Abstract
Purpose of the review
Juvenile idiopathic arthritis (JIA) is the most common arthritis in the pediatric population. Manifestation of arthritis in the temporomandibular joint (TMJ) presents unique challenges in diagnosis and treatment. This review critically analyzes recent literature, emphasizes new findings, and offers guidance on controversial clinical practices.
Recent findings
Imaging: Magnetic resonance imaging with gadolinium contrast (Gd-MRI) is the current gold standard for diagnosis. A new TMJ-MRI scoring system has been developed by the Omeract JIA interest group. Clinical examination: Consensus-based clinical orofacial examination recommendations for monitoring patients have been developed and are currently validated. Treatment: Treatment of TMJ arthritis includes local and systemic drug therapy, treatment with orthodontic devices, and potentially maxilla-facial surgery.
Summary
A novel Gd-MRI scoring system and clinical examination recommendations for evaluating TMJ arthritis in JIA patients are available, enabling physicians to compare patients and treatment responses. Intra-articular injections should only be used in certain patients with caution. A combination of systemic medications combined with orthodontic appliances is necessary to treat these patients, warranting a multidisciplinary approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Juvenile idiopathic arthritis and temporomandibular joint involvement
Juvenile idiopathic arthritis (JIA) is the most common joint disease in childhood and is classified based on the International League of Associations for Rheumatology [1]. Arthritis of the temporomandibular joint (TMJ) in JIA has been increasingly described in the past decade [2,3,4,5,6,7]. TMJ arthritis can be present at diagnosis or develop during the disease and occurs in all ILAR subtypes [5, 7]. Depending on the cohort studied and the diagnostic test used, TMJ involvement occurs in up to 87% of children with JIA [2, 3, 5, 7].
In some cases, the TMJ is the only joint involved [8, 9]. Isolated TMJ arthritis remains a controversial issue; some question this entity to be idiopathic condylar resorption (ICR) rather than TMJ arthritis. A multicenter study by Hugle et al. [10•] reported 55 cases of isolated TMJ arthritis; during the disease course, six patients developed peripheral joint arthritis and four patients developed uveitis. On cone beam computer tomography (CBCT) imaging, the appearance of ICR and TMJ arthritis is very identical; it remains uncertain if these conditions are based on a different etiology or two presentations in the same spectrum of TMJ inflammation [10•, 11].
The purpose of this paper is to critically evaluate TMJ arthritis in JIA literature published over the previous 3 years and to address the challenges in diagnosis, treatment, and outcomes.
Clinical signs and symptoms of TMJ arthritis
Clinical signs and symptoms of TMJ arthritis have been challenging, and many studies have been dedicated to find reliable clinical features [4, 5, 7, 12, 13]. TMJ arthritis can be asymptomatic at presentation, or patients can present with symptoms of TMJ discomfort. However, patients with previous TMJ arthritis and damage to the joint can also present with TMJ symptoms and discomfort in absence of any active signs of arthritis on the MRI. Some recent studies have confirmed findings of older studies, increased TMJ arthritis in patients with younger age at onset, and the association of decreased maximal mouth opening and TMJ arthritis. All subtypes can be affected and involvement can lead to decreased growth of the mandible [14,15,16]. A systematic review on clinical predictors concluded the low level of evidence and study heterogeneity, which made it impossible to indicate a singular clinical outcome measure [17]. Kristensen et al. [17] advised the development of standardized terminology and evidence-based guidelines for clinical orofacial parameters in JIA patients to enhance study comparability. Stoustrup and colleagues of euroTMjoint have developed consensus-based orofacial examination recommendations for monitoring patients in clinical practice and research studies [18••]. Five recommendations were proposed for the orofacial examination of JIA patients to improve the clinical practice and aid standardized data collection for future studies [18••]. The five domains of the recommendations belong to include medical history, orofacial symptoms, muscle and TMJ function, orofacial function, and dentofacial growth [18••].
Due to the lack of reliable clinical predictors, the diagnosis of TMJ arthritis cannot be based on clinical signs and symptoms alone but needs to be confirmed by imaging [13, 19]. In a Pediatric Rheumatology International Trails Organisation (PRINTO) cross sectional study, clinical TMJ involvement was observed in 387 of 3343 JIA patients [20]. Polyarticular involvement was seen more in patients with clinical TMJ involvement and was associated with a higher disease activity score Juvenile Arthritis Disease Activity Score (JADAS), a higher disability, and impaired health-related quality of life compared to the patients without clinical TMJ involvement [20]. No radiological examinations were available for these patients to correlate the clinical TMJ involvement to active or chronic TMJ arthritis changes.
