Abstract
Background
No study has evaluated the cardiovascular effects of diazepam in elderly subjects that assume diazepam to induce sleep.
Purpose
The present study was carried out in order to evaluate the effects of chronic administration of diazepam as hypnotic drug on blood pressure (BP) and heart rate (HR) in healthy elderly subjects.
Patients and methods
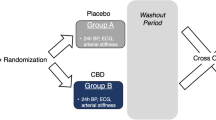
Healthy, elderly subjects, aged 65–74 years, were treated with diazepam 5 mg or placebo—both administered once a day in the evening—for 4 weeks in two cross-over periods, each separated by a 2-week placebo period, according to a randomized, double-blind, cross-over design. At the end of each study period, clinical as well as 24-h ambulatory BP and HR were evaluated.
Results
A total of 25 subjects were included in the analysis. At the end of a 4-week diazepam treatment, clinical as well 24-h BP and HR mean values were not significantly affected. Analysis of sub-periods showed that during night-time, systolic BP (SBP) values under diazepam were 7.6% higher than under placebo, with a mean difference of 7.9 mmHg (p < 0.01), diastolic BP (DBP) values were 5.8% higher, with a mean difference of 3.7 mmHg (p < 0.05 vs placebo) and HR values were 6.6% higher with a mean difference of 4.2 b/min (p < 0.05). The HR increase observed with diazepam persisted during the morning hours, whereas during the afternoon and evening hours SBP, DBP and HR values were similar in the two treatment groups.
Conclusions
In elderly subjects chronic assumption of diazepam as hypnotic agent produced an increase in BP, in particular SBP, during night-time and of HR during night-time and morning hours. These effects, which probably depend on a diazepam-mediated increase in sympathetic drive and decrease in vagal tone, might be of clinical relevance due to the role of increased BP and HR as independent predictors of cardiovascular morbidity and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prevalence of insomnia is known to increase with age, and benzodiazepines (BDZ) are the most widely prescribed hypnotic drugs: observational studies suggest that 13–25% of subjects aged 65 or older regularly assume BDZ to induce sleep [1, 2]. Several reports have demonstrated that chronic use of BDZ is associated with both cognitive/psycho-motorial impairment [3] and increased risk of falls [4]. Conversely, a few studies have assessed the cardiovascular effects of BDZ, in particular those of diazepam, which is one of the most used BDZ and the only one which does not seem to increase the risk of falls in elderly persons [5].
The studies which assessed the cardiovascular effects of diazepam in young and adult individuals, although not univocal and difficult to compare due to their great methodological variety, yet suggest that diazepam assumption produces, on the one hand, an attenuation of sympathetic drive, with consequent slight reduction of blood pressure (BP) [6] and, on the other hand, a reduction of vagal tone, with consequent heart rate (HR) increase [7, 8]. These findings, however, cannot be shifted to elderly subjects, since pharmacokinetic properties of diazepam—as well as its receptor binding properties—significantly change with increasing age.
As to the pharmacokinetic characteristics, diazepam’s steady-state plasma levels are attained more slowly and reach higher values in elderly patients, while elimination half-life of the drug is three to fourfold greater than in the young patients [9]. These characteristics are mainly related to the increase in the diazepam’s volume of distribution in elderly subjects, and this depends, in turn, on age-related changes in the relative proportion of adipose and lean tissues [10, 11]. A minor role seems to be played by the clearance rate of the drug from the systemic circulation, which is only slightly reduced [11].
With respect to the age-related changes in diazepam receptor binding, a reduced sensitivity of BDZ receptors to their agonist with increasing age has been described [12, 13]. This seems to be due neither to a reduced binding potential nor to a reduced receptor number, but rather to an alteration of the GABA-BDZ receptor complex, that modifies its molecular composition and pharmacological properties [14]. In particular, a decrease in γ2 molecular subunit expression has been described in the elderly [15, 16].
Only two observational studies have specifically evaluated the cardiovascular effects of diazepam in the elderly: the first one included subjects over 70 years with coronary heart disease in which intravenous administration of diazepam was accompanied by a slight and transient increase in BP [17]; the other one concerned patients aged 60 years and over in which diazepam was administered as a pre-medication before cataract surgery and it reduced the BP rise that often occurs during this operation [18]. To the best of our knowledge, to date no study has evaluated the cardiovascular effects of diazepam in a large population of healthy elderly subjects chronically assuming diazepam to induce sleep.
With this background, the present study was undertaken to assess the effects of chronic evening administration of diazepam on clinical and 24-h ambulatory BP and HR in healthy, elderly subjects.
