Abstract
The human placenta is an important organ that forms a barrier where maternal and fetal exchange takes place. The placenta transport iodine to the fetal circulation by transfer of maternal iodine and deiodination of thyroid hormones (THs). The aim of the study was to examine the distribution of iodine and thyroid hormone transporters in the maternal and fetal sides of human-term placenta. A cross-sectional study was performed at the First Affiliated Hospital of China Medical University. Placental samples (maternal and fetal surfaces) were collected from 113 healthy-term pregnant women. The iodine content; the concentration of thyroxine (T4), triiodothyronine (T3), and reverse T3 (rT3); and the enzyme activity of placental type 2 iodothyronine deiodinase (D2) and D3 were examined. The mRNA and protein localization/expression of iodine and thyroid hormone transporters in the placenta were also studied. We also analyzed the association between expression level of Na+/I− symporter (NIS), thyroid hormone transporter protein, D3 activity in maternal and fetal surfaces of placenta with iodine content, and thyroid hormone levels. Iodine levels in placental samples from the maternal side were significantly higher than those in samples from the fetal side. T3 and T4 expression in fetal placenta was significantly lower than in maternal placenta. D3 activity in the fetal side of the placentas was significantly higher than that in the maternal side. The mRNA and protein expression of monocarboxylate transporters 8 (MCT8), L-amino acid transporters 1 (LAT1), organic anion transporting polypeptides 4A1 (OATP4A1), and TH binding protein transthyretin (TTR) were significantly increased in maternal side, while the NIS expression was higher in fetal side of human-term placenta. In conclusion, the enzymatic deiodination of thyroid hormones forms a barrier which reduces transplacental passage of the hormones and that the maternal part of the placenta is the primary factor in the mechanism regulating the hormonal transfer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The supply of iodine for fetal synthesis of thyroid hormones (THs) is dependent on the uptake of maternal iodine and placental deiodination of thyroxine (T4), as well as placental capacity to store and transport iodine to the fetal circulation [1,2,3]. The fetal thyroid begins to generate iodine, for the synthesis and secretion of THs, at 12–16 weeks gestation [4]. The placenta transports iodine to the fetal circulation by transfer of maternal iodine and deiodination of maternal THs. Iodine transport in the placenta, as in the thyroid, is regulated by the sodium iodine symporter (NIS) and Pendrin (PDS), the gene encoding which is mutated in Pendred syndrome. Both transporters are highly expressed in trophoblasts in human placenta at all stages of gestation and are also expressed in choriocarcinoma cell lines [5,6,7]. NIS is highly expressed in the apical (maternal) layer of syncytiotrophoblasts and regulates iodine uptake into trophoblasts, whereas PDS is localized in the basal membrane of syncytiotrophoblasts and plays a role in the efflux of iodine [5, 6]. BeWo cells are a human trophoblast cell line, which are used to study placental iodine transporters [5]. Increased expression of NIS in both the maternal and fetal side of the placenta has been demonstrated under low iodine conditions in rats, indicating that NIS compensates for insufficient iodine supply to assure adequate iodine transportation for fetal growth [8].
The human placenta is an important organ that forms a barrier where maternal and fetal exchange takes place. It transmits all the essential nutrients from mother to fetus and can also act as a barrier to protect against transfer of toxic substances to the fetus. THs play a vital role in fetal development, especially in the development of the central nervous system; even minimal fluctuations in maternal THs can affect the development of children in later life [9]. Synthesis of THs by the fetal thyroid relies on the transport of maternal iodine and THs across the placenta. Maternal thyroxine (T4) is the major TH transported across the placenta to the fetal circulation, although triiodothyronine (T3) can also be transferred from the maternal circulation. The activity of THs is dependent on T4 and T3 levels, which are mainly regulated by deiodinases and TH transporters. The iodothyronine deiodinases expressed in human placenta are deiodinase types 2 and 3 (D2 and D3) [10]. D2 has outer ring deiodinase activity and converts T4 to T3, thus ensuring that the fetus is exposed to only a small amount of T3 throughout gestation [11]. D3 inactivates THs by catalyzing the inner ring deiodination of T4 to give inactive reverse triiodothyronine (rT3) and of T3 to give 3,3′-diiodothyronine (T2), thus protecting the fetus from excess THs [12]. The predominant deiodinase in the placenta is D3 and D2 is expressed at much lower levels [5, 13]. D2 and D3 mRNA and enzymatic activity have been previously reported in human placenta, and the activities of both deiodinases decrease throughout gestation [5, 13]. D2 is present in villous cytotrophoblasts during the first trimester and in syncytiotrophoblasts during the third trimester, whereas D3 is localized to the syncytiotrophoblast layer in both the first and third trimester of gestation [13].
It has been long believed that TH transporters regulate the intake and efflux of iodothyronines across the placenta [14, 15]. To date, seven TH transporters, which are presumed to regulate T4 and T3 transport, have been reported to be expressed in the placenta [16,17,18]. These include monocarboxylate transporters 8 and 10 (MCT8, MCT10), L-amino acid transporters 1 and 2 (LAT1, LAT2), organic anion transporting polypeptides 1A2 and 4A1 (OATP1A2, OATP4A1), and TH binding protein transthyretin (TTR). The OATP family is a large family of homologous proteins, which have been found to transport THs. OATP4A1, also known as OATP-E, has the ability to transport T3 and T4, and even a small amount of rT3 [19]. It has been reported that MCT8 mRNA expression is elevated during gestation [20]. MCT8 has been detected in both syncytiotrophoblasts and cytotrophoblasts, and even in the endothelial cells of fetal capillaries, indicating that MCT8 may play an important role in the transportation of THs across the placenta [21]. MCT8 has been reported to regulate T3 uptake in the syncytiotrophoblast layer of human-term placenta [22]. MCT10, which is highly correlated with MCT8, has also been reported to induce accumulation of T3 in JEG3 cells [22]. The LAT1 and LAT2 transporter subtypes have been studied in BeWo cells, in which the System L transporter is responsible for almost 30% of T3 uptake [23]. TTR is a high-affinity T4 transport protein, and also transports retinol bound to retinol binding protein [24]. It was previously reported that TTR is expressed in the trophoblasts of placenta [25]. TTR was found in the placenta 6 weeks into pregnancy and increased in a time-dependent manner during early gestation, with levels remaining constant from 13 weeks to term [26]. The mechanisms that mediate TH transport from the maternal to fetal circulation remain largely unknown.
