Abstract
As major sporting events are often held in hot environments, increased interest in ways of optimally heat acclimating athletes to maximise performance has emerged. Heat acclimation involves repeated exercise sessions in hot conditions that induce physiological and thermoregulatory adaptations that attenuate heat-induced performance impairments. Current evidence-based guidelines for heat acclimation are clear, but the application of these recommendations is not always aligned with the time commitments and training priorities of elite athletes. Alternative forms of heat acclimation investigated include hot water immersion and sauna bathing, yet uncertainty remains around the efficacy of these methods for reducing heat-induced performance impairments, as well as how this form of heat stress may add to an athlete’s overall training load. An understanding of how to optimally prescribe and periodise heat acclimation based on the performance determinants of a given event is limited, as is knowledge of how heat acclimation may affect the quality of concurrent training sessions. Finally, differences in individual athlete responses to heat acclimation need to be considered. This article addresses alternative methods of heat acclimation and heat exposure, explores gaps in literature around understanding the real world application of heat acclimation for athletes, and highlights specific athlete considerations for practitioners.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Post-exercise sauna bathing and/or hot water immersion may represent a practical means of implementing heat acclimation (HA) in athletes when barriers to traditional exercise-based HA are present. |
To optimise HA, the timing of implementation, sport specificity and other concurrent training sessions should all be considered in order to maintain training quality and maximise performance in the heat. |
Several unique athlete considerations, including their history and physical characteristics, should be understood by practitioners before implementing HA protocols, as individual characteristics often elicit different heat stress and HA responses. |
1 Introduction
Several major sporting events are held each year in hot environments. Some of the largest high profile events, including most Summer Olympic Games, the Tour de France, the FIFA World Cup, as well as several annual World Cups and World Championships are held in the summer months when high temperatures are often expected. For athletes and support teams preparing for pinnacle events, executing performance to their maximum potential is of the utmost importance. Heat-induced performance decrements can range from 6 to 16% in trained athletes during endurance and team sport events [1–3], while lack of acclimation is a major risk factor for exertional heat injury (EHI) [4]. Heat acclimation (HA) or acclimatisation involves repeated exercise sessions in hot conditions (typically ~30–40 °C, 20–60% relative humidity (RH) for athletic circumstances) either by artificial means (acclimation; heated room or chamber) or outdoors (acclimatisation; hot ambient temperature), and is a routine strategy employed to induce physiological adaptations that will attenuate heat-induced performance impairments and offer protection against heat stress and EHI [5–7]. Recent consensus recommendations offer practitioners an understanding of the key concepts needed to prescribe HA for individual and team sport athletes [8, 9]. Briefly, these best practice guidelines state that HA should be comprised of daily ~60 min training sessions in hot conditions for a minimum of 1 week, and ideally over 2 weeks to achieve further thermoregulatory and performance benefits. The HA protocol should mimic the event demands while inducing high sweat rates and increased body (skin and core) temperature [9].
A number of scenarios have been proposed in the literature to administer HA within an athlete’s season to maximise performance in hot conditions, including pre- or in-season training camps to augment the training response, or as a taper tool when training volume is reduced and high-intensity quality is to be maintained [8, 9]. While such recommendations are based on decades of evidence, limitations and barriers to adhering to such guidelines, within the context of elite athlete training needs, pose frequent conundrums for coaches and sport scientists. In short, best practice guidelines are often not entirely attainable within the confines of highly demanding physical preparation and travel, which are necessary requirements for the elite athlete. The purpose of this current opinion piece, therefore, is to review alternative methods of HA and heat exposure, explore the gaps in literature for understanding how HA might be integrated into an athlete’s existing training program, and highlight specific athlete considerations for practitioners.
2 Alternative Heat Acclimation (HA) Methods
Sport-specific HA, simulating competition-like conditions, is now considered best practice HA for athletes [9]. Unfortunately, several barriers may prevent athletes from achieving HA in this way, especially for those athletes living in cold-to-temperate climates. HA protocol design challenges may include limited access to environmental chambers, constrained training modes not attainable within the small confines of most environmental chambers, high costs associated with international travel to conduct heat camps, and potential interference that HA may have with higher-prioritised training phase objectives. Alluring alternative HA strategies for athletes, such as post-exercise hot water immersion and sauna bathing, have been shown to elicit the desired physiological adaptations [10, 11], while overcoming the aforementioned barriers that traditional HA present. These HA alternatives and their reported effects are summarised in Table 1 and described briefly below.
