Abstract
This study investigated the hypothesis that muscle damage would be attenuated in muscles subjected to passive hyperthermia 1 day prior to exercise. Fifteen male students performed 24 maximal eccentric actions of the elbow flexors with one arm; the opposite arm performed the same exercise 2–4 weeks later. The elbow flexors of one arm received a microwave diathermy treatment that increased muscle temperature to over 40°C, 16–20 h prior to the exercise. The contralateral arm acted as an untreated control. Maximal voluntary isometric contraction strength (MVC), range of motion (ROM), upper arm circumference, muscle soreness, plasma creatine kinase activity and myoglobin concentration were measured 1 day prior to exercise, immediately before and after exercise, and daily for 4 days following exercise. Changes in the criterion measures were compared between conditions (treatment vs. control) using a two-way repeated measures ANOVA with a significance level of P < 0.05. All measures changed significantly following exercise, but the treatment arm showed a significantly faster recovery of MVC, a smaller change in ROM, and less muscle soreness compared with the control arm. However, the protective effect conferred by the diathermy treatment was significantly less effective compared with that seen in the second bout performed 4–6 weeks after the initial bout by a subgroup of the subjects (n = 11) using the control arm. These results suggest that passive hyperthermia treatment 1 day prior to eccentric exercise-induced muscle damage has a prophylactic effect, but the effect is not as strong as the repeated bout effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unaccustomed eccentric exercise induces muscle damage; the typical symptoms of which include delayed onset muscle soreness (DOMS), prolonged decreases in muscle function, and swelling (Clarkson et al. 1992; Proske and Morgan 2001). These symptoms are attenuated however when the same eccentric exercise is performed several weeks beforehand (Clarkson et al. 1992; Nosaka et al. 2005). This protective effect conferred by a single bout of eccentric exercise has often been referred to as the repeated bout effect (Clarkson et al. 1992). The mechanisms underlying the repeated bout effect are not clearly understood, but several theories have been documented. In his review, McHugh (2003) categorized the potential adaptations caused by the repeated bout effect into neural (increased recruitment of slow motor units, activation of larger motor unit pool), mechanical (increased dynamic and passive muscle stiffness), cellular (longitudinal addition of sarcomeres, adaptation in inflammatory response, adaptation to maintain excitation–contraction coupling), and others (heat shock proteins, removal of weak sarcomeres or muscle fibers), and concluded that several mechanisms might work both independently and collectively.
One potential mechanism McHugh (2003) suggested as having a possible role in protecting against eccentric exercise-induced muscle damage was that of the heat shock proteins (HSPs). HSPs are a family of stress proteins that play an important role in situations involving both systemic and cellular stress (Kregel 2002). Eccentric exercise induces HSPs such as HSP27 and HSP70 in exercised human muscles (Thompson et al. 2001, 2002, 2003). Koh (2002) stated in his review that HSPs (18–30 kDa) might be involved in protection of skeletal muscle fibers from eccentric exercise-induced muscle damage. It has been known that expression of HSPs in skeletal muscle increases when the muscle temperature is increased over 40°C (Oishi et al. 2002; Selsby and Dodd 2005). It is possible to assume then that increasing muscle temperature to greater than 40°C could attenuate the muscle damage that is commonly induced by eccentric exercise. Among the various methods of increasing local muscle temperature in humans, shortwave or microwave electromagnetic diathermy and ultrasound appear to be effective, and an electromagnetic diathermy (short wave, microwave) increases muscle temperature by 3–4°C at depths of 30–50 mm (Draper et al. 1999).
Some studies have examined the effect of increasing muscle temperature immediately before exercise on the eccentric exercise-induced muscle damage response (Nosaka et al. 2004; Symons et al. 2004). Nosaka et al. (2004) reported that a microwave diathermy treatment to increase muscle temperature by approximately 3°C conducted within 15 min prior to eccentric exercise did not affect changes in indirect markers of muscle damage in comparison to the control condition in which no treatment was given before exercise. Symons et al. (2004) also showed no significant attenuation of the muscle damage response following an ultrasound treatment that increased muscle temperature by approximately 2°C immediately prior to eccentric exercise. However, no study yet has investigated the effect of an increased muscle temperature beyond 40°C. Oishi et al. (2002) showed that HSP72 increased in rat soleus (0–4 h) or plantaris (24–60 h) muscles following a prolonged (60 min) exposure to heat stress (muscle temperature maintained at 42°C). Selsby and Dodd (2005) recently reported that an elevation of HSP expression peaked between 24 and 48 h following a heat treatment where the core temperature of rats was maintained at around 41°C for 30 min by wrapping their body in a thermal blanket. No data is available for HSP expression following a heat treatment of local muscle in humans, but we assumed from the animal study data that HSP expression would increase for at least 24 h after a microwave diathermy treatment to increase muscle temperature beyond 40°C. We hypothesized that such a treatment performed within 24 h prior to eccentric exercise would attenuate the muscle damage.