The aim of the present study was to examine iodine and TH transporters in the maternal side and fetal side of human-term placenta and to determine the transfer of T4, T3, and rT3 from the maternal to fetal circulation. Levels of deiodinase mRNA and enzymatic activity were also measured to analyze the effect of deiodination on TH transfer.
Methods
Study Groups
A cross-sectional study was performed at the First Affiliated Hospital of China Medical University and registered with ClinicalTrials.gov (ChiCTR-TRC-12002326), which started in June 2012 in Liaoning Province in northeastern China. The study protocols were approved by the ethics committee of China Medical University. A total of 113 healthy-term pregnant women, scheduling for cesarean section (37–40 weeks gestation), were enrolled in this study. Maternal blood and urine samples were obtained from each subject between 8 A.M. and 10 A.M. after an overnight fast. Serum was collected and stored at − 80 °C until further analysis. All subjects were between 21 and 40 years of age. Informed consent was provided by all subjects. Patients with hypertension, gestational diabetes, renal and cardiac diseases, autoimmune diseases, polycystic ovarian syndrome, and multi-gestations were excluded from the study. During the delivery, immediately after removal of the placenta, samples (2 × 1 × 1 cm) were collected from the maternal side of the placenta, close to the decidua, and from the fetal side of the placenta, close to the amnion. All samples of placenta were stored at − 80 °C until further use. The general information of the study population is exhibited in Table 1.
Placental Iodine Levels
Samples of placenta from both maternal and fetal sides were thawed at room temperature, washed three times with 0.9% NaCl solution, and dried with filter paper to remove excess water. The placental samples (500 mg wet weight) were then placed in quartz tubes and digested using a mixed menstruum of 1.5 mL (BV-grade III) containing nitric acid (1 mL) and H2O2 (0.5 mL) in a high-pressure microwave digestion system (Milpitas, CA, USA). After digestion, all placental samples were transferred to vessels containing ultrapure deionized water (0.7 mL). Iodine levels were determined by inductively coupled plasma mass spectrometry (ICP-MS), using a PerkinElmer Sciex Elan mass spectrometer (PerkinElmer, Inc., Waltham, MA, USA). Iodine levels are presented as μg/g. Certification using Chinese national reference material was used for affirmation and adjustment of the specification curve.
Placental Thyroid Hormone Levels
T3, T4, and rT3 concentrations were measured in samples of both maternal and fetal sides of the placenta. Extraction and radioimmunoassay were carried out as previous described [27,28,29]. Hormone levels are presented as ng/g.
Determination of D2 and D3 Activities
D2 activity was assayed as previously described [30], but the activity in all samples was below the limit of detection. To measure D3 activity [31], samples were homogenized in a balanced solution (1 mL), containing EDTA (2 mM), DTT (1 mM), and phosphate (100 mM). The culture mixture comprised diluted homogenate (100 μl), T3 (1 nM), [125I]-T3 (150,000 cpm), and rT3 (1 μM). Propylthiouracil (0.1 mM) was added to rule out interference by D1. The mixture was incubated for 2 h. D3 activity is reported as the quantity of hormone deiodinated/mg/min.
Quantitative Real-Time-PCR Analysis
Expression levels of mRNAs for 11 iodine and TH transporters were measured using TaqMan Quantitative Real-Time-PCR. Total RNA was extracted from 113 placental samples from both the maternal and fetal sides using TRIzol reagent (Invitrogen, Thermo Fisher Scientific Inc., Waltham, MA, USA), following the standard protocol. A Nano Drop 2000C UV-Vis spectrophotometer (Thermo Fisher Scientific Inc.) was used to determine RNA purity and concentration. The OD 260/280 absorbance ratio was 1.8–2.0 for each sample. Total RNA was reverse transcribed with primers using a PrimeScript™ RT Reagent Kit (TaKaRa Biotechnology Co., Ltd., Dalian, China). RT-PCR was carried out using an ABI 7500 Sequence Detection System (Applied Biosystems, Thermo Fisher Scientific Inc.). All PCR reactions were performed in a total volume of 20 μL, and single transcripts of gene expression were determined using SYBR® Premix Ex Taq TM II (TaKaRa Biotechnology Co., Ltd.), according to the manufacturer’s instructions. Reactions began with a 10-s hot-start activation of the Taq polymerase at 95 °C, followed by 40 to 45 cycles of amplification in three steps (denaturation at 95 °C for 5 s, followed by annealing at 60 °C for 30 s and extension at 72 °C for 30 s). The reactions were carried out in a total volume of 20 μL in a 0.2-mL flat cap PCR tube (Axygen, Tewksbury, MA, USA). The primers for qRT-PCR are shown in Table 2.
Analysis of Iodine and Thyroid Hormone Transporter by Immunohistochemistry
A total of 113 term placental samples, from both maternal and fetal sides, were embedded in paraffin and sectioned coronally into 5-μm sections using a microtome. Sections were dewaxed, rehydrated, and treated for endogenous peroxidase using 3% hydrogen peroxide-methanol for 10 min. All sections were incubated with primary antibody at 4 °C overnight and were then incubated for 40 min at room temperature. The primary antibodies against D3, NIS, pendrin, LAT1, LAT2, MCT8, MCT10, OATP1A2, OATP4A1, and TTR (Abcam, Cambridge, UK) were used at concentrations of 1:200, 1:200, 1:150, 1:200, 1:150, 1:250, 1:150, 1:300, and 1:100, respectively. The tissue sections were incubated with biotin-conjugated secondary antibodies (Zhongshan Biotechnology, Beijing, China) for 10 min and then with streptavidin-peroxidase complex (Zhongshan Biotechnology) for 10 min. Sections were then treated with a solution of 3, 3′-diaminobenzidine (DAB; Zhongshan Biotechnology) for 1 to 3 min, depending upon the staining of the DAB reaction product observed under light microscopy. Finally, the sections were counterstained with hematoxylin, dehydrated, rinsed, and mounted in neutral gum (China National Medicines, Shanghai, China). All placental sections were observed at × 400 magnification. D2 staining was not analyzed because the specific antibody for D2 in placenta was unavailable.
