Abstract
Metformin (MF) accumulation during acute kidney injury is associated with high anion gap lactic acidosis type B (MF-associated lactic acidosis, MALA), a serious medical condition leading to high mortality. Despite dose adjustment for renal failure, diabetic patients with chronic kidney disease (CKD) stage III–IV are at risk for rapid decline in renal function by whatever reason, so that MF toxicity might arise if the drug is not timely withdrawn. Sixteen consecutive patients were admitted to our Hospital’s Emergency Department with clinical findings consistent with MALA. Fifteen had prior history of CKD, 60 % of them with GFR between 30 and 60 ml/min. Of these, 5 required mechanical ventilation and cardiovascular support; 3 promptly recovered renal function after rehydration, whereas 10 (62 %) required continuous veno-venous renal replacement treatment. SOFA and SAPS II scores were significantly related to the degree of lactic acidosis. In addition, lactate levels were relevant to therapeutic choices, since they were higher in dialyzed patients than in those on conservative treatment (11.92 mmol/l vs 5.7 mmol/l, p = 0.03). The overall death rate has been 31 %, with poorer prognosis for worse acidemia, as serum pH was significantly lower in non-survivors (pH 6.96 vs 7.16, p > 0.04). Our own data and a review of the literature suggest that aged, hemodynamically frail patients, with several comorbidities and CKD, are at greater risk of MALA, despite MF dosage adjustment. Moreover, renal replacement therapy rather than simple acidosis correction by administration of alkali seems the treatment of choice, based on eventual renal recovery and overall outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metformin (dimethylbiguanide, MF) is a long-known oral hypoglycemic agent, increasingly used in recent years as a first-line therapy in Diabetes Mellitus (DM). Long-term treatment with MF results in better day-time glucose profile regulation with less risk of hypoglycemia, better adipose mass control, lower rates of cardiovascular disease and overall mortality [1–6]. MF decreases hepatic gluconeogenesis from lactate and enhances peripheral glucose uptake. Absorption occurs in the small intestine. It has negligible plasma protein binding and a large distribution volume (from 63 to 276 L). It undergoes virtually no hepatic metabolism and it is excreted by the kidney [7–9]. Consequently, it may accumulate during acute or chronic kidney injury (AKI/CKD), resulting in high anion gap lactic acidosis type B (MF-associated lactic acidosis, MALA), a rare but severe metabolic adverse effect (43 cases/100,000 patients/years) [10–14].
The mechanism by which MF increases blood lactate concentration is complex, with mitochondrial inhibition of the respiratory chain complex as a likely major player [7, 8]. MF promotes (i) the conversion of glucose to lactate by the intestinal mucosa, and (ii) blocks mitochondrial oxidative metabolism, decreasing hepatic gluconeogenesis from lactate, pyruvate and alanine; this, in turn, results in anaerobic glycolysis and lactate accumulation at concentrations relevant to clinical intoxication [7, 15, 16]. At variance with other biguanides, MF does not inhibit lactate oxidation and does not enhance lactate release from muscle. This may attenuate the risk of lactic acidosis upon MF accumulation due to reduced renal clearance [17].
MALA seems to occur in certain settings only. This has led to the development of exclusion criteria for its use in the management of DM, such as renal insufficiency, cardiopulmonary insufficiency, liver disease, sepsis, alcohol abuse, administration of i.v. radiographic contrast agents, and a previous history of lactic acidosis [5, 18–22].
In renal failure, strict biochemical parameters monitoring and adherence to dose adjustment are recommended by current treatment guidelines. As far as renal dysfunction is concerned, MF may be initiated or continued with eGFR <60 mL/min/1.73 m2, but renal function should be assessed at regular intervals (3–6 months). Doses should be reduced by 50 % in subjects with eGFR <45 mL/min/1.73 m2. MF should be stopped whenever eGFR drops below 30 mL/min/1.73 m2 [23–31].
