21–30 and IRLS scores 31–40, respectively), as previously clustered in a unique group named HS-RLS, in comparison to the same controls of the earlier study. In the current work, due to unavailability of the complete set of previous plasma samples, the analyses were performed on 29 samples, which comprised of 14 HS-RLS patients and 15 healthy control subjects.
It is important to point out that RLS is a complex disorder, in which genetic and environmental interactions contribute to its phenotype; moreover, the cumulative effect of comorbidities was prospected as a strong risk factor for RLS (Trenkwalder et al. 2016; Szentkiralyi et al. 2014). Based on the above, patients with primary RLS without the major disease-related comorbidities could be considered a poorly representative sample, but this is essential to avoid interference in the results due to the presence of other diseases. The study was performed in conformity with the Helsinki Declaration and with the informed consent of each enrolled subject, after the approval of the local Ethical Committee.
RLS data and rating scales
For each RLS patient were considered the following information: the severity degree based on the IRLSSG rating scale, the RLS duration, namely the onset time of early symptoms and the time of disease diagnosis. Furthermore, were applied the following rating scales: the Epworth Sleepiness Scale (ESS) (Izci et al. 2008), the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al. 1989) and the Beck Depression Inventory (Beck et al. 1988), to respectively, evaluate the daytime sleepiness, the sleep quality and the level of depression.
ELISA test
Venous blood was collected into EDTA tubes from patients and controls after 12–14 h fast. Plasma samples, obtained by centrifugation, were aliquoted and immediately stored at − 80 °C until analysis. Specifically, the expression level of the following proteins was evaluated: KNG1 (human kininogen-1 ELISA kit, Cusabio Biotech, TX, USA) and A1AT (human α1-antitrypsin ELISA kit, Cusabio Biotech, TX, USA). Both kits applied the quantitative sandwich enzyme immunoassay technique and were carried out according to the manufacturer’s instructions. Briefly, diluted plasma samples, calibrants, and quality controls were dispensed into the microplate wells, containing immobilized pre-coated specific antibody for KNG1 or A1AT. Then, a solution containing horseradish peroxidase (HRP)—conjugated antibody was added to each well and allowed to react with a substrate solution, to develop a blue color in proportion to the amount of sample protein. An acid stop solution leaded to yellow product; the absorbance was measured at λ 450 nm in a microplate reader (Multiscan FC, Thermo Scientific, USA). KNG1 and A1AT concentrations were calculated by calibration curves, generated by the respective protein standards supplied with the kits.
Statistical analysis
Statistical analysis was performed using IBM SPSS v23 software (Chicago, IL, USA). Normal distribution of the variables KNG1 and A1AT were determined using Shapiro–Wilk test. The Student’s t test was used for comparisons of the variables normally distributed between the groups, while the Chi-square test (χ2) was used for categorical variables. Quantitative data were expressed as mean ± standard deviation (SD) in normally distributed variables, while categorical data were reported as frequency and percentage. Spearman’s rho test was used to analyze the correlation between KNG1 and A1AT levels and age, RLS onset, RLS diagnosis, ESS, PSQI and Beck depression scores in RLS group. For all analysis, a p value lower than 0.05 was considered as statistically significant.
Results
Patients and controls data
In Table 1 are reported the demographic data and smoking habits of HS-RLS patients in comparison to controls. The two groups resulted closely matched for age and gender. Moreover, no significant difference was found regarding cigarette smoking habit between patients and controls (p > 0.05). All RLS patients, as well as controls, reported iron parameters (hemoglobin, serum iron, ferritin), mean cell volume and hematocrit in the normal reference range. Subjects with anaemia and iron deficiency were excluded from the study. The HS-RLS group was composed of patients with severe (64%) and very severe score degree (36%), according to IRLS scores (IRLSSG rating scale) (Fig. 1a). For most patients (64%), the onset time of early symptoms was > 5 years (Fig. 1b), as well as the time of disease diagnosis (> 5 years for 43% and 1–5 years for 36% of patients, respectively) (Fig. 1c). In Fig. 2 are illustrated the scores obtained from the RLS rating scales, expressed in percentage. According to the Epworth Sleepiness Scale (ESS), only 29% of RLS patients reported excessive daytime sleepiness (Fig. 2a), while, by PSQI, the great majority of patients (86%) showed poor sleep quality (Fig. 2b). Nonetheless, only one has declared to use sleep medications. Finally, the depression level, evaluated by the Beck Depression Inventory Scale, was assessed as normal for most patients (Fig. 2c).
