Abstract
Background and Objective
Cardiovascular disease is the main cause of death in Germany and other industrialized countries. However, until now, little has been known about how people with acute coronary syndrome (ACS) value aspects of their medical treatment. The objective of this study was to evaluate patients’ preferences regarding different antiplatelet medication options following an ACS.
Method
After identification of patient-relevant treatment attributes (a literature review and qualitative interviews), a discrete-choice experiment (DCE) including five patient-relevant attributes was conducted. The DCE used a forced-choice approach in which no “opt out” was present, as no treatment is not an option after ACS. The attribute and level combinations were created using a fractional–factorial NGene design with priors. Data analysis was performed using a random-effects logit model. An additional generalized linear latent and mixed models (GLLAMM) analysis was performed to evaluate subgroup differences.
Results
ACS patients (N = 683) participated in computer-assisted personal interviews. Preference analysis showed a clear dominance of the attribute “mortality risk” (coefficient: 0.803). Ranked second was “side effect: dyspnea” (coefficient: 0.550) followed by “risk of a new myocardial infarction” (coefficient: 0.464) and “side effect: bleeding” (coefficient: 0.400). “Frequency of intake” was less important (coefficient: 0.025). Within the 3-class GLLAMM, the variables “marital status” (p = 0.008), “highest level of education” (p = 0.003), and “body-mass index” (according to World Health Organization cluster; p = 0.014) showed a significant impact on the estimated class probabilities.
Conclusion
Our study found “mortality risk” to be of the highest value for patients. Patient-centered care and decision making requires consideration of patient preferences; moreover, the information on preferences can be used to develop effective therapies after an ACS. The data generated will enable healthcare decision makers and stakeholders to understand patient preferences to promote patients’ benefit.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Discrete-choice experiments are a suitable and theoretically grounded method. |
Reduction of mortality risk was of the highest value to patients, followed by all side effects, and mode of administration, which was not significant. |
Information on preferences can be used to develop effective therapies for acute coronary syndrome. |
1 Introduction: Treatment After Acute Coronary Syndrome
Of the approximately 2 million emergency patients diagnosed with acute coronary syndrome (ACS) in Germany each year, approximately 15 % have suffered a myocardial infarction [1]. In 2011, approximately 218,253 people in Germany experienced a heart attack, of whom 217,681 had an acute myocardial infarction [2]. In the same year, a total of 55,286 people died from myocardial infarction [3]. Therefore, the term ACS summarizes the major forms of heart attack (acute myocardial infarction and sudden cardiac death) and unstable angina [4]. The primary goal of ACS treatment is the reduction of the extremely high mortality rate that characterizes this disease. This central objective can be achieved by improving preventive, diagnostic, and therapeutic interventions. In particular, medicinal therapy with anticoagulant drugs is an important starting point [5]. After successful acute treatment, patients are still faced with an increased risk of a myocardial infarction (re-infarction or post-infarction), stroke, or similar long-term risks, depending on the severity of their coronary heart disease [6, 7]. The risk can only be reduced by targeted (secondary) prevention, such as lifestyle changes, long-term medical treatment with β-blockers (β-adrenoceptor antagonists), ACE inhibitors, angiotensin receptor antagonists, and oral antiplatelet therapy [5, 6].
Within the different treatment options, allocative decisions for the optimal ACS treatment or therapy are usually examined from the perspective of experts. Expert judgments are focused on clinical effectiveness based on randomized clinical trials. Furthermore, the value of an alternative treatment depends on the subjective assessment of different decision criteria by the decision maker. The question of how ACS patients value different aspects of their treatment are not always evaluated or considered. However, a systematic review showed that the judgments of experts do not always correlate with the subjective needs or preferences of patients [8]. Treatment goals of the patient are, therefore, not necessarily congruent with defined endpoints of drug therapy established by medical experts [9]. Therefore, it is necessary to include both sources of evidence (clinical evidence as well as patient evidence) during the allocative decision-making process.
