Abstract
Background
The combination of polymyxins, meropenem, and sulbactam demonstrated efficacy against multi-drug-resistant bacillus Acinetobacter baumannii. These three antibiotics are commonly used against major blood, skin, lung, and heart muscle infections.
Objective
The objective of this study was to predict drug disposition and extrapolate the efficacy in these tissues using a physiologically based pharmacokinetic modeling approach that linked drug exposures to their target pharmacodynamic indices associated with antimicrobial activities against A. baumannii.
Methods
An adult physiologically based pharmacokinetic model was developed for meropenem, colistin, and sulbactam and scaled to pediatrics accounting for both renal and non-renal clearances. The model reliability was evaluated by comparing simulated plasma and tissue drug exposures to observed data. Target pharmacodynamic indices were used to evaluate whether pediatric and adult dosing regimens provided sufficient coverage.
Results
The modeled plasma drug exposures in adults and pediatric patients were consistent with reported literature data. The mean fold errors for meropenem, colistin, and sulbactam were in the range of 0.710–1.37, 0.981–1.47, and 0.647–1.39, respectively. Simulated exposures in the blood, skin, lung, and heart were consistent with reported penetration rates. In a virtual pediatric population aged from 2 to < 18 years, the interpretive breakpoints were achieved in 85–90% of subjects for their targeted pharmacodynamic indices after administration of pediatric dosing regimens consisting of 30 mg/kg of meropenem, and 40 mg/kg of sulbactam three times daily as a 3-h or continuous infusion and 5 mg/kg/day of colistin base activity.
Conclusions
The physiologically based pharmacokinetic modeling supports pediatric dosing regimens of meropenem/colistin/sulbactam in a co-administration setting against infections in the blood, lung, skin, and heart tissues due to A. baumannii.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Physiologically based pharmacokinetic modeling evaluated drug exposures of meropenem, colistin, and sulbactam in major body tissues including the blood, heart, lung, and skin for pediatric dosing regimens. The efficacy in these tissues was extrapolated by linking drug exposures to their target pharmacodynamic indices associated with antimicrobial activities against a Gram-negative bacillus using Acinetobacter baumannii as an example. |
The results confirm that pediatric weight-based dosing regimens of the three antibiotics used clinically are expected to provide adequate drug exposures required for their antimicrobial activities. |
This physiologically based pharmacokinetic/pharmacodynamic analysis of antibiotic exposures in the major body tissues where the relevant infection occurs supports a paradigm for evaluating optimal dosing of antimicrobial agents in pediatric patients at the site of infection. |
1 Introduction
Overuse of antibiotics worldwide has led to the emergence of multidrug-resistant (MDR) bacteria. Many antibiotics in monotherapy use are no longer efficacious against MDR bacteria [1]. This problem has led to a renewed interest in colistin and polymyxin-B, which were discovered in 1949 but have not been frequently used since the 1980s, primarily because of nephrotoxicity [2, 3]. As a way to reduce its toxicity, colistin is administered as colistin methanesulfonate (CMS), which is spontaneously hydrolyzed to the active drug colistin in vivo [4, 5].
Adaptive resistance to polymyxins in Gram-negative bacteria has complicated the clinical use of polymyxins [6]. Consequently, the combination of colistin with other antibiotics has become a routine treatment practice. The treatment regimen consisting of a combination of a carbapenem, CMS, and ampicillin/sulbactam has been associated with a lower mortality rate in patients with mostly ventilator-associated pneumonia caused by colistin-resistant A. baumannii infection [7]. Acinetobacter baumannii can cause serious nosocomial infections resulting in a high mortality rate from endocarditis, pneumonia, and skin and bloodstream infections. These infections often occur during invasive surgery and in intensive care units [8, 9]. Synergistic activities of sulbactam/meropenem/polymyxin-B against pan-resistant A. baumannii have been demonstrated using in vitro simulated drug concentrations similar to that in the blood [10, 11].
Many infections occur in tissues other than the blood. While the efficacy of antibiotics is dependent on drug exposure at the site of infection, it is difficult to obtain tissue drug concentration–time profiles from humans. Physiologically based pharmacokinetic (PBPK) modeling provides a non-invasive alternative to evaluate drug efficacy in the tissues where the infection occurs.
