Abstract
Cutaneous adverse drug reactions are unpredictable and include various different skin conditions of varying degrees of severity. The most concerning are usually referred to as severe cutaneous adverse reactions (SCARs) and include acute generalized exanthematous pustulosis (AGEP), drug reaction with eosinophilia and systemic symptoms (DRESS), also known as drug-induced hypersensitivity syndrome (DiHS) or hypersensitivity syndrome (HSS), Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). All are delayed type IV hypersensitivity reactions in which a T-cell-mediated drug-specific immune response is responsible for causing the disease. Nonetheless, specific T-cell subpopulations develop in response to certain environmental conditions and produce cytokines that orchestrate the various phenotypes. Cytotoxic T lymphocytes (CTLs), T-helper type 1 (Th1), Th2, Th17, and regulatory T cells (Treg), among other T-cell subpopulations, participate in the development of SCAR phenotypes. Cell subpopulations belonging to the innate immune system, comprising natural killer cells, innate lymphoid cells, monocytes, macrophages and dendritic cells, can also participate in shaping specific immune responses in various clinical conditions. Additionally, tissue-resident cells, including keratinocytes, can contribute to epidermal damage by secreting chemokines that attract pro-inflammatory immunocytes. The final phenotypes in each clinical entity result from the complex interactions between a variety of cell lineages, their products, soluble mediators and genetic and environmental factors. Although the pathophysiology of these reactions is not fully understood, intensive research in recent years has led to major progress in our understanding of the contribution of certain cell types and soluble mediators to the variability of SCAR phenotypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Aside from the intended therapeutic objective, the use of medications is associated with the risk of adverse drug reactions (ADRs). The World Health Organization defines an ADR as a harmful and unintended response to a drug that occurs upon patients’ exposure to medication doses normally used for the prophylaxis, diagnosis or therapy of disease or for the adjustment of physiological functions [1]. ADRs are a common complication in medical practice and an important cause of morbidity. They are typically classified into two categories: type A, which depend on the pharmacological properties of the drug (“on-target” ADRs), and type B, classically understood as not dependent on the pharmacological properties of the compound (“off-target” ADRs) [2]. Type B ADRs are often referred to as dose-independent and unpredictable, and most of them are considered to be drug hypersensitivity reactions.
According to the World Allergy Organization, hypersensitivity causes objectively reproducible symptoms or signs initiated by exposure to a defined stimulus that is tolerated by normal subjects [3]. It comprises both non-allergic hypersensitivity (the term of choice to describe reactions in which immunological mechanisms cannot be proven) and allergic hypersensitivity, which refers to immunologically mediated drug hypersensitivity reactions. These may be further classified as either immunoglobulin E (IgE)-mediated (immediate) or non–IgE-mediated (delayed) hypersensitivity reactions.
Cutaneous ADRs represent a diversity of diseases ranging in severity from mild, self-limited cutaneous eruptions such as maculopapular exanthema (MPE) to severe cutaneous adverse reactions (SCARs) [4, 5] that represent an uncommon but potentially life-threatening form of delayed hypersensitivity. Illnesses range from acute generalized exanthematous pustulosis (AGEP) to drug reaction with eosinophilia and systemic symptoms (DRESS), also known as drug-induced hypersensitivity syndrome (DiHS) or hypersensitivity syndrome (HSS), and the spectrum of Stevens–Johnson syndrome/toxic epidermal necrolysis (SJS/TEN), which is the most severe form of SCAR, with an overall mortality of 34% at 1 year post-reaction [6].
The pathophysiology of these reactions was hitherto not fully understood. However, intensive research in recent years has contributed greatly to our understanding of the roles played by specific cell types in the variability of SCAR phenotypes. All of them are delayed type IV hypersensitivity reactions triggered by a T-cell-mediated drug-specific immune response. Nonetheless, specific T-cell subpopulations develop in response to certain environmental conditions and produce cytokines that orchestrate a variety of specific immune responses. T-cell subpopulations such as cytotoxic T lymphocytes (CTLs), T-helper type 1 (Th1), Th2, Th17, and regulatory T cells (Treg), among others, may contribute to the development of SCARs. Cell populations belonging to the innate immune system, including natural killer (NK) cells, innate lymphoid cells, monocytes, macrophages and dendritic cells (DCs), can also participate in shaping clinical phenotypes. Additionally, tissue-resident cells, including keratinocytes, can contribute to epidermal damage by secreting chemokines that attract pro-inflammatory immunocytes [7, 8]. In addition, environmental and genetic factors may participate in the pathophysiological mechanisms responsible for the various clinical pictures.
2 Clinical Entities and Clinicopathological Features
2.1 Acute Generalized Exanthematous Pustulosis (AGEP)
AGEP is characterized by the acute appearance of numerous non-follicular sterile pustules on erythematous background, fever and neutrophilia [9]. It is generally attributed to drugs, most frequently aminopenicillins [9], but other triggers have also been reported [10, 11]. Subcorneal or intraepidermal pustules formed by the accumulation of neutrophils are the main histologic findings. Exocytosis of neutrophils and eosinophils can be observed, and lymphocytes are also present in dermal infiltrates with a predominance of cluster of differentiation (CD)-4 + cells [10, 12, 13].
The incidence is low, with fewer than ten cases per million inhabitants per year [14]. An acute onset and spontaneous resolution within 2 weeks upon drug withdrawal are characteristics. An international case–control study (EuroSCAR) estimated a mortality rate of around 4% [9, 15], although a review of cases reported to the French Pharmacovigilance Centres suggested that the rate could be lower [16].
2.2 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
DRESS is characterized by a polymorphous skin rash, hematologic alterations (eosinophilia, atypical lymphocytosis), lymphadenopathy and internal organ involvement [17, 18]. Sequential herpesvirus reactivation has been observed [19]. It is characterized by a delayed onset (up to 8 weeks) and a prolonged course with frequent relapses. Terms such as anticonvulsant hypersensitivity syndrome, allopurinol hypersensitivity syndrome and drug-induced pseudolymphoma [17, 20, 21] have also been used to refer to this condition. The Japanese Research Committee on Severe Cutaneous Adverse Reactions (JSCAR) proposed the acronym DiHS [22]. Diagnostic criteria for DRESS were published by the RegiSCAR group [23]. Diagnostic criteria for DiHS include human herpesvirus (HHV)-6 reactivation as a requisite for diagnosis of a definitive case [24]. It is of note that HHV-6 reactivation is detected at 2–4 weeks after onset exclusively in DiHS/DRESS but not in SJS/TEN [25]. Nonetheless, the exact role of HHV-6 in the pathogenesis of the disease has not yet been established. The term DRESS is hereinafter used to refer to this condition.
Drug causality has been reported as highly probable in about 80% of cases of DRESS [26, 27]. Anticonvulsants, allopurinol, sulfonamides and antibiotics were responsible for 96% of cases in a European study [27]. Antiretroviral agents such as nevirapine and abacavir are commonly reported in association with this syndrome [26, 28, 29], although hypersensitivity reactions to abacavir generally exhibit earlier onset and different symptoms from those of classical DRESS [14, 30, 31]. Therefore, severe adverse reactions to abacavir are preferably classified as abacavir hypersensitivity.
Various inflammatory patterns can be found in a single biopsy, namely interface dermatitis, lichenoid, eczematous, AGEP-like vascular damage, superficial perivascular infiltration, peri-appendage infiltration and erythema-multiforme-like patterns. Although no single pathological finding is specific enough to confirm a diagnosis, the co-existence of three histopathological patterns in a skin specimen has a higher likelihood of being a definite case and is correlated with clinical severity. Interestingly, despite being considered a Th2 disease, infiltrating cutaneous lymphocytes include high numbers of CD8 + and granzyme B + T cells [32, 33].
The exact incidence is difficult to calculate because of the variable presentation of this syndrome. It was estimated as ten cases per million inhabitants per year in Japanese patients [34]. Nonetheless, the frequency could be growing, as milder forms of the disease are being described [18, 35, 36]. Retrospective analyses have reported the principal causes of death as multiorgan failure and septic or cardiogenic shock, with mortality rates of 5–10% [26, 37], and a prospective study reported a mortality rate of 1.7% [27].
Key aspects of management are withdrawal of the culprit drug and close monitoring, with evaluation of hepatic and renal function. Evidence is insufficient to support the best pharmacological treatment for SCARs. Systemic corticosteroids are the mainstay treatment for patients with DRESS, although other alternatives have been proposed (reviewed by Cho and Chu [38]).
2.3 Stevens–Johnson Syndrome/Toxic Epidermal Necrolysis (SJS/TEN)
Epidermal detachment mimicking burned skin and mucosal involvement are typical manifestations of SJS/TEN. Two or more mucous membranes are affected, with often severe conjunctival affectation. Internal organs may also be involved, and lymphopenia, primarily affecting CD4 + T cells, has also been reported [39,40,41].
SJS and TEN are severity variants of the same clinical condition, differing only in the percentage of body surface area (BSA) detached: < 10% in SJS, > 30% in TEN, and cases with 10–30% of detached BSA are considered as SJS-TEN overlapping forms [42]. Full-thickness epidermal necrosis is the pathognomonic feature of SJS/TEN. Although in skin biopsies the infiltrate is scarce, the analysis of blister fluids reveals the presence of large amounts of lymphocytes [43] and monocytes at later stages [44, 45]. Although epidermal necrolysis (EN) has been proposed as an alternative name for this spectrum of conditions [46], the term SJS/TEN continues to be used.
A drug reaction is most often the etiological cause [47, 48]. Aromatic anticonvulsants, allopurinol, sulfonamides, nonsteroidal anti-inflammatory drugs (NSAIDs) and antibiotics are most frequently associated [49]. However, other etiologic factors may be responsible in up to 15% of cases. Idiopathic cases of SJS/TEN are more common in children, and only a very small fraction of these can be consistently attributed to infectious agents such as Mycoplasma pneumoniae [50, 51]. A variant of Coxsackie virus A6 has been reported to cause a severe mucocutaneous blistering condition that is indistinguishable from SJS/TEN, principally in children [52].
A prospective population-based registry in Germany estimated an incidence of 1.53–1.89 cases per million inhabitants per year [15], although rates may be higher in certain ethnic groups such as patients of Asian descent [53], and the occurrence is approximately 100-fold higher among HIV-infected individuals [54]. Mortality rates are related to the % BSA affected. Frequencies of 12%, 29% and 46% for SJS, SJS/TEN overlap, and TEN, respectively, have been reported by the RegiSCAR study group [6]. Moreover, patients surviving SJS/TEN are at risk for a multitude of sequelae, including cutaneous scarring; dyspigmentation; dental, genitourinary and pulmonary complications; and, most often, ocular lesions [55]. Most of these have a considerable impact on the patient’s quality of life and make SJS/TEN a chronic condition [56, 57].
As mentioned, evidence is insufficient to support a pharmacological treatment for SJS/TEN. The mainstay of treatment is the identification and removal of the culprit drug, and no therapies beyond supportive care have been established. Several immunomodulatory treatments have been used, including systemic corticosteroids, cyclosporine, intravenous immunoglobulin, plasmapheresis, and anti-TNF-α, among others [38].
3 Immune-Mediated Mechanisms Involved in Severe Cutaneous Adverse Reactions (SCARs)
SCARs are delayed T-cell-mediated type IV hypersensitivity reactions in the Gell and Coombs classification [58] in which drug-specific T cells can be identified in the peripheral blood or skin infiltrates. The variation in clinical conditions has resulted in type IV reactions being further sub-classified according to different cytokine production patterns by T cell subsets and to the contribution of certain subpopulations of leukocytes to the inflammation and tissue damage. In this classification, type IVa reactions include Th1 immune responses with the release of large quantities of interferon (IFN)-γ and the participation of monocytes. Type IVb reactions correspond to Th2 responses with production of interleukin (IL)-4, IL-13 and IL-5, which result in the eosinophilia characteristics in some drug allergies. In type IVc reactions, CTLs are the main effectors of tissue injury. Finally, in type IVd reactions, T cells promote the recruitment of neutrophils to affected tissue through the secretion of IL-8/CXCL8 [59, 60]. Traditionally, DRESS is considered a type IVb Th2-driven reaction, SJS/TEN a type IVc cytotoxic reaction, and AGEP a type IVd reaction [61] (Fig. 1). Although this classification may be useful for the understanding of T-cell-mediated adverse reactions, there is overlap between the subtypes, and they are not mutually exclusive. For example, high IFN-γ levels (typical of type IVa) have been identified in serum and blister fluid from patients with SJS/TEN [41, 62], and drug-specific CD8 + cytotoxic T cells (typical of type IVc) may also be involved in DRESS and AGEP [12, 32, 63]. On the other hand, any of these reactions may occur in response to any drug, meaning that similar immune mechanisms are triggered in response to different chemical compounds.
