Abstract
Purpose
Iodine plays a pivotal role in adaptation during the transition from intrauterine to extrauterine life. Although it is well known that the placenta plays a role in iodine storage, a relationship between the neonatal thyroid stimulating hormone (TSH) peak and placental iodine concentration has not been established. This study focuses on the role of placental iodine concentration in the TSH surge after delivery.
Materials and methods
This study included 42 mothers and their newborns, none of whom had perinatal risk factors. The following samples were collected to analyze iodine: placental tissue, amniotic fluid (AF), and 24-h maternal urine. Blood was drawn from the umbilical cord (uc), newborns (at the 1st–24th hours), and mothers (at 1st hour) to analyze the following hormones: TSH, freeT4/T3(fT4/fT3), human chorionic gonadotrophin (hCG), prolactin (PRL), follicle stimulating hormone (FSH), luteinizing hormone (LH), and cortisol.
Results
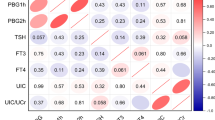
The mean iodine levels of placental tissue, AF, and 24-h maternal urine were as follows: 29.06 ± 45.88 μg/kg, 182.80 ± 446.51 µg/L, and 498.35 ± 708.34 µg/L, respectively. The mean TSH and hCG values were 32.41 ± 13.96mIU/ml and 30.66 ± 18.55mIU/ml, respectively, at the 1st hour. Placental iodine had strong, very strong, and weak negative correlations with TSH, hCG, and PRL, respectively (rTSH = − 0.763, p < 0.001;rHCG = − 0.919, p < 0.001; rPRL = − 0.312, p = 0.044).
Conclusion
This study showed that the placental iodine level was inversely correlated with neonatal TSH, hCG, and PRL. It indicates that placental iodine concentration is an efficient driving force shaping the dynamic pattern of the neonatal TSH peak in addition to hCG and PRL surges, which reflects the adaptive effort in the transition from intrauterine to extrauterine life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The neonatal thyroid stimulating hormone (TSH) surge occurs immediately after birth. Thyroid hormones (TH) are master molecules that play a pivotal role in adaptation to ecological transitions and metamorphosis events through fast and effective responses to environmental signs [1]. One of the main tasks of THs is to store iodine [2]. As an iodine reservoir, THs play a critical role in the hormonal regulation of metabolic activities required to adapt during the transition from aquatic to terrestrial life. Ontogenetically, the neonatal TSH surge after delivery is an evolutionary trait, which reflects the adaptive effort of ecological transition [3].
Foetal TH synthesis undergoes dynamic changes during intrauterine life. During the first gestational weeks, placental hormones including human chorionic gonadotrophin (hCG) that has a thyrotropic (TSH stimulating) effect. TH synthesis and iodine supply, while fetal TSH begins to stimulate its downstream hormones in the second half of pregnancy [4]. Placenta, which is an interface between mother and fetus, not only plays a role in the uptake and transport of maternal iodine sources to the fetus, but is also the most important extrathyroidal iodine reservoir organ throughout the pregnancy [5]. The placenta also provides iodine regulation varying depending on the requirement of the developing fetus, who is extremely sensitive to iodine fluctuations. Therefore, fetal iodine regulation is associated with a functional placenta rather than maternal dietary iodine intake [6]. It has a compensatory role for the fetus as an iodine reservoir organ [5]. Postnatal iodine delivery to the newborn from the placenta is suddenly interrupted following the cutting of the umbilical cord.