This study aimed to investigate drug exposure in the blood and major tissues including the lung, skin, and heart for pediatric dosing regimens of sulbactam/meropenem/colistin combination therapy. The three antibiotics have been indicated for infections related to these organs. The pharmacokinetics of meropenem, colistin, and sulbactam have been reported in pediatrics [12,13,14], but drug concentrations in the body tissues of corresponding antibiotics are lacking. In this report, we use PBPK modeling linked to pharmacodynamic (PD) attainment as an exposure-based PD evaluation to explore whether sufficient drug exposure has been achieved in these organs. The goal is to establish a rationale for pediatric dosing regimens of meropenem/colistin/sulbactam. The current pediatric dosing recommendation for colistin is 2.5–5 mg/kg/day of colistin base activity (CBA, administered as CMS) in combination with other antibiotics [15]; for meropenem, the recommendation is 20–40 mg/kg intravenously every 8 h (q8h) [16]; and for sulbactam pediatric doses, it ranged from 12.5 to 40 mg/kg intravenously every q8h [14, 17].
2 Materials and Methods
2.1 Clinical Data Used for PBPK Model Development and Evaluation
Web of science and PubMed databases were used to search for the pharmacokinetic profiles and exposure parameters of meropenem, colistin, and sulbactam. The literature containing demographic information such as sex, age, weight, and renal function, as well as dosing regimen and drug exposures were collected. Key parameters for the PBPK model were optimized according to reference information. The plasma drug concentration–time profiles from the literature were extracted using WebPlotDigitizer (version 4.5 https://automeris.io/WebPlotDigitizer) for meropenem, colistin, and sulbactam.
Systemic exposures from single-dosing and multiple-dosing regimens of meropenem, colistin, and sulbactam via an intravenous bolus or infusion in healthy volunteers and patients were used to develop and evaluate the adult PBPK model. After scaling, the adult model to the pediatric population, the pediatric PBPK models of these antibiotics were validated with data extracted from the literature.
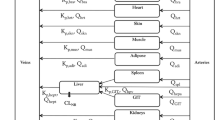
2.2 Development of the Adult PBPK Model
The adult PBPK models of meropenem, colistin, and sulbactam were developed using PK-Sim® (Version 10.0; part of the Open Systems Pharmacology Suite, www.open-systems-pharmacology.com). Drug pharmacokinetic (PK) models utilized a whole-body PBPK model with each tissue described as perfusion rate-limited kinetics assuming both renal and non-renal clearances [18, 19]. All tissues were assumed to be well-stirred compartments that equilibrated instantaneously with the plasma; the distribution of the drug into the tissue is governed by the blood flow rates. The physicochemical characteristics and physiological parameters for meropenem, colistin, and sulbactam are listed in Table 1. Tissue-to-plasma partition coefficients were computed using the Rodgers and Rowland [20] and Rodgers et al. [21] method; standard deviations of the partition coefficients were adjusted by comparing the inter-individual variability in drug tissue exposures to that reported in the literature. Demographical information such as age, sex, weight, and height, as well as dosing regimen and plasma concentration–time profiles (Tables S3–S5 of the Electronic Supplementary Material [ESM]), were utilized in the model development. The dosing regimens for the three drugs used for the model development were as follows: 240 mg for colistin methanesulfonate (~ 90 mg of CBA), 500 mg for meropenem, and 500 mg for sulbactam as a 0.5-h infusion. Additional adult dosing regimens by renal function listed in Table S1 of the ESM were simulated to compare PBPK simulations to that of population PK models. Details of the population PK models are provided in the ESM and their parameters are listed in Table S2 of the ESM.
Meropenem is a broad-spectrum carbapenem whose antimicrobial activity is mediated by binding to penicillin-binding proteins to inhibit the synthesis of the cell wall [22]. The model-predicted pharmacokinetic characteristics of meropenem in adults were compared to the literature [23,24,25]. Approximately 70% of the meropenem is recovered unchanged in the urine, indicating that the elimination of meropenem is primarily cleared by the renal elimination pathway including glomerular filtration and renal tubular secretion. Organic-anion transporters 1 and 3 expressed in renal tubules mediated the transport of meropenem. The other 20–34% of meropenem total clearance is eliminated by hydrolysis of the beta-lactam ring by dehydropeptidase I to its only inactive metabolite; biliary clearance is involved following meropenem metabolism [25, 26]. Renal clearance was 2.3 mL/min/kg; dehydropeptidase I was applied as a first-order process with a value of 20 mL/min; and biliary clearance was 6.5 × 10−4 mL/min/kg. Meropenem is relatively unstable in the aqueous solution, with the concentration dropping to 90% within 6 h at 33 °C [27]. The rate of this spontaneous hydrolysis in the blood is considered much slower than its renal clearance and is already accounted for in its total clearance in the model. The PBPK model for meropenem took into account these elimination pathways.