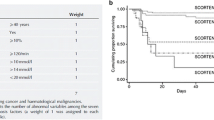
Proposed model for severe cutaneous adverse reaction immunopathogenesis. a Drug-specific T cells release cytolytic proteins and other mediators of inflammation. b A revised Gell and Coombs classification has been proposed according to the effector cells and cytokine profiles involved. AGEP acute generalized exanthematous pustulosis, DRESS drug reaction with eosinophilia and systemic symptoms, HLA human leukocyte antigen, IL interleukin, NK natural killer, SCAR severe cutaneous adverse reaction, SJS Stevens–Johnson syndrome, TcR T-cell receptor, TEN toxic epidermal necrolysis, Th2 T-helper type 2
3.1 Soluble Mediators, Cytokines, Chemokines and Leukocyte Subpopulations Involved
3.1.1 Soluble Mediators and Leukocyte Subpopulations in AGEP
In addition to drug-specific T cells, neutrophils and the neutrophil chemotactic factor IL-8/CXCL8 are key players in the skin phenotype in AGEP. IL-8/CXCL8 may also contribute to the activation and mobilization of neutrophils from the bone marrow to the peripheral blood, causing leukocytosis and neutrophilia. Drug-specific CD4 + T cells expanded from patients with AGEP have been shown to produce IL-8/CXCL8 and granulocyte macrophage colony-stimulating factor (GM-CSF) [12, 64, 65], which could also stimulate myelopoiesis. These T-cell clones also expressed the IL-8/CXCL8-specific receptor CXCR1, which could explain their recruitment to the skin [12]. Drug-specific T-cell clones also released IFN-γ and TNF-α [65], and a small proportion secreted IL-4 and IL-5 [12]. The expression of IL-8/CXCL8 by keratinocytes was also detected in skin biopsies from patients with AGEP [12, 13, 66]. The local production of IL-8 in the skin may create a gradient for neutrophil and T-cell recruitment to the epidermis. Early infiltration by CD8 + cytotoxic T cells can also facilitate epidermal leukocyte exocytosis [64].
The cytokines IL-17 and IL-22 are hallmarks of Th17 immune responses. Increased frequencies of circulating Th17 cells as well as elevated serum concentrations of IL-22 have been reported in AGEP [67]. In addition, Th17 cells have been identified in skin infiltrates [68]. In this sense, IL-17 has been shown to cooperate with IFN-γ and TNF-α in stimulating the production of IL-8 by keratinocytes [69, 70]. C-C motif chemokine receptor (CCR)-6 expression is a distinctive feature of Th17 lymphocytes [71]. Interestingly, CCR6 +-infiltrating lymphocytes have been described in affected skin [65], as has the expression of the CCR6 ligand CCL20 [66]. Altogether, these findings suggest cooperation between IL-8/CXCL8 and Th17 lymphocytes in the neutrophilic inflammation characteristic of this clinical condition (Fig. 2a).
Various immunocytes and skin stromal cells cooperate to induce the clinical phenotypes in SCARs. Subcorneal pustules are generated in AGEP-affected skin by the accumulation of neutrophils (PMN) recruited through CXCL8/IL-8 production by CD4 + T cells and keratinocytes. The chemokine CCL20 recruits CCR6 + Th17 lymphocytes to the skin (a). DRESS-affected skin is infiltrated with CD4 +, CD8 + and Tregs as well as with monomyeloid cells such as pDCs and Mo. The chemokine CCL17/TARC produced by dermal DCs recruits CCR4 + Th2 T cells. High levels of IL-5 and Th2 chemokines produced by Th2 and ILC2 promote peripheral and tissular eosinophilia (b). Detachment of the dermo-epidermal junction, and keratinocyte necrosis are the hallmarks of SJS/TEN. The chemokine CCL27/TARC recruits CCR10 + T cells to the skin. CTLs as well as NK cells secrete cytolytic molecules leading to keratinocyte necrosis. Among them, granulysin may also act as an alarmin in recruiting Mo and DCs, which in turn may produce death ligands such as TNF-α, Tweak and TRAIL. Th17 cells may also contribute to create a pro-inflammatory environment (c). AGEP acute generalized exanthematous pustulosis, BM bone marrow, CD cluster of differentiation, CTL cytotoxic T lymphocyte, DC dendritic cell, DRESS drug reaction with eosinophilia and systemic symptoms, GNLY granulysin, GM-CSF granulocyte macrophage colony-stimulating factor, IFN interferon, IL interleukin, ILC2 type 2 innate lymphocytes, Mo monocytes, NK natural killer, NO nitric oxide, PBC, pDCs plasmacytoid dendritic cells, PMNs polymorphonuclear neutrophils, SCAR severe cutaneous adverse reaction, SJS Stevens–Johnson syndrome, TEN toxic epidermal necrolysis, Th2 T-helper type 2, TNF tumor necrosis factor, Treg regulatory T cells
Genetic studies have suggested that the IL-36–IL-36Ra axis could be involved in AGEP [72]. IL-36α and IL-36γ expression was observed in in AGEP skin biopsies [73, 74], being keratinocytes, T cells and macrophages the main source of IL-36 in the skin, and monocytes are the main source of IL-36 in peripheral blood mononuclear cells (PBMCs) stimulated in vitro with the culprit drugs [74]. However, further research is needed to elucidate the involvement of IL-36 in the pathophysiological mechanisms of the disease.
3.1.2 Soluble Mediators and Leukocyte Subpopulations in DRESS
Activated lymphocytes and eosinophils are the main players in the cutaneous and systemic inflammation in DRESS. CD4 + and cytotoxic T cells were identified in biopsies of skin and affected organs [75], as were dense infiltrations of eosinophils [76, 77], supporting a role for these leukocyte subpopulations as mediators of tissue damage (Fig. 2b). Increased levels of IL-5, an eosinophil-specific differentiation factor and a Th2 chemokine, are associated with the development of eosinophilia [78, 79]. As a result of these findings, the anti-IL-5 monoclonal antibody mepolizumab was recently proposed as a novel therapeutic approach for DRESS [80]. IL-13- and IL-4-producing CD4 + T cells may also play a role [81], which confirms a Th2 pattern for this disease. On the other hand, CCL17 (TARC), which is also regarded as a Th2 chemokine expressed by dermal macrophages in skin biopsies, has been associated with the recruitment of CCR4 + Th2 lymphocytes to the skin. Moreover, the frequencies of Th2 lymphocytes positively correlated with serum TARC levels in patients with DRESS. Additionally, serum TARC levels correlated with HHV-6 reactivation [76, 82]. The serum levels of other proinflammatory cytokines such as TNF-α and IFN-γ were also found to be elevated in the acute stages of DRESS [83].
Innate type 2 lymphoid cells (ILC2s) expressing the IL-33 receptor ST2 were recently identified in the skin and blood of patients with DRESS during the acute phase, together with high serum concentrations of soluble ST2 and IL-33 [84].
3.1.3 Soluble Mediators and Leukocyte Subpopulations in SJS/TEN
Full-thickness epidermal necrosis upon massive apoptosis of keratinocytes is the characteristic feature of SJS/TEN [85]. Cytotoxic CD8 + T cells are thought to be the principal effectors of epidermal necrosis [86], although some researchers have suggested that a fratricide killing mediated through Fas–FasL interactions on the membrane of adjacent cells could also induce apoptosis of keratinocytes [87]. However, multiple players may be involved (Fig. 2c).
Early studies found increased serum and blister fluid concentrations of TNF-α, IFN-γ, IL-6, IL-1 and IL-10. Gene expression studies indicated that only IFN-γ and IL-18 were produced by mononuclear cells present in the vesicles and suggested that other cytokines present, such as TNF-α, sFas-L and IL-10, more likely originated from tissue-resident or stromal cells [62, 88, 89]. Fas-L was indeed overexpressed on the membranes of keratinocytes in affected skin [62]. However, the role of Fas-L as an effector molecule in SJS/TEN remains a matter of debate as previous findings have not always been reproduced [90]. On the other hand, elevated concentrations of soluble Fas-L (sFas-L) in blister fluid and serum, and the release of sFas-L by drug-activated lymphocytes, led to the hypothesis of T-cell-derived sFas-L involvement in the induction of keratinocyte apoptosis [91, 92]. This hypothesis was confronted by the finding that only membrane-bound Fas-L is essential for T-cell-induced apoptosis [93]. In the same publication, the authors stated that excess sFas-L appeared to promote autoimmunity and tumorigenesis through non-apoptotic activities. However, it was recently reported that sFas-L could induce keratinocyte apoptosis and epidermal detachment in a murine model of pemphigus vulgaris [94]. These novel findings suggest that further investigation into the putative role of Fas–Fas-L interactions in affected skin in SJS/TEN is needed and highlight the relevance of accurate differential diagnosis, as different findings may be associated with different clinical presentations.
Recent reports have also identified IL-17-expressing cells in the peripheral blood and blister fluid of patients with SJS/TEN [95, 96], as well as high frequencies of CCR6 + Th17 lymphocytes infiltrating the skin [95]. IL-17 and IFN-γ may act synergistically to increase the production of pro-inflammatory cytokines by human keratinocytes [69].
In addition to pro-inflammatory cytokines, the blister fluid of patients with SJS/TEN is rich in cytolytic proteins such as perforin, granzyme B and granulysin, in agreement with the identification of CD3 + CD8 + T cells and other cytotoxic lymphocytes such as CD3-CD56 + NK cells [41, 97]. Previous studies have reported drug-specific, major histocompatibility complex (MHC) class I-restricted, perforin/granzyme-mediated cytotoxicity of CTLs [86], as well as NK cell activity within blisters of patients with SJS/TEN [44]. Among the cytolytic proteins evaluated, granulysin, a component of the cytotoxic granules of CTLs and NK cells, was highly expressed at the messenger RNA (mRNA) and protein levels. In vitro studies showed that blister fluids may decrease keratinocyte viability in a granulysin-dependent manner, and the cutaneous injection of granulysin led to epidermal necrosis in mice. Granulysin was then proposed as the principal mediator of disseminated keratinocyte death in SJS/TEN [97]. Various levels of granulysin were also detected in CD8 + and NKP46 + (NK) cells in other cutaneous drug reactions [98].
The presence of NK cells expressing granulysin within the blister fluid suggests that this lymphocyte subpopulation may cooperate with CTLs in the killing of keratinocytes. While T-cell activation is highly dependent on T-cell receptor (TCR) recognition of the specific antigen, NK cell activity is the result of a balance between activating and inhibitory signals, which are sensed by an array of activating and inhibitory receptors [99]. Among NK-activating receptors, CD94/NKG2C might be involved in the killing of keratinocytes through the recognition of its ligand human leukocyte antigen (HLA)-E [41].
A recent report identified serum IL-15 as a biomarker of SJS/TEN [100]. IL-15 and granulysin levels were significantly correlated with the severity of the disease as measured with the SCORTEN scale [101]. Furthermore, serum IL-15 concentrations were positively correlated with mortality. Therefore, the study proposed serum IL-15 as a diagnostic and prognostic molecule in SJS/TEN [100]. The results are particularly relevant, as IL-15 is one of the main factors supporting the differentiation and acquisition of effector functions by cytotoxic lymphocytes, including CTLs and NK cells [102]. In particular, the expression of granulysin in CTLs and NK cells is highly dependent on IL-15 [103]. It has been thus suggested that IL-15 could not only be a diagnostic and prognostic marker but also a therapeutic target in SJS/TEN [104].
Single nucleotide polymorphisms of IKZF1 encoding ikaros, a transcription factor involved in T-cell development, have been identified as risk factors for SJS/TEN with severe mucosal involvement [105].
The keratinocyte-specific chemokine CCL27 (CTACK) recruits CCR10 + lymphocytes. Increased CCL27 expression in SJS/TEN-affected skin, along with increased levels of CCR10 transcripts within the infiltrate and in blister fluid cells, strongly suggests that CCL27 may be involved in the recruitment of CCR10 + lymphocytes to the epidermis. Moreover, higher frequencies of CCR10 + lymphocytes were found in the peripheral blood of patients in the acute phase of SJS/TEN [106].
Other than lymphocytes, monocytes, macrophages and DCs may also infiltrate the skin and contribute to cutaneous inflammation through the release of soluble mediators. Tohyama et al. [107] reported finding CD137L-expressing pro-inflammatory CD14 + CD16 + monocytes in the dermo-epidermal junction in SJS/TEN skin lesions and suggested that they may stimulate the activity of CTLs. Araujo et al. [108] found CD1a + and CD14 + monocytes in blister fluid and demonstrated that these cells were able to produce the death ligands TNF-α, TWEAK and TRAIL. Moreover, concentrations of these proteins in blister fluid from patients with SJS/TEN were higher than those in normal human serum or blister fluid from patients with other clinical conditions [108]. Among these, TNF-α has been proposed as a therapeutic target in SJS/TEN [109].