Protein quantification by ELISA test
The expression levels of KNG1 and A1AT were evaluated in plasma samples by ELISA test. As shown in Fig. 3, plasma concentration of KNG1 was significantly higher (p = 0.0067) in HS-RLS patients (mean ± SD, 454.4 ± 126.9 μg/mL; range 230.0–676.1 μg/mL) compared to control subjects (221.8 ± 127.2 μg/mL; range 50.2–442.5 μg/mL). Conversely, the amount of A1AT was found significantly decreased (p = 0.0394) in HS-RLS group (693.2 ± 375.1 nIU/μL; range 124.6–1180 nIU/μL) in respect to controls (1132.0 ± 675.5 nIU/μL; range 414.6–2100 nIU/μL), as illustrated in Fig. 4. These results agree with our previous data obtained by proteomic analysis (Bellei et al. 2018). No significant correlation was found by Spearman’s rho test among the proteins levels and age, RLS onset, RLS diagnosis, ESS scores, PSQI total score and Beck Depression scores in RLS patients (Table 2). Moreover, no significant differences were found between smokers and non-smokers patients and KNG1 concentrations (439.6 ± 133.6 μg/mL and 474.1 ± 126.5 μg/mL, respectively, p = 0.634) and A1AT concentrations (723.0 ± 397.2 nIU/μL and 653.5 ± 375.9 nIU/μL, respectively, p = 0.746).
Discussion
The relationship between RLS and the increased risk for CVD has been discussed in many previous researches. Some studies reported a strong positive association between RLS and CVD, including coronary heart disease (Li et al. 2012), stroke (Walters and Rye 2009; Koo et al. 2018), and cerebrovascular disease (Ferini-Strambi et al. 2014), or with CVD risk factors (Szentkiralyi et al. 2013), such as hypertension (Hwang et al. 2018). In contrast, other analysis did not provide evidence for increased cardiovascular outcomes in RLS (Winter et al. 2012; Katsanos et al. 2018). This variability may be due to the heterogeneity of the studies, that is different subject recruitment, patient population, RLS severity and duration, sample size/resources and research methodology, or to casual interferences or key potential confounders, such as age, sex, other sleep disorders and adverse lifestyle factors, e.g., smoking and obesity (Innes et al. 2012). In the present study we applied restrictive exclusion criteria during the recruitment of patients with primary RLS and controls (as fully reported in Methods section). Moreover, the two groups were strictly matched for age, gender and smoke habits (Table 1).
Based on our previous findings (Bellei et al. 2018), KNG1 and A1AT proteins were here further investigated, in the search of a potential relation with CVD risk. KNG1 is the precursor protein for the nonenzymatic cofactor high-molecular weight kininogen, which is part of the plasma kallikrein–kinin system, a mediator of coagulation and inflammation since it presents proinflammatory, prothrombotic, and vasoactive properties (Wu 2015). Protein quantification by ELISA test confirmed the over-expression of KNG1 in plasma of patients with severe/very severe RLS compared to controls (Fig. 3). Recently it has been demonstrated a high KNG1 level in patients with in-stent restenosis after angioplasty, suggesting a possible increased basal activity of kinins, a signal of proinflammatory and atherogenic state (Ribeiro et al. 2014). Another study proposed KNG1 as candidate gene for internal elastic lamina lesions, the early events causing atherosclerosis (Stoll et al. 2001). Moreover, a Chinese population study presented, for the first time, novel evidence for the central effect of KNG1 gene on ischemic stroke (IS) susceptibility, revealing its crucial role in vascular disease. Variants in this gene potentiate the risk of IS via a genetic main effect and interactions with other atherogenic genes, including ALOX5AP, which is involved in the oxidative stress system (Hu et al. 2015). In this regard, some studies evaluated the atherosclerosis risk in RLS patients by the assessment of the oxidative stress status. Baskol et al. (2012) found increased advanced oxidation protein products and malondialdehyde levels, together with decreased total thiol and nitric oxide amounts, suggesting that RLS patients are under oxidative stress. Both lipid peroxidation and protein oxidation may have a role in the atherosclerosis onset and progression, so RLS patients could be more exposed to the risk of developing atherosclerosis. It is important to point out that our RLS patients were not sequenced for KNG1 or other genes, as well as for allelic variations or polymorphisms. This may be a significant starting point for a next phase of the work, focused on genetics analysis.