Craniofacial growth in JIA
Still already indicated the retrognathic mandible as a sign of TMJ arthritis in his opinion paper on childhood arthritis in 1897 [21]. In the last two decades, many manuscripts have highlighted the impaired craniofacial growth in JIA patients [22, 23]. Although the severe “bird-face” profile seems to be less frequently seen in the current rheumatology practice, craniofacial growth abnormalities are still observed, even in the biologic era. Unilateral involvement leads to asymmetry due to ramus symmetry [24], and bilateral involvement leads to retrognathic mandible, retruded chin, steep occlusal and mandibular planes, and a hyperdivergent pattern [15, 16]. These changes are, even with potent medication, still present even into adulthood [25]. The following association between dentofacial growth deviations and orofacial signs and symptoms has been described: Dentofacial growth deviations may cause asymmetric loading of joints and muscles, which in turn may lead to pain and reduced TMJ function and secondary pain spread to the TMJ-related orofacial muscles [17, 26].
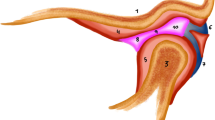
Imaging of the temproromandibular joint in JIA
The gold standard to detect active TMJ arthritis is the gadolinium-enhanced magnetic resonance imaging (Gd-MRI). However, other techniques are used and have better qualities than Gd-MRI, to evaluate the chronic changes and craniofacial growth abnormalities. The imaging technique used should be based on its use for diagnosing active TMJ arthritis or the assessment of chronic structural changes of TMJ and/or dentofacial growth deviations related to previous TMJ arthritis. Table 1 shows an overview of the advantage and disadvantage of the different imaging techniques used to depict the TMJs.
Magnetic resonance imaging
MRI with gadolinium contrast medium is currently considered the gold standard for identifying TMJ arthritis in JIA patients [19]. Previous studies have shown the high prevalence of TMJ arthritis in JIA on TMJ-MRI [2, 3, 27]. Although not all clinicians use Gd-MRI due to practical obstacles (availability, need for sedation), most clinicians do perform an MRI once clinical signs and symptoms are present [28]. Hauser et al. [29] showed that Gd-MRI findings lead to initiation of TMJ-specific treatments; 62% of patients received intra-articular joint injections and 6% started systemic medication based on findings on the first TMJ-MRI. The use of gadolinium in imaging, overall, is under scrutiny and questions have been raised if a Gd-MRI is needed to determine TMJ arthritis in JIA. A systemic review was performed and showed grade B (fair) evidence for accurate diagnosis of early and intermediate TMJ involvement changes, and contrast-enhanced MRI was superior in the detection of TMJ arthritis [30]. Unfortunately, to receive an accurate reading of the arthritis activity in the TMJ and Gd-MRI is necessary. An MRI without contrast will not be sufficient to differentiate between active and damage in TMJ arthritis. Physicians should consider the intervals between Gd-MRI and the treatments instigated in between treatments to justify repeated Gd-MRIs.
The interpretation and scoring of TMJ-MRIs have been increasingly studied. Resnick et al. showed thresholds of enhancement ratios of synovium relative to surrounding anatomy to be a consistent method for detecting low-grade synovitis [31, 32]. Signal intensity of synovium relative to the longus capitis muscle is particularly useful for diagnosis [31, 32] unlike the non-homogenous pterygoid and masticatory muscles [33]. In addition to synovitis, articular disk abnormalities (flat, fragmented, adherent, displaced) in both early and late TMJ arthritis are also frequently present [34]. Small amounts of joint fluid with intense contrast enhancement [35], osteochondral changes, and synovial thickening [36] are not reliable indicators for disease. As a further consideration, ultrasonography assessing capsular width has some correlation with synovitis identified through Gd-MRI [37]; however, the accuracy of TMJ ultrasonography is far lacking the Gd-MRI specificity and sensitivity. Three previous Gd-MRI scoring systems have been published: a Swiss, a German, and an US scoring system [38,39,40]. These three groups together with other members of the Outcome Measures in Rheumatoid Arthritis and Clinic Trails (OMERACT) JIA special interest group are developing a standardized MRI scoring system for TMJs in JIA. Tolend et al. [41•] reported the first results of a consensus-based TMJ-MRI scoring system including eight items: bone marrow edema and enhancement, condylar flattening, effusions, erosions, synovial enhancement and thickening, and disk abnormalities. The OMERACT TMJ-JIA special interest group is currently studying iterative refinements and reliability testing of the scoring system.
CBCT is not recommended over Gd-MRI for identifying active TMJ arthritis. However, CBCT is superior to Gd-MRI in evaluating dentofacial morphology and bone integrity and is used more to assess TMJ damage and dentofacial growth deviations in JIA [38, 42, 43].
