Abstract
Background
MRI manifestation of temporomandibular joint arthritis is frequently reported in children with juvenile idiopathic arthritis. However, little attention has been paid to temporomandibular joint disk abnormalities.
Objective
To assess combinations of MRI findings in the symptomatic temporomandibular joint in children with juvenile idiopathic arthritis with focus on disk abnormalities.
Materials and methods
This was a retrospective study of 46 patients with juvenile idiopathic arthritis, mean age 12 years (range: 5-17 years). Mean disease duration was 70 months (standard deviation: 61 months). MR images of 92 temporomandibular joints were scored for thickness of abnormally enhancing synovium (synovitis), joint effusion, bone marrow oedema, abnormal bone shape, bone erosion and disk abnormalities.
Results
The 92 temporomandibular joints were categorized as A: No synovitis and normal bone shape (30/92; 33%), B: Synovitis and normal bone shape (14/92: 15%), C: Synovitis and abnormal bone shape (38/92; 41%) and D: No synovitis but abnormal bone shape (10/92; 11%). Thirty-six of the 46 patients (78%) had synovitis and 33/46 (72%) had abnormal bone shape, most frequently in combination (30/46; 65%). Disk abnormalities (flat disk, fragmented disk, adherent disk and displaced disk) were found in 29/46 patients (63%). Disk abnormalities were found in all categories of juvenile idiopathic arthritis involved temporomandibular joints (B: 8/14 [57%]; C: 25/38 [66%] and D: 7/10 [70%]). Disk displacement was found in half of the joints (7/14) in category B. Synovitis was most pronounced in this category.
Conclusion
Disk abnormalities were frequent. Disk displacement also occurred in joints with early temporomandibular joint arthritis, i.e., with normal bone shape. Other disk abnormalities were found in joints with bone abnormalities. Attention should be paid to disk abnormalities both in early and long-standing temporomandibular joint arthritis in children with juvenile idiopathic arthritis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Juvenile idiopathic arthritis is the most common juvenile inflammatory musculoskeletal disease and an important cause of short- and long-term disability. The incidence is reported to be about 15 in 100,000 children per year [1, 2] and the prevalence about 150 in 100,000 children [3, 4].
The temporomandibular joint is frequently involved in juvenile idiopathic arthritis. A longitudinal investigation of temporomandibular joint involvement and facial growth in consecutive patients with juvenile idiopathic arthritis with repeated examinations and a final 27-year follow-up (mean age: 35 years) showed MR imaging abnormalities in the temporomandibular joint consistent with juvenile idiopathic arthritis in 70% [5]. Using a similar protocol that was introduced in our hospital on adults with rheumatoid arthritis [6, 7], the present study will focus on temporomandibular joint abnormalities in symptomatic children with juvenile idiopathic arthritis.
The diagnostic assessment of arthritis, in general, seems to be more challenging in the growing child than in an adult [8]. The terminology and the definitions of pathologies as expressed by MR imaging are inconsistently used and reported. This could be one reason for the substantial variation in the frequency of temporomandibular joint involvement in two recent studies of consecutive children with a mean age of 9 and 11 years (43% and 96%, respectively) [9, 10]. It is also reflected in the recently proposed systems for grading temporomandibular joint arthritis in patients with juvenile idiopathic arthritis [11, 12] and in a pictorial essay [13]. A specific challenge is that the normal variations of MR imaging findings in the temporomandibular joint in children are not well-known. To our knowledge, only three studies of healthy temporomandibular joints are available [14–16].
Definitions of joint abnormalities in children with juvenile idiopathic arthritis seen on MR imaging are needed to distinguish pathology from the spectrum of normalcy and to compare observations reported in different studies. This is particularly important for the temporomandibular joint since the decision for treatment using site-specific targeted injections often is based on MR imaging signs of inflammation when the clinical symptoms are subtle [17].