This assumption is valid for steadily impaired renal function but, as a result of the combination of chronic kidney disease, diabetes and other traditional risk factors (elderly pts., inadequate fluid intake, marked volume losses obligated by the renal excretion of non-reabsorbable solutes in CKD), certain individuals are at particularly high risk of hemodynamic changes leading to sudden drops of GFR [32–34]. Therefore, it should be envisioned that in CKD stage 3–4 there is a risk for rapid, further decline in renal function and, consequently, MF may suddenly accumulate, leading to metabolic/lactic acidosis. In order to better clarify the clinical picture and outcomes of MALA, we retrospectively reviewed the charts of 16 consecutive patients admitted to our Hospital’s Emergency Dept. with clinical findings consistent with the diagnosis of MALA. Our experience is herein summarized in light of the vast literature that is rapidly accumulating as a result of the revival and widespread use of this old oral antidiabetic agent.
Patients and methods
All patients with MALA admitted to our Center over a 5-year period (from January 2009 to June 2014) were included in the present study, whenever matching the following inclusion criteria: history of type 2 DM in MF treatment, blood pH <7.3, serum HCO3 − <22 mEq/l, serum lactate >5 mmol/l. Survivors gave an informed consent to data collection as requested by the Institution’s Ethics Committee. Exclusion criteria were: self-administered overdose, lactic acidosis type A, diabetic ketoacidosis, tumor lysis syndrome, history of severe hepatic, respiratory and cardiac ins ufficiency (Table 1).
The study variables analyzed were: (1) demographic-anamnestic data (age, sex, pre-existing chronic kidney disease, cause of acute kidney injury (AKI), MF dose, other potentially nephrotoxic therapies); (2) laboratory data [basal serum creatinine and eGFR, biochemistry including serum glucose levels, anion gap and arterial blood gas analyses (ABG) at admission and discharge]; (3) biological parameters at admission (blood pressure, heart rate, body temperature, urine output, Glasgow Coma Scale); (4) illness severity scores of patients presenting to the Emergency Dept., including Sequential Organ Failure Assessment (SOFA) and Simplified Acute Physiology Score II (SAPS II), with the probability of death calculated for each patient based on these scores; (5) therapies; (6) outcomes.
Data analysis was performed using the PASW Statisitics 17 software for Windows. Univariate analysis was used to describe the sample characteristics. Simple linear regression analysis was used to determine strength and direction of the relationship between each dependent variable (SOFA score, SAPS II, baseline GFR) and each explanatory variable, all of which pre-HD (pCO2, lactates, pH, HCO3 −). Scatterplot graphs were created and Pearson’s correlation coefficients with the associated test of statistical significance were computed. Adjusted R square was used to calculate the proportion of variation in the dependent variable accounted by the explanatory variables. Multiple linear regression analysis was used to investigate the relationship between a set of predictor variables and a single dependent variable.
Results
We identified 16 consecutive type 2 diabetic patients with diagnosis of MALA (Tables 2, 3) within 24 h of admission to our Unit or the Emergency Dept. All patients presented with AKI following a prolonged episode of dehydration, with variable SOFA and SAPS II scores.
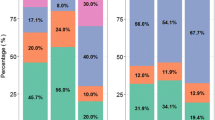
Prior to admission, the patients’ renal functional status—retrospectively assessed—ranged from normal kidney function to K/DOQI stage 5 chronic kidney disease (Table 4). Dosage of MF was properly adjusted except for 5 patients, which were otherwise on a stable medication regimen until the occurrence of a superimposed AKI and subsequent development of MALA. The clinical picture was generally more serious as a function of worsening renal dysfunction. Among all subjects with prior renal impairment (15 pts.), 60 % of them with GFR between 30 and 60 ml/min (Table 4). Acidosis in this group was more severe, with an average pH <7.0, HCO3 − <10 mEq/l and lactate >10 mmol/l.