Panoramic radiographs (orthopantomogram) do not have any purpose in the diagnosis of active TMJ arthritis. However, panoramic radiographs are a low-risk screening tool and they are used widespread in the dental field. Dental professionals should be aware that regular dental imaging has the potential to detect abnormal condyle morphology and antegonial notching, which have been shown to be predictive of TMJ synovitis [44, 45]. The correct imaging modality for TMJ arthritis is dependent on the questions to be answered. If the reason for imaging is to visualize active arthritis, a Gd-MRI is the imaging technique. In case of TMJ or craniofacial morphology questions, a CBCT is superior to a Gd-MRI and is the appropriate imaging modality in this situation.
Treatment
Specific treatment of the TMJs in JIA was ignored for many decades after the first description by Still in 1897. Treatments used include the systemic rheumatological drug therapies, local therapies, including intra-articular injections and orthodontic appliances and surgical intervention, although this is not a treatment but a solution for permanent damage accrued over the disease course. An international survey among pediatric rheumatologists revealed the most popular first-line treatment for TMJ arthritis to be non-biologic DMARDs (36%) and NSAIDs (33%), followed by intra-articular corticosteroid injections (IACI) (26%) and anti-TNF agents (5%) [46]. Treatment of TMJ arthritis and/or involvement includes three distinct aspects: (1) the treatment of active inflammation with local or systemic drug treatments, (2) treatment of arthritis-induced signs and/or symptoms (e.g., stabilization splints for pain), and (3) treatment of dentofacial growth deviation with orthopedic devices or surgery.
Animal models have been used to investigate TMJ-focused treatments. Rabbit studies with ovalbumin-induced TMJ arthritis have shown systemic methotrexate to curtail reduced mandibular growth [47] and decrease the TMJ inflammatory process without complete resolution [48, 49]. Simvastatin, a cholesterol-lowering medication previously shown to reduce inflammation, offered promising results in maintaining normal condylar bone growth in rats with complete Freund’s adjuvant (CFA)-induced TMJ arthritis [50]. Another rat study with CFA-induced TMJ arthritis successfully reduced inflammation with a prodrug of dexamethasone, particularly with systemic administration rather than intra-articular [51].
IACI are often used as adjunct to systemic treatments such as DMARDs and biologics. Sixty-five percent of centers worldwide use IACI as treatment for TMJ involvement [46]. Injections typically consist of triamcinolone hexacetonide at a dose of 5 to 20 mg/joint. These injections are often image-guided instead of landmark-based [52]. Resnick et al. [53] showed that outcomes of IACI do not improve with image guidance (intra-operative ultrasound and computed tomography); however, this might be operator-dependent. A systematic review performed to identify the efficacy and safety of IACI revealed that the level of evidence only allowed minimal conclusions [26]. The 2012 review alluded to the potential controversial effect of IACI on mandibular growth [26]. A retrospective study by Lochbuhler et al. [54••] evaluated the effect of IACI on mandibular growth disturbances and found that, while inflammation is decreased, mandibular growth is not normalized and may be impeded. IACI may furthermore inflict damage to the condylar growth plates that is of superior importance to mandibular development, because these structures are positioned uniquely, superficial on the condylar surface in contrast to other growth plates in long bones, and may be more vulnerable to the effect of corticosteroids. Another negative aspect of IACI is the formation of intra-articular calcifications/osteophytes in approximately 20% of the patients, leading to significant functional problems [54••]. The potential for significant damage due to the IACI treatment is alarming and has led to a significant decrease in the use of IACI for TMJ arthritis [55]. There is minimal evidence to show that IACI improve long-term pain and function of the TMJ. A retrospective study of 10-mg injections found that 18% of patients had resolution of synovitis at a follow-up time of 23 months [56]. An observational pilot study assessing short- and long-term effects of TMJ IACI on pain and function found merely a temporary pain-relief effect rather than a long-term effect on pain control [57]. This study was not designed to look at the long-term effect on the inflammatory process.
Two additional divergent local techniques have shown promising results and may be applicable treatment options. Case studies of IACI combined with arthroscopic lysis and lavage have shown some improvement in TMJ pain and range of motion [58]. Arthrocentesis alone without steroids has also been shown to be just as effective as with corticosteroid injections; 21 patients showed improvement in both pain and overall function [59].
Stoll et al. studied the benefit of TMJ intra-articular infliximab following insufficient benefit of systemic and IACI therapy and found no improvement of refractory acute or chronic symptoms [60]. Notably, the population studied had very refractory TMJ arthritis and treatment might be more successful if applied earlier in the disease process.
Unfortunately, no systemic drug studies have been performed with specific attention on the TMJ. The biologic trails performed in pediatric rheumatology have not focused on TMJ arthritis, notably they have not included imaging of the TMJ in their evaluation or any clinical signs and/or symptoms. The pediatric rheumatologist involved in TMJ arthritis research have often pondered the refractory nature of this joint. Suggestions have been mentioned that the TMJ should be treated more aggressively and active TMJ arthritis warrants initial treatment with a biologic agent; however, no studies have been performed to confirm these suspicions. The clinicians involved in euroTMjoint have become hesitant to use intra-articular steroid injections and are leaning towards early and aggressive systemic treatment as soon as active TMJ arthritis is present.