Statistical Analysis
All statistical analyses were performed using SPSS software 20.0 (SPSS, Inc., Chicago, IL, USA). Results are displayed as mean ± standard deviation. The Bonferroni test was used for pairwise comparisons. GraphPad Prism 5 software (GraphPad Software, La Jolla, CA, USA) was used to analyze study graphs. p values < 0.05 were considered to be statistically significant.
Results
Placental Iodine Levels
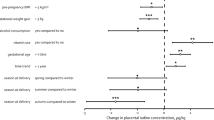
Iodine levels (μg/g) were measured in a total of 226 placental samples (113 from the maternal side and 113 from the fetal side), collected from women from Liaoning Province (Fig. 1). Iodine levels in placental samples from the maternal side (1.38 ± 0.32 μg/g) were significantly higher than those in samples from the fetal side (0.45 ± 0.13μg/g, p < 0.01). There was no correlation between fetal side of human-term placenta and either urinary iodine concentration (UIC) or urinary iodine to creatinine ratio (UI/Cr). However, iodine levels in maternal side of human-term placenta were correlated with UIC (r = 0.316, p < 0.05) and UI/Cr (r = 0.339, p < 0.05).
Dot plots showing placental iodine content in the fetal and maternal sides of human-term placenta. Iodine contents were measured by ICP-MS. The data were expressed as μg/g. Values were shown as mean± SD. Differences between fetal and maternal groups were compared using the Mann-Whitney U test. **p < 0.01
Placental Iodothyronine Concentrations
The concentrations of T3, T4, and rT3 in the maternal and fetal sides of human-term placentas were compared. T4 levels in the fetal side (44.96 ± 6.35 ng/g) were much lower than those in the maternal side (67.72 ± 18.2 ng/g, p < 0.05, Fig. 2a). Similarly, T3 expression in fetal placenta (4.34 ± 0.29 ng/g) was significantly lower than in maternal placenta (5.93 ± 0.78 ng/g, p < 0.05, Fig. 2b). Levels of rT3, however, were not significantly different in fetal placenta (1.56 ± 0.13 ng/g) and maternal placenta (1.47 ± 0.35 ng/g, Fig. 2c).
T4 (a), T3 (b), and rT3 (c) concentration in fetal and maternal side of human-term placenta. The data were expressed as μg/g. Values were shown as mean ± SD. Differences between fetal and maternal groups were compared using the Mann-Whitney U test. *p < 0.05.FP, fetal placenta; MP, maternal placenta
Deiodinase Activity
D2 activity was undetectable in both the maternal and fetal sides of the placentas. D3 activity in the fetal side of the placentas (9.03 ± 3.08 fmol/min/mg) was significantly higher than that in the maternal side (5.45 ± 0.85 fmol/min/mg, p < 0.01, Fig. 3)
Bar graphs compare the mRNA expression of iodine and thyroid hormone transporters in the maternal and fetal side of human-term placenta. The expression was measured by real-time PCR using GAPDH as endogenous control. Values were shown as mean ± SD. Differences between fetal, and maternal groups were compared using the Mann-Whitney U test. *p < 0.05. **p < 0.01.FP, fetal placenta; MP, maternal placenta
Placental mRNA Expression
Expression of mRNA for iodine and TH transporters was measured by RT-PCR in a total of 226 samples of term placenta (113 from the maternal side and 113 from the fetal side). Expression levels of MCT8, OATP4A1, LAT1, and TTR were significantly higher in maternal placenta (p < 0.01, p < 0.05, p < 0.01, p < 0.05, respectively) than in fetal placenta (Figs. 3 and 4, whereas NIS expression was higher in the fetal side than in the maternal side. There were no significant differences in the mRNA expression of D2, D3, Pendrin, MCT10, OATP1A2, and LAT2 between the maternal and fetal sides of the placenta.
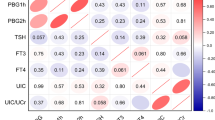
Association Between Expression Level of NIS, Thyroid Hormone Transporter Protein, D3 Activity with Iodine Content, and Thyroid Hormone Levels
In this study, we also analyzed the association between expression level of NIS, thyroid hormone transporter protein, D3 activity in maternal and fetal surfaces of placenta with iodine content and thyroid hormone levels. As exhibited in Table 3, NIS expression did not correlate with thyroid hormone levels, but its expression was correlated with iodine content (r = 0.3, p < 0.05 in maternal side; r = 0.41, p < 0.05 in fetal side). A positive correlation between D3 expression with iodine and TT3 levels was found in maternal side of placenta (r = 0.4, p < 0.05; r = 0.36, p < 0.05). D3 expression in fetal side of placenta was correlated with iodine (r = 0.31, p < 0.05) and TT3 (r = 0.42, p < 0.05). In addition, TT3 levels were also positively associated with D3 activity in maternal (r = 0.37, p < 0.05) and fetal surfaces of placenta (r = 0.44, p < 0.05). Moreover, placental MCT8 expression in maternal side of human-term placenta was correlated with TT3 (r = 0.34, p < 0.05). We could not demonstrate any statistically significant correlations between other thyroid hormone transporter protein with iodine and thyroid hormone levels.
