Abstract
Background and objectives
Opicapone is a novel third generation catechol-O-methyltransferase (COMT) inhibitor. The purpose of this study was to compare the levodopa pharmacokinetic profile throughout a day driven by the COMT inhibition either following repeated doses of opicapone or concomitant administration with entacapone.
Methods
A randomized, double-blind, gender-balanced, parallel-group study was performed in 4 groups of 20 healthy subjects each. Four subjects in each group received placebo during the entire study. Sixteen subjects in one group received placebo once daily for 11 days and on day 12, 200 mg entacapone concomitantly with each levodopa/carbidopa dose (three times separated by a 5-h interval). Sixteen subjects in each of the remaining three groups received respectively 25, 50, and 75 mg opicapone once daily for 11 days and on day 12, placebo concomitantly with each levodopa/carbidopa dose.
Results
Levodopa minimum plasma concentration (Cmin) for each levodopa/carbidopa dose and for the mean of all levodopa/carbidopa doses increased substantially with all active treatments (entacapone and opicapone) when compared to the control group (placebo), with values ranging from 1.7-fold (200 mg entacapone) to 3.3-fold (75 mg opicapone). No statistical difference was found for levodopa peak of systemic exposure (as assessed by maximum observed plasma concentration (Cmax)) between all active treatments and placebo. A significant increase in the levodopa extent of systemic exposure (as assessed by concentration-time curve (AUC)) occurred with all opicapone treatments in relation to placebo. No statistical difference was found for levodopa AUC when entacapone was compared to placebo. When compared to entacapone, both 50 and 75 mg opicapone presented a significant increase for the levodopa AUC. All active treatments significantly inhibited both peak (as assessed by Emax) and extent (as assessed by effect-time curve (AUEC)) of the COMT activity in relation to placebo. When compared to entacapone, all opicapone treatments significantly decreased the extent (AUEC) of the COMT activity due to a long-lasting and sustained effect. The tolerability profile was favorable for all active treatments.
Conclusion
Opicapone, a novel third generation COMT inhibitor, when compared to entacapone, provides a superior response upon the bioavailability of levodopa associated to more pronounced, long-lasting, and sustained COMT inhibition. The tolerability profile was favorable. On the basis of the results presented in this study and along with the earlier pharmacology studies, it is anticipated that opicapone adjunct therapy at the dosages of 25 and 50 mg will provide an enhancement in levodopa availability that will translate into clinical benefit for Parkinson’s disease patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite decades of clinical use, levodopa still remains the most effective symptomatic treatment in Parkinson’s disease (PD) [1, 2]. The therapeutic effect of levodopa (l-DOPA) depends on its biotransformation to dopamine in the brain. However, levodopa undergoes rapid and extensive metabolization by peripheral aromatic l-amino acid decarboxylase (AADC) and catechol-O-methyltransferase (COMT), and only 1 % of an oral dose of levodopa actually reaches the brain [3, 4]. Therefore, levodopa is usually co-administered with an AADC inhibitor (carbidopa or benserazide), which increases levodopa bioavailability, but still, approximately 90 % of a levodopa dose is converted by COMT to 3-O-methyldopa, which competes with levodopa at the level of the blood-brain barrier for transport [5–8]. Thus, an additional strategy to further inhibit peripheral levodopa metabolism and increase the delivery of levodopa to the brain is the administration of a COMT inhibitor [9, 10]. Only two COMT inhibitors (tolcapone and entacapone) are currently available for clinical use, and both have some clinical limitations. The use of tolcapone requires liver function monitoring and thus is limited to fluctuating patients poorly controlled with other therapies [11]. Entacapone (ENT) is considered to be safe [12], but its efficacy is limited and requires frequent dosing [3]. Therefore, there is a need for more efficacious and safer COMT inhibitors.
Opicapone (2,5-dichloro-3-[5-(3,4-dihydroxy-5-nitrophenyl]-1,2,4-oxadiazol-3-yl)-4,6-dimethylpyridine 1-oxide, also known as BIA 9-1067) is a novel third generation COMT inhibitor currently under phase III clinical trials by BIAL—Portela & Cª, S.A. (S. Mamede do Coronado, Portugal) for use as adjunctive therapy in levodopa-treated PD patients. Opicapone (OPC) was designed as a hydrophilic 1,2,4-oxadiazole analogue with a pyridine N-oxide residue at position 3 to provide high COMT inhibitory potency and avoid cell toxicity [13]. OPC is endowed with an exceptionally high-binding affinity (sub-picomolar K d) [14] that translates into a slow complex dissociation rate constant and a long duration of action in vivo [15, 16]. In the liver and brain homogenates from rats administered with OPC, tolcapone, and ENT by gastric tube, OPC showed to have a stronger and more sustained COMT inhibitory effect than the comparing COMT inhibitors tolcapone and ENT. One hour after administration, COMT inhibition was 99 % with OPC versus 82 % with tolcapone and 68 % with ENT. Nine hours after administration, ENT showed no COMT inhibition and tolcapone produced minimal inhibitory effect (16 %), whereas OPC continued to inhibit COMT activity by 91 % [15]. OPC was well tolerated in studies in several animal species (data on file—BIAL—Portela & Cª, S.A.).