This study compared changes in indirect markers of muscle damage of the elbow flexors seen in a control arm with those observed in a treatment arm that received a local diathermy heat treatment that increased muscle temperature to over 40°C, 16–20 h prior to the eccentric exercise. To compare the effect that the treatment had with that of the repeated bout effect, the control arm performed the second eccentric exercise bout, and changes in the markers of muscle damage were compared between the treatment arm and the second bout of the control arm.
Methods
Study design
This study used an arm-to-arm comparison model, in which one arm was used for a treatment condition, while the same subject’s contralateral arm acted as a control. Each arm performed a bout of maximal eccentric exercise of the elbow flexors separated by 2–4 weeks, but only the treatment arm received the microwave diathermy treatment 1 day prior to the exercise. The elapsed time between the diathermy treatment and exercise varied among subjects, but all subjects performed the exercise 16–20 h after the treatment. The control arm did not receive a placebo treatment as we felt that any potential placebo effect on changes in the criterion measures explained below would be minor at best. No information about a potential prophylactic effect induced by the treatment was given to any of the subjects. Dominant and non-dominant arms were randomly chosen for the treatment and control conditions, and the order of the conditions was counter-balanced among subjects (n = 15).
The experimental period consisted of two 6-day blocks. Indirect markers of muscle damage were measured before and within 5 min after the treatment for the treatment arm, and before, within 5 min after, and 1, 2, 3 and 4 days after exercise for both treatment and control arms. The markers included maximal voluntary isometric contraction strength (MVC), relaxed and flexed elbow joint angles, range of motion (ROM), upper arm circumference, muscle soreness, and plasma creatine kinase (CK) activity and myoglobin (Mb) concentration. These measures are commonly used to assess muscle damage in previous studies (Clarkson et al. 1992; Nosaka et al. 2004).
A subgroup of the subjects (n = 11) performed an additional bout of eccentric exercise of the elbow flexors with the arm used for the control condition 4–6 weeks following the first exercise bout to compare the effects that the treatment had on changes in the criterion measures with the repeated bout effects. The 4–6 week period was set because a previous study (Nosaka et al. 2005) has shown strong repeated bout effects on changes in these markers of muscle damage following eccentric exercise of the elbow flexors performed 4 or 8 weeks after the first bout, without a significant difference between 4 and 8 weeks. The reason for the reduced number of subjects was due to the fact that 4 out of the 15 subjects were unable to perform the second bout because of a conflict of schedule.
Subjects
Fifteen male students who had not performed resistance-training at least 1 year prior to this study and had not performed the eccentric exercise of the elbow flexors were recruited for this study following approval from the Institutional Human Research Ethics Committee. Subjects gave written informed consent conforming to the statement of protection for human subjects in the Declaration of Helsinki. The subject’s mean ± SD (range) age, height, and body mass were 23.1 ± 1.0 (19–31) year, 172.9 ± 6.8 (159–182) cm, and 63.4 ± 7.9 (52–82) kg, respectively. Subjects were instructed not to perform any exercise other than that performed in the study during the investigation period. All subjects were free from musculoskeletal disorders of the upper extremities, and refrained from medications and dietary supplements for at least 7 days prior to, and 4 days subsequent to, the eccentric exercise. During the experimental period, the subjects were restricted to any other types of interventions such as icing, heating, and massage.
The physical characteristics of the subgroup subjects (n = 11) who performed an additional eccentric exercise with their control arm were not significantly different from those of the initial 15 subjects.