Additional products of monomyeloid cells, such as matrix metalloproteinase (MMP)-9 and lipocalin 2, were also found to be overexpressed in acute SJS/TEN [110,111,112], suggesting their involvement in epidermal detachment. A recent report also identified MMP-9 in tears from patients with SJS [113].
3.2 Damage-Associated Molecular Patterns (Alarmins) in SCARs
Immune cells recognize broadly expressed pathogen-associated molecular patterns (PAMPs) through an array of pattern-recognition receptors (PRRs) such as toll-like receptors (TLRs). Damage-associated molecular patterns (DAMPs), or “alarmins”, are endogenous agonists of PRRs released by injured tissues to alert and activate the immune system [114, 115]. Overexpression of genes encoding several alarmins has been found in acute SJS/TEN samples [110], including S100A8 and S100A9 genes, among others. In line with this finding, S100A8/S100A9 protein complexes (calprotectin) have been identified in skin biopsies from patients with SJS/TEN [116, 117].
Transcripts of other members of the alarmin family, such as antimicrobial human neutrophil peptides (HNP)-1, 3 and HNP4, also known as α-defensins, were found to be overexpressed in T cells, and protein levels in blister fluid were higher than those in plasma samples from the same donors [118]. Besides their antimicrobial properties, α-defensins may regulate inflammatory processes such as wound healing [119], and elevated concentrations can show cytotoxic activity against mammalian cells [120], suggesting that they could also mediate epidermal damage.
Interestingly, granulysin has been reported to be a TLR4 ligand and to function as an endogenous alarmin through the activation and recruitment of antigen-presenting cells (APCs) [121]. Moreover, differentiation of monocytes into antigen-presenting DCs is induced by 15 KDa granulysin [122].
HMGB1 is a well-known member of the DAMP/alarmin family. It is a non-histone chromatin protein with dual functions: transcriptional regulation and extracellular triggering of inflammation through the recruitment and activation of immunocompetent cells. High levels of HMGB-1 have been detected in blood and skin lesions in the active phase of DRESS [123,124,125]. However, other authors have found higher levels in the serum of patients with SJS/TEN than in serum from patients with DRESS [126, 127] and in blister fluid from patients with SJS/TEN than in serum samples from the same donors [128].
IL-33 is a recently identified DAMP/alarmin. Like HMGB1, it is a nuclear protein that is released to the extracellular space upon cell damage. Recent investigations have identified high serum levels of IL-33 specifically in patients with TEN compared with patients with SJS, DRESS, mild cutaneous reactions, and healthy individuals [125]. Therefore, the presence of IL-33 in serum at high concentrations has been proposed as a biomarker of severity in SJS/TEN. On the other hand, high serum levels of IL-33 were recently reported in the acute stages of DRESS, and it was suggested as a potential biomarker of severity [84].
Further research is needed to clarify the involvement of DAMPs in SCARs.
3.3 Human Leukocyte Antigens as Determinants of Drug-Specific Immune Responses and Genetic Risk Factors for SCARs
Early studies suggesting a weak association between some HLA serotypes and SJS/TEN [129] and the report of a few family cases [130, 131] led researchers to suspect a genetic susceptibility to SCARs. This was strongly supported by the finding of a robust association between HLA-B*57:01 and hypersensitivity reactions to abacavir [132, 133] followed by the report of a 100% association of HLA-B*15:02 with SJS/TEN to carbamazepine [134] and the identification of HLA-B*58:01 as a risk factor for allopurinol-induced SCARs in Han Chinese patients [135]. These seminal investigations have been followed by HLA-typing studies confirming the significant associations of these alleles across various populations in which the respective alleles are prevalent (reviewed in White et al. [136], Sousa-Pinto et al. [137] and Chen et al. [138]). It is of note that the HLA encoding genes are the most polymorphic of the whole human genome, and the distribution of the various alleles is quite heterogeneous across human populations from different geographic locations. This makes necessary specific studies on defined ethnic groups and hinders the identification of strongly associated HLA alleles in populations with high rates of genetic exchange resulting from migration, such as the populations of Europe and North America [139]. In this regard, it is interesting that the prognostic value of HLA-B*57:01 as a risk factor to develop abacavir hypersensitivity was initially questioned after reports of low sensitivity in some population groups such as Hispanic patients and those of African descent. However, further studies showed a strong association for patch test-confirmed cases across all ethnicities [140].
A study in European patients found an association between HLA-A*31:01 and cutaneous hypersensitivity reactions to carbamazepine [141]. A further analysis found this allele was strongly associated with DRESS to carbamazepine in Europeans and Han Chinese and weakly associated with SJS/TEN in Europeans but not Han Chinese patients [142]. Interestingly, the association between HLA-A*31:01 and carbamazepine-induced MPE had been previously described in Han Chinese patients [143].
Associations between HLA-B*38:01 and lamotrigine-induced SJS/TEN and between HLA-A*24:02 and lamotrigine-induced DRESS have been reported in Spanish patients [144]. The association between HLA-B*38:01 and lamotrigine-induced SJS/TEN had been previously reported among European patients [145]. On the other hand, HLA-A*24:02 was found to be a genetic risk factor for lamotrigine-induced MPE in Norwegian [146] and Korean populations [147].
Altogether, these findings underscore the importance of accurate phenotyping to perform genetic studies and suggest that the HLA allele may somehow shape the clinical phenotype. Moreover, the common alleles in carbamazepine- and maybe also lamotrigine-induced DRESS and MPE suggest a continuum between MPE and DRESS, in agreement with recent publications [35, 36]. Further research is needed to confirm these data and to clarify how specific HLA alleles may influence the clinical picture.
Strong associations were recently identified between HLA-B*13:01 and dapsone-induced hypersensitivity reactions in Asians [148], between HLA-B*59:01 and methazolamide-induced SJS/TEN in Korean, Japanese and Han Chinese patients [149] and between HLA-A*32:01 and vancomycin-induced DRESS in North American patients [150] (Table 1).
The identification of certain HLA-I alleles as risk factors has impelled the implementation of genetic testing for the prevention of severe hypersensitivity reactions [151]. HLA-B*57:01 has 100% negative predictive value (NPV) for abacavir hypersensitivity reactions and 55% positive predictive value (PPV) [136]. This makes HLA-B*57:01 testing highly cost effective for the prevention of hypersensitivity reactions. HLA-B*57:01 screening before abacavir prescription is part of guideline-based routine HIV practice in the developed world [30]. With respect to other HLA alleles that show strong associations with SCARs, high NPVs have also been calculated for HLA-B*15:02 in relationship with carbamazepine-induced SJS/TEN and for HLA-B*58:01 in allopurinol-induced SCARs in Asian populations. Although the PPV is low in both cases [152], HLA-B*15:02 screening before carbamazepine prescription has been introduced into routine clinical practice in several Southeast Asian countries such as Taiwan, Singapore, and Hong Kong, where significant reductions in carbamazepine-associated SJS/TEN have been achieved [153].
3.4 Mechanisms of Drug-Specific T-Cell Recognition
The in vitro development of drug-specific T-cell clones and the identification of memory T-cell responses to drugs in the peripheral blood of patients strongly support the concept that cutaneous ADRs are drug-specific T-cell-mediated diseases.
The specificity of each T-cell clone results from its unique TCR. Somatic recombination of the TCR genes can lead to a theoretical number of 1016 different specificities [154]. Unlike immunoglobulins, the TCR cannot recognize soluble antigens. In order to be stimulated, T cells need APCs that display antigen-derived proteolytic peptides bound to HLA molecules on the cell surface. Under conditions of homeostasis, HLA molecules are loaded with endogenous peptides, and T cells are “educated” during thymic development not to be reactive against those endogenous peptides. According to this model, since most drugs are small non-peptide molecules, they cannot be directly recognized by the TCR and thus cannot stimulate T cells. However, some drugs, such as β-lactam antibiotics, behave as haptens, as they spontaneously form covalent bonds with peptide residues in serum or cellular proteins. In this way, drugs can be presented by APCs and recognized by specific T cells. Other compounds do not have chemically reactive groups but can acquire them through cellular metabolism and subsequently form covalent bonds to cellular proteins. The ability to form protein adducts is the basis for the hapten/pro-hapten model of T-cell drug recognition. However, many drugs, such as carbamazepine, allopurinol or sulfamethoxazole, have been shown to be directly recognized by the TCR upon non-covalent interactions with HLA and/or TCR molecules. This mechanism of T-cell recognition was called “pharmacological interaction” or “p-i” concept and also works for drugs that are capable of forming covalent bonds, such as β-lactams [155]. These models (hapten, pro-hapten and “p-i”) involve a direct interaction or recognition of the drug by the TCR. More recently, three different research groups have independently and simultaneously described an additional mechanism for drug-specific T-cell activation [156,157,158]. In particular, this mechanism was described specifically for T-cell stimulation of abacavir-specific HLA-B*57:01-restricted T cells. Several groups have reported the exquisite restriction of HLA-B*57:01 for T-cell responses to abacavir, as highly homologous alleles such as HLA-B*57:02 cannot stimulate T cells in response to abacavir [156]. The crystal structure of HLA-B*57:01 in complex with abacavir and peptide was solved and revealed that, in this case, the drug (abacavir) binds to the F pocket of the peptide-binding groove in HLA-B*57:01, changing its stoichiometry and thus the amino acid sequences of the peptides presented by the HLA-B*57:01 molecule to the TCR. In this case, abacavir-stimulated T cells do not recognize the drug directly, instead recognizing a set of endogenous autologous peptides that were not previously captured by HLA-B*57:01 in the absence of abacavir, and thus no thymic education could be achieved in order not to be reactive. The response to abacavir in HLA-B*57:01 carriers is likely polyclonal as an array of new peptides are exposed in all tissues, and HLA class I molecules are expressed in all the nucleated cells of the body. This is a possible explanation for the high PPV of HLA-B*57:01 for predicting abacavir hypersensitivity. This model is known as the “altered peptide” model [159]. To date, it has only been described for the recognition of abacavir, but its potential applicability to other small compounds cannot be ruled out (Fig. 3).
Models of T-cell activation by drugs. Three models have been proposed. The hapten/pro-hapten model postulates that drugs form covalent bonds with protein residues to generate neoantigens that are recognized by T cells. This model may require protein metabolism and antigen processing of haptenized proteins. The pharmacologic interaction (p-i) model postulates that labile non-covalent interactions are established between the drug and the HLA molecule (or the TCR). This model does not require drug metabolism and may require high concentrations of soluble drugs. In the third model, known as the altered peptide model, the drug binds with high affinity to the peptide-binding cleft before peptide loading. This alters its conformation and causes an alteration of the peptide repertoire presented by the HLA molecule. The new peptides are then recognized as “foreigners” by the T cells. HLA human leukocyte antigen, TCR T-cell receptor
Mechanistic studies following epidemiological studies have also confirmed that carbamazepine-specific T cells are restricted by HLA-B*15:02 [160]. Other HLA-B15 members of the B75 serotype may also facilitate carbamazepine-induced keratinocyte killing in vitro [160]. The mechanism for T-cell recognition involves non-covalent interactions between carbamazepine and HLA-B*15:02. Site-directed mutagenesis analysis suggest that a few heavy chain residues are key to allowing carbamazepine presentation and a shared and restricted (public) TCR clonotype was identified as being responsible for carbamazepine recognition within the context of HLA-B*15:02 [161]. As the somatic rearrangement of TCR genes is a stochastic process, this may explain why only a small fraction of the population develops carbamazepine-induced SCARs. Yet, we cannot explain why certain HLA alleles determine a specific cutaneous phenotype. The model for T-cell recognition involves a direct interaction between TCR and carbamazepine on the surface of the peptide–HLA–drug molecular complex. Much less is known about HLA-A*31:01-restricted carbamazepine recognition by T cells even though HLA-A*31:01-restricted specific T-cell clones were identified in a carbamazepine-allergic patient [162].
Regarding allopurinol, oxypurinol (the principal metabolite) has been described as being responsible for eliciting most of the HLA-B*58:01-restricted T-cell responses [163], although allopurinol-specific T cells were also detected. Oxypurinol-specific T cells were mainly restricted by HLA-B*58:01, whereas allopurinol-specific T cells were less allotype specific. Current evidence suggests that oxypurinol-specific T-cell recognition also occurs upon non-covalent interactions between the drug and the HLA molecule. However, mutagenesis analysis indicated that R97V substitution, involving the antigen-binding cleft of HLA-B*58:01 reduced T-cell activation. In silico models also support a role of the antigen-binding cleft as a docking site for oxypurinol. The model proposes that, at high concentrations, oxypurinol may be incorporated into the HLA-peptide complex on the cell surface, thereby altering its conformation and creating a new antigen that would be recognized by specific TCRs. The generation of a multiple collection of novel HLA–peptide–drug complexes is consistent with the private and diverse TCR usage in allopurinol/oxypurinol allergic and control donors [163,164,165]. In this case, and unlike the model proposed for carbamazepine, the surface of interaction would involve primarily the peptide and the TCR. Interestingly, a protruding peptide conformation (consistent with the model proposed for carbamazepine presentation to T cells) has been observed for some public TCRs [154].
