Abstract
A single-tablet regimen of ledipasvir and sofosbuvir (ledipasvir/sofosbuvir; Harvoni®) was recently approved in the EU. The phase 3 ION trials included treatment-naïve (ION-1 and -3) or treatment-experienced (ION-2) patients with chronic hepatitis C virus (HCV) genotype 1 infection; ≈20 % of patients in ION-1 and -2 had cirrhosis, whereas none of the patients in ION-3 had cirrhosis. In ION-1, a 12-week regimen of ledipasvir/sofosbuvir achieved high rates of sustained virological response 12 weeks’ post-treatment (SVR12) in treatment-naïve patients, with no additional benefit conferred by the addition of ribavirin or extending the treatment duration to 24 weeks. An 8-week regimen also achieved high SVR12 rates in patients with a baseline HCV RNA level of <6 million IU/mL in ION-3. High SVR12 rates were seen in treatment-experienced patients who received ledipasvir/sofosbuvir for 12 or 24 weeks in ION-2. Data also support the use of ledipasvir/sofosbuvir in chronic HCV genotype 4 infection, in HCV and HIV co-infection and, in combination with ribavirin, in patients with chronic HCV genotype 1 or 4 infection who have decompensated cirrhosis or are liver transplant recipients and in chronic HCV genotype 3 infection. Oral ledipasvir/sofosbuvir was generally well tolerated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adis evaluation of ledipasvir/sofosbuvir in chronic hepatitis C
Single-tablet regimen administered once daily, with potential for improved treatment adherence |
Achieves high sustained virological response rates 12 weeks’ post-treatment in treatment-naïve and -experienced patients with chronic HCV genotype 1 infection |
Data support its use in chronic HCV genotype 4 infection and in HCV and HIV co-infection |
Data support its use, in combination with ribavirin, in chronic HCV genotype 1 or 4 infection with decompensated cirrhosis or liver transplantation, or in chronic HCV genotype 3 infection |
Generally well tolerated |
Cost may represent a barrier to treatment |
What is the rationale for developing ledipasvir/sofosbuvir?
Combination therapy with peginterferon-α and ribavirin was the mainstay of treatment in chronic hepatitis C for a number of years [1]. However, peginterferon-α is often poorly tolerated and a large proportion of patients are not eligible or willing to receive it [2]. Recently, the treatment of chronic hepatitis C has been transformed by direct-acting antiviral agents, with interferon-free regimens now a reality. Interferon-free treatment with the direct-acting antiviral agents ledipasvir and sofosbuvir is now available in the EU as a single-tablet regimen (ledipasvir/sofosbuvir; Harvoni®) [3].
How do ledipasvir and sofosbuvir work?
Ledipasvir inhibits the hepatitis C virus (HCV) NS5A protein and sofosbuvir inhibits HCV NS5B RNA-dependent RNA polymerase; both NS5A and NS5B RNA-dependent RNA polymerase are essential for viral replication [3]. Ledipasvir has potent antiviral activity against HCV genotypes 1a and 1b, with lower activity against HCV genotypes 4a, 4d, 5a and 6a, and substantially lower activity against HCV genotypes 2a, 2b, 3a and 6e [3]. Sofosbuvir has pangenotypic antiviral activity [4].
In cell culture, reduced ledipasvir susceptibility was associated with certain NS5A amino acid substitutions (e.g. Y93H in HCV genotypes 1a and 1b and Q30E in HCV genotype 1a) [3]. Among patients with chronic HCV genotype 1 infection who received ledipasvir/sofosbuvir in the pivotal 3 ION trials [5–7], some of the patients who qualified for resistance testing had at least one NS5A resistance-associated variant as determined by deep sequencing [3].
In cell culture, reduced sofosbuvir susceptibility was associated with the primary NS5B substitution S282T in multiple HCV genotypes [3]. However, sofosbuvir has a high genetic barrier to resistance; the NS5B S282T variant was not detected during the ION trials [5–7] in patients with chronic HCV genotype 1 infection who received ledipasvir/sofosbuvir [3]. No cross resistance was seen between ledipasvir and sofosbuvir [3].
For whom is ledipasvir/sofosbuvir indicated?