Although a number of studies have demonstrated the various MR imaging abnormalities that may occur in the temporomandibular joint of patients with juvenile idiopathic arthritis, little attention has been given to disk abnormalities. In the majority of studies, disk abnormalities were not reported or not observed [10–12, 18–22], not even in the two largest series of 187 and 223 children [10, 22]. To our knowledge, only three studies have reported such abnormalities, two on children [9, 23] and one on adults with juvenile idiopathic arthritis [5]. In both studies on children, disk abnormalities predominantly occurred in joints with long-standing changes; the frequencies of abnormal bone shape were as high as 87% and 96% [9, 23]. In adult patients with juvenile idiopathic arthritis with long-standing temporomandibular joint arthritis, disk abnormalities were frequently observed [5]. Also, others have emphasized that disk abnormalities are late changes of temporomandibular joint arthritis in patients with juvenile idiopathic arthritis [12, 20]. It thus seems to be generally accepted that disk abnormalities occur late in temporomandibular joint arthritis. We have, however, during routine clinical work, occasionally encountered patients with disk abnormalities in joints with normal bone morphology, i.e., early in the disease process. Our hypothesis is, therefore, that disk abnormalities in the temporomandibular joint of patients with juvenile idiopathic arthritis not only may occur late but also early in the disease process.
We have used definitions of temporomandibular joint findings in juvenile idiopathic arthritis based on MR imaging observations in known juvenile idiopathic arthritis involved temporomandibular joints and in asymptomatic volunteers. The aim was to assess the occurrence of different combinations of MR imaging findings with special focus on disk abnormalities in symptomatic temporomandibular joints in children with juvenile idiopathic arthritis and relate these findings to previously reported observations in children and adults with juvenile idiopathic arthritis.
Materials and methods
This study was approved by the Data Protection Officer at our hospital, who represented the ethical committee in quality assurance studies. The material consisted of temporomandibular joint MR images of patients referred from the Department of Rheumatology at our hospital, during the period 2005-2012. The MR images were part of a retrospective study comparing US and MR imaging. Patients in the original study were all patients in our picture archiving and communication system who had MRI and US within 1 week. The results of that study will be reported elsewhere. In all patients, the reasons for referral were symptoms or clinical findings suspicious of temporomandibular joint arthritis. Twenty-eight patients had painful joints and 27 had restricted mouth opening, separately or in combination. Facial growth disturbances and joints sounds were also registered, although not systematically. Forty-six patients were included. Each patient had one MR examination.
Chart reviews were performed, and only patients classified according to the criteria of the International League of Associations for Rheumatology (ILAR) [24] were included. Laboratory tests, the number of active joints and medications were registered. Assessments of active joints were done using 71 joint scores where active joints were defined as swollen joints, or mobility restricted plus tender or painful joints [25].
All MR images were obtained on 1.5-T units (Magnetom Avanto, Magnetom Symphony or Magnetom Sonata; Siemens, Erlangen, Germany) with either surface coils or phased array head coil. Examinations were performed according to our routine protocol. Pre-contrast oblique sagittal T1-weighted (TR: 400-471 ms, TE: 12-15 ms) spin echo, and oblique sagittal PD/T2-weighted (TR: 2,080-3,090 ms, TE: 14-16/82-98 ms) turbo spin echo (TSE) images with or without fat suppression (frequency-selective saturation), and then post-contrast oblique sagittal and oblique coronal T1-weighed images with or without fat suppression (frequency-selective saturation) were obtained with closed mouth. Post-contrast oblique sagittal T2*-weighted gradient echo images (TR: 125-133 ms, TE: 10.8-11.0 ms, flip angle: 30°) with open mouth with the use of an occlusal step wedge were also obtained. The slice thickness was 3 mm. The in-plane resolution was 0.273 × 0.273 mm. The contrast media used were 0.1 mmol/kg of either gadopentetate dimeglumine (Magnevist; Bayer, Berlin, Germany) or, because the institution changed product, gadoterate meglumine (Dotarem; Guerbet, Paris, France). The post-contrast imaging started immediately after contrast medium injection. There were no sedations.
Two maxillofacial radiologists (T.A.L. and L.Z.A.) with 30 and 10 years of experience, respectively, in MR imaging and temporomandibular joint interpretation, aware of age and gender, analysed the MR images in consensus. Two months later, 25 cases were reassessed by the same two observers in consensus for evaluation of intraobserver variation. The data set was selected randomly and was not fully balanced but included all findings.