2.1 Hot Water Immersion
Hot water immersion applied in untrained men as a form of passive HA has been shown to enhance thermoregulation [12–14] and improve exercise performance in the heat [11]. In one study, seven 45-min hot water baths (44 °C) completed over a 2-week period were shown to reduce thermal and cardiovascular strain, through reductions in core temperature (0.30 °C) and heart rate (12 beats/min (bpm)) [13]; an effect comparable to what is typically shown after conventional short-term HA [15]. Likewise, Zurawlew et al. [11] showed reductions in both resting (0.27 °C) and end-exercise (0.28 °C) core temperature, as well as a 4.9% improvement in 5-km run time trial (TT) performance in hot conditions (33 °C) following six consecutive post-exercise hot water baths (40 min running at 65% maximal oxygen consumption (\({\dot{\text{VO}}}_{{{\text{2max}}}}\)) in 18 °C; 40 min bath in 40 °C water). This performance improvement seems meaningful given that the coefficient of variation (CV) for a 5-km TT performance is 2% [16]. Given many training facilities have hot baths available to athletes for hydrotherapy purposes, hot water immersion holds potential as an accessible and time-efficient means of inducing HA. Further research with trained individuals is needed to understand the effects of hot water immersion compared with best practice HA methods.
2.2 Post-Exercise Sauna
The high thermal load (80–100 °C, 10–20% RH) imposed by sauna bathing presents its use as a potentially practical HA approach. Sauna bathing in a rested state has been shown to impose considerable heat stress, resulting in increased core and skin temperature, sweat rate and heart rate [17]. Consecutive days of sauna bathing in healthy untrained men has been shown to increase heat tolerance after only 3-day exposures, as evidenced by reductions in core temperature [18]. Sauna exposure immediately following a training session may enhance the thermoregulatory-adaptive response, as core temperature, considered a key contributor to HA-induced adaptations [19], has been shown to rise to a greater extent compared with sauna bathing without exercise [20]. Furthermore, post-exercise heat stress may additively enhance endurance training-induced mitochondrial function through increased citrate synthase enzyme activity [21]. To date, only two studies have reported on the use of post-exercise sauna bathing in trained athletes; however, neither study examined the typical spectrum of HA-induced adaptations [10, 22]. Both studies used ~10–15 post-exercise sauna sessions and reported significant plasma volume expansion (7–17%) [10, 22]. Only one study showed a possible improvement in running performance, equivalent to a ~2% improvement in 5-km TT performance in temperate conditions [10], and equal to the performance test CV [16]. Similar to hot water immersion, post-exercise sauna bathing may be more accessible than heat chambers for some athletes, and can be conveniently added to a training schedule with minimal disruption. While post-exercise sauna bathing is currently recommended by specialists as an HA alternative [9], no studies have reported its efficacy to induce thermoregulatory adaptations and enhance performance in hot conditions.
3 Integration with Training
3.1 Prescription and Periodization
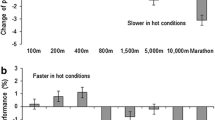
The majority of HA-induced adaptations (reduced body temperature, cardiovascular strain, perceived effort and discomfort) are actualised following short-term HA (4–7 days) [23], with further thermoregulatory (increased sweat rate) [24] and exercise capacity enhancement [25] requiring moderate-term HA (8–14 days) or even long-term HA (≥15 days). Long-term HA, though often overlooked as an HA strategy for athletes, may have merit for athletes preparing to perform ultra-endurance events in the heat, as longer-term HA has been shown to enhance molecular and cellular adaptations leading to improved cardiac contractile efficiency during exercise in the heat, and a greater accumulation of heat shock proteins, albeit in untrained animal models [26]. Direct comparisons of differing HA intervention length on performance outcomes would aid the development of HA dose recommendations based on competition length, thus providing an evidence-based menu that practitioners could refer to. For instance, long-term HA may be more optimal for endurance events over 2 h, where larger heat performance decrements are often evident (~3%) compared with middle-distance events (1%) [25], in which short- to moderate-term HA may be sufficient.
The appeal and ease of implementing short-term HA within an athlete’s training schedule has driven research to determine the minimal dose of HA required to elicit thermal adaptations and enhance performance in the heat. Rapid HA with just 2 days of twice-daily HA was recently shown to improve 3-km TT running performance (3.5%) in hot conditions (30 °C, 60% RH) in moderately-trained males [27]. Five sessions of short-duration (27 min) high-intensity intermittent HA, over a 9-day normal training period, in Australian Rules Football players reduced RPE, thermal discomfort and blood lactate during a submaximal heat stress test in hot conditions (~38 °C, 30% RH) [28]. Core temperature, sweat rate and heart rate were unaffected by these low-volume short-term HA protocols, supporting the notion that HA strategies should include a minimal duration at which an athlete’s core temperature is elevated [29]. However, caution is warranted when attempting ‘rapid’ short-term HA strategies, as the protective effects (reduced core temperature and heart rate; increased sweat rate) that longer-term HA elicit appear to be lacking, and therefore these strategies may not sufficiently eliminate heat-induced performance impairments nor reduce an athlete’s risk of EHI [4, 25].