Through the analysis of patient preferences it is possible to analyze patient benefit alongside clinical effectiveness. Thereby, attributes of new treatments can be identified that can generate added value to patients. Thus, preference data can create a new source of information (evidence). In this way, the added value of innovative treatment options can be complemented by the patient-perceived benefit based on clinical trial data [9]. The identification and weighting of patient-relevant endpoints has recently gained attention in medical innovation, particularly in the pharmaceutical market [early benefit assessment by the Institute for Quality and Efficiency in Health Care (IQWiG)] [10, 11]. Moreover, regulatory decisions regarding approval and pricing require explicit or implicit trade-offs between potential efficacies, risks of side effects, costs, and, in certain circumstances, mode of administration. IQWiG proposes that discrete-choice experiments (DCEs) (alongside analytic hierarchy process [AHP]) should be used in medical research to display patient preferences [12]. Therefore, the DCE method is seen as appropriate to answer the present research question: what are the essential properties of an optimal platelet inhibitor ACS drug therapy (which decreases the platelet aggregation) from the patient perspective?
Although patient-relevant endpoints are one of the main topics on healthcare policy-makers’ agenda, very little patient preference data exist regarding the treatment of ACS. The identification and weighting of patient-relevant therapy attributes seems necessary from the patient perspective. The aim of the present empirical study was the estimation of patient preferences for long-term drug treatment after a coronary event. The information of additional patient benefit and how patients value different treatment characteristics should be available for all stakeholders. Therefore, the patient-relevant endpoints essential for successful treatment were identified, analyzed, and weighted using a DCE. In addition, a generalized linear latent and mixed models (GLLAMM) estimation was used to test for possible subgroup differences.
2 Methods
2.1 Discrete-Choice Experiments
The DCE method is a choice-based version of the conjoint analysis, which was made possible by the theoretical work of Lancaster [13] and McFadden [14]. Instead of ranking or rating different therapeutic features (as in traditional importance elicitation formats and conjoint analysis), DCE performs a pair-wise comparison of hypothetical alternatives (differently configured therapy options) and asks the participants to choose (decide) between them [15], thus forcing respondents to make trade-offs between attributes, based on the respective levels of the alternatives. This method offers practical advantages such as closeness to reality, as trade-off decisions are part of everybody’s everyday life. The implementation of pair-wise comparisons considerably reduces the degree of complexity of the tasks for the participants [16–18]. Therefore, DCEs are increasingly used in health economics and health services research [19]. The structure and design of a DCE and its evaluation have multiple steps; several checklists are available and were considered during the design of the study [9, 16, 18, 20].
2.2 Study Design
2.2.1 Decision Model: Attributes and Levels
At the beginning of the study, a systematic literature review on the indication of the ACS was conducted to document the available state-of-the-art of treatment options (PubMed, MEDLINE, and Cochrane Library). The aim of the search was to identify potential properties and characteristics of long-term ACS treatments using platelet inhibitors, in general and from the patient perspective. In total, 243 full texts were included and analyzed.
Prior to the main survey, a preliminary qualitative study phase was conducted. During qualitative, semi-structured interviews with ACS patients in a rehabilitation clinic (N = 10), five treatment characteristics extracted from the literature were tested to see if they are relevant to the patient during a potential treatment decision. As all participants named all five treatment characteristics to be important with a treatment decision, their relevance for the study could be confirmed. Furthermore, patients identified additional, previously unidentified, treatment attitudes that would be patient relevant. This allowed for reflection of the subjective views of the patients surveyed. Moreover, the interviews were used to evaluate the clarity of the questionnaire design, the quality of the scales used, and the understandability of the attributes, levels, and trade-offs included.
Finally, the preliminary study (AHP with 19 patients) was used to generate approximate values for the weights of each treatment attribute or level (with eigenvector estimation). All level characteristics mirrored realistic studies. This means that within the literature review all relevant and available randomized controlled trial (RCT) results were collected and all maxima and minima of the included attributes were allocated. The level ranges used within the DCE are centered on the means of the available RCT data. This approach enabled the use of the estimated preference weights for regulatory assessments because the levels are derived from clinical trial data. The attributes and levels were used for the creation of an optimal experimental design in the main study.