Patients and methods
Both male and female healthy volunteers, between 65 and 74 years, were enrolled in this randomized, double-blind, cross-over study, subject to their compliance with the following inclusion criteria: normal blood pressure values (sitting SBP < 140 mmHg and DBP < 90 mmHg) at the end of an initial 2 week placebo period; normal depression and anxiety evaluation (scores < 16 on the Hamilton Rating Scale for Depression, HRSD and < 14 on the Hamilton Rating Scale for Anxiety, HRSA); normal BMI (< 24.9 kg/m2); no use of any type of drugs, no smoking habit; normal ECG; and normal kidney function (serum creatinine < 1.3 mg/dL, eGFR ≥ 90 mL/min per 1.73 m2, albumin excretion rate < 30 mg/24 h). Subjects with diabetes mellitus, hepatic failure, pregnancy, history of cardiovascular events or known hypersensibility to the drugs used in the study were excluded.
The study protocol was approved by the local Ethical Committee, and informed consent in writing was obtained from all volunteers at the time of their enrolment. Following an initial 2-week, wash-out period during which placebo was administered and any eventual drug was withdrawn, the subjects satisfying the inclusion/exclusion criteria were randomized to treatment either with diazepam 5 mg or placebo, both administered once per day at the same hour in the evening (between 10 p.m. and 11 p.m.) for 4 weeks in two cross-over periods, each separated by a 2 week placebo period. A 2-week, placebo wash-out period between the first and the second cross-over periods was considered to be sufficient to prevent any carry-over effect or, more generally, a treatment-by-period interaction [19]. To maintain double-blindness, diazepam and placebo were provided in capsules of identical appearance (i.e., same size, color and taste). At the end of each study period, clinical and non-invasive 24-h ambulatory BP and HR were assessed. Clinical BP and HR were measured in the morning, about 10–11 h after drug assumption, by a standard mercury sphygmomanometer and by pulse palpation in seated subjects. Three BP measurements were taken at 2-min intervals after 10 min of sitting and their averages were used as clinical BP reference values. Ambulatory BP and HR monitoring was performed by a clinically validated device (Spacelabs 90207, Spacelabs Inc, Redmond, Washington) [20] that was programmed to take BP every 15 min during the entire course of the recording. Each recording was started in the morning immediately after clinical BP measurement and was performed throughout a full 24 h period, during which subjects were allowed to follow their normal daily routine after they left the laboratory. Patients were instructed to remain motionless each time a reading was taken. The analysis of 24-h BP recordings was preceded by removal of artifacts, according to previously described editing criteria [20]. Recordings were excluded from the analysis when more than 10% of all readings, or more than one reading per hour, were missing or incorrect. For each patient, the following data relating to SBP, DBP and HR were provided by the computed analysis of the recordings: 24-h, daytime (7 a.m.–11 p.m.), night-time (11 p.m.–7 a.m.) and morning (7 a.m.–12 p.m.) mean values. At each visit, adverse events spontaneously reported were recorded.
Statistical analysis
The statistical analysis was performed using analysis of variance (ANOVA). In order to verify the basic assumptions of cross-over design, besides the estimation of periodic effects, the presence of carry-out or sequence effect was also investigated [19]. However, a period effect or, more significantly, a sequence effect was not found for any variables. Statistical analysis of data was performed by means of the SPSS statistical software package for Windows (version 11.0: Chicago, Illinois, USA); data are presented as means ± standard deviations. Paired tests were also used: a one-sample t test was used to compare values obtained after treatment administration; a two-sample t test was used to compare the change score (treatment-placebo) for a given parameter between the two groups. For all statistical analyses, a p value of < 0.05 was considered statistically significant.
Results
Out of the 30 healthy elderly subjects recruited for the study, only 25 had the first ambulatory blood pressure recording, meeting the quality criteria previously defined, and thus only these 25 subjects were randomized to treatment with placebo or diazepam and included in the analysis. Their main demographic and clinical characteristics are shown in Table 1.
The main results of the study are reported in Table 2. Ambulatory monitoring data showed that 24-h SBP, DBP and HR mean values were not significantly affected by diazepam. However, when analyzing separately the sub-periods of the day, different behaviors were observed. During night-time, that is over the 8 h immediately following the drug or placebo ingestion, both treatment preserved the physiologic BP and HR reduction as compared to day-time values. However, during diazepam administration their values were higher than those observed under placebo: in particular, SBP value was 7.6% higher than that observed under placebo with a mean difference of 7.9 mmHg (p < 0.01 vs placebo), whereas DBP value was 5.8% higher with a mean difference of 3.7 mmHg (p < 0.05 vs placebo). HR means values were 6.6% higher than those observed under placebo with a mean difference of 4.2 beats/min (p < 0.05).