The periodisation of HA poses complex questions around how best to schedule HA into an athlete’s training and competition calendar, where multiple events held in hot environments are likely throughout a competitive season. While more evidence is needed around its application in highly-trained populations, current literature has shown that adaptations following HA appear to decay after 2–4 weeks depending on HA length [30], while re-acclimation may occur with fewer sessions [31, 32]. As highly-trained individuals may have slower rates of HA decay [33], and because periodic exposure to heat following HA can allow for the retention of HA over several weeks [34], it may be worth periodising HA intermittently throughout a competitive season. Furthermore, a ‘thermal memory’ or ‘thermal plasticity’ concept may exist, where rapid re-acclimation is possible in those who have used HA routinely [19]. These concepts were recently applied in a case study where HA decay was perhaps lessened following 2 weeks of HA in an elite sailor [35]. Indeed, 2 days of consecutive re-acclimation provided further thermoregulatory enhancement [35], and is supported by similar findings in occupational settings [31, 32]. Figure 1 offers an example of how HA might be implemented in the build-up phase for athletes departing for a competition in hot conditions. Introducing HA 2–3 weeks prior to travel, combined with re-acclimation sessions before departure, poses an attractive strategy to ‘top up’ heat tolerance adaptations following a period of HA decay, and may alleviate training disruptions caused by repeating subsequent HA periods. More work is needed to understand how to optimise the periodisation of HA within an athlete’s annual training plan.
Overview of the periodised heat acclimation (HA) protocol used for two elite Laser sailors preparing for the world championships in Oman. A 4-week mesocycle included three heavy-build weeks and one recovery week (TSS = training stress score). HA [35 °C, 65% relative humidity (RH)] occurred during the first week with a heat response test (HRT) on day 1 and day 5 of HA. HRTs were repeated during the two following weeks of decay, and 3 days post re-acclimation (RA). Reproduced from Casadio et al. [35], with permission
3.2 Concurrent Training Considerations
The training programme structure of an elite athlete is often complex and multifaceted, with multiple layers of stress applied at various times, altogether aiming to develop the physical and mental resiliency needed for peak performance. When heat stress is added to training, coaches and sport scientists must consider the impact that HA will have on the athlete’s overall state of stress. For example, heat stress on top of normal training stress is likely to impact upon an athlete’s overall sympathovagal balance [36–39] and resulting hypothalamic-pituitary-adrenal axis response [40]. While recommendations have been made to adjust overall training intensity, volume and recovery practices during periods of HA [25], detail is lacking on exactly how practitioners should do so. Horowitz [19] explains that heat stress is a potent stimulus affecting every cell of the body, translating to heat-induced augmentations in sympathetic nervous system activity [41], cardiac strain [42] and rate of fuel utilisation [43, 44], thus resulting in an increased energy cost for a given exercise intensity [45]. Such added stress has been shown to not only amplify internal training load [46], but could potentially impair an athlete’s ability to recover for subsequent training sessions [47]. This scenario provokes questions as to how concurrent training should be structured around HA, which sessions heat should be added to, and how subsequent routine training sessions should be adjusted based on prior heat stress.
It seems logical to use sport-specific exercise modes for HA sessions that provide opportunities for athletes to simulate competition in hot conditions to fine tune pacing and cooling strategies prior to competition [48]. However, a number of authors speculate that low- to moderate-intensity sessions may be performed best in the heat during HA periods, and that so-called ‘key’ training sessions of higher-intensity might be performed in cool conditions, to avoid reduced training quality that could potentially lead to a diminished high-intensity stimulus and associated peripheral adaptations over an extended HA period [25, 48]. Conversely, key sessions may warrant their place in the heat chamber in sports where there is an anaerobic or power component. For example, a recent comparison of low- [90 min at 40% maximal aerobic power output (P max)] versus high-intensity (5 × 3 min at 70% P max, 3 min at 30% P max) HA resulted in performance enhancement that was somewhat specific to the type of HA undertaken [49]. Specifically, low-intensity HA resulted in improved 20-km TT endurance performance (5.9%), while high-intensity HA showed improvements in anaerobic performance (early sprint peak power output, vertical jump, counter-movement jump), without performance changes in the 20-km TT [49]. As with normal variations in training intensity, perhaps a combination of high- and low-to-moderate-intensity training in the heat would elicit a wider range of performance benefits in the heat for sports with multiple performance determinants. In addition, introducing high-intensity HA sessions may be best placed following 2–3 days of HA once initial adaptations to the heat have occurred, thus supporting the maintenance of intensity in hot conditions.