Recent reports have also confirmed the involvement of HLA-B*13:01 in drug presentation to dapsone-specific T cells [166, 167].
An exhaustive review of the mechanisms involved in drug recognition by T cells can be found in Illing et al. [168].
3.5 Mechanisms Proposed for the Development of Drug-Specific T Cells: De Novo Immune Responses and Heterologous Immunity
3.5.1 De Novo Immune Responses
Few data are available regarding the nature of drug-specific immune responses in drug hypersensitivity reactions. Some research has focused on finding pathways that would facilitate de novo immune responses to medications within the context of sterile inflammation. Naïve T cells need to receive at least two signals to be activated and to acquire effector functions, namely the antigenic signal (signal 1) received through stimulation of the TCR, and costimulatory signals (signal 2), provided by professional APCs, such as mature DCs. DCs might receive maturation signals from other cells (keratinocytes, NK cells and B cells). However, some reports suggest that DCs may be able to metabolize certain drugs and that these drugs or drug adducts could induce a semimature status in DCs, enabling them to induce a T-cell response. Moreover, a proinflammatory environment could enhance the formation of protein adducts in DCs [169, 170]. Not only drug–protein conjugates but also anticonvulsants or oxypurinol can stimulate phenotypic and functional changes in DCs. Activation of the p38 mitogen-activated protein kinase (MAPK) signaling pathway may be involved in drug-induced maturation of DCs [171].
3.5.2 Heterologous Immunity
A second hypothesis postulates that pre-existing memory T cells are responsible for the development of drug-induced hypersensitivity reactions.
Heterologous immunity refers to the phenomenon whereby a history of an immune response against one previously encountered pathogen can provide a level of immunity to another unrelated pathogen or graft. It is generally attributed to the generation of immunological cross-reactivity between viral epitopes and grafts or other antigens and can be mediated via memory CD8 + T cells. Heterologous immunity has been demonstrated for cytomegalovirus (CMV) and Epstein-Barr virus (EBV) and is mostly beneficial, mediating protective immunity. However, in some individuals, it may trigger a cascade of events that result in severe immunopathology [172].
As we have outlined, although the high NPV for certain HLA risk alleles indicates that the presence of a particular HLA allele may be necessary for the development of HLA-class I-restricted drug hypersensitivities, the low PPV indicates that the HLA allotype alone is not enough. The pathophysiological mechanism responsible for this “positive predictive gap” and the foundations of the variety of clinical phenotypes and tissue distribution of a given reaction remain unknown. In an attempt to fill this gap, a double HLA restriction-heterologous immunity model has been proposed. This model postulates that type IV T-cell-mediated drug hypersensitivity reactions may result from the cross-reaction between memory T cells developed during a previous immune response to a prevalent and persistent pathogen (likely a virus) and a new epitope that is created when the drug is present [173]. In this model, resident memory T cells could provide for the tissue specificity of clinical phenotypes [174]. The finding that abacavir-responsive and oxypurinol-responsive CD8 + T lymphocytes could be expanded from drug-naïve individuals [175, 176] and that these cells arise from both naïve and memory T-cell compartments, as well as long-lasting memory T-cell responses as assessed by skin patch tests and drug-specific proliferation assays, established the grounds for this theory.
3.6 Regulatory T Cells in SCARs
Tregs may play a critical role in maintaining self-tolerance and immune homeostasis. They are CD127-CD4 + T cells characterized by the high cell surface expression of CD25 and induced expression of the nuclear transcription factor FoxP3. Tetsuo Shiohara’s group first reported an expansion of Foxp3 + Tregs during acute DRESS as well as skin infiltration by Tregs [63]. The frequencies of FoxP3 + Tregs returned to the normal range after resolution of DRESS and were normal among CD4 + T cells in acute TEN cases. However, a functional Treg impairment was detected in acute TEN as well as in lymphocytes isolated from DRESS cases after resolution [63]. The lack of Treg function during acute TEN could lead to excessive activation of effector T cells. On the other hand, it has been speculated that expansions of Tregs during acute DRESS could explain the delayed onset of this clinical entity and that Treg skin infiltration in DRESS could limit epidermal damage by effector T cells [177].
Plasticity is a central feature of Tregs, which, depending on the cytokine microenvironment, can acquire different transcriptional profiles, including the possibility of differentiation into Th17 cells [178]. In fact, the balance and interplay between Th17 and Tregs is thought to play a major role in the regulation of immune homeostasis and inflammation [179]. Reciprocal contribution of Tregs and Th17 lymphocytes to SCARs has been suggested [95]. A recent report in patients with DRESS undergoing resolution of the disease found that as Treg frequencies decreased there was a parallel increase in the frequencies of Th17 lymphocytes. The authors also observed that the population of proinflammatory CD14 + CD16 + monocytes was severely reduced in acute DRESS and recovered after resolution. Moreover, the frequencies of CD16 + monocytes were inversely correlated with those of Tregs and positively correlated with those of Th17. As CD14 + CD16 + monocytes are major producers of IL-6, and IL-6 promotes the development of the Th17 phenotype in Tregs, the authors proposed that low IL-6 levels due to reduced frequencies of proinflammatory monocytes would be the mechanism leading to expansion of T regs during acute DRESS [180].
It is noteworthy that, although the frequencies of Foxp3 among CD4 + T cells were not altered in acute TEN, sustained lymphopenia affecting mainly the CD4 + population in patients [39, 40] would severely decrease the absolute numbers of circulating Tregs. In this sense, it has been proposed that the loss of skin-protective CD4 + CD25 + Tregs may contribute to an increased risk for developing SJS/TEN in HIV patients [181]. Along this line, results obtained from a transgenic mouse model analyzing abacavir-induced hypersensitivity strongly suggest that CD4 + T cells (which contain the Treg population) are key players in the induction of active tolerance to the new antigens induced by abacavir [182].
4 Mechanisms of Cell Death in SCARs: Apoptosis and Necroptosis
The full-thickness necrosis of all epidermal layers with dermoepidermal detachment is the pathognomonic characteristic of SJS/TEN. Early studies described that massive apoptosis of the keratinocytes was the cause of epidermal death [85, 183].
Current knowledge establishes two pathways eliciting apoptosis. The extrinsic pathway relies on the stimulation of death receptors by ligands, whereas the intrinsic pathway is triggered by disruption of the mitochondrial outer membrane. Both routes converge in the activation of caspase-3 and DNA degradation (Fig. 4).
Pathways of signaling for apoptotic cell death. The extrinsic pathway is initiated by the ligation of death receptors with their cognate ligands, such as FASL, TRAIL or TNF. As a consequence, an adaptor molecule (FADD) activates caspase-8. Activated caspase-8 can directly cleave and activate executioner caspases such as caspase-3, thus promoting apoptosis. The intrinsic pathway is modulated by the activation of proteins sensing different types of cell stress, and then activating BAX/BAK. These molecules then migrate to the mitochondria where they facilitate or induce the release of apoptogenic factors, such as cytochrome c to the cytosol. Cytochrome c associates with APAF-1 and pro-caspase-9 to form the apoptosome, resulting in the activation of caspase-9, which activates caspase-3, where both pathways interface. Granzyme B is released to the cytosol of target cells upon cytotoxic cell degranulation. It may directly activate caspase-3 or induce Bax activation. BCL2 family proteins are negative regulators of the intrinsic pathway. The human microRNA mir-18a-5p is a negative regulator of the expression of BCL2 family members such as BCL2L10. High levels of mir-18a-5p in SJS/TEN may favor apoptosis by releasing the negative regulation of the intrinsic pathway. CTL cytotoxic T lymphocyte, SJS Stevens–Johnson syndrome, TEN toxic epidermal necrolysis, TNFR tumor necrosis factor receptor
In SJS/TEN, two principal mechanisms have been proposed for the induction of keratinocyte apoptosis, namely Fas–FasL interactions and lymphocyte cytotoxicity.
Early reports suggested a pivotal role for Fas–FasL-induced “fratricide” keratinocyte apoptosis [87]. Moreover, it has been suggested that the proinflammatory cytokines TNF-α and IFN-γ indirectly upregulate membrane FasL expression in keratinocytes through the induction of inducible nitric oxide synthase (iNOS) [184]. As we have outlined, the role of Fas–FasL remains controversial. However, as explained in Sect. 3.1.3, additional ligands for death receptors such as TRAIL or TWEAK [108] have been identified in blister fluids from patients with SJS/TEN, which could induce apoptosis through the extrinsic pathway.
On the other hand, the cytotoxic killing of targets induced by degranulation of CTLs and NK cells also induces caspase-3 activation and apoptosis. There is ample evidence of the involvement of cytotoxic proteins such as perforin, granzymes and granulysin in the pathogenesis of SJS/TEN [122, 183, 185]. Granzymes are a family of serine proteases present in the cytotoxic granules of CTLs and NK cells. The formation of the immune synapse upon target cell recognition leads to the rapid delivery of cytotoxic granules to a precisely defined point between the effector and target. Granzyme B is a major constituent of CTL/NK granules and promotes apoptosis in humans either by direct cleavage of caspase-3 or by increasing the permeability of the mitochondrial outer membrane (intrinsic pathway) [186].
The intrinsic pathway of apoptosis is inhibited by BCL2 proteins. A recent report identified the microRNA (miRNA) mir-18a-5p as significantly upregulated in the skin of patients with SJS/TEN. Among the identified targets of this miRNA, BCL2L10 mRNA and protein expression levels were found to be downregulated in the skin of patients with SJS/TEN, supporting a role for mir-18a-5p in the pathogenesis of SJS/TEN through the release of control mechanisms for keratinocyte apoptosis [187].
Electron microscopy examination of morphological changes in active skin lesions of patients with SJS/TEN led to the recent observation of both apoptotic and necrotic cells in affected skin. Necrotic features were also observed in skin biopsies from erythematous areas with no epidermal detachment, suggesting that this is an early event leading to epidermal cell death. Supernatants from drug-stimulated PBMCs from patients with SJS/TEN reduced the viability of keratinocytes cultured in vitro in a necrostatin-1-dependent manner. The authors identified annexin A1 in the supernatants of drug-stimulated PBMCs and concluded that cell death in at least a fraction of keratinocytes in the epidermis of SJS/TEN cases occurred through programmed cell necrosis or necroptosis and that this process was initiated by annexin-1 binding to FPR1 expressed in keratinocytes [188].
Necroptosis is a form of programmed cell death that is activated by the “necrosome”, which consists of the kinases RIP1 and RIP3 and the pseudokinase MLKL. The activation of the necrosome induces phosphorylation of MLKL, which can then form aggregates that lead to the disruption of the cellular membrane and necrosis. Many proapoptotic stimuli or death ligands such as TNF-α or FasL may also induce necroptosis in conditions in which caspases are inactivated [189]. Necroptosis is also favored under conditions of RIP3 overexpression. Saito et al. [188] found high levels of RIP3 expression in the epidermis of patients with SJS/TEN. This finding was further confirmed [190] and phosphorylation of MLKL was detected in the affected epidermis, supporting the hypothesis of necroptosis as a cell death mechanism in SJS/TEN. Interestingly, it was recently discovered that RIP3 levels are regulated by PELI1, a protein that catalyzes the degradation of RIP3. The expression of PELI1 was extremely low in SJS/TEN-affected tissue compared with healthy skin biopsies [191], thus favoring necroptosis through the maintenance of high RIP3 epidermal levels (Fig. 5). Further research is needed to confirm these results and to analyze how the expression of PELI1 is regulated in keratinocytes.
Death receptors may induce necroptosis. Death receptor stimulation promotes the activation of caspase-8 by RIP1 via the adaptor protein FADD, and this leads to apoptosis. When caspases are inhibited, or in conditions where RIP3 is overexpressed, RIP1 can associate with RIP3 and MLKL. Upon activation, RIP3 phosphorylates MLKL, which promotes oligomerization and insertion into the plasma membrane to execute necroptosis. PELI1 is a negative regulator of RIP3 levels. In SJS/TEN, low levels of PELI1 expression in keratinocytes lead to RIP3 overexpression, allowing necroptosis. Activation of the receptor FPR1 upon binding to annexin A1 could also lead to keratinocyte death by necroptosis in SJS/TEN. SJS Stevens–Johnson syndrome, TEN toxic epidermal necrolysis
5 Other Non-Immune, Environmental and Genetic Factors Involved in SCARs
Some environmental factors, such as certain infectious agents, may cause or modulate the course of SCARs. As we have outlined, certain pathogens such as Mycoplasma pneumoniae, herpesviruses or enteroviruses may also induce mucocutaneous blistering diseases mediated by CTLs and NK cells. Reactivation of certain herpesviruses such as CMV may worsen the clinical course in DRESS [192] and HIV active infection is a risk factor for developing SCARs [193].