2.2.2 Data Collection Plan: Sample Size, Stratification, and Recruitment
The survey was conducted from December 2012 to February 2013 using computer-assisted personal interviews (CAPIs). The recruitment of patients for the main survey and interviews were performed by Kantar Health (Bielefeld). Patients who were diagnosed with ACS (self reported), hospitalized because of ACS within the last 2 years, and older than 18 years were included in the survey. Additionally, patients were asked to indicate whether they suffered from ST-segment elevation myocardial infarction (STEMI) or non-STEMI/unstable angina (NSTEMI/UA). The sample strategy used a ratio of 30 % STEMI and 70 % NSTEMI/UA patients, which corresponds to the actual distribution within the ACS population [21]. The minimum sample size according to the Orme calculation (two alternatives, 36 choice sets, three levels) was 29, which is seen as the lowest possible sample size for main effects estimation [22].
2.2.3 Ethical Considerations
The study is a social science survey and does not contain personal data (completely anonymous survey), surgeries (tests, experiments, and medication), biomedical research, or additional data, as in many epidemiological investigations. Therefore, a consideration by an ethics board in Germany was not mandatory. However, all respondents were informed about the study and its potential risks and benefits prior to participation and all respondents signed an informed consent form. Participation was voluntary and could be stopped at any time. The ethics committee reviewed the study principles, all informational material, and the survey instrument, and approved the study (IB: 2268600/12).
2.2.4 Data Collection: Instrument, Elicitation Technique, Tasks, and Experimental Design
The final decision model was established based on the qualitative pilot study. Five patient-relevant characteristics, described by three levels each, were extracted and included in the main survey instrument.
The DCE contained 13 choice sets of hypothetical treatment options. Patients were asked to indicate which of the two therapies shown they would choose in each case (trade-off relationships; Fig. 1). No opt-out possibility was given, as “no treatment” is not applicable with ACS. To simplify the choice tasks for the participants, each level of each attribute was displayed together with a visual aid.
2.3 Experimental Design
In favor of manageability and minimal participant burden, a minimum required number of trade-off decisions (choice sets) for the experimental design were chosen for the DCE.
The preliminary study approximations were used as priors for the development of the fractional factorial experimental design [5 × 3 multi-nomial logit (MNL) design] of the DCE, which was created using NGene software (ChoiceMetrics Pty Ltd). The selected D-efficient design (D-error: 0.08572) included 36 choices, which were divided into three blocks with 12 tasks each. To check the consistency of responses in each set, the first choice was repeated at the end. Thus, each participant had to answer 13 DCE choice tasks. Moreover, a dominant choice set was presented at the beginning. Failure of both consistency tests led to exclusion of the dataset.
During conduct of the survey, a randomization of attribute order was included within the instrument. Each participant saw a different order of attributes.
2.4 Data Analysis: Data Structure, Statistical Model, Subgroup Analysis, and Interpretation
The estimation of DCE parameters was performed using linear main effects models and GLLAMM using STATA® 10 (StataCorp LP, College Station, TX, USA). Effect coding was applied within all model estimations. The “best” level by content was coded positive. The effect coding coefficients show the difference to the grand mean. Therefore, it is likely that the middle category of a three-level attribute will be close to the grand mean and thus less likely to significantly differ from the grand mean. Furthermore, the level margins were presented using level difference method and an additional normalization was conducted (Fig. 2). For all analyses, statistical significance of p < 0.05 was applied.
The GLLAMMs were fitted using an MNL link function and binomial distribution for the binary response. At the beginning, a main effects model (1-class model), which assumes that the population of respondents is homogeneous in the weighting (expected utility), was calculated for each attribute. In addition, “multi-group models” (2-class, 3-class, and 4-class GLLAMMs) were calculated by specifying latent class models using a discrete random coefficients vector. Identification of groups made it possible to identify patterns related to these groups using structural variables. The group models thus provided information about the likelihood of possible patients falling into a specific group based on the respective structural variables. “Likelihood ratio tests”, Akaike Information Criterion (AIC), and Bayesian Information Criterion (BIC) were used to check the accuracy of the model, determine the most appropriate model, and test for parameters that might improve the model fit.
3 Results
3.1 Results of the Literature Review and Personal Interviews
After content analysis of the interviews, five final criteria were determined (three levels each) which were used for the quantitative DCE survey. A patient-friendly introduction with a short explanation about the content of each attribute and the segmentation of the related levels was given to the participants (Table 1). The description of the attribute levels was created in the style of the classification scheme of the US Department of Health and Human Services and the Office of Human Research Protection of the US FDA [23].