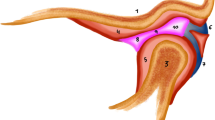
A normal joint has an oval mandibular condyle in the axial plane and a convex, round mandibular condyle that may be somewhat flat on reformatted oblique sagittal computed tomography (CT) images [26, 27]. In the oblique coronal plane, the condyle can be flat, convex, angled or round [28]. With conventional X-ray imaging, the mandibular fossa-eminence has been shown to be rather flat by birth, but during the first year becomes adult-like S-shaped [29]. A normal bone marrow has age-related symmetrical distribution of red and yellow marrow, with generally lower T1- and corresponding higher T2-weighted signal intensity in the immature compared to the mature skeleton [30], the highest T2-weighted signal intensity seen in the growth zone immediately beneath the fibrocartilaginous articular surface of the condyle [31]. The cortical bone plate begins to form around 12-14 years of age and is not fully developed until around the age of 20 [32, 33]. The disk is biconcave with its posterior band located on top of the condyle at closed mouth [34]. A disk that is partially displaced at closed mouth but normally located at the mouth opening is observed in about one-third of healthy volunteers [35]. Small amounts of joint fluid appear as dots or lines of high signal intensity along the articular surfaces on T2-weighted images in at least half of healthy individuals [16, 36]. Intravenous contrast medium enhancement in these dots and lines is considered a normal finding because of early leakage through the synovial membrane [7, 16].
MRI findings suggestive of synovitis, in the following referred to as synovitis, were defined as post-gadolinium enhancement (signal increase) in thickened synovium on T1-weighted images compared to pre-contrast T1-weighted images. The amount of synovitis was reported using a 1-3 grading scale: grade 1 (slight synovitis): slight synovial thickening more than dots or lines; grade 2 (moderate synovitis): moderate band-like thickening including slight distension of the joint space, and grade 3 (extensive synovitis): extensive thickening with extensive distension of the joint space. Effusion was defined as intra-articular fluid seen as more than dots or lines with high signal intensity on T2-weighted images and no contrast enhancement on T1-weighted images. Bone marrow oedema was defined as diffusely circumscribed areas in the mandibular condyle with low signal intensity on T1-weighted images and corresponding high signal intensity on T2-weighted images, typically higher signal intensity than that of red bone marrow, indicating increased water content. Bone erosion was defined as a sharply marginated bone lesion visible in more than one slice [37]. Irregular but intact articular surfaces were not considered erosions but abnormal bone shape. Erosion alone was not considered abnormal bone shape. A joint was considered to be involved by juvenile idiopathic arthritis when synovitis and/or abnormal bone shape was present on MR images.
Disks were registered as being absent, flat, ruptured/fragmented, displaced or adherent. The flat disk was either evenly thin or thin in the anterior band. The adherent disk was a disk that did not move normally together with the condyle at the mouth opening. A displaced disk could be located in an anterior, posterior, lateral or medial position relative to the condyle at closed mouth, reducing to normal position or being anteriorly displaced at the mouth opening [35].
Cohen kappa statistics for presence of synovitis and abnormal bone shape were performed to determine intraobserver consistency among the raters. Owing to small numbers, no intraobserver evaluations of the other variables were made. The continuous variables of age, age at disease onset and disease duration were normally distributed and described by mean and standard deviation. Categorical data were described as frequency and percentage. Odds ratio with 95% confidence interval (95% CI) was calculated in order to detect associations between patient characteristics and MR imaging suggestive of temporomandibular joint involvement. Significance level was set to P < 0.05. The statistical analyses were performed using IBM SPSS Statistics version 20.0 (IBM, Armonk, NY).
Results
The distribution of subtypes in 46 patients with juvenile idiopathic arthritis was systemic juvenile idiopathic arthritis (1/46, 2%); persistent oligoarthritis (18/46, 39%); extended oligoarthritis (1/46, 2%); polyarthritis rheumatoid factor negative (16/46, 35%); polyarthritis rheumatoid factor positive (5/46, 11%), psoriasis arthritis (1/46, 2%); enthesitis-related arthritis (2/46, 4%) and undifferentiated arthritis (2/46, 4%). The patient and disease characteristics at the time of the examinations are shown in Table 1. The following association between the characteristics and the MR imaging variables were statistically significant: Age at examination was higher in the 23 patients with bilateral temporomandibular joint involvement (synovitis and/or abnormal bone shape present on MR images) than in the 23 patients with unilateral or no temporomandibular joint involvement (odds ratio 1.26 [95% CI 1.04, 1.53; P = 0.019]), and it was higher in the 12 patients with displaced disk than in the 34 patients without (odds ratio 1.79 [95% CI 1.23, 2.59; P = 0.002]). Age at disease onset (symptom debut) was higher in the 23 patients with bilateral temporomandibular joint involvement than in the 23 patients with unilateral or no temporomandibular joint involvement (odds ratio 1.21 [95% CI 1.04, 1.41; P = 0.012]), and it was higher in the 36 patients with temporomandibular joint synovitis than in the 10 patients without (odds ratio 1.29 [95% CI 1.02, 1.64; P = 0.034]).