Athletes undergoing HA could be training up to 2–3 times per day, yet an understanding of how previous and subsequent routine training sessions surrounding HA may affect an athlete’s response is largely unexplored and possibly overlooked by practitioners. Exercise-induced muscle damage, through high-volume eccentric training, has been shown to increase core temperature (0.2–0.3 °C) during a subsequent exercise bout and may be explained by an augmented inflammatory response [50, 51]. However, this eccentric training-induced increase in heat strain is diminished with repeated bouts of eccentric training (repeated bout effect) [52]. Practically speaking, if eccentric training is introduced during a period of HA, heat strain may be elevated during the initial days. Interestingly, heat strain itself imparts a prophylactic effect against muscle damage [53], so it might be used as a tool in endurance athletes, i.e. heat applied in the period before introduction to eccentric resistance training to reduce muscle soreness. In addition, low-intensity short-term HA (5 days; 90 min of cycling at 40% of power) has been shown to reduce mean and peak torque during a maximal voluntary contraction [49]. This finding supports the concept that endurance-based HA might impair training quality and adaptive responses during routine concurrent resistance training. In contrast, some have shown that applying heat to skeletal muscle, with or without resistance training, can augment maximal force and muscle cross-sectional area over a 10-week period in untrained men [54, 55]. Mechanistic studies have shown that heat stimulates the Akt/mammalian target of rapamycin (mTOR) signalling pathway, a key regulator of protein synthesis and hypertrophy [56, 57]. Thus heat, applied in various ways, could provide an ergogenic effect when combined with resistance training. In summary, practitioners should consider the effects of HA on concurrent resistance training sessions. Introducing eccentric training during a period of HA should be avoided when the maintenance of a specific heat strain level during HA is required. Long-duration endurance sessions in the heat may impair the quality of concurrent resistance training. Finally, heat may be used as a training tool to incur protection against muscle damage or to augment muscle strength and hypertrophy adaptations.
4 Athlete Considerations
As no two athletes are the same, the high variation in individual responses to training [58–60] and environmental stress [3, 61] is unsurprising. Understanding how each athlete responds to added heat stress and acclimation through repeat heat response testing is therefore key and should be conducted well before any critical event in hot conditions [3, 62]. Heat response tests can be sport-specific, be comprised of a steady-state effort, and/or include a performance measure. The protocol should complement normal training so it can be easily repeated, possibly multiple times a season, to assess an athlete’s level of acclimation. Simple measures, such as heart rate, sweat rate, thermal perception and rating of perceived exertion can be easily employed without specialised equipment, while core temperature and plasma volume (or at least their change) can add further valuable information if available. High inter-individual variability in responses to heat response testing can be expected, even within similar athlete cohorts, which may be explained by several factors, summarised in Table 2. These include sex differences [24, 63, 64], differences in ethnicity [6, 65–68], athlete type [69], training status [33, 70–72], anthropometric characteristics [73–77], previous HA [31–33, 35], history of EHI [78, 79], and sleep quality and duration [78]. For female athletes, thermoregulatory changes due to menstrual cycle phase [80–83] and oral contraceptive use [84–86] could cause false-negative or -positive responses to heat response testing following HA, and should be noted prior to any thermoregulatory assessment. In addition, practitioners working with female athletes should consider that HA induction may require moderate-term HA [81, 87], as short-term HA may be less effective in females [88] compared with males [24]. Paralympic athletes require special considerations when training and competing in the heat, especially those with spinal cord injuries whose sudomotor cooling capacity is limited [89–91]. Finally, there is merit in discerning the immune status of an athlete prior to HA commencement. Individuals presenting with a fever or upper respiratory tract infection are predisposed to EHI [92, 93] and should not perform HA sessions for risk of further harm to themselves and their fellow athletes. Although HA does not appear to alter the immune response in healthy individuals [25, 94], athletes with suspected immune suppression may avoid further inflammatory exacerbation by avoiding HA sessions.
5 Perspectives
The purpose of this current opinion piece was to address practical considerations for integrating HA within an athlete’s programme and stimulate new research. When considering an HA approach several factors need to be reviewed in order to determine the appropriate heat load (temperature and humidity), mode, intensity, duration, frequency and periodization of adding heat to the existing training plan (Fig. 2). Often the priorities of training and the confines of an athlete or team’s schedule and location outweigh the ability to implement best-practice HA. Advancing research offers potential solutions to overcome common barriers to HA. Alternatives to conventional HA through post-exercise hot water immersion and sauna bathing add little disruption to normal training and may be used to induce HA adaptations if sport-specific training cannot be performed in a hot environment. While some form of heat exposure prior to competition in the heat would be better than none at all, caution is nevertheless warranted when using alternative forms of HA, and thermoregulatory markers should be monitored to measure heat adaptation progress. Before the length and intensity of HA are chosen, practitioners should consider the event duration and demands, and be aware that short-term HA may not induce the thermoregulatory and performance enhancement that longer-term HA provides. Implementing a re-acclimation strategy prior to an event in hot conditions may offer flexibility for athletes and their schedules when other key elements of training are more crucial. When adjusting routine training, the added stress imposed by HA should be considered, and the volume and intensity of other routine training in normal conditions may need to be reduced based on physiological and subjective athlete feedback during a heat camp. Finally, understanding individual athlete responses to heat stress and HA will assist practitioners to tailor protocols to their individual needs.