After birth, neonatal TSH increases dramatically within minutes and decreases within days, physiologically. There are many well-known perinatal factors such as maternal age, gestational week, mode of delivery, order of birth, perinatal asphyxia, duration of labour, seasonality, gestational diseases, and iodine deficiency affecting the neonatal TSH surge [7]. These factors pose the challenge to distinguish the physiological pattern of the neonatal TSH from congenital hypothyroidism. Many previous studies have reported inconsistent results regarding the relationship between neonatal TSH surge and perinatal factors [8,9,10]. Some of these studies were conducted, retrospectively, and the data were obtained from medical records. Moreover, the reports do not seem to sufficiently explain causality. Although it is well known that the placenta plays a pivotal role in iodine metabolism to synthesize foetal THs, the relationship between the neonatal TSH peak and placental iodine concentration is unclear [6].
It can be predicted that postpartum removal of the placenta, which plays a compensatory role for the fetus as an iodine reservoir, may has a remarkable effect on the neonatal TSH pattern. This study focused on the potential relationship between the neonatal TSH peak, which emerged as an adaptation mechanism in the transition from intrauterine to extrauterine life, and the placental iodine level as a driving force of TH synthesis.
Materials and methods
This is a prospective, single-center study conducted between March 2019 and February 2020. The participants included 42 mothers, aged from18 to 41 years, and their newborns; the mothers gave birth by elective cesarean section following uncomplicated pregnancies at 38 to 42 weeks of gestation. The following variables were registered: birth history, exposure to perinatal asphyxia, Apgar scores, and the newborn's length and weight at birth. The exclusion criteria were as follows: twin pregnancy, newborn with perinatal asphyxia, gestational diabetes, newborn who was < 37 or > 42 weeks of gestational age, eclampsia/pre-eclampsia, intrauterine growth retardation, birth weight less than 2600 g (gm), vaginal delivery, maternal smoking or drug use, maternal thyroid disease, diagnosis of congenital hypothyroidism by heel-stick screening, maternal thyroid-stimulating hormone (TSH) higher than 8 IU/mL, emergency cesarean section, newborn with isolated or multiple anomalies, and Apgar score < 8 points at five minutes. Informed consent was obtained from all mothers for the study.
The samples collected and assays studied are as follows: iodine in placental tissue, amniotic fluid (AF), and maternal urine. Blood was drawn for the following hormone assays from the umbilical cords (uc) (within 10 min),the mothers (at the first hour), and the newborns (postnatal first and 24th hours after birth): TSH, free T4 and T3 (fT4 and fT3), human chorionic gonadotrophin (hCG), prolactin hormone (PRL), follicle stimulating hormone (FSH), luteinizing hormone (LH), and cortisol. Hormone results at the first or 24th hours will be presented by adding “1” and “24” to the end of the abbreviations (TSH1/TSH24, etc.). Within 10 min of the birth, 5 cubic centimeters (cc) of blood was drawn from the umbilical vein. After delivery, 5 cc of blood was taken from the newborn (at the first and 24th hours) and from the mother (at the first hour). The sera that were separated after the blood samples were centrifuged. Hormone analysis was performed on the Beckman Coulter Inc.UniCelDxI800 Access Immunoassay System (U.S.A.). All hormone assays were analyzed through the chemiluminescence immunoassay method using TSH;3rd IS, total β-HCG;5th IS. The newborns were divided into three groups according to serum TSH levels at the first hour. The groups were determined based on cut-off values from previous screening programs, which are1-low: 0–9.9mIU/mL, 2-moderate: 20–39.9mIU/mL, and 3-high: ≥ 40mIU/mL [11].
Iodine analysis in samples
Placental tissue collection for iodine analysis
All placentas (n = 42) were obtained from pregnant women who had undergone elective cesarean section delivery. Within 10 min of the time the following umbilical cord had been cut, biopsies were performed from placental tissue by applying the principles determined by Kristof Y et al. [12]. Placental biopsies were obtained from three cotyledons located in the front, right, and left of the larger umbilical artery lines (Fig. 1). Placental tissues measuring 2 × 2 centimeters (cm) were cut at distances of 2cm from the umbilical cord. The tissue pieces were rubbed and dried with filter paper to purify them from wet and bloody content and then placed in plastic tubes. An average of 1gm of each sample was obtained from three tissue pieces for analysis. The samples were placed in glass Petri dishes and dried for 24 h in an oven at 105°Celsius (C). The pieces were weighed and recorded a second time after drying and were prepared for iodine analysis. Iodine measurements of placental tissues were analyzed using the inductively coupled plasma-mass spectrometry (ICP–MS) method. Measurements were determined in micrograms per kilogram (µg/kg).