Thirty-nine of 46 patients (85%) (92 joints) were found to have juvenile idiopathic arthritis-involved temporomandibular joints, of whom 23/39 (59%) had bilateral and 16/39 (41%) had unilateral involvement (Table 2). Thirty of 39 (77%) had synovitis and abnormal bone shape, 6/39 (15%) had synovitis and normal bone shape and 3/39 (8%) had no synovitis but abnormal bone shape. The corresponding figures for the total series of 46 patients were 65%, 13% and 7%. Thus, 36 of 46 patients (78%) showed temporomandibular joint synovitis and 33/46 (72%) showed abnormal bone shape. In the group of patients with synovitis and abnormal bone shape, one patient had synovitis and normal bone shape in one joint and abnormal bone shape without synovitis in the contralateral. Twenty-nine of 46 patients (63%) had disk abnormalities. In the 39 children with temporomandibular joint abnormality, the corresponding figure was 28/39 (71%).
The 92 temporomandibular joints in the 46 patients were categorized according to MR imaging findings: A: No synovitis and normal bone shape (30/92; 33%); B: Synovitis and normal bone shape (14/92; 15%) (Figs. 1 and 2), C: Synovitis and abnormal bone shape (38/92; 41%) (Figs. 3 and 4), and D: No synovitis but abnormal bone shape (10/92; 11%) (Fig. 5).
Temporomandibular joint arthritis (category B: synovitis, normal bone shape) in a 15-year-old girl with juvenile idiopathic arthritis. Non-enhanced (a) and contrast-enhanced (b) oblique sagittal T1-weighted images show moderate synovial thickening (grade 2 synovitis) (thick arrows in b) and anterior disk displacement (thin arrow in a, b). Oblique sagittal T2*-weighted GRE image at open mouth (c) shows a non-reducing disk (arrow)
Temporomandibular joint arthritis (category B: synovitis, normal bone shape) in a 14-year-old girl with juvenile idiopathic arthritis. Oblique sagittal T2-weighted image with fat suppression (a), and non-enhanced oblique sagittal (b), contrast-enhanced oblique sagittal (c) and oblique coronal (d) T1-weighted images show non-enhancing fluid (open arrow in a, c), extensive synovial thickening (grade 3 synovitis) (thick arrows in c, d) and anterolateral disk displacement (thin arrow in c, d). Sagittal T2*-weighted GRE image at open mouth (e) shows a reducing disk (arrow)
Temporomandibular joint arthritis (category C: synovitis, abnormal bone shape) in a 9-year-old boy with juvenile idiopathic arthritis. Oblique sagittal T2-weighted image with fat suppression (a), and non-enhanced oblique sagittal (b), contrast-enhanced oblique sagittal (c) and oblique coronal (d) T1-weighted images show moderate synovial thickening (grade 2 synovitis) (thick arrows in c, d) and slight bone marrow oedema (asterisk in a) together with a deformed condyle. Oblique sagittal T2*-weighted GRE image at open mouth (e) shows reduced condylar translation with a non-moving (adherent) disk (arrow)
Temporomandibular joint arthritis (category C: synovitis, abnormal bone shape) in a 15-year-old girl with juvenile idiopathic arthritis. Oblique sagittal T2-weighted image with fat suppression (a), and non-enhanced oblique sagittal (b), contrast-enhanced oblique sagittal (c) and oblique coronal (d) T1-weighted images show moderate synovial thickening (grade 2 synovitis) (thick arrows in c, d) and erosions together with a deformed condyle. The slightly flat disk is anteromedially displaced (thin arrow in c, d). Oblique sagittal T2*-weighted GRE image at open mouth (e) shows a reducing disk (arrow)
Temporomandibular joint arthritis (category D: no synovitis but abnormal bone shape) in a 12-year-old girl with juvenile idiopathic arthritis. Non-enhanced oblique sagittal (a), and contrast-enhanced oblique sagittal (b) and oblique coronal (c) T1-weighted images show no synovial contrast enhancement but deformed condyle (c in a, b, c) and fossa/eminence
In category B (14 joints), the synovial thickening was slight, moderate or extensive, rather equally distributed. In category C (38 joints), the synovial thickening was predominantly slight or moderate (Table 3).
In 11/14 (79%) of the joints in category B, additional abnormalities were found: effusion in six and bone marrow oedema in three. Disk abnormalities were also frequent: seven joints showed anterior disk displacement, five without reduction (Tables 3 and 4).
