Abstract
Background
Juvenile idiopathic arthritis (JIA) has an incidence that ranges from 1 to 22 per 100,000 children worldwide, with involvement of the temporomandibular joint (TMJ) in 17–87% of patients. Intraarticular corticosteroid injections are beneficial in the local treatment of JIA and of other types of arthritis.
Objective
To describe and assess the accuracy of an US-guided technique for visualization of needle placement within the TMJ in children.
Materials and methods
Between January 2000 and November 2007, 180 TMJ injections were performed during 116 encounters in 83 children with arthritis (71 girls, 12 boys; mean age 12.0 years). Access was obtained under sterile conditions using US guidance (linear 15-MHz or curvilinear 8-MHz transducers) in a coronal plane, and confirmed with CT. To minimize radiation, a limited focused CT protocol was developed.
Results
A bilateral injection was performed in 65 encounters (57%). Twenty-three children had repeat TMJ injections. All injections were performed using US guidance. CT confirmation was used in 127/180 TMJs (70%). In those confirmed with CT, the needle tip was intra-articular in 91% of cases. Triamcinolone hexacetonide was used in 92% of injections and triamcinolone acetonide in 8%. One major complication was encountered (skin atrophy at the injection site).
Conclusion
In our experience, TMJ injections using sonographic guidance is a safe, effective and accurate procedure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The temporomandibular joint (TMJ) can be affected in different types of arthritis, with juvenile idiopathic arthritis (JIA) being the most frequent in childhood. The term JIA refers to a group of disorders characterized by chronic arthritis in children [1]. It is the most common chronic rheumatic disease in childhood [1, 2] with an incidence that ranges from 1 to 22 per 100,000 and with a prevalence of 8–150 per 100,000 [1]. JIA is defined as persistent arthritis for more than 6 weeks with an onset at younger than 16 years of age, after excluding other causes of joint inflammation [3]. The etiology is unclear but appears to be multifactorial and may be related to genetic factors associated with triggering events such as psychological stress, abnormal hormone levels, trauma, or infections [1]. The histopathology of the inflamed joints shows infiltration by lymphocytes, plasma cells, macrophages and dendritic cells associated with a proliferation of fibroblasts and macrophage-like synoviocytes [4]. The classification of children with arthritis has been challenging. There are three different classification systems in use. In the 1970s, two sets of criteria were developed: the Juvenile Rheumatoid Arthritis (JRA) criteria from the American College of Rheumatology (ACR), and the Juvenile Chronic Arthritis (JCA) criteria from the European League Against Rheumatism (EULAR). More recently, the ILAR criteria were developed by the International League of Associations for Rheumatology in the 1990s [1, 4]. In this article we use the ILAR classification, in which the term “juvenile idiopathic arthritis” describes seven subtypes of arthritis according to the clinical features during the first 6 months of disease and with the following frequencies: oligoarticular JIA (50–60%); polyarticular JIA, both rheumatoid factor positive and negative (30–35%); systemic JIA (10–20%); juvenile psoriatic arthritis (2–15%); enthesitis-related arthritis (1–7%) [1], and undifferentiated arthritis.
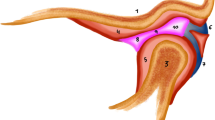
The TMJ can be involved in any type of JIA with a reported prevalence that has varied between 17% and 87% based on the subtype of JIA, method of diagnosis and population studied [5]. The TMJ is a complex synovial condylar joint whose surfaces are covered with fibrocartilage, and which may be affected by inflammatory or degenerative arthropathies. In children, the mandibular growth plate is adjacent to the fibrocartilage of the condylar head, making it vulnerable to inflammatory damage [6]. This can result in micrognathia and retrognathia in up to 30% of the patients and malocclusion in up to 69% [6]. Other complications include facial asymmetry, decreased mouth opening, chewing difficulties and pain with jaw movement. In many cases the inflammation is asymptomatic. The gold standard for the diagnosis is contrast-enhanced MRI, which can detect early signs of inflammation before joint destruction [6].
The treatment alternatives for JIA include systemic therapy (e.g., NSAIDS, methotrexate, sulfasalazine, biologics) and local therapy (arthrocentesis, occlusal devices, intraarticular injections of steroids or sodium hyaluronate) [6]. Intraarticular corticosteroids are used to induce a rapid resolution of synovitis with minimal systemic effects, showing good outcomes in terms of symptoms and functionality [7]. The literature is limited but promising on TMJ corticosteroid injections. Cahill et al. [8] reported 27 joint injections with an improvement of symptoms (decrease of pain in 88% of the patients) and on imaging findings (decrease or resolution of the effusion in 73% of the treated joints). Arabshahi et al. [6] also observed decrease in pain, improvement of the maximal incisor opening and a decrease in the signs of inflammation on imaging following intraarticular steroids in 23 patients [6].