Ledipasvir/sofosbuvir is indicated in the EU for the treatment of adults with chronic hepatitis C [3]. A summary of the EU prescribing information for ledipasvir/sofosbuvir is shown in Table 1.
What is the clinical efficacy of ledipasvir/sofosbuvir?
A ledipasvir/sofosbuvir dosage of 90/400 mg once daily was administered to patients in the trials discussed in this section. A number of trials included treatment arms in which patients also received ribavirin. Some of the trials/analyses discussed in this section are only available as abstracts, posters and/or slide presentations [9–19].
In chronic HCV genotype 1 infection
The pivotal, phase 3 ION-1 [5], ION-2 [6] and ION-3 [7] trials examined the efficacy of ledipasvir/sofosbuvir in patients aged ≥18 years with chronic HCV genotype 1 infection. These randomized, open-label, multicentre trials included patients who were treatment-naïve (ION-1 [5] and ION-3 [7]) or had experienced virological failure after treatment with peginterferon-α plus ribavirin with or without a NS3/4A protease inhibitor (ION-2 [6]). Approximately 20 % of patients in ION-1 [5] and ION-2 [6] could have compensated cirrhosis, whereas ION-3 enrolled patients without cirrhosis [7]. The primary endpoint was the rate of sustained virological response (SVR) 12 weeks’ post-treatment (SVR12) [5–7]; SVR12 has been shown to be an appropriate measure of durable response to ledipasvir/sofosbuvir [9].
SVR12 rates were ≥97 % in treatment-naïve patients in ION-1, regardless of whether ledipasvir/sofosbuvir was administered for 12 or 24 weeks or administered with or without ribavirin (Table 2) [5].
In ION-3, an SVR12 rate of 94 % was achieved in treatment-naïve patients without cirrhosis who received ledipasvir/sofosbuvir for 8 weeks (Table 2) [7]. The 8-week regimen of ledipasvir/sofosbuvir was noninferior to the 12-week regimen of ledipasvir/sofosbuvir or to the 8-week regimen of ledipasvir/sofosbuvir plus ribavirin in terms of SVR12 (Table 2) [7]. Moreover, post hoc analysis of ION-3 demonstrated that an 8-week regimen of ledipasvir/sofosbuvir appeared sufficient in treatment-naïve patients without cirrhosis who had a baseline HCV RNA level of <6 million IU/mL, with an SVR12 rate of 97 % (Table 2) and a relapse rate of 2 % [10].
High SVR12 rates were seen across various patient subgroups in ION-1 and ION-3, including in patients with traditional predictors of poor response [5, 7]. For example, across the four treatment groups in ION-1, SVR12 rates were 94–100 % in patients with cirrhosis, 97–99 % in patients with chronic HCV genotype 1a infection, 97–99 % in those with non-CC IL28B and 91–100 % in Black patients [5]. Thus, factors that traditionally predicted a poor response to interferon-based therapy do not predict response to ledipasvir/sofosbuvir treatment [10].
Among patients who had failed prior peginterferon-α-based treatment, high SVR12 rates were seen with ledipasvir/sofosbuvir administered for 12 or 24 weeks, with or without ribavirin, in the ION-2 trial (Table 2) [6]. In ION-2, ledipasvir/sofosbuvir achieved high SVR12 rates regardless of whether patients had no response to prior treatment or prior virological breakthrough or relapse, and regardless of whether patients had failed previous treatment with an HCV protease inhibitor plus peginterferon-α and ribavirin or with peginterferon-α plus ribavirin [6].
In the ION trials, ledipasvir/sofosbuvir was effective regardless of the degree of liver fibrosis or the method of fibrosis determination [11]. In addition, among patients achieving SVR12, improvements in patient-reported outcomes were seen regardless of fibrosis stage (e.g. early or advanced hepatic fibrosis) [20].
Significant (p < 0.001 vs. baseline) improvements in most patient-reported outcomes occurred as early as week 2 of treatment with ledipasvir/sofosbuvir without ribavirin, and were maximized by the end of treatment in the ION trials [21]. Changes in measures of health-related quality of life, fatigue and work productivity significantly (p < 0.0001) favoured ledipasvir/sofosbuvir over ledipasvir/sofosbuvir plus ribavirin on the last day of treatment [21].