The other protein that we investigated in this work was A1AT, found significantly decreased in HS-RLS patients vs controls (Bellei et al. 2018); for this glycoprotein also, ELISA quantification confirmed the earlier result (Fig. 4). A1AT is the most abundant circulating serine proteinase inhibitor in human blood, exerting anti-inflammatory and immuno-modulatory effects. Another important function is the inhibition of the proteolytic enzyme neutrophil elastase, that increase in case of inflammation, infections, smoking and inhaled fumes, helping to maintain the integrity of connective tissues, elastic fibers and collagen filaments (Beiko et al. 2018). In a recent study, Feng et al. (2015) reported the cytoprotective role of A1AT in vascular endothelial cell under hypoxia/reoxygenation condition, providing evidences that A1AT protects the endothelium by suppressing oxidative stress and apoptosis. In our present study, the expression level of A1AT was significantly lower (p < 0.05) in HS-RLS group compared to healthy subjects (Fig. 4), suggesting a greater risk of CVD in RLS at high severity. This is in strict accordance with Winkelman et al. (2008), who found a stronger association between RLS and CVD in patients with severe symptoms than those with moderate gravity. A recent study conducted in RLS patients showed compromised cardiovagal control and greater peripheral vascular resistance, potentially due to heightened sympathetic outflow; these autonomic alterations may be one mechanism to explain the higher prevalence of CVD in RLS (Bertisch et al. 2016).
It is important to emphasize that our study was based on homogeneous parameters, both between the two different groups (such as age, gender, smoking) and within the RLS group (all patients were diagnosed as primary RLS and all presented a high degree of disease severity). This means that the outcomes have not been conditioned by those confounding factors that often influence the data, such as significant differences in age and gender among the enrolled subjects, or differences regarding various aspects of the considered pathology. Moreover, in the present study, no positive correlations were found between the plasma proteins levels and patients age, RLS onset, RLS diagnosis and all the considered rating scale scores (Table 2), as well as with smoking habit. Additionally, patients did not show any disease-related comorbidities, therefore, only the RLS itself can be considered the main cause for the differences observed in KNG1 and A1AT concentrations. However, another important consideration concerns the medications taken by RLS patients before blood samples collection: 7 patients were under treatment with pramipexole (0.25–0.75 mg/day) and seven patients were taking pregabalin (150–300 mg/day) and pramipexole combination regularly, changing the doses over time according to the severity of the symptoms. Moreover, recent studies have individuated a painful RLS phenotype (Cho et al. 2015; Karroum et al. 2015), but in this work patients were not categorized as painful and non-painful phenotypes. Medications could have an impact on proteomic analysis, so this matter should be investigated in future works, as well as to consider the presence or absence of a characteristic painful form of the disease as potential variables. Finally, it is well known that anxiety, depression, and sleep disturbances may be potential risk factors for CVD. In the current study, only 14% of HS-RLS patients showed serious depression symptoms, while 29% reported excessive daytime sleepiness and 86% a poor sleep quality (Fig. 2), which is an intrinsic feature of this sleep disorder.
Conclusions
To date, there are still conflicting opinions regarding the relationship between RLS and CVD. Starting from a proteomic study, by which we detected KNG1 and A1AT proteins as indicative targets of a greater RLS severity, here we confirmed the previous results. Furthermore, as described in the current literature and found in our plasma samples from HS-RLS group, the up-regulation of KNG1 and the decreased levels of A1AT could be strongly linked with cardiovascular disorders. Accordingly, patients with RLS at high severity grade may be prone toward a higher risk of developing CVD, and these proteins may be considered as predictive candidate biomarkers. However, it should be noted that additional patients are needed to expand the present results, together with genetic analysis. In conclusion, the present findings provide further considerations to elucidate the debate concerning CVD comorbidity in RLS, underlining the importance to accurately diagnose and treat this sleep disorder for CVD prevention and control.