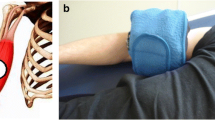
Treatment
One arm received a microwave diathermy treatment to the upper arm 16–20 h (18.9 ± 0.4 h) prior to the eccentric exercise bout using a Microrader (model KTM-250, Ito Microwave Co. Ltd., Osaka, Japan). The probe of the Microrader (15 cm in diameter) was placed approximately 15 cm from the surface of the upper arm to be exercised, directing the center of the probe toward the mid-portion of the bicep brachii, and the microwave (150 W) was applied for 20 min to increase the muscle temperature. During the heating period, the subject sat in a chair with the treatment arm relaxed and stretched on an arm curl bench placed in front of the body. Pilot data using six men of similar physical characteristics to those in the present study measured changes in muscle temperature of the biceps brachii using a needle thermometer (model N550, Nissho-YSI Co. Ltd., Tokyo, Japan) before, immediately after, and 10 min after the treatment, and showed that the muscle temperature (approximately 2 cm below the skin) increased from 34.2 (33.8–34.7) °C to 41.4 (40.2–42.0) °C immediately after, and fell to 38.0 (37.4–39.0) °C at 10 min following the treatment (unpublished data). The target muscle temperature (>40°C) was set on the assumption that HSPs would be induced by the heat treatment based on animal studies (Oishi et al. 2002; Selsby and Dodd 2005).
Eccentric exercise
All subjects performed 24 maximal eccentric actions of the elbow flexors of each arm separated by 2–4 weeks on a modified arm curl machine specially adapted to extend the elbow joint manually from a flexed to an extended position; force generation at the wrist was recorded for all eccentric actions (Nosaka et al. 2001). The interval between the two exercise bouts was set on an assumption that it would need 2 weeks for elevated CK and Mb to return to baseline. Since the contralateral arm was used for the second bout, it did not matter when the second bout was to be performed, but considering the plan to examine the repeated bout effect of the control arm, the maximal interval was set at 4 weeks. No warm-up exercise was performed before the eccentric exercise. During the exercise, one arm was positioned in front of the body on a padded support that secured the shoulder angle at 0.79 rad (45°) flexion, and the forearm was kept supinated with the wrist placed against the lever arm. The subject’s elbow joint was forcibly extended after 1 s of maximal isometric contraction from a flexed 1.57 rad (90°) to an extended 3.14 rad (180°) position in 3 s. Subjects were verbally encouraged to generate maximal isometric force at the starting position and to maximally resist against the elbow extending action throughout the full range of motion. This was repeated every 15 s for 24 times. This exercise protocol has been used in previous studies (Nosaka et al. 2001, 2004), and has been shown to induce similar muscle damage to the right and left elbow flexors (unpublished data). The force during eccentric exercise was measured by a load transducer (9E01-L43, NEC San-ei, Japan) installed in a specially designed wrist attachment and was monitored and recorded by a digital indicator (F360A, UNIPULSE, Japan) and a computer (Macintosh Performer 5410, USA). The peak force of each eccentric action was recorded, and the total force–time integral during the exercise was calculated as the sum of the 24 integrated forces for 4 s (1 s isometric +3 s eccentric) using a software program.
Criterion measures
Maximal voluntary isometric contraction strength
Maximal voluntary isometric contraction strength (MVC) was measured using a transducer (model 100, Takei Scientific Instruments, Niigata, Japan) connected to an Apple computer (Macintosh Performer 5410, Apple Computer, Cupertino, USA) via a Power Lab system and its associated software program (PowerLab /8SP, ADInstruments, Castle Hill, Australia). Subjects were seated on a specially designed bench with their arm positioned in front of their body with both their shoulder and elbow joint angles at 90° (1.57 rad) flexion. A wristband worn by the subject was attached to the transducer via a metal cable. Subjects were familiarized with the measurements by practicing several submaximal and maximal contractions prior to the test, and asked to perform 2 maximal isometric contractions for 3 s each with 30 s rest in between the efforts. The reliability of this protocol has been established in the previous study (Nosaka et al. 2004). The mean of these two peak values was used for further analysis.
Elbow joint angles and range of motion (ROM)
Relaxed, and voluntary extended and flexed elbow joint angles were measured using a plastic goniometer, and ROM was defined as the difference between the extended and flexed angles. Relaxed elbow joint angle (RANG) was defined as the elbow joint angle obtained when subjects allowed their arm to hang in a relaxed manner by their side. For the extended elbow joint angle (EANG), the angle was measured after subjects extended their elbow joint as much as possible. For the flexed elbow joint angle (FANG), the angle was determined after subjects flexed their elbow as much as possible, attempting to touch their shoulder with the palm of their hand while keeping their elbow joint at their side. In this study, the elbow joint angles made by the upper arm and the forearm were measured, in which a fully extended elbow angle was close to 180°, and a fully flexed elbow angle was around 30°. All measurements were in duplicate and an average of the two measurements was reported. To ensure that measurements were taken from the same point each time, a semi-permanent ink pen was used to mark a point over the apex of the deltoid, the axis of rotation of the elbow, the styloid process and dorsal tubercle of the radius.