A randomized, open-label, multicentre, phase 3 Japanese trial included treatment-naïve or treatment-experienced patients with chronic HCV genotype 1 infection who received ledipasvir/sofosbuvir (n = 171) or ledipasvir/sofosbuvir plus ribavirin (n = 170) for 12 weeks; 76 patients (22 %) had compensated cirrhosis at baseline [22]. The SVR12 rate (primary endpoint) was 100 % in ledipasvir/sofosbuvir recipients and 98 % in ledipasvir/sofosbuvir plus ribavirin recipients, with SVR12 rates of 100 and 96 % in treatment-naïve patients and 100 and 100 % in treatment-experienced patients [22].
In patients with chronic HCV genotype 1 infection and compensated cirrhosis who have failed prior treatment with a regimen including peginterferon-α and an HCV protease inhibitor (n = 155), the SVR12 rate (primary endpoint) was 96 % in patients receiving ledipasvir/sofosbuvir plus ribavirin for 12 weeks and 97 % in patients receiving ledipasvir/sofosbuvir for 24 weeks, according to a randomized, double-blind, multicentre phase 2 trial (SIRIUS) [23].
A post hoc, integrated analysis of phase 2/3 trial data also support the use of a 24-week regimen of ledipasvir/sofosbuvir or a 12-week regimen of ledipasvir/sofosbuvir plus ribavirin in treatment-experienced patients with chronic HCV genotype 1 infection who have compensated cirrhosis, including those who have failed prior treatment with an HCV protease inhibitor-containing regimen [24].
In HCV and HIV co-infection
The open-label, multicentre, phase 3 ION-4 trial examined the efficacy of 12 weeks’ therapy with ledipasvir/sofosbuvir in 335 treatment-naïve or -experienced patients co-infected with HCV genotype 1 or 4 and HIV-1 [12]. At baseline, 20 % of patients had compensated cirrhosis and 55 % of patients had not responded to prior anti-HCV therapy; all patients were receiving stable antiretroviral therapy. The overall SVR12 rate (primary endpoint) was 96 %, with SVR12 rates of 94 % in treatment-naïve patients, 97 % in treatment-experienced patients, 96 % in patients without cirrhosis and 94 % in patients with cirrhosis [12].
Results of the open-label, single-centre ERADICATE trial also support the use of ledipasvir/sofosbuvir in patients co-infected with HCV genotype 1 and HIV [25]. ERADICATE included 50 patients without cirrhosis who had not received prior treatment for chronic HCV infection and were antiretroviral naïve or experienced. The SVR12 rate (primary endpoint) was 100 % in antiretroviral-naïve patients and 97 % in antiretroviral-experienced patients following 12 weeks of ledipasvir/sofosbuvir [25].
In HCV genotype 1 or 4 infection following liver transplantation or with decompensated cirrhosis
The open-label, multicentre SOLAR-1 trial included a cohort of treatment-naïve or -experienced patients with recurrence of HCV genotype 1 or 4 infection following liver transplantation (223 evaluable patients) [13]. SVR12 rates (primary endpoint) in patients receiving ledipasvir/sofosbuvir plus ribavirin for 12 or 24 weeks were 96 and 98 % in patients with a fibrosis score of F0–F3 (n = 111), 96 and 96 % in Child-Pugh-Turcotte (CPT) class A cirrhosis, 85 and 83 % in CPT class B cirrhosis and 60 and 67 % in CPT class C cirrhosis [13].
SOLAR-1 also included a cohort of treatment-naïve or -experienced patients with chronic HCV genotype 1 or 4 infection who had decompensated cirrhosis and had not undergone liver transplantation (n = 108) [14]. SVR12 rates (primary endpoint) in patients receiving ledipasvir/sofosbuvir plus ribavirin for 12 or 24 weeks were 87 and 89 % overall, 87 and 89 % in CPT class B cirrhosis and 86 and 90 % in CPT class C cirrhosis [14].
