Abstract
Levodopa treatment remains the gold standard for Parkinson’s disease, but shortcomings related to the pharmacological profile, notably, oral administration and the consequent occurrence of motor complications, have led to the development of several add-on levodopa treatments or to research to improve the method of delivery. Motor fluctuations, and to a lesser extent non-motor fluctuations, concern half of the patients with Parkinson’s disease after 5 years of disease and patients identified them as one of their most bothersome symptoms. Catechol-O-methyl transferase inhibitors (COMT-Is) are one of the recommended first-line levodopa add-on therapies for the amelioration of end-of dose motor fluctuations in patient with advanced Parkinson’s disease. Currently, two peripheral COMT-Is are considered as first-line choices - entacapone (ENT), which was approved by the US Food and Drug Administration in 1999 and the European Committee in 1998; and opicapone (OPC), which was approved by the European Committee in 2016. A second-line COMT-I that requires regular hepatic monitoring, tolcapone (TOL), was approved by the Food and Drug Administration in 1998 and the European Committee in 1997. Of note, OPC also received Food and Drug Administration approval in 2021, but it is still only marketed in a few countries, including Germany, UK, Spain, Portugal, Italy, Japan, and USA, while ENT and TOL have a wider market. Our narrative review summarizes the pharmacokinetic/pharmacodynamic properties, clinical efficacy in terms of motor fluctuations, motor/non-motor symptoms, quality of life, and safety data of these three COMT-Is, as evidenced by randomized clinical trials, as well as by real-life observational studies. Overall, a phase III non-inferiority trial showed a similar effect between ENT and OPC on off-time (−60.8 min/day and −40.3 min/day, vs placebo, respectively), with a possible additional off-time reduction of 39 min/day, obtained when there is a switch from ENT to OPC. Concomitantly, TOL can reduce off-time by an average of 98 min/day. A significant though discrete concomitant reduction on the Unified Parkinson's Disease Rating Scale motor section (2–3 points) is obtained with all three drugs vs placebo. Data on quality of life are fewer and more heterogeneous, with positive results obtained especially in open-label studies. Effects on non-motor symptoms were investigated as secondary outcome only in a few studies, frequently by means of non-specific scales and a benefit was observed in open-label studies. Dopaminergic adverse effects were the most frequent, dyskinesia being the most common for the three drugs eventually requiring levodopa dose reductions. No urine discoloration and a very low incidence of diarrhea were found with OPC compared with ENT and TOL. Regular hepatic monitoring is needed only for TOL. A combination of COMT-Is with new formulations of levodopa, including the subcutaneous, intrajejunal, or new extended-release formulation, merits further exploration to improve the management of both mild and severe motor fluctuations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Catechol-O-methyl transferase inhibitors (COMT-Is) are one of the treatments that can be combined with levodopa to improve motor fluctuations in Parkinson’s disease. |
Three COMT-Is are currently available: the first choices are entacapone, which is administered with each dose of levodopa, and opicapone, which is administered once a day, at bedtime, 1 h after the last dose of levodopa. The second choice is tolcapone, which is more efficacious on motor fluctuation than entacapone, but which has limited practical utility because of required frequent liver function monitoring. |
Opicapone has been shown to be non-inferior compared to entacapone on off-time reduction and to provide a possible additional reduction on off-time while switching from entacapone to opicapone. However, opicapone is only available in a few European countries, Japan, and the USA. |
The use of COMT-Is in combination with device-aided treatment and new levodopa formulations merits further investigations. |
1 Introduction
Parkinson’s disease (PD) is the second most common, age-related neurodegenerative disorder after Alzheimer’s disease. In 2015, the Global Burden of Disease Study estimated that 6.2 million individuals had PD and that considering the growth rate, this number will double to up to 12.9 million affected people by 2040 [1].
Currently, no disease-modifying therapies are available, and levodopa (l-dopa) treatment is still the gold standard for the control of parkinsonian motor symptoms [2]. However, because of the short pharmacologic half-life of l-dopa, which is about 60–90 min, there are fluctuations in plasma levels, leading to clinically bothersome motor fluctuations and l-dopa-induced dyskinesia (LID) [2].
End-of-dose motor fluctuations at the end of inter-dose intervals are the most common motor complications, occurring in 22% of the patients by 2.5 years, 50% or more of patients with PD treated for longer than 5 years, and increasing up to 70% of patients after 9 years [3]. At the same time, a survey of 320 patients with PD found early morning off-time periods among 44% of the patients in early disease stages and an overall prevalence of 60% [4], enlarging the spectrum of possibly early motor complications.
Numerous pharmacological efforts have been made to overcome the limitations related to the short half-life of l-dopa, aimed at smoothing l-dopa-related motor complications and extending the effect. They include the use of l-dopa add-on strategies or the development of newer apomorphine and l-dopa formulations, including new oral extended-release (ER) formulations such as IPX066 [5] or subcutaneous infusions. In fact, issues related to the oral route and intestinal absorption of l-dopa in later disease stages may render this route lengthy and inefficacious [2]. Subsequently, a subcutaneous continuous apomorphine infusion and l-dopa intestinal gel treatments have been developed and proved their efficacy in the treatment of motor complications and, recently, two other on-demand therapies have been approved for sudden off-time episodes, i.e., sublingual apomorphine film and inhaled l-dopa [6]. At the same time, we should bear in mind that continuous delivery of l-dopa-carbidopa intestinal gel (LCIG) is effective but invasive, and cannot be employed in all patients. Several contraindications and constraints should also be considered for continuous apomorphine infusion (CAI) [7].
Regarding oral treatment, several add-on l-dopa treatments are currently available and are recommended by the International Parkinson and Movement Disorder Society (MDS) to manage motor fluctuations, including dopamine agonists (DAs), monoamine oxidase type B inhibitors (MAO-B-Is), and catechol-O-methyl transferase inhibitors (COMT-Is) [8]. The choice is often based on the patients’ clinical profile, the previous treatment regimen/response, and the physician’s experience [8]. Two COMT-Is are currently used as first-line l-dopa add-on therapy to improve end-of dose motor fluctuations and a third is used as a “second-line choice” [9]: (i) entacapone (ENT), a peripheral COMT-I approved by the US Food and Drug Administration (FDA) in 1999 and widely used since then [10, 11]; (ii) opicapone (OPC, known as BIA 9-1067 and commercialized as Ongentys®), a third-generation COMT-I approved by the European Commission (European Union) in June 2016 [12]; and (iii) tolcapone (TOL), a central and peripheral COMT-I approved by the FDA in 1998 and currently considered a second-line treatment as it has a less favorable safety profile compared with other COMT-Is and requires continuous liver function monitoring [13].
This is a narrative review that focuses on the role of COMT-Is in the management of PD. The three drugs that are marketed are considered, along with the key differences in pharmacological profiles and the available efficacy, safety, and tolerability data from clinical trials and real-world studies. Practical clinical and future implications are also discussed.
2 Chemistry and Mechanism of Action
Levodopa is rapidly metabolized mainly by peripheral aromatic l-amino acid decarboxylase (70%) and O-methylation (10%) and only 1% of an oral dose of l-dopa reaches the brain [2]. As a result, l-dopa is administered with dopa decarboxylase inhibitors (DDCIs), such as carbidopa and benserazide. Catechol-O-methyl transferase inhibitors also act on l-dopa metabolism [14]. Catechol-O-methyl transferase is an intracellular enzyme, widely distributed in peripheral tissues, such as the liver, kidney, and intestinal tract [15]. The substrates of COMT include l-dopa, catecholamines, catecholestrogens, and some drugs, such as benserazide, carbidopa, dobutamide, and isoprenaline. The COMT enzyme catalyzes the O-methylation of l-dopa to yield 3-O-methyldopa (3-OMD), which competes with l-dopa for transport at the blood–brain barrier (BBB) [15]. 3-O-methyldopa has a long elimination half-life of 15–18 h [16], which leads to an accumulation during long-term l-dopa treatment. Therefore, COMT-Is are usually used to peripherally inhibit l-dopa metabolism by reducing 3-OMD levels and increasing the delivery of l-dopa to the brain [15] (Fig. 1).
Metabolism of levodopa (L-DOPA) and dopamine: effects of catechol-O-methyltransferase (COMT) inhibition by opicapone (OPC), tolcapone (TOL), and entacapone (ENT). 3-MT 3-methoxytyramine, 3-OMD 3-O-methyldopa, AAD aromatic amino acid decarboxylase, DOPAC 3,4-dihydroxyphenylacetic acid, HVA homovanillic acid, MAO monoamine oxidase
2.1 TOL
The chemical name for TOL is 3,4-dihydroxy-4¢-methyl-5-nitrobenzophenone, also known as Ro 40-7592. Tolcapone is a reversible selective COMT-I that can cross the BBB and is considered both a peripherally and centrally acting COMT-I.
2.2 ENT
The chemical name for ENT is (E)-2-cyano-N,N-diethyl-3-(3,4-dihydroxy-5-nitrophenyl) propenamide, also known as OR-611. Entacapone is poorly lipophilic and does not penetrate the BBB to any significant extent. Therefore, the clinical effects are due to peripheral, selective, and reversible COMT inhibition.
2.3 OPC
The chemical name for OPC is 2,5-dichloro-3-[5-(3,4-dihydroxy-5-nitrophenyl]-1,2,4-oxadiazol-3-yl)-4,6-dimethylpyridine 1-oxide, also known as BIA 9-1067. Opicapone is a hydrophilic 1,2,4-oxadiazole analog with a pyridine N-oxide residue at position 3 intended to provide high COMT inhibitory potency and avoid the risk of cell toxicity [17]. Opicapone has a long duration of action in vivo due to a high binding affinity (sub-picomolar Kd), resulting in a long residence time of the reversible COMT–OPC complex, manifested by a slow complex dissociation rate constant [18]. In liver homogenates of Wistar rats, OPC led to complete inhibition of COMT, with higher inhibition periods (99% after 1 h of administration) than both TOL (82%) and ENT (68%), and resulted in sustained increase of l-dopa plasma levels (up to 24 h) when administrated with l-dopa/benserazide [19]. These properties allow once-daily administration. Opicapone does not cross the BBB and [20] has been defined as a peripheral COMT enzyme inhibitor (see Table 1).
3 Pharmacokinetics
3.1 TOL
Tolcapone reaches peak concentration approximately 2 h (range 1–3.1 h) after administration of a 200-mg dose, with stable linear pharmacokinetics at up to 200 mg three times daily (t.i.d). The pharmacokinetic profile of TOL 100 mg or 200 mg, alone or in combination with l-dopa/DDCI is similar. It undergoes extensive metabolism, with 0.5% of the drug excreted unchanged, as it is primarily glucuronidated to inactive 3-O-β,d-glucuronic acid conjugate [21]. The terminal elimination half-life is 2 h after a single oral 200-mg dose (1.7 h for 5 mg to 3.4 h for 800 mg). With multiple dosing of 400–800 mg, TOL accumulation can be observed, resulting in a prolongation of up to 19.0 h of the terminal elimination half-life [22]. Approximately 3% of TOL is O-methylated into 3-O-methyltolcapone (Ro 40-7591), which has poor COMT-I activity and a dose-independent terminal elimination half-life (30–40 h) [23]. However, only minor accumulation of 3-O-methyltolcapone occurs. Additionally, TOL has two oxidated metabolites but because of their low concentration (less than 3%), they minimally contribute to the inhibitory effect. Finally, approximately 30% of TOL is combined to glucuronides, which do not inhibit COMT. The pharmacokinetics of TOL does not vary in the presence of food, after single vs repeated doses, or according to age.
3.1.1 Effect on l-Dopa Pharmacokinetics
In healthy volunteers, it has been shown that single graded doses (10–800 mg) of TOL dose-dependently decrease the area under the plasma concentration–time curve (AUC) of 3-OMD and concomitantly double the l-dopa AUC and the terminal elimination half-life, without affecting the maximum concentration (Cmax) or time to Cmax (tmax) [24]. This maximum two-fold increase in l-dopa AUC is reached at 100–200 mg of TOL and maintained throughout 1 week of multiple dosing. Concomitantly, an 800-mg dose of TOL t.i.d. decreases the AUC of 3-OMD by up to 98% and 200 mg t.i.d. by 64–93% [22]. Nevertheless, TOL 400–800 mg tends to prolong the absorption and tmax of l-dopa [22, 24].