Oral splints
Oral splints are used to (1) normalize mandibular and dentofacial development in growing patients with arthritis-induced dentofacial growth deviation and (2) to reduce TMJ arthritis-induced orofacial signs and symptoms. The outline of the different types of splints varies with the aim of the splint treatment.
In terms of dentofacial growth deviations, functional appliances (a specific type of oral splint) are used to normalize the mandibular growth and minimize morphological issues due to JIA. The functional appliances offer a safe, reversible, and relatively economical option alongside pharmacological therapy. The Andersen appliance has been described to balance mandibular development and improve facial profile, showed reduced TMJ pain and inflammation, and improved jaw function if used for 2 years [61]. For JIA patients with unilateral TMJ involvement, González et al. [62] found a wide range of responses to a distraction splint, including halting the condylar deformity. In contrast, Stoustrup et al. [63•] found a reduction in mandibular asymmetry using an orthopedic splint in patients with unilateral TMJ involvement. Interestingly, in a recent experimental study by von Bremen et al. [64], growing rabbits with experimental TMJ arthritis treated with and intra-oral mandibular advancement appliance showed significantly less condylar resorption when compared to a group of untreated rabbits with experimental TMJ arthritis. In terms of orofacial signs and symptoms, current studies of functional appliances have shown promising results in improving and maintaining TMJ function and reducing pain. Functional therapy preventing teeth from achieving intercuspal contact showed decreased pain with jaw movement, increased maximal mouth opening, and reduced TMJ sounds [65]. Stoustrup et al. [66•] found that 8 weeks of therapy with the stabilization splint decreases pain frequency and intensity while improving mouth opening and laterotrusion.
Surgical treatments are used to correct severe craniofacial morphologic changes and are not part of the actual treatment of active TMJ arthritis. These procedures are usually not performed until patients have reached adulthood, due to the continued mandibular growth up to 25 years. However, in growing patients, treatment of severe arthritis-induced dentofacial deformities with mandibular surgical distractions has shown to be a predictable and safe treatment option [67].
Conclusions
The TMJ is frequently involved in JIA. TMJ arthritis can lead to dentofacial asymmetry and mandibular retrognathia and have a significant impact on the orofacial-related quality of life in JIA patients. The diagnosis is challenging and should include medical history, clinical examination, and imaging. Gd-MRI is the gold standard to diagnose active TMJ arthritis. Treatment should be multidisciplinary and should include systemic and local treatment options. Caution is warranted for the use of IACI and the potential detrimental effect on mandibular growth. Recent functional appliance studies have shown very promising morphological and functional benefits. The treatment of TMJ arthritis in JIA should include rheumatologists, dental and orthodontic professionals, physiotherapists, and oral and maxillofacial surgery. Examination of a child with JIA should include an orofacial examination. Efforts are currently undertaken to provide interactive videos to explain the orofacial examination for non-dental professionals.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31(2):390–2.
Kuseler A, Pedersen TK, Herlin T, Gelineck J. Contrast enhanced magnetic resonance imaging as a method to diagnose early inflammatory changes in the temporomandibular joint in children with juvenile chronic arthritis. J Rheumatol. 1998;25(7):1406–12.
Kuseler A, Pedersen TK, Gelineck J, Herlin T. A 2 year follow-up study of enhanced magnetic resonance imaging and clinical examination of the temporomandibular joint in children with juvenile idiopathic arthritis. J Rheumatol. 2005;32(1):162–9.
Pedersen TK, Kuseler A, Gelineck J, Herlin T. A prospective study of magnetic resonance and radiographic imaging in relation to symptoms and clinical findings of the temporomandibular joint in children with juvenile idiopathic arthritis. J Rheumatol. 2008;35(8):1668–75.
Twilt M, Mobers SM, Arends LR, ten Cate R, van Suijlekom-Smit L. Temporomandibular involvement in juvenile idiopathic arthritis. J Rheumatol. 2004;31(7):1418–22.
Twilt M, Arends LR, Cate RT, van Suijlekom-Smit LW. Incidence of temporomandibular involvement in juvenile idiopathic arthritis. Scand J Rheumatol. 2007;36(3):184–8. https://doi.org/10.1080/03009740601154368.
Weiss PF, Arabshahi B, Johnson A, Bilaniuk LT, Zarnow D, Cahill AM, et al. High prevalence of temporomandibular joint arthritis at disease onset in children with juvenile idiopathic arthritis, as detected by magnetic resonance imaging but not by ultrasound. Arthritis Rheum. 2008;58(4):1189–96. https://doi.org/10.1002/art.23401.