In the open-label, multinational SOLAR-2 trial, treatment-naïve or -experienced patients with HCV genotype 1 or 4 infection who had decompensated cirrhosis (n = 107) or HCV recurrence following liver transplantation (n = 220) were randomized to receive ledipasvir/sofosbuvir plus ribavirin for 12 or 24 weeks [18]. The SVR rate 4 weeks’ post-treatment (SVR4) in patients with decompensated cirrhosis who had not undergone liver transplantation and had received 12 or 24 weeks’ therapy was 86 and 100 % in those with CPT class B cirrhosis and 88 and 50 % in those with CPT class C cirrhosis. SVR4 in patients with HCV recurrence post-liver transplantation who had received 12 or 24 weeks’ therapy was 94 and 100 % in those with a fibrosis score of F0–F3, 97 and 92 % in those with CPT class A cirrhosis, 100 and 100 % in those with CPT class B cirrhosis and 100 and 50 % in those with CPT class C cirrhosis [18].
In chronic HCV genotype 3, 4 or 5 infection
Results of the ELECTRON-2 trial support the efficacy of ledipasvir/sofosbuvir in patients with chronic HCV genotype 3 infection. This trial included treatment arms in which treatment-naïve patients received ledipasvir/sofosbuvir (n = 25) or ledipasvir/sofosbuvir plus ribavirin (n = 26) for 12 weeks [15] and treatment-experienced patients received ledipasvir/sofosbuvir plus ribavirin for 12 weeks (n = 50) [16]. In treatment-naïve patients, SVR12 was seen in 64 % of ledipasvir/sofosbuvir recipients and in 100 % of ledipasvir/sofosbuvir plus ribavirin recipients [15]. In treatment-experienced patients, SVR12 was seen in 82 % of patients overall, with an SVR12 rate of 89 % in patients without cirrhosis and 73 % in patients with cirrhosis [16].
In the open-label SYNERGY trial, treatment-naïve or -experienced patients with chronic HCV genotype 4 infection (n = 21) received ledipasvir/sofosbuvir for 12 weeks, with an SVR12 rate of 95 % [17].
An open-label, multicentre study included treatment-naïve or -experienced patients with chronic HCV genotype 4 (n = 44) or 5 (n = 41) infection who received ledipasvir/sofosbuvir for 12 weeks [19]. SVR4 rates in patients with chronic HCV genotype 4 or 5 infection were 93 and 93 % [19].
What is the tolerability profile of ledipasvir/sofosbuvir?
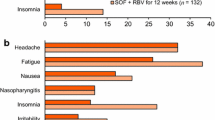
Oral ledipasvir/sofosbuvir was generally well tolerated in patients with chronic hepatitis C. In a pooled analysis of the ION-1, -2 and -3 trials in patients with chronic HCV genotype 1 infection who received ledipasvir/sofosbuvir (n = 1080) or ledipasvir/sofosbuvir plus ribavirin (n = 872), the incidence of adverse events was 74 versus 85 % and the incidence of treatment-related adverse events was 45 versus 71 % [26].
In patients receiving ledipasvir/sofosbuvir (without ribavirin) for 8–24 weeks, the most commonly reported adverse events were fatigue (21–24 % of patients), headache (14–24 %), nausea (7–11 %), diarrhoea (7–10 %), insomnia (5–9 %), arthralgia (4–8 %), irritability (1–6 %), rash (1–6 %), cough (1–6 %) and pruritus (1–4 %) [26]. Most adverse events were of mild to moderate severity [5, 6]. Adverse drug reactions attributed to ledipasvir/sofosbuvir were headache and fatigue [3, 23].
The incidence of adverse events known to be associated with ribavirin was numerically higher in patients receiving ledipasvir/sofosbuvir plus ribavirin than in patients receiving ledipasvir/sofosbuvir [26]. For example, with ledipasvir/sofosbuvir plus ribavirin for 8–24 weeks versus ledipasvir/sofosbuvir for 8–24 weeks, fatigue occurred in 35–40 % versus 21–24 % of patients and insomnia occurred in 12–20 % versus 5–9 %. Anaemia was reported in 7 % of ledipasvir/sofosbuvir plus ribavirin recipients versus 0.09 % of ledipasvir/sofosbuvir recipients [26].