3.2 ENT
In healthy volunteers, it has been shown that ENT has dose-proportional pharmacokinetics for a dose range of 5–800 mg and is absorbed in a tmax of 44 min for a 200-mg dose [25]. In fact, the Cmax and the AUC are dose related and systemic availability increases with the dose. Entacapone is metabolized mainly in the liver, and it is eliminated mainly by the kidneys, but also via the biliary route and undergoes enterohepatic circulation. After oral administration, the elimination half-life is 0.5–0.7 h for 90% elimination and 2.4–3.5 h for 10% elimination.
The main metabolite of ENT is the Z-isomer. The AUC of the Z-isomer accounts for only 5% of the total AUC [26]. The Z-isomer is as effective a COMT-I such as ENT in vitro, but it barely contributes to the ENT-induced COMT inhibition because of the low plasma levels in humans. Only about 10% of an oral dose of ENT is excreted in the urine mainly as ENT glucuronides and its Z-isomer. Therefore, ENT seems to be eliminated more by biliary than by urinary excretion [27].
3.2.1 Effect on l-Dopa Pharmacokinetics
After administration of ENT 200 mg, an increase of 32–75% (25 min) in the elimination half-life and 29–48% in the AUC0–4 h of l-dopa is obtained, compared with a placebo (Plc) [15]. The Cmax and tmax of l-dopa remain virtually unaffected after a single dose of ENT 200 mg, but repeated ENT dosing results in increased inter-dose trough l-dopa concentrations for 1 day and decreased variability in concentrations. Single doses of ENT do not usually influence the plasma 3-OMD levels or the AUC in l-dopa-treated patients, but repeated administration of ENT 200 mg along with each l-dopa dose decreases the plasma 3-OMD levels by 43–63% as well as the AUC [28,29,30].
3.3 OPC
The apparent terminal elimination half-life OPC is between 0.8 (for 50 mg) and 3.2 h (for 1200 mg), with an increase in the extent of systemic exposure in an approximately dose-proportional manner. Sulfation is the main metabolic pathway in humans [31]. Opicapone metabolites recovered in urine account for less than 3% of the amount of OPC administered, thereby suggesting that bile is probably the main route of excretion. Because of the stable and long duration of COMT inhibition at steady state, OPC can be administered concomitantly with a moderate meal without the soluble COMT (S-COMT) activity inhibition being affected. However, both a high-fat/high-calorie and a moderate meal decreases the rate and extent of OPC absorption, with delayed peak plasma concentrations compared with drug administration under fasting conditions [32, 33].
3.3.1 Effect on l-Dopa Pharmacokinetics
Among healthy volunteers, OPC 25-50-75 mg administered once daily increased the minimum plasma concentration of l-dopa without significant differences in the peak of l-dopa systemic exposure (Cmax) compared with Plc [34]. An increment in AUC probably occurred with all OPC doses compared with Plc, and with both OPC 50 and 75 mg, compared with ENT [34]. Additionally, the concomitant administration of OPC with repeated doses of 100/25 l-dopa/carbidopa, at a steady state, increases the bioavailability of l-dopa in a dose-dependent manner and reduces the formation of 3-OMD [35]. Phase I pharmacokinetic studies have shown that when OPC 25–50–75 mg is administered concomitantly with l-dopa, it increases the rate of l-dopa absorption (Cmax) in a dose-dependent manner and with a possible risk of LID. Conversely, when OPC 50 mg is administered 1 h after the l-dopa dose, it reduced the Cmax of l-dopa by ~10% and increased the extent of absorption (AUC0–t) also by ~10%. In light of these data, the practical advice was to give OPC at bedtime, 1 h after the last dose of l-dopa [36] (see Table 2).
4 Pharmacodynamics
4.1 TOL
Compared with ENT, TOL induces longer lasting COMT inhibition in erythrocytes, reversibly decreasing S-COMT activity in a dose-dependent manner. In fact, in erythrocytes of healthy subjects, a single TOL dose causes a COMT inhibition of 20% at 5 mg and 80% at 200 mg, whereas 90% inhibition for approximately 4 hours is reached with an 800-mg dose. Complete recovery of COMT activity occurs 24 hours after the doses of 5–800 mg [37, 38]. Additionally, repeated dosing of TOL 200 mg t.i.d. during l-dopa/carbidopa administration induces approximately a maximum of 80% COMT inhibition in erythrocytes in healthy elderly subjects [39]. No pharmacodynamic study comparison was performed for TOL vs OPC.
4.2 ENT
Entacapone has been shown to be an effective COMT inhibitor both in healthy volunteers [25] and in patients with PD [28] in a dose-dependent manner. Entacapone 200 mg causes rapid inhibition of 65% of S-COMT in erythrocytes, which increases to 82% at the highest dose of 800 mg. In patients with PD 1 h after administration of ENT 200 mg and l-dopa/DDCI, the inhibition is 38% [28, 40]. Erythrocyte S-COMT activity recovers within 8 h of the doses of 5–800 mg of entacapone.
4.3 OPC
Opicapone allows a maximum COMT inhibition (Emax) range from 34.5% (10 mg) to 100% (1200 mg), including an inhibition of 25.1–76.5% that persisted 24 h post-dose [32, 41]. In Wistar rats, a single administration of OPC increased the l-dopa plasma levels with a concomitant reduction in 3-OMD from 2 h up to 24 h post-administration, and was superior to TOL, as assessed by evaluating COMT activity and l-dopa pharmacokinetics in the periphery through microdialysis [19].
In a randomized double-blind (DB) phase II study of 40 patients with PD with oral administration of Plc, 5 mg, 15 mg, or 30 mg of OPC still exerted relevant inhibition at 24 hours, with a maximum S-COMT inhibition (Emax) range from 52.0% (OPC 5 mg) to 79.8% (OPC 30 mg) and occurring between 0.9 h (OPC 30 mg) and 2.6 h (OPC 15 mg) post-dose (tEmax) [42], a significant increase in the l-dopa AUC with both OPC 15 mg and 30 mg. Therefore, despite the short half-life, OPC exerts a very long-lasting effect because of the slow dissociation of the tightly bound COMT-OPC complex.
When concomitantly administered with ER/immediate-release (IR) 100/25 l-dopa/carbidopa or ER/IR 100/25 l-dopa/benserazide, OPC 25–100 mg increases the l-dopa and benserazide Cmax and extent (AUC), but not this is not the case for carbidopa. The increase was higher with IR than with ER formulations [36] (see Table 1).
5 Clinical Evidence
5.1 Search Strategy and Methodology
As explained in the Introduction, this is a narrative review with no intention to perform a systematic analysis or a meta-analysis, but rather to summarize the evidence of the main clinical trials or meta-analyses on efficacy and safety data for TOL, ENT, and OPC in the management of patients with PD. Evidence is divided into five different clinical topics: (a) reduction in daily off-time; (b) motor complication delay; (c) improvement in Unified Parkinson’s Disease Rating Scale (UPDRS) motor score; (d) reduction in the daily dose of l-dopa; (e) quality-of-life (QoL) benefit; and (f) non-motor symptoms (NMS) effect. As expected, clinical evidence related to TOL and ENT was obtained from older randomized clinical trials (RCTs) or even older meta-analyses, while data on OPC are more recent, i.e., published within the past 6 years. Therefore, because of its recent appearance on the market and recent literature data, a specific section on ongoing or expected phase IV studies is dedicated to OPC alone.
Regarding efficacy and safety data, we searched PubMed for clinical trials (randomized, DB and/or open-label [OL]), observational studies, and meta-analyses prior to 1 July, 2021 with data on patients diagnosed with idiopathic PD treated with TOL, ENT, or OPC, using the following search strings: “tolcapone AND Parkinson’s disease,” “entacapone AND Parkinson’s disease,” and “opicapone AND Parkinson’s disease”. Only studies on human subjects published in English were considered.
5.2 Reduction in Daily Off-Time
Considering that COMT-Is were developed primarily to overcome motor fluctuations, a reduction in daily off-time has been the main primary outcome of phase III efficacy trials in this drug category, and the clinical outcome for which we have the most data. Despite an expected difference in terms of publication dates, the main RCTs on TOL and ENT having been published between 1998 and 2010, while those on OPCs date back to the past 6 years, the study populations of patients with PD share quite common clinical features among the trials for the three drugs. In fact, the study patients are usually at Hoehn and Yahr (H&Y) stages 1–3 for l-dopa treatment (with a mean of four doses per day) and do present with motor fluctuations, but the severity of which varies among the trials. At the same time, older trials on ENT and TOL do not often specify the duration of motor fluctuations required for patient inclusion and patients at H&Y stages 4–5 may have been included, which is not the case for more recent studies. This could result in a certain degree of heterogeneity in baseline characteristics. Unfortunately, we only have one trial in which COMT-Is were formally compared, i.e., ENT vs OPC (see below in the OPC paragraph on clinical efficacy) [43], which highlights the fact that there are few studies on the performances of different COMT-Is on the same population.
5.2.1 TOL
In 2020, a systematic review of the efficacy and safety profile of TOL summarized the results of 12 studies (nine RCTs, one cross-over trial, one before-and-after study, and one prospective cohort study), for a total of 967 patients with a median follow-up of 1.7 months (range 0.7–7) [13]. The median reduction in off-time/day was 126 min/day, with a range from 1 to 192 min/day. The TOL dose ranged from 100 mg t.i.d to 200 mg t.i.d. The effect of TOL plus l-dopa on off-time reduction was compared to l-dopa plus Plc or l-dopa plus bromocriptine/pergolide/ENT. A significantly higher reduction of off-time in the TOL group was noted compared with the ENT group [44], while a similar effect was noted compared to pergolide and bromocriptine [45, 46]. In addition, a Cochrane systematic review published in 2010 found evidence of a difference between ENT and TOL with participants randomized to a TOL arm achieving a reduction of almost an hour of off-time (−96 min/day, confidence interval [CI] −122.4 to −69; p < 0.00001) compared with those randomized to ENT (−36.6 min/day, CI −51 to −22.2; p < 0.00001) [47].
5.2.2 ENT
A pivotal randomized DB trial on ENT, among 301 patients with PD, showed that ENT administration with each dose of l-dopa could decrease off-time by 54 min/day compared with Plc over a period of 24 weeks, with a concomitant increment of 72 min/day in on-time [48]. In 2017, a meta-analysis on the efficacy and safety of ENT reported the main findings based on 14 RCTs that compared ENT with Plc or another add-on therapy (pramipexole or rasagiline) [11] in patients with advanced PD. Compared to Plc, ENT 200 mg in combination with l-dopa significantly reduced patients’ off-time (mean difference −58.8 min/day, 95% CI −79.8 to −37.8, p < 0.01) [11]. The RCTs included in this meta-analysis were published between 1998 and 2010. In 2010, a slightly lower effect was reported in the Cochrane meta-analysis, with a −36.6 min/day reduction in off-time [47]. Comparable results have been obtained when ENT was used with Sinemet controlled release [48, 49].
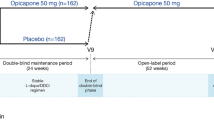
5.2.3 OPC
Two global randomized, DB, Plc-controlled, phase III trials with 1027 patients with advanced PD have shown the efficacy of OPC; the BIPARK I [43] and BIPARK II [50] studies, and one Japanese randomized, DB, phase IIb trial (COMFORT-PD) with 437 patients and a 14- to 15-week follow-up [51]. The main methodological difference among the trials was the use of OPC 5 mg and ENT arms in the BIPARK I trial, as a comparator to prove the non-inferiority of OPC vs ENT. Arms with OPC 25 mg and OPC 50 mg were included in all three trials. Opicapone trials included patients with PD with H&Y stages 1–3 (during the ON state) and a mean total awake time in the OFF state of ≥1.5 h (excluding morning akinesia), but excluded patients with severe LIDs (a score of >3 on the UPRS item 33), severe and/or unpredictable periods in the OFF state, and previous or planned deep brain stimulation (DBS) for PD. Overall, DB trials found a reduction in absolute time in the OFF state (range from −37.2 min/day in the Japanese trial [51] to −54.3 min/day and −60.8 min/day in the BIPARK II [50] and I [43], respectively, compared with Plc). The reduction in off-time was mirrored by significant increases in ON time without bothersome LIDs and no significant differences were observed for ON time with bothersome LIDs. Regarding ENT, OPC 50 mg proved to be non-inferior for a reduction in off-time (−26.2 min/day; p = 0.0051).