Many joints are injected by rheumatologists using anatomic landmarks only while others require image guidance [9, 10]. Increasingly, over the last 8–10 years, patients in our institution are referred to interventional radiology by the rheumatology service for image-guided tendon sheath and joint injections (such as shoulder, hip, subtalar, and temporomandibular joints). The TMJ is a difficult joint to image by fluoroscopy because this modality assesses only the bony components of the joint, and overlapping bony structures can make interpretation and guidance difficult. Alternative modalities include CT, MRI and US [11, 12]. CT gives good bony anatomical detail but involves radiation close to the eye and the thyroid. MRI gives excellent anatomical and pathological detail but still requires further development before it becomes a routine modality for interventional procedures. Endoarticular US imaging using 2-mm US transducers of the TMJ has been proposed as a diagnostic tool [12], but has not gained widespread acceptance.
Given our experience with and availability of US, we applied it for image guidance during TMJ injections. CT became available in one of our interventional suites in 2001, enabling us to confirm the accuracy of needle tip position within the joint. The use of CT confirmation has become a routine practice in most cases.
The purpose of this paper is to describe the sonographic technique used to visualize and inject the TMJ and to assess the accuracy of needle placement in those confirmed by CT.
Materials and methods
Research Ethics Board approval was obtained for this study. A retrospective review was undertaken of all cases of US-guided TMJ injections between 2000 and 2007. No patients who underwent US-guided TMJ injections were excluded. Patients were identified through our dedicated interventional database (Esh-IGT) and in our PACS system (General Electric Centricity, GE Healthcare Canada, Mississauga, Ontario). The sonographic study was performed with HDI 5000 units (Philips Medical Systems, Bothell, WA, USA); CT was performed using an Asteion system (Toshiba America Medical Systems, Tustin, CA, available from May 2001). Patient demographics, disease classification and procedural details were captured. Each separate visit to the interventional suite was identified as an encounter, irrespective of the number of joints injected. Each joint injected was counted separately (i.e. bilateral TMJ injections were counted as two joints). Procedures were performed by staff interventionalists and/or supervised interventional fellows. Healthy patients (American Society of Anesthesiologists physical status classification I–III) with good mouth opening and few joint/tendon injections were considered for nurse-administered sedation; the remainder of the patients were referred for management by an anesthesiologist. The use of CT did not influence the choice of sedation or anaesthesia.
The imaging and radiological reports were independently and retrospectively reviewed by two of the investigators (B.C. and D.P.). Needle position was defined as acceptable or unacceptable depending on whether the tip was within the joint space deep to the capsule. An acceptable position was defined on the confirmatory CT, when the needle tip was positioned deeper than an imaginary line drawn between the lateral aspect of the articular tubercle of the anterior eminence and the lateral aspect of the postglenoid process (Fig. 1), below the roof of the glenoid fossa and above the junction of the mandibular ramus with its rounded condyle (Fig. 1). An unacceptable position was defined when the needle tip was seen outside of these margins.
Axial (a) and sagittal (b) CT images illustrate the anatomical landmarks used to confirm the needle placement in TMJ injections. A needle tip is considered in an acceptable (intraarticular) position when it is located deeper than an imaginary line drawn between the lateral aspect of the articular tubercle of the anterior eminence (1) and the lateral aspect of the postglenoid process (2), on the axial plane; and between the roof of the glenoid fossa (3) and the junction of the mandibular ramus with its rounded condyle (4), on the sagittal plane
When adjustment of the needle tip was performed, we categorized the adjustments as major or minor. If the needle was “acceptable” (i.e. within the joint capsule), but was moved slightly to optimize its position, it was considered a minor adjustment. When the needle tip was “unacceptable” (i.e. outside the joint capsule), any reorientation was considered a major adjustment. We further categorized the minor and major adjustments as advancement, withdrawal or re-orientation.
The patients were classified as best as possible according to the ILAR classification based on available clinical and laboratory information obtained from the charts. Not all the patients had a rheumatoid factor tested or repeated more than once; therefore, in these cases the diagnosis used was based on clinical criteria.