6 Conclusion
Heat strain associated with exercise in hot conditions has a negative impact on exercise performance. HA improves thermoregulation and cardiovascular stability, and attenuates heat-induced performance impairments. While the present HA guidelines provide a sound starting point for practitioners working with athletes, new research aimed at reducing the limitations and barriers of translating evidence-based guidelines to the real world of elite sport is needed. Alternative HA methods may be beneficial and easier to apply with athletes. An understanding of how HA may affect established training load would assist practitioners towards optimising the implementation of HA within the complex intricacies of an athlete’s training programme. Finally, the unique individual athlete response to HA should be considered when attempting to achieve optimal performance outcomes in hot condition events.
References
Sunderland C, Nevill ME. High-intensity intermittent running and field hockey skill performance in the heat. J Sports Sci. 2005;23(5):531–40.
Tatterson AJ, Hahn AG, Martini DT, et al. Effects of heat stress on physiological responses and exercise performance in elite cyclists. J Sci Med Sport. 2000;3(2):186–93.
Racinais S, Mohr M, Buchheit M, et al. Individual responses to short-term heat acclimatisation as predictors of football performance in a hot, dry environment. Br J Sports Med. 2012;46(11):810–5.
Binkley HM, Beckett J, Casa DJ, et al. National athletic trainers’ association position statement: exertional heat illnesses. J Athl Train. 2002;37(3):329.
Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25(S1):20–38.
Taylor NAS. Human heat adaptation. Compr Physiol. 2014;4:325–65.
Tyler CJ, Reeve T, Hodges GJ, et al. The effects of heat adaptation on physiology, perception and exercise performance in the heat: a meta-analysis. Sports Med. 2016;46(11):1699–724.
Chalmers S, Esterman A, Eston R, et al. Short-term heat acclimation training improves physical performance: a systematic review, and exploration of physiological adaptations and application for team sports. Sports Med. 2014;44(7):971–88.
Racinais S, Alonso JM, Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Scand J Med Sci Sports. 2015;25(S1):6–19.
Scoon GSM, Hopkins WG, Mayhew S, et al. Effect of post-exercise sauna bathing on the endurance performance of competitive male runners. J Sci Med Sport. 2007;10(4):259–62.
Zurawlew MJ, Walsh NP, Fortes MB, et al. Post-exercise hot water immersion induces heat acclimation and improves endurance exercise performance in the heat. Scand J Med Sci Sports. 2015;26:745–54.
Bonner RM, Harrison MH, Hall CJ, et al. Effect of heat acclimatization on intravascular responses to acute heat stress in man. J Appl Physiol. 1976;41(5):708–13.
Brazaitis M, Skurvydas A. Heat acclimation does not reduce the impact of hyperthermia on central fatigue. Eur J Appl Physiol. 2010;109(4):771–8.
Shin YO, Lee JB, Min YK, et al. Heat acclimation affects circulating levels of prostaglandin E 2, COX-2 and orexin in humans. Neurosci Lett. 2013;542:17–20.
Garrett AT, Creasy R, Rehrer NJ, et al. Effectiveness of short-term heat acclimation for highly trained athletes. Eur J Appl Physiol. 2012;112(5):1827–37.
Laursen PB, Francis GT, Abbiss CR, et al. Reliability of time-to-exhaustion versus time-trial running tests in runners. Med Sci Sports Exerc. 2007;39(8):1374–9.
Hannuksela ML, Ellahham S. Benefits and risks of sauna bathing. Am J Med. 2001;110(2):118–26.
Leppäluoto J, Tuominen M, Väänänen A, et al. Some cardiovascular and metabolic effects of repeated sauna bathing. Acta Physiol Scand. 1986;128(1):77–81.
Horowitz M. Heat acclimation: phenotypic plasticity and cues to the underlying molecular mechanisms. J Therm Biol. 2001;26(4):357–63.
Ridge BR, Pyke FS. Physiological responses to combinations of exercise and sauna. Aust J Sci Med Sport. 1986;18:25–8.
Tamura Y, Matsunaga Y, Masuda H, et al. Postexercise whole body heat stress additively enhances endurance training-induced mitochondrial adaptations in mouse skeletal muscle. Am J Physiol Reg Integr Comp Physiol. 2014;307(7):R931–43.