Martini G, Bacciliero U, Tregnaghi A, Montesco MC, Zulian F. Isolated temporomandibular synovitis as unique presentation of juvenile idiopathic arthritis. J Rheumatol. 2001;28(7):1689–92.
Scolozzi P, Bosson G, Jaques B. Severe isolated temporomandibular joint involvement in juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2005;63(9):1368–71. https://doi.org/10.1016/j.joms.2005.05.300.
• Hugle B, Spiegel L, Hotte J, Wiens S, Herlin T, Cron RQ, et al. Isolated arthritis of the temporomandibular joint as the initial manifestation of juvenile idiopathic arthritis. J Rheumatol. 2017. This is a relative large cohort of children who presented with isolated TMJ arthritis.
Posnick JC, Fantuzzo JJ. Idiopathic condylar resorption: current clinical perspectives. J Oral Maxillofac Surg. 2007;65(8):1617–23. https://doi.org/10.1016/j.joms.2007.03.026.
Twilt M, Schulten AJ, Verschure F, Wisse L, Prahl-Andersen B, van Suijlekom-Smit LW. Long-term follow up of temporomandibular joint involvement in juvenile idiopathic arthritis. Arthritis Rheum. 2008;59(4):546–52. https://doi.org/10.1002/art.23532.
Koos B, Twilt M, Kyank U, Fischer-Brandies H, Gassling V, Tzaribachev N. Reliability of clinical symptoms in diagnosing temporomandibular joint arthritis in juvenile idiopathic arthritis. J Rheumatol. 2014;41(9):1871–7. https://doi.org/10.3899/jrheum.131337.
Kalaykova SI, Klitsie AT, Visscher CM, Naeije M, Lobbezoo FA. Retrospective study on possible predictive factors for long-term temporomandibular joint degeneration and impaired mobility in juvenile arthritis patients. J Oral Facial Pain Headache. 2017;31(2):165–71. https://doi.org/10.11607/ofph.1656.
Gorska A, Przystupa W, Rutkowska-Sak L, Kwiatkowska M, Chlabicz S, Szarmach I. Temporomandibular joint dysfunction and disorders in the development of the mandible in patients with juvenile idiopathic arthritis—preliminary study. Adv Clin Exp Med. 2014;23(5):797–804. https://doi.org/10.17219/acem/37256.
Hsieh YJ, Darvann TA, Hermann NV, Larsen P, Liao YF, Bjoern-Joergensen J, et al. Facial morphology in children and adolescents with juvenile idiopathic arthritis and moderate to severe temporomandibular joint involvement. Am J Orthod Dentofac Orthop. 2016;149(2):182–91. https://doi.org/10.1016/j.ajodo.2015.07.033.
Kristensen KD, Stoustrup P, Kuseler A, Pedersen TK, Twilt M, Herlin T. Clinical predictors of temporomandibular joint arthritis in juvenile idiopathic arthritis: a systematic literature review. Semin Arthritis Rheum. 2016;45(6):717–32. https://doi.org/10.1016/j.semarthrit.2015.11.006.
•• Stoustrup P, Twilt M, Spiegel L, Kristensen KD, Koos B, Pedersen TK, et al. Clinical orofacial examination in juvenile idiopathic arthritis: international consensus-based recommendations for monitoring patients in clinical practice and research studies. J Rheumatol. 2017;44(3):326–33. This study provides a recommendation for routine clinical examination of the TMJ
Keller H, Muller LM, Markic G, Schraner T, Kellenberger CJ, Saurenmann RK. Is early TMJ involvement in children with juvenile idiopathic arthritis clinically detectable? Clinical examination of the TMJ in comparison with contrast enhanced MRI in patients with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2015;13:56.
Frid P, Nordal E, Bovis F, Giancane G, Larheim TA, Rygg M, et al. Temporomandibular joint involvement in association with quality of life, disability, and high disease activity in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2017;69(5):677–86. https://doi.org/10.1002/acr.23003.
Still GF. On a form of chronic joint disease in children. Med Chir Trans. 1897;80:47–60 9.
Twilt M, Schulten AJ, Nicolaas P, Dulger A, van Suijlekom-Smit LW. Facioskeletal changes in children with juvenile idiopathic arthritis. Ann Rheum Dis. 2006;65(6):823–5. https://doi.org/10.1136/ard.2005.042671.
Twilt M, Schulten AJ, Prahl-Andersen B, van Suijlekom-Smit LW. Long-term follow-up of craniofacial alterations in juvenile idiopathic arthritis. Angle Orthod. 2009;79(6):1057–62. https://doi.org/10.2319/093008-511R.1.