The information on colistin pharmacokinetic properties reported in the literature is far from sufficient. Renal clearance was the primary route for its prodrug CMS, which is also hydrolyzed to the active form colistin, and subsequently eliminated through non-renal clearance [4, 5, 28]. In renal failure, CMS conversion to colistin is higher because more CMS is available in the systemic circulation [29, 30]. A reduction in the daily CBA dose was implemented in patients with decreased renal function (Table S1 of the ESM). Colistin undergoes extensive tubular reabsorption up to as much as 80% of the drug filtered through the kidney [31, 32]; the glomerular filtration rate fraction was fixed to 0.2 to account for tubular reabsorption. A previous PBPK model of colistin and CMS developed in rats determined that tubular reabsorption of colistin was ninefold of the urine flow rate [33] and in the pig was fixed to 106 L/h [34]. The non-renal clearance of colistin is largely based on empirical information [35]. In the PBPK model, renal clearance of 0.29 mL/min/kg accounted for a small portion of the total clearance, whereas the remaining non-renal clearance of 4.0 mL/min/kg accounted for the majority of the total clearance of colistin [5].
Sulbactam is generally combined with other β-lactam antibiotics to enhance their activities; this is achieved by inhibiting β-lactamase enzymes that are responsible for degrading the β-lactam ring [36, 37]. Sulbactam is mainly eliminated by the kidney with renal clearance accounting for nearly 80% of its total clearance [17, 38]. A renal clearance value of 4.0 mL/min/kg was used in the model. An unspecific non-renal clearance of 1.0 mL/min/kg was also added to the PBPK model to account for the remaining 20% [38].
2.3 Adult PBPK Model Evaluation
For meropenem, colistin, and sulbactam, a typical individual is an adult with normal renal function. A virtual adult population consisting of 100 subjects with a 50:50 male-to-female ratio was used; the corresponding demographics are listed in Tables S6–S8 of the ESM. Model performance was evaluated based on the comparison of simulated and observed PK data including the maximum concentration (Cmax) and the area under the concentration–time curve (AUC) for the three antibiotics from various populations [39, 40]. The observed Cmax and AUC data for comparison were determined from digitally extracted concentration–time profiles. The performance of the simulations was evaluated by the mean fold error (MFE) (Eq. 1) for the two PK parameters. The PBPK models were deemed acceptable when all the predicted PK parameters were within the twofold range to the corresponding observed data (MFE = 0.5–2.0).
The variability in pharmacokinetics produced by the PBPK model in adults by renal function category was compared to the simulations from population PK models using a summary of the concentration–time course.
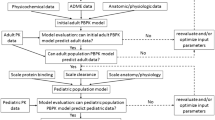
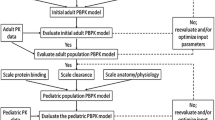
2.4 Pediatric PBPK Model Development and Evaluation
2.4.1 Physiological Parameters in the Pediatric Population
A virtual pediatric population consisted of individuals with normal renal function from 2 to 17 years of age; this age range was selected because the pediatric renal function is deemed to be fully developed by 2 years of age. Pediatric age-matched body weights were generated using a polynomial function and constant coefficients previously developed to describe the inter-individual variability of body weight by age and sex [41]. Developmental changes in anatomic and physiological parameters including organ volumes, blood flows, organ composition, plasma protein concentrations, protein binding, and maturation of elimination processes in PK-Sim® utilized population data from previous studies [42, 43] for its ontogeny database [44]. The pediatric virtual populations were generated using these algorithms to adjust for age-dependent changes in anthropometric (height and weight) and physiological parameters (blood flow, organ volume, organ composition, hematocrit, and cardiac output). For scaling of unbound fraction of colistin and sulbactam in children, the method of McNamara and Alcorn was applied to account for changes in α1-acid glycoprotein and albumin [45].
The non-renal elimination of colistin and the DEPE1 expression information of meropenem are absent in pediatrics. Both renal and non-renal clearances were scaled by age-dependent maturation of organ weight.