Upper arm circumference
Upper arm circumference was assessed at 3, 5, 7, 9 and 11 cm proximal to the elbow joint using a tape measure with the arm hanging relaxed by the side. Two measurements were taken from each site and averaged. Since each site showed a similar change, the mean of five measurements was used for further analysis. Marks were made using a semi-permanent ink marker to clearly show these assessment points and were visible throughout the experimental period.
Muscle soreness
Muscle soreness was evaluated using a visual analogue scale. This scale possessed a 50-mm line that had the words “no pain” on one end and “extremely sore” on the other. Subjects were asked to indicate their pain level on that line while their elbow flexors were: (1) being palpated (three sites on the upper arm: mid-belly of the biceps brachii, 3-cm above and below the mid-belly), (2) being extended, and (3) being flexed by the investigator. For the palpation measure, the highest score of the three sites was used for further analysis.
Blood markers
Approximately 5-ml of blood was drawn into a tube containing lithium heparin from an antecubital vein at each measurement time point except immediately after exercise. Blood was centrifuged at 3,000 RPM for 10 min, and the separated plasma was removed and stored at −20°C. Plasma samples were analyzed for CK activity spectrophotometrically using an automatic blood analyzer (Model 7170; Hitachi, Tokyo, Japan) and standard test kit (Shikarikid CK; Kanto Chemical Co. Ltd, Tokyo, Japan) and for Mb concentration using a γ-counter (ARC-950; Aloka Co. Ltd., Tokyo, Japan) with a commercially available kit (Daichi Radioisotope, Tokyo, Japan). According to the information provided with these kits the normal reference range for men using these methods is 45–135 IU l−1 for CK and <60 ng ml−1 for Mb.
Statistical analysis
The baseline values for all criterion measures were compared between control and treatment arms by a Student’s t test. Changes in the criterion measures from pre to post-treatment were analyzed by a one-way analysis of variance (ANOVA). Changes in all criterion measures over time were compared between the treatment and control conditions using a two-way (treatment × time) repeated-measures ANOVA. For the subjects (n = 11) who performed two bouts of eccentric exercise with the control arm, changes in all criterion measures over time were compared between the first and second bouts, and between the treatment and the second bout of the control condition using a two-way repeated measures ANOVA. For muscle soreness, comparison between the three measures was made by a two-way ANOVA. Where the ANOVA revealed a significant main effect, a Student’s t test with Bonferroni adjustment was used to detect differences between conditions at each time point. Statistical significance was set at P < 0.05 for the ANOVA, and P < 0.008 for the post-hoc test. Data are presented as means ± SEM, unless otherwise stated.
Results
Acute effects of microwave treatment
Following the microwave diathermy treatment, the skin of the upper arm appeared reddish in color and warmer than pre-treatment; however, this did not cause significant changes in MVC (P = 0.89), elbow joint angles (P = 0.75–0.85), ROM (P = 0.81), and upper arm circumference (P = 0.69). There was no significant difference between these measures taken before the treatment and 1 day after the treatment (immediately before exercise) for all measures (P = 0.62–0.89).
Peak force output during exercise
Peak force significantly decreased over 24 eccentric actions (P < 0.01), and the magnitude of the decrease from the first action to the 24th action was approximately 50% (Fig. 1). However, no significant difference existed between conditions (P = 0.56). The total force–time integral during the exercise for the control and treatment condition was 17,524 ± 1,322 Ns, and 19,012 ± 1,417 Ns, respectively, without a significant difference between conditions (P = 0.47).
MVC
No significant (P = 0.79) difference in MVC was evident before exercise between the control (269.5 ± 8.8 N) and treatment (253.8 ± 8.8 N) conditions. Figure 2a shows the changes in MVC before and after exercise. MVC decreased significantly (P < 0.01) immediately after exercise without a significant difference between conditions. However, a significant difference between conditions was evident between 1 and 4 days after exercise showing significantly (P < 0.01) greater MVC for the treatment condition compared with the control condition. For example, MVC at 4 days post-exercise was significantly (P < 0.01) greater for the treatment (79.7 ± 4.4% of pre-exercise) compared with the control condition (61.2 ± 4.9% of pre-exercise).