Koos B, Gassling V, Bott S, Tzaribachev N, Godt A. Pathological changes in the TMJ and the length of the ramus in patients with confirmed juvenile idiopathic arthritis. J Craniomaxillofac Surg. 2014;42(8):1802–7. https://doi.org/10.1016/j.jcms.2014.06.018.
Resnick CM, Dang R, Henderson LA, Zander DA, Daniels KM, Nigrovic PA, et al. Frequency and morbidity of temporomandibular joint involvement in adult patients with a history of juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2017;75(6):1191–200. https://doi.org/10.1016/j.joms.2016.11.013.
Stoustrup P, Kristensen KD, Verna C, Kuseler A, Pedersen TK, Herlin T. Intra-articular steroid injection for temporomandibular joint arthritis in juvenile idiopathic arthritis: a systematic review on efficacy and safety. Semin Arthritis Rheum. 2013;43(1):63–70. https://doi.org/10.1016/j.semarthrit.2012.11.003.
Muller L, Kellenberger CJ, Cannizzaro E, Ettlin D, Schraner T, Bolt IB, et al. Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: a pilot study comparing clinical examination and ultrasound to magnetic resonance imaging. Rheumatology (Oxford). 2009;48(6):680–5. https://doi.org/10.1093/rheumatology/kep068.
Zwir LM, Terreri MT, Sousa SA, Fernandes AR, Guimaraes AS, Hilario MO. Are temporomandibular joint signs and symptoms associated with magnetic resonance imaging findings in juvenile idiopathic arthritis patients? A longitudinal study. Clin Rheumatol. 2015;34(12):2057–63. https://doi.org/10.1007/s10067-015-2925-y.
Hauser RASS, Cannizzaro E, Muller L, Kellenberger CJ, Saurenmann RK. How improtant is early magnetic resonance imaging of the temporormandibular joint for the treatment of children with juvenile idiopathic arthritis: a retrospective analysis. Pediatr Rheumatol Online J. 2014;12(1):36. https://doi.org/10.1186/1546-0096-12-36.
Munir S, Patil K, Miller E, Uleryk E, Twilt M, Spiegel L, et al. Juvenile idiopathic arthritis of the axial joints: a systematic review of the diagnostic accuracy and predictive value of conventional MRI. AJR Am J Roentgenol. 2014;202(1):199–210. https://doi.org/10.2214/AJR.12.10475.
Resnick CM, Vakilian PM, Breen M, Zurakowski D, Caruso P, Henderson L, et al. Quantifying temporomandibular joint synovitis in children with juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2016;68(12):1795–802. https://doi.org/10.1002/acr.22911.
Peacock ZS, Vakilian P, Caruso P, Resnick CM, Vangel M, Kaban LB. Quantifying synovial enhancement of the pediatric temporomandibular joint. J Oral Maxillofac Surg. 2016;74(10):1937–45. https://doi.org/10.1016/j.joms.2016.03.010.
von Kalle T, Stuber T, Winkler P, Maier J, Hospach T. Early detection of temporomandibular joint arthritis in children with juvenile idiopathic arthritis—the role of contrast-enhanced MRI. Pediatr Radiol. 2015;45(3):402–10. https://doi.org/10.1007/s00247-014-3143-5.
Kirkhus E, Arvidsson LZ, Smith HJ, Flato B, Hetlevik SO, Larheim TA. Disk abnormality coexists with any degree of synovial and osseous abnormality in the temporomandibular joints of children with juvenile idiopathic arthritis. Pediatr Radiol. 2016;46(3):331–41. https://doi.org/10.1007/s00247-015-3493-7.
Kottke R, Saurenmann RK, Schneider MM, Muller L, Grotzer MA, Kellenberger CJ. Contrast-enhanced MRI of the temporomandibular joint: findings in children without juvenile idiopathic arthritis. Acta Radiol. 2015;56(9):1145–52. https://doi.org/10.1177/0284185114548506.
Ma GM, Amirabadi A, Inarejos E, Tolend M, Stimec J, Moineddin R, et al. MRI thresholds for discrimination between normal and mild temporomandibular joint involvement in juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2015;13(1):53. https://doi.org/10.1186/s12969-015-0051-7.
Kirkhus E, Gunderson RB, Smith HJ, Flato B, Hetlevik SO, Larheim TA, et al. Temporomandibular joint involvement in childhood arthritis: comparison of ultrasonography-assessed capsular width and MRI-assessed synovitis. Dentomaxillofac Radiol. 2016;45(8):20160195. https://doi.org/10.1259/dmfr.20160195.
Koos B, Tzaribachev N, Bott S, Ciesielski R, Godt A. Classification of temporomandibular joint erosion, arthritis, and inflammation in patients with juvenile idiopathic arthritis. J Orofac Orthop. 2013;74(6):506–19. https://doi.org/10.1007/s00056-013-0166-8.