In the morning hours, i.e. during the 5 h following awakening, both diazepam and placebo administration preserved the physiologic increase in HR and BP as compared to night-time values. However, HR mean values were still 4.4% higher with diazepam as compared to placebo, with a mean difference of 3.3 beats/min (p < 0.05). By contrast, morning SBP and DBP mean values were similar in diazepam and placebo treated subjects.
During the afternoon–evening hours (12 p.m.–11 p.m.), HR as well as SBP and DBP mean values were not significantly different in the two treatment groups.
Clinical BP and HR results are shown in Table 3: no significant difference was detected between diazepam and placebo-treated subjects.
With regards to adverse events spontaneously reported by the diazepam-treated volunteers, eight of them complained of mild difficulty in awakening and four of them also reported mild somnolence during the first daily hours, four complained of dry mouth at awakening, two reported occasional nocturnal palpitations and one reported an episode of nocturnal awakening with agitation and tachycardia (with an auto-measured HR at pulse palpation of about 100–110 beats/min), which persisted for about 1 h and resolved spontaneously. No episode of fall either spontaneously reported or elicited by specific questioning was detected.
Discussion
The main finding of the present study is that during night-time, i.e., in the hours following drug administration, when its plasma concentration is higher, diazepam, although not interfering with the circadian decrease in BP and HR, significantly affected BP and HR values. In fact, both BP and HR values decreased less than under placebo, with particular regard to SBP. This type of BP behavior was completely and qualitatively different from the one observed in young adults: these latter ones, when evaluated with the same methodology and treated with the same dosage of diazepam, showed nocturnal BP values not different from placebo treated controls [8]. This unexpected effect of diazepam in the elderly could be at least theoretically explained bearing in mind several factors that change with increasing age: firstly, the alterations of GABAA/BDZ receptors and their consequences; secondly, the neurohormonal changes affecting the mechanisms that regulate circulation; finally, the different pharmacokinetic properties of diazepam in the elderly subject.
As regards the first issue, the age-related modifications in the subunit composition of the GABAA receptor and the consequent disruption of the GABAminergic transmission [15, 16] could interfere with the agonist effect of BDZ on the inhibitory functions of GABA system, which affect BP through the sympathetic outflow. This latter can be increased or reduced depending on the brain regions mostly involved [21,22,23], as well as on the presence or not of anxiety [24]. In young subjects without anxiety and depression, the stimulating effect on sympathetic outflow is probably counterbalanced by the sympathetic inhibitory effect, with no significant influence of diazepam on BP values, which are substantially superimposable to those observed with placebo, particularly during night-time [8].
In the elderly, the age-related receptor alterations could be responsible for a disruption of the balance between the activating and inhibitory effect of diazepam on sympathetic drive, with consequent less reducing effect on sympathetic drive. In this regard, it should be considered that genetically hypertensive rats and mice—such as spontaneously hypertensive rats (SHR) and Schlager BPH/2 mice—have a marked alteration of GABA system function with GABA receptors totally resistant to diazepam stimulation, which results in excessive sympathetic activation [25, 26]. In elderly humans, the GABA receptor system is not so altered as in genetically hypertensive rats, but its partial alteration could be enough to reduce all the cardiovascular effects mediated by BDZ stimulation of GABA receptors. In particular it seems to be blunted the inhibitory effect of BDZ on sympathetic activity, which is already significantly increased in the elderly as compared to younger age, as demonstrated by the high levels of plasma and urinary catecholamines [27,28,29]. This rise in catecholamine levels does not seem to depend on an increased synthesis in adrenal glands, which indeed significantly decreases with advancing age [30, 31], but rather it seems to be an expression of an increased sympathetic activity. This increase in endogenous noradrenaline release occurs in the presence of circulating diazepam, which has been demonstrated to induce a potentiation of the c-AMP-dependent positive inotropic effect of endogenous noradrenaline in the heart via the selective inhibition of phoshodiesterase 4 isoenzyme activity [32]. As a consequence, in the elderly this positive inotropic effect of diazepam should likely be increased. When considering that diazepam, due to its specific pharmacokinetic properties, reaches higher plasma concentrations in the elderly as compared to young adults, it seems clear that its positive inotropic effect can only be increased, particularly in the presence of the highest plasma concentrations of the drug, i.e., in the night-time. An increased inotropism could per se produce a rise in SBP, but this effect is amplified in the presence of an increased arterial stiffness, which is associated with advancing age [33,34,35].