Drug metabolism and the patient’s underlying illnesses may also affect the clinical course of SCARs. In this sense, it has been shown that renal insufficiency or chronic kidney disease considerably impact the clearance of oxypurinol, leading to elevated plasma concentrations with subsequent worsening of the clinical course of allopurinol-induced SCARs [194]. Slow introduction of allopurinol may be beneficial to induce tolerance in at-risk patients [151].
The cytochrome P450 (CYP) enzymes metabolize endogenous and exogenous chemicals and are highly involved in drug metabolism. A recently published genome-wide association study (GWAS), including individuals from Taiwan, Japan, and Malaysia with phenytoin-related SCARs, identified 16 single nucleotide polymorphisms (SNPs) in the CYP2C gene, encoding a hepatic enzyme responsible for metabolizing phenytoin. The variant identified (CYP2C9*3) was strongly associated with the development of SCARs and reduced phenytoin clearance leading to high circulating concentrations [195]. Reduced phenytoin clearance was also found in patients not carrying this allele, which suggests that additional factors, such as liver or renal function, may also affect the development of phenytoin-induced SCARs.
Along this line, a genetic association related to the reduced clearance of nevirapine has been reported among carriers of allelic variants of CYP2B6 G516T and T983C, who are at higher risk for developing nevirapine-induced SJS/TEN, whereas the wild-type genotype for both SNPs showed a protective effect [196]. The null phenotype for glutathione transferase GSTM1 also showed a weak association with SJS/TEN susceptibility in patients treated with nevirapine [197].
A novel bioinformatics analysis of GWAS results revealed that the ABC transporter pathway was significantly enriched in genetic variants associated with SJS/TEN. The same study also identified genetic variants of the proteasome [198]. The proteasome complex pathway was identified not only in genetic variants but also in genes that were differentially expressed in blister fluid cells as assessed in a previous study by another group [97]. Proteasome-mediated protein degradation is implicated in generating the peptide repertoire to be presented in HLA molecules and plays an important role in T-cell proliferation, activation and apoptosis processes. Genetic variants of proteins involved in this pathway could affect the development of SJS/TEN in some patients.
6 Conclusions
Current data position HLA-I genes as the main susceptibility risk factors in SJS/TEN and DRESS and support a major role for CD8 + T cells as triggers of the disease in an HLA-I and drug-specific manner. In vitro development of drug-specific T-cell clones strongly supports this hypothesis. In this sense, and although traditionally type B ADR were claimed to be unpredictable and concentration-independent, at least for SCARs, the genetic associations allow for some predictability regarding at-risk patients, and studies on drug metabolism suggest that higher circulating levels may favor the development of hypersensitivity reactions.
NK cells, monocytes, macrophages, DCs, eosinophils and neutrophils might interact and cooperate with CTLs, Th1, Th17 and Tregs for the final phenotype. Several chemokines that may drive lymphocyte recruitment to the skin have been identified. Despite these advances, the ultimate reason for the diversity of clinical presentations and the pathogenic T-cell clones have yet to be identified, and little information is available regarding mechanisms of systemic inflammation affecting patients with DRESS, partly because of the complexity involved in analyzing tissue-specific immune responses in internal organs.
It is tempting to speculate that tissue-resident memory T-cell clones are triggered by certain drugs when the right allele is present and that phenotypic differences may reside in the available repertoire of cross-reactive T cells available and their respective specificities. Nevertheless, we must keep in mind that the final clinical presentation is likely the result of multiple events occurring in vivo and that several mechanisms may be at work, including current or past pathogen infections and physical conditions or genetic factors, leading to a higher availability of the culprit drug for its interaction with immune receptors. Accurate diagnosis and phenotyping are crucial to achieve consistent and reliable data.
Unanswered questions, such as the relevance of drug-specific immune tolerance mechanisms versus immune ignorance, and new activities discovered for old players, such as the cleavage of extracellular matrix proteins by granzyme B [199], deserve more attention. New or old drugs able to target soluble mediators of inflammation and apoptotic or necroptotic pathways could be explored for the treatment of SJS/TEN.
References
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000;356(9237):1255–9.
Rawlins MD, Thompson JW. Pathogenesis of adverse drug reactions. In: Davies DM, editor. Textbook of adverse drug reactions. Oxford: Oxford University Press; 1977. p. 10–31.
Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004;113(5):832–6.
Paulmann M, Mockenhaupt M. Severe drug-induced skin reactions: clinical features, diagnosis, etiology, and therapy. J Dtsch Dermatol Ges. 2015;13(7):625–45.
Bellón T, Cabañas R, González-Herrada C, Ramírez E, González-Ramos J, López San Martín M, et al. Approach to severe cutaneous adverse drug reactions. Curr Treat Options Allergy. 2017;4(2):201–21.
Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, et al. Comprehensive survival analysis of a cohort of patients with Stevens–Johnson syndrome and toxic epidermal necrolysis. J Investig Dermatol. 2013;133(5):1197–204.
Bellón T, Blanca M. The innate immune system in delayed cutaneous allergic reactions to medications. Curr Opin Allergy Clin Immunol. 2011;11(4):292–8.
Bellon T. Effector cells and downstream mediators in severe cutaneous adverse reactions. Curr Immunol Rev. 2014;10(1):24–32.
Sidoroff A, Dunant A, Viboud C, Halevy S, Bavinck JNB, Naldi L, et al. Risk factors for acute generalized exanthematous pustulosis (AGEP)-results of a multinational case-control study (EuroSCAR). Br J Dermatol. 2007;157(5):989–96.
Halevy S, Kardaun SH, Davidovici B, Wechsler J, EuroSCAR and RegiSCAR study group. The spectrum of histopathological features in acute generalized exanthematous pustulosis: a study of 102 cases. Br J Dermatol. 2010;163(6):1245–52.
De A, Das S, Sarda A, Pal D, Biswas P. Acute generalised exanthematous pustulosis: an update. Indian J Dermatol. 2018;63(1):22–9.
Britschgi M, Steiner UC, Schmid S, Depta JP, Senti G, Bircher A, et al. T-cell involvement in drug-induced acute generalized exanthematous pustulosis. J Clin Investig. 2001;107(11):1433–41.
Padial MA, Alvarez-Ferreira J, Tapia B, Blanco R, Mañas C, Blanca M, et al. Acute generalized exanthematous pustulosis associated with pseudoephedrine. Br J Dermatol. 2004;150(1):139–42.
Roujeau JC, Haddad C, Paulmann M, Mockenhaupt M. Management of nonimmediate hypersensitivity reactions to drugs. Immunol Allergy Clin N Am. 2014;34(3):473–87.
Mockenhaupt M. Epidemiology of cutaneous adverse drug reactions. Chem Immunol Allergy. 2012;97:1–17.
Saissi EH, Beau-Salinas F, Jonville-Béra AP, Lorette G, Autret-Leca E, Centres Régionaux de Pharmacovigilance. Drugs associated with acute generalized exanthematic pustulosis. Ann Dermatol Venereol. 2003;130(6–7):612–8.
Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996;15(4):250–7.
Walsh S, Diaz-Cano S, Higgins E, Morris-Jones R, Bashir S, Bernal W, et al. Drug reaction with eosinophilia and systemic symptoms: is cutaneous phenotype a prognostic marker for outcome? A review of clinicopathological features of 27 cases. Br J Dermatol. 2013;168(2):391–401.
Kano Y, Hiraharas K, Sakuma K, Shiohara T. Several herpesviruses can reactivate in a severe drug-induced multiorgan reaction in the same sequential order as in graft-versus-host disease. Br J Dermatol. 2006;155(2):301–6.
Shear NH, Spielberg SP. Anticonvulsant hypersensitivity syndrome. In vitro assessment of risk. J Clin Investig. 1988;82(6):1826–32.
Lupton GP, Odom RB. The allopurinol hypersensitivity syndrome. J Am Acad Dermatol. 1979;1(4):365–74.
Shiohara T, Kano Y. A complex interaction between drug allergy and viral infection. Clin Rev Allergy Immunol. 2007;33(1–2):124–33.
Kardaun SH, Sidoroff A, Valeyrie-Allanore L, Halevy S, Davidovici BB, Mockenhaupt M, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156(3):609–11.
Shiohara T, Iijima M, Ikezawa Z, Hashimoto K. The diagnosis of a DRESS syndrome has been sufficiently established on the basis of typical clinical features and viral reactivations. Br J Dermatol. 2007;156(5):1083–4.
Ishida T, Kano Y, Mizukawa Y, Shiohara T. The dynamics of herpesvirus reactivations during and after severe drug eruptions: their relation to the clinical phenotype and therapeutic outcome. Allergy. 2014;69(6):798–805.
Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124(7):588–97.
Kardaun SH, Sekula P, Valeyrie-Allanore L, Liss Y, Chu CY, Creamer D, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169(5):1071–80.
Peyriere H, Dereure O, Breton H, Demoly P, Cociglio M, Blayac J-P, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2006;155(2):422–8.
Shiohara T, Kano Y. Drug reaction with eosinophilia and systemic symptoms (DRESS): incidence, pathogenesis and management. Expert Opin Drug Saf. 2017;16(2):139–47.
Phillips E, Mallal S. Successful translation of pharmacogenetics into the clinic: the abacavir example. Mol Diagn Ther. 2009;13(1):1–9.
Fernando SL. Drug-reaction eosinophilia and systemic symptoms and drug-induced hypersensitivity syndrome. Australas J Dermatol. 2014;55(1):15–23.
Ortonne N, Valeyrie-Allanore L, Bastuji-Garin S, Wechsler J, de Feraudy S, Duong T-A, et al. Histopathology of drug rash with eosinophilia and systemic symptoms syndrome: a morphological and phenotypical study. Br J Dermatol. 2015;173(1):50–8.
Cho YT, Liau JY, Chang CY, Yang CW, Chen KL, Chen YC, et al. Co-existence of histopathological features is characteristic in drug reaction with eosinophilia and systemic symptoms and correlates with high grades of cutaneous abnormalities. J Eur Acad Dermatol Venereol. 2016;30(12):2077–84.
Shiohara T, Kano Y, Takahashi R, Ishida T, Mizukawa Y. Drug-induced hypersensitivity syndrome: recent advances in the diagnosis, pathogenesis and management. In: French LE, editor. Adverse cutaneous drug eruptions. Basel: Karger; 2012. p. 122–38.
George C, Sears A, Selim A-G, Walsh S, Creamer D. Systemic hypersensitivity reaction to Omnipaque radiocontrast medium: a case of mini-DRESS. Clin Case Rep. 2016;4(4):336–8.
Ortonne N. Is DRESS syndrome a single entity or within a spectrum of adverse reactions to drug? Br J Dermatol. 2016;175(6):1142–4.
Chen YC, Chiu HC, Chu CY. Drug reaction with eosinophilia and systemic symptoms. Arch Dermatol. 2010;146(12):1373–9.
Cho Y-T, Chu C-Y. Treatments for severe cutaneous adverse reactions. J Immunol Res. 2017. https://doi.org/10.1155/2017/1503709.
Roujeau JC, Moritz S, Guillaume JC, Bombal C, Revuz J, Weil B, et al. Lymphopenia and abnormal balance of T-lymphocyte subpopulations in toxic epidermal necrolysis. Arch Dermatol Res. 1985;277(1):24–7.
Correia O, Delgado L, Ramos JP, Resende C, Torrinha JA. Cutaneous T-cell recruitment in toxic epidermal necrolysis. Further evidence of CD8 + lymphocyte involvement. Arch Dermatol. 1993;129(4):466–8.
Morel E, Escamochero S, Cabañas R, Díaz R, Fiandor A, Bellón T. CD94/NKG2C is a killer effector molecule in patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Allergy Clin Immunol. 2010;125(3):703–10.
Bastuji-Garin S, Rzany B, Stern RS, Shear NH, Naldi L, Roujeau JC. Clinical classification of cases of toxic epidermal necrolysis, Stevens–Johnson syndrome, and erythema multiforme. Arch Dermatol. 1993;129(1):92–6.
Phillips EJ. New strategies to predict and prevent serious immunologically mediated adverse drug reactions. Trans Am Clin Climatol Assoc. 2018;129:74–87.