Iodine analysis in amniotic fluid and urine
5 cc of amniotic fluid were withdrawn and placed in plastic tubes. After delivery, urine was collected every 24 h from the mothers and placed in plastic tubes. Iodine measurements in both samples were analyzed through the ICP-MS method. Measurements were determined in µg/liter (L).The samples were kept in a freezer at − 80°C until analysis.
Results
All newborns (with birth weights of 2.600 to 3.900 gr) who were not exposed to perinatal asphyxia. The mean maternal age was 27.23 ± 6.25 years. Table 1 presents the mean values for possible perinatal factors associated with the newborn TSH peaks. The mean iodine levels of the placental tissue were found to be 29.06 ± 45.88 μg/kg (5.58–276.01) (Table 2). The AF and 24-h maternal urine iodine levels were 182.80 ± 446.51 µg/liter (16.87–2658.55) and 498.35 ± 708.34 (37.38–3652.7), respectively. The mean value of TSH1 (at the first hour) was 32.41 ± 13.96 mIU/mL (3.02–58.34). The mean value of neonatal HCG1 (at the first hour) was found to be 30.66 ± 18.55 mIU/mL. Table 2 also provides the iodine and hormonal values in all samples.
None of the perinatal factors including maternal weight, height, placental weight, Apgar scores, birth length, birth weight, and birth order had a significant association with the TSH1 peaks in three groups according to TSH1 levels (Table 3). There was a weak correlation of the TSH1 peaks with birth order, placental weight, and maternal urine iodine levels (r = 0.310, p = 0.394; r = 0.313, p = 0.648).
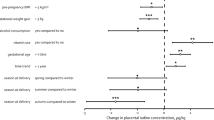
There was a significant difference between the three groups (low, moderate, and high TSH surge levels) regarding neonatal TSH1, HCG1, and placental iodine levels (p < 0.001 for each variable) (Table 4). The mean values between the three groups (low, moderate, and high groups according to TSH1 levels, respectively) were, for TSH1:12.09 ± 7.86 mIU/mL (5.3–19.2), 30.46 ± 5.47 mIU/mL (23.5–38.7), and 48.06 ± 5.71 mIU/mL (40.45–58.3), for HCG1:11.28 ± 5.17 mIU/mL (3.8–18.3), 29.75 ± 14.56 mIU/mL (7.89–67.1), and 44.07 ± 18.99 mIU/mL (5.12–80.95), for and placental iodine: 82.30 ± 87.00 88 μg/kg (49.01–276.03), 20.10 ± 13.6188 μg/kg (6.85–69.48), and 10.75 ± 8.7988 μg/kg (5.58–38.85) (Fig. 2). Figure 3 shows the comparisons of each group to the others (low–moderate, low–high, and moderate–high) and the differences between the means of the TSH1, HCG1, and placental iodine.
One of the study's most important findings is that there is an inverse relationship between the TSH1 peak and placental iodine levels (r = − 0.763, p < 0.001) (Fig. 4, Table 5). There was no correlation between the mean levels of the AF and urine iodine and the mean TSH1 peaks (r = − 0.133, p = 0.696, r = − 0.036, p = 0.816, respectively). While TSH1 peaks were not correlated with umbilical cord TSH (rumbilicalTSH = 0.151, p = 0.339), it was correlated with neonatal and umbilical PRL levels (rneonatalPRL = 0.282, p = 0.092; rumbilicalPRL = 0.455, p = 0.011) (Table 5).