Stanley J, Halliday A, D’Auria S, et al. Effect of sauna-based heat acclimation on plasma volume and heart rate variability. Eur J Appl Physiol. 2015;115(4):785–94.
Garrett AT, Rehrer NJ, Patterson MJ. Induction and decay of short-term heat acclimation in moderately and highly trained athletes. Sports Med. 2011;41(9):757–71.
Mee JA, Gibson OR, Doust J, et al. A comparison of males and females’ temporal patterning to short- and long-term heat acclimation. Scand J Med Sci Sports. 2015;25(S1):250–8.
Guy JH, Deakin GB, Edwards AM, et al. Adaptation to hot environmental conditions: an exploration of the performance basis, procedures and future directions to optimise opportunities for elite athletes. Sports Med. 2015;45(3):303–11.
Horowitz M. From molecular and cellular to integrative heat defense during exposure to chronic heat. Comp Biochem Physiol A Mol Integr Physiol. 2002;131(3):475–83.
Willmott AGB, Gibson OR, Hayes M, et al. The effects of single versus twice daily short term heat acclimation on heat strain and 3000 m running performance in hot, humid conditions. J Therm Biol. 2016;56:59–67.
Kelly M, Gastin PB, Dwyer DB, et al. Short duration heat acclimation in Australian football players. J Sports Sci Med. 2016;15(1):118–25.
Houmard JA, Costill DL, Davis JA, et al. The influence of exercise intensity on heat acclimation in trained subjects. Med Sci Sports Exerc. 1990;22(5):615–20.
Garrett AT, Goosens NG, Rehrer NG, et al. Induction and decay of short-term heat acclimation. Eur J Appl Physiol. 2009;107(6):659–70.
Weller AS, Linnane DM, Jonkman AG, et al. Quantification of the decay and re-induction of heat acclimation in dry-heat following 12 and 26 days without exposure to heat stress. Eur J Appl Physiol. 2007;102(1):57–66.
Wyndham CH, Jacobs GE. Loss of acclimatization after six days of work in cool conditions on the surface of a mine. J Appl Physiol. 1957;11(2):197–8.
Pandolf KB, Burse RL, Goldman RF. Role of physical fitness in heat acclimatisation, decay and reinduction. Ergonomics. 1977;20(4):399–408.
Moseley PL. Heat shock proteins and heat adaptation of the whole organism. J Appl Physiol. 1997;83(5):1413–7.
Casadio JR, Kilding AE, Siegel R, et al. Periodizing heat acclimation in elite Laser sailors preparing for a world championship event in hot conditions. Temperature. 2016;3(3):437–43.
Yamamoto S, Iwamoto M, Inoue M, et al. Evaluation of the effect of heat exposure on the autonomic nervous system by heart rate variability and urinary catecholamines. J Occup Health. 2007;49(3):199–204.
Sollers JJ III, Sanford TA, Nabors-Oberg R, et al. Examining changes in HRV in response to varying ambient temperature. IEEE Eng Med Biol Mag. 2002;21(4):30–4.
Dranitsin OV. The effect on heart rate variability of acclimatization to a humid, hot environment after a transition across five time zones in elite junior rowers. Eur J Sport Sci. 2008;8(5):251–8.
Epstein Y, Moran DS, Heled Y, et al. Acclimation to heat interpreted from the analysis of heart-rate variability by the multipole method. J Basic Clin Physiol Pharmacol. 2010;21(4):315–24.
Brenner IKM, Zamecnik J, Shek PN, et al. The impact of heat exposure and repeated exercise on circulating stress hormones. Eur J Appl Physiol Occup Physiol. 1997;76(5):445–54.
Arngrímsson SÁ, Stewart DJ, Borrani F, et al. Relation of heart rate to percent VO2 peak during submaximal exercise in the heat. J Appl Physiol. 2003;94(3):1162–8.
Périard JD, Cramer MN, Chapman PG, et al. Cardiovascular strain impairs prolonged self-paced exercise in the heat. Exp Physiol. 2011;96(2):134–44.
Edwards RHT, Harris RC, Hultman E, et al. Effect of temperature on muscle energy metabolism and endurance during successive isometric contractions, sustained to fatigue, of the quadriceps muscle in man. J Physiol. 1972;220(2):335–52.
King DS, Costill DL, Fink WJ, et al. Muscle metabolism during exercise in the heat in unacclimatized and acclimatized humans. J Appl Physiol. 1985;59(5):1350–4.
Wingo JE, Lafrenz AJ, Ganio MS, et al. Cardiovascular drift is related to reduced maximal oxygen uptake during heat stress. Med Sci Sports Exerc. 2005;37(2):248–55.