In an entry-into-man study in healthy male volunteers, single doses of OPC ranging from 10 to 1,200 mg were well tolerated. The adverse event (AE) profile did not differ from that of placebo (PLC), and the clinical safety tests showed no sign of concern. The extent of systemic exposure to OPC increased in an approximately dose-proportional manner, and despite the short half-life (t1/2) (0.8 to 3.2 h), a dose-dependent and long-lasting COMT inhibitory effect was observed with a maximum S-COMT inhibition (Emax) ranging from 34.5 % (10 mg) to 100 % (1,200 mg), and an inhibition of 25.1 to 76.5 % remained 24-h post-dose [17, 18]. Following once-daily multiple doses up to 30 mg OPC, sulfation was the main metabolic pathway and the bile is likely the main route of excretion. Maximum S-COMT inhibition (Emax) ranged from 69.9 to 98.0 % following the last dose of OPC [18]. In PD patients, OPC administered once daily markedly increased the extent of systemic exposure to levodopa, decreased exposure to 3-O-methyldopa (3-OMD), and decreased S-COMT activity. The study was not designed to detect any significant differences in motor performance, but exploratory analyses showed an improvement in various motor outcomes [19]. On basis of these promising results, it was decided to proceed to further clinical trials with OPC [20, 21].
Therefore, taking into account the PK/pharmacodynamic profiles of both ENT and OPC, and their effects on the PK of levodopa, it may be anticipated that the therapeutic regimen of levodopa could be enhanced and better optimized with OPC due to its higher, long-lasting, and sustained COMT inhibition, ensured by a once-daily regimen. Thus, the present study aimed to investigate the effect of once-daily 25, 50, and 75 mg OPC on the levodopa PK, in comparison to PLC and 200 mg ENT in healthy volunteers.
Methods
Study design
This was a randomized, double-blind, gender-balanced, placebo-controlled study (trial registration EudraCT No. 2011-000173-31) performed at SGS aster center (3-5 rue EugèneMillon, 75015 Paris, France) in 4 groups of 20 healthy subjects each (10 males and 10 females).
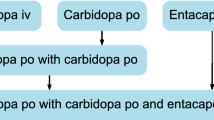
Eligible subjects were enrolled into one of the dosing groups. From the 20 healthy subjects per group, 4 received PLC during the entire study. Sixteen subjects in one of the groups received PLC once daily for 11 days, and on day 12, 200 mg ENT concomitantly with each levodopa/carbidopa (LC) dose (three times separated by a 5-h interval). Sixteen subjects in each of the remaining three groups received respectively 25, 50, and 75 mg OPC once daily for 11 days, and on day 12, PLC concomitantly with each LC dose.
The clinical part consisted of an ambulatory period of 11 days (from day 1 to day 11), during which subjects returned to the clinical unit every evening, followed by an institutionalization of 1.5 days from day 11 evening to day 13 morning (i.e., 14 h after the third and last administration of LC). The study medication was OPC (manufactured by BIAL—Portela & Cª, S.A.) administered as over-encapsulated capsules of 25 and 50 mg OPC, PLC (manufactured by BIAL—Portela & Cª, S.A.) as capsules, ENT (Comtan®, manufactured by Novartis Europharm Ltd.) as over-encapsulated tablets of 200 mg ENT, and LC (Sinemet®, manufactured by Merck Sharp & Dohme acquired as commercial product) as tablets of 100/25 mg LC. PLC capsules and over-encapsulated OPC capsules and ENT tablets were identical in terms of size, appearance, and taste.
Sample size estimation was based on a primary levodopa parameter (AUC0–∞). In a previous study [22], a within-subject variability (%CV) of 27.5 % was observed for levodopa AUC0–∞. Assuming an alpha error of 5 % (two-tailed) and an approximate inter-subject CV of 27.5 %, 72 subjects (18 subjects per treatment group) provided 80 % probability (power) to detect a 30 % difference in the geometric means of levodopa AUC0–∞. Taking into account 10 % of possible major protocol violators, 80 subjects were planned to be included to allow the completion of 72 subjects.
Potential subjects were screened for eligibility within 3 weeks of admission. Screening consisted of discussion of informed consent, medical history, physical examination, vital signs, 12-lead ECG, clinical laboratory tests (hematology, plasma biochemistry, coagulation, urinalysis, viral serology, drugs of abuse screen, and pregnancy test), and review of the selection criteria. Subjects were to be aged 18–45 years, within 18–30 kg/m2 of body mass index (BMI) and non-smokers or ex-smokers; women had to be not of childbearing potential by reason of surgery or postmenopausal for at least 1 year, or if of childbearing potential use double-barrier or intrauterine device pregnancy protection. No medication other than the study drugs or necessary for the treatment of AEs was allowed from the initial day of screening until final discharge.