SOFA and SAPS II scores, used to assess severity of comorbidities, were significantly influenced by all parameters linked to MALA (pH, HCO3 −, lactates: p < 0.01; as an example, SAPS II vs lactates is shown in Fig. 1). Patients were initially treated with iv fluid infusions, including administration of NaHCO3. Five patients required mechanical ventilation and cardiovascular support. Three promptly recovered renal function after rehydration, whereas 13 required renal replacement therapy, 77 % of whom treated with continuous veno-venous techniques. Serum lactate was an important benchmark for therapeutic choices: mean lactate concentration was significantly higher in dialyzed patients compared with those in conservative treatment (lactate 11.9 vs 5.7 mmol/l, p = 0.03, Table 5).
The overall death rate was 31 % (n = 5 patients, Table 6). There were no significant differences in demographic, biochemical and physical data for the group of patient who survived compared to those who died. The poor prognosis was primarily associated with the degree of acidemia, as shown by the threshold ABG results correlated with the hard outcome: n = 3 deaths out of 5 patients with pH <7.0, 3 out of 6 with lactate >10 mmol/l, and 3 out of 9 with HCO3 − <10 mEq/l. The magnitude of decrease in pH was, indeed, significantly greater in non-survivors (pH 6.96 vs 7.16, p < 0.04, Table 6).
Discussion
Lactic acidosis is a recognized adverse effect of MF treatment, with a modest overall incidence of 3–10 per 100,000 person-years [14, 20]. The range of reported incidence varies widely based on the general conditions and/or renal function of diabetic individuals receiving MF treatment. Of course, the possibility that MALA could occur unrecognized in a number of patients must not be discounted. Whenever strict criteria for withdrawal of MF (e.g. a cutoff of eGFR <30 ml/min) are met, the occurrence of MALA decreases below 5 per 100,000 person-years, which is not different from the rates observed with other oral antidiabetic agents. A series of Cochrane systematic reviews by Salpeter et al. has pooled some 347 studies encompassing 70,490 type 2 diabetic patient-years receiving MF treatment, without noting a single case of MALA. Of these, 43 % of patients were enrolled without evaluating renal function, so that the data should not be considered censored for renal failure [13, 19]. These figures, and the fact that MF levels in individuals with lactic acidosis have often been found normal or only slightly elevated, have led some Investigators to question the strength of this association [13, 35–37]. Moreover, even the relationship between MF serum levels and renal failure is uncertain. Despite the fact that MF is excreted unmodified mostly by the kidney, evidence that the drug accumulates to high levels in patients with acute kidney injury or CKD stages 4–5 is lacking [10, 13, 24, 26, 38]. Even though a review of 223,968 patients employing MF reported a higher hazard ratio for MALA whenever eGFR decreased below 60 mL/min, and even more so below 45 ml/min, the study suffered from several biases, including lack of renal data in 25 % of the patients, younger average age and lactate measurements in the MF group only [24]. Another analysis on the same database yielded a trend in increasing incidence ratio of MALA among individuals with impaired renal function, which was not statistically significant due to rarity of the event [38]. It should also be pointed out that severity of lactic acidosis is not directly proportional to MF serum levels, with some critical patients exhibiting only mild MF accumulation [33]. Other factors are evidently implicated in lactic acidosis, consistent with a number of known causes of the A, B1, B2, and B3 subtypes of this metabolic derangement. On the other hand, severity of lactic acidosis is clearly linked to a worse clinical condition and prognosis, as also shown by our series.
Nevertheless, MALA is a severe condition with poor prognosis in the absence of immediate treatment [30, 31, 39, 40]. Because administration of MF is associated with a lower incidence of cardiovascular events and mortality, several regulatory Agencies and Authorities advocated in recent years a less restrictive use of this agent, provided that dose reduction was granted on the basis of eGFR, according to current guidelines [41–45]. However, this assumption takes into account mostly subjects with stable renal impairment. In fact, we herein noted once more how renal function may suddenly decline significantly as a consequence of effective circulatory volume or renal hemodynamics in patients with CKD. As a matter of fact, in 100 % of our patients MALA was associated with prerenal AKI superimposed to an underlying CKD.