2.4.2 Pediatric Dosing Regimens
For the extrapolation of efficacy, pediatric dosing regimens used were 30 and 40 mg/kg q8h as 3-h infusions for meropenem and sulbactam, and 5 mg/kg/day of CBA, administered as CMS. The maximum recommended dose of colistin by the European Medicines Agency and the US Food and Drug Administration is 5 mg/kg/day of CBA as a 0.5-h infusion but higher doses are sometimes needed to achieve an acceptable probability of target attainment (PTA) [46]. In general, a meropenem dose of 20–40 mg/kg q8h can achieve sufficient PTA in pediatrics [25]. The dosing regimen of sulbactam in pediatrics normally ranged from 12.5 to 40 mg/kg three times daily [14, 17]. For meropenem and sulbactam, 3-h and continuous infusions were simulated. Pediatric dosing regimens were selected based on dosing regimens that would produce similar exposure to that in adults [11].
2.4.3 Scaling Renal Clearance and Non-renal Clearance
A ratio of 70%:30% renal to non-renal clearances was assumed in the simulation of meropenem in the pediatric population. Clearance due to DPEP1 in both pediatric patients and adults was incorporated into the model as non-renal clearance [25]. As for sulbactam, the ratio of renal to non-renal clearances was 80%:20%. For colistin, the primary elimination pathway is by non-renal clearance, while the specific mechanism of non-renal clearance remains to be elucidated. Dosing regimens in renally impaired patients were simulated for meropenem, sulbactam, and colistin. The renal function categories were evaluated based on a uniform distribution range from 10 to 150 mL/min of creatinine clearance (Table 1). The renal impairments were simulated via a decrease in the glomerular filtration rate in the renal impaired populations.
2.4.4 Pediatric PBPK Model and Evaluation
A virtual pediatric population comprised 1000 individuals with a 50:50 male-to-female ratio and an age range of 2–17 years (Tables S6–8 of the ESM). The PBPK model simulated Cmax and AUC values were compared with observed data digitized from literature values for the three antibiotics. The AUC over 24 h and Cmax were determined by a non-compartmental method. The performance of the pediatric model was accepted when the MFE was within the range of 0.5–2.
2.5 Tissue Drug Concentrations and Penetration Rates
The concentrations of meropenem, colistin, and sulbactam in the heart, lung, and skin were predicted for pediatrics of various age groups and adults using the PBPK model. Drug exposure parameters, Cmax and AUC, were computed from the concentration–time profiles; penetration rates in each tissue were evaluated by the ratio of drug exposure in the tissue to that in the blood. Colistin methanesulfonate and colistin do not distribute into cells [47]. The tissue drug concentrations were taken from the interstitial fluid.
2.6 Pharmacodynamic Indices and PTA
The PD indices of meropenem, sulbactam, and colistin were established for A. baumannii. Meropenem antimicrobial activities are time dependent and are associated with the percentage of time over a 24-h period wherein the free drug concentration is above the minimum inhibitory concentration (fT>MIC) of at least 40%, which was shown to result in a 2-log10 kill [48]. The PD index of sulbactam is fT>MIC of at least 60% [49]. Target PD indices of 60%, 80%, and 100% [50] were also evaluated for meropenem and sulbactam. For colistin, the PD index is best characterized by the ratio of free drug AUC over a 24-h period relative to an MIC of at least 7.4 associated with a 2-log10 kill [51].
The PTA was computed as the percentage of the 1000 simulated profiles of each dosing regimen in the population group that achieved the minimum target PD index value in each of the tissues wherein the concentration–time profiles were generated from the PBPK simulations. Computed PTA took into account the plasma protein binding for the drug concentrations in the blood and mucin binding in the lung as reported from the literature. For the PTA computed from the heart and skin, no drug binding was assumed.
3 Results
3.1 PBPK Model Qualification in Adult and Pediatric Populations
After a comprehensive literature search, data from ten, six, and four reports for meropenem, colistin, and sulbactam were used for the model development, and 13, six, and six populations were used for the model verification, respectively. Then, 207, 50, and 70 observations were included in the model development, respectively. The observed mean concentrations of meropenem, sulbactam, and colistin digitized from the literature were contained within the 95% prediction interval of the corresponding simulations (Fig. 1). The simulated pharmacokinetic parameters Cmax and AUC of the three antibiotics in adults and pediatric patients were all in the acceptable range of 0.5–2 compared to published data (Fig. 2 and Tables S3–5 of the ESM). In Fig. 2, the dashed lines represent the 0.5-fold and twofold boundaries. All data were within these boundaries.