On each evening from days 1 to 11, subjects were fasting of all food for a minimum of 2 h before dosing and remained fasted until 1-h post-dose. On day 12, subjects had an overnight fast for at least 8 h before the first LC administration and remained fasted until at least 2 h after the LC dose. Subjects were also fasting for at least 2 h before and after the second and third LC administrations. Water drinking was allowed as desired except for 1 h before and after dosing.
From 24 h before the admission day until the end of study, subjects were requested to abstain from smoking, drinking alcohol, coffee, tea, or beverages containing methylxanthines (theophylline, caffeine, or theobromine) and eating meals containing poppy seeds. The consumption of starfruit, grapefruit, or grapefruit juice was not allowed starting from 1 week before dosing until end of clinical part.
The study was conducted according to the Helsinki Declaration, ICH Good Clinical Practice recommendations, and applicable local regulations. The study was approved by an Independent Ethics Committee (CPP—Comité de Protection des Personnes, Ile-De-France VIII, Boulogne-Billancourt, France) and by the French Medicines Agency (AFSSAPS). Written informed consent was obtained for each study participant.
Safety assessments
Safety and tolerability assessments included routine laboratory test (blood chemistries, hematological profile, coagulation, and urinalysis), physical examination, ECG, and vital signs. Any undesirable sign, symptom, or medical condition occurring after starting the study, whether reported spontaneously or when prompted, was recorded regardless of suspected relation to the study medication.
Blood sampling and plasma drug assays
Blood samples (6 mL) for PK analyses of levodopa, its metabolite 3-OMD, carbidopa, and ENT were drawn by direct venipuncture or intravenous catheter into potassium ethylenediaminetetraacetic acid (EDTA) tubes, at the following time points on day 12: pre-first LC dose and then at 0.5, 1, 1.5, 2, 3, 4, and 5-h post-each LC dose, and additionally 8.0 and 14.0-h post-third LC dose. Blood samples collected at 5.0-h post-first and post-second LC dose were collected immediately before the subsequent LC administration. After collection, blood samples were centrifuged at approximately 1,500 g for 10 min at 4 °C, and the resulting plasma was then separated into four aliquots of 0.5 mL which were stored at −70 °C until required for analysis.
Blood sampling for S-COMT assay
Blood samples collected for PK assays on day 12 served for the pharmacodynamic assessments. A blood sample was also collected on days 1, 3, 5, 7, 9, and 11 and at the end-of-study (EOS) visit for evaluation of S-COMT activity. After centrifugation and removal of plasma, the supernatant (uppermost erythrocyte layer) was removed and the tubes containing the erythrocytes were placed in ice. Then, a volume of cold 0.9 % NaCl solution equal to double that of erythrocytes was added. The erythrocytes were centrifuged (at 4 °C and approximately 1,500 g for 10 min), and the washing procedure was repeated three times. Then, two accurately pipetted 500-mL aliquots of washed erythrocytes were prepared and stored at −70 °C until required for analysis.
Bioanalysis of analytes
The determination of the plasma concentrations of levodopa and 3-OMD was carried out in compliance with Good Laboratory Practice (GLP) at Nuvisan GmbH (Neu-Ulm, Germany) by liquid chromatography with electrochemical detection (HPLC-EC) using a validated method with a lower limit of quantification (LLOQ) of 25 ng/mL. The assay accuracy was between 99.3 and 100.8 % for levodopa and −100.7 and 100.9 % for 3-OMD; the precision (%CV) was between 3.4 and 6.9 % for levodopa and 5.8 and 8.0 % for 3-OMD.
The determination of the plasma concentrations of carbidopa was carried out in compliance with GLP at Nuvisan GmbH (Neu-Ulm, Germany) by liquid chromatography with tandem mass detection (MS/MS) using a validated method with a LLOQ of 2.5 ng/mL. The assay accuracy was between 95.9 and 97.7 %; the precision (%CV) was between 3.6 and 8.8 %.
The determination of the plasma concentrations of ENT was carried out in compliance with GLP at AlgorithmePharma Inc. (Laval, Quebec, Canada) by liquid chromatography with tandem mass detection (MS/MS) using a validated method with a LLOQ of 10.0 ng/mL. The assay accuracy was between 101.1 and 106.7 %; the precision (%CV) was between 2.1 and 7.3 %.
S-COMT assay
The determination of S-COMT activity was carried out in compliance with GLP at BIAL’s Pharmacological Laboratory (S. Mamede do Coronado, Portugal) according to a validated method [23, 24].