3.2 Results of the Main Survey
3.2.1 Respondents’ Characteristics
A total of 743 complete records were transferred to the database. After an internal consistency test and the exclusion of all invalid questionnaires, 683 patients were included in the final quantitative data analysis.
3.2.2 Sociodemographic Data
About half of the study participants (58.9 %) were male. The youngest patients were between 23 and 27 years old and the oldest patients were between 88 and 92 years. The largest age group of patients surveyed (47.6 %; N = 325) were between 53 and 67 years old. Nearly two-thirds of the patients were married (66 %). The highest proportion within educational levels was an intermediate high school certificate (27.1 % of respondents). In regard to employment status, 259 patients surveyed (37.9 %) were in retirement and 236 (34.6 %) were employed full-time at the time of the survey (Table 2).
3.3 Results of the Discrete-Choice Experiment
Overall, 8.879 choice-decisions from the DCE choice task could be included in the final estimations. Table 3 shows the results of the multivariate analysis for long-term ACS drug therapy.
It can be seen that four of the five enclosed attributes led to significant values. Only “frequency of intake” does not show significant values. From the coefficients obtained from the DCE, the treatment characteristics appear in the following chronological order: (1) “mortality risk” (coefficient: 0.803); (2) “side effect: dyspnea” (coefficient: 0.550); (3) “risk of a new myocardial infarction” (coefficient: 0.464); (4) “side effect: bleeding” (coefficient: 0.400); and (5) “frequency of intake” (coefficient: 0.025). The same order also resulted from the calculation of the level difference, which is shown in the last column of Table 3.
Figure 2 is used to better illustrate the coefficients in terms of the average importance of the endpoints (normalized to 10). All significant properties show an approximately linear behavior, which confirms the basic assumption of the calculation models. It can be seen that the middle level of each attribute is near zero on the x-axis, which is another assumption of the underlying calculation model and hereby confirmed.
3.4 Results of the Latent Class Model and Analysis of Subgroups
3.4.1 Preference Differences Depending on Structural Variables
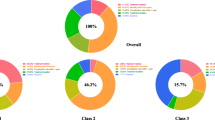
To identify possible subgroup differences starting from the initial main effects model, a 2-class model and, subsequently, a 3-class model were generated. Based on the examination of model fit using the AIC and BIC (both indicators for the assessment of overall quality of models), the 3-class model could be identified as suitable for the illustration of existing heterogeneity in response behavior as well as for the representation of the probable allocation of patients per group (Table 4).
Preference Patterns Class 1 The preference pattern of Class 1 (N = 199; 29.1 %) shows that the attributes “bleeding” and “risk of a new myocardial infarction” are weighted highest. The attribute “mortality risk” is ranked third. This suggests that respondents within this class are weighting this attribute less than participants within the other two classes. For the mode of administration attribute “frequency of intake”, no significant coefficient was calculated, which would indicate that this attribute again had no effect on the decision of this subpopulation.
Preference Patterns Class 2 The preference pattern of Class 2 (N = 279; 40.8 %) is very similar to the linear model for the estimation of the main effects (relative importance). In comparison to the main model, four of the five enclosed attributes led to significant values and “frequency of intake” still does not show a significant estimate. Characteristic of the second class, however, is that the side effect attributes “bleeding” and “dyspnea” have nearly identical coefficients, and the differences between the outcome attributes and the side effect attributes are higher than in either the first or third class or than in the main effects model. Furthermore, “mortality risk” presents an outstanding high coefficient, which allows the assumption that this attribute has a clear dominant position within the decision of this subpopulation.
Preference Patterns Class 3 It is striking in the evaluation of the preference pattern in Class 3 (N = 205; 30 %) that the weighting of the side effect “dyspnea” is much higher than either in the first or second class or than in the main effects model. Furthermore, for the first time “frequency of intake” shows a clear tendency towards being a significant coefficient (p = 0.04), which would indicate that this attribute has a more important role within this subpopulation.
3.4.2 Evaluation of Structural Variables for All Classes
Within the 3-class GLLAMM, the variables “marital status” (p = 0.008), “highest level of education” (p = 0.003), and “body-mass index” (BMI; according to World Health Organization cluster; p = 0.014) showed significant impact on the estimated class probabilities.