Across the ION-1, -2 and -3 trials, serious adverse events were reported in 0–8 % of patients receiving ledipasvir/sofosbuvir for 8–24 weeks and in 0–3 % of patients receiving ledipasvir/sofosbuvir plus ribavirin for 8–24 weeks [5–7]; no deaths were reported [26]. Discontinuation of ledipasvir/sofosbuvir because of adverse events occurred in 0–3 % of patients [5–7], and dose modification or interruption of treatment because of adverse events occurred in 0.6 % of ledipasvir/sofosbuvir recipients versus 14 % of ledipasvir/sofosbuvir plus ribavirin recipients [26].
The tolerability profile of ledipasvir/sofosbuvir in patients with compensated cirrhosis appeared similar to that in patients without cirrhosis [24]. In the SOLAR trials, ledipasvir/sofosbuvir plus ribavirin was generally well tolerated in patients with recurrence of HCV post-transplantation [13, 18] or in those with decompensated cirrhosis [14, 18].
Ledipasvir/sofosbuvir was also generally well tolerated in patients co-infected with HCV and HIV in the ION-4 [12] and ERADICTAE [25] trials, with no discontinuations because of adverse events. In general, there were no clinically significant changes in CD4 + cell counts [25], HIV RNA levels [12, 25] or renal function [25].
What is the current positioning of ledipasvir/sofosbuvir?
The single-tablet regimen of ledipasvir/sofosbuvir represents a significant advance in the treatment of chronic hepatitis C. A 12-week regimen of ledipasvir/sofosbuvir achieves high SVR12 rates in treatment-naïve patients, with no additional benefit conferred by the addition of ribavirin or extending the treatment duration to 24 weeks. Moreover, an 8-week regimen also achieves high SVR12 rates, with a low relapse rate, in patients with a baseline HCV RNA level of <6 million IU/mL. High SVR12 rates are seen in treatment-experienced patients who receive ledipasvir/sofosbuvir for 12 or 24 weeks. Data also support the use of ledipasvir/sofosbuvir in chronic HCV genotype 4 infection, in HCV and HIV co-infection and, in combination with ribavirin, in patients with chronic HCV genotype 1 or 4 infection who have decompensated cirrhosis or are liver transplant recipients and in chronic HCV genotype 3 infection. Ledipasvir/sofosbuvir plus ribavirin also shows efficacy in the retreatment of patients with chronic HCV genotype 1 infection who did not achieve SVR with prior sofosbuvir-containing therapy [27]. Oral ledipasvir/sofosbuvir is generally well tolerated.
The low pill burden associated with once-daily administration of the single-tablet regimen of ledipasvir/sofosbuvir and shorter treatment durations have the potential to improve treatment adherence. However, ledipasvir/sofosbuvir is an expensive therapy and its acquisition cost represents a barrier to treatment. Analyses of its cost effectiveness in the European setting would be of interest.
Ledipasvir/sofosbuvir is included in recently updated treatment guidelines from the European Association for the Study of the Liver (EASL) [1]. These guidelines recommend ledipasvir/sofosbuvir in a number of settings, including the following:
-
Patients with chronic HCV genotype 1a or 1b infection without cirrhosis who are treatment naïve or treatment experienced should be treated with ledipasvir/sofosbuvir for 12 weeks. Treatment may be shortened to 8 weeks in treatment-naïve patients without cirrhosis who have a baseline HCV RNA level of <6 million IU/mL (this should be done with caution).
-
Patients with chronic HCV genotype 1a or 1b infection and compensated cirrhosis who are treatment naïve or treatment experienced should be treated with ledipasvir/sofosbuvir plus ribavirin for 12 weeks. Patients who cannot receive ribavirin because of contraindications or tolerability issues should receive ledipasvir/sofosbuvir for 24 weeks. Treatment with ledipasvir/sofosbuvir plus ribavirin can be extended to 24 weeks in treatment-experienced patients with negative predictors of response.
-
Patients with chronic HCV genotype 4, 5 or 6 infection without cirrhosis who are treatment naïve or treatment experienced should be treated with ledipasvir/sofosbuvir for 12 weeks.