Comparison of meropenem, colistin, and sulbactam concentration–time profiles in the blood, lung, heart, and skin for adult and pediatric dosing regimens between observed and physiologically based pharmacokinetic modeling. Symbols and error bars, observed data; lines and shaded areas, median and 90% prediction intervals. CBA colistin base activity, CrCL creatinine clearance, h hours
Comparison between simulated and observed exposure parameters from several studies in the literature for different populations. Solid lines represent a line of unity; dashed lines represent a twofold difference. AUC area under the concentration–time curve, Cmax maximum concentration, HV healthy volunteers
The PK variabilities between simulations from the PBPK model and that of the population PK model were comparable as shown in Figs. S1–S3 of the ESM for adult dosing regimens by renal functions of meropenem, sulbactam, and colistin, respectively. The PK variabilities were generated not only from demographical factors such as sex, age, and body weight, but also from the distribution of the partition coefficients listed in Table 1. Given that the variability in partition coefficients can affect the variability in tissue concentrations, we also compared the coefficient of variation (CV) of the tissue exposures generated from PBPK simulations with that reported in the literature. The CV values of simulated meropenem exposures in the lung and skin were 52.7% and 35.2%; these values are comparable to the values reported in the literature (i.e., 49.4% for lung and 30% for skin) [52, 53]. For tissue colistin exposures, a CV value of 36.3% in brain cerebrospinal fluid reported in the literature was also similar to our PBPK simulation in brain interstitial fluid (CV: 33%) [54]. As for sulbactam, the variability due to PBPK simulation in the lung was 31.0%, which is close to the corresponding CV of 29.6% from the literature [55].
The model also predicted higher unbound fractions of colistin and sulbactam in pediatrics (Table 1). Given that meropenem is not bound to plasma protein, we assumed that the unbound fraction in pediatrics is the same as that in adults.
3.2 Tissue Exposures
Drug concentrations in the lung, skin, and heart were simulated based on the interstitial drug concentration as the three antibiotics are commonly used to treat infections in these sites (Table 2). Performance evaluation of the model in some tissues could not be carried out because of the lack of literature on tissue drug concentrations. Consequently, we also simulated drug concentrations in other tissues where the information is available in the literature, for example, colistin drug concentration in the brain, and determined their penetration rates into tissues.
The penetration ratios comparing meropenem AUC values in tissue and plasma were 0.36, 0.63–0.64, and 0.21–0.23 for the lung, skin, and heart, respectively, whereas for sulbactam, the penetration ratios were 0.58–0.60, 0.28–0.31, and 0.50–0.51, respectively. For colistin, these values were 0.56, 0.42, 0.15–0.16, and 0.04–0.05 for exposures in the lung, skin, heart, and interstitial fluid in the brain (interstitial fluid), respectively. Table 3 shows the penetration rates for the Cmax parameter.
Our simulation results were consistent with those reported for various tissues. The penetration ratio of meropenem into human lung tissue compared to plasma was reported to be 38% and heart valve tissue compared to plasma was 15–66% [52]. Meropenem concentration in skin blister fluid was 67% that of plasma [53, 56]. For colistin, the penetration into the cerebrospinal fluid was approximately 5% [54, 57]. In addition, we can assume a similar human lung penetration of 61% as in mice [58]. The sulbactam pulmonary penetration ratio was 52% following intravenous administration in healthy adult subjects [55].
The drug exposures of meropenem and sulbactam after continuous infusions are listed in Tables S9–10 of the ESM. As expected, there were minimal changes in either tissue drug exposures or penetration ratios between continuous and 3-h infusions.
3.3 PTA for Pediatric Dosing Regimens
To obtain the desired drug concentration in body tissues, this study optimized the dosing regimens of three antibiotics in the pediatric population. The dosing regimen for meropenem in pediatrics was 30 mg/kg q8h as either a 3-h or continuous infusion. This dosing regimen is equivalent to the high dose of 2 g q8h in adults, assuming a median body weight of 70 kg [59]. The breakpoint of meropenem for A. baumannii is 2 µg/mL, while it can be considered resistant when the MIC reaches 8 µg/mL [60]. As these dosing regimens are intravenous infusions, drug exposure is highest in the blood, followed by the skin, lung, and heart. The computation of PTA assumed that meropenem has negligible plasma protein binding. The pharmacodynamic index used to determine the PTA of meropenem was 40% fT > MIC. Sufficient PTAs (≥ 85 or 90%) were achieved at 8, 4, 4, and 2 µg/mL MICs in the blood, skin, lung, and heart, respectively (Fig. 3). This high dose is effective against lung and heart infections caused by susceptible bacteria, otherwise, combination antibiotics that can confer susceptibility to meropenem would be required. Overall, the lower body weight in smaller children aged < 12 years may require higher weight-based doses in order to achieve sufficient PTA in tissues with lower drug exposures.