Class 1 is likely to have a higher proportion of the marital status “widowed” (17.7 %) than in Class 2 (10.0 %) or Class 3 (11.2 %). Furthermore, divorced people are more likely to be in Class 3 (13.2 %) than in Class 1 (6.0 %) or Class 2 (8.6 %). It seemed that the people who are involuntarily alone might give more importance to the side effects than to the outcome attribute as displayed in Classes 1 and 3.
With regard to the education level, people with “intermediate high school certificate, secondary school certificate” were more likely to be in Class 3 (30.7 %) than in Class 2 (22.9 %), whereas people with “completed technical college” are more likely to be in Class 2 (20.8 %) than in Class 3 (8.2 %) or Class 1 (9.0 %). With respect to the higher educated proportion within Class 2, it may be assumed that the importance of the outcome attribute “mortality risk” is more anticipated and, therefore, weighted higher than the side effect attributes, as displayed within the other two classes.
People in the higher BMI group [30–35 (obesity)] are more likely to be in Class 3 (15.1 %) than in Class 2 (10.0 %), whereas people in the lower BMI group [20–25 (normal weight)] are more likely to be in Class 2 (30.5 %) than in Class 3 (20.0 %). It might be reasonable to expect that overweight people already face problems with breathing and, therefore, put more importance on this attribute, which would explain the dominance of the attribute “dyspnea” in this group.
The sociodemographic characteristics “age” (divided into four groups; p = 0.088), “gender” (p = 0.294), “family structure/living situation” (p = 0.576), and “risk perception” (p = 0.300) did not influence the calculated latent class model. It is concluded that these characteristics have no influence on the different preference patterns in the present decision-making model.
4 Discussion: Interpretation of Preference Data
4.1 Interpretation of Discrete-Choice Experiment Results
The results show that four of the five included treatment attributes are relevant to patients in the decision-making process for a drug therapy after ACS. The non-significance of “frequency of intake” suggests that this attribute has no relevance within the decision-making process for patients. More simply, it does not matter to the patient whether he or she has to take the tablets once, twice, or three times a day, as long as the therapy reduces the risk of death. Therefore, the reduction of “mortality risks” is most important to patients when deciding on a long-term ACS treatment. Hence, clinical evaluation and the assessment of patient preference are in concordance.
As can be seen, the original hypotheses could be confirmed within the results. The “mortality risk” is the dominant attribute in prioritization of therapy alternatives. “Mode of administration” and “side effects” are dominated by the endpoint “mortality”.
It was surprising that “side effect: dyspnea” was in second place within the preference weighting of the main effects model and rated higher than possible “bleeding”. An explanation for this could be that patients are affected by shortness of breath in their daily lives which allows them to perform fewer activities by themselves, e.g., walking stairs causes problems. Therefore “dyspnea” might be associated with restriction of achievement potential and a possible reduction in quality of life. “Possible bleeding” is more likely connected to a necessary medical intervention. “Bleeding” might be seen as treatable and, thus, might be perceived as “less restrictive”, even if it can have life-threatening consequences. At the same time, many ACS patients have already experienced shortness of breath and the associated consequences. Bleeding as a side effect, which in severe cases can be life-threatening, is valued much higher within clinical trials and usually represents a primary safety endpoint [24].
The huge benefit expectations related to low “mortality risk” shows that a high degree of acceptance can be expected for a drug therapy that provides this benefit. The consideration of patient preferences in therapeutic decisions implies stronger patient focus and can be valuable in the development of new drug therapies for the treatment of ACS.
4.2 Limitations of the Study
DCEs could be used to estimate patient preferences successfully within the indication of ACS. Nevertheless, some limitations should be mentioned. As preferences can be influenced by various conditions, the information provided (properties and characteristics) and the experiences of patients within the indication, as well as cognitive skills, can play a role in this [30, 31]. Therefore, preferences may vary depending on the decision context. This has to be taken into consideration during the interpretation of the results. Furthermore, it should be mentioned that the level ranges of the attributes have an influence on respondents’ choices. The realistic level range of dyspnea from “no dyspnea” to “severe dyspnea” might have influenced the relative importance of this attribute because all other attributes had no “zero (none)” level. In addition, a new methodological discussion is the issue of potential rescaling effects within preference estimates. To be able to test this aspect, a validity test of sensitivity to scope should have been included. As this was not part of the empirical study, this issue needs to be addressed in further methodological research.