In 30/38 (79%) of the joints in category C, additional abnormalities were found: effusion in 10 joints, bone marrow oedema in 8, and disk abnormalities in 25 joints, most frequently a flat disk (19 joints). Seven joints showed anterior disk displacement (Tables 3 and 4).
In category D (10 joints), additional imaging findings were recorded in 7/10 joints (70%): adherent disk in five and anterior disk displacement in three (Tables 3 and 4).
Of the total series of 92 joints (of which 62 were judged to have juvenile idiopathic arthritis involvement), synovitis was found in 52/92 (57%), abnormal bone shape in 48/92 (52%), effusion in 16/92 (17%) and bone marrow oedema in 11/92 (12%) (Table 3). Effusion and bone marrow oedema were always found in combination with synovitis, and thus only in categories B and C. Bone erosion was found in 9/92 joints (10%) and almost exclusively in category C. All joints with abnormal bone shape (categories C and D) showed abnormal condyle morphology with additional, flat fossa/eminence in about half. Disk abnormalities including displacements, 40/92 (44%) were found in all categories; the most frequent disk finding in category B being anterior disk displacement 7/14 (50%), in category C flat disk 19/38 (50%), and in category D adherent disk 5/10 (50%). The disks were only occasionally fragmented and never completely destroyed or absent.
Substantial intraobserver agreement was found with a к 0.79 (95% CI 0.64-0.94) for the detection of synovial thickening. There was almost perfect agreement with a к 0.89 (95% CI 0.75-1.00) for the detection of abnormal shape of the condyle.
Discussion
The most frequent observations were synovitis and abnormal bone shape in 78% and 72% of the 46 children, respectively. A large proportion of patients (65%) had combined synovitis and abnormal bone shape. The majority also had additional joint findings, in particular, disk abnormalities.
A flat disk was the most frequent disk abnormality, followed by a displaced disk and an adherent disk. In patients with a rheumatic disease, a flat disk in the temporomandibular joint was observed for the first time in adult rheumatoid arthritis [6] and later confirmed in patients with juvenile idiopathic arthritis with long-standing temporomandibular joint arthritis [5, 9, 23].
The displacement of the disk was a particularly interesting finding in the present study as it was observed in half of the 14 joints with normal bone shape and synovitis. The occurrence in joints with early signs of juvenile idiopathic arthritis has, to our knowledge, not been reported before. On the contrary, it was recently stated that disk displacement is a sign of chronic, long-standing disease [12], in accordance with the study by Müller et al. [20]. A similar statement was made almost 20 years ago by Taylor et al. [23], with reference to a case report of adult rheumatic temporomandibular joint disease, followed longitudinally for 15 months with MR imaging [38]. The development of an anterior disk displacement was observed, probably due to destruction of the posterior disk attachment. From the present study, we learned that disk displacement also may be an early finding in children with juvenile idiopathic arthritis with temporomandibular joint arthritis. Both in children and adults with juvenile idiopathic arthritis, the temporomandibular joint arthritis may be completely asymptomatic [5, 39, 40]. We also know that disk displacement may occur without symptoms, both in children and in adults [35, 41]. From the present study, one can speculate whether a combination of the two conditions is particularly symptomatic. It should be mentioned that non-reducing disk displacements like the ones that were found in the present study are not found among asymptomatic volunteers [35].
Patients with juvenile idiopathic arthritis and disk displacement and normal bone may represent a differential diagnostic problem. Also non-rheumatic patients with disk displacement and normal bone may have synovitis [7, 42, 43]. In such cases, there are actually no imaging differences between rheumatic and non-rheumatic patients. Due to the extensive synovitis and effusion in the seven joints with disk displacement in group B in the present study, and due to the much higher frequency of disk displacement than in healthy temporomandibular joints in children [16], we consider these joints to have juvenile idiopathic arthritis involvement.
A flat disk was most frequently found in category C, which represents a more severe temporomandibular joint involvement than category B. An adherent disk dominated in category D, which represents a stage with joint abnormalities but no active inflammation. In adult patients with juvenile idiopathic arthritis and really long-standing temporomandibular joint arthritis, ruptured, fragmented or absent disks were seen in 63% of the involved temporomandibular joints [5]. In the present series of children, no absent disks were observed. In the two previous studies on children with long-standing temporomandibular joint arthritis, completely destroyed disks were occasionally seen [9, 23].
The frequent findings of disk abnormalities, including disk displacement in the present study, suggest that the disk is vulnerable to the disease from early on, and that the severity of the disk abnormalities seems to increase during the course of the disease.