The outcomes or efficacy of the treatment was based on the records from the patient’s first follow-up visit at the rheumatology clinic, usually 6 weeks post procedure. Patients having significant decrease in pain, improvement in mouth opening and decrease in tenderness on physical examination were classified as having a good response to the treatment. If there was only a partial decrease of the patient’s symptoms or signs, he or she was classified as having a partial response. A poor response was defined as no improvement in the symptoms after the injection(s).
Medical records were examined for potential complications including infection, skin atrophy, swelling and bruising. Complications were classified as minor or major according to the Society for Interventional Radiology (SIR) guidelines [13].
Technique
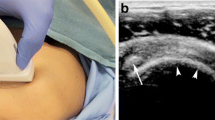
After obtaining informed consent, patient pain and anxiety was controlled either in the form of nurse-administered intravenous sedation (fentanyl (Sandoz Inc., Quebec, Canada.), midazolam (Sandoz Inc., Quebec, Canada)), +/− ketamine (Sandoz Inc., Quebec, Canada) or by an anesthetist (using a wide variety of sedative agents or a general anesthetic). Gauze was placed in the external auditory canal to prevent irritation of the tympanic membrane from the preparation solution (Betadine; 10% povidone-iodine topical solution USP; Purdue Pharma, Pickering, Canada). The procedure was performed with the mouth closed. Under sterile conditions the US transducer (15-MHz linear or 8-MHz curvilinear) was used in a coronal plane and swept posteriorly along the zygomatic arch towards the TMJ. The zygomatic arch was seen as a convex echogenic surface casting a shadow, surrounded by muscle (Fig. 2). The US was then swept superiorly along the ramus of the mandible cranially to the TMJ. The mandibular ramus was well recognized as a flat bone ascending to the condyle (Fig. 2), which terminates in the joint. The TMJ lies where the zygomatic arch and mandible intersect (Fig. 2); however, the articular disc itself could not be seen by US. The glenoid fossa in the temporal bone was seen just cranial to the condyle and the superficial aspect of the joint could be seen as a gap between these two bony structures. Care was made to ensure the coronoid process was not mistaken for the condyle of the mandible, the latter being more posterior, near the tragus of the ear. The needle (25 gauge) was advanced under direct US vision into the joint, perpendicular to the US transducer (Fig. 3), usually at a slightly cephalad and posterior angle. Limited noncontrast axial CT slices (2–3 mm thickness, 20 mA, 120 kVp. DLP:8.4 mGy.cm) confirmed the placement of the needle(s) in the joint (either upper or lower compartment) and adjustments were made if necessary (Fig. 4). Once the needle’s position was confirmed, the medication was injected. The agent most commonly injected was Aristospan (triamcinolone hexacetonide, Valeo Pharma Inc., Montreal, Canada) and less commonly triamcinolone acetonide (Sandoz Inc., Quebec, Canada) at a dose prescribed by the referring rheumatologist (usually 5–10 mg = 0.25–0.5 mls). This was followed by local anesthetic (1% lidocaine; Xylocaine, AstraZeneca Canada Inc., Mississauga, Ontario) of similar volume.
US examination. a Sonographic view of the zygomatic arch (ZA) obtained with a 15 MHz linear transducer. Coronal view shows the zygomatic arch as a convex echogenic surface casting a shadow. b Coronal view obtained with the 8 MHz curvilinear probe shows the mandibular ramus (MR), the mandibular condyle (C) and glenoid fossa (GF). c Coronal view of the TMJ (*) obtained with a 15 MHz linear transducer
Results
Eighty-three children were identified who underwent a total of 180 TMJ injections in 116 separate encounters. There were 71 girls and 12 boys, ranging in age from 4 years and 3 months to 17 years (mean 12 years, median 12.2 years). Seventy-eight of the children were classified in the different subtypes of JIA (Table 1). There were five additional children included in the study who did not fall into the ILAR classification: three children who had inflammatory bowel disease-related arthritis, one child with a pseudorheumatoid dysplasia and another with inflammatory linear verrucous epidermal nevus (ILVEN) syndrome.
Of the 83 children, 18 underwent two separate encounters, while three had three encounters; one patient had five and another had six repeat encounters. A total of 180 TMJ injections were performed under US guidance. Limited CT was employed to check needle placement in 127 joints (70%). In the remaining 53/180 (30%) CT was not used either because of lack of availability or radiologist preference. Needle placement was “acceptable” (i.e. within the joint) in 115/127 joints (91%). Of these 115 cases, no adjustment at all was required in 95 needle tips (75%) (Fig. 4). Minor needle adjustment was made in 20 (16%) (Fig. 5) and categorized as reorientation in 10, advancement in 6 and withdrawal in 4. In 12/127 joints (9%) the CT images showed that the needle tip was “unacceptable” and a major adjustment (reorientation) was required (Fig. 6). Triamcinolone hexacetonide was employed in 92% of the injections.