Localization and Immunostaining of Iodine and Thyroid Hormone Transporters
Iodine and TH transporters in placental tissues from both maternal and fetal sides of placentas were determined by immunostaining. D3 was highly expressed in the syncytiotrophoblast and cytotrophoblast layers of the placenta (Fig. 5) and was also expressed in the fetal endothelium and decidua. NIS was highly expressed at the apical side of syncytiotrophoblast layers of the placenta. Pendrin was detected in the syncytiotrophoblast and cytotrophoblast layers of the placenta. MCT8 was strongly expressed in syncytiotrophoblasts, but weakly expressed in cytotrophoblasts, of term placentas. MCT10 and OATP1A2 staining was localized in both syncytiotrophoblasts and cytotrophoblasts. LAT2 was expressed in both apical and basal membranes of syncytiotrophoblasts, whereas LAT1 and OATP4A1 were predominantly located at the apical membrane of syncytiotrophoblasts. TTR was more easily detected in syncytiotrophoblast cells. Additionally, immunostaining of MCT8, LAT1, OATP4A1, and TTR was increased in trophoblasts in samples of placenta from the maternal side compared to those from the fetal side. In contrast, expression of NIS in syncytiotrophoblasts was significantly lower in samples of placenta from the maternal side than in those from the fetal side. The intensity of Pendrin, D3, MCT10, LAT2, and OATP1A2 staining was comparable in syncytiotrophoblasts from maternal and fetal placentas.
Discussion
In this study, we have demonstrated a significant difference in levels of iodine between the maternal and fetal sides of the placenta. In addition, iodine levels in maternal side of human-term placenta were correlated with UIC and UI/Cr. To the best of our knowledge, this is the first study to examine iodine levels in both sides of the placenta. This is also the first study to analyze placental iodine by ICP-MS. These results of our study support the theory that the placenta has the ability to store iodine [32]. The placenta may not only transport, but also store, iodine to supply iodine to the fetal circulation. Burns et al. demonstrated that the placenta contains more iodine than any other tissue, except the thyroid, supporting the theory that the placenta not only plays an important role in iodine uptake but also in iodine storage as a potential method to protect the fetus from exposure to excess iodine [32]. Although iodine levels in the placenta are significantly lower than those in the thyroid, the placenta and thyroid seem to have similar mechanisms for uptake and efflux of iodine. It has been demonstrated that BeWo cells take up iodine via the NIS and efflux iodine via pendrin, as does the thyroid [33]. Maternal iodine is transported by trophoblasts and released into the fetal circulation by an active transfer process that is regulated by NIS. It has been reported that NIS is upregulated in the placentas of iodine-deficient rats [34]. NIS was detected primarily in the fetal side of the placenta and was barely detectable in the maternal side, even under conditions of iodine deficiency. It is likely that the maternal placenta is still responsible for limited iodine transport, and that other transporters are expressed in the maternal side of the placenta. Our results supported this finding because we showed that NIS mRNA expression was upregulated in the fetal side of the placenta.
We also examined TH levels in term placenta and found that T4, T3, and rT3 accumulated in both maternal and fetal sides of the placenta. These results indicated that high levels of T3 and T4, or any other unidentified changes in the maternal circulation, may result in the predominant expression of T4 and T3 in the maternal side of the placenta. Because increased D3 activity in the placenta instantly converts the majority of the T4 and T3 into inactive rT3 and T2, only minimal amounts of T3 and T4 are transported from the maternal circulation to the fetus [35]. Transfer of T4 from the maternal compartment to the fetal side is extremely low and rT3 expression is elevated in the fetal and maternal circulation. In the presence of iopanoic acid, an inhibitor of D3 activity, the concentration of T4 is highly elevated in the fetal circulation while levels of rT3 are reduced [35]. Because guinea pig placenta has many similar features to human placenta, it is potentially a model for the study of placental TH transfer [13]. A previous study demonstrated that, in guinea pig placenta, an extremely limited amount of maternal T4 is converted to rT3 in the fetal circulation [36]. The placenta may be responsible for mediating fetal TH levels. High concentrations of rT3 may play a vital role in maintaining low levels of T3 in the fetal circulation since rT3 is a useful antagonist of conversion of T4 to T3. Our results are further supported by the findings in guinea pigs, where T3 and T4 were consistently higher in the maternal side of the placenta than in the fetal side throughout gestation, whereas rT3 was always elevated in the maternal placenta [36]. These results suggested that T3 and T4 remained at high levels in the maternal placenta and could be actively reduced during transplacental passage into the fetal placenta. The concentration of rT3 failed to reach statistical significance. Deiodination of T4 by the fetal placenta makes a dramatic contribution to the fetal rT3 concentration, whereas deiodination of T4 by the maternal placenta is likely to make a very limited contribution to fetal rT3 levels.
Although T3 and T4 can cross the placenta, it was demonstrated long ago that the placenta is impermeable to TH [36]. The placenta does, however, express high levels of D3, which converts T4 to inactive rT3, indicating that placental deiodination may have an inhibitory effect [10]. In the present study, we found that D2 activity was undetectable in both maternal and fetal sides of the placenta and that D3 activity was higher in the fetal side of the placenta than the maternal side. It has been previously reported that, during normal pregnancy, the placental lobule near the cord has higher D3 activity than the middle and outer side of the cord insertion into the placenta [37]. These results indicated that the major deiodinase in human-term placenta was D3. D2 activity in both the maternal and fetal sides of term placenta was below the limitation of detection in this study, confirming previous research [37]. Placental D2 activity is 100–300-fold lower than D3 activity and decreases with gestational age [35]. The high level of D3 activity results in a high level of silent T4 conversion to rT3 in the maternal circulation from the very beginning of gestation [38, 39]. D3 activity is the main reason for the minimal transfer of maternal T4 through the placenta in the perfused human placenta lobule model. Iopanoic acid can increase maternal transfer of T4 to the fetal side of the placenta almost 3000-fold [35]. In order to transfer into the fetal circulation, THs must cross through the apical and basal membranes of the syncytiotrophoblast and then pass intracellularly through the cytotrophoblasts to reach the fetal endothelium. The high D3 activity in fetal placenta has also been assumed to contribute to the transfer of iodine into the fetus, which is essential for the synthesis of THs by the fetus. These results indicated that the fetal side of the placenta made a fundamental contribution to the limitation of deiodination of iodothyronines.