In the present series, 14 joints showed synovitis and normal bone shape (category B) with extensive thickening of the synovium in about one-third. Effusion and bone marrow oedema were seen in almost one-half and in about one-fifth of these joints, respectively. Thus, the inflammation seems to be more pronounced in this category. Synovitis without bone abnormality is rarely demonstrated convincingly by imaging in previous studies [9–12, 19, 40].
Synovitis was demonstrated in 78% of the patients. However, synovial contrast enhancement has also been reported in individuals with healthy temporomandibular joints [7, 14–16]. We therefore defined synovitis as post-Gd enhancement on T1-weighted images when the enhancement was of a thickness greater than dots or lines. This is in accordance with the studies by Müller et al. [20] and by Abramowicz et al. [9] and with the general definition of synovitis in Outcome Measures in Rheumatology Clinical Trials studies [37].
Joint effusion was found in 33% of the present patients, supporting some studies on children with juvenile idiopathic arthritis [9, 10, 20, 44], but not others with much higher frequencies [35, 36]. In the present study, effusion always occurred in combination with synovitis.
Small amounts of fluid may be hard to distinguish from synovial thickening although fluid has a slightly higher T2 signal and should be interpreted with caution, in particular if occurring as the only sign suggesting pathology. In individuals with healthy temporomandibular joints, small amounts of fluid are common [16, 36].
Bone marrow oedema of the condyle was infrequently seen, roughly in accordance with Abramowicz et al. [9]. In other studies, marrow oedema is not observed or not reported [10, 18, 19, 23]. In the present study, it only occurred in combination with synovitis, indicating more active inflammation.
In adult patients with juvenile idiopathic arthritis, temporomandibular joint synovitis was less frequent (42%), and only observed as slight to moderate contrast enhancement [5]. Besides, effusions and marrow oedemas were almost nonexistent, indicating less active inflammation in adults than in children. One should note that the adults were not selected based on symptoms [5].
Also in previous studies on children with juvenile idiopathic arthritis, temporomandibular joint synovitis is frequently combined with bone involvement. One study in particular emphasized that involved temporomandibular joints typically present with more than one abnormal finding [9]. The present study is in accordance with this since two-thirds of the involved temporomandibular joints showed more than two abnormal findings.
Abnormal bone shape was a frequent observation whereas bone erosion was not. Besides various degrees of flat articular eminence/fossa in half of the joints, various degrees of flat condyle or other condylar deformations were consistently seen. The condylar articular surface with or without a cortical delineation was usually intact. Such changes could be interpreted as local (intra-articular) growth disturbances due to inflammation, or even healed destructive processes, as discussed by Arvidsson et al. [5].
The bone surface assessed by MR imaging should be interpreted with caution since studies have shown that this modality is inferior to CT [45]. Besides, the condylar cortex does not begin to form until adolescence [32]. In healthy schoolchildren ages 9-14 years, 40% showed discontinuities of the condylar contour and this finding was most frequently seen in the youngest age groups [33].
Bone-productive changes (sclerosis, osteophytes) were rarely observed, in contrast to the 58% secondary osteoarthritis in adult patients with juvenile idiopathic arthritis with long-standing temporomandibular joint disease [5].
Interestingly, temporomandibular joint involvement was associated with a high onset age in accordance with the study by Stoll et al. [10] but in contrast to most other studies.
A limitation of the present study is the small sample of patients from a single institution. One should therefore be careful to generalize the results. There was a lower frequency of oligoarthritis (about 41%) than in epidemiological studies [1]. Whereas the frequency of oligoarthritis and polyarthritis was almost equal, most studies on temporomandibular joint involvement in juvenile idiopathic arthritis clearly have more patients with oligoarthritis than polyarthritis [10, 22]. This suggests that our study group is representative for hospital-based patient groups, and comprises more patients with severe disease than population-based patient groups.
Conclusion
Synovitis was seen in 78% of the patients with temporomandibular joint symptoms, frequently with abnormal bone shape and disk abnormalities. A displaced disk in particular was found in joints with early temporomandibular joint arthritis, i.e., with normal bone shape. Other disk abnormalities were observed in later stages of the disease, i.e., with bone abnormalities. Longitudinal studies may elucidate the significance of the disk displacement.