Another important finding of the study is that there is a correlation between placental iodine levels and neonatal HCG1 levels (Fig. 5). A very strong inverse correlation was found between the mean levels of neonatal HCG1 and placental iodine (rHCG-pliodine = -0.919, p < 0.001) (Fig. 5) (Table 5). There is a similar relationship between both neonatal TSH1 and HCG1 levels and other variables (with iodine and PRL levels) (Table 5).
Neonatal PRL1s had a weak but positive correlation with levels of TSH1 and HCG1 (rPRL1-TSH1 = 0.282, p = 0.890 and rPRL1-HCG = 0.340, p = 0.027), and there were positive moderate correlations between the mean TSH1-TSH24 and HCG1-HCG24 levels (rTSH1-TSH24 = 0.552 versus rHCG1-HCG24 = 0.583, respectively).
Discussion
This study focused on the pivotal role of placental iodine content as a driving force in remarkable surges in TSH levels that reflect the efforts to adapt in the transition from intrauterine to extrauterine life after birth. It has been shown that thyroid glands and hormones have throughout the course of history pursued an evolutionary pathway that contributes to the adaptation to the transition from iodine-rich aquatic life to iodine-deficient terrestrial life in terms of structure and function [2]. The results of this study suggest that the dynamic fluctuation in TSH levels during the perinatal period reflects the ontogenetic heritage from evolutionary processes that have emerged for iodine regulation.
The present study was established by designing a homogeneous population, as much as was possible, with regard to potential perinatal factors associated with neonatal TSH to measure iodine influence. All newborns had birth weights of 2600–3900 gm and none were exposed to perinatal asphyxia. In this study, no difference was found in terms of perinatal factors in the three groups classified by the TSH peak levels. Previous studies have reported contradictory results in terms of perinatal factors [7,8,9]. To our knowledge, there has been no previous report investigating the relationship between placental iodine levels and neonatal TSH peaks. Therefore, it is still unclear from previous studies that found a relationship between perinatal risk factors, including perinatal asphyxia and neonatal TSH peaks, whether the placental iodine reserve had an influence on these results. Moreover, perinatal asphyxia leads to changes in placental iodine storage [13]. Oxygen acts as a signal for iodine regulation. Similarly, when mothers smoke, this causes changes in placental iodine regulation [14]. These findings suggest that the interaction between perinatal factors and neonatal TSH can be carried out through placental iodine regulation. When all perinatal factors in the groups were compared, there was no difference between the three groups (low, moderate, and high). However, significant differences were found between the levels of the mean placental iodine, neonatal TSH1, and ucTSH and the neonatal HCG1 levels in each group. While neonatal TSH1 levels correlated with HCG1 levels in the same direction, TSH1 levels were found to have an inverse correlation with levels of placental iodine. This finding indicates that the neonatal TSH peak levels can be determined by placental iodine levels under conditions, where there are no perinatal risk factors.
One of the perinatal factors affecting neonatal TSH levels is the mode of delivery [15]. It is generally known that TSH levels in newborns delivered by cesarean section are lower than those delivered by normal vaginal delivery [16]. However, there are some previous studies that did not find any difference [17]. Even, some studies have reported higher TSH levels in newborns delivered with an elective cesarean section [18]. Moreover, there are studies reporting differences between elective-emergency cesarean section and spontaneous-instrumental vaginal deliveries [10]. These differences depending on the type of delivery are explained by the interaction between stress-cortisol and THs associated with vaginal delivery. Study designs investigating the relationship between delivery mode and neonatal TSH are always faced with some challenges, as they may coincide with other perinatal risk factors [19]. However, it seems that the mode of delivery alone, without other perinatal factors, does not significantly affect neonatal TSH levels, at least no requiring changes in TSH cutoff levels in screening programs [15, 17]. To clearly examine the relationship between neonatal TSH and placental iodine in the present study, all women were chosen from participants who underwent elective unlabored caesarean section following uncomplicated pregnancies at term.