The onset of MALA is associated with worsening general health conditions, as evaluated with SOFA and SAPS II scores. Severity of comorbidities is strictly connected to ABGs: our study underlines a significant correlation between illness severity, serum HCO3 − and lactate levels. Likewise, these changes are also critical for the selection of therapeutic options [46–49].
In our series, intensive management in the Emergency Dept. upon admission usually included intravenous fluid and NaHCO3 − administration, vital function support (5 pts required mechanical ventilation and cardiovascular support), HD in selected cases, and treatment of underlying conditions [50–52]. A conservative treatment was recommended by our consultant Nephrologists in 19 % of cases (average pH 7.31, HCO3 − 16.0 mEq/l, lactate 5.3 mmol/l, SOFA score 4, SAPS II 47.67). In these patients, i.v. rehydration therapy led to rapid GFR recovery and parallel reduction of serum lactate levels.
In most critically ill patients (81 %) with severe multiorgan damage and hemodynamic instability (pH 7.06, HCO3 − 8.87 mEq/l, lactate 10.34 mmol/l, SOFA 7.7, SAPS II 63.31), MALA required management by continuous renal replacement therapy (CRRT, 49). Goals of resuscitation in severe metabolic acidosis include maintenance of CVP >8 mmHg, ScvO2 >70 % and normalization of lactate, while NaHCO3 administration remains controversial [48]. Most current guidelines do not recommend administration of NaHCO3 in patients with lesser degrees of lactic acidosis (i.e., pH >7.1), since prompt correction of acidosis may remove any obstacle to anaerobic glycolysis and hence actually promote lactate accumulation and further intracellular acidification [49, 50]. Intracellular acidosis itself is actually a powerful inhibitor of lactate generation [49]. Moreover, NaHCO3 promotes CO2 accumulation through dehydration of H2CO3 resulting from combination of H+ and HCO3 −. In the absence of sufficient CO2 elimination, NaHCO3 exacerbates intracellular CO2 influx, paradoxically leading to intracellular acidification. Furthermore, intracellular acidification due to accumulation of CO2 after NaHCO3 infusion brings about a pH-dependent decrease in levels of [Ca2+]i, a modulator of cardiac contractility. Additional risks of NaHCO3 administration include increased plasma CO2, hyperosmolality, hypernatremia, volume overload, and pH overcorrection, resulting in metabolic alkalosis [48]. This increases the need for respiratory assistance in these subjects. Overall, HD is an efficient method of drug removal and acidosis correction, particularly in critically ill patients [51, 52]. In survivors (69 %), gradual improvement in all AB variables has been observed. At the other hand of the spectrum, worsening of acidosis portends a less favourable prognosis. It has been actually shown that late-referral patients, with a higher degree of acidemia at the time of admission, have a worse prognosis compared to earlier identified cases. Based on our series, it seems fair to conclude that aged, hemodynamically frail patients, with several comorbidities and renal impairment from moderate to severe, are at greater risk of MALA, despite dosage adjustment. The most serious the threat, with high lactate and low HCO3 − levels, the worse was the clinical outcome.
In conclusion, while data in the literature seem to support an “MF to all, all the time” paradigm, our report suggests a more careful approach, particularly among patients with CKD stage 3–4 who may have serious clinical conditions predisposing to AKI. It seems sensible to withdraw MF whenever subjects at risk of abrupt worsening of renal function are identified through frequent monitoring of eGFR and other hemodynamic parameters, switching to other oral antidiabetic agents or insulin whenever unstable clinical conditions are detected. Moreover, early detection of any acid–base imbalance not solely explained by renal failure (i.e., high anion gap acidosis) should prompt the search for elevated serum lactate levels, and raise concerns about routine alkali administration.