Participants in BIPARK I and BIPARK II who completed the DB part, participated in 1-year OL extension studies. All patients received adjunctive OPC 25 mg once daily for 1 week, after which l-dopa and OPC dosages were adjusted based on efficacy and tolerability. Open-label extensions showed that the effect on off-time reduction was maintained up to 1 year [50, 52]. Efficacy was maintained in patients who were originally treated with OPC 50 mg in the DB phase, while switching treatments from ENT to OPC led to further decreases in off-time of about −39.3 min/day [53]. Similarly, during the OL extension of the COMFORT study [54], the mean change in off-time from the DB baseline was −106.68 min/day at 28 weeks and it was almost unchanged at 52 weeks, i.e., 101.89 min/day.
5.3 Delay in Motor Complications
Not only the effect on motor fluctuations severity but also the effect in their delay of appearance is a key point in PD treatment management. Consequently, the Stalevo Reduction in Dyskinesia Evaluation in PD (STRIDE-PD) study compared the initiation of antiparkinsonian treatment with l-dopa/carbidopa vs l-dopa/carbidopa/ENT in a prospective, multicenter, DB, randomized study in patients with early PD (mean disease duration = 2 years) requiring the initiation of l-dopa therapy. Unfortunately, the STRIDE-PD study failed to demonstrate that initiating l-dopa therapy in association with ENT could delay the time of onset or reduce the frequency of LIDs, compared with l-dopa treatment alone [55]. Conversely, the study showed that patients with PD in the l-dopa/carbidopa/ENT arm had a shorter time to LID onset vs those in the l-dopa/carbidopa arm. However, it should be noted that no reduction in l-dopa dose was allowed during the entire study period and the dose was progressively titrated up to 100/25 or 150/37.5 mg × 4/day, administered at 3.5-hour intervals, which does not reflect current clinical practice for patients with early PD [55]. The same patients subsequently participated in an OL study to investigate the risks related to the development of LIDs and wearing-off, which showed that these phenomena were positively correlated to the dose of l-dopa [56]. Along the same lines as the STRIDE-PD study, the FIRST-STEP trial compared the efficacy and tolerability of l-dopa vs l-dopa/carbidopa/ENT in patients with early PD, and found a significant difference in the UPDRS-II score in favor of the l-dopa/carbidopa/ENT arm at week 4 and maintained through the 39th week, with no difference in wearing-off or dyskinesia [57]. The STRIDE-PD and FIRST-STEP Study Group are the only published studies that aimed to better explicate the role of COMT-Is in the delay of motor complications. Despite the benefit in terms of activities of daily living reported in these studies, the aggravation of LIDs with the early use of ENT highlighted by STRIDE-PD, neither contributed to the development of further studies nor justified the early use of COMT-Is (see Expert Opinion section).
5.4 Improvement in UPDRS Motor Score
Modifications in UPDRS part III (motor score) are universally monitored in clinical trials on motor fluctuation treatment. At the same time, when considering UPDRS-III scores, clinicians should be aware of the possible impact of dopaminergic medication on patients with motor-fluctuating PD, the effect of which is not always strictly considered in clinical trial evaluation, and on the impact of the disease severity. In fact, an annual increase in motor impairment has been estimated at approximately 2.4 points on the UPDRS-III within the first 5 years of disease [58], with a standardized annual progression rate of 2.4% at H&Y stages 1–2.5 [59], but possibly with a slower rate of progression in a more advanced stage, and finally a tendency for greater deterioration in the score in the late stage of the disease [60]. On that note, we should bear in mind that a reduction of at least 5 points on the UPDRS-III has been indicated as minimally clinically meaningful in patients at H&Y stages 1–3 [61]. Therefore, when comparing the effect on the UPDRS-III score of different COMT-Is, we should fully consider the clinical features of the study population and the trial design.
5.4.1 Motor Score Improvement in Patients with Stable PD
Regarding patients with early non-motor-fluctuating PD, data on the UPDRS-III are available only for treatment with TOL and ENT, while data for OPC should be published in the next few years (see On-going trials section). TOL at 100 or 200 mg t.i.d produced a significant reduction in the UPDRS part III (−2.0 and −2.3 points, respectively vs Plc) scores in patients with nonfluctuating stable PD over 6 months, with an effect that lasted 12 months without significantly increasing motor fluctuations [62]. Conversely, no difference was observed in the FIRST-STEP study, which compared l-dopa/carbidopa/ENT vs l-dopa/carbidopa over 39 months, and no differences were noted in the STRIDE-PD study either. However, data from the motor section are presented together with the activities of daily living section of the UPDRS [55].
5.4.2 Motor Score Improvement in Patients with Fluctuating Advanced PD
5.4.2.1 TOL
A recent systematic review reported a median reduction in UPDRS-III in the OFF medication state of a mean of −3.6 points (range: −1.1 to −6.5) [13]. This reduction was found by analyzing 12 RCTs, one cross-over trial, one non-RCT, and one OL study, for a total of 1113 patients and a median follow-up of 2.2 months (range: 0.7–12). The UPDRS-III score changes obtained with l-dopa plus TOL were vs l-dopa plus Plc or plus bromocriptine (n = 1) [46], pergolide (n = 1) [45], or ENT (n = 3) [44, 63, 64]. Tolcapone vs an active control showed no difference, while vs Plc, 3/8 studies found a significant difference in favor of TOL-treated patients.
5.4.2.2 ENT
A statistically significant reduction in the UPDRS-III was found when ENT was compared with Plc (mean difference −2.38, 95% CI −3.42 to −1.34, p < 0.01), based on a recent meta-analysis of six RCTs [11]. In the 2010 Cochrane meta-analysis that compared ENT with TOL, no difference was noted with −2.14 points, CI −2.92 to −1.36 for ENT and −1.73 points, CI −2.96 to −0.51 for TOL [47].
5.4.2.3 OPC
In the BIPARK I DB trial, only the total UPDRS score is reported, not the motor score, and it was numerically improved from baseline in all treatment groups, i.e., Plc, ENT, and OPC, but with no statistically significant differences between groups. A non-statistical improvement was reported for the UPDRS-III score in the BIPARK II DB trial with OPC vs Plc [−2.0 (0.5); p = 0.88] [43, 50]. The Japanese COMFORT PD trial showed a significant reduction for OPC 50 mg vs Plc on the UPDRS-III score [−3.6 (0.4); p = 0.04] [51].
5.5 Reduction in the Daily Dose of l-dopa
When adding a new oral therapy to l-dopa, a reduction in the dose may be required. A reduction in approximately half of the l-dopa equivalent daily dose (LEDD) is also usually reached early after subthalamic nucleus (STN)-DBS implantation. Such reductions in LEDD may not have a particularly practical clinical interest, but they could mirror the effectiveness of the new treatment and imply a simplification in the patient’s treatment regimen. It is also interesting to note that an l-dopa dose reduction could be principally caused by the occurrence of LIDs, which may both mirror the effectiveness of treatment but is also an adverse event (AE) for the patient.
5.5.1 TOL
Based on the analysis of 16 studies (11 RCTs, one cross-over trial, one non-RCT, two before-and-after studies, and one case-control study), for a total of 995 patients treated with TOL, Artusi and colleagues found a median reduction in l-dopa of 108.9 mg (range: 1–251.5 mg) over a follow-up period of 2.5 months (range 0.5–12) [13]. Six out of eight studies vs Plc found a significantly lower daily dose of l-dopa compared with TOL. Two studies vs ENT and one study vs bromocriptine reported a significantly higher reduction in l-dopa in the TOL group, while a comparable l-dopa reduction was reported in one study vs pergolide. In the 2010 Cochrane meta-analysis that compared TOL with ENT, a greater reduction in the l-dopa dose was noted with TOL (−116.47 mg/day, CI −140.62 to −92.32) than with ENT (−41.62 mg/day, CI −51.35 to −31.89), but with significant heterogeneity between trials that was not explained by drug dose [47].
5.5.2 ENT
Based on a meta-analysis of eight RCTs, a significant reduction in l-dopa dose was reported with ENT compared with Plc (mean difference: −37.82, 95% CI −64.80 to −10.83, p < 0.01) [11] (see previous paragraph for a comparison of TOL vs ENT for the l-dopa dose reduction). Data from a 3-year OL extension of the 6-month DB-PLC-controlled Nordic trial (NOMECOMT) found a mean daily decrease in l-dopa dose from 737 mg at baseline to 649 mg in 1 year, which rose slightly to 696 mg in 3 years of ENT treatment, which was still below the baseline dose [65].
5.5.3 OPC
In the pooled data of the dose adjustment period (3 weeks) of the BIPARK I and BIPARK II DB phases, a reduction in approximately 23% in l-dopa dose (~200 mg) was obtained in the OPC 50-mg arm [66]. Thereafter, in the OL extension, patients who switched from DB Plc to OPC 50 mg decreased from l-dopa 701 mg/day at the DB baseline to 655 mg/day at the end of the OL extension, while those treated with OPC 50 mg for the entire study period went from 718 mg/day to 679 mg/day.
5.6 QoL Benefit
Patients’ QoL is becoming a recognized relevant outcome in pharmacological, non-pharmacological, and surgical PD trials. Nevertheless, it is not usually the primary but rather a secondary outcome, although it may support the benefit, if any, showed by the primary endpoint analysis. Considering that the power of a study is not calculated on the basis of secondary endpoints, the effect on QoL should be cautiously interpreted, especially if negative.
5.6.1 TOL
In the recent systematic review by Artusi and colleagues, the results of nine studies on the effect of TOL on QoL were reported. They included four RCTs, with data vs Plc and one vs pergolide [13]. Two of the four studies vs Plc [62, 67,68,69] and one study that compared TOL vs pergolide [45] found a significantly greater improvement in QoL in patients treated with TOL compared with Plc or an active control, although based on different QoL measures. The study vs pergolide lasted 3 months, and reported a greater benefit with TOL on the Sickness Impact Profile and on the Parkinson’s Disease Questionnaire (PDQ)-39 scores [45]. One trial with a short follow-up of 42 days vs Plc reported an improvement in QoL on the Sickness Impact Profile [68] and the other found no improvement on the Sickness Impact Profile, only on the UPDRS-II [62] over a follow-up period of 6 months.
5.6.2 ENT
In a DB Plc-controlled phase IV study of 270 patients with PD randomized to receive either ENT 200 mg or Plc, no differences were found for QoL measures, i.e., PDQ-39, the Short-Form-36, or the European Quality of Life five-dimension questionnaire (EQ-5D), over a period of 13 weeks [70]. Similar results were found in a randomized, DB, Plc-controlled, 3-month study of 162 patients with PD, based on Short Form-36 scales [71]. Conversely, OL studies or observational studies found an improvement on QoL scales during ENT treatment for a short-term follow-up. A prospective, multicenter, observational, 12-month study found a mild and statistically significant improvement on the Parkinson’s Disease Questionnaire-8 (PDQ-8) [from 12.1 ± 5.7 at baseline to 9.2 ± 5.2 at 12 months] [72], with a more significant improvement among patients at H&Y stages 2 or 3 at baseline, compared to patients at H&Y stage 4. Similarly, an uncontrolled OL study of 479 patients with PD with wearing-off found a statistically significant improvement of 4 points (range: −5.9; −2.2) on the PDQ-39 after 8 weeks of treatment [73], especially for “mobility,” “activities of daily living,” “emotional well-being,” and “bodily discomfort” domains. Similar results were obtained in a multicenter observational study of 498 patients with PD, with QoL improved by a mean of 10% in all categories of the PDQ-39 (p < 0.001), except for social support and cognition, after 8 weeks of ENT treatment [74].