This study found no significant correlation between iodine levels in AF and neonatal TSH1 peaks. Iodine levels in AF are reported as not being dependent on iodine intake in the maternal diet [20]. In a previous study, it was reported that there was a positive correlation between amniotic and maternal urine iodine levels and neonatal TSH peaks [21]. However, the correlations in this study are not significant and weak (r = 0.170, p = 0.01, and r = 0.210, p = 0.015). The results show that the placental iodine level is the main determinant in iodine-thyroid regulation between the mother and the fetus rather than the amniotic fluid or urine. The present study showed that there was a moderate positive correlation between ucTSH and postpartum TSH1 levels (r = 0.548, p < 0.001). Although studies report that there is a relationship between urine iodine and AF iodine levels and ucTSH, those correlations were weak [21, 22]. Our findings show that umbilical cord TSH and neonatal TSH1 act in the same direction.
There is a well-known relationship between maternal iodine status and neonatal thyroid functions or congenital hypothyroidism. While congenital hypothyroidism is common in iodine-deficient countries, it has decreased in countries, where iodine replacement is applied to pregnant women [6]. However, the relationship between maternal dietary iodine intake and neonatal thyroid functions is not fully explained. While maternal excessively low iodine intake is expected to cause low TH biosynthesis in their newborns, it is reported that most of the newborns of these pregnant women do not present with a clear thyroid dysfunction symptoms [23]. On the other hand, a linear relationship could not be established between urinary iodine analyzes used to determine maternal iodine status and neonatal THs levels [24,25,26]. Most of the studies did not found any relationship between maternal urinary iodine levels and neonatal TSH levels. Similar to these studies, the present study did not find a correlation between maternal urinary iodine and neonatal TSH levels at the 1st and 24th hours. Previous researches reveal that the placenta does not only provide the delivery of maternal iodine resources to the fetus, but also acts as a compensatory iodine storage organ that protects the fetus susceptible to iodine fluctuations in case of insufficient maternal iodine supplies [6]. The present study found a significant correlation between placental iodine content and neonatal TSH peak. The results of the present study confirm the role of placental iodine on TSH regulation.
One of the most important findings of the study is that there was a strong negative correlation between the postpartum TSH1 peaks and placental iodine levels (r = − 0.763, p < 0.001). This finding suggests that the placental iodine content is the main driving force in determining perinatal TSH fluctuations. Although it is well known that the placenta plays an important role in iodine regulation throughout pregnancies, there are limited numbers of studies on iodine content within placental tissue [5, 12]. It is reported that the placenta is the largest organ following the thyroid gland to serve as an iodine reservoir. The placenta plays an important role in the uptake, storage, and fetal transport of the iodine that is required for thyroid hormone synthesis from the beginning of fetal implantation [27]. The placenta supplies the iodine and thyroid hormones that the fetus needs in the first half of pregnancy. It is known that sodium/iodide (Na/I) symporter pumps in the thyroid have also been found in the placenta [28]. Not only is iodine taken in by mothers who have sufficient diets, but it must also be transported to fetuses. Our study not only found that the placental iodine content did not correlate with the AF and maternal urine iodine levels but also showed a strong correlation with neonatal TSH levels. Developing fetuses are very sensitive to iodine fluctuations throughout the intrauterine period and have placenta iodine reservoirs as compensatory mechanisms that supply the fetal requirements. The placenta can be considered as "an iodine islet in the ocean within us," providing iodine-rich oceanic living circumstances throughout the intrauterine period. The results of our study reveal the clinical importance of placental iodine content. The higher the placental iodine content, the lower the neonatal TSH peak, and vice versa. Placental iodine storage determines the pattern of the TSH surge, contributing to adaptation in the transition from intrauterine to extrauterine life. The iodine content in the placenta may also play a role in determining the levels of TSH peak in newborns with varying perinatal risk factors. That is, the levels of the TSH peak are designed by the placental iodine levels. As a result, the TSH surge reflecting efforts to adapt to the transition from iodine-rich aquatics to iodine-deficient terrestrial life.