References
Oulahiane A, Anaddam S, Ouleghzal H et al (2012) Diabetes management issues for patients with chronic kidney disease. Nephrol Ther 8:135–140. doi:10.1016/j.nephro.2011.07.410 (Epub 2011 Oct 20)
NICE (2009) Type 2 diabetes: the management of type 2 diabetes. NICE guideline CG87. http://www.nice.org.uk/guidance/cg87/chapter/guidance
Inzucchi SE, Bergenstal RM, Buse JB et al (2012) Management of hyperglycemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 35:1364–1379. doi:10.2337/dc12-0413 (Epub 2012 Apr 19)
Lipska KJ, Bailey CJ, Inzucchi SE (2011) Use of metformin in the setting of mild-to-moderate renal insufficiency. Diabetes Care 34:1431–1437. doi:10.2337/dc10-2361
Nathan DM, Buse JB, Davidson MB (2006) Management of hyperglycaemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. A Consensus Statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia 49:1711–1721
(2014) Standards of medical care in diabetes. Diabetes Care 37 Suppl 1:S14–S80. doi:10.2337/dc14-S014
Viollet B, Guigas B, Sanz Garcia N et al (2012) Cellular and molecular mechanisms of metformin: an overview. Clin Sci (Lond) 122:253–270. doi:10.1042/CS20110386
Bailey CJ, Turner RC (1996) Metformin. N Engl J Med 334:574–579
Duong JK, Kumar SS, Kirkpatrick CM et al (2013) Population pharmacokinetics of metformin in healthy subjects and patients with type 2 diabetes mellitus: simulation of doses according to renal function. Clin Pharmacokinet 52:373–384. doi:10.1007/s40262-013-0046-9
Vecchio S, Giampreti A, Petrolini VM et al (2014) Metformin accumulation: lactic acidosis and high plasmatic metformin levels in a retrospective case series of 66 patients on chronic therapy. Clin Toxicol (Phila) 52:129–135. doi:10.3109/15563650.2013.860985 (Epub 2013 Nov 28)
Kajbaf F, Lalau JD (2014) Mortality rate in so-called “metformin-associated lactic acidosis”: a review of the data since the 1960s. Pharmacoepidemiol Drug Saf 23:1123–1127. doi:10.1002/pds.3689 (Epub 2014 Jul 31)
Pasquel FJ, Klein R, Adigweme A (2015) Metformin-associated lactic acidosis. Am J Me Sci 349:263–267. doi:10.1097/MAJ.0b013e3182a562b7
Salpeter SR, Greyber E, Pasternak GA et al (2010) Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev. doi:10.1002/14651858.CD002967.pub3
Shaw JS, Wilmot RL, Kilpatrick ES (2007) Establishing pragmatic estimated GFR thresholds to guide metformin prescribing. Diabet Med 24:1160–1163
Foretz M, Guigas B, Bertrand L et al (2014) Metformin: from mechanisms of action to therapies. Cell Metab 20:953–966. doi:10.1016/j.cmet.2014.09.018 (Epub 2014 Oct 30)
Sliwinska A, Drzewoski J (2015) Molecular action of metformin in hepatocytes: an updated insight. Curr Diabetes Rev 11:175–181
Pernicova I, Korbonits M (2014) Metformin—mode of action and clinicla implications for diabetes and cancer. Nat Rev Endocrinol 10:143–156. doi:10.1038/nrendo.2013.256 (Epub 2014 Jan 7)
Sulkin TV, Bosman D, Krentz AJ (1997) Contraindications to metformin therapy in patients with NIDDM. Diabetes Care 20:925–928
Inzucchi SE, Lipska KJ, Mayo H et al (2014) Metformin in patients with type 2 diabetes and kidney disease: a systematic review. JAMA 312:2668–2675. doi:10.1001/jama.2014.15298
Hung SC, Chang YK, Liu JS et al (2015) Metformin use and mortality in patients with advanced chronic kidney disease: national, retrospective, observational, cohort study. Lancet Diabetes Endocrinol 3:605–614. doi:10.1016/S2213-8587(15)00123-0 (Epub 2015 Jun 17)
Makehei S, Sam R (2015) Does lactate account for all of the increase in anion gap in cases of metformin-induced lactic acidosis? Clin Exp Nephrol 19:1210–1211. doi:10.1007/s10157-015-1124-0 (Epub 2015 May 16)