5.6.3 OPC
The randomized, DB, PLC-controlled phase III BIPARK I [43] and BIPARK II [50] trials and the randomized, DB, phase IIb Japanese COMFORT-PD [51] trial found no statistically significant improvement in QoL, as measured by the PDQ-39, nor vs ENT or vs Plc, over a period of 14–15 weeks. Recently, a phase IV prospective, OL trial, OPTIPARK trial was conducted in Germany (3 months) and the UK (6 months) under normal conditions of clinical practice, including a heterogeneous population of 495 patients with PD with motor fluctuations [75]. Patients were treated with OPC 50 mg, in addition to l-dopa and a small but statistically significant improvement on the PDQ-8 (−3.4 ± 12.8 points) was reported [75].
5.7 Effect on Non-Motor Symptoms
The importance of parkinsonian NMS, their impact on patient QoL, and the effect of dopaminergic and non-dopaminergic treatments on these symptoms have become recognized factors in PD over the past 15 years [76]. This time-line bias highlights obvious limitations in comparing the effects of three COMT-Is, considering that for TOL and ENT most of the trials were conducted before 2005. Conversely, one on-going trial on OPC specifically targets NMS (see "Section 6").
5.7.1 TOL
The recently published systematic review on TOL reported on ten studies that investigated the effect of the drug on NMS and included six RCTs vs Plc, one switch-over trial, one OL study on a group of patients enrolled from the RCT, one before-and-after study, and one prospective cohort study [13]. Only one study adopted a specific scale validated for the assessment of NMS, i.e., the ‘Non-Motor Symptoms Scale for Parkinson’s Disease’ (NMSS), another study focused on sleep assessment and a third on cognitive functions, but none of these studies had a control group. The others only used the UPDRS-I. The switch-over trial found no improvement on the UPDRS-I in the TOL or the ENT group [64]. The only study that adopted the NMSS was on an observational trial that found a mean improvement of 15 points on the total score after 4 weeks of treatment, which was statistically significant for the following scale domains: cardiovascular, sleep/fatigue, mood/cognition, gastrointestinal, urinary, and pain/smell/weight/sweating [77]. One prospective cohort study was specifically focused on sleep and reported a significant improvement on the PD Sleep Scale, from 21.6 ± 8.1 at baseline to 16.3 ± 7.7 on the final assessment, mirrored by a reduction on the Epworth Sleepiness Scale after 4 weeks of treatment [78]. A study that specifically assessed cognitive functions, although only eight patients with PD were included, found an improvement in attentional task, auditory verbal short-term memory, visuo-spatial recall, and constructional apraxia after 6 weeks of treatment [79].
5.7.2 ENT
No study has specifically explored the effect of ENT on NMS. In a 6-month randomized Plc-controlled DB study of 301 patients with PD with motor fluctuations, no differences were found in the UPDRS-I score comparing ENT with Plc after 24 weeks of treatment, but there was a statistically significant worsening after 2 weeks of ENT withdrawal [48]. The BIPARK-I trial was the only one that analyzed NMS changes by means of a specific scale, and found a mean reduction of −4.7 ± 1.5 on the NMSS, which was not statistically significant, as was the case for OPC (−2 ± 1.5) [43].
5.7.3 OPC
No study has specifically explored the effect of OPC on NMS, but the BIPARK I and II studies explored its effect on NMS by analyzing the NMSS data [43, 50]. Overall, a non-significant improvement in NMSS total score was observed and was more evident with OPC 50 mg, with numerical differences in favor of OPC for the sleep/fatigue domains. This trend was confirmed during the OL phase, with a mean improvement of −4.2 in the NMSS total score and no worsening in any specific domain [80]. In the phase IV prospective OL trial, OPTIPARK, a significant mean reduction of −6.8 ± 19.7 points in the NMSS total score was found after 3 months of treatment with OPC 50 mg, which was significant for all scale domains except for “perceptual problems/hallucinations”, which showed a non-significant aggravation of 2.01 ± 17.0 [75].
6 OPC: Ongoing and Expected Phase III–IV Trials and Observational Studies
Several phase III–IV trials are currently ongoing or about to start in a short time, which focus mainly on NMS and patients with PD at the stage of early motor complications:
(1) ADOPTION, NCT04990284, a prospective, OL, exploratory, low-interventional 1-month trial aimed at evaluating the add-on effect of OPC 50 mg or l-dopa 100 mg as a first-line strategy for the treatment of wearing-off in early fluctuators.
(2) OCEAN, NCT04986982, a DB, randomized, Plc-controlled 6-month trial aimed at investigating the efficacy of OPC 50 mg in patients with PD with end-of-dose motor fluctuations and associated pain. A change from baseline to month 6 in Domain 3 (fluctuation-related pain) of the King’s Parkinson’s Disease Pain Scale is the primary outcome, while changes in anxiety, depression, sleep, and wakefulness will be secondary efficacy measures.
(3) OASIS, NCT04986995, a pilot, prospective, OL, single-arm, interventional 6-week study aimed at evaluating the effect of OPC 50 mg in patients with PD with sleep disorder and end-of-dose motor fluctuations. A change in the PD Sleep Scale-2 total scores will be the primary endpoint while secondary measures will include the change from baseline on the PD Fatigue Scale (PFS-16) and in Domain K (sleep and wakefulness) of the MDS-sponsored Non-motor Rating Scale.
(4) Early ParkinSon wIth l-dopA and OpicapoNe [EPSILON] study NCT04978597; EudraCT number 2020-005011-52, a phase III, DB, randomized, Plc-controlled 24-week phase trial to evaluate the efficacy and safety of OPC 50 mg in early PD, without any motor complications, followed by an OL extension phase of 1 year. Patients included should be treated with three to four daily oral doses (up to 500 mg of l-dopa) and have signs of treatable motor impairment but no motor complications. During the DB phase, the patients’ current l-dopa/DDCI regimen should remain stable. The change in the MDS-UPDRS Part III score from baseline to the end of the DB period is the primary endpoint.
(5) NCT04821687, a phase IV multicenter randomized, OL trial to evaluate the add-on effect of OPC 50 mg or l-dopa 100 mg for the treatment of wearing-off as a first-line strategy.
(6) NCT04787965, OPTI-ON, an observational study to describe the treatment patterns and clinical outcomes observed with OPC as an add-on treatment to l-dopa/carbidopa in patients with PD experiencing “off” episodes with motor fluctuations. The Non-Motor Fluctuation Assessment (NoMoFa) will be used to better quantify the severity of both static and fluctuating NMS.
(7) A phase II, open-label trial with 203 patients to assess the effect of OPC 50 mg on l-dopa pharmacokinetics in different l-dopa/carbidopa treatment regimens among patients with end-of-dose motor fluctuations. Twenty-four patients will receive five doses of 500/125 mg l-dopa/carbidopa for 2 weeks, and will be randomized to either four or five doses of 400/100 mg l-dopa/carbidopa plus OPC 50 mg for 2 weeks. The pharmacokinetics of l-dopa at the end of both 2-week treatment periods will be the primary endpoint.
7 COMT-I Genetic Polymorphism and Treatment Implications
A single autosomal locus with two codominant alleles regulates COMT activity. The variability in COMT activity is due to a polymorphism in the COMT gene (rs4608) that results in the conversion in the enzyme of valine 158 to methionine (Val158Met). The 158Val allele is associated with higher enzymatic activity (COMTH allele) and the 158Met allele with lower activity (COMTL allele). When a Caucasian population of patients with PD was compared to the general population, a similar distribution of the COMTH and COMTL alleles was found, including 25% low (COMTLL), 50% intermediate (COMTHL), and 25% high (COMTHH) activity [81]. Regarding ENT, a small DB crossover trial with 33 patients with PD demonstrated higher COMT inhibition by ENT in COMTHH than in COMTLL patients, by means of a l-dopa challenge test [82]. Regarding OPC and TOL, at present, we do not know to what extent the COMT genotype modulates the magnitude of response, but the role of pharmacogenetics in PD treatment could gain relevance in the next years. Indeed, a pre-treatment stratification of patients according to COMT polymorphisms could further improve COMT-I treatment management and should be further explored for OPC and TOL.
8 COMT-Is and l-dopa Carbidopa Intestinal Gel/Subcutaneous l-dopa Combination
l-dopa/carbidopa intestinal gel is a treatment developed for patients with advanced PD and motor complications that cannot be optimally treated by oral drugs [83]. Continuous infusion of l-dopa, resulting in a more stable plasma concentration, stabilizes motor fluctuations (on–off phenomenon) and decreases LID time [83].
More recently, the new combination of l-dopa/ENT/carbidopa intestinal gel (LECIG) has been proposed. In fact, a pilot study showed that the addition of oral ENT or TOL (every 5 hours) to LCIG treatment allowed a decrement of approximately 20% in the LCIG dose, with the plasma concentrations at steady state (0.5–8 hours) that were not different from LCIG administered alone without a dose adjustment [84]. At the same time, a small pharmacokinetic study on 11 patients with PD, all genotyped for rs4680 (polymorphism of the COMT gene), rs921451, and rs3837091 (polymorphisms of the DDC gene), suggested that the continuous maintenance dose of LECIG should be decreased by approximately 35% regardless of the COMT rs4680 genotype, but individuals with higher DDC and COMT enzyme activity had a tendency towards higher l-dopa estimated apparent clearances [85]. As a result, LECIG was approved by the Swedish Medical Products Agency in 2018 and has been reimbursed in Sweden since 2019. More recently, an observational study on LECIG, with half of the patients switched directly from LCIG, showed that this new pump is probably more user friendly owing to the lower weight and size [86]. However, one third of 21 patients stopped the treatment because of diarrhea [86].
Regarding TOL, a unique case series of four patients reported its use among patients with persistent severe motor fluctuations despite a high dose of LCIG [87]. The authors suggested the early need to reduce the LCIG dose by up to 50% once TOL was introduced, to prevent dopaminergic AEs, especially among older patients. Finally, this combination was recently tested with OPC in a small retrospective analysis of 11 patients with PD, which showed that a consistent reduction of approximately 25% in LEDD was reached over 1 month, when OPC 50 mg was combined with LCIG, with a consequent cost reduction [88]. Overall, the combination of COMT-Is and LCIG is still anecdotally recommended in the case of persistent motor fluctuations and suboptimal motor control once this device-aided treatment is started. [88].
Similarly, it would be particularly interesting to combine COMT-Is with continuous subcutaneous infusions of soluble l-dopa/carbidopa (ND0612 and ABBV-951), for which trials are ongoing or recently completed, but results are not yet published. In fact, these formulations do not allow the infusion of a daily dose of l-dopa above 700 mg/day to 1000 mg/day, and the combination with a COMT-I could enhance the applicability and effectiveness. Moreover, a recent randomized, Plc-controlled, DB, phase IIa trial reported an increase in l-dopa exposure reached by a combination of ENT plus ND0612 compared with ND0612 monotherapy [89].
9 Tolerability and Safety
9.1 TOL
Safety issues have characterized the marketing and utilization patterns of TOL in the past 20 years. In fact, safety concerns related to the potential hepatotoxicity of TOL have limited its use in clinical practice over the past decades, owing to four cases of liver failure described in 1998 [90,91,92]. The four patients in question developed liver failure 9–12 weeks after starting TOL treatment, although one patient remained taking TOL until death, while the other three stopped treatment soon after liver enzymes increased. Only one patient recovered from symptoms, three died [92]. This led to a marketing ban imposed in Europe and Canada for 7 years and later remarketing with some restrictions including frequent liver enzyme monitoring. Because of these events, TOL is currently indicated only for patients with l-dopa-responsive idiopathic PD with motor fluctuations, who did not respond to or are intolerant to another COMT-I. As a result, the main safety data related to TOL concern liver enzyme elevation or liver failure.
As mentioned, a recent systematic review on safety and tolerability data up to February 2020, concerning interventional and non-interventional studies on TOL treatment, was published on PubMed in January 2021 [13]. Beyond the four cases of liver failure described in 1998, no other cases were found in the literature, which analyzed 21 studies with 4182 patients [13]. Additionally, the authors retrieved AE reports in the FDA Adverse Event Reporting System and “EudraVigilance” and identified 61 reports of hepatitis, liver failure, liver toxicity, and jaundice, 19 of which described the co-occurrence of major diseases or syndromes [13].