Another important finding is that there is a very strong negative correlation between levels of placental iodine and neonatal HCG1 (r = − 0.919, p < 0.001). Based on this, it seems that HCG acts in a similar direction to TSH1. HCG begins to be synthesized by the syncytiotrophoblasts immediately after the placental invasion [29]. HCG plays a critical role in fetoplacental iodine regulation and thyroid hormone support, especially during the first half of pregnancy. It is known that HCG increases iodine uptake over Na/I symporter expression. HCG levels are regulated by negative feedback with the iodine levels [30]. Postpartum neonatal HCG peak has a pattern similar to the TSH peak. In vitro studies have shown that the HCG response to iodine occurs within 3 days [31]. If the dramatic TSH peak postpartum reflects an effort to treat iodine deficiency, it may be asked, then, why it declines rapidly within days. The reason for this rapid decline may be the cessation of the placental support of HCG, a TSH stimulator after the umbilical cord is cut and the placenta is separated.
Another remarkable result of the study is that neonatal PRL1 also shows correlations similar to TSH1 and HCG1. Although the interaction of PRL1 in placental iodine regulation is unknown, it has been reported to increase Na/I symporter expression in the mammary glands and increase iodine uptake [32]. Given the correlation of PRL with HCG in the same direction, the same effect is likely to be on the placental iodine. The role of PRL in neonatal TSH regulation is not known enough.
There was a moderate positive correlation between ucTSH and TSH1 (r = 0.548, p < 0.001). In addition, ucTSH can provide predictions with the neonatal TSH1 peak. Investigations are reporting that umbilical TSH measurement is predictive in predicting perinatal risk factors [33, 34].
Conclusion
This study shows that although placental iodine levels demonstrate a strong inverse correlation with neonatal TSHs and HCGs, these levels have a weak but inverse correlation with PRL levels, and there are moderate-weak but positive correlations between the levels of HCG and PRL and the TSH levels. This indicates that HCG and PRL act in the same direction as TSH, which plays a primary role in adaptation to the transition from intrauterine to extrauterine life, and that placental iodine content is a pivotal player that drives the hormonal regulation that determines the course of neonatal TSHs.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Crockford SJ (2009) Integr Comp Biol. Evolutionary roots of iodine and thyroid hormones in cell-cell signaling. 49(2):155–166. https://doi.org/10.1093/icb/icp053
Sebastiano V (2011) Evolutionary significance of ıodine. Curr Chem Biol 5(3):155–162
Burrow GN, Fisher DA, Larsen PR (1994) Maternal and fetal thyroid function. N Engl J Med 331(16):1072–1078
Hillman NH, Kallapur SG, Jobe AH (2012) Physiology of transition from intrauterine to extrauterine life. Clin Perinatol 39(4):769–783. https://doi.org/10.1016/j.clp.2012.09.009
Burns R, Herlihy C, Smyth PP (2011) The placenta as a compensatory iodine storage organ. Thyroid 21(5):541–546. https://doi.org/10.1089/thy.2010.0203
Burns R, Azizi F, Hedayati M, Mirmiran P, Herlihy C, Smyth PP (2011) Is placental iodine content related to dietary iodine intake. Clin Endocrinol (Oxf) 75(2):261–264. https://doi.org/10.1111/j.1365-2265.2011.04039.x
Tim IM, Korevaar LC, Vincent WV, Jaddoe TJ, Visser MM, Robin P (2016) Peeters, maternal and birth characteristics are determinants of offspring thyroid function. J Clin Endocrinol Metab 10:206–213. https://doi.org/10.1210/jc.2015-3559