Normalized changes in maximal isometric strength of the elbow flexors from baseline (pre:100%), immediately (post) and 1–4 days after exercise for the treatment (T) and control (C) conditions (a), and for the first and second bouts (b). *Significantly different between conditions or bouts (P < 0.05 for the interaction effect, P < 0.008 for the group effect)
Elbow joint angles and ROM
RANG was similar between the control (159.3 ± 1.2°) and treatment (158.1 ± 1.4°) conditions before exercise. RANG decreased significantly (P < 0.01) immediately after exercise for both conditions and a significant (P < 0.01) difference between conditions existed. The control condition showed further decreases in RANG and the nadir was seen 3 days after exercise (140.6 ± 3.4°); however, no further decrease in RANG was observed for the treatment condition. EANG was approximately 20° greater than RANG before exercise, but the difference between EANG and RANG decreased after exercise. For example, at 3 days after exercise, when RANG was smallest (140.6 ± 3.4°), EANG was 153.4 ± 3.8° for the control arm. FANG was not significantly (P = 0.55) different between the control (28.8 ± 1.3°) and treatment (32.5 ± 1.6°) conditions before exercise, increased significantly (P < 0.01) immediately post exercise for both conditions (control: 41.5 ± 1.3°, treatment: 43.9 ± 1.4°) and then gradually decreased. No significant (P = 0.11) difference in the change in FANG following exercise was evident between conditions. Figure 3a shows the changes in ROM over time. Pre-exercise ROM was not significantly (P = 0.75) different between the control (142.3 ± 1.4°) and treatment (138.3 ± 2.0°) conditions; however, compared to the control condition, the treatment condition resulted in significantly (P = 0.03) smaller decreases in ROM over time following exercise.
Absolute changes in range of motion from baseline (pre: 0), immediately (post) and 1–4 days after exercise for the treatment (T) and control (C) conditions (a), and for the first and second bouts (b). *Significantly different between conditions or bouts (P < 0.05 for the interaction effect, P < 0.008 for the group effect)
Upper arm circumference
Before exercise, upper arm circumference was not significantly different between the control (246.2 ± 5.2 mm) and treatment (248.3 ± 5.0 mm) conditions (P = 0.77). As shown in Fig. 4a, both conditions showed significant (P < 0.01) increases in upper arm circumference after exercise, but the amount of increase from the pre-exercise value at 4 days post-exercise was not significantly (P = 0.65) different between the control (13.3 ± 2.5 mm) and treatment (10.1 ± 2.3 mm) conditions.
Absolute changes in upper arm circumference from baseline (pre: 0), immediately (post) and 1–4 days after exercise for the treatment (T) and control (C) conditions (a), and for the first and second bouts (b). n.s. not significantly different between conditions, *significantly different between bouts (P < 0.05 for the interaction effect, P < 0.008 for the group effect)
Muscle soreness
Changes in muscle soreness are shown in Fig. 5. Muscle soreness increased significantly (P < 0.01) 1 day after exercise in a similar manner (P = 0.80) for both palpation and extension soreness, but the level of perceived soreness during flexion was significantly (P < 0.05) less when compared with palpation and extension. Compared to the control condition, muscle soreness with extension was significantly (P = 0.04) smaller for the treatment condition, but no significant (P = 0.13, P = 0.71) difference between conditions was seen for the palpation and flexion assessments.
Changes in muscle soreness upon palpation, extension, and flexion before (P) and 1–4 days after exercise for the treatment (T) and control (C) conditions (a, c, e), and for the first and second bouts (b, d, f). *Significantly different between conditions or bouts (P < 0.05 for the interaction effect, P < 0.01 for the group effect)
Plasma CK activity and Mb concentration
Before exercise, plasma CK activity and Mb concentration were within the normal range with no significant (P = 0.88) difference between conditions, but increased significantly (P < 0.01) from the baseline following exercise (Fig. 6). No significant (P = 0.76, 0.36) differences between conditions were evident for the changes in plasma CK activity and Mb concentration following exercise.