To investigate the role of iodine and TH transport, we also examined the mRNA and protein expression/localization of iodine and TH transporters, including NIS, pendrin, D2, D3, MCT8, MCT10, LAT1, LAT2, OATP4A1, OATP1A2, and TTR, in both maternal and fetal sides of the placenta by real-time PCR and immunohistochemistry. This study is the first to demonstrate a difference in TH transporters in the two sides of the placenta. mRNA and protein expression of MCT8, OATP4A1, LAT1, and TTR were significantly higher in maternal placenta than in fetal placenta, while NIS expression was higher in the fetal side than the maternal side. There were no significant differences between the maternal and fetal side of placenta in mRNA or protein expression of D2, D3, pendrin, MCT10, OATP1A2, and LAT2.
We found that D3 was highly expressed in the syncytiotrophoblast and cytotrophoblast layers of the placenta, and also expressed in the fetal endothelium and decidua, which was in direct contact with the maternal circulation and was optimally positioned to protect the fetus from inadequate TH transfer and also to regulate the release of iodine into the fetal circulation [13]. This expression pattern is in agreement with a study conducted by Huang et al. [40]. In a rat study, D3 levels were comparable in maternal and fetal sides of the placenta on gestational day 18 [41]. Another study also demonstrated that mRNA expression of D3 was similar in maternal and fetal sides of human placentas [42]. These results suggested that the predominant change was in D3 activity rather than mRNA expression and that deiodinase reacts only to a minor disturbance in TH levels.
In this study, we also analyzed the association between expression level of NIS, thyroid hormone transporter protein, D3 activity in maternal and fetal surfaces of placenta with iodine content and thyroid hormone levels. NIS expression was positively correlated with iodine content. In addition, D3 expression was significantly correlated with iodine and TT3 in maternal and fetal side of human-term placenta. TT3 levels were also positively associated with D3 activity in maternal and fetal surfaces of placenta. Moreover, placental MCT8 expression in maternal side of human-term placenta was correlated with TT3. We could not demonstrate any statistically significant correlations between other thyroid hormone transporter protein with iodine and thyroid hormone levels. The relationship between iodine and thyroid hormone transporter protein with iodine content and thyroid hormone levels has not been fully demonstrated until now. The mechanism needs to be further elucidated in the future research.
NIS was highly expressed in the apical membranes of syncytiotrophoblast layers of the placenta, while pendrin was detected in the syncytiotrophoblast and cytotrophoblast layers of the placenta. mRNA and protein expression of NIS were upregulated in the fetal side of the placenta compared with the maternal side. This study is consistent with previous research in rats, which found NIS expression in fetal placenta [34]. These two iodine transporters regulate iodine transport in the placenta [5], suggesting that iodine transporters may play an important role in the development of the placenta.
It has been previously demonstrated that placenta expresses a number of membrane TH transporters and that these transporters play an important role in transplacental supply of THs and iodine [43]. In term placentas, MCT8 is strongly located in the syncytiotrophoblast and only weakly expressed in the cytotrophoblast. We also found upregulated MCT8 expression in trophoblast cells from the maternal side of the placenta. This abundant staining of MCT8 confirmed the results of a previous study on placenta [20]. This study assumed that preferential expression of MCT8 in the syncytiotrophoblast of human-term placenta made an important contribution to the T3-mediation of the placenta, which provided a balance between fetal development and placental function. The high expression of MCT8 in maternal placenta may provide a compensatory mechanism that facilitates T3 uptake by trophoblasts and increases the transfer of TH back to these cells. MCT10 expression is comparable in both maternal and fetal sides of the placenta, which may be because of its abundance in cytotrophoblast and syncytiotrophoblast basal membranes in the fetal placenta [44, 45]. In our study, LAT1 was found to be abundant in the syncytiotrophoblast layer of the microvillous plasma membrane in human-term placenta and was elevated in maternal placenta. This result is in agreement with a study conducted by Prasad et al. [46], which demonstrated that LAT1 is predominantly expressed in the brush border membranes (maternal facing) and that the presence of LAT1 could support the uptake of THs from the maternal circulation. Studies using western blotting and immunohistochemistry showed that LAT1 is mainly expressed in the apical membrane of the syncytiotrophoblast [47]. These results were consistent with our findings. In contrast, similar amounts of LAT2 were found in both the apical and basal membranes of syncytiotrophoblasts. It has been reported that LAT2 is present in the syncytiotrophoblast layer of human-term placenta, which is in agreement with our results [48, 49]. Other investigators demonstrated that LAT2 is localized in the apical plasma membrane [49]. This localization of LAT2 in the apical and basal membranes may explain the mechanism by which this transporter can regulate transfer of THs from the syncytiotrophoblast layer to the fetal circulation. OATP1A2 staining was localized in both syncytiotrophoblasts and cytotrophoblasts, and there were no differences between maternal and fetal placentas. The localization of OATP1A2 was previously described by Loubiere et al. [44], whose findings were similar to our own. Loubiere et al. found that OATP4A1 was predominantly located at the apical membrane of syncytiotrophoblasts. In our study, OATP4A1 was highly expressed in the apical side of the syncytiotrophoblast membrane, as previously demonstrated by Sato et al. [19]. Immunostaining of OATP4A1 was more intense in the syncytiotrophoblast layer of the maternal side of placentas compared with the fetal side. OATP4A1 is a Na+-independent TH transporter, which transports T3, T4, and rT3 [50]. The unsymmetrical localization in the syncytiotrophoblast indicated that OATP4A1 played an important role in transporting THs from the maternal circulation to the fetus. In the present study, we demonstrated that TTR was widely present in the apical side of the syncytiotrophoblast layer in human-term placenta and that immunostaining of TTR was increased in the trophoblast from the maternal side of placentas compared with that from the fetal side. It has been confirmed that trophoblasts synthesize TTR in the maternal and fetal placental compartments. Apical secretion of TTR would thus increase the maternal circulation of TTR through the apical membranes of the trophoblast and might accelerate the transport of maternal THs to the fetal circulation [25]. It has also been shown that 63% of TTR is secreted apically and 37% basally in JEG-3 cells, suggesting that TTR secreted by human-term placenta may account for the transfer of THs from the maternal to the fetal circulation. TTR, secreted and synthesized by the placenta, may contribute to transfer of maternal THs to the fetal circulation [25]. The increased expression of TTR at the maternal placenta may transfer maternal T4 to the fetal circulation. This result of our study indicated that TTR could be involved in a system where trophoblast TTR is secreted into the maternal circulation and effluxes back into the trophoblast. This mechanism could provide high levels of TTR at the maternal facing of the placenta, since secreted TTR could combine with maternal T4, supporting a hypothesis for priority transfer of T4 from the trophoblast into the fetal circulation.