Review of the charts showed a follow-up clinic note after 99/116 encounters (85%). In 80/99 (81%) follow-up visits, a good response was documented; in 10/99 (10%) there was a partial response; and in 9/99 visits (9%) there was a poor response.
There was one major complication of skin atrophy over the TMJ area. Ten patients experienced minor self-limiting side effects (transient early swelling and pain), all of which settled spontaneously.
Discussion
Involvement of the TMJs in JIA is a common occurrence [1–4]. This joint is one of the most underdiagnosed and undertreated conditions of JIA, probably because its involvement is often asymptomatic and the joint is difficult to examine [14]. Involvement of the growing condyle can result in significant functional and aesthetic sequelae [6, 14]. Injection of intraarticular corticosteroids appears to be a valuable therapeutic option with a good response of the symptoms, improvement of the inflammatory changes on MRI and reduction in potential of significant sequelae [6–8].
In recent years the use of radiography for evaluation of TMJs has become less common as it has been replaced by cross-sectional imaging (i.e. CT and MRI). For injections, fluoroscopy has difficulties with overlapping bone structures when visualizing the TMJs. Experience with musculoskeletal US continues to increase, with reports of its application in joint and tendon sheath injections [9, 10]. Although literature in the use of US in TMJ evaluation is limited, we attempted to use it for TMJ injections. A learning curve was seen amongst radiologists in identifying sonographic TMJ landmarks, approach and needle position. US proved to be a quick, efficient, reliable and reproducible method for accessing the TMJ, and was relatively easy to learn. Although we most commonly use a 15-MHz linear “hockey stick” transducer for musculoskeletal interventions, we find the curvilinear 8-MHz probe also useful for TMJs. The addition of limited CT slices acted as a useful internal quality control check. The choice to confirm needle position with a few CT slices was largely dependent on radiologist preference at the time and on the availability of the scanner. The accuracy of the needle tip placement was balanced against the exposure to radiation and lengthening the procedure time. Placing the needle under US control and using CT for confirmation of position only, involves less radiation than if CT is used to guide the entire procedure. While learning the technique, CT provides not only reassurance for the operator regarding tip position but also assists with needle tip optimization.
We recognize that few centers may have the facility to use CT to confirm needle placement in a TMJ. It therefore is important to report the technique for those interventionalists who wish to use this US method, with the reassurance of the accuracy found in those cases in which CT was used. In 127 joints imaged by CT, we noted that in 115 (91%), the needle position was acceptable (with only a minor adjustment performed in 20/115) and in 9% of joints a major adjustment was required. In the cases of minor adjustments a repeat CT was not always performed. It should be noted that a good clinical response can occur even when medication is injected in the periarticular tissues of the joint; therefore, an overall good response does not, of itself, indicate definitive intraarticular placement [9]. However, periarticular injection of steroids can predispose to skin atrophy, a complication that was seen in one of the patients in our series. In that particular patient, both at the time and on retrospective review, the needle tip position was satisfactory with US and CT; the skin atrophy may therefore have related to leakage of the steroid along the needle tract.
In those cases in which the needle required a major adjustment, the most common error was being too ventral or too caudal. To compensate for this, in a coronal plane one should place the transducer anterior to the tragus of the ear and puncture the TMJ with the needle perpendicular to the tranducer and directed slightly cephalad and posteriorly.
Initially when using CT for confirmation of needle position, we had no set protocol. A self audit several years ago revealed a wide range in the number of slices, slice thickness, imaging parameters (kVp, mA) and area imaged. Since then, we adjusted our CT protocol to keep the radiation to a minimum. We now access the joints with a 25G needle using US initially. We position the scanner using the laser marker. We adjust the patient’s head to align the needle(s) as well as possible to lie within the line of the laser. We tilt the scan beam away from the eyes if necessary. We perform the scan without any scout, obtaining 3–4 slices 3-mm thick, using a low mA (20 mA), from just below the needle level(s) to just above, scanning both needles simultaneously if bilateral TMJs are being injected. We do not have experience with the use of cone-beam CT and its associated dose.