Lee SY (2016) Perinatal factors associated with neonatal thyroid-stimulating hormone in normal newborns. Ann Pediatr Endocrinol Metab. 21(4):206–211. https://doi.org/10.6065/apem.2016.21.4.206
Trumpff C, Vandevijvere S, Moreno-Reyes R, Vanderpas J, Tafforeau J, Van Oyen H, De Schepper J (2015) Neonatal thyroid-stimulating hormone level is influenced by neonatal, maternal, and pregnancy factors. Nutr Res 35(11):975–981. https://doi.org/10.1016/j.nutres.2015.09.002
Herbstman J, Apelberg BJ, Witter FR, Panny S, Goldman LR (2008) Maternal, infant, and delivery factors associated with neonatal thyroid hormone status. Thyroid 18(1):67–76. https://doi.org/10.1089/thy.2007.0180
Simsek E, Karabay M, Kocabay K (2005) Neonatal screening for congenital hypothyroidism in West Black Sea area. Turkey Int J Clin Pract 59(3):336–341
Neven KY, Marien CBD, Janssen BG, Roels HA, Waegeneers N, Nawrot TS, Ruttens A (2020) Variability of iodine concentrations in the human placenta. Sci Rep 10(1):161. https://doi.org/10.1038/s41598-019-56775-3
Li H, Landers K, Patel J, Richard K, Mortimer RH (2011) Effect of oxygen concentrations on sodium iodide symporter expression and iodide uptake and hCG expression in human choriocarcinoma BeWo cells. Am J Physiol Endocrinol Metab 300(6):E1085–E1091. https://doi.org/10.1152/ajpendo.00679.2010
Andersen S, Nøhr SB, Wu CS, Olsen J, Pedersen KM, Laurberg P (2013) Thyroglobulin in smoking mothers and their newborns at delivery suggests autoregulation of placental iodide transport overcoming thiocyanate inhibition. Eur J Endocrinol 168(5):723–731. https://doi.org/10.1530/EJE-12-0759
Miyamoto N, Tsuji M, Imataki T, Nagamachi N, Hirose S, Hamada Y (1991) Influence of mode of delivery on fetal pituitary-thyroid axis. Acta Paediatr Jpn 33(3):363–368. https://doi.org/10.1111/j.1442-200x.1991.tb01567.x
Fan P, Luo ZC, Tang N, Wang W, Liu Z, Zhang J, Ouyang F (2020) Advanced maternal age, mode of delivery, and thyroid hormone levels in chinese newborns. Front Endocrinol 10:913. https://doi.org/10.3389/fendo.2019.00913
Turan S, Bereket A, Angaji M et al (2007) The effect of the mode of delivery on neonatal thyroid function. J Matern Fetal Neonatal Med 20(6):473–476. https://doi.org/10.1080/14767050701398314
McElduff A, McElduff P, Wiley V, Wilcken B (2005) Neonatal thyrotropin as measured in a congenital hypothyroidism screening program: influence of the mode of delivery. J Clin Endocrinol Metab 90(12):6361–6363. https://doi.org/10.1210/jc.2005-0786
Velasco I, Sánchez-Gila M, Manzanares S, Taylor P, García-Fuentes E (2020) Iodine status, thyroid function, and birthweight: a complex relationship in high-risk pregnancies. J Clin Med 9(1):177. https://doi.org/10.3390/jcm9010177
García-Fuentes E, Gallo M, García L, Prieto S, Alcaide-Torres J et al (2008) Amniotic fluid iodine concentrations do not vary in pregnant women with varying iodine intake. Br J Nutr 99(6):1178–1181. https://doi.org/10.1017/S0007114507862398
Velasco I, Martín J, Gallego M, Gutiérrez-Repiso C, Santiago P et al (2013) Maternal-fetal thyroid function at the time of birth and its relation with iodine intake. Thyroid 23(12):1619–1626. https://doi.org/10.1089/thy.2013.0035
Alves ML, Maciel RM, Kunii I, Iazigi N (2005) Correlation between urinary iodine levels and TSH of umbilical cord from newborns of the University Hospital at the School of Medicine from Ribeirão Preto São Paulo. Arq Bras Endocrinol Metabol 49(4):516–520