Probability of target attainment of meropenem pharmacodynamic index of free drug concentration is above the minimum inhibitory concentration (fT > MIC) of at least 40% in the blood, lung, heart, and skin for dosing regimens in pediatric patients (30 mg/kg every 8 h [q8h]) and adults (2 g q8h) as a 3-h infusion. yrs years
The breakpoint of colistin against Acinetobacter spp. is ≤ 2 µg/mL for intermediate; when the MIC is ≥ 4 µg/mL, the infection is considered resistant [60]. The pediatric dosing regimen of 5 mg/kg/day of CBA is equivalent to a 300-mg loading dose followed by 180 mg of CBA every 12 h (q12h) in adults, which is a relatively high dose required to obtain sufficient drug concentration in the tissues [61]. Colistin has a high and variable plasma protein binding and also mucin binding [62, 63]; we assumed 30% and 15% free drug in the blood and lung. For the drug exposures in the blood, both pediatric and adult dosing regimens can achieve sufficient coverage (PTA ≥ 85–90%) at a MIC of 2 µg/mL (Fig. 4). The skin has higher coverage because we assumed no drug binding in the skin. Because of the low penetration rate to cardiac tissues, PTA ≥ 85–90% cannot be achieved at the breakpoint of 2 µg/mL; this PTA can only be achieved at the lower MIC of 1 µg/mL. Colistin poorly distributes to the pleural cavity, lung parenchyma, bones, and cerebrospinal fluid [29], owing to its high polarity and its binding to mucin. The PTA can reach 85–90% only when the MIC is ≤ 1 µg/mL. The low colistin exposures in the tissues suggest that colistin should be administered as a combination therapy to capitalize on its synergistic effects. Pediatric subjects with body weights approaching that of adults tend to have higher colistin drug exposure in the tissues for weight-based dosing. This would result in a higher PTA after an administration of 5 mg/kg/day of CBA divided three times daily as compared to a lower age pediatric group with smaller weights.
Probability of target attainment of colistin pharmacodynamic index of ratio of free drug area under the concentration–time curve over a 24-h period relative to minimum inhibitory concentration (fAUC/MIC) ratio of at least 7.4 in the blood, lung, heart, and skin for dosing regimens of colistin base activity (CBA) in pediatric patients (5 mg/kg/day) and adults (300-mg loading dose plus 180 mg every 12 h [q12h]) as a 3-h infusion. q12h every 12 h
There is no recommended breakpoint for ampicillin/sulbactam against A. baumannii, but its breakpoint against Enterobacteriaceae is ≤ 8/4 µg/mL. The pediatric dosing regimen of a 40-mg/kg q8h infusion over 3 h was selected as an equivalent to the adult dosing regimen. The resultant concentration was previously shown to achieve ≥ 90% PTA for 60% fT > MIC at 4 µg/mL MIC against A. baumannii [49]. Plasma protein binding was assumed to be 5% [64]; no binding was assumed for other tissues. At this dose, the blood exposure of sulbactam in pediatric patients of all age groups reached ≥ 90% PTA at a MIC of 4 µg/mL (Fig. 5). There was sufficient coverage at 4, 2, and 2 µg/mL MICs in the lung, skin, and heart, respectively. Similar to the trend that was found with colistin, the 40-mg/kg q8h regimen resulted in lower drug exposure in pediatric patients aged 2 to < 12 years who have smaller body weights.