Suh S (2015) Metformin-associated lactic acidosis. Endocrinol Metab (Seoul) 30:45–46. doi:10.3803/EnM.2015.30.1.45
Adam WR, O’Brien RC (2014) A justification for less restrictive guidelines on the use of metformin in stable chronic renal failure. Diabet Med 31:1032–1038. doi:10.1111/dme.12515
Eppenga WL, Lalmohamed A, Geerts AF et al (2014) Risk of lactic acidosis or elevated lactate concentrations in metformin users with renal impairment: a population-based cohort study. Diabetes Care 37:2218–2224. doi:10.2337/dc13-3023 (Epub 2014 May 19)
Heaf J (2014) Metformin in chronic kidney disease: time for a rethink. Perit Dial Int 34:353–357. doi:10.3747/pdi.2013.00344 (Epub 2014 Apr 7)
Lalau JD, Arnouts P, Sharif A (2015) Metformin and other antidiabetic agents in renal failure patients. Kidney Int 87:308–322. doi:10.1038/ki.2014.19 (Epub 2014 Mar 5)
Huang W, Castelino RL, Peterson GM (2014) Metformin usage in type 2 diabetes mellitus: Are safety guidelines adhered to? Intern Med J 44:266–272. doi:10.1111/imj.12369
Lu WR, Defilippi J, Braun A (2013) Unleash metformin: reconsideration of the contraindication in patients with renal impairment. Ann Pharmacother 47:1488–1497. doi:10.1177/1060028013505428 (Epub 2013 Oct 10)
Sambol NC, Chiang J, Lin ET, Goodman AM et al (1995) Kidney function and age are both predictors of pharmacokinetics of metformin. J Clin Pharmacol 35:1094–1102
Emslie-Smith AM, Boyle DIR, Evans JMM et al (2001) Contraindications to metformin therapy in patients with type 2 diabetes—a population-based study of adherence to prescribing guidelines. Diabet Med 18:483–488
Scheen AJ (2015) Metformin should not be contraindicated in patients with type 2 diabetes and mild to moderate renal impairment. Evid Based Med 20:115. doi:10.1136/ebmed-2015-110184 (Epub 2015 Mar 31)
Kim MJ, Han JY, Shin JY et al (2015) Metformin-associated lactic acidosis: predisposing factors and outcome. Endocrinol Metab (Seoul) 30:78–83. doi:10.3803/EnM.2015.30.1.78 (Epub 2014 Jul 18)
Lalau JD, Lacroix C, Compagnon P et al (1995) Role of metformin accumulation in metformin-associated lactic acidosis. Diabetes Care 18:779–784
Kajbaf F, Bennis Y, Hurtel-Lemaire AS, Andréjak M, Lalau JD (2015) Unexpectedly long half-life of metformin elimination in cases of metformin accumulation. Diabet Med. doi:10.1111/dme.12959 (Epub ahead of print)
Juurlink DN, Roberts DM (2014) The enigma of metformin-associated lactic acidosis. Clin Toxicol (Phila) 52:85–87. doi:10.3109/15563650.2014.880174
Almirall J, Briculle M et al (2008) Metformin-associated lactic acidosis in type 2 diabetes mellitus: incidence and presentation in common clinical practice. Nephrol Dial Transplant 23:2436–2438. doi:10.1093/ndt/gfn152 (Epub 2008 Apr 3)
McNamara K, Isbister GK (2015) Hyperlactataemia and clinical severity of acute metformin overdose. Intern Med J 45:402–408. doi:10.1111/imj.12713
Richy FF, Sabidó-Espin M, Guedes S, Corvino FA, Gottwald-Hostalek U (2014) Incidence of lactic acidosis in patients with type 2 diabetes with and without renal impairment treated with metformin: a retrospective cohort study. Diabetes Care 37:2291–2295. doi:10.2337/dc14-0464 (Epub 2014 May 30)
Lalau JD, Kajbaf F (2014) Interpreting the consequences of metformin accumulation in an emergency context: impact of the time frame on the blood metformin levels. Int J Endocrinol 2014:717198. doi:10.1155/2014/717198 (Epub 2014 Dec 17)