Regarding liver enzyme elevation, the authors identified 17 studies with a mean follow-up of approximately 2 months, reporting liver enzyme elevation in 0–27.5% of the study population, although only 0.9% of the patients had a consistent elevation of liver enzymes >2 at the upper limit of normal. Because of liver enzyme elevation, 0.6% of the patients withdrew from the studies. Interestingly, 13 reviews targeted liver enzyme elevation among controls and three studies were found (two on ENT and one on pergolide as active controls) with liver enzyme elevation in up to 20% of the patients.
Of all the AEs, the most common were LIDs (1–95%), followed by nausea (0–68%), diarrhea (up to 29%), hallucinations (0–24%), liver enzyme elevation (up to 27%), urine discoloration (up to 23%), and dizziness (up to 16%) [13]. Since the systematic review published by Artusi and colleagues, no other trials or observational studies have been published on TOL treatment. In the 2010 Cochrane Review, the intra-class comparison considered ENT and TOL for any AE and found no significant differences between these two COMT-Is (ENT: odds ratio 1.85, CI 1.47–2.33; p < 0.00001 vs TOL: OR 2.89, CI 1.74–4.79; p < 0.0001) [47].
9.2 ENT
The safety of ENT has been extensively investigated and is based on large-scale controlled trials [48, 93,94,95,96], long-term follow-up studies and Plc-controlled [71] and uncontrolled studies [73, 74], post-marketing surveillance, and a few more recent meta-analyses [11, 97]. As ENT increases the bioavailability of l-dopa, dopaminergic AEs are the most frequent, dyskinesia being the most common, at times requiring an extension of the dose interval or a reduction in the dose of l-dopa. The second most-common dopaminergic AE is nausea. Some of the most common non-dopaminergic AEs are abdominal pain, diarrhea, and harmless urine discoloration, which may appear within weeks or months after starting ENT and may disappear during therapy. Interestingly, in a 6-month OL observation study with 132 patients with fluctuating PD, ENT 200 mg at each l-dopa dose induced mainly sleep and neuropsychiatric AEs with quite a high rate of insomnia (29.5%) and hallucinations (14.4%), associated with an early incidence of LIDs (12%) and nausea (19.7%) and managed by LEDD reduction [65]. In older trials, such as in the pooled safety data of the first phase III trials on ENT, which including an entire population of 806 patients, a higher percentage of 30.4% LIDs is reported, followed by nausea (13.6%) and diarrhea (10.3%) [98]. Conversely, in a recent meta-analysis published between 2005 and 2014 on l-dopa/ENT/carbidopa treatment, which analyzed six RCT results for a total of 1938 patients, the frequencies for the following lower percentage of AEs were reported: nausea 23%, diarrhea 12.9%, dyskinesia 5.9%, dizziness 10.6%, and urine abnormality 13.6%, which were significantly higher compared with the control group [97], but with no mention of hallucinations. This probably indicates better knowledge in LID management or the clinical indication for ENT treatment over the years.
9.3 OPC
To date, there has been no hepatic safety concerns related to OPC, as is the case for ENT. The most frequent AEs are dopaminergic, namely, LIDs. In fact, in the DB and OL BIPARK I and BIPARK II trials, 24% of the patients were reported to have LIDs (vs 8.1% taking Plc, BIPARK II, DB) [12]. At the same time, the frequency and intensity of LIDs seems to decrease with subsequent l-dopa adjustments, as observed in the OL extensions, with frequency decreasing to 14.5% and 21.5% in the BIPARK I and II, respectively [50, 52]. The second most frequent dopaminergic AE was nausea, which was present in approximately 3% of the patients (and 7% in the ENT arm of BIPARK-I). For common non-dopaminergic events noted in BIPARK I and II, we identified constipation, insomnia, dry mouth, and hypertension [99]. Conversely, whereas severe diarrhea was described as the most frequent cause of treatment discontinuation with TOL (up to 10%) and ENT, a lower incidence (<2%) and no urine discoloration were noted with OPC [99, 100]. When data are stratified by age (<70 years vs ≥70 years), OPC continued to maintain a good safety profile compared to Plc, but with a slightly higher incidence of TEAEs among older (age ≥70 years) compared with younger patients (age <70 years), with regard to constipation (9.3% vs 5%), nausea (5.2% vs 3%), dizziness (7.2% vs. 2.2%), hallucinations (4.6% vs 0.6%), and weight loss (7% vs 2.2%).
The data from the OL clinical study OPTIPARK are similar to that of the DB trial; LIDs were the most frequent treatment-emergent AE [TEAE] (11.5%), followed by dry mouth (6.5%), dizziness (4.8%), nausea (4.4%), constipation (4.0%), insomnia (2.4%), hallucination (2.2%), falls (2.0%), and diarrhea (0.6%). An OPTIPARK post-hoc analysis showed that the majority of potential drug-related TEAEs were reported during the first week of OPC treatment, LIDs being the most common (6.5%), but with a very low impact on patient discontinuation (<0.5%). From the third week onwards, the incidence of these TEAEs was consistently low (<4%) [101].
10 COMT-Is in the Portfolio of Advanced PD Management: Expert Opinion
As previously stated in the introduction, COMT-Is, including TOL, ENT, and OPC, are all considered as “efficacious” in the treatment of motor fluctuations in patients with PD by the recently published MDS Evidence-Based Medicine Review [9]. At the same time, TOL is actually considered a “second-line” treatment owing to the requirement for liver enzyme monitoring, although quite reassuring safety data have been recently summarized [13]. The same level of MDS recommendations related to the treatment of motor fluctuations has been assigned to other add-on oral treatments including several DAs, rasagiline, and l-dopa/DDC formulations, including a new formulation of ER l-dopa, i.e., IPX066 [9]. Conversely, there are no indications for COMT-I treatment for patients with early-stable PD to date, such as the treatment of stable motor or non-motor parkinsonian symptoms or to prevent l-dopa-induced motor complications and, in keeping with good clinical practice, clinicians usually avoid them in the management of patients with late-stage PD and dementia who are already experiencing or are at high risk for experiencing hallucinations [8]. As previously illustrated regarding the prevention of LIDs, in 2010, the STRIDE PD study failed to support the early use of add-on ENT therapy to l-dopa in patients with early PD (disease duration = 2 years) [55] compared to l-dopa alone. To date, no similar study has been conducted on TOL and OPC regarding LID prevention. The same could be inferred for the prevention/delay of motor fluctuations, although there is some pharmacodynamic hypothesis that justified a study to verify the utility/efficacy of OPC in early fluctuators (see below). In fact, a phase III trial (NCT04978597) is underway to verify the efficacy in patients with PD with no motor fluctuations, with the intention of using COMT-I to promote continuous dopaminergic stimulation (see below).
Overall, in pragmatic terms, the main questions for clinicians are:
(a) When to introduce a COMT-I/what is the best patient profile?
As previously mentioned, COMT-Is are indicated as add-on therapy for patients with PD with motor fluctuations. For patients with motor fluctuations, several treatment strategies can be adopted, usually based on the patient’s profile (tendency to develop certain AEs and his/her preference) and the treatment already established, including the increment of l-dopa doses and number of doses. Should a DA be added or the dose incremented, or should a MAO B-I or a COMT-I be added? Over the past decade, physicians have developed the tendency to be more aware of the possibility of TEAEs and are more cautious about incrementing the dose if treatment with DAs is already established. Compared with the past, the preference is now to add a COMT-I or incrementing the l-dopa dose. Recently, IPX066, an ER l-dopa/carbidopa formulation, showed its efficacy in off-time reduction vs IR l-dopa/carbidopa in a phase III DB RCT with 391 patients with H&Y stages 1–4 PD who had a baseline mean value of 5.9 hours/day of motor fluctuations (−2.18 [2.91] vs −1.01 [2.53] hours/day, p < 0.0001), with a concomitant reduction in l-dopa doses/day [102]. However, IPX066 is currently approved by the FDA and used in USA, but not in Europe. Regarding the efficacy in terms of the reduction in motor fluctuations, there are no head-to-head trials that have systematically compared COMT-Is efficacy with DAs or MAO B-Is, with the exception of: (a) an old trial that compares ENT with cabergoline, which found a similar efficacy profile but a safer profile for ENT [103]; (b) two old trials that compare TOL with pergolide [45] and bromocriptine [46], and which found no differences. Additionally, one phase III cross-over trial showed that IPX066 was more effective in off-time reduction over 2 weeks, compared with l-dopa/carbidopa/ENT (−3.8 vs −5.2 h/day; p < 0.0001) [104]. According to a Cochrane meta-analysis, overall, DAs may have the highest impact on off-time reduction (up to −1.81 h/day for pramipexole), followed by TOL (1.6 h/day), safinamide (0.86 h/day), rasagiline (0.84 hour/day), and ENT (0.61 hour/day) [47]. Additionally, despite a lack of recommendations, more cautious use of l-dopa add-on therapy with COMT-Is, MAO B-Is, or DAs is usually adopted as good clinical practice in elderly patients with PD (age >75–80 years) in the presence or with risks of hallucinations, orthostatic hypotension, as well as cognitive decline. Therefore, if an elderly patient starts complaining of motor fluctuations, the first-line treatment that physicians should adopt is an increase in the l-dopa dose, IR or ER formulations, and as a second choice a COMT-I or MAO B-I can be added, but with careful monitoring of TEAEs.
(b) How to choose from the different COMT-Is?
One randomized trial, one longitudinal observational study, and one switch-over study have compared ENT with TOL in terms of the efficacy in motor fluctuations and confirmed a slightly higher efficacy of TOL [44]. Concerning OPC, no head-to-head trial vs TOL has been performed. However, the primary non-inferiority BIPARK I trial showed that OPC 50 mg is non-inferior compared with ENT [43]. In addition, the OL BIPARK I trial extension has shown a further benefit in terms of off-time reduction (approximately 39 min/day) when switching from ENT to OPC, with OPC appearing to be also efficacious in ENT non-responders, with similar additional benefits in off-time reduction [53]. In fact, for the ENT non-responders in the BIPARK I trial, as assessed by PGI-C at the end of the DB phase, 45% (over 100 on ENT) were classified as non-responders. After 1 year of treatment with OPC, ENT-treated patients defined as ‘non-responders’ at the DB endpoint who switched to OPC showed a statistically significant additional reduction in off-time (−45.3 min, p = 0.0399) [105]. Even in terms of night-time/morning akinesia, we found some data in favor of OPC. In the post-hoc analysis of BIPARK I data, reductions of 14%, 46%, and 64% were noted for the Plc, ENT, and OPC 50-mg arms, respectively, for night-time akinesia [106]. Regarding morning akinesia, a post-hoc analysis of the BIPARK I trial found a reduction in morning off-time that was twice the percentage for OPC 50 mg vs ENT (20% vs 10%) and no early morning OFF was observed for OPC 50 mg, but rather for ENT [107].
The initial choices of COMT-Is are ENT and OPC. The main reason to choose ENT first is related to availability. Opicapone is still not marketed in many countries all over the world, although it is available in Italy, Germany, Spain, the UK, Japan, and the USA, while ENT has a wider market. However, if OPC is available, some factors should be considered: (a) a worldwide economic comparison is difficult to make, as costs for patients may vary according to the health insurance system. A recent medico-economic USA analysis estimated that OPC is more cost effective despite a higher total life cost, based on a quality-adjusted life-year analysis [107, 108]. However, it should also be borne in mind that in the USA, the cost of ENT (four times a day) is estimated at US$141, and OPC at US$1875; (b) OPC offers a single daily administration, which could be convenient compared with taking ENT with each l-dopa dose, especially if a concomitant reduction in l-dopa doses is possible. At the same time, a triple l-dopa/carbidopa/ENT formulation is available in a single tab at variable doses, which could be particularly convenient for a fine adjustment of the dose of 25 mg of l-dopa. (c) Opicapone and ENT have similar efficacy on motor fluctuations as shown in the non-inferiority BIPARK I trial. At the same time, OPC has been shown to perform better vs ENT on the Clinician and Patients Global Impression of Change scale, and an additional benefit in off-reduction is obtained when switching from ENT to OPC. (d) No severe diarrhea and the lowest rate of urine discoloration or none at all were reported with OPC treatment compared to ENT. Urine discoloration is a harmless AE, although it is sometime perceived as bothersome by patients. In addition, no studies on OPC non-responders have been published so far and we do not currently know the percentage of patients with PD who may not benefit from its initiation. Further treatment strategies should be developed for COMT-Is non-responders, and the role of new ER l-dopa formulations should also be considered.