Analyses
Pharmacokinetic analysis
The PK parameters of ENT, carbidopa, levodopa, and 3-OMD were derived, where appropriate, from the individual plasma concentration-time profiles and included the minimum plasma concentration (Cmin) (only for levodopa), maximum observed plasma concentration (Cmax), time at which Cmax was observed (tmax), area under the plasma concentration-time curve (AUC) calculated using the trapezoidal method from zero to the last quantifiable drug concentration (AUC0–t) and from zero to infinity (AUC0–∞), the apparent clearance (CL/F), the apparent volume of distribution (V/F), and the apparent terminal half-life (t1/2). Summary statistics were prepared for each parameter. For levodopa and 3-OMD plasma, Cmax and AUC were compared between treatment groups using a one-way analysis of variance (ANOVA) with treatment as fixed effect. Point estimates (PEs) of the geometric mean ratios (GMR) and corresponding 90 % confidence intervals (90 % CI) for each parameter and for the ratios OPC/PLC, ENT/PLC, and OPC/ENT were presented and compared to (80–125 %) reference interval.
Pharmacodynamic analysis
The following pharmacodynamic parameters were derived from the individual S-COMT activity profiles: maximum inhibition of COMT activity post-dose (Emax), time to occurrence of Emax (tEmax), and area under the effect-time curve (AUEC).
The value observed before the first dose was taken as the baseline value (E0). From time plots of percentage COMT activity, relative to baseline, the maximum inhibition of COMT activity (Emax), and the time to its occurrence (tEmax) were directly read. The area under the effect-time curve (AUEC0–5) was calculated by linear-trapezoidal summation from the time of each levodopa dosing to 5-h post each corresponding levodopa dose taking E0 as the value at dosing time. The AUEC0–14 was calculated by linear-trapezoidal summation from the time of last levodopa dosing to 14-h post-levodopa dose taking E0 as the value at dosing time. AUEC0–all was calculated by summation of AUEC0–5 from first and second levodopa administration and AUEC0–14 from the last levodopa administration.
Descriptive statistics were prepared for each parameter. Emax and AUEC were compared between treatment groups using ANOVA with treatment as fixed effect. PEs of the arithmetic mean ratios (AMR) and corresponding 90 % CI for each parameter and for the ratios OPC/PLC, ENT/PLC, and OPC/ENT were presented and compared to (80–125 %) reference interval.
Adverse events
AEs were coded according to the Medical Dictionary for Regulatory Activities (MedDRA, version 14.0). For the laboratory safety data, clinically significantly abnormal values were considered as AEs.
Statistical analysis
The pharmacokinetic and pharmacodynamic parameters were calculated by using WinNonlin (version 5.2, Pharsight Co., Palo Alto, CA, USA). Statistical analysis used SAS software 9.2 release (SAS Institute Inc., Cary, NC, USA). Statistical tests were performed two-sided with the level of significance set at 5 %.
Results
Populations
A total of 80 subjects (40 males and 40 females) were enrolled, and 79 subjects completed the study. The mean age (range) was 29.8 years (20–45), height of 171.0 cm (154–197), and BMI of 23.5 kg/m2 (28.6–29.8) (Table 1). One subject (25 mg OPC group) withdrew the consent due to personal reasons (on day 10) and was not replaced. Therefore, all 80 subjects enrolled constituted the safety population set and the 79 subjects that completed the study constituted the PK population set.
Pharmacokinetics
Levodopa
Figure 1 displays the plasma levodopa concentration-time profiles on day 12 following administration of LC 100/25 mg three times per day (separated by 5 h) or concomitant administrations of 200 mg ENT or PLC with each LC dose; 3 of the 4 groups administered LC 100/25 mg plus PLC on day 12 were given once-daily oral administrations of 25, 50, and 75 mg OPC for 11 days (days 1 to 11). Table 2 presents the main PK parameters of plasma levodopa. The statistical comparisons of active groups (OPC or ENT) in relation to control group (PLC) and between active groups (OPC in relation to ENT) are presented in Table 3.
The levodopa Cmin for each LC dose and for the mean of all LC doses increased substantially with all active treatments (ENT and OPC groups) when compared to the control group (PLC) with values ranging from 1.7-fold (200 mg ENT) to 3.3-fold (75 mg OPC). Moreover, OPC was found to increase levodopa Cmin in a dose-dependent manner with values ranging from 2.5-fold to 3.2-fold and with all OPC groups showing a higher increase in relation to ENT (Table 4).
The levodopa Cmax was usually higher following OPC when compared to PLC, namely following the second and third LC doses with 50 and 75 mg OPC. Levodopa Cmax following ENT was similar and slightly lower (except for the third LC dose) when compared to PLC (Tables 2, 3, and 4). No statistical difference was found for levodopa Cmax between all active treatments (OPC and ENT) and PLC. However, a marked increase (>30 %) to levodopa Cmax occurred with 75 mg OPC following the second and third LC doses (Table 3).
The mean levodopa Cmax–Cmin was comparable between all active treatments (OPC and ENT) and PLC with a ratio versus PLC of 0.8 with 200 mg ENT and 0.9, 1.0, and 1.0 with 25, 50, and 75 mg OPC, respectively (Table 4).