Markou K, Georgopoulos N, Kyriazopoulou V et al (2001) Iodine-induced hypothyroidism. Thyroid 11:501–510
Kutlu Yaman A, Demirel F, Ermis B, Pişkin IE (2013) Maternal and Neonatal Urinary Iodine Status and its Effect on Neonatal TSH Levels in a Mildly Iodine-Deficient Area. J Clin Res Pediatr Endocrinol 5:90–94
Travers CA, Guttikonda K, Norton CA et al (2006) Iodine status in pregnant women and their newborns: are our babies at risk of iodine deficiency? Med J Aust 184(12):617–620
Dei-Tutu SA, Manful A, Heimburger DC et al (2020) Correlating maternal iodine status with neonatal thyroid function in two hospital populations in Ghana: a multicenter cross-sectional pilot study. BMC Pediatr 20(1):26. https://doi.org/10.1186/s12887-020-1932-6
Glinoer D (1997) The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from physiology to pathology. Endocr Rev 18(3):404–433
Burns R, O’Herlihy C, Smyth PP (2013) Regulation of iodide uptake in placental primary cultures. Eur Thyroid J 2(4):243–251. https://doi.org/10.1159/000356847
Kota SK, Gayatri K, Jammula S, Meher LK, Kota SK, Krishna SV, Modi KD (2013) Fetal endocrinology. Indian J Endocrinol Metab 17(4):568–579. https://doi.org/10.4103/2230-8210.113722
Li H, Richard K, McKinnon B, Mortimer RH (2007) Effect of ıodide on human choriogonadotropin, sodium-ıodide symporter expression, and ıodide uptake in bewo choriocarcinoma cells. J Clin Endocrinol Metab. 92(10):4046–4051
Arturi F, Presta I, Scarpelli D, Bidart JM, Schlumberger M, Filetti S, Russo D (2002) Stimulation of iodide uptake by human chorionic gonadotropin in FRTL-5 cells: effects on sodium/iodide symporter gene and protein expression. Eur J Endocrinol 147(5):655–661
Rillema JA, Rowady DL (1997) Characteristics of the prolactin stimulation of iodide uptake into mouse mammary gland explants. Proc Soc Exp Biol Med 215(4):366–369
Gupta A, Srivastava S, Bhatnagar A (2014) Cord blood thyroid stimulating hormone level–interpretation in light of perinatal factors. Indian Pediatr 51(1):32–36
Rashmi SA, Sekhri T, Agarwal A (2007) Effect of perinatal factors on cord blood thyroid stimulating hormone levels. J Pediatr Endocrinol Metab 20(1):59–64
Acknowledgements
We would like to thank Anesthesiologist Dr. Cengiz İsbilen for helping to collect samples including placenta, blood, and urine from the mothers and their newborns.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Dr. Karaoglan conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. Dr. Isbilen analyzed placental iodine,studied hormone assays, collected and analyzed data.
Corresponding author
Ethics declarations
Conflict of interest
We have no conflict of interest.
Ethical approval
This research was approved by Gaziantep University Clinical Research Ethics Committee with decision no 2018/353;19.12.2018.
Research involving human participants and/or animals
Authors declared that all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Authors declare that informed consent was obtained from all mothers for the study.
Consent for publication
Mothers have signed an consent publication form to use their data and placental photos. We also declare that these forms were held by the treating institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karaoglan, M., İşbilen, E. The role of placental iodine storage in the neonatal thyroid stimulating hormone surge: iodine as a driving force to adapt the terrestrial life. J Endocrinol Invest 44, 1041–1052 (2021). https://doi.org/10.1007/s40618-020-01399-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01399-y