Le Cleach L, Delaire S, Boumsell L, Bagot M, Bourgault-Villada I, Bensussan A, et al. Blister fluid T lymphocytes during toxic epidermal necrolysis are functional cytotoxic cells which express human natural killer (NK) inhibitory receptors. Clin Exp Immunol. 2000;119(1):225–30.
Yang Y, Li F, Du J, Shen Y, Lin J, Zhu X, et al. Variable levels of apoptotic signal-associated cytokines in the disease course of patients with Stevens–Johnson syndrome and toxic epidermal necrolysis. Australas J Dermatol. 2017;58(3):e61–7.
Heng YK, Lee HY, Roujeau J-C. Epidermal necrolysis: 60 years of errors and advances. Br J Dermatol. 2015;173(5):1250–4.
Hoetzenecker W, Nägeli M, Mehra ET, Jensen AN, Saulite I, Schmid-Grendelmeier P, et al. Adverse cutaneous drug eruptions: current understanding. Semin Immunopathol. 2016;38(1):75–86.
Dodiuk-Gad RP, Chung W-H, Valeyrie-Allanore L, Shear NH. Stevens–Johnson syndrome and toxic epidermal necrolysis: an update. Am J Clin Dermatol. 2015;16(6):475–93.
Sassolas B, Haddad C, Mockenhaupt M, Dunant A, Liss Y, Bork K, et al. ALDEN, an algorithm for assessment of drug causality in Stevens–Johnson Syndrome and toxic epidermal necrolysis: comparison with case-control analysis. Clin Pharmacol Ther. 2010;88(1):60–8.
Olson D, Watkins LKF, Demirjian A, Lin X, Robinson CC, Pretty K, et al. Outbreak of Mycoplasma pneumoniae-associated Stevens–Johnson syndrome. Pediatrics. 2015;136(2):e386–94.
Fournier S, Bastuji-Garin S, Mentec H, Revuz J, Roujeau JC. Toxic epidermal necrolysis associated with Mycoplasma pneumoniae infection. Eur J Clin Microbiol Infect Dis. 1995;14(6):558–9.
Chung WH, Shih SR, Chang CF, Lin TY, Huang YC, Chang SC, et al. Clinicopathologic analysis of coxsackievirus a6 new variant induced widespread mucocutaneous bullous reactions mimicking severe cutaneous adverse reactions. J Infect Dis. 2013;208(12):1968–78.
Hsu DY, Brieva J, Silverberg NB, Silverberg JI. Morbidity and mortality of Stevens–Johnson syndrome and toxic epidermal necrolysis in United States adults. J Investig Dermatol. 2016;136(7):1387–97.
Mittmann N, Knowles SR, Koo M, Shear NH, Rachlis A, Rourke SB. Incidence of toxic epidermal necrolysis and Stevens–Johnson syndrome in an HIV cohort. Am J Clin Dermatol. 2012;13(1):49–54.
Palmares J, Correia O, Delgado L, Vazsilva M, Mesquita-Guimaraes J, Castro-Correia J. Ocular involvement in toxic epidermal necrolysis. Ocul Immunol Inflamm. 1993;1(1–2):171–8.
Schwartz RA, McDonough PH, Lee BW. Toxic epidermal necrolysis: part II. Prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. J Am Acad Dermatol. 2013;69(2):187–216.
Yang CW, Cho YT, Chen KL, Chen YC, Song HL, Chu CY. Long-term sequelae of Stevens–Johnson syndrome/toxic epidermal necrolysis. Acta Dermato Venereol. 2016;96(4):525–9.
Coombs R, Gell P. Classification of allergic reactions responsible for drug hypersensitivity reactions. In: Coombs RRA, Gells PGH, editors. Clinical aspects of immunology. Oxford: Blackwell Scientific Publications, Ltd; 1968. p. 575–96.
Pichler WJ. Delayed drug hypersensitivity reactions. Ann Intern Med. 2003;139(8):683–93.
Pichler WJ. Drug hypersensitivity reactions: classification and relationship to T-cell activation. In: Pichler WJ, editor. Drug hypersensitivity. Basel: Karger; 2007. p. 168–89.
Redwood AJ, Pavlos RK, White KD, Phillips EJ. HLAs: key regulators of T-cell-mediated drug hypersensitivity. HLA. 2018;91(1):3–16.
Nassif A, Moslehi H, Le Gouvello S, Bagot M, Lyonnet L, Michel L, et al. Evaluation of the potential role of cytokines in toxic epidermal necrolysis. J Investig Dermatol. 2004;123(5):850–5.
Takahashi R, Kano Y, Yamazaki Y, Kimishima M, Mizukawa Y, Shiohara T. Defective regulatory T cells in patients with severe drug eruptions: timing of the dysfunction is associated with the pathological phenotype and outcome. J Immunol. 2009;182(12):8071–9.
Britschgi M, Pichler WJ. Acute generalized exanthematous pustulosis, a clue to neutrophil-mediated inflammatory processes orchestrated by T cells. Curr Opin Allergy Clin Immunol. 2002;2(4):325–31.
Schaerli P, Britschgi M, Keller M, Steiner UC, Steinmann LS, Moser B, et al. Characterization of human T cells that regulate neutrophilic skin inflammation. J Immunol. 2004;173(3):2151–8.
Keller M, Spanou Z, Schaerli P, Britschgi M, Yawalkar N, Seitz M, et al. T cell-regulated neutrophilic inflammation in autoinflammatory diseases. J Immunol. 2005;175(11):7678–86.
Kabashima R, Sugita K, Sawada Y, Hino R, Nakamura M, Tokura Y. Increased circulating Th17 frequencies and serum IL-22 levels in patients with acute generalized exanthematous pustulosis. J Eur Acad Dermatol Venereol. 2011;25(4):485–8.
Kakeda M, Schlapbach C, Danelon G, Tang MM, Cecchinato V, Yawalkar N, et al. Innate immune cells express IL-17A/F in acute generalized exanthematous pustulosis and generalized pustular psoriasis. Arch Dermatol Res. 2014;306(10):933–8.
Teunissen MBM, Bos JD, Koomen CW, de Waal Malefyt R, Wierenga EA. Interleukin-17 and interferon-γ synergize in the enhancement of proinflammatory cytokine production by human keratinocytes. J Investig Dermatol. 1998;111(4):645–9.
Albanesi C, Cavani A, Girolomoni G. IL-17 is produced by nickel-specific T lymphocytes and regulates ICAM-1 expression and chemokine production in human keratinocytes: synergistic or antagonist effects with IFN-gamma and TNF-alpha. J Immunol. 1999;162(1):494–502.
Romagnani S, Maggi E, Liotta F, Cosmi L, Annunziato F. Properties and origin of human Th17 cells. Mol Immunol. 2009;47(1):3–7.
Navarini AA, Valeyrie-Allanore L, Setta-Kaffetzi N, Barker JN, Capon F, Creamer D, et al. Rare variations in IL36RN in severe adverse drug reactions manifesting as acute generalized exanthematous pustulosis. J Investig Dermatol. 2013;133(7):1904–7.
Song HS, Kim SJ, Park T-I, Jang YH, Lee E-S. Immunohistochemical comparison of IL-36 and the IL-23/Th17 axis of generalized pustular psoriasis and acute generalized exanthematous pustulosis. Ann Dermatol. 2016;28(4):451–6.
Meier-Schiesser B, Feldmeyer L, Jankovic D, Mellett M, Satoh TK, Yerly D, et al. Culprit drugs induce specific IL-36 overexpression in acute generalized exanthematous pustulosis. J Investig Dermatol. 2018;139(4):848–58.
Mennicke M, Zawodniak A, Keller M, Wilkens L, Yawalkar N, Stickel F, et al. Fulminant liver failure after vancomycin in a sulfasalazine-induced DRESS syndrome: fatal recurrence after liver transplantation. Am J Transplant. 2009;9(9):2197–202.
Kitcharoensakkul M, Ree N, Bloomberg GR, Dehner LP, Heidingsfelder JA, White AJ, et al. Vancomycin-induced DRESS with evidence of T-cell activation in a 22-month-old patient. Ann Allergy Asthma Immunol. 2012;109(4):280–1.
An J, Lee JH, Lee H, Yu E, Lee DB, Shim JH, et al. Drug rash with eosinophilia and systemic symptoms syndrome following cholestatic hepatitis A: a case report. Korean J Hepatol. 2012;18(1):84–8.
Choquet-Kastylevsky G, Intrator L, Chenal C, Bocquet H, Revuz J, Roujeau JC. Increased levels of interleukin 5 are associated with the generation of eosinophilia in drug-induced hypersensitivity syndrome. Br J Dermatol. 1998;139(6):1026–32.
Ogawa K, Morito H, Hasegawa A, Daikoku N, Miyagawa F, Okazaki A, et al. Identification of thymus and activation-regulated chemokine (TARC/CCL17) as a potential marker for early indication of disease and prediction of disease activity in drug-induced hypersensitivity syndrome (DIHS)/drug rash with eosinophilia and systemic symptoms (DRESS). J Dermatol Sci. 2013;69(1):38–43.
Ange N, Alley S, Fernando SL, Coyle L, Yun J. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) syndrome successfully treated with mepolizumab. J Allergy Clin Immunol Pract. 2018;6(3):1059–60.
Teraki Y, Fukuda T. Skin-homing IL-13-producing T cells expand in the circulation of patients with drug rash with eosinophilia and systemic symptoms. Dermatology. 2017;233(2–3):242–9.
Ogawa K, Morito H, Hasegawa A, Miyagawa F, Kobayashi N, Watanabe H, et al. Elevated serum thymus and activation-regulated chemokine (TARC/CCL17) relates to reactivation of human herpesvirus 6 in drug reaction with eosinophilia and systemic symptoms (DRESS)/drug-induced hypersensitivity syndrome (DIHS). Br J Dermatol. 2014;171(2):425–7.
Picard D, Janela B, Descamps V, D’Incan M, Courville P, Jacquot S, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): a multiorgan antiviral T cell response. Sci Transl Med. 2010;2(46):46ra62.
Tsai YG, Liou JH, Hung SI, Chen CB, Chiu TM, Wang CW, et al. Increased type 2 innate lymphoid cells in patients with drug reaction with eosinophilia and systemic symptom. J Investig Dermatol. 2019;78:98. https://doi.org/10.1016/j.jid.2018.10.048.
Paul C, Wolkenstein P, Adle H, Wechsler J, Garchon HJ, Revuz J, et al. Apoptosis as a mechanism of keratinocyte death in toxic epidermal necrolysis. Br J Dermatol. 1996;134(4):710–4.
Nassif A, Bensussan A, Dorothée G, Mami-Chouaib F, Bachot N, Bagot M, et al. Drug specific cytotoxic T-cells in the skin lesions of a patient with toxic epidermal necrolysis. J Investig Dermatol. 2002;118(4):728–33.
Viard I, Wehrli P, Bullani R, Schneider P, Holler N, Salomon D, et al. Inhibition of toxic epidermal necrolysis by blockade of CD95 with human intravenous immunoglobulin. Science. 1998;282(5388):490–3.
Paquet P, Piérard GE. Soluble fractions of tumor necrosis factor-alpha, interleukin-6 and of their receptors in toxic epidermal necrolysis: a comparison with second-degree burns. Int J Mol Med. 1998;1(2):459–62.
Correia O, Delgado L, Barbosa IL, Campilho F, Fleming-Torrinha J. Increased interleukin 10, tumor necrosis factor alpha, and interleukin 6 levels in blister fluid of toxic epidermal necrolysis. J Am Acad Dermatol. 2002;47(1):58–62.
Cho YT, Lin JW, Chen YC, Chang CY, Hsiao CH, Chung WH, et al. Generalized bullous fixed drug eruption is distinct from Stevens–Johnson syndrome/toxic epidermal necrolysis by immunohistopathological features. J Am Acad Dermatol. 2014;70(3):539–48.
Chang HY, Cooper ZA, Swetter SM, Marinkovich MP. Kinetics and specificity of Fas ligand induction in toxic epidermal necrolysis. Arch Dermatol. 2004;140(2):242–4.
Abe R, Shimizu T, Shibaki A, Nakamura H, Watanabe H, Shimizu H. Toxic epidermal necrolysis and Stevens–Johnson syndrome are induced by soluble Fas ligand. Am J Pathol. 2003;162(5):1515–20.
O’Reilly LA, Tai L, Lee L, Kruse EA, Grabow S, Fairlie WD, et al. Membrane-bound Fas ligand only is essential for Fas-induced apoptosis. Nature. 2009;461(7264):659–63.
Lotti R, Shu E, Petrachi T, Marconi A, Palazzo E, Quadri M, et al. Soluble Fas ligand is essential for blister formation in pemphigus. Front Immunol. 2018. https://doi.org/10.3389/fimmu.2018.00370.