All active treatments (ENT and OPC groups), in relation to the PLC group, presented a higher extent of exposure (AUC0–24) to levodopa following each and all LC doses (Table 2 and 3). A significant increase in the levodopa AUC occurred with all OPC dose groups in relation to PLC. PEs of GMR OPC/PLC ranged from 141.42 to 178.90 % with 25 and 75 mg OPC, respectively. The 90 % CI ranged from 104.08–192.14 to 132.32–241.86 %, respectively (Table 3). This is in correlation to the observed increase of approximately 1 h of the levodopa t1/2 with any OPC group when compared to the PLC group. No statistical difference was found for levodopa extent of exposure (as assessed by AUC) when ENT was compared to PLC. PE of the GMR ENT/PLC was 102.97 %, and the 90 % CI was 76.16–139.21 % (Table 3). When compared to ENT, both 50 and 75 mg OPC presented a statistical difference for the levodopa AUC increase (PE OPC/ENT [90 % CI] = 148.23 % [105.88–207.50 %]) with 50 mg OPC and 173.74 % [124.11–243.22 %] with 75 mg OPC) (Table 3).
3-OMD
Figure 2 displays the plasma 3-OMD concentration-time profiles, and Table 5 presents the PK parameters of plasma 3-OMD, following the administration of LC 100/25 mg three times per day (separated by 5 h) on day 12 and the once-daily oral administrations of 25, 50, and 75 mg OPC for 11 days (days 1 to 11) or the concomitantly administrations of 200 mg ENT or PLC with each LC dose. Statistical comparisons of active groups (OPC or ENT) in relation to PLC group and between active groups (OPC in relation to ENT) are presented in Table 6.
All active treatments (ENT and OPC groups), in relation to the PLC group, presented a significant decrease in extent of exposure (AUC0–24) to 3-OMD following each and all LC doses (Table 6). Furthermore, OPC decreased the peak (Cmax) and extent (AUC) of 3-OMD in a dose-dependent manner.
Carbidopa
All active treatments (ENT and OPC groups), in relation to the PLC group, presented a similar systemic exposure to carbidopa following each and all LC doses (data not shown).
Entacapone
Systemic exposure to ENT was comparable to its bioavailability described in literature following concomitant administration with 100/25 mg LC (mean Cmax was approximately 1,000 ng/mL, tmax of approximately 1.5 h, and a mean AUC0–t of approximately 1,600 ng h/mL) [25–27].
Pharmacodynamics
Figure 3a depicts S-COMT activity over time and on day 12. Table 7 presents the pharmacodynamic parameters of S-COMT. The statistical comparisons of active groups (OPC or ENT) in relation to PLC group and between active groups (OPC in relation to ENT) are presented in Table 8.
a Mean S-COMT activity (% of baseline) versus time on day 12 following once-daily oral administrations of 25, 50, and 75 mg OPC or PLC for 11 days (days 1 to 11) or co-administrations of 200 mg ENT or PLC with each LC dose (n = 16, n = 15 for 25 and 50 mg OPC). b Mean “trough” S-COMT activity (% of baseline) from days 1 to 11 and up to end-of-study visit (EOS) following once-daily oral administrations of 25, 50, and 75 mg OPC or PLC
A sustained inhibitory effect of OPC upon S-COMT activity was observed. From day 1 to the follow-up (FU) visit, the time to return to baseline enzyme activity with OPC was not possible to determine because at FU, there was still inhibition. However, the recovery tendency observed after day 11 suggests a full recovery of S-COMT activity of approximately 2 weeks in the conditions of this study (Fig. 3b).
On day 12, the time to return to baseline enzyme activity with 200 mg ENT was between 5 and 7 h. Contrary to ENT, OPC presented a long-lasting and sustained S-COMT inhibition and it was not possible to determine the exact time to return to baseline enzyme activity for all OPC doses because at 24-h post-dose (last time-point of the profile), there was still a marked inhibition. Maximum S-COMT inhibition (Emax) on day 12 occurred between 0.6 h (75 mg OPC) and 2.3 h (200 mg ENT) post-dose (tEmax), and ranged from 67.1 % (200 mg ENT) to 94.2 % (75 mg OPC) (Table 7). All active treatments (OPC and ENT groups) significantly inhibited both peak (as assessed by Emax) and extent (as assessed by AUEC) of S-COMT activity in relation to PLC (Tables 7 and 8). When compared to ENT, all OPC treatments significantly decreased the extent (AUEC) of S-COMT activity (Table 8). Peak and extent of S-COMT inhibition with OPC followed a dose-dependent manner although not proportional. In fact, in relation to PLC and taking the 50-mg OPC dose as reference, there was always a decrease difference from the 25 to 50 mg OPC higher than 10 %. Likewise, for the 50 to 75 mg OPC dosages, the decrease difference was always below than 4 % in both peak and extent of S-COMT inhibition.