Crowcroft S, Duffield R, McCleave E, et al. Monitoring training to assess changes in fitness and fatigue: the effects of training in heat and hypoxia. Scand J Med Sci Sports. 2015;25(S1):287–95.
Minett GM, Gale R, Wingfield G, et al. Sleep quantity and quality during heat-based training and the effects of cold-water immersion recovery. Extrem Physiol Med. 2015;4(1):1.
Taylor NAS, Cotter JD. Heat adaptation: guidelines for the optimisation of human performance. Int Sport Med J. 2006;7(1):33–57.
Wingfield GL, Gale R, Minett GM, et al. The effect of high versus low intensity heat acclimation on performance and neuromuscular responses. J Therm Biol. 2016;58:50–9.
Montain SJ, Latzka WA, Sawka MN. Impact of muscle injury and accompanying inflammatory response on thermoregulation during exercise in the heat. J Appl Physiol. 2000;89(3):1123–30.
Fortes MB, Di Felice U, Dolci A, et al. Muscle-damaging exercise increases heat strain during subsequent exercise heat stress. Med Sci Sports Exerc. 2013;45(10):1915–24.
Dolci A, Fortes MB, Walker FS, et al. Repeated muscle damage blunts the increase in heat strain during subsequent exercise heat stress. Eur J Appl Physiol. 2015;115(7):1577–88.
Nosaka K, Muthalib M, Lavender A, et al. Attenuation of muscle damage by preconditioning with muscle hyperthermia 1-day prior to eccentric exercise. Eur J Appl Physiol. 2007;99(2):183–92.
Goto K, Oda H, Kondo H, et al. Responses of muscle mass, strength and gene transcripts to long-term heat stress in healthy human subjects. Eur J Appl Physiol. 2011;111(1):17–27.
Goto K, Oda H, Morioka S, et al. Skeletal muscle hypertrophy induced by low-intensity exercise with heat-stress in healthy human subjects. Jpn J Aerosp Env Med. 2007;44(1):13–8.
Kakigi R, Naito H, Ogura Y, et al. Heat stress enhances mTOR signaling after resistance exercise in human skeletal muscle. J Physiol Sci. 2011;61(2):131–40.
Yoshihara T, Naito H, Kakigi R, et al. Heat stress activates the Akt/mTOR signalling pathway in rat skeletal muscle. Acta Physiol. 2013;207(2):416–26.
Borresen J, Lambert MI. The quantification of training load, the training response and the effect on performance. Sports Med. 2009;39(9):779–95.
Kraemer WJ, Duncan ND, Volek JS. Resistance training and elite athletes: adaptations and program considerations. J Orthop Sports Phys Ther. 1998;28(2):110–9.
Plews DJ, Laursen PB, Stanley J, et al. Training adaptation and heart rate variability in elite endurance athletes: opening the door to effective monitoring. Sports Med. 2013;43(9):773–81.
Chapman RF, Stray-Gundersen J, Levine BD. Individual variation in response to altitude training. J Appl Physiol. 1998;85(4):1448–56.
Bergeron MF, Bahr R, Bärtsch P, et al. International olympic committee consensus statement on thermoregulatory and altitude challenges for high-level athletes. Br J Sports Med. 2012;46(11):770–9.
Gagnon D, Kenny GP. Sex modulates whole-body sudomotor thermosensitivity during exercise. J Physiol. 2011;589(24):6205–17.
Gagnon D, Kenny GP. Sex differences in thermoeffector responses during exercise at fixed requirements for heat loss. J Appl Physiol. 2012;113(5):746–57.
Ulmasov KA, Shammakov S, Karaev K, et al. Heat shock proteins and thermoresistance in lizards. Proc Natl Acad Sci USA. 1992;89(5):1666–70.
Ladell WS. Terrestrial animals in humid heat: man. In: Dill DB, Adolph EF, Wilber CG, editors. Adaptations to the environment. Handbook of physiology. American Physiological Society. Washington, D. C; 1964.
Lyashko VN, Vikulova VK, Chernicov VG, et al. Comparison of the heat shock response in ethnically and ecologically different human populations. Proc Natl Acad Sci USA. 1994;91(26):12492–5.
Horowitz M. Heat acclimation, epigenetics, and cytoprotection memory. Compr Physiol. 2014;4:199–230.
Amano T, Koga S, Inoue Y, et al. Characteristics of sweating responses and peripheral sweat gland function during passive heating in sprinters. Eur J Appl Physiol. 2013;113(8):2067–75.
Cheung SS, McLellan TM. Heat acclimation, aerobic fitness, and hydration effects on tolerance during uncompensable heat stress. J Appl Physiol. 1998;84(5):1731–9.
Piwonka RW, Robinson S, Gay VL, et al. Preacclimatization of men to heat by training. J Appl Physiol. 1965;20(3):379–83.