Hashizume H, Fujiyama T, Tokura Y. Reciprocal contribution of Th17 and regulatory T cells in severe drug allergy. J Dermatol Sci. 2016;81(2):131–4.
Teraki Y, Kawabe M, Izaki S. Possible role of TH17 cells in the pathogenesis of Stevens–Johnson syndrome and toxic epidermal necrolysis. J Allergy Clin Immunol. 2013;131(3):907–9.
Chung WH, Hung SI, Yang JY, Su SC, Huang SP, Wei CY, et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens–Johnson syndrome and toxic epidermal necrolysis. Nat Med. 2008;14(12):1343–50.
Schlapbach C, Zawodniak A, Irla N, Adam J, Hunger RE, Yerly D, et al. NKp46 + cells express granulysin in multiple cutaneous adverse drug reactions. Allergy. 2011;66(11):1469–76.
Lanier LL. NK cell recognition. Annu Rev Immunol. 2005;23(1):225–74.
Su SC, Mockenhaupt M, Wolkenstein P, Dunant A, Le Gouvello S, Chen CB, et al. Interleukin-15 is associated with severity and mortality in Stevens–Johnson syndrome/toxic epidermal necrolysis. J Investig Dermatol. 2017;137(5):1065–73.
Sekula P, Liss Y, Davidovici B, Dunant A, Roujeau J-C, Kardaun S, et al. Evaluation of SCORTEN on a cohort of patients with Stevens–Johnson syndrome and toxic epidermal necrolysis included in the RegiSCAR study. J Burn Care Res. 2011;32(2):237–45.
Castillo EF, Schluns KS. Regulating the immune system via IL-15 transpresentation. Cytokine. 2012;59(3):479–90.
Clayberger C, Krensky AM. Granulysin. Curr Opin Immunol. 2003;15(5):560–5.
Stern RS, Divito SJ. Stevens–Johnson syndrome and toxic epidermal necrolysis: associations, outcomes, and pathobiology—thirty years of progress but still much to be done. J Investig Dermatol. 2017;137(5):1004–8.
Ueta M, Sawai H, Sotozono C, Hitomi Y, Kaniwa N, Kim MK, et al. IKZF1, a new susceptibility gene for cold medicine–related Stevens–Johnson syndrome/toxic epidermal necrolysis with severe mucosal involvement. J Allergy Clin Immunol. 2015;135(6):1538–45.
Tapia B, Padial A, Sánchez-Sabaté E, Alvarez-Ferreira J, Morel E, Blanca M, et al. Involvement of CCL27-CCR106 interactions in drug-induced cutaneous reactions. J Allergy Clin Immunol. 2004;114(2):335–40.
Tohyama M, Watanabe H, Murakami S, Shirakata Y, Sayama K, Iijima M, et al. Possible involvement of CD14 + CD16 + monocyte lineage cells in the epidermal damage of Stevens–Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2012;166(2):322–30.
de Araujo E, Dessirier V, Laprée G, Valeyrie-Allanore L, Ortonne N, Stathopoulos EN, et al. Death ligand TRAIL, secreted by CD1a + and CD14 + cells in blister fluids, is involved in killing keratinocytes in toxic epidermal necrolysis. Exp Dermatol. 2011;20(2):107–12.
Wang CW, Yang LY, Chen CB, Ho HC, Hung SI, Yang CH, et al. Randomized, controlled trial of TNF-α antagonist in CTL-mediated severe cutaneous adverse reactions. J Clin Investig. 2018;128(3):985–96.
Bellón T, Alvarez L, Mayorga C, Morel E, Torres MJ, Martín-Díaz MA, et al. Differential gene expression in drug hypersensitivity reactions: induction of alarmins in severe bullous diseases. Br J Dermatol. 2010;162(5):1014–22.
Paquet P, Nusgens BV, Piérard GE, Lapière CM. Gelatinases in drug-induced toxic epidermal necrolysis. Eur J Clin Investig. 1998;28(7):528–32.
Gaultier F, Ejeil A-L, Igondjo-Tchen S, Dohan D, Dridi SM, Maman L, et al. Possible involvement of gelatinase A (MMP2) and gelatinase B (MMP9) in toxic epidermal necrolysis or Stevens–Johnson syndrome. Arch Dermatol Res. 2004;296(5):220–5.
Arafat SN, Suelves AM, Spurr-Michaud S, Chodosh J, Foster CS, Dohlman CH, et al. Neutrophil collagenase, gelatinase, and myeloperoxidase in tears of patients with Stevens–Johnson syndrome and ocular cicatricial pemphigoid. Ophthalmology. 2014;121(1):79–87.
Piccinini AM, Midwood KS. DAMPening inflammation by modulating TLR signalling. Mediators Inflamm. 2010. https://doi.org/10.1155/2010/672395.
Yang D, Han Z, Oppenheim JJ. Alarmins and immunity. Immunol Rev. 2017;280(1):41–56.
Paquet P, Piérard GE. Epidermal calprotectin in drug-induced toxic epidermal necrolysis. J Cutan Pathol. 1999;26(6):301–5.
Paquet P, Piérard GE. Keratinocyte injury in drug-induced toxic epidermal necrolysis: simultaneous but distinct topographic expression of CD95R and calprotectin. Int J Mol Med. 2002;10(2):145–7.
Morel E, Alvarez L, Cabañas R, Fiandor A, Díaz R, Escamochero S, et al. Expression of α-defensin 1-3 in T cells from severe cutaneous drug-induced hypersensitivity reactions. Allergy. 2011;66(3):360–7.
Ganz T. Defensins: antimicrobial peptides of innate immunity. Nat Rev Immunol. 2003;3(9):710–20.
Lehrer RI, Lu W. α-Defensins in human innate immunity. Immunol Rev. 2012;245(1):84–112.
Tewary P, Yang D, de la Rosa G, Li Y, Finn MW, Krensky AM, et al. Granulysin activates antigen-presenting cells through TLR4 and acts as an immune alarmin. Blood. 2010;116(18):3465–74.
Deng A, Chen S, Li Q, Lyu S-C, Clayberger C, Krensky AM. Granulysin, a cytolytic molecule, is also a chemoattractant and proinflammatory activator. J Immunol. 2005;174(9):5243–8.
Hashizume H, Fujiyama T, Kanebayashi J, Kito Y, Hata M, Yagi H. Skin recruitment of monomyeloid precursors involves human herpesvirus-6 reactivation in drug allergy. Allergy. 2013;68(5):681–9.
Fujita H, Matsukura S, Watanabe T, Komitsu N, Watanabe Y, Takahashi Y, et al. The serum level of HMGB1 (high mobility group box 1 protein) is preferentially high in drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms. Br J Dermatol. 2014;171(6):1585–8.
Adachi A, Komine M, Tsuda H, Nakajima S, Kabashima K, Ohtsuki M. Differential expression of alarmins: IL-33 as a candidate marker for early diagnosis of toxic epidermal necrolysis. J Allergy Clin Immunol Pract. 2019;7(1):325–7.
Carr DF, Chung W-H, Jenkiins RE, Chaponda M, Nwikue G, Cornejo Castro EM, et al. 7th drug hypersensitivity meeting: part one. Clin Transl Allergy. 2016;6(S3):31.
Nakajima S, Watanabe H, Tohyama M, Sugita K, Iijima M, Hashimoto K, et al. High-mobility group box 1 protein (HMGB1) as a novel diagnostic tool for toxic epidermal necrolysis and Stevens–Johnson syndrome. Arch Dermatol. 2011;147(9):1110–2.
Carr DF, Wang C-W, Bellón T, Ressel L, Nwikue G, Shrivastava V, et al. Serum and blister-fluid elevation and decreased epidermal content of HMGB1 protein in drug-induced Stevens–Johnson syndrome/toxic epidermal necrolysis. Br J Dermatol. 2019. https://doi.org/10.1111/bjd.17610.
Roujeau JC, Huynh TN, Bracq C, Guillaume JC, Revuz J, Touraine R. Genetic susceptibility to toxic epidermal necrolysis. Arch Dermatol. 1987;123(9):1171–3.
Pellicano R, Silvestris A, Iannantuono M, Ciavarella G, Lomuto M. Familial occurrence of fixed drug eruptions. Acta Derm Venereol. 1992;72(4):292–3.
Melsom RD. Familial hypersensitivity to allopurinol with subsequent desensitization. Rheumatology (Oxford). 1999;38(12):1301.
Mallal S, Nolan D, Witt C, Masel G, Martin AM, Moore C, et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet. 2002;359(9308):727–32.
Hetherington S, Hughes AR, Mosteller M, Shortino D, Baker KL, Spreen W, et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet. 2002;359(9312):1121–2.
Chung WH, Hung SI, Hong HS, Hsih MS, Yang LC, Ho HC, et al. A marker for Stevens–Johnson syndrome. Nature. 2004;428(6982):486.
Hung SI, Chung WH, Liou LB, Chu CC, Lin M, Huang HP, et al. HLA-B*5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinol. Proc Natl Acad Sci USA. 2005;102(11):4134–9.
White KD, Abe R, Ardern-Jones M, Beachkofsky T, Bouchard C, Carleton B, et al. SJS/TEN 2017: building multidisciplinary networks to drive science and translation. J Allergy Clin Immunol Pract. 2018;6(1):38–69.
Sousa-Pinto B, Correia C, Gomes L, Gil-Mata S, Araújo L, Correia O, et al. HLA and delayed drug-induced hypersensitivity. Int Arch Allergy Immunol. 2016;170(3):163–79.
Chen CB, Abe R, Pan RY, Wang CW, Hung SI, Tsai YG, et al. An updated review of the molecular mechanisms in drug hypersensitivity. J Immunol Res. 2018. https://doi.org/10.1155/2018/6431694.
Phillips EJ. Defining regional differences in drug-induced Stevens–Johnson syndrome/toxic epidermal necrolysis: a tool to improve drug safety? Clin Pharmacol Ther. 2019;105(1):22–5.
Sousa-Pinto B, Pinto-Ramos J, Correia C, Gonçalves-Costa G, Gomes L, Gil-Mata S, et al. Pharmacogenetics of abacavir hypersensitivity: a systematic review and meta-analysis of the association with HLA-B*57:01. J Allergy Clin Immunol. 2015;136(4):1092–4.
McCormack M, Alfirevic A, Bourgeois S, Farrell JJ, Kasperavičiūtė D, Carrington M, et al. HLA-A*3101 and carbamazepine-induced hypersensitivity reactions in europeans. N Engl J Med. 2011;364(12):1134–43.
Genin E, Chen D-P, Hung S-I, Sekula P, Schumacher M, Chang P-Y, et al. HLA-A*31:01 and different types of carbamazepine-induced severe cutaneous adverse reactions: an international study and meta-analysis. Pharmacogenom J. 2014;14(3):281–8.
Hung SI, Chung WH, Jee SH, Chen WC, Chang YT, Lee WR, et al. Genetic susceptibility to carbamazepine-induced cutaneous adverse drug reactions. Pharmacogenet Genom. 2006;16(4):297–306.
Ramírez E, Bellón T, Tong HY, Borobia AM, de Abajo FJ, Lerma V, et al. Significant HLA class I type associations with aromatic antiepileptic drug (AED)-induced SJS/TEN are different from those found for the same AED-induced DRESS in the Spanish population. Pharmacol Res. 2017;115:168–78.
Lonjou C, Borot N, Sekula P, Ledger N, Thomas L, Halevy S, et al. A European study of HLA-B in Stevens–Johnson syndrome and toxic epidermal necrolysis related to five high-risk drugs. Pharmacogenet Genom. 2008;18(2):99–107.
Shirzadi M, Thorstensen K, Helde G, Moen T, Brodtkorb E. Do HLA-A markers predict skin-reactions from aromatic antiepileptic drugs in a Norwegian population? A case control study. Epilepsy Res. 2015;118:5–9.
Moon J, Park H-K, Chu K, Sunwoo J-S, Byun J-I, Lim J-A, et al. The HLA-A*2402/Cw*0102 haplotype is associated with lamotrigine-induced maculopapular eruption in the Korean population. Epilepsia. 2015;56(10):e161–7.
Zhang F-R, Liu H, Irwanto A, Fu X-A, Li Y, Yu G-Q, et al. HLA-B*13:01 and the dapsone hypersensitivity syndrome. N Engl J Med. 2013;369(17):1620–8.
Tangamornsuksan W, Lohitnavy M. Association between HLA-B*5901 and methazolamide-induced Stevens–Johnson syndrome/toxic epidermal necrolysis: a systematic review and meta-analysis. Pharmacogenom J. 2018. https://doi.org/10.1038/s41397-018-0052-2.