Vaid YN, Dunnavant FD, Royal SA, Beukelman T, Stoll ML, Cron RQ. Imaging of the temporomandibular joint in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2014;66(1):47–54. https://doi.org/10.1002/acr.22177.
Kellenberger CJALZ, Larheim TA. Magnetic resonance imaging of the temporomandibular joints in juvenile idiopathic arthritis. Semin Orthod. 2015;21(2):111–20. https://doi.org/10.1053/j.sodo.2015.02.007.
• Tolend MA, Twilt M, Cron RQ, Tzaribachev N, Guleria S, von Kalle T, et al. Towards establishing a standardized magnetic resonance imaging scoring system for temporomandibular joints in juvenile idiopathic arthritis Arthritis Care Res (Hoboken). 2017. This Omeract study provides the framework for a TMJ-MRI scoring system specifically for JIA patients.
Larheim TA, Abrahamsson AK, Kristensen M, Arvidsson LZ. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol. 2015;44(1):20140235. https://doi.org/10.1259/dmfr.20140235.
Al-Shwaikh H, Urtane I, Pirttiniemi P, Pesonen P, Krisjane Z, Jankovska I, et al. Radiologic features of temporomandibular joint osseous structures in children with juvenile idiopathic arthritis. Cone beam computed tomography study. Stomatologija. 2016;18(2):51–60.
Abramowicz S, Simon LE, Susarla HK, Lee EY, Cheon JE, Kim S, et al. Are panoramic radiographs predictive of temporomandibular joint synovitis in children with juvenile idiopathic arthritis? J Oral Maxillofac Surg. 2014;72(6):1063–9. https://doi.org/10.1016/j.joms.2013.11.021.
Piancino MG, Cannavale R, Dalmasso P, Tonni I, Filipello F, Perillo L, et al. Condylar asymmetry in patients with juvenile idiopathic arthritis: could it be a sign of a possible temporomandibular joints involvement? Semin Arthritis Rheum. 2015;45(2):208–13. https://doi.org/10.1016/j.semarthrit.2015.04.012.
Foeldvari I, Tzaribachev N, Cron RQ. Results of a multinational survey regarding the diagnosis and treatment of temporomandibular joint involvement in juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2014;12(1):6. https://doi.org/10.1186/1546-0096-12-6.
Prager TM, Meyer P, Rafayelyan S, Minden K, Jost-Brinkmann PG. Effect of methotrexate on the mandibular development of arthritic rabbits. Eur J Orthod. 2015;37(5):514–21. https://doi.org/10.1093/ejo/cju070.
Rafayelyan S, Meyer P, Radlanski RJ, Minden K, Jost-Brinkmann PG, Prager TM. Effect of methotrexate upon antigen-induced arthritis of the rabbit temporomandibular joint. J Oral Pathol Med. 2015;44(8):614–21. https://doi.org/10.1111/jop.12265.
Rafayelyan S, Radlanski RJ, Minden K, Pischon N, Jost-Brinkmann PG, Prager TM. Histomorphometry in antigen-induced arthritis of the rabbit temporomandibular joint. J Oral Pathol Med. 2015;44(1):67–74. https://doi.org/10.1111/jop.12201.
Holwegner C, Reinhardt AL, Schmid MJ, Marx DB, Reinhardt RA. Impact of local steroid or statin treatment of experimental temporomandibular joint arthritis on bone growth in young rats. Am J Orthod Dentofac Orthop. 2015;147(1):80–8. https://doi.org/10.1016/j.ajodo.2014.09.016.
Knudsen M, Bury M, Holwegner C, Reinhardt AL, Yuan F, Zhang Y, et al. Effect of dexamethasone prodrug on inflamed temporomandibular joints in juvenile rats. Arthritis Res Ther. 2015;17(1):267. https://doi.org/10.1186/s13075-015-0772-5.
Parra DA, Chan M, Krishnamurthy G, Spiegel L, Amaral JG, Temple MJ, et al. Use and accuracy of US guidance for image-guided injections of the temporomandibular joints in children with arthritis. Pediatr Radiol. 2010;40(9):1498–504. https://doi.org/10.1007/s00247-010-1581-2.
Resnick CM, Vakilian PM, Kaban LB, Peacock ZSI. Intra-articular steroid injection to the temporomandibular joint for juvenile idiopathic arthritis more effective and efficient when performed with image guidance? J Oral Maxillofac Surg. 2017;75(4):694–700. https://doi.org/10.1016/j.joms.2016.09.045.