(c) How to manage potential TEAEs?
The first rule that should be adopted when prescribing COMT-I is caution in terms of selecting the right patient profile and knowing the most common AEs. Physicians should carefully monitor the incidence of LIDs, which are the most common dopaminergic AEs for all three COMT-Is and may require a LEED reduction to improve patients’ adherence to treatment. However, if OPC 50 mg has the desired effect on on-time without bothersome LIDs, according to pooled data of DB and OL extension trials, an increment of approximately 64 minutes can be expected vs PLC (without increment of on-time with bothersome LIDs). These data on OPC simply confirm the possibility to manage LIDs appropriately, even during COMT-I treatment. Additionally, the availability of several intermediate doses of l-dopa/carbidopa/ENT simplifies a fine dose adjustment.
Constipation, nausea, dizziness, hallucinations, and weight loss probably related to LIDs or disease progression, may also be most common among elderly patients, compared with patients aged younger than 70 years, as reported for OPC [12]. Of note, one of the main concerns related to DAs, especially among young patients with PD, is impulse control disorder. However, there were no particular impulse control disorder issues with any of the three COMT-Is, except for a low rate of approximately 0.2–05% with OPC treatment. The recent approval of OPC and its availability on the market have stimulated the possibility for further clinical research, which implies the use of COMT-Is to better exploit their effects and explore some aspects that might deserve clarification.
From a clinical research point of view, the main key points are:
(a) The role of COMT-Is in patients with stable non-fluctuating PD
From a clinical standpoint, there are two potential goals for early use of COMT-Is: (a) to improve motor symptoms and stabilize the disease and (b) to delay the appearance of l-dopa-induced motor complications. While the STRIDE-PD study has clearly shown how multiple daily ENT doses failed to prevent the appearance of dyskinesia in stable early PD, a motor benefit, manifested by an improvement in activities of daily living has been shown with early use of TOL and ENT (FIRST-STEP study) [57]. The same motor improvement can be expected with OCP. Concerning the delay in the appearance of motor complications, some authors have suggested that it might be interesting to verify whether a daily administration of OCP could promote a continuous dopaminergic stimulation, smoothing out the peaks and troughs of l-dopa delivery and the pulsatile stimulation of post-synaptic dopamine receptors [109, 110]. This hypothesis should be verified. With regard to this, the EPSILON study that aims to investigate the motor effects of OPC 50 mg in patients with early non-fluctuating PD, is currently underway. Particular attention should be paid to the dose of concomitant l-dopa treatment and a decrement should be considered. In fact, in the STRIDE-PD study, a significantly higher LEDD was noted in the l-dopa/ENT arm (659 mg) compared with the l-dopa alone arm (535 mg), which consequently resulted in higher percentages of LIDs.
(b) The role of COMT-Is in NMS and NMS Fluctuations
We can safely conclude that the data on NMS and COMT-Is are scarce, and often not assessed by specific NMS questionnaires. The role of OPC on pain and sleep is currently under investigation in phase IV trials, based on the benefit observed in the BIPARK trials. Considering the role of COMT-Is in treating motor fluctuations, a benefit could also be expected for non-motor fluctuations. Non-motor fluctuations are often underestimated, although they occur alongside motor fluctuations and less frequently, even in the absence of motor off-time, in 17–100% of patients with PD according to different studies [111]. Sensory (diffuse pain, neuralgic pain, dysesthesia, akathisia, burning sensation, sensation of dyspnea, and restless legs) and behavioral non-motor (depression, apathy, fatigue, anxiety, attacks of pain, attention disorders, hallucinations, irritability, and drowsiness) fluctuations may be more bothersome than cardinal parkinsonian motor symptoms. A potential role of COMT-I treatment in patients with PD with both motor and non-motor fluctuations would be worth exploring.
(c) The usefulness of COMT-Is as a first-line treatment in early fluctuators
So far, there is no evidence to support the use of COMT-Is as a first-line treatment for motor fluctuations compared to other add-on therapies, nor for its use as soon as motor fluctuations start. According to a personalized medicine approach, instead of conducting a head-to-head trial to compare the effectiveness of each COMT-I vs each DA or rasagiline/safinamide, a long-term observational study aimed at determining the best clinical profile for each add-on l-dopa therapy could be helpful in choosing the best prescription, according to the patient’s preference and the safety profile. Concerning the early use of COMT-Is in early-mid fluctuators, we only have data on OPC that could support its use, although they are based on exploratory post hoc analyses. In fact, when the efficacy of OPC 50 mg in patients with l-dopa-treated PD with motor fluctuation periods of 1 year (‘recent motor fluctuators’) or more than 1 year (“long-standing motor fluctuators”) is compared to Plc, it is significant and comparable in both arms in reducing off-time (−65.2 minutes [p = 0.00135] and −60.5 minutes [p = 0.0014], respectively, vs Plc) with a lower incidence of LIDs among patients with a shorter period (11.8%) of motor fluctuations compared to >1 year of fluctuations (23.5%), as expected [112].
(d) The role of COMT-Is in the management of patients with PD with device-aided treatments
As mentioned in the text, few reports on the co-administration of LCIG and COMT-Is (TOL, ENT, and OPC) have noted any success with this combination, which is aimed at improving the control of resistant motor fluctuations when there is a need to reduce the dose of l-dopa gel to prevent dopaminergic AEs. Moreover, there are no data on the efficacy and tolerability of concomitant administration of COMT-Is and other device-aided treatments, including CAI and DBS. It is well known that CAI is an effective treatment for l-dopa motor complications, but it can be less effective in terms of off-time reduction compared with LCIG and DBS [8]. A combination of COMT-Is, CAI, and an l-dopa subcutaneous liquid formulation could be interesting for patients who are not optimally treated for motor fluctuations and who are not suitable for or do not want to be submitted to DBS or LCIG. Moreover, we should consider that bothersome/severe and unpredictable motor fluctuations, and severe LIDs remain a clinically unmet need, with Level A evidence assigned only to DBS [113], but with no effective oral treatment available. At the same time, no RCTs on COMT-Is have specifically included/targeted patients with PD with unpredictable motor fluctuations or severe LIDs. The use of COMT-Is in combination with device-aided treatments for this subgroup of patients with advanced PD merits further investigation.
References
Dorsey ER, Bloem BR. The Parkinson pandemic: a call to action. JAMA Neurol. 2018;75(1):9–10.
LeWitt PA. Levodopa therapy for Parkinson’s disease: pharmacokinetics and pharmacodynamics. Move Disord. 2015;30(1):64–72.
Ray Chaudhuri K, Poewe W, Brooks D. Motor and nonmotor complications of levodopa: phenomenology, risk factors, and imaging features. Move Disord. 2018;33(6):909–19.
Rizos A, Martinez-Martin P, Odin P, Antonini A, Kessel B, Kozul TK, et al. Characterizing motor and non-motor aspects of early-morning off periods in Parkinson’s disease: an international multicenter study. Parkinsonism Relat Disord. 2014;20(11):1231–5.
Greig SL, McKeage K. Carbidopa/levodopa ER capsules (Rytary®, Numient™): a review in Parkinson’s disease. CNS Drugs. 2016;30(1):79–90.
Olanow CW, Poewe W, Rascol O, Stocchi F. On-demand therapy for OFF episodes in Parkinson’s disease. Move Disord. 2021;36(10):2243–53.
Dijk JM, Espay AJ, Katzenschlager R, de Bie RMA. The choice between advanced therapies for Parkinson’s disease patients: why, what, and when? J Parkinsons Dis. 2020;10(s1):S65-73.
Fabbri M, Rosa MM, Ferreira JJ. Adjunctive therapies in Parkinson’s disease: how to choose the best treatment strategy approach. Drugs Aging. 2018;35(12):1041–54.
Fox SH, Katzenschlager R, Lim SY, Barton B, de Bie RMA, Seppi K, et al. International Parkinson and Movement Disorder Society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s disease. Move Disord. 2018;33(8):1248–66.
Schrag A. Entacapone in the treatment of Parkinson’s disease. Lancet Neurol. 2005;4(6):366–70.
Li J, Lou Z, Liu X, Sun Y, Chen J. Efficacy and safety of adjuvant treatment with entacapone in advanced Parkinson’s disease with motor fluctuation: a systematic meta-analysis. Eur Neurol. 2017;78(3–4):143–53.
Fabbri M, Ferreira JJ, Lees A, Stocchi F, Poewe W, Tolosa E, et al. Opicapone for the treatment of Parkinson’s disease: a review of a new licensed medicine. Move Disord. 2018;33(10):1528–39.
Artusi CA, Sarro L, Imbalzano G, Fabbri M, Lopiano L. Safety and efficacy of tolcapone in Parkinson’s disease: systematic review. Eur J Clin Pharmacol. 2021;77(6):817–29.
Poewe W. The role of COMT inhibition in the treatment of Parkinson’s disease. Neurology. 2004;62(1 Suppl. 1):S31–8.
Ruottinen HM, Rinne UK. COMT inhibition in the treatment of Parkinson’s disease. J Neurol. 1998;245(11 Suppl. 3):P25-34.
Dingemanse J, Jorga K, Zürcher G, Fotteler B, Sedek G, Nielsen T, et al. Multiple-dose clinical pharmacology of the catechol-O-methyl-transferase inhibitor tolcapone in elderly subjects. Eur J Clin Pharmacol. 1996;50(1–2):47–55.
Kiss LE, Ferreira HS, Torrao L, Bonifacio MJ, Palma PN, Soares-da-Silva P, et al. Discovery of a long-acting, peripherally selective inhibitor of catechol-O-methyltransferase. J Med Chem. 2010;53(8):3396–411.
Palma N, Bonifacio MJ, Loureiro AI, Soares-Da-Silva P. Computation of binding affinity of catechol-O-methyltransferase-opicapone complexes. Parkinsonism Relat Disord. 2012;18:S125.
Bonifacio MJ, Torrao L, Loureiro AI, Palma PN, Wright LC, Soares-da-Silva P. Pharmacological profile of opicapone, a third-generation nitrocatechol catechol-O-methyl transferase inhibitor, in the rat. Br J Pharmacol. 2015;172(7):1739–52.
Bicker J, Alves G, Fortuna A, Soares-da-Silva P, Falcao A. A new PAMPA model using an in-house brain lipid extract for screening the blood-brain barrier permeability of drug candidates. Int J Pharm. 2016;501(1–2):102–11.
Truong DD. Tolcapone: review of its pharmacology and use as adjunctive therapy in patients with Parkinson’s disease. Clin Interv Aging. 2009;4:109–13.
Dingemanse J, Jorga K, Zürcher G, Schmitt M, Sedek G, Da Prada M, et al. Pharmacokinetic-pharmacodynamic interaction between the COMT inhibitor tolcapone and single-dose levodopa. Br J Clin Pharmacol. 1995;40(3):253–62.
Prada MBJ, Napolitano A. Improved therapy of Parkinson’s disease with tolcapone, a central and peripheral COMT inhibitor with an S-adenosyl-L-methionine-sparing effect. Clin Neuropharmacol. 1994;17:S26–37.
Sêdek G, Jorga K, Schmitt M, Burns RS, Leese P. Effect of tolcapone on plasma levodopa concentrations after coadministration with levodopa/carbidopa to healthy volunteers. Clin Neuropharmacol. 1997;20(6):531–41.
Keränen T, Gordin A, Karlsson M, Korpela K, Pentikäinen PJ, Rita H, et al. Inhibition of soluble catechol-O-methyltransferase and single-dose pharmacokinetics after oral and intravenous administration of entacapone. Eur J Clin Pharmacol. 1994;46(2):151–7.