-
Patients with chronic HCV genotype 4, 5 or 6 infection and compensated cirrhosis who are treatment naïve or treatment experienced should be treated with ledipasvir/sofosbuvir plus ribavirin for 12 weeks. Patients who cannot receive ribavirin because of contraindications or tolerability issues should receive ledipasvir/sofosbuvir for 24 weeks. Treatment with ledipasvir/sofosbuvir plus ribavirin can be extended to 24 weeks in treatment-experienced patients with negative predictors of response.
-
Patients co-infected with HCV and HIV should receive the same treatment as those with HCV monoinfection (taking into account potential drug interactions).
EASL guidelines also discuss the use of ledipasvir/sofosbuvir in patients who have failed treatment with a regimen containing a direct-acting antiviral agent (including sofosbuvir), in patients with decompensated cirrhosis and in patients with recurrent HCV infection following liver transplantation [1].
References
European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C 2015. J Hepatol. 2015;63(1):199–236.
American Association for the Study of Liver Diseases and Infectious Diseases Society of America. Recommendations for testing, managing, and treating hepatitis C (December 19). 2014. http://www.hcvguidelines.org/full-report-view. Accessed 29 Apr 2015.
Harvoni (ledipasvir/sofosbuvir) film-coated tablets: EU summary of product characteristics. London: European Medicines Agency; 2015.
Hebner C, Lee Y-J, Han B, et al. In vitro pan-genotypic and combination activity of sofosbuvir (GS-7977) in stable replicon cell lines [abstract no. 1875]. Hepatology. 2012;56(4 Suppl):1066A.
Afdhal N, Zeuzem S, Kwo P, et al. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med. 2014;370(20):1889–98.
Afdhal N, Reddy KR, Nelson DR, et al. Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N Engl J Med. 2014;370(16):1483–93.
Kowdley KV, Gordon SC, Reddy KR, et al. Ledipasvir and sofosbuvir for 8 or 12 weeks for chronic HCV without cirrhosis. N Engl J Med. 2014;370(20):1879–88.
EMA recommends avoidance of certain hepatitis C medicines and amiodarone together. London: European Medicines Agency; 2015.
Bernstein DE, Mangia A, Brau N, et al. Concordance between SVR4, SVR12 and SVR24 in genotype 1 HCV-infected patients who received all oral fixed-dose combination ledipasvir/sofosbuvir with or without ribavirin in phase 3 clinical trials [abstract no. 1947 plus slide presentation]. Hepatology. 2014;60(4 Suppl):1142A–3A.
Jacobson IM, Kwo PY, Kowdley KV, et al. Virologic response rates to all oral fixed-dose combination ledipasvir/sofosbuvir regimens are similar in patients with and without traditional negative predictive factors in phase 3 clinical trials [abstract no. 1945 plus poster]. Hepatology. 2014;60(4 Suppl):1141A–2A.
Gordon SC, Fried MW, Kwo PY, et al. No differences in the efficacy of fixed-dose combination ledipasvir/sofosbuvir in patients according to fibrosis stage determined by liver biopsy or laboratory biomarker in phase 3 clinical trials [abstract no. 1958 plus poster]. Hepatology. 2014;60(4 Suppl):1149A–50A.
Naggie S, Cooper C, Saag MS, et al. Ledipasvir/sofosbuvir for 12 weeks in patients coinfected with HCV and HIV-1 [abstract no. 152LB]. In: 2015 Conference on Retroviruses and Opportunistic Infections. 2015.
Reddy KR, Everson GT, Flamm SL, et al. Ledipasvir/sofosbuvir with ribavirin for the treatment of HCV in patients with post-transplant recurrence: preliminary results of a prospective, multicenter study [abstract no. 8 plus slide presentation]. Hepatology. 2014;60(4 Suppl):200A–1A.
Flamm SL, Everson GT, Charlton M, et al. Ledipasvir/sofosbuvir with ribavirin for the treatment of HCV in patients with decompensated cirrhosis: preliminary results of a prospective multicenter study [abstract no. 239 plus slide presentation]. Hepatology. 2014;60(4 Suppl):320A–1A.
Gane E, Hyland RH, Pang P, et al. Sofosbuvir/ledipasvir fixed dose combination is safe and effective in HCV infected populations including decompensated patients and patients with prior sofosbuvir treatment experience [abstract no. 238 plus slide presentation]. Gastroenterology. 2014;146(5 Suppl 1):S904–5.