Tolerability
The tolerability profile of all the treatments was favorable. Overall, a total of 94 AEs were reported by 41 (51.3 %) subjects. Among these, 93 AEs were considered treatment emergent (TEAEs). The majority of TEAEs were of mild intensity. Seventy-eight TEAEs experienced by 38 subjects were considered at least possibly related to the study products. Among these 78 TEAEs, the most frequent consisted in gastrointestinal disorders (52 TEAEs reported by 30 subjects) and nervous system disorders (17 TEAEs reported by 14 subjects), accounting for 88.5 % of the treatment-related TEAEs (69 out of 78). In the period from days 1 to 11, the frequency of AEs was low and similar between all OPC groups and PLC. On day 12, the day of LC administration in addition to PLC or ENT, nausea and vomiting were the most common reported treatment-related TEAEs, followed by headache and dizziness. Nausea was more common with OPC higher doses, affecting 18.8 % (n = 3), 43.8 % (n = 7), and 50 % (n = 8) of subjects taking 25, 50, and 75 mg OPC, respectively, compared to 31.3 % (n = 5) for ENT and 18.8 % (n = 3) for PLC groups. Vomiting was reported for 18.8 % (n = 3), 12.5 % (n = 2), and 18.8 % (n = 3) for 25, 50, and 75 mg OPC, compared to 6.3 % for ENT and PLC groups (n = 1, each). There were no severe or serious AEs reported during the study on randomized subjects. One SAE was reported by a screened subject before his randomization in the study. The relationship to the study medication was therefore completely excluded. No corrective treatment was given for treatment-related TEAEs. No AEs led to the discontinuation of the study treatment. Neither trends nor relevant changes from baseline were observed in vital signs, ECG parameters, physical examination, and in any laboratory parameters assessed.
Discussion
The purpose of this study was to compare the effectiveness of OPC versus ENT upon COMT activity and the pharmacokinetic profile of a typical scenario of three daily levodopa administrations. In the case of ENT, it was administered concomitantly with levodopa, whereas OPC was last administered 12 h before the first administration of levodopa under steady-state conditions for COMT inhibition, i.e., after 11 once-daily administrations [17].
In the present study, OPC was found to significantly increase the trough levels (Cmin) of levodopa and its systemic extent of exposure (AUC0–24). Even with a LC regimen of only three times daily at 5-h intervals, the reduced clearance (CL) and prolonged half-life (t1/2) of levodopa, with any OPC dose, resulted in a dose-dependent increase of levodopa “trough” levels (Cmin) of at least 2.5-fold (25 mg OPC). This cumulative effect, together with a presumed increased availability of levodopa for absorption, could have been responsible for the marked enhancement in the levodopa peak of exposure (Cmax) following OPC. Despite the well-known relatively large inter-individual variability in levodopa absorption [28], the gut and liver play a major role in the O-methylation of levodopa [26], and the high inhibitory pattern of both OPC and carbidopa may well have prevented the formation of 3-OMD and dopamine and as a consequence, to a levodopa Cmax increase. Although an increase in Cmax may enhance the risk of dyskinesia at peak dose and compromise tolerability [29], which deserves further evaluation, it was previously postulated that reduced motor complications are associated with avoiding low plasma levodopa trough levels and are not adversely affected by relatively high plasma levodopa concentrations [30].
In fact, motor complications are thought to be related to deficient dopaminergic stimulation in striatal dopamine receptors with consequent plastic changes in intracellular signals and neuronal firing patterns [30]. These changes are normally related to drugs, such as levodopa, with a relatively short half-life and low trough levels. Thus, OPC may enhance stable levodopa plasma concentrations, perceived a key factor in optimizing treatment response and reducing motor complications, as it increases levodopa trough levels (Cmin) with no impact on levodopa fluctuation (as assessed by Cmax–Cmin). Furthermore, it could be hypothesized that the therapeutic regimen of levodopa may even be optimized by reducing the levodopa/DDCI dose following the first morning dose in order to minimize the potential increase of Cmax and shortening the levodopa fluctuation (Cmax–Cmin) [31], which could have clinical benefits [32].
When compared to ENT, OPC provides a superior response in increasing the levodopa trough levels (Cmin) and extent of exposure (AUC0–24), accompanied by a prolonged half-life (t1/2), which is believed to be associated with its more pronounced, long-lasting, and sustained COMT inhibition.
Actually, peak (Emax) and extent (AUEC) of S-COMT inhibition with OPC followed a dose-dependent manner although not entirely proportional to the dose administered. Considering the 50 mg OPC dose as a reference, there was a 10 % difference between 25 and 50 mg OPC in both peak and extent of S-COMT inhibition. Likewise, the difference between 50 and 75 mg OPC in both peak and extent of S-COMT inhibition was less than 4 %, which suggests that the 75 mg OPC may not provide a significant advantage with respect to S-COMT inhibition versus the 50-mg OPC dose. These observations fit well with the observations on the dose-dependent effects upon 3-OMD availability and exposure. The tolerability profile was favorable and similar between ENT and OPC.