The observed increase in HR values during treatment with diazepam as compared to placebo is in accordance with previous experimental and clinical findings and has been related to the vagolytic effect due to the stimulation of the BDZ site of the GABAA/BDZ receptor complex. It is of interest to remark that in young adults evaluated with the same methodology and diazepam dosage such HR increase persisted over the entire 24-h period [8], whereas in old subjects it was present only during night-time and in the morning hours. This different HR behavior seems to confirm that in the elderly the GABAA/BDZ receptor system is less responsive to BDZ stimulation and produce peripheral effects, as the vagolytic one, only in the presence of high plasma concentrations of the drug.
As regards the adverse events, they were limited, mild and never demanded treatment withdrawn. The more frequently reported side effects were mild difficulty in awakening with persistence of light somnolence in the early morning hours and dry mouth at awakening. The subject who complained of a single episode of agitation with nocturnal tachycardia underwent further cardiologic examination, including basal and 24-h ECG recordings, stress ECG and echocardiogram. The outcome if these examinations resulted to be normal both at the end of the study and at an another control repeated after 1 month under treatment with placebo and the same dose of diazepam. It is of interest that no patient complained of falls. This finding, which confirms previous data in the literature [5] could some way be related to the cardiovascular effects of diazepam or perhaps only to the relatively “young” age of our elderly patients coupled to the absence of comorbidities.
The present study however had some limitations. First, the duration of the trial was of only 4 weeks, which does not allow us to transfer our findings to more prolonged diazepam treatment. It is well known that chronic benzodiazepine therapy is accompanied by the development of tolerance regarding the anti-anxiety, relaxant and hypnotic effects of these drugs, but nowadays we do not know whether these phenomena also influence their cardiovascular effects. Second, in the present study we did not specifically evaluate the effect of diazepam therapy on cognitive function, which can be impaired by chronic treatment with benzodiazepines. We limited ourselves to observe that no patient spontaneously complained of memory impairment, learning difficulty or car accidents.
Conclusions
The results of this study showed that chronic diazepam assumption, as hypnotic agent in healthy normotensive elderly subjects, mainly resulted in an increase in BP, particularly in SBP, during night-time and in HR during night-time and morning hours. These findings, which could be possibly related to a diazepam-induced increase in sympathetic dive and decrease in vagal tone, might be of clinical relevance since increased BP and HR are both independent predictors of cardiovascular morbidity and mortality [36, 37].
References
Morgan K, Dallosso H, Ebrahim S et al (1988) Prevalence, frequency, and duration of hypnotic drug use among the elderly living at home. Br Med J (Clin Res Ed) 296:601–602
Jackson G, Gerard C, Minko N et al (2014) Variation in benzodiazepine and antipsychotic use in people aged 65 years and over in New Zealand. N Z Med J 127:67–78
Fancourt G, Castleden M (1986) The use of benzodiazepines with particular reference to the elderly. Br J Hosp Med 35:321–326
Pariente A, Dartigues JF, Benichou J et al (2008) Benzodiazepines and injurious falls in community dwelling elders. Drugs Aging 25:61–70
Tamblyn R, Abrahamowicz M, du Berger R et al (2005) A 5-year prospective assessment of the risk associated with individual benzodiazepines and doses in new elderly users. J Am Geriatr Soc 53:233–241
Kitajima T, Kanbayashi T, Saito Y et al (2004) Diazepam reduces both arterial blood pressure and muscle sympathetic nerve activity in human. Neurosci Lett 355:77–80
Adinoff B, Mefford I, Waxman R et al (1992) Vagal tone decreases following intravenous diazepam. Psychiatry Res 41:89–97
Costa A, Bosone D, Zoppi A et al (2018) Effect of diazepam on 24 hour blood pressure and heart rate in healthy volunteers. Pharmacology 101:85–91
Klotz U, Avant GR, Hoyumpa A et al (1975) The effects of age and liver disease on the disposition and elimination of diazepam in adult man. J Clin Investig 55:347–359
Ochs HR, Greenblatt DJ, Divoll M et al (1981) Diazepam kinetics in relation to age and sex. Pharmacology 23:24–30
Herman RJ, Wilkinson GR (1996) Disposition of diazepam in young and elderly subjects after acute and chronic dosing. Br J Clin Pharmacol 42:147–155