One further issue that might be raised is that only patients with a self-reported diagnosis were part of the inclusion criteria. To ensure valid recruitment, Kantar Health used specific recruitment strategies to guarantee the right participants, and CAPIs ensured the quality of the participants. Finally, it should be noted that the use of a market research company panel for recruitment may have influenced some individual parameters of the study population, and that there is always the possibility that patients may not have read the preliminary information appropriately.
5 Conclusion
The measurement of the priorities, expectations, and preferences of patients showed that reducing “mortality risk” is by far the most important criterion in ACS drug treatment. Thus, this endpoint holds decisive importance for ACS treatment and dominates relevance in patients’ decisions regarding a possible choice of therapy. In the context of this study, it could be demonstrated that use of the DCE is an appropriate method to identify and weight patient-relevant characteristics in terms of possible treatment alternatives. Moreover, DCE is characterized by a high degree of realism and an appropriate measure for the patient.
This empirical DCE study was able to evaluate the most important attributes of optimal drug therapy for the treatment of ACS from the ACS patient perspective. Subsequently, it revealed how patients evaluate the different potential aspects of drug therapy. DCEs therefore present a practical approach that can improve communication between patients, providers, and other stakeholders. In addition, the DCE method has the potential to support clinical decision making (e.g., within clinical practice or Health Technology Assessment decisions) and to improve the quality of patient care in the long term, and therapies can be designed based on patient-oriented findings.
References
Post F, Münzel T. Das akute Koronarsyndrom. Der Internist. 2010;51(8):953–62.
Statistisches Bundesamt: Diagnosedaten der Krankenhäuser ab 2000. Krankenhausstatistik—Diagnosedaten der Patienten und Patientinnen in Krankenhäusern. 2011. https://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/WS0100/_XWD_PROC?_XWD_6/2/XWD_CUBE.DRILL/_XWD_32/D.946/14358.
Statistisches Bundesamt: Todesursachen in Deutschland. In: Gesundheit. Wiesbaden: Statistisches Bundesamt; 2012.
Kelm M, Strauer BE. Das akute Koronarsyndrom. Der Internist. 2005;46(3):265–74.
Hamm CW, Arntz HR, Bode C, Giannitsis E, Katus H, Levenson B, Nordt T, Neumann FJ, Tebbe U, Zahn R. Pocket-Leitlinien: Akutes Koronarsyndrom (ACS). Deutschen Gesellschaft für Kardiologie – Herz- und Kreislaufforschung e.V., Düsseldorf (2004).
Löwel H, Meisinger C, Schneider A, Kaup U, Gösele U, Hymer H. Koronare Herzkrankheit und akuter Myokardinfarkt. In: Gesundheitsberichterstattung des Bundes, vol 33. Berlin: Robert Koch-Institut; 2006.
Johansson G, Stallberg B, Tornling G, Andersson S, Karlsson GS, Falt K, Berggren F. Asthma treatment preference study: a conjoint analysis of preferred drug treatments. Chest. 2004;125(3):916–23.
Mühlbacher AC, Juhnke C. Patient preferences versus physicians’ judgement: does it make a difference in healthcare decision making? Appl Health Econ Health Policy. 2013;11(3): 163–80.
Mühlbacher A, Bethge S, Tockhorn A. Präferenzmessung im Gesundheitswesen: Grundlagen von Discrete-Choice-Experimenten [measuring preferences in healthcare: introduction to discrete-choice experiments]. Gesundheitsökon Qualitätsmanag. 2013;4:159–72.
Glaeske G. The dilemma between efficacy as defined by regulatory bodies and effectiveness in clinical practice. Deutsches Ärzteblatt Int. 2012;109(7):115.
Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG). Prasugrel bei akutem Koronarsyndrom, Dokumentation und Würdigung der Anhörung zum Berichtsplan. Köln: IQWiG; 2010.
Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG). Allgemeine Methoden, Entwurf für Version 4.2 vom 18.06.2014. Köln: IQWiG; 2014.
Lancaster KJ. A new approach to consumer theory. J Polit Econ. 1966;74(2):132–57.