In conclusion, OPC, a novel third generation COMT inhibitor, when compared to ENT, provides a superior response upon the bioavailability of levodopa associated to its more pronounced, long-lasting, and sustained COMT inhibition. The tolerability profile was favorable and similar between OPC and ENT. On the basis of the results presented in this study and along with the earlier pharmacology studies, it is anticipated that OPC adjunct therapy at the dosages of 25 and 50 mg will provide an enhancement in levodopa availability that will translate into clinical benefit for Parkinson’s disease patients.
Conflict of interest
This study was sponsored by BIAL—Portela & Cª, S.A. All authors were involved in the design or conduct of the study; the collection, management, or analysis of the data; and the preparation or review of the manuscript. Dr Amílcar Falcão received consultancy honoraria from BIAL—Portela & Cª, S.A. Drs. José-Francisco Rocha, Ana Santos, Roberto Pinto, Nelson Lopes, Teresa Nunes, Lyndon C. Wright, Manuel Vaz-da-Silva, and P. Soares-da-Silva are or were employees of BIAL at the time of the study.
References
Morgan JC, Sethi KD (2006) Emerging drugs for Parkinson’s disease. Expert Opin Emerg Drugs 11(3):403–417
Schapira AH, Emre M, Jenner P, Poewe W (2009) Levodopa in the treatment of Parkinson’s disease. Eur J Neurol: Off J Eur Fed Neurol Soc 16(9):982–989. doi:10.1111/j.1468-1331.2009.02697.x
Dingemanse J (2000) Issues important for rational COMT inhibition. Neurology 55(11 Suppl 4):S24–S27, discussion S28-32
Palma PN, Bonifácio MJ, Almeida L, Soares-Da-Silva P (2007) Restoring dopamine levels. In: Simth HJ, Simons C, Sewell RDE (eds) Protein misfolding in neurodegenerative diseases: mechanisms and therapeutic strategies. CRC Press, pp415-445
Gomes P, Soares-da-Silva P (1999) Interaction between L-DOPA and 3-O-methyl-L-DOPA for transport in immortalised rat capillary cerebral endothelial cells. Neuropharmacology 38(9):1371–1380
Gervas JJ, Muradas V, Bazan E, Aguado EG, de Yebenes JG (1983) Effects of 3-OM-dopa on monoamine metabolism in rat brain. Neurology 33(3):278–282
Nutt JG, Woodward WR, Gancher ST, Merrick D (1987) 3-O-methyldopa and the response to levodopa in Parkinson’s disease. Ann Neurol 21(6):584–588. doi:10.1002/ana.410210610
Wade LA, Katzman R (1975) 3-O-methyldopa uptake and inhibition of L-dopa at the blood-brain barrier. Life Sci 17(1):131–136
Olanow CW, Stocchi F (2004) COMT inhibitors in Parkinson’s disease: can they prevent and/or reverse levodopa-induced motor complications? Neurology 62(1 Suppl 1):S72–S81
Bonifácio MJ, Palma PN, Almeida L, Soares-da-Silva P (2007) Catechol-O-methyltransferase and its inhibitors in Parkinson’s disease. CNS Drug Rev 13:352–379. doi:10.1111/j.1527-3458.2007.00020.x
Lang AE, Lees A (2002) Management of Parkinson’s disease: an evidence-based review. Mov Disord 17(Suppl 4):S45–S51
Brooks DJ (2004) Safety and tolerability of COMT inhibitors. Neurology 62(1 Suppl 1):S39–S46
Kiss LE, Ferreira HS, Torrao L, Bonifacio MJ, Palma PN, Soares-da-Silva P, Learmonth DA (2010) Discovery of a long-acting, peripherally selective inhibitor of catechol-O-methyltransferase. J Med Chem 53(8):3396–3411
Palma PN, Bonifácio MJ, Loureiro AI, Soares-da-Silva P (2012) Computation of the binding affinities of catechol-O-methyltransferase inhibitors: multisubstate relative free energy calculations. J Comput Chem 33(9):970–986
Bonifácio MJ, Torrão L, Loureiro AI, Wright LC, Soares-da-Silva P (2012) Opicapone: characterization of a novel peripheral long-acting catechol-O-methyltransferase inhibitior. Parkinsonism Relat Disord 18(S2):S125
Bonifácio MJ, Sutcliffe JS, Torrão L, Wright LC, Soares-da-Silva P (2012) Brain and peripheral levodopa pharmacokinetics in the Cynomolgus monkey following administration of opicapone, a novel catechol-O-methyltransferase inhibitor. Parkinsonism Relat Disord 18(S2):S125
Almeida L, Rocha J-F, Falcão A, Palma N, Loureiro AI, Pinto R, Bonifácio M, Wright LC, Nunes T, Soares-da-Silva P (2013) Pharmacokinetics, pharmacodynamics and tolerability of opicapone, a novel catechol-O-methyltransferase inhibitor, in healthy subjects: prediction of slow enzyme-inhibitor complex dissociation of a short-living and very long-acting inhibitor. Clin Pharmacokinet 52(2):139–151