The results of this review highlight the importance of this clinical application of US. Its most advantageous feature is the ability to obtain real-time images without exposure to radiation and it is currently less expensive and more available than CT or MRI. US guidance allows therapy to be administered with precision and (considerable) reliability into the intraarticular compartment of the TMJ, with safety and few side effects. As we progress along our learning curve with US in the TMJ, it is foreseeable that individual experienced staff may obviate the need for CT altogether.
There are several limitations to this study. It is a retrospective review and there were no consistent specific clinical criteria applied to assess the severity of TMJ disease prior to joint injection or efficacy of response post injection. We relied on the radiological report for documentation of any difficulties during the procedure (e.g., confidence in US guidance) and we acknowledge this may underestimate technical issues.
We chose to classify patients using the ILAR criteria, since it is the most current classification system for juvenile arthritis. However, a number of the patients studied were diagnosed prior to the existence of the ILAR criteria. Therefore, in this “historical” group there were missing data including measurement of two serial rheumatoid factors and a HLA-B27. Although we tried our best to assign patients to appropriate subgroups on disease course and available laboratory data, accurate assignment to an ILAR subgroup may had been somewhat compromised. The archiving of US images for guidance obtained during the procedure was inconsistent. We cannot make any comment on the variety of the sonographic appearances of the joints secondary to the severity of their involvement by the primary disease. The CT technique varied during the time of this review. Neither US nor CT permits visualization of the articular disc. We cannot therefore know with certainty whether injections were made into the superior or inferior compartment of the TMJ and the difference it would make. Future research may focus on the possibility of MR guidance for injections, which would enable visualization of the disc, to address such questions.
However, despite these limitations, we were able to achieve the study’s primary purpose by describing this sonographic technique and assessing the accuracy of needle placement by US, using CT for confirmation.
Conclusion
US guidance for TMJ injections is a minimally invasive, safe, reliable and accurate method that provides an effective therapeutic approach in pediatric patients with arthritis.
References
Weiss J, Ilowite N (2005) Juvenile idiopathic arthritis. Pediatr Clin N Am 52:413–442
Manners PJ, Bowers C (2002) Worldwide prevalence of juvenile arthritis: why does it vary so much? J Rheumatol 29:1520–1530
Haskes P, Laxer R (2005) Medical treatment of juvenile idiopathic arthritis. JAMA 294:1671–1684
Borchers A, Selmi C, Cheema G et al (2006) Juvenile idiopathic arthritis. Autoimmun Rev 5:279–298
Pedersen TK, Jensen JJ, Melsen B et al (2001) Resorption of the temporomandibular condylar bone according to subtypes of juvenile chronic arthritis. J Rheumatol 28:2109–2115
Arabshahi B, Dewitt EM, Cahill AM et al (2005) Utility of corticoesteroid injection for temporomandibular arthritis in children with juvenile idiopathic arthritis. Arthritis Rheum 52:3563–3569
Cleary AG, Murphy HD, Davidson JE (2003) Intraarticular corticosteroid injections in juvenile idiopathic arthritis. Arch Dis Child 88:192–196
Cahill AM, Baskin KM, Kaye RD et al (2007) CT-Guided percutaneous steroid injection for management of inflammatory arthropathy of the temporomandibular joint in children. AJR 188:182–186
Raza K, Lee CY, Pilling D et al (2003) Ultrasound guidance allows accurate needle placement and aspiration from small joints in patients with early inflammatory arthritis. Rheumatology 42:976–979
Grassi W, Lamanna G, Farina A et al (1999) Synovitis of small joints: sonography guided diagnostic and therapeutic approach. Ann Rheum Dis 58:595–597
Landes C, Walendzik H, Klein C (2000) Sonography of the temporomandibular joint from 60 examinations and comparison with MRI and axiography. J Craniomaxillofacial Surg 28:352–361
Patonay L, Nagy K, Engelke W (2002) Real-time endoarticular ultrasound imaging of the TMJ—a new diagnostic possibility? A cadaver study. Int J Oral Maxillofac Surg 31:553–557
SIR Quality Improvement Documents (2003) Quality improvement guidelines for the reporting and archiving of interventional radiology procedures. J Vasc Interv Radiol 14:S293–S295
Arabshahi B, Cron R (2006) Temporomandibular joint arthritis in juvenile idiopathic arthritis: the forgotten joint. Curr Opin Rheumatol 18:490–495
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parra, D.A., Chan, M., Krishnamurthy, G. et al. Use and accuracy of US guidance for image-guided injections of the temporomandibular joints in children with arthritis. Pediatr Radiol 40, 1498–1504 (2010). https://doi.org/10.1007/s00247-010-1581-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-010-1581-2