Salpeter SR, Greyber E, Pasternak GA, Salpeter EE (2003) Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus: systematic review and meta-analysis. Arch Intern Med 163:2594–2602
Kajbaf F, Arnouts P, de Broe M (2013) Metformin therapy and kidney disease: a review of guidelines and proposals for metformin withdrawal around the world. Pharmacoepidemiol Drug Saf 22:1027–1035. doi:10.1002/pds.3501 (Epub 2013 Aug 19)
Scheen AJ, Paquot N (2013) Metformin revisited: a critical review of the benefit-risk balance in at-risk patients with type 2 diabetes. Diabetes Metab 39:179–190. doi:10.1016/j.diabet.2013.02.006 (Epub 2013 Mar 23)
Petrie MC, Boyle JG, McKay GA (2015) Use of metformin in chronic kidney disease should continue to be based on common sense in the absence of an evidence base. Diabet Med 32:981–982. doi:10.1111/dme.12709
Mathieu C (2015) Metformin-associated lactic acidosis: time to let it go? J Diabetes Complications. doi:10.1016/j.jdiacomp.2015.07.022 (Epub ahead of print)
Stanton RC (2015) Metformin use in type 2 diabetes mellitus with CKD: Is it time to liberalize dosing recommendations? Am J Kidney Dis 66:193–195. doi:10.1053/j.ajkd.2015.04.001 (Epub 2015 May 8)
Kajbaf F, Lalau JD (2013) The prognostic value of blood pH and lactate and metformin concentrations in severe metformin-associated lactic acidosis. BMC Pharmacol Toxicol 14:22. doi:10.1186/2050-6511-14-22
Kraut JA, Madias NE (2014) Lactic acidosis. N Engl J Med 371:2309–2319. doi:10.1056/NEJMra1309483
Velissaris D, Karamouzos V, Ktenopoulos N et al (2015) The use of sodium bicarbonate in the treatment of acidosis in sepsis: a literature update on a long term debate. Crit Care Res Pract 2015:605830. doi:10.1155/2015/605830 (Epub 2015 Jul 30)
Adeva-Andany M, López-Ojén M, Funcasta-Calderón R et al (2014) Comprehensive review on lactate metabolism in human health. Mitochondrion 17:76–100. doi:10.1016/j.mito.2014.05.007 (Epub 2014 Jun 12)
Calello DP, Liu KD, Wiegand TJ et al (2015) Extracorporeal treatment for metformin poisoning: systematic review and recommendations from the Extracorporeal Treatments in Poisoning Workgroup. Crit Care Med 43:1716–1730. doi:10.1097/CCM.0000000000001002
Lebiedz P, Knickel L, Engelbertz C et al (2014) Impact of preexisting chronic kidney disease on acute and long-term outcome of critically ill patients on a medical intensive care unit. J Nephrol 27(1):73–80. doi:10.1007/s40620-013-0016-1 (Epub 2013 Dec 7)
Thongprayoon C, Cheungpasitporn W, Srivali N et al (2015) The impact of fluid balance on diagnosis, staging and prediction of mortality in critically ill patients with acute kidney injury. J Nephrol (Epub ahead of print) PMID: 26012379
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The manuscript has not been submitted to more than one journal for simultaneous consideration. The manuscript has not been published previously (partly or in full). The study is not split up into several parts to increase the quantity of submissions and submitted to various journals or to one journal over time. No data, text, or theories by others are presented as if they were the author’s own.
Informed consent
As this is a retrospective study formal consent is not required, nor identifying information concerning any individual patient is included in this article.
Rights and permissions
About this article
Cite this article
Moioli, A., Maresca, B., Manzione, A. et al. Metformin associated lactic acidosis (MALA): clinical profiling and management. J Nephrol 29, 783–789 (2016). https://doi.org/10.1007/s40620-016-0267-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-016-0267-8