Rocha JF, Almeida L, Falcao A, Palma PN, Loureiro AI, Pinto R, Bonifacio MJ, Wright LC, Nunes T, Soares-da-Silva P (2013) Opicapone: a short lived and very long acting novel catechol-O-methyltransferase inhibitor following multiple dose administration in healthy subjects. Br J Clin Pharmacol 76(5):763–775. doi:10.1111/bcp.12081
Ferreira JJ, Rocha JF, Falcão A, Pinto R, Nunes T, Soares-da-Silva P (2013) Effect of opicapone multiple-dose regimens on levodopa pharmacokinetics, motor response, and erythrocyte-COMT activity in Parkinson’s patients co-administered with levodopa/dopa-decarboxylase inhibitor. Mov Disord 28(Suppl 1):S154–S431
Ferreira JJ, Rocha JF, Santos A, Nunes T, Soares-da-Silva P (2012) The design of a double-blind, placebo- and active-controlled, multi-national phase-III trial in patients with Parkinson’s disease and end-of-dose motor fluctuations: Opicapone superiority vs. placebo and non-inferiority vs. entacapone. Mov Disord 27(Suppl 1):S118
Lees A, Costa R, Oliveira C, Lopes N, Nunes T, Soares-da-Silva P (2012) The design of a double-blind, placebo-controlled, multi-national phase-III trial in patients with Parkinson’s disease and end-of-dose motor fluctuations: opicapone superiority vs. placebo. Mov Disord 27(Suppl 1):S127
Silveira P, Vaz-da-Silva M, Almeida L, Maia J, Falcão A, Loureiro AI, Torrão L, Machado R, Wright LC, Soares-da-Silva P (2003) Pharmacokinetic-pharmacodynamic interaction between BIA 3-202, a novel COMT inhibitor, and levodopa/benserazide. Eur J Clin Pharmacol 59:603–609
Vieira-Coelho MA, Soares-da-Silva P (1996) Ontogenic aspects of liver and kidney catechol-O-methyltransferase sensitivity to tolcapone. Br J Pharmacol 117(3):516–520
Vieira-Coelho MA, Soares-da-Silva P (1999) Effects of tolcapone upon soluble and membrane-bound brain and liver catechol-O-methyltransferase. Brain Res 821(1):69–78
Heikkinen H, Varhe A, Laine T, Puttonen J, Kela M, Kaakkola S, Reinikainen K (2002) Entacapone improves the availability of L-dopa in plasma by decreasing its peripheral metabolism independent of L-dopa/carbidopa dose. Br J Clin Pharmacol 54(4):363–371
Keranen T, Gordin A, Harjola VP, Karlsson M, Korpela K, Pentikainen PJ, Rita H, Seppala L, Wikberg T (1993) The effect of catechol-O-methyl transferase inhibition by entacapone on the pharmacokinetics and metabolism of levodopa in healthy volunteers. Clin Neuropharmacol 16(2):145–156
Rouru J, Gordin A, Huupponen R, Huhtala S, Savontaus E, Korpela K, Reinikainen K, Scheinin M (1999) Pharmacokinetics of oral entacapone after frequent multiple dosing and effects on levodopa disposition. Eur J Clin Pharmacol 55(6):461–467
Kurlan R, Nutt JG, Woodward WR, Rothfield K, Lichter D, Miller C, Carter JH, Shoulson I (1988) Duodenal and gastric delivery of levodopa in parkinsonism. Ann Neurol 23(6):589–595. doi:10.1002/ana.410230611
Mouradian MM, Heuser IJ, Baronti F, Fabbrini G, Juncos JL, Chase TN (1989) Pathogenesis of dyskinesias in Parkinson’s disease. Ann Neurol 25(5):523–526. doi:10.1002/ana.410250521
Stocchi F, Vacca L, Ruggieri S, Olanow CW (2005) Intermittent vs continuous levodopa administration in patients with advanced Parkinson disease: a clinical and pharmacokinetic study. Arch Neurol 62(6):905–910. doi:10.1001/archneur.62.6.905
Ingman K, Naukkarinen T, Vahteristo M, Korpela I, Kuoppamaki M, Ellmen J (2012) The effect of different dosing regimens of levodopa/carbidopa/entacapone on plasma levodopa concentrations. Eur J Clin Pharmacol 68(3):281–289. doi:10.1007/s00228-011-1121-5
Jorga K, Banken L, Fotteler B, Snell P, Steimer JL (2000) Population pharmacokinetics of levodopa in patients with Parkinson’s disease treated with tolcapone. Clin Pharmacol Ther 67(6):610–620. doi:10.1067/mcp.2000.106795
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 39 kb)
Rights and permissions
About this article
Cite this article
Rocha, JF., Falcão, A., Santos, A. et al. Effect of opicapone and entacapone upon levodopa pharmacokinetics during three daily levodopa administrations. Eur J Clin Pharmacol 70, 1059–1071 (2014). https://doi.org/10.1007/s00228-014-1701-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-014-1701-2