References
Berntson L, Andersson Gäre B, Fasth A et al (2003) Incidence of juvenile idiopathic arthritis in the Nordic countries. A population based study with special reference to the validity of the ILAR and EULAR criteria. J Rheumatol 30:2275–2282
Riise ØR, Handeland KS, Cvancarova M et al (2008) Incidence and characteristics of arthritis in Norwegian children: a population-based study. Pediatrics 121:e299–e306
Moe N, Rygg M (1998) Epidemiology of juvenile chronic arthritis in northern Norway: a ten-year retrospective study. Clin Exp Rheumatol 16:99–101
Ravelli A, Martini A (2007) Juvenile idiopathic arthritis. Lancet (Lond) 369:767–778
Arvidsson L, Smith H-J, Flatø B et al (2010) Temporomandibular joint findings in adults with long-standing juvenile idiopathic arthritis: CT and MR imaging assessment. Radiology 256:191–200
Larheim TA, Smith HJ, Aspestrand F (1990) Rheumatic disease of the temporomandibular joint: MR imaging and tomographic manifestations. Radiology 175:527–531
Smith HJ, Larheim TA, Aspestrand F (1992) Rheumatic and nonrheumatic disease in the temporomandibular joint: gadolinium-enhanced MR imaging. Radiology 185:229–234
Damasio MB, Malattia C, Martini A et al (2010) Synovial and inflammatory diseases in childhood: role of new imaging modalities in the assessment of patients with juvenile idiopathic arthritis. Pediatr Radiol 40:985–998
Abramowicz S, Cheon J-E, Kim S et al (2011) Magnetic resonance imaging of temporomandibular joints in children with arthritis. J Oral Maxillofac Surg 69:2321–2328
Stoll M, Sharpe T, Beukelman T et al (2012) Risk factors for temporomandibular joint arthritis in children with juvenile idiopathic arthritis. J Rheumatol 39:1880–1887
Koos B, Twilt M, Kyank U et al (2014) Reliability of clinical symptoms in diagnosing temporomandibular joint arthritis in juvenile idiopathic arthritis. J Rheumatol 41:1871–1877
Vaid Y, Dunnavant FD, Royal S et al (2014) Imaging of the temporomandibular joint in juvenile idiopathic arthritis. Arthritis Care Res 66:47–54
Meyers A, Laor T (2013) Magnetic resonance imaging of the temporomandibular joint in children with juvenile idiopathic arthritis. Pediatr Radiol 43:1632–1641
Tzaribachev N, Fritz J, Horger M (2009) Spectrum of magnetic resonance imaging appearances of juvenile temporomandibular joints (TMJ) in non-rheumatic children. Acta Radiol 50:1182–1186
von Kalle T, Winkler P, Stuber T (2013) Contrast-enhanced MRI of normal temporomandibular joints in children--is there enhancement or not? Rheumatology 52:363–367
Kottke R, Saurenmann RK, Schneider MM et al (2014) Contrast-enhanced MRI of the temporomandibular joint: findings in children without juvenile idiopathic arthritis. Acta Radiol 59:1145–1152
Cahill AM, Baskin KM, Kaye RD et al (2007) CT-guided percutaneous steroid injection for management of inflammatory arthropathy of the temporomandibular joint in children. AJR Am J Roentgenol 188:182–186
Kuseler A, Pedersen TK, Herlin T et al (1998) Contrast enhanced magnetic resonance imaging as a method to diagnose early inflammatory changes in the temporomandibular joint in children with juvenile chronic arthritis. J Rheumatol 25:1406–1412
Weiss PF, Arabshahi B, Johnson A et al (2008) High prevalence of temporomandibular joint arthritis at disease onset in children with juvenile idiopathic arthritis, as detected by magnetic resonance imaging but not by ultrasound. Arthritis Rheum 58:1189–1196
Müller L, Kellenberger CJ, Cannizzaro E et al (2009) Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: a pilot study comparing clinical examination and ultrasound to magnetic resonance imaging. Rheumatology 48:680–685
Argyropoulou MI, Margariti PN, Karali A et al (2009) Temporomandibular joint involvement in juvenile idiopathic arthritis: clinical predictors of magnetic resonance imaging signs. Eur Radiol 19:693–700
Cannizzaro E, Schroeder S, Muller LM et al (2011) Temporomandibular joint involvement in children with juvenile idiopathic arthritis. J Rheumatol 38:510–515
Taylor DB, Babyn P, Blaser S et al (1993) MR evaluation of the temporomandibular joint in juvenile rheumatoid arthritis. J Comput Assist Tomogr 17:449–454
Petty R, Southwood T, Manners P et al (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31:390–392