Gane EJ, Hyland RH, An D, et al. High efficacy of LDV/SOF regimens for 12 weeks for patients with HCV genotype 3 or 6 infection [abstract no. LB-11 plus poster]. Hepatology. 2014;60(1 Suppl):22.
Kapoor R, Kohil A, Sidharthan S, et al. All oral treatment for genotype 4 chronic hepatitis C infection with sofosbuvir and ledipasvir: interim results from the NIAID SYNERGY trial [abstract no. 240 plus slide presentation]. Hepatology. 2014;60(4 Suppl):321A.
Manns M, Forns X, Samuel D, et al. Ledipasvir/sofosbuvir with ribavirin is safe and efficacious in decompensated and post liver transplantation patients with HCV infection: preliminary results of the prospective SOLAR 2 trial [abstract no. G02]. J Hepatol. 2015;62(Suppl):S187–8.
Abergel A, Loustaud-Ratti V, Metivier S, et al. Ledipasvir/sofosbuvir treatment results in high SVR rates in patients with chronic genotype 4 and 5 HCV infection [abstract no. O056]. J Hepatol. 2015;62(Suppl):S219–20.
Younossi ZM, Stepanova M, Afdhal N, et al. Improvement of health-related quality of life and work productivity in chronic hepatitis C patients with early and advanced fibrosis treated with ledipasvir and sofosbuvir. J Hepatol. 2015;63(2):337–45.
Younossi ZM, Stepanova M, Marcellin P, et al. Treatment with ledipasvir and sofosbuvir improves patient-reported outcomes: results from the ION-1, 2 and 3 clinical trials. Hepatology. 2015;61(6):1798–808.
Mizokami M, Yokosuka O, Takehara T, et al. Ledipasvir and sofosbuvir fixed-dose combination with and without ribavirin for 12 weeks in treatment-naive and previously treated Japanese patients with genotype 1 hepatitis C: an open-label, randomised, phase 3 trial. Lancet Infect Dis. 2015;15(6):645–53.
Bourlière M, Bronowicki JP, de Ledinghen V, et al. Ledipasvir-sofosbuvir with or without ribavirin to treat patients with HCV genotype 1 infection and cirrhosis non-responsive to previous protease-inhibitor therapy: a randomised, double-blind, phase 2 trial (SIRIUS). Lancet Infect Dis. 2015;15(4):397–404.
Reddy KR, Bourliere M, Sulkowski M, et al. Ledipasvir and sofosbuvir in patients with genotype 1 HCV and compensated cirrhosis: an integrated safety and efficacy analysis. Hepatology. 2015;62(1):79–86.
Osinusi A, Townsend K, Kohli A, et al. Virologic response following combined ledipasvir and sofosbuvir administration in patients with HCV genotype 1 and HIV co-infection. JAMA. 2015;313(12):1232–9.
Alqahtani SA, Afdhal N, Zeuzem S, et al. Safety and tolerability of ledipasvir/sofosbuvir with and without ribavirin in patients with chronic hepatitis C virus genotype 1 infection: analysis of phase III ION trials. Hepatology. 2015;62(1):25–30.
Wyles D, Pockros P, Morelli G, et al. Ledipasvir-sofosbuvir plus ribavirin for patients with genotype 1 hepatitis C virus previously treated in clinical trials of sofosbuvir regimens. Hepatology. 2015;61(6):1793–7.
Keating GM. Ledipasvir/sofosbuvir: a review of its use in chronic hepatitis C. Drugs. 2015;75(6):675–85.
Acknowledgments
The review was updated from Drugs 2015;75(6):675–85 [28] and was reviewed by: S. Saluja, Saran Ashram Hospital, Dayalbagh, Agra, India; R. B. Shah, Department of Pharmacology, GMERS Medical College and Hospital, Gandhinagar, Gujarat, India. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on the manuscript. Changes resulting from comments received were made by the authors on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
Gillian M. Keating is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Rights and permissions
About this article
Cite this article
Keating, G.M. Ledipasvir/sofosbuvir in chronic hepatitis C: a guide to its use in the EU. Drugs Ther Perspect 31, 289–295 (2015). https://doi.org/10.1007/s40267-015-0232-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-015-0232-y