•• Lochbuhler N, Saurenmann RK, Muller L, Kellenberger CJ. Magnetic resonance imaging assessment of temporomandibular joint involvement and mandibular growth following corticosteroid injection in juvenile idiopathic arthritis. J Rheumatol. 2015;42(8):1514–22. This paper shows the negative effect of intra-articular TMJ steroid injections on the craniofacial growth
Stoustrup P, Twilt M. Therapy. Intra-articular steroids for TMJ arthritis—caution needed. Nat Rev Rheumatol. 2015;11(10):566–7. https://doi.org/10.1038/nrrheum.2015.97.
Resnick CM, Vakilian PM, Kaban LB, Peacock ZS. Quantifying the effect of temporomandibular joint intra-articular steroid injection on synovial enhancement in juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2016;74(12):2363–9. https://doi.org/10.1016/j.joms.2016.06.189.
Stoustrup P, Kristensen KD, Kuseler A, Pedersen TK, Herlin T. Temporomandibular joint steroid injections in patients with juvenile idiopathic arthritis: an observational pilot study on the long-term effect on signs and symptoms. Pediatr Rheumatol Online J. 2015;13(1):62. https://doi.org/10.1186/s12969-015-0060-6.
Kinard BE, Bouloux GF, Prahalad S, Vogler L, Abramowicz S. Arthroscopy of the temporomandibular joint in patients with juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2016;74(7):1330–5. https://doi.org/10.1016/j.joms.2016.01.028.
Olsen-Bergem H, Bjornland T. A cohort study of patients with juvenile idiopathic arthritis and arthritis of the temporomandibular joint: outcome of arthrocentesis with and without the use of steroids. Int J Oral Maxillofac Surg. 2014;43(8):990–5. https://doi.org/10.1016/j.ijom.2014.03.018.
Stoll ML, Morlandt AB, Teerawattanapong S, Young D, Waite PD, Cron RQ. Safety and efficacy of intra-articular infliximab therapy for treatment-resistant temporomandibular joint arthritis in children: a retrospective study. Rheumatology (Oxford). 2013;52(3):554–9. https://doi.org/10.1093/rheumatology/kes318.
Portelli M, Matarese G, Militi A, Logiudice G, Nucera R, Lucchese A. Temporomandibular joint involvement in a cohort of patients with juvenile idiopatic arthritis and evaluation of the effect induced by functional orthodontic appliance: clinical and radiographic investigation. Eur J Paediatr Dent. 2014;15(1):63–6.
Gonzalez MF, Pedersen TK, Dalstra M, Herlin T, Verna C. 3D evaluation of mandibular skeletal changes in juvenile arthritis patients treated with a distraction splint: a retrospective follow-up. Angle Orthod. 2016;86(5):846–53. https://doi.org/10.2319/081715-549.1.
• Stoustrup P, Kuseler A, Kristensen KD, Herlin T, Pedersen TK. Orthopaedic splint treatment can reduce mandibular asymmetry caused by unilateral temporomandibular involvement in juvenile idiopathic arthritis. Eur J Orthod. 2013;35(2):191–8. This study shows the importance and potential of splint treatment in JIA patients with unilateral involvement
von Bremen J, Kohler K, Siudak K, Zahner D, Ruf S. Histologic effects of mandibular protrusion splints in antigen-induced TMJ arthritis in rabbits. Pediatr Rheumatol Online J. 2017;15(1):27. https://doi.org/10.1186/s12969-017-0158-0.
Isola G, Ramaglia L, Cordasco G, Lucchese A, Fiorillo L, Matarese G. The effect of a functional appliance in the management of temporomandibular joint disorders in patients with juvenile idiopathic arthritis. Minerva Stomatol. 2017;66(1):1–8. https://doi.org/10.23736/S0926-4970.16.03995-3.
• Stoustrup P, Kristensen KD, Kuseler A, Verna C, Herlin T, Pedersen TK. Management of temporomandibular joint arthritis-related orofacial symptoms in juvenile idiopathic arthritis by the use of a stabilization splint. Scand J Rheumatol. 2014;43(2):137–45. This study shows the positive effect of a stabilization splint on the management of TMJ pain
Norholt SE, Pedersen TK, Herlin T. Functional changes following distraction osteogenesis treatment of asymmetric mandibular growth deviation in unilateral juvenile idiopathic arthritis: a prospective study with long-term follow-up. Int J Oral Maxillofac Surg. 2013;42(3):329–36. https://doi.org/10.1016/j.ijom.2012.09.012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Rheumatology
Rights and permissions
About this article
Cite this article
Kovalko, I., Stoustrup, P. & Twilt, M. Temporomandibular Joint Involvement in Juvenile Idiopathic Arthritis: Challenges in Diagnosis, Treatment, and Outcomes. Curr Treat Options in Rheum 4, 44–54 (2018). https://doi.org/10.1007/s40674-018-0086-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-018-0086-2