Comparison between the first and second bouts for the subgroup
No significant (P = 0.57–0.78) differences between the first and second bouts performed by the subgroup were evident for any of the pre-exercise criterion measures. Changes in peak force during eccentric exercise were not significantly (P = 0.65) different from those shown in Fig. 1, and no significant (P = 0.69) difference between bouts was found. Changes in the criterion measures (shown in Figs. 2, 3, 4, 5, 6) after the first exercise bout for the subgroup were not significantly different from those found in the control condition (P = 0.54–0.89). Comparison between the first and second bouts revealed that recovery of MVC was significantly (P < 0.01) faster after the second bout, and changes in other measures (ROM, upper arm circumference, muscle soreness, plasma CK activity and Mb concentration) were significantly (P < 0.01) smaller after the second bout compared with the first bout.
Comparison between the effects of treatment and repeated bout effect
When comparing the criterion measures between the treatment arm and the second bout of the control arm for the subgroup, no significant differences in any of the pre-exercise criterion measures were evident (P = 0.60–0.88). Compared with the changes in the treatment arm, the second bout resulted in a significantly (all P < 0.01) smaller increase in CIR, muscle soreness, and plasma CK activity and Mb concentration, but no significant difference was evident for MVC (P = 0.32) and ROM (P = 0.55).
Discussion
This study investigated whether changes in indirect markers of muscle damage were attenuated when the elbow flexors of one arm received a microwave diathermy treatment (increasing muscle temperature to over 40°C) 16–20 h prior to eccentric exercise compared with a contralateral control arm performing the same exercise without treatment. Compared to the control arm, the treatment arm showed a significantly faster recovery of MVC (Fig. 2), smaller changes in ROM (Fig. 3), and smaller development of muscle soreness with extension (Fig. 5). However, no significant differences between arms were evident for the change in upper arm circumference (Fig. 4), muscle soreness with palpation and flexion (Fig. 5), and plasma CK activity and Mb concentration (Fig. 6). Since no significant difference between arms was found for any of the pre-exercise measures, and the eccentric exercise was performed similarly for both conditions as shown by Fig. 1 and the similar force–time integral between the conditions, the significant attenuation of some indirect markers of muscle damage between conditions was likely to have been caused by the microwave diathermy treatment.
The microwave diathermy treatment used in the present study was expected to increase the temperature of the biceps brachii and brachialis muscles to over 40°C, although this was not directly verified in this study. Had invasive verification of muscle temperature using a needle thermometer been used in the present study, this would have likely induced damage to muscle fibers and connective tissue in the subjects. Instead, we performed a pilot study using six men of similar physical characteristics to those subjects of the present study. These data showed that the biceps brachii muscle temperature (approximately 2 cm below the skin) increased from 34.2 to 41.4°C immediately after the treatment, and remained elevated to 38.0°C at 10 min post-treatment (unpublished data). It is not known as to how long the muscle temperature would have remained elevated above 40°C during and following the 20 min treatment, but it seems unlikely that the elbow flexors were exposed to temperatures greater than 40°C for much more than 20 min. It is reasonable to assume that the treatment did not have any acute effects on the measures, since no significant changes in MVC, elbow joint angles, ROM, and upper arm circumference occurred immediately after the treatment. Based on the similar exercise performance between bouts (Fig. 1), the diathermy treatment did not appear to have any adverse effects on muscle function. We speculate that the elbow flexors were pre-conditioned by something occurring in the muscles themselves such as expressions of molecules (i.e. HSPs) involved in the protective effect in the time elapsed between the treatment and the exercise (16–20 h) causing the influence on MVC, ROM, and muscle soreness upon extension. It is also possible that the microwave diathermy treatment affected other body systems such as the central nervous system and the immune system, which might be associated with the attenuation responses.
The involvement of HSPs as a partial mechanism for the protective effect conferred by a bout of eccentric exercise has been suggested by Koh (2002) and McHugh (2003). McArdle et al. (2004a) showed that transgenic mice overexpressing HSP70 had significantly smaller decreases in force, faster recovery of force, and a higher percentage of intact muscle fibers after eccentric exercise of the EDL muscle compared with the wild type mice. Miyabara et al. (2005) demonstrated that necrosis and decreases in muscle fiber cross-sectional area after cryolesion were attenuated for transgenic mice overexpressing HSP70 and wild type mice treated with a HSP inducer compared to wild type mice. In contrast, McArdle et al. (2004b) wrapped anaesthetized mice in a heating blanket to raise their core temperature to 42°C for 15 min and examined release of CK following a damaging contraction protocol of the hindlimb muscles in vitro performed 4 and 12 h after the hyperthermia treatment. The authors did not find that the CK release was affected by the whole body hyperthermia treatment, and argued against a role for HSPs in the protection mechanism (McArdle et al. 2004b). The present study did not find a significant difference between the treatment and control conditions for changes in CK following exercise (Fig. 6), which is in line with the finding of McArdle et al. (2004b).