Greenblatt DJ, Shader RI, Harmatz JS (1989) Implications of altered drug disposition in the elderly: studies of benzodiazepines. J Clin Pharmacol 29:866–872
Dalezios Y, Matsokis N (1998) Brain benzodiazepine binding in aged rats. Neurochem Int 32:213–217
Suhara T, Inoue O, Kobayashi K et al (1993) No age-related changes in human benzodiazepine receptor binding measured by PET with [11C]Ro 15-4513. Neurosci Lett 159:207–210
Rissman RA, De Blas AL, Armstrong DM (2007) GABA(A) receptors in aging and Alzheimer’s disease. J Neurochem 103:1285–1292
Hoekzema E, Rojas S, Herance R et al (2012) In vivo molecular imaging of the GABA/benzodiazepine receptor complex in the aged rat brain. Neurobiol Aging 33:1457–1465
Lepage JY, Blanloeil Y, Pinaud M et al (1986) Hemodynamic effects of diazepam, flunitrazepam, and midazolam in patients with ischemic heart disease: assessment with a radionuclide approach. Anesthesiology 65:678–683
Cakmak H, Kocaturk T, Dundar SO et al (2014) The effects of diazepam on blood pressure levels in cataract surgery. Saudi Med J 35:669–673
Senn S (1993) Cross-over trials in clinical research, 1st edn. Wiley, New York, pp 10–53
Parati G, Bosi S, Castellano M et al (1995) Guidelines for 24-h non-invasive ambulatory blood pressure monitoring: report from the Italian Society of Hypertension. High Blood Press 4:168–174
Wong TP (2002) Aging of the cerebral cortex. MJM 6:104–113
Kubo T, Okatani H, Nishigori Y et al (2004) Involvement of the medial amygdaloid nucleus in restraint stress-induced pressor responses in rats. Neurosci Lett 354:84–86
Davern PJ, Head GA (2011) Role of the medial amygdala in mediating responses to aversive stimuli leading to hypertension. Clin Exp Pharmacol Physiol 38:136–143
Sorock GS, Shimkin EE (1988) Benzodiazepine sedatives and the risk of falling in a community-dwelling elderly cohort. Arch Intern Med 148:2441–2444
Kunkler PE, Hwang BH (1995) Lower GABAA receptor binding in the amygdala and hypothalamus of spontaneously hypertensive rats. Brain Res Bull 36:57–61
Davern PJ, Chowdhury S, Jackson KL et al (2014) GABAA receptor dysfunction contributes to high blood pressure and exaggerated response to stress in Schlager genetically hypertensive mice. J Hypertens 32:352–362
Blandini F, Martignoni E, Melzi d’Eril GV et al (1992) Free plasma catecholamine levels in healthy subjects: a basal and dynamic study. The influence of age. Scand J Clin Lab Investig 52:9–17
Deane R, Chummun H, Prashad D (2002) Differences in urinary stress hormones in male and female nurses at different ages. J Adv Nurs 37:304–310
Saxena AR, Chamarthi B, Williams GH et al (2014) Predictors of plasma and urinary catecholamine levels in normotensive and hypertensive men and women. J Hum Hypertens 28:292–297
Gerlo EA, Schoors DF, Dupont AG (1991) Age- and sex-related differences for the urinary excretion of norepinephrine, epinephrine, and dopamine in adults. Clin Chem 37:875–878
Amano A, Tsunoda M, Aigaki T et al (2013) Age-related changes of dopamine, noradrenaline and adrenaline in adrenal glands of mice. Geriatr Gerontol Int 13:490–496
Juan-Fita MJ, Vargas ML, Hernández J (2003) Comparative actions of diazepam and other phosphodiesterase inhibitors on the effects of noradrenaline in rat myocardium. Pharmacol Toxicol 93:23–28
McEniery CM, Wilkinson IB, Avolio AP (2007) Age, hypertension and arterial function. Clin Exp Pharmacol Physiol 34:665–671
Lim MA, Townsend RR (2009) Arterial compliance in the elderly: its effect on blood pressure measurement and cardiovascular outcomes. Clin Geriatr Med 25:191–205
Yannoutsos A, Ahouah M, Dreyfuss Tubiana C et al (2018) Aortic stiffness improves the prediction of both diagnosis and severity of coronary artery disease. Hypertens Res 41:118–125
Ho JE, Larson MG, Ghorbani A et al (2014) Long-term cardiovascular risks associated with an elevated heart rate: the Framingham Heart Study. J Am Heart Assoc 3:e000668
Collins R, MacMahon S (1994) Blood pressure, antihypertensive drug treatment and the risks of stroke and of coronary heart disease. Br Med Bull 50:272–298
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the present study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
A written informed consent for the research protocol was obtained from all individual participants included in the study population.
Rights and permissions
About this article
Cite this article
Fogari, R., Costa, A., Zoppi, A. et al. Diazepam as an oral hypnotic increases nocturnal blood pressure in the elderly. Aging Clin Exp Res 31, 463–468 (2019). https://doi.org/10.1007/s40520-018-0991-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-0991-0