In the present study, we found that iodine and TH transporters were mostly expressed in the syncytiotrophoblast of the maternal facing microvillous membrane, which may facilitate permeation of T4 and T3 from the maternal to the fetal circulation. These results verified the assumption that transplacental transport was mediated by maternal and fetal TH exchange, which served to balance fetal requirements with hormone levels of the mother.
The limitation of this study is only pregnant women from an iodine-sufficient city were studied, and the conclusion, therefore, shortage for the effect of iodine nutritional status on placental iodine and thyroid hormone distribution. At present, there is a lack of research on the association of iodine excess and placental iodine nutrition. A recent study has explored the relationship between iodine deficiency and placental iodine and maternal thyroid function [51]. It was reported in an animal study that iodine concentration in the placenta was related to the pre-gestational iodine nutrition status, and the concentration in the low-iodine-pregnant group was significantly lower than in the normal-pregnant group. Therefore, the effect of iodine status should be taken into consideration.
Conclusion
The results of this study supported the hypothesis that enzymatic deiodination of THs forms a barrier which reduces transplacental passage of these hormones. The maternal side of the placenta was found to play the major role in regulating hormone transfer, suggesting that enzymatic deiodination is controlled in some way by the thyroid status of the fetus. These changes might be important and help to stabilize transportation of THs between mother and fetus.
References
Glinoer D (1997) The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from physiology to pathology. Endocr Rev 18(3):404–433. https://doi.org/10.1210/edrv.18.3.0300
Delange F (2001) Iodine deficiency as a cause of brain damage. Postgrad Med J 77(906):217–220
Delange F (1998) Screening for congenital hypothyroidism used as an indicator of the degree of iodine deficiency and of its control. Thyroid 8(12):1185–1192. https://doi.org/10.1089/thy.1998.8.1185
Moleti M, Trimarchi F, Vermiglio F (2014) Thyroid physiology in pregnancy. Endocr Pract 20(6):589–596. https://doi.org/10.4158/EP13341.RA
Bidart JM, Lacroix L, Evain-Brion D, Caillou B, Lazar V, Frydman R, Bellet D, Filetti S, Schlumberger M (2000) Expression of Na+/I- symporter and Pendred syndrome genes in trophoblast cells. J Clin Endocrinol Metab 85(11):4367–4372. https://doi.org/10.1210/jcem.85.11.6969
Mitchell AM, Manley SW, Morris JC, Powell KA, Bergert ER, Mortimer RH (2001) Sodium iodide symporter (NIS) gene expression in human placenta. Placenta 22(2–3):256–258. https://doi.org/10.1053/plac.2000.0609
Di Cosmo C, Fanelli G, Tonacchera M, Ferrarini E, Dimida A, Agretti P, De Marco G, Vitti P, Pinchera A, Bevilacqua G, Naccarato AG, Viacava P (2006) The sodium-iodide symporter expression in placental tissue at different gestational age: an immunohistochemical study. Clin Endocrinol 65(4):544–548. https://doi.org/10.1111/j.1365-2265.2006.02577.x
Manley SW, Li H, Mortimer RH (2005) The BeWo choriocarcinoma cell line as a model of iodide transport by placenta. Placenta 26(5):380–386. https://doi.org/10.1016/j.placenta.2004.07.004
Bernal J (2007) Thyroid hormone receptors in brain development and function. Nature clinical practice. Endocrinol Metab 3(3):249–259. https://doi.org/10.1038/ncpendmet0424
Koopdonk-Kool JM, de Vijlder JJ, Veenboer GJ, Ris-Stalpers C, Kok JH, Vulsma T, Boer K, Visser TJ (1996) Type II and type III deiodinase activity in human placenta as a function of gestational age. J Clin Endocrinol Metab 81(6):2154–2158. https://doi.org/10.1210/jcem.81.6.8964844
Salvatore D, Bartha T, Harney JW, Larsen PR (1996) Molecular biological and biochemical characterization of the human type 2 selenodeiodinase. Endocrinology 137(8):3308–3315. https://doi.org/10.1210/endo.137.8.8754756
Kohrle J (1999) Local activation and inactivation of thyroid hormones: the deiodinase family. Mol Cell Endocrinol 151(1–2):103–119
Chan S, Kachilele S, Hobbs E, Bulmer JN, Boelaert K, McCabe CJ, Driver PM, Bradwell AR, Kester M, Visser TJ, Franklyn JA, Kilby MD (2003) Placental iodothyronine deiodinase expression in normal and growth-restricted human pregnancies. J Clin Endocrinol Metab 88(9):4488–4495. https://doi.org/10.1210/jc.2003-030228
Grumbach MM, Werner SC (1956) Transfer of thyroid hormone across the human placenta at term. J Clin Endocrinol Metab 16(10):1392–1395. https://doi.org/10.1210/jcem-16-10-1392
Vulsma T, Gons MH, de Vijlder JJ (1989) Maternal-fetal transfer of thyroxine in congenital hypothyroidism due to a total organification defect or thyroid agenesis. N Engl J Med 321(1):13–16. https://doi.org/10.1056/NEJM198907063210103