McFadden D. Conditional logit analysis of qualitative choice behavior. Zarembka. 1974;1974:105–42.
Ben-Akiva ME, Lerman SR. Discrete choice analysis: theory and application to travel demand. MIT Press series in transportation studies. Cambridge: MIT Press; 1985.
Hensher DA, Rose JM, Greene WH. Applied choice analysis: a primer. Cambridge: Cambridge University Press; 2005.
Johnson FR. Why not ask?: Measuring patient preferences for healthcare decision making. Patient. 2008;1(4):245–8.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–78.
Ryan M, Gerard K, Amaya-Amaya M. Using discrete choice experiments to value health and health care. The economics of non-market goods and resources, vol. 11. Dordrecht: Springer; 2008.
Bridges JFP, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis use in health studies—a checklist: a report of the ISPOR conjoint analysis in health good research practices task force. ISPOR TF Report. 2011;14:403–13.
Höer A, Behrendt S. Versorgung und Kosten von Versicherten mit akutem Koronarsyndrom (ACS) in Deutschland (berichtigte Fassung). Berlin: IGES Institut GmbH; 2012.
Orme BK. Sample size issues for conjoint analysis. In: Getting started with conjoint analysis: strategies for product design and pricing research. 2nd ed. Madison: Research Publishers LLC; 2010. pp. 57–66.
US Department of Health and Human Services, Office of Human Research Protection. Guidance on reviewing and reporting unanticipated problems involving risks to subjects or others and adverse events. 2007. http://www.hhs.gov/ohrp/policy/advevntguid.html. Accessed 1 Dec 2013.
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57.
Behan MW, Chew DP, Aylward PE. The role of antiplatelet therapy in the secondary prevention of coronary artery disease. Curr Opin Cardiol. 2010;25(4):321–8. doi:10.1097/HCO.0b013e328338f7b5.
Storey RF, Becker RC, Cannon CP, Cools F, Emanuelsson H, Harrington RA, et al. Ticagrelor does not affect pulmonary function tests compared to clopidogrel in acute coronary syndromes: results of the PLATO pulmonary substudy. J Am Coll Cardiol. 2010;55(10 Suppl 1):A108.E1007.
Storey RF, Becker RC, Harrington RA, Husted S, James SK, Cools F, et al. Characterization of dyspnoea in PLATO study patients treated with ticagrelor or clopidogrel and its association with clinical outcomes. Eur Heart J. 2011;32(23):2945–53.
Storey RF, Becker RC, Harrington RA, Husted S, James SK, Cools F, et al. Pulmonary function in patients with acute coronary syndrome treated with ticagrelor or clopidogrel (from the platelet inhibition and patient outcomes [PLATO] pulmonary function substudy). Am J Cardiol. 2011;108(11):1542–6.
Storey RF, Bliden KP, Patil SB, Karunakaran A, Ecob R, Butler K, et al. Incidence of dyspnea and assessment of cardiac and pulmonary function in patients with stable coronary artery disease receiving ticagrelor, clopidogrel, or placebo in the ONSET/OFFSET study. J Am Coll Cardiol. 2010;56(3):185–93.
Helm R, Steiner M. Präferenzmessung: Methodengestützte Entwicklung zielgruppenspezifischer Produktinnovationen. Stuttgart: W. Kohlhammer; 2008.
Louviere JJ, Islam T, Wasi N, Street D, Burgess L. Designing discrete choice experiments: do optimal designs come at a price? J Consum Res. 2008;35(2):360–75.
Acknowledgments
The authors would like to thank E. Piletzki and Dr. H. Brauer (Rehaklinik Silbermühle, Plau am See, Germany) for their help organizing the pre-test interviews and all of the participants taking part in the study.
Author’s declaration
AM developed, designed and coordinated the study, contributed to data analysis, data interpretation and revised the paper. SB carried out the questionnaire studies, contributed to data analysis, study design and drafted the paper.
Conflict of interest
This study was funded by AstraZeneca GmbH, Germany. AM and SB declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mühlbacher, A.C., Bethge, S. Reduce Mortality Risk Above All Else: A Discrete-Choice Experiment in Acute Coronary Syndrome Patients. PharmacoEconomics 33, 71–81 (2015). https://doi.org/10.1007/s40273-014-0223-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-014-0223-1