Probability of target attainment of sulbactam pharmacodynamic index of free drug concentration is above the minimum inhibitory concentration (fT > MIC) of at least 60% in the blood, lung, heart, and skin for dosing regimens in pediatric patients (40 mg/kg every 8 h [q8h]) and adults (3 g q8h) as a 3-h infusion, yrs years
For critically ill patients, a more aggressive PK/PD target is necessary for time-dependent antibiotics such as meropenem and sulbactam [50]. Therefore, we included target PD indices of 60%, 80%, and 100% fT > MIC for meropenem and 80%, 100% fT > MIC for sulbactam. For the 3-h infusion, the MIC at which ≥ 85–90% PTA reduced as the target fT > MIC increased (Figs. S4–S6 of the ESM). However, no change in the meropenem breakpoint was observed for continuous infusion with increasing fT>MIC requirements (Figs. S7–S9 of the ESM). With the exception of 100% fT > MIC, ≥ 85% PTAs were achieved at 8, 4, 1, and 1 µg/mL MICs in the blood, skin, lung, and heart, respectively, similar to the 3-h infusion using a target of 40% fT > MIC. The same dosing regimen in younger children (aged 2 to <6 years) had lower breakpoints for blood, heart, lung, and skin tissues, as weight-based dosing tends to result in lower exposure in patients with smaller body weights.
A similar trend was also observed for sulbactam (Figs. S10–14 of the ESM); no change in breakpoint in increasing fT > MIC up to 100% in the blood can be expected for continuous infusions. For sulbactam PD targets of 60% and 80% fT>MIC, ≥ 85% PTA was attained at 8, 2, 4, and 4 µg/mL MICs in the blood, skin, lung, and heart, respectively; these breakpoints were comparable to the 3-h infusion using a target 60% fT > MIC. Using a PD target of 100% fT > MIC, ≥ 85% PTA were reached at 8, 1, 2, and 4 µg/mL MICs in the blood, skin, lung, and heart, respectively.
4 Discussion and Conclusions
Both meropenem and ampicillin/sulbactam are commonly used to treat sepsis, acute pulmonary exacerbations, and complex skin and skin structure infections in pediatrics [65,66,67], whereas the use of colistin against these types of infections is anecdotal [68, 69]. For dose optimization, it is important to characterize antibiotic exposures and target attainment in commonly infected major tissues including the heart, lung, and skin. Several studies indicated that a combination consisting of meropenem, colistin, and sulbactam is effective in treating MDR A. baumannii [11, 70]. The combination with colistin showed synergistic activities and reduced the required concentrations of companion antibiotics against the infection [71, 72]. Combination therapy could confer the susceptibility of microorganisms at the infection site with the drug concentrations generated from current commercial dosing regimens.
The plasma pharmacokinetics of meropenem in adults and pediatric patients were well studied [25, 73]. Although blood distribution of colistin and sulbactam has been reported in adults, few have been reported in children, especially at the infected tissues and organs [17, 74, 75]. In this study, we established and validated a PBPK model in adults and extrapolated it to pediatric patients in order to simulate antibiotic exposures in some commonly infected organs and to evaluate the treatment effect at these sites.
The PBPK model is a good method for simulating the tissue distribution of antibiotics in pediatrics. We calculated the AUC and the Cmax of the three antibiotics in the target tissues and estimated the penetration rate by the ratios of AUCTissue/AUCPlasma and Cmax Tissue/Cmax Plasma. Meropenem have been reported to be 38% permeable to human lung tissue compared with plasma and 15–66% permeable to heart valve tissue compared with plasma [52, 56]. These results are consistent with those simulated by our PBPK model for meropenem. No further tissue permeability has been reported for colistin and sulbactam, except in the cerebrospinal fluid and lung, respectively. Therefore, this study used the permeability of these two tissues to demonstrate the reliability of our model. The lung permeability of sulbactam after intravenous administration in healthy adult subjects was 52% [76]. In addition, the distribution of these three antibiotics in children between the ages of 12 and < 18 years is close to that of adults owing to their physiological similarity under comparable dosage conditions.
No randomized clinical trial has been conducted to formally evaluate the efficacy of the combination regimen of colistin/meropenem/sulbactam in infections caused by MDR A. baumannii. However, we obtained some useful information from in vitro studies and clinical case reports. For MDR A. baumannii strains with moderately higher MICs for meropenem (MIC ≤ 64 µg/mL) and sulbactam (MIC ≤ 16 µg/mL), the combination of colistin plus meropenem and/or sulbactam produced synergistic bactericidal activities [56, 70, 77]. The dosing regimens and duration of infusion selected for our simulations were based on the literature on combination therapy. In an in vitro PK/PD study, Liu et al. simulated a drug exposure from a 3-h infusion of 1 g of meropenem combined with a steady-state concentration of 1 µg/mL of colistin, resulting in a synergistic killing effect against carbapenem-resistant A. baumannii [78]. Saelim et al. demonstrated that 150 mg of CBA (administered as CMS) every 12 h combined with daily sulbactam ≥ 6 g/day can improve efficacy against carbapenem-resistant A. baumannii in patients with normal renal function while reducing nephrotoxicity [79]. Using an in vitro time-kill infection model, Lim et al. simulated 2 g of meropenem combined with 4 g of sulbactam q8h and demonstrated a PTA of 2-log kill of 34% at 24 h [80]. Their low PTA could be improved by adding a colistin regimen to the combination.