Giannini EH, Ruperto N, Ravelli A et al (1997) Preliminary definition of improvement in juvenile arthritis. Arthritis Rheum 40:1202–1209
Brooks SL, Westesson PL, Eriksson L et al (1992) Prevalence of osseous changes in the temporomandibular joint of asymptomatic persons without internal derangement. Oral Surg Oral Med Oral Pathol 73:118–122
Karlo CA, Stolzmann P, Habernig S et al (2010) Size, shape and age-related changes of the mandibular condyle during childhood. Eur Radiol 20:2512–2517
Yale SH, Allison BD, Hauptfuehrer JD (1966) An epidemiological assessment of mandibular condyle morphology. Oral Surg Oral Med Oral Pathol 21:169–177
Larheim TA (1981) Radiographic appearance of the normal temporomandibular joint in newborns and small children. Acta Radiol Diagn 22:593–599
Yamada M, Matsuzaka T, Uetani M et al (1995) Normal age-related conversion of bone marrow in the mandible: MR imaging findings. AJR Am J Roentgenol 165:1223–1228
Morimoto Y, Tominaga K, Konoo T et al (2004) Detection and significance of the characteristic magnetic resonance signals of mandibular condyles in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97:269–275
Lei J, Liu MQ, Yap AU et al (2013) Condylar subchondral formation of cortical bone in adolescents and young adults. Br J Oral Maxillofac Surg 51:63–68
Morimoto Y, Konoo T, Tominaga K et al (2007) Relationship between cortical bone formation on mandibular condyles and alternation of the magnetic resonance signals characteristic of growth. Am J Orthod Dentofacial Orthop 131:473–480
Drace JE, Enzmann DR (1990) Defining the normal temporomandibular joint: closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology 177:67–71
Larheim TA, Westesson P, Sano T (2001) Temporomandibular joint disk displacement: comparison in asymptomatic volunteers and patients. Radiology 218:428–432
Larheim TA, Katzberg RW, Westesson PL et al (2001) MR evidence of temporomandibular joint fluid and condyle marrow alterations: occurrence in asymptomatic volunteers and symptomatic patients. Int J Oral Maxillofac Surg 30:113–117
Østergaard M, Peterfy C, Conaghan P et al (2003) OMERACT Rheumatoid Arthritis Magnetic Resonance Imaging Studies. Core set of MRI acquisitions, joint pathology definitions, and the OMERACT RA-MRI scoring system. J Rheumatol 30:1385–1386
Larheim TA, Smith HJ, Aspestrand F (1991) Rheumatic disease of temporomandibular joint with development of anterior disk displacement as revealed by magnetic resonance imaging. A case report. Oral Surg Oral Med Oral Pathol 71:246–249
Arabshahi B, Cron RQ (2006) Temporomandibular joint arthritis in juvenile idiopathic arthritis: the forgotten joint. Curr Opin Rheumatol 18:490–495
Ringold S, Cron RQ (2009) The temporomandibular joint in juvenile idiopathic arthritis: frequently used and frequently arthritic. Pediatr Rheumatol Online J 7:11
Tominaga K, Konoo T, Morimoto Y et al (2007) Changes in temporomandibular disc position during growth in young Japanese. Dentomaxillofac Radiol 36:397–401
Suenaga S, Hamamoto S, Kawano K et al (1996) Dynamic MR imaging of the temporomandibular joint in patients with arthrosis: relationship between contrast enhancement of the posterior disk attachment and joint pain. AJR Am J Roentgenol 166:1475–1481
Farina D, Bodin C, Gandolfi S et al (2009) TMJ disorders and pain: assessment by contrast-enhanced MRI. Eur J Radiol 70:25–30
Kuseler A, Pedersen T, Gelineck J et al (2005) A 2 year followup study of enhanced magnetic resonance imaging and clinical examination of the temporomandibular joint in children with juvenile idiopathic arthritis. J Rheumatol 32:162–169
Alkhader M, Ohbayashi N, Tetsumura A et al (2010) Diagnostic performance of magnetic resonance imaging for detecting osseous abnormalities of the temporomandibular joint and its correlation with cone beam computed tomography. Dentomaxillofac Radiol 39:270–276
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Kirkhus, E., Arvidsson, L.Z., Smith, HJ. et al. Disk abnormality coexists with any degree of synovial and osseous abnormality in the temporomandibular joints of children with juvenile idiopathic arthritis. Pediatr Radiol 46, 331–341 (2016). https://doi.org/10.1007/s00247-015-3493-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3493-7