James SR, Franklyn JA, Kilby MD (2007) Placental transport of thyroid hormone. Best practice and research. Clin Endocrinol Metab 21(2):253–264. https://doi.org/10.1016/j.beem.2007.03.001
Chan SY, Vasilopoulou E, Kilby MD (2009) The role of the placenta in thyroid hormone delivery to the fetus. Nature clinical practice. Endocrinol Metab 5(1):45–54. https://doi.org/10.1038/ncpendmet1026
Landers KA, McKinnon BD, Li H, Subramaniam VN, Mortimer RH, Richard K (2009) Carrier-mediated thyroid hormone transport into placenta by placental transthyretin. J Clin Endocrinol Metab 94(7):2610–2616. https://doi.org/10.1210/jc.2009-0048
Sato K, Sugawara J, Sato T, Mizutamari H, Suzuki T, Ito A, Mikkaichi T, Onogawa T, Tanemoto M, Unno M, Abe T, Okamura K (2003) Expression of organic anion transporting polypeptide E (OATP-E) in human placenta. Placenta 24(2–3):144–148
Chan SY, Franklyn JA, Pemberton HN, Bulmer JN, Visser TJ, McCabe CJ, Kilby MD (2006) Monocarboxylate transporter 8 expression in the human placenta: the effects of severe intrauterine growth restriction. J Endocrinol 189(3):465–471. https://doi.org/10.1677/joe.1.06582
Kinne A, Kleinau G, Hoefig CS, Gruters A, Kohrle J, Krause G, Schweizer U (2010) Essential molecular determinants for thyroid hormone transport and first structural implications for monocarboxylate transporter 8. J Biol Chem 285(36):28054–28063. https://doi.org/10.1074/jbc.M110.129577
van Mullem AA, van Gucht ALM, Visser WE, Meima ME, Peeters RP, Visser TJ (2016) Effects of thyroid hormone transporters MCT8 and MCT10 on nuclear activity of T3. Mol Cell Endocrinol 437:252–260. https://doi.org/10.1016/j.mce.2016.07.037
Ritchie JW, Taylor PM (2001) Role of the system L permease LAT1 in amino acid and iodothyronine transport in placenta. Biochem J 356(Pt 3):719–725
Landers KA, Li H, Subramaniam VN, Mortimer RH, Richard K (2013) Transthyretin-thyroid hormone internalization by trophoblasts. Placenta 34(8):716–718. https://doi.org/10.1016/j.placenta.2013.05.005
McKinnon B, Li H, Richard K, Mortimer R (2005) Synthesis of thyroid hormone binding proteins transthyretin and albumin by human trophoblast. J Clin Endocrinol Metab 90(12):6714–6720. https://doi.org/10.1210/jc.2005-0696
Patel J, Landers KA, Li H, Mortimer RH, Richard K (2011) Ontogenic changes in placental transthyretin. Placenta 32(11):817–822. https://doi.org/10.1016/j.placenta.2011.09.007
Reyns GE, Janssens KA, Buyse J, Kuhn ER, Darras VM (2002) Changes in thyroid hormone levels in chicken liver during fasting and refeeding. Comp Biochem Physiol B Biochem Mol Biol 132(1):239–245
Reyns GE, Verhoelst CH, Kuhn ER, Darras VM, Van der Geyten S (2005) Regulation of thyroid hormone availability in liver and brain by glucocorticoids. Gen Comp Endocrinol 140(2):101–108. https://doi.org/10.1016/j.ygcen.2004.10.006
Castro MI, Braverman LE, Alex S, Wu CF, Emerson CH (1985) Inner-ring deiodination of 3,5,3′-triiodothyronine in the in situ perfused guinea pig placenta. J Clin Invest 76(5):1921–1926. https://doi.org/10.1172/JCI112188
Obregon MJ, Ruiz de Ona C, Hernandez A, Calvo R, Escobar del Rey F, Morreale de Escobar G (1989) Thyroid hormones and 5′-deiodinase in rat brown adipose tissue during fetal life. Am J Phys 257(5 Pt 1):E625–E631. https://doi.org/10.1152/ajpendo.1989.257.5.E625
Hernandez A, Obregon MJ (1995) Presence of growth factors-induced type III iodothyronine 5-deiodinase in cultured rat brown adipocytes. Endocrinology 136(10):4543–4550. https://doi.org/10.1210/endo.136.10.7664675
Burns R, O'Herlihy C, Smyth PP (2013) Regulation of iodide uptake in placental primary cultures. Eur Thyroid J 2(4):243–251. https://doi.org/10.1159/000356847
Li H, Patel J, Mortimer RH, Richard K (2012) Ontogenic changes in human placental sodium iodide symporter expression. Placenta 33(11):946–948. https://doi.org/10.1016/j.placenta.2012.08.002
Schroder-van der Elst JP, van der Heide D, Kastelijn J, Rousset B, Obregon MJ (2001) The expression of the sodium/iodide symporter is up-regulated in the thyroid of fetuses of iodine-deficient rats. Endocrinology 142(9):3736–3741. https://doi.org/10.1210/endo.142.9.8377
Mortimer RH, Galligan JP, Cannell GR, Addison RS, Roberts MS (1996) Maternal to fetal thyroxine transmission in the human term placenta is limited by inner ring deiodination. J Clin Endocrinol Metab 81(6):2247–2249. https://doi.org/10.1210/jcem.81.6.8964859
Cooper E, Gibbens M, Thomas CR, Lowy C, Burke CW (1983) Conversion of thyroxine to 3,3′,5′-triiodothyronine in the guinea pig placenta: in vivo studies. Endocrinology 112(5):1808–1815. https://doi.org/10.1210/endo-112-5-1808
Kurlak LO, Mistry HD, Kaptein E, Visser TJ, Broughton Pipkin F (2013) Thyroid hormones and their placental deiodination in normal and pre-eclamptic pregnancy. Placenta 34(5):395–400. https://doi.org/10.1016/j.placenta.2013.02.009