Banfi G, Malavazos A, Iorio E, et al. Plasma oxidative stress biomarkers, nitric oxide and heat shock protein 70 in trained elite soccer players. Eur J Appl Physiol. 2006;96(5):483–6.
Havenith G. Human surface to mass ratio and body core temperature in exercise heat stress—a concept revisited. J Therm Biol. 2001;26(4):387–93.
Havenith G, Luttikholt VGM, Vrijkotte TGM. The relative influence of body characteristics on humid heat stress response. Eur J Appl Physiol Occup Physiol. 1995;70(3):270–9.
Selkirk GA, McLellan TM. Influence of aerobic fitness and body fatness on tolerance to uncompensable heat stress. J Appl Physiol. 2001;91(5):2055–63.
Hayward JS, Eckerson JD, Dawson BT. Effect of mesomorphy on hyperthermia during exercise in a warm, humid environment. Am J Phys Anthropol. 1986;70(1):11–7.
Chung NK, Pin CH. Obesity and the occurrence of heat disorders. Mil Med. 1996;161(12):739–42.
Armstrong LE, De Luca JP, Hubbard RW. Time course of recovery and heat acclimation ability of prior heatstroke patients. Med Sci Sports Exerc. 1990;22:36–48.
Johnson EC, Kolkhorst FW, Richburg A, et al. Specific exercise heat stress protocol for a triathlete’s return from exertional heat stroke. Curr Sports Med Rep. 2013;12(2):106–9.
Inoue Y, Tanaka Y, Omori K, et al. Sex-and menstrual cycle-related differences in sweating and cutaneous blood flow in response to passive heat exposure. Eur J Appl Physiol. 2005;94(3):323–32.
Avellini BA, Kamon E, Krajewski JT. Physiological responses of physically fit men and women to acclimation to humid heat. J Appl Physiol. 1980;49:254–61.
Carpenter AJ, Nunneley SA. Endogenous hormones subtly alter women’s response to heat stress. J Appl Physiol. 1988;65(5):2313–7.
Kolka MA, Stephenson LA. Control of sweating during the human menstrual cycle. Eur J Appl Physiol Occup Physiol. 1989;58(8):890–5.
Stachenfeld NS, Silva C, Keefe DL. Estrogen modifies the temperature effects of progesterone. J Appl Physiol. 2000;88(5):1643–9.
Tenaglia SA, McLellan TM, Klentrou PP. Influence of menstrual cycle and oral contraceptives on tolerance to uncompensable heat stress. Eur J Appl Physiol Occup Physiol. 1999;80(2):76–83.
Armstrong LE, Maresh CM, Keith NR, et al. Heat acclimation and physical training adaptations of young women using different contraceptive hormones. Am J Physiol Endocrinol Metab. 2005;288(5):E868–75.
Frye AJ, Kamon E, Webb M. Responses of menstrual women, amenorrheal women, and men to exercise in a hot, dry environment. Eur J Appl Physiol Occup Physiol. 1982;48(2):279–88.
Sunderland C, Morris JG, Nevill ME. A heat acclimation protocol for team sports. Br J Sports Med. 2008;42(5):327–33.
Castle PC, Kularatne BP, Brewer J, et al. Partial heat acclimation of athletes with spinal cord lesion. Eur J Appl Physiol. 2013;113(1):109–15.
Sawka MN, Latzka WA, Pandolf KB. Temperature regulation during upper body exercise: able bodied and spinal cord injured: US Army Research Institute of Environmental Medicine. Med Sci Sports Exerc. 1989;21(5 Suppl):S132–40.
Price MJ, Campbell IG. Thermoregulatory responses during prolonged upper body exercise in cool and warm conditions. J Sports Sci. 2002;20(7):519–44.
Sithinamsuwan P, Piyavechviratana K, Kitthaweesin T, et al. Exertional heatstroke: early recognition and outcome with aggressive combined cooling. A 12-year experience. Mil Med. 2009;174(5):496–502.
Cooper KE. Some responses of the cardiovascular system to heat and fever. The Can J Cardiol. 1994;10(4):444–8.
Yamada PM, Amorim FT, Moseley PL, et al. Effect of heat acclimation on heat shock protein 72 and interleukin-10 in humans. J Appl Physiol. 2007;103(4):1196–204.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
Julia Casadio, Andrew Kilding, James Cotter and Paul Laursen declare that they have no conflicts of interest relevant to the content of this review.
Rights and permissions
About this article
Cite this article
Casadio, J.R., Kilding, A.E., Cotter, J.D. et al. From Lab to Real World: Heat Acclimation Considerations for Elite Athletes. Sports Med 47, 1467–1476 (2017). https://doi.org/10.1007/s40279-016-0668-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-016-0668-9