References
Allen RP, Auerbach S, Bahrain H, Auerbach M, Earley CJ (2013) The prevalence and impact of restless legs syndrome on patients with iron deficiency anemia. Am J Hematol 88:261–264
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, Zucconi M, Ferri R, Trenkwalder C, Lee HB (2014) Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria—history, rationale, description, and significance. Sleep Med 15:860–873
American Academy of Sleep Medicine (2014) International classification of sleep disorders (ICSD3), 3rd edn. American Academy of Sleep Medicine, Darien
Baskol G, Korkmaz S, Erdem F, Caniklioglu A, Kocyigit M, Aksu M (2012) Assessment of nitric oxide, advanced oxidation protein products, malondialdehyde, and thiol levels in patients with restless legs syndrome. Sleep Med 13:414–418
Beck AT, Steer RA, Carbin MG (1988) Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 8(1):77–100
Beiko T, Ma S, Strange C, Turino GM (2018) Biomarker indicators of elastin degradation in asymptomatic alpha-1 antitrypsin deficiency. Pulm Crit Care Med 3(3):1–5
Bellei E, Monari E, Ozben S, Koseoglu Bitnel M, Topaloglu Tuac S, Tomasi A, Bergamini S (2018) Discovery of restless legs syndrome plasmatic biomarkers by proteomic analysis. Brain Behav 8(10):e01062. https://doi.org/10.1002/brb3.1062
Benes H, Walters AS, Allen RP, Hening WA, Kohnen R (2007) Definition of restless legs syndrome, how to diagnose it, and how to differentiate it from RLS mimics. Mov Disord 22:S401–S408
Bertisch SM, Muresan C, Schoerning L, Winkelman JW, Taylor JA (2016) Impact of restless legs syndrome on cardiovascular autonomic control. Sleep 39(3):565–571
Bogan RK (2006) Effects of restless legs syndrome (RLS) on sleep. Neuropsychiatr Dis Treat 2(4):513–519
Budhiraja R (2013) Is restless legs syndrome associated with cardiovascular disease? Am J Med 126(3):189–190
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Cho YW, Song ML, Earley CJ, Allen RP (2015) Prevalence and clinical characteristics of patients with restless legs syndrome with painful symptoms. Sleep Med 16:775–778
Curjuric I, Imboden M, Bettschart R, Caviezel S, Dratva J, Pons M, Rothe T, Schmidt-Trucksass A, Stolz D, Thun GA, von Eckardstein A, Kronenberg F, Ferrarotti I, Probst-Hensch NM (2018) Alpha-1 antitrypsin deficiency: from the lung to the heart? Atherosclerosis 270:166–172
Fang Z, Liu YW, Zhao LY, Xu Y, Zhang FX (2015) Sleep-associated movement disorders and the risk of cardiovascular disease: a systematic review and meta-analysis. World J Meta-Anal 3(3):181–187
Feng Y, Hu L, Xu Q, Yuan H, Ba L, He Y, Che H (2015) Cytoprotective role of alpha-1 antitrypsin in vascular endothelial cell under hypoxia/reoxygenation condition. J Cardiovasc Pharmacol 66:96–107
Ferini-Strambi L, Walters AS, Sica D (2014) The relationship among restless legs syndrome (Willis-Ekbom Disease), hypertension, cardiovascular disease, and cerebrovascular disease. J Neurol 261:1051–1068
Gottlieb DJ, Somers VK, Punjabi NM, Winkelman JW (2017) Restless legs syndrome and cardiovascular disease: a research roadmap. Sleep Med 31:10–17
Guo S, Huang J, Jiang H, Han C, Li J, Xu X, Zhang G, Lin Z, Xiong N, Wang T (2017) Restless legs syndrome: from pathophysiology to clinical diagnosis and management. Front Aging Neurosci 9:171
Hu Z, Liu J, Song Z, Hou Q, Fan X, Hou D (2015) Variants in the atherogenic ALOX5AP, THBD, and KNG1 genes potentiate the risk of ischemic stroke via a genetic main effect and epistatic interactions in a Chinese population. J Stroke Cardiovasc Dis 24(9):2060–2068
Hwang IC, Na KS, Lee YJ, Kang SG (2018) Higher prevalence of hypertension among individuals with restless legs syndrome: a meta-analysis. Psychiatry Investig 15(7):701–709
Innes KE, Selfe TK, Agarwal P (2012) Restless legs syndrome and conditions associated with metabolic dysregulation, sympathoadrenal dysfunction, and cardiovascular disease risk: a systematic review. Sleep Med Rev 16:309–339
Izci B, Ardic S, Firat H, Sahin A, Altinors M, Karacan I (2008) Reliability and validity studies of the Turkish version of the Epworth Sleepiness Scale. Sleep Breath 12:161–168
Karroum EG, Golmard JL, Leu-Semenescu S, Arnulf I (2015) Painful restless legs syndrome: a severe, burning form of the disease. Clin J Pain 31:459–466
Katsanos AH, Kosmidou M, Konitsiotis S, Tsivgoulis G, Fiolaki A, Kyritsis AP, Giannopoulos S (2018) Restless legs syndrome and cerebrovascular/cardiovascular events: systematic review and meta-analysis. Acta Neurol Scand 137:142–148