Weeke J, Dybkjaer L, Granlie K, Eskjaer Jensen S, Kjaerulff E, Laurberg P, Magnusson B (1982) A longitudinal study of serum TSH, and total and free iodothyronines during normal pregnancy. Acta Endocrinol 101(4):531–537
Laurberg P, Andersen SL, Pedersen IB, Andersen S, Carle A (2013) Screening for overt thyroid disease in early pregnancy may be preferable to searching for small aberrations in thyroid function tests. Clin Endocrinol 79(3):297–304. https://doi.org/10.1111/cen.12232
Huang SA, Dorfman DM, Genest DR, Salvatore D, Larsen PR (2003) Type 3 iodothyronine deiodinase is highly expressed in the human uteroplacental unit and in fetal epithelium. J Clin Endocrinol Metab 88(3):1384–1388. https://doi.org/10.1210/jc.2002-021291
Steinsapir J, Bianco AC, Buettner C, Harney J, Larsen PR (2000) Substrate-induced down-regulation of human type 2 deiodinase (hD2) is mediated through proteasomal degradation and requires interaction with the enzyme's active center. Endocrinology 141(3):1127–1135. https://doi.org/10.1210/endo.141.3.7355
Akturk M, Oruc AS, Danisman N, Erkek S, Buyukkagnici U, Unlu E, Tazebay UH (2013) Na+/I- symporter and type 3 iodothyronine deiodinase gene expression in amniotic membrane and placenta and its relationship to maternal thyroid hormones. Biol Trace Elem Res 154(3):338–344. https://doi.org/10.1007/s12011-013-9748-y
Perez-Lopez FR (2007) Iodine and thyroid hormones during pregnancy and postpartum. Gynecol Endocrinol 23(7):414–428. https://doi.org/10.1080/09513590701464092
Loubiere LS, Vasilopoulou E, Bulmer JN, Taylor PM, Stieger B, Verrey F, McCabe CJ, Franklyn JA, Kilby MD, Chan SY (2010) Expression of thyroid hormone transporters in the human placenta and changes associated with intrauterine growth restriction. Placenta 31(4):295–304. https://doi.org/10.1016/j.placenta.2010.01.013
Cleal JK, Glazier JD, Ntani G, Crozier SR, Day PE, Harvey NC, Robinson SM, Cooper C, Godfrey KM, Hanson MA, Lewis RM (2011) Facilitated transporters mediate net efflux of amino acids to the fetus across the basal membrane of the placental syncytiotrophoblast. J Physiol 589(Pt 4):987–997. https://doi.org/10.1113/jphysiol.2010.198549
Prasad PD, Wang H, Huang W, Kekuda R, Rajan DP, Leibach FH, Ganapathy V (1999) Human LAT1, a subunit of system L amino acid transporter: molecular cloning and transport function. Biochem Biophys Res Commun 255(2):283–288. https://doi.org/10.1006/bbrc.1999.0206
Gaccioli F, Aye IL, Roos S, Lager S, Ramirez VI, Kanai Y, Powell TL, Jansson T (2015) Expression and functional characterisation of system L amino acid transporters in the human term placenta. Reprod Biol Endocrinol 13:57. https://doi.org/10.1186/s12958-015-0054-8
Hoeltzli SD, Smith CH (1989) Alanine transport systems in isolated basal plasma membrane of human placenta. Am J Phys 256(3 Pt 1):C630–C637. https://doi.org/10.1152/ajpcell.1989.256.3.C630
Lewis RM, Glazier J, Greenwood SL, Bennett EJ, Godfrey KM, Jackson AA, Sibley CP, Cameron IT, Hanson MA (2007) L-serine uptake by human placental microvillous membrane vesicles. Placenta 28(5–6):445–452. https://doi.org/10.1016/j.placenta.2006.06.014
Fujiwara K, Adachi H, Nishio T, Unno M, Tokui T, Okabe M, Onogawa T, Suzuki T, Asano N, Tanemoto M, Seki M, Shiiba K, Suzuki M, Kondo Y, Nunoki K, Shimosegawa T, Iinuma K, Ito S, Matsuno S, Abe T (2001) Identification of thyroid hormone transporters in humans: different molecules are involved in a tissue-specific manner. Endocrinology 142(5):2005–2012. https://doi.org/10.1210/endo.142.5.8115
Sun X, Lu L, Shan L, Shan Z, Teng W (2017) Iodine storage and metabolism of mild to moderate iodine-deficient pregnant rats. Thyroid 27(6):846–851. https://doi.org/10.1089/thy.2016.0611
Funding
This study was funded by the Chinese National Science Foundation (grant numbers 81170730, 81570709, 81670719) and 973 Plan preliminary research project (2011CB512112).
Author information
Authors and Affiliations
Contributions
SP and CL performed the experimental work, analyzed the results, and composed the manuscript. XX, XZ, and DW performed the study and collected the samples. XL reviewed and edited the manuscript. MS and TM participated in the experiments. SW and YJ collected the general information of study populations and contributed to the interpretation and analysis of data; ZS helped with coordination of this study; WT supervised the statistical analyses; contributed to the design of the study, analyses, and interpretation of the results; and produced the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peng, S., Li, C., Xie, X. et al. Divergence of Iodine and Thyroid Hormones in the Fetal and Maternal Parts of Human-Term Placenta. Biol Trace Elem Res 195, 27–38 (2020). https://doi.org/10.1007/s12011-019-01834-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-019-01834-z