Since the present study did not measure HSPs, it is not possible to discuss further whether the protective effect found in the present study was associated with HSPs or not, and changes in HSPs after microwave diathermy treatment should be examined in future studies. However, even if the treatment did induce HSPs, it may be either that the amount or duration of elevated HSPs required to induce such a prophylactic effect is much smaller than that used in past studies, such as in the case of the transgenic mice (McArdle et al. 2004a). To induce HSPs by increasing body temperature, previous studies have exposed animals to a whole body heat stress for 30–60 min, and core temperature in these animals increased to higher than 41°C (Selsby and Dodd 2005). In contrast, the present study placed only the upper arm under the microwave diathermy treatment for 20 min, and it seems unlikely that whole body temperature would have increased to levels much greater than normal body temperature. It would be interesting therefore to repeat the present study design but with increased treatment exposure time and treatment type (i.e., use of a hot bath).
The present study is the first to demonstrate a prophylactic or pre-conditioning effect of heat treatment on eccentric exercise-induced muscle damage. It is important to note that the microwave diathermy muscle treatment, which seemed likely to increase muscle temperature beyond 40°C, was performed 16–20 h before the eccentric exercise bout. This temperature treatment is greater than that used in previous studies reporting no prophylactic effect following heat treatments (Nosaka et al. 2004; Symons et al. 2004); these studies used a muscle temperature treatment of approximately 38°C immediately prior to the bout of eccentric exercise. Moreover, Jayaraman et al. (2004) reported that a 2-h heating pad treatment (41°C) every day following eccentric exercise of the knee extensors (until muscle soreness completely subsided) did not affect recovery of muscle strength, muscle soreness, swelling, or changes in T2 relaxation time of magnetic resonance images. It would appear therefore, that the muscle temperature, the timing of the treatment and/or the type of treatment are essential to produce the protective effect. It would be interesting to examine whether or not a microwave diathermy treatment (>40°C) implemented immediately prior to eccentric exercise would induce a similar protective effect as that found in the present study.
When the second eccentric exercise bout was performed 4–6 weeks after the first bout, changes in all of the criterion measures were smaller compared with those measured after the first bout (Figs. 2, 3, 4, 5, 6), which is in line with the previous reports (Clarkson et al. 1992; McHugh 2003; Nosaka et al. 2005). This is different from the control versus treatment comparison, which showed a significant difference between conditions only for MVC, ROM, and muscle soreness upon extension. It would appear that the magnitude of the protection conferred by the microwave diathermy heat treatment against eccentric exercise-induced muscle damage is less effective than that by prior eccentric exercise. Among the three measures of muscle soreness, only the soreness upon extension measure showed a significant difference between conditions (Fig. 5). It may be that the reduced extension soreness was linked to the smaller decreases in ROM (Fig. 3). Because of an increase in the muscle stiffness following eccentric exercise, which limits extension of the elbow joint, it may be that subjects felt greater pain when the elbow joint was extended for the muscle soreness assessment under the control condition. It is difficult to explain how the microwave diathermy treatment enhanced the recovery of MVC and attenuated the changes in ROM from the data obtained from the present study. Further research is necessary to understand the mechanism(s) underlying the phenomenon.
In summary, the present study has shown that the treatment arm with microwave diathermy results in a faster recovery of muscle strength, smaller decreases in ROM, and less development of muscle soreness with extension compared with the untreated control arm. These findings suggest that the use of a hyperthermic microwave diathermy treatment has a prophylactic effect on reducing muscle damage. When attenuation of muscle damage induced by eccentric exercise is necessary, raising muscle temperature 1-day prior to the exercise may be effective. However, the magnitude of the protective effect induced by the hyperthermic microwave diathermy treatment does not appear to be as strong as the repeated bout effect. The underlying mechanisms of the protective effect conferred by the treatment are currently unknown, but we speculate that HSPs are partially involved in the mechanisms.