Katsi V, Katsimichas T, Kallistratos MS, Tsekoura D, Makris T, Manolis AJ, Tousoulis D, Stefanadis C, Kallikazaros I (2014) The association of restless legs syndrome with hypertension and cardiovascular disease. Med Sci Monit 20:654–659
Koo DL, Nam H, Thomas RJ, Yun CH (2018) Sleep disturbances as a risk factor for stroke. J Stroke 20(1):12–32
Langhauser F, Göb E, Kraft P, Geis C, Schmitt J, Brede M, Gobel K, Helluy X, Pham M, Bendszus M, Jakob P, Stoll G, Meuth SG, Nieswandt B, McCrae KR, Kleinschnitz C (2012) Kininogen deficiency protects from ischemic neurodegeneration in mice by reducing thrombosis, blood-brain barrier damage, and inflammation. Blood 120(19):4082–4092
Li Y, Walters AS, Chiuve SE, Rimm EB, Winkelman JW, Gao X (2012) Prospective study of restless legs syndrome and coronary heart disease among women. Circulation 126:1689–1694
Li Y, Li Y, Winkelman JW, Walters AS, Han J, Hu FB, Gao X (2018) Prospective study of restless legs syndrome and total and cardiovascular mortality among women. Neurology 90:e135–e141
Morange PE, Suchon P, Trégouet DA (2015) Genetic of venous thrombosis: update in 2015. Thromb Haemost 114:910–919
Picchietti DL, Van Den Eeden SK, Inoue Y, Berger K (2017) Achievements, challenges, and future perspectives of epidemiologic research in restless legs syndrome (RLS). Sleep Med 31:3–9
Ribeiro MS, Dellalibera-Joviliano R, Becari C, Roberti Teixeira F, Vasconcelos Araujo P, Piccinato CE, Campos CP, Evora PRB, Joviliano EE (2014) Characterization of the kallikrein-kinin system, metalloproteinases, and their tissue inhibitors in the in-stent restenosis after peripheral percutaneous angioplasty. Ann Vasc Surg 28:1005–1015
Sateia MJ (2014) International classification of sleep disorders-third edition: highlights and modifications. Chest 146(5):1387–1394
Sevim S, Dogu O, Kaleagasi H, Aral M, Metin O, Camdeviren H (2004) Correlation of anxiety and depression symptoms in patients with restless legs syndrome: a population based survey. J Neurol Neurosurg Psychiatry 75:226–230
Stoll M, Cowley AW Jr, Tonellato PJ, Greene AS, Kaldunski ML, Roman RJ, Dumas P, Schork NJ, Wang Z, Jacob HJ (2001) A genomic-systems biology map for cardiovascular function. Science 294:1723–1726
Szentkiralyi A, Volzke H, Hoffmann W, Happe S, Berger K (2013) A time sequence analysis of the relationship between cardiovascular risk factors, vascular diseases and restless legs syndrome in the general population. J Sleep Res 22:434–442
Szentkiralyi A, Volzke H, Hoffmann W, Trenkwalder C, Berger K (2014) Multimorbidity and the risk of restless legs syndrome in 2 prospective cohort studies. Neurology 82:2026–2033
Trenkwalder C, Allen R, Högl B, Paulus W, Winkelmann J (2016) Restless legs syndrome associated with major diseases: a systematic review and new concept. Neurology 86:1336–1343
Varim P, Varim C, Acar T, Acar BA, Gokosmanoglu F, Yaylaci S, Cengiz H, Karacaer C (2019) Frequency of cardiovascular diseases in the patients with restless legs syndrome. Int J Adv Med 6(1):131–134
Vila N, Millan M, Ferrer X, Riutort N, Escudero D (2003) Levels of α-1-antitrypsin in plasma and risk of spontaneous cervical artery dissection: a case-control study. Stroke 34:e168–e169
Walters AS, Rye DB (2009) Review of the relationship of restless legs syndrome and periodic limb movements in sleep to hypertension, heart disease, and stroke. Sleep 32(5):589–597
Winkelman JW, Shahar E, Sharief I, Gottlieb DJ (2008) Association of restless legs syndrome and cardiovascular disease in the Sleep Heart Health Study. Neurology 70:35–42
Winkelman JW, Blackwell T, Stone K, Ancoli-Israel S, Redline S (2017) Associations of incident cardiovascular events with restless legs syndrome and periodic leg movements of sleep in older men, for the Outcomes of Sleep Disorders in Older Men Study (MrOS Sleep Study). Sleep 40
Winter AC, Schurks M, Glynn RJ, Buring JE, Gaziano JM, Berger K, Kurth T (2012) Restless legs syndrome and risk of incident cardiovascular disease in women and men: prospective cohort study. BMJ Open 2:e000866
Wu Y (2015) Contact pathway of coagulation and inflammation. Thrombosis J 13:17
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All Authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bellei, E., Bergamini, S., Monari, E. et al. Evaluation of potential cardiovascular risk protein biomarkers in high severity restless legs syndrome. J Neural Transm 126, 1313–1320 (2019). https://doi.org/10.1007/s00702-019-02051-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-019-02051-7