The combination of these three antibiotics is unlikely to produce drug–drug interactions because renal clearance of meropenem and sulbactam accounted for a high percentage of total clearance, whereas colistin is mainly eliminated by non-renal clearance. Combination therapy consisting of meropenem and colistin was previously shown to increase the incidence of diarrhea but decreased the incidence of mild renal failure, as compared with colistin alone [81]. Meropenem, colistin, and sulbactam are unlikely to affect the drug exposure of companion drugs in the combination.
The current analysis has its limitations. The MIC-based PK/PD indices do not take into account the time courses of drug concentration and pathogen response and do not reflect dosing frequency or treatment duration [82]. Our application of the PBPK model to determine site-specific drug concentration is based on the assumption that the PK/PD indices and thresholds that are correlated with microbiological outcomes apply not only to the assessment in blood but also to that in the infected tissues. Knowledge gaps of actual tissue drug concentrations limit our ability to validate our simulations of tissue drug concentrations. The complexity of organ tissue structure may affect the accuracy of simulated drug concentrations. In addition, tissue microanatomy can result in gradients between histological compartments. The simulations of tissue drug concentrations were from the interstitial space and may not necessarily represent the microcompartments where bacteria proliferate.
Our evaluation of clinical efficacy did not include the influence of human autoimmunity on the antibacterial effect. In the in vivo infection models that were used to define the PK/PD indices, mice are made neutropenic prior to infecting the animal. These breakpoints reflect a worst-case scenario in the case of an immunocompromised individual. A reason for using a neutropenic model could be that animal immunity, especially that in rodents is not easily translatable to human immunity. Thorsted and colleagues recently utilized a pig model infused with bacterial endotoxin to characterize innate immune responses resulting from cytokine induction [83]. Given the emergence of antibiotic drug resistance, the immune system will play a more important role as it does not distinguish between resistant and susceptible bacteria [82].
In conclusion, our analysis showed that the dosing regimen consisting of 30 mg/kg of meropenem q8h, 5 mg/kg/day of CBA, and 40 mg/kg of sulbactam q8h as a prolonged infusion could result in sufficient drug exposures in the blood, lung, skin, and heart. The findings from this study remain to be confirmed in a clinical trial. Combination antibiotics provide potential therapeutic options against tissue infections caused by drug-resistant bacteria that are increasingly threatening human health. At a time when new antibiotics are becoming increasingly scarce, effective antibiotic combination therapy has a practical significance to resolve this pressing problem of drug resistance.
References
Oo C, Sy SKB. Learning and augmenting natural processes: potential means of combating antimicrobial resistance from a drug R&D perspective. Drug Discov Today. 2020;25(1):1–3.
Brown JM, Dorman DC, Roy LP. Acute renal failure due to overdosage of colistin. Med J Aust. 1970;2(20):923–4.
Koch-Weser J, Sidel VW, Federman EB, Kanarek P, Finer DC, Eaton AE. Adverse effects of sodium colistimethate: manifestations and specific reaction rates during 317 courses of therapy. Ann Intern Med. 1970;72(6):857–68.
Bergen PJ, Li J, Rayner CR, Nation RL. Colistin methanesulfonate is an inactive prodrug of colistin against Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2006;50(6):1953–8.
Zhao M, Wu XJ, Fan YX, Zhang YY, Guo BN, Yu JC, et al. Pharmacokinetics of colistin methanesulfonate (CMS) in healthy Chinese subjects after single and multiple intravenous doses. Int J Antimicrob Agents. 2018;51(5):714–20.
Olaitan AO, Morand S, Rolain JM. Mechanisms of polymyxin resistance: acquired and intrinsic resistance in bacteria. Front Microbiol. 2014;5:643.