Ruottinen HM, Rinne UK. A double-blind pharmacokinetic and clinical dose-response study of entacapone as an adjuvant to levodopa therapy in advanced Parkinson’s disease. Clin Neuropharmacol. 1996;19(4):283–96.
Wikberg T, Vuorela A, Ottoila P, Taskinen J. Identification of major metabolites of the catechol-O-methyltransferase inhibitor entacapone in rats and humans. Drug Metab Dispos. 1993;21(1):81–92.
Lyytinen J, Kaakkola S, Ahtila S, Tuomainen P, Teräväinen H. Simultaneous MAO-B and COMT inhibition in l-dopa-treated patients with Parkinson’s disease. Move Disord. 1997;12(4):497–505.
Nutt JG, Woodward WR, Beckner RM, Stone CK, Berggren K, Carter JH, et al. Effect of peripheral catechol-O-methyltransferase inhibition on the pharmacokinetics and pharmacodynamics of levodopa in parkinsonian patients. Neurology. 1994;44(5):913–9.
Ruottinen HM, Rinne UK. Entacapone prolongs levodopa response in a one month double blind study in parkinsonian patients with levodopa related fluctuations. J Neurol Neurosurg Psychiatry. 1996;60(1):36–40.
Loureiro A, Fernandes-Lopes C, Wright L, et al. Sulfation of opicapone, a nitrocatechol-type COMT inhibitor, by human recombinant SULTs and human S9 fraction. Abstract, XX World Congress on Parkinson’s Disease and Related Disorders 2013, Switzerland.
Almeida L, Rocha JF, Falcao A, Palma PN, Loureiro AI, Pinto R, et al. Pharmacokinetics, pharmacodynamics and tolerability of opicapone, a novel catechol-O-methyltransferase inhibitor, in healthy subjects: prediction of slow enzyme-inhibitor complex dissociation of a short-living and very long-acting inhibitor. Clin Pharmacokinet. 2013;52(2):139–51.
Santos AFA, Rocha J, Soares-Da-Silva P. Influence of food on opicapone pharmacokinetics and pharmacodynamics. Eur J Neurol. 2017;24(Suppl. 1):123–444.
Rocha JF, Falcao A, Santos A, Pinto R, Lopes N, Nunes T, et al. Effect of opicapone and entacapone upon levodopa pharmacokinetics during three daily levodopa administrations. Eur J Clin Pharmacol. 2014;70(9):1059–71.
Rocha JF, Falcao A, Lopes N, Pinto R, Santos A, Nunes T, et al. Opicapone effect on levodopa pharmacokinetics in comparison with placebo and entacapone when administered with immediate release 100/25 mg levodopa/carbidopa in healthy subjects. J Neurol. 2014;261:S119.
Falcão ASA, Ferreira JJ, Rocha J, Soares-Da-Silva P. Opicapone’s bedtime regimen and the decision-making process. Eur J Neurol. 2017;24.
Zürcher G, Da Prada M, Dingemanse J. Assessment of catechol-O-methyltransferase activity and its inhibition in erythrocytes of animals and humans. BMC. 1996;10(1):32–6.
Dingemanse J, Jorga KM, Schmitt M, Gieschke R, Fotteler B, Zürcher G, et al. Integrated pharmacokinetics and pharmacodynamics of the novel catechol-O-methyltransferase inhibitor tolcapone during first administration to humans. Clin Pharmacol Ther. 1995;57(5):508–17.
Jorga KM, Sedek G, Fotteler B, Zürcher G, Nielsen T, Aitken JW. Optimizing levodopa pharmacokinetics with multiple tolcapone doses in the elderly. Clin Pharmacol Ther. 1997;62(3):300–10.
Ruottinen HM, Rinne UK. Effect of one month’s treatment with peripherally acting catechol-O-methyltransferase inhibitor, entacapone, on pharmacokinetics and motor response to levodopa in advanced parkinsonian patients. Clin Neuropharmacol. 1996;19(3):222–33.
Rocha JF, Almeida L, Falcao A, Palma PN, Loureiro AI, Pinto R, et al. Opicapone: a short lived and very long acting novel catechol-O-methyltransferase inhibitor following multiple dose administration in healthy subjects. Br J Clin Pharmacol. 2013;76(5):763–75.
Ferreira JJ, Rocha JF, Falcao A, Santos A, Pinto R, Nunes T, et al. Effects of opicapone on levodopa pharmacokinetics, catechol-O-methyltransferase activity and motor fluctuations in patients with Parkinson's disease. Eur J Neurol. 2015;22(5):815–25e56.
Ferreira JJ, Lees A, Rocha JF, Poewe W, Rascol O, Soares-da-Silva P. Opicapone as an adjunct to levodopa in patients with Parkinson’s disease and end-of-dose motor fluctuations: a randomised, double-blind, controlled trial. Lancet Neurol. 2016;15(2):154–65.
Factor SA, Molho ES, Feustel PJ, Brown DL, Evans SM. Long-term comparative experience with tolcapone and entacapone in advanced Parkinson’s disease. Clin Neuropharmacol. 2001;24(5):295–9.
Koller W, Lees A, Doder M, Hely M. Randomized trial of tolcapone versus pergolide as add-on to levodopa therapy in Parkinson’s disease patients with motor fluctuations. Move Disord. 2001;16(5):858–66.
Efficacy and tolerability of tolcapone compared with bromocriptine in levodopa-treated parkinsonian patients. Tolcapone Study Group. Move Disord. 1999;14(1):38–44.
Stowe R, Ives N, Clarke CE, Deane K, Wheatley K, Gray R, et al. Evaluation of the efficacy and safety of adjuvant treatment to levodopa therapy in Parkinson's disease patients with motor complications. Cochrane Database Syst Rev. 2010;7:CD007166.
Poewe WH, Deuschl G, Gordin A, Kultalahti ER, Leinonen M. Efficacy and safety of entacapone in Parkinson’s disease patients with suboptimal levodopa response: a 6-month randomized placebo-controlled double-blind study in Germany and Austria (Celomen study). Acta Neurol Scand. 2002;105(4):245–55.
Piccini P, Brooks DJ, Korpela K, Pavese N, Karlsson M, Gordin A. The catechol-O-methyltransferase (COMT) inhibitor entacapone enhances the pharmacokinetic and clinical response to Sinemet CR in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2000;68(5):589–94.
Lees AJ, Ferreira J, Rascol O, Poewe W, Rocha JF, McCrory M, et al. Opicapone as adjunct to levodopa therapy in patients with Parkinson disease and motor fluctuations: a randomized clinical trial. JAMA Neurol. 2017;74(2):197–206.
Takeda A, Takahashi R, Tsuboi Y, Nomoto M, Maeda T, Nishimura A, et al. Randomized, controlled study of opicapone in Japanese Parkinson’s patients with motor fluctuations. Move Disord. 2021;36(2):415–23.
Ferreira JJ, Lees A, Rocha JF, Poewe W, Rascol O, Soares-da-Silva P. Long-term efficacy of opicapone in fluctuating Parkinson’s disease patients: a pooled analysis of data from two phase 3 clinical trials and their open-label extensions. Eur J Neurol. 2019;26(7):953–60.
Ferreira JJ, Lees AJ, Poewe W, Rascol O, Rocha JF, Keller B, et al. Effectiveness of opicapone and switching from entacapone in fluctuating Parkinson disease. Neurology. 2018;90(21):e1849–57.
Takeda ATR, Tsuboi Y, Nomoto M, Maeda T, Nishimura A, Hattori N. An open-label, 1-year extension clinical study in Japan of opicapone treatment for Parkinson’s disease: comfort-PD study part 2. Move Disord. 2019;34(S2).
Stocchi F, Rascol O, Kieburtz K, Poewe W, Jankovic J, Tolosa E, et al. Initiating levodopa/carbidopa therapy with and without entacapone in early Parkinson disease: the STRIDE-PD study. Ann Neurol. 2010;68(1):18–27.
Warren Olanow C, Kieburtz K, Rascol O, Poewe W, Schapira AH, Emre M, et al. Factors predictive of the development of levodopa-induced dyskinesia and wearing-off in Parkinson’s disease. Move Disord. 2013;28(8):1064–71.
Hauser RA, Panisset M, Abbruzzese G, Mancione L, Dronamraju N, Kakarieka A. Double-blind trial of levodopa/carbidopa/entacapone versus levodopa/carbidopa in early Parkinson’s disease. Move Disord. 2009;24(4):541–50.
Velseboer DC, Broeders M, Post B, van Geloven N, Speelman JD, Schmand B, et al. Prognostic factors of motor impairment, disability, and quality of life in newly diagnosed PD. Neurology. 2013;80(7):627–33.
Schrag A, Dodel R, Spottke A, Bornschein B, Siebert U, Quinn NP. Rate of clinical progression in Parkinson’s disease: a prospective study. Move Disord. 2007;22(7):938–45.
Fabbri M, Coelho M, Abreu D, Guedes LC, Rosa MM, Godinho C, et al. Dysphagia predicts poor outcome in late-stage Parkinson’s disease. Parkinsonism Relat Disord. 2019;64:73–81.
Schrag A, Sampaio C, Counsell N, Poewe W. Minimal clinically important change on the unified Parkinson’s disease rating scale. Move Disord. 2006;21(8):1200–7.
Waters CH, Kurth M, Bailey P, Shulman LM, LeWitt P, Dorflinger E, et al. Tolcapone in stable Parkinson’s disease: efficacy and safety of long-term treatment. Tolcapone Stable Study Group. Neurology. 1998;50(5 Suppl. 5):S39-45.
Onofrj M, Thomas A, Iacono D, Di Iorio A, Bonanni L. Switch-over from tolcapone to entacapone in severe Parkinson’s disease patients. Eur Neurol. 2001;46(1):11–6.
Entacapone to tolcapone switch. Multicenter double-blind, randomized, active-controlled trial in advanced Parkinson’s disease. Move Disord. 2007;22(1):14–9.
Larsen JP, Worm-Petersen J, Sidén A, Gordin A, Reinikainen K, Leinonen M. The tolerability and efficacy of entacapone over 3 years in patients with Parkinson’s disease. Eur J Neurol. 2003;10(2):137–46.
Hauser RRO, Poewe W, Ferreira JJ, Lees A, Klepitskaya G, Liang G, et al. Opicapone as a levodopa sparing agent: pooled analysis of BIPARK-I and II double-blind trials. Move Disord. 2019;34(Suppl. S2):S46.
Adler CH, Singer C, O'Brien C, Hauser RA, Lew MF, Marek KL, et al. Randomized, placebo-controlled study of tolcapone in patients with fluctuating Parkinson disease treated with levodopa-carbidopa. Tolcapone Fluctuator Study Group III. Arch Neurol. 1998;55(8):1089–95.
Welsh MD, Dorflinger E, Chernik D, Waters C. Illness impact and adjustment to Parkinson’s disease: before and after treatment with tolcapone. Move Disord. 2000;15(3):497–502.
Baas H, Beiske AG, Ghika J, Jackson M, Oertel WH, Poewe W, et al. Catechol-O-methyltransferase inhibition with tolcapone reduces the “wearing off” phenomenon and levodopa requirements in fluctuating parkinsonian patients. J Neurol Neurosurg Psychiatry. 1997;63(4):421–8.
Reichmann H, Boas J, Macmahon D, Myllyla V, Hakala A, Reinikainen K. Efficacy of combining levodopa with entacapone on quality of life and activities of daily living in patients experiencing wearing-off type fluctuations. Acta Neurol Scand. 2005;111(1):21–8.
Fénelon G, Giménez-Roldán S, Montastruc JL, Bermejo F, Durif F, Bourdeix I, et al. Efficacy and tolerability of entacapone in patients with Parkinson’s disease treated with levodopa plus a dopamine agonist and experiencing wearing-off motor fluctuations: a randomized, double-blind, multicentre study. J Neural Transm (Vienna). 2003;110(3):239–51.
Grandas F, Hernandez B. Long-term effectiveness and quality of life improvement in entacapone-treated Parkinson’s disease patients: the effects of an early therapeutic intervention. Eur J Neurol. 2007;14(3):282–9.
Gershanik O, Emre M, Bernhard G, Sauer D. Efficacy and safety of levodopa with entacapone in Parkinson’s disease patients suboptimally controlled with levodopa alone, in daily clinical practice: an international, multicentre, open-label study. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(6):963–71.