Konvinse KC, Trubiano JA, Pavlos R, James I, Shaffer CM, Bejan CA, et al. HLA-A*32:01 is strongly associated with vancomycin-induced drug reaction with eosinophilia and systemic symptoms. J Allergy Clin Immunol. 2019. https://doi.org/10.1016/j.jaci.2019.01.045.
Jung J-W, Kim D-K, Park H-W, Oh K-H, Joo K-W, Kim Y-S, et al. An effective strategy to prevent allopurinol-induced hypersensitivity by HLA typing. Genet Med. 2015;17(10):807–14.
White KD, Chung WH, Hung SI, Mallal S, Phillips EJ. Evolving models of the immunopathogenesis of T cell-mediated drug allergy: the role of host, pathogens, and drug response. J Allergy Clin Immunol. 2015;136(2):219–34.
Chen P, Lin J-J, Lu C-S, Ong C-T, Hsieh PF, Yang C-C, et al. Carbamazepine-induced toxic effects and HLA-B*1502 screening in Taiwan. N Engl J Med. 2011;364(12):1126–33.
Venturi V, Price DA, Douek DC, Davenport MP. The molecular basis for public T-cell responses? Nat Rev Immunol. 2008;8(3):231–8.
Pichler WJ, Adam J, Watkins S, Wuillemin N, Yun J, Yerly D. Drug hypersensitivity: how drugs stimulate T cells via pharmacological interaction with immune receptors. Int Arch Allergy Immunol. 2015;168(1):13–24.
Illing PT, Vivian JP, Dudek NL, Kostenko L, Chen Z, Bharadwaj M, et al. Immune self-reactivity triggered by drug-modified HLA-peptide repertoire. Nature. 2012;486(7404):554–8.
Norcross MA, Luo S, Lu L, Boyne MT, Gomarteli M, Rennels AD, et al. Abacavir induces loading of novel self-peptides into HLA-B*57: 01: an autoimmune model for HLA-associated drug hypersensitivity. AIDS. 2012;26(11):F21–9.
Ostrov DA, Grant BJ, Pompeu YA, Sidney J, Harndahl M, Southwood S, et al. Drug hypersensitivity caused by alteration of the MHC-presented self-peptide repertoire. Proc Natl Acad Sci USA. 2012;109(25):9959–64.
Illing PT, Vivian JP, Purcell AW, Rossjohn J, McCluskey J. Human leukocyte antigen-associated drug hypersensitivity. Curr Opin Immunol. 2013;25(1):81–9.
Wei CY, Chung WH, Huang HW, Chen YT, Hung SI. Direct interaction between HLA-B and carbamazepine activates T cells in patients with Stevens–Johnson syndrome. J Allergy Clin Immunol. 2012;129(6):1562–9.
Ko TM, Chung WH, Wei CY, Shih HY, Chen JK, Lin CH, et al. Shared and restricted T-cell receptor use is crucial for carbamazepine-induced Stevens–Johnson syndrome. J Allergy Clin Immunol. 2011;128(6):1266–76.
Lichtenfels M, Farrell J, Ogese MO, Bell CC, Eckle S, McCluskey J, et al. HLA restriction of carbamazepine-specific T-cell clones from an HLA-A*31:01-positive hypersensitive patient. Chem Res Toxicol. 2014;27(2):175–7.
Yun J, Mattsson J, Schnyder K, Fontana S, Largiadèr CR, Pichler WJ, et al. Allopurinol hypersensitivity is primarily mediated by dose-dependent oxypurinol-specific T cell response. Clin Exp Allergy. 2013;43(11):1246–55.
Yun J, Marcaida MJ, Eriksson KK, Jamin H, Fontana S, Pichler WJ, et al. Oxypurinol directly and immediately activates the drug-specific T cells via the preferential use of HLA-B*58:01. J Immunol. 2014;192(7):2984–93.
Chung WH, Pan RY, Chu MT, Chin SW, Huang YL, Wang WC, et al. Oxypurinol-specific T cells possess preferential TCR clonotypes and express granulysin in allopurinol-induced severe cutaneous adverse reactions. J Investig Dermatol. 2015;135(9):2237–48.
Chen WT, Wang CW, Lu CW, Chen CB, Lee HE, Hung SI, et al. The function of HLA-B*13:01 involved in the pathomechanism of dapsone-induced severe cutaneous adverse reactions. J Investig Dermatol. 2018;138(7):1546–54.
Zhao Q, Alhilali K, Alzahrani A, Almutairi M, Amjad J, Liu H, et al. Dapsone- and nitroso dapsone-specific activation of T-cells from hypersensitive patients expressing the risk allele HLA-B*13:01. Allergy. 2019. https://doi.org/10.1111/all.13769.
Illing PT, Mifsud NA, Purcell AW. Allotype specific interactions of drugs and HLA molecules in hypersensitivity reactions. Curr Opin Immunol. 2016;42:31–40.
Rodriguez-Pena R, Lopez S, Mayorga C, Antunez C, Fernandez TD, Torres MJ, et al. Potential involvement of dendritic cells in delayed-type hypersensitivity reactions to β-lactams. J Allergy Clin Immunol. 2006;118(4):949–56.
Lavergne SN, Wang H, Callan HE, Park BK, Naisbitt DJ. “Danger” conditions increase sulfamethoxazole-protein adduct formation in human antigen-presenting cells. J Pharmacol Exp Ther. 2009;331(2):372–81.
Gonçalo M, Martins J, Silva A, Neves B, Figueiredo A, Cruz T, et al. Systemic drugs inducing non-immediate cutaneous adverse reactions and contact sensitizers evoke similar responses in THP-1 cells. J Appl Toxicol. 2015;35(4):398–406.
Welsh RM, Selin LK. No one is naive: the significance of heterologous T-cell immunity. Nat Rev Immunol. 2002;2(6):417–26.
Pavlos R, White KD, Wanjalla C, Mallal SA, Phillips EJ. Severe delayed drug reactions: role of genetics and viral infections. Immunol Allergy Clin N Am. 2017;37(4):785–815.
Pavlos R, Mallal S, Ostrov D, Pompeu Y, Phillips E. Fever, rash, and systemic symptoms: understanding the role of virus and HLA in severe cutaneous drug allergy. J Allergy Clin Immunol Pract. 2014;2(1):21–33.
Lucas A, Lucas M, Strhyn A, Keane NM, McKinnon E, Pavlos R, et al. Abacavir-reactive memory T cells are present in drug naïve individuals. PLoS One. 2015. https://doi.org/10.1371/journal.pone.0117160.
Adam J, Wuillemin N, Watkins S, Jamin H, Eriksson KK, Villiger P, et al. Abacavir induced T cell reactivity from drug naïve individuals shares features of allo-immune responses. PLoS One. 2014. https://doi.org/10.1371/journal.pone.0095339.
Shiohara T, Ushigome Y, Kano Y, Takahashi R. Crucial role of viral reactivation in the development of severe drug eruptions: a comprehensive review. Clin Rev Allergy Immunol. 2015;49(2):192–202.
Omenetti S, Pizarro TT. The Treg/Th17 axis: a dynamic balance regulated by the gut microbiome. Front Immunol. 2015. https://doi.org/10.3389/fimmu.2015.00639.
Chen X, Oppenheim JJ. Th17 cells and T regs: unlikely allies. J Leukoc Biol. 2014;95(5):723–31.
Ushigome Y, Mizukawa Y, Kimishima M, Yamazaki Y, Takahashi R, Kano Y, et al. Monocytes are involved in the balance between regulatory T cells and Th17 cells in severe drug eruptions. Clin Exp Allergy. 2018;48(11):1453–63.
Yang C, Mosam A, Mankahla A, Dlova N, Saavedra A. HIV infection predisposes skin to toxic epidermal necrolysis via depletion of skin-directed CD4 + T cells. J Am Acad Dermatol. 2014;70(6):1096–102.
Cardone M, Garcia K, Tilahun ME, Boyd LF, Gebreyohannes S, Yano M, et al. A transgenic mouse model for HLA-B*57:01–linked abacavir drug tolerance and reactivity. J Clin Investig. 2018;128(7):2819–32.
Inachi S, Mizutani H, Shimizu M. Epidermal apoptotic cell death in erythema multiforme and Stevens–Johnson syndrome. Contribution of perforin-positive cell infiltration. Arch Dermatol. 1997;133(7):845–9.
Viard-Leveugle I, Gaide O, Jankovic D, Feldmeyer L, Kerl K, Pickard C, et al. TNF-α and IFN-γ are potential inducers of Fas-mediated keratinocyte apoptosis through activation of inducible nitric oxide synthase in toxic epidermal necrolysis. J Investig Dermatol. 2013;133(2):489–98.
Nassif A, Bensussan A, Boumsell L, Deniaud A, Moslehi H, Wolkenstein P, et al. Toxic epidermal necrolysis: effector cells are drug-specific cytotoxic T cells. J Allergy Clin Immunol. 2004;114(5):1209–15.
Ewen CL, Kane KP, Bleackley RC. A quarter century of granzymes. Cell Death Differ. 2012;19(1):28–35.
Ichihara A, Wang Z, Jinnin M, Izuno Y, Shimozono N, Yamane K, et al. Upregulation of miR-18a-5p contributes to epidermal necrolysis in severe drug eruptions. J Allergy Clin Immunol. 2014;133(4):1065–74.
Saito N, Qiao H, Yanagi T, Shinkuma S, Nishimura K, Suto A, et al. An annexin A1-FPR1 interaction contributes to necroptosis of keratinocytes in severe cutaneous adverse drug reactions. Sci Transl Med. 2014. https://doi.org/10.1126/scitranslmed.3008227.
Kearney CJ, Martin SJ. An inflammatory perspective on necroptosis. Mol Cell. 2017;65(6):965–73.
Kim SK, Kim W-J, Yoon J-H, Ji J-H, Morgan MJ, Cho H, et al. Upregulated RIP3 expression potentiates MLKL phosphorylation-mediated programmed necrosis in toxic epidermal necrolysis. J Investig Dermatol. 2015;135(8):2021–30.
Choi S-W, Park H-H, Kim S, Chung JM, Noh H-J, Kim SK, et al. PELI1 selectively targets kinase-active RIP3 for ubiquitylation-dependent proteasomal degradation. Mol Cell. 2018;70(5):920–35.
Mizukawa Y, Hirahara K, Kano Y, Shiohara T. Drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms severity score: a useful tool for assessing disease severity and predicting fatal cytomegalovirus disease. J Am Acad Dermatol. 2019;80(3):670–8.
Coopman SA, Johnson RA, Platt R, Stern RS. Cutaneous disease and drug reactions in HIV infection. N Engl J Med. 1993;328(23):1670–4.
Chung W-H, Chang W-C, Stocker SL, Juo C-G, Graham GG, Lee M-HH, et al. Insights into the poor prognosis of allopurinol-induced severe cutaneous adverse reactions: the impact of renal insufficiency, high plasma levels of oxypurinol and granulysin. Ann Rheum Dis. 2015;74(12):2157–64.
Chung WH, Chang WC, Lee YS, Wu YY, Yang CH, Ho HC, et al. Genetic variants associated with phenytoin-related severe cutaneous adverse reactions. JAMA. 2014;312(5):525–34.
Ciccacci C, Di Fusco D, Marazzi MC, Zimba I, Erba F, Novelli G, et al. Association between CYP2B6 polymorphisms and nevirapine-induced SJS/TEN: a pharmacogenetics study. Eur J Clin Pharmacol. 2013;69(11):1909–16.
Ciccacci C, Latini A, Politi C, Mancinelli S, Marazzi MC, Novelli G, et al. Impact of glutathione transferases genes polymorphisms in nevirapine adverse reactions: a possible role for GSTM1 in SJS/TEN susceptibility. Eur J Clin Pharmacol. 2017;73(10):1253–9.
Nicoletti P, Bansal M, Lefebvre C, Guarnieri P, Shen Y, Peer I, et al. ABC transporters and the proteasome complex are implicated in susceptibility to Stevens–Johnson syndrome and toxic epidermal necrolysis across multiple drugs. PLoS One. 2015. https://doi.org/10.1371/journal.pone.0131038.
Turner CT, Lim D, Granville DJ. Granzyme B in skin inflammation and disease. Matrix Biol. 2019. https://doi.org/10.1016/j.matbio.2017.12.005.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Teresa Bellón has no conflicts of interest that are directly relevant to the content of this review.
Funding
This work was supported by Grant FIS PI13/01768 from Instituto de Salud Carlos III (co-founded by FEDER).
Rights and permissions
About this article
Cite this article
Bellón, T. Mechanisms of Severe Cutaneous Adverse Reactions: Recent Advances. Drug Saf 42, 973–992 (2019). https://doi.org/10.1007/s40264-019-00825-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-019-00825-2