References
Clarkson PM, Nosaka K, Braun B (1992) Muscle function after exercise-induced muscle damage and rapid adaptation. Med Sci Sports Exerc 24:512–520
Draper DO, Knight K, Fujiwara T, Castel JC (1999) Temperature change in human muscle during and after pulsed short-wave diathermy. J Orthop Sports Phys Ther 29:13–22
Jayaraman RC, Reid RW, Foley JM, Prior BM, Dudley GA, Weingand KW, Meyer RA (2004) MRI evaluation of topical heat and static stretching as therapeutic modalities for the treatment of eccentric exercise-induced muscle damage. Eur J Appl Physiol 93:30–38
Koh TJ (2002) Do small heat shock proteins protect skeletal muscle from injury? Exer Sport Sci Rev 30:117–121
Kregel KC (2002) Heat shock proteins: modifying factors in physiological stress responses and acquired themotolerance. J Appl Physiol 92:2177–2186
McArdle A, Dillmann WH, Mestril R, Faulkner JA, Jackson MJ (2004a) Overexpression of HSP70 in mouse skeletal muscle protects against muscle damage and age-related muscle dysfunction. FASEB J 18:355–357
McArdle F, Spiers S, Aldemir H, Vasilaki A, Beaver A, Iwanejko L, McArdle A, Jackson MJ (2004b) Preconditioning of skeletal muscle against contraction-induced damage: the role of adaptations to oxidants in mice. J Physiol 561:233–244
McHugh MP (2003) Recent advances in the understanding of the repeated bout effect: the protective effect against muscle damage from a single bout of eccentric exercise. Scan J Med Sci Sports 13:88–97
Miyabara EH, Martin JL, Griffin TM, Moriscot AS, Mestril R (2005) Overexpression of inducible 70-kDa heat shock protein (HSP70) in mouse attenuates skeletal muscle damage induced by cryolesion. Am J Physiol Cell Physiol 290:C1128–C1138
Nosaka K, Sakamoto K, Newton M, Sacco P (2001) How long does the protective effect on eccentric exercise-induced muscle damage last? Med Sci Sports Exerc 33:1490–1495
Nosaka K, Sakamoto K, Newton M, Sacco P (2004) Influence of pre-exercise muscle temperature on responses to eccentric exercise. J Athletic Training 39:132–137
Nosaka K, Newton MJ, Sacco P (2005) Attenuation of protective effect against eccentric exercise-induced muscle damage. Can J Appl Physiol 30:529–542
Oishi Y, Taniguchi K, Matsumoto H, Ishihara A, Ohira Y, Roy RR (2002) Muscle type-specific responses of HSP60, HSP72, and HSC73 during recovery after elevation of muscle temperature. J Appl Physiol 92:1097–1103
Proske U, Morgan DL (2001) Muscle damage from eccentric exercise: mechanism, mechanical signs, adaptation and clinical applications. J Physiol 537:333–345
Selsby JT, Dodd SL (2005) Heat treatment reduces oxidative stress and protects muscle mass during immobilization. Am J Physiol Regul Integr Comp Physiol 289:R134–R139
Symons TB, Clasey JL, Gater DR, Yates JW (2004) Effects of deep heat as a preventative mechanism on delayed onset muscle soreness. J Strength Cond Res 18:155–161
Thompson HS, Scordilis SP, Clarkson PM, Lohrer WA (2001) A single bout of eccentric exercise increases HSP27 and HSC/HSP70 in human skeletal muscle. Acta Physiol Scand 171:187–193
Thompson HS, Clarkson PM. Scordilis SP (2002) The repeated bout effect and heat shock proteins: intramuscular HSP27 and HSP70 expression following two bouts of eccentric exercise in humans. Acta Physiol Scand 174:47–56
Thompson HS, Maynard EB, Morales ER, Scordilis SP (2003) Exercise-induced HSP27, HSP70 and MAPK responses in human skeletal muscle. Acta Physiol Scand 178:61–67
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nosaka, K., Muthalib, M., Lavender, A. et al. Attenuation of muscle damage by preconditioning with muscle hyperthermia 1-day prior to eccentric exercise. Eur J Appl Physiol 99, 183–192 (2007). https://doi.org/10.1007/s00421-006-0331-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-006-0331-5