Durif F, Devaux I, Pere JJ, Delumeau JC, Bourdeix I. Efficacy and tolerability of entacapone as adjunctive therapy to levodopa in patients with Parkinson’s disease and end-of-dose deterioration in daily medical practice: an open, multicenter study. Eur Neurol. 2001;45(2):111–8.
Reichmann H, Lees A, Rocha JF, Magalhães D, Soares-da-Silva P. Effectiveness and safety of opicapone in Parkinson’s disease patients with motor fluctuations: the OPTIPARK open-label study. Transl Neurodegener. 2020;9(1):9.
Schapira AHV, Chaudhuri KR, Jenner P. Non-motor features of Parkinson disease. Nat Rev Neurosci. 2017;18(7):435–50.
Müller T. Tolcapone addition improves Parkinson’s disease associated nonmotor symptoms. Ther Adv Neurol Disord. 2014;7(2):77–82.
Ebersbach G, Hahn K, Lorrain M, Storch A. Tolcapone improves sleep in patients with advanced Parkinson's disease (PD). Arch Gerontol Geriatr. 2010;51(3):e125–8.
Gasparini M, Fabrizio E, Bonifati V, Meco G. Cognitive improvement during tolcapone treatment in Parkinson’s disease. J Neural Transm (Vienna). 1997;104(8–9):887–94.
Oliveira C, Lees A, Ferreira J, Lopes N, Costa R, Pinto R, et al. Evaluation of non-motor symptoms in opicapone treated Parkinson’s disease patients: results from a double-blind, randomized, placebo-controlled study and open-label extension. Eur J Neurol. 2015;22:191.
Hernán MA, Checkoway H, O’Brien R, Costa-Mallen P, De Vivo I, Colditz GA, et al. MAOB intron 13 and COMT codon 158 polymorphisms, cigarette smoking, and the risk of PD. Neurology. 2002;58(9):1381–7.
Corvol JC, Bonnet C, Charbonnier-Beaupel F, Bonnet AM, Fiévet MH, Bellanger A, et al. The COMT Val158Met polymorphism affects the response to entacapone in Parkinson’s disease: a randomized crossover clinical trial. Ann Neurol. 2011;69(1):111–8.
Olanow CW, Kieburtz K, Odin P, Espay AJ, Standaert DG, Fernandez HH, et al. Continuous intrajejunal infusion of levodopa-carbidopa intestinal gel for patients with advanced Parkinson’s disease: a randomised, controlled, double-blind, double-dummy study. Lancet Neurol. 2014;13(2):141–9.
Nyholm D, Johansson A, Lennernäs H, Askmark H. Levodopa infusion combined with entacapone or tolcapone in Parkinson disease: a pilot trial. Eur J Neurol. 2012;19(6):820–6.
Senek M, Nyholm D, Nielsen EI. Population pharmacokinetics of levodopa gel infusion in Parkinson’s disease: effects of entacapone infusion and genetic polymorphism. Sci Rep. 2020;10(1):18057.
Öthman M, Widman E, Nygren I, Nyholm D. Initial experience of the levodopa-entacapone-carbidopa intestinal gel in clinical practice. J Pers Med. 2021;11(4):254.
Schröter N, Ahrendt S, Hager A, Rijntjes M. Addition of tolcapone in intrajejunal levodopa infusion therapy requires a pronounced cost reduction. Move Disord. 2020;7(7):854–6.
Leta V, van Wamelen DJ, Sauerbier A, Jones S, Parry M, Rizos A, et al. Opicapone and levodopa-carbidopa intestinal gel infusion: the way forward towards cost savings for healthcare systems? J Parkinsons Dis. 2020;10(4):1535–9.
Giladi N, Gurevich T, Djaldetti R, Adar L, Case R, Leibman-Barak S, et al. ND0612 (levodopa/carbidopa for subcutaneous infusion) in patients with Parkinson’s disease and motor response fluctuations: a randomized, placebo-controlled phase 2 study. Parkinsonism Relat Disord. 2021;91:139–45.
Assal F, Spahr L, Hadengue A, Rubbia-Brandt L, Burkhard PR. Tolcapone and fulminant hepatitis. Lancet. 1998;352(9132):958.
Olanow CW. Tolcapone and hepatotoxic effects. Tasmar Advisory Panel Arch Neurol. 2000;57(2):263–7.
Olanow CW, Watkins PB. Tolcapone: an efficacy and safety review (2007). Clin Neuropharmacol. 2007;30(5):287–94.
Entacapone improves motor fluctuations in levodopa-treated Parkinson's disease patients. Parkinson Study Group. Ann Neurol. 1997;42(5):747–55.
Rinne UK, Larsen JP, Siden A, Worm-Petersen J. Entacapone enhances the response to levodopa in parkinsonian patients with motor fluctuations. Nomecomt Study Group. Neurology. 1998;51(5):1309–14.
Brooks DJ, Sagar H, Group UK-IES. Entacapone is beneficial in both fluctuating and non-fluctuating patients with Parkinson's disease: a randomised, placebo controlled, double blind, six month study. J Neurol Neurosurg Psychiatry. 2003;74(8):1071–9.
Myllyla VV, Kultalahti ER, Haapaniemi H, Leinonen M, Group FS. Twelve-month safety of entacapone in patients with Parkinson's disease. Eur J Neurol. 2001;8(1):53–60.
Liao X, Wu N, Liu D, Shuai B, Li S, Li K. Levodopa/carbidopa/entacapone for the treatment of early Parkinson’s disease: a meta-analysis. Neurol Sci. 2020;41(8):2045–54.
Haapaniemi HRK, Leinonen M. Tolerability and safety of entacapone in the treatment of Parkinson’s disease. Parkinsonism Relat Disord. 2000;7(Suppl. 1):S57.
Castro Caldas A, Teodoro T, Ferreira JJ. The launch of opicapone for Parkinson’s disease: negatives versus positives. Expert Opin Drug Saf. 2018;17(3):331–7.
Lees A, Ferreira JJ, Rocha JF, Rascol O, Poewe W, Gama H, et al. Safety profile of opicapone in the management of Parkinson’s disease. J Parkinsons Dis. 2019;9(4):733–40.
Lees ARH, Rocha JF, Magalhães D, Soares-da-Silva P. Onset of drug-related adverse events in Parkinson’s disease patients with motor fluctuations treated with opicapone in clinical practice: OPTIPARK post-hoc analysis. Mov Disord. 2020;35.
Hauser RA, Hsu A, Kell S, Espay AJ, Sethi K, Stacy M, et al. Extended-release carbidopa-levodopa (IPX066) compared with immediate-release carbidopa-levodopa in patients with Parkinson’s disease and motor fluctuations: a phase 3 randomised, double-blind trial. Lancet Neurol. 2013;12(4):346–56.
Deuschl G, Vaitkus A, Fox GC, Roscher T, Schremmer D, Gordin A. Efficacy and tolerability of entacapone versus cabergoline in parkinsonian patients suffering from wearing-off. Move Disord. 2007;22(11):1550–5.
Stocchi F, Hsu A, Khanna S, Ellenbogen A, Mahler A, Liang G, et al. Comparison of IPX066 with carbidopa-levodopa plus entacapone in advanced PD patients. Parkinsonism Relat Disord. 2014;20(12):1335–40.
Ferreira JJLA, Poewe P, Rascol O, Santos A, Magalhães D, Rocha JF, Soares-da-Silva P. Switching entacapone ‘non-responders’ to open-label opicapone: change in absolute OFF-time following the 1-year extension BIPARKI study. Move Disord. 2019;34(Suppl. S2):S1–937.
Hauser RALM, Videnovic A, Poewe Q, Rascol O, Ferreira JJ, Liang GS, et al. Effects of once-daily opicapone on duration of overnight OFF and time to morning ON in patients with Parkinson’s disease and motor fluctuations. Ann Neurol. 2020;88(Suppl 25): S189.
Videnovic APW, Lees A, Ferreira JJ, Klepitskaya O, Loureiro R, Magalhães D, et al. Effect of opicapone and entacapone on early morning-OFF pattern in Parkinson’s disease patients with motor fluctuations. Move Disord. 2020;34(Suppl. S2):S486.
Hansen RN, Suh K, Serbin M, Yonan C, Sullivan SD. Cost-effectiveness of opicapone and entacapone in reducing OFF-time in Parkinson’s disease patients treated with levodopa/carbidopa. J Med Econ. 2021;24(1):563–9.
Jenner P, McCreary AC, Scheller DK. Continuous drug delivery in early- and late-stage Parkinson’s disease as a strategy for avoiding dyskinesia induction and expression. J Neural Transm (Vienna). 2011;118(12):1691–702.
Jenner P, Rocha JF, Ferreira JJ, Rascol O, Soares-da-Silva P. Redefining the strategy for the use of COMT inhibitors in Parkinson’s disease: the role of opicapone. Expert Rev Neurother. 2021;21(9):1019–33.
Martínez-Fernández R, Schmitt E, Martinez-Martin P, Krack P. The hidden sister of motor fluctuations in Parkinson’s disease: a review on nonmotor fluctuations. Move Disord. 2016;31(8):1080–94.
Ebersbach GRO, Ferreira J, Costa R, Rocha JF, Magalhães D, Soares-da-Silva P. Efficacy and safety of opicapone in Parkinson’s disease patients according to duration of motor fluctuations: post-hoc analysis of BIPARK-I and II. Move Disord. 2020;35(Suppl. 1):35.
Ferreira JJ, Katzenschlager R, Bloem BR, Bonuccelli U, Burn D, Deuschl G, et al. Summary of the recommendations of the EFNS/MDS-ES review on therapeutic management of Parkinson’s disease. Eur J Neurol. 2013;20(1):5–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No specific funding was received for this work.
Conflicts of interest
Margherita Fabbri declares the following conflicts of interest: honoraria to speak: BIAL and AbbVie. Joaquim J. Ferreira declares the following conflicts of interest: consultancy for BIAL and principal investigator of the BIPARK I study; stock ownership in medically related fields: none; consultancies: Ipsen, GlaxoSmithKline, Novartis, Teva, Lundbeck, Solvay, Abbott, Merck-Serono, and Merz; advisory boards: none; partnership: none; honoraria to speak: none; grants: GlaxoSmithKline, Grunenthal, Teva, and Fundação MSD. Olivier Rascol declares the following conflicts of interest: advisory board and consultancy: BIAL; advisory boards and consultancy: AbbVie, Adamas, Acorda, Addex, AlzProtect, Apopharma, Astrazeneca, Axovant, Biogen, Britannia, Buckwang, Cerespir, Clevexel, Denali, INC Reasearch, Lundbeck, Lupin, Merck, MundiPharma, Neuratris, Neuroderm, Novartis, ONO Pharma, Osmotica, Parexel, Pfizer, Prexton Therapeutics, Quintiles, Roche, Sanofi, Servier, Sunovion, Théranexus, Takeda, Teva, UCB, Vectura, Watermark Research, XenoPort, XO, and Zambon; grant: Agence Nationale de la Recherche (ANR), CHU de Toulouse, France-Parkinson, INSERM-DHOS Recherche Clinique Translationnelle, MJFox Foundation, Programme Hospitalier de Recherche Clinique, European Commission (FP7, H2020), and Cure Parkinson IK; other: grant to participate in a symposium and contribute to the review of an IPMDS article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
All co-authors have been substantially involved in the preparation of the manuscript; all the co-authors have also seen and approved the final submitted version and agreed to be accountable for the work. 1. Research project: A. Conception, B. Organization, C. Execution; 2. Statistical Analysis: A. Design, B. Execution, C. Review and Critique; 3. Manuscript Preparation: A. Writing of the first draft, B. Review and Critique. MF: 1A, 1B, 1C, 3A; JJF: 1A, 1B, 3B; OR: 1A, 2A, 3B.
Rights and permissions
About this article
Cite this article
Fabbri, M., Ferreira, J.J. & Rascol, O. COMT Inhibitors in the Management of Parkinson’s Disease. CNS Drugs 36, 261–282 (2022). https://doi.org/10.1007/s40263-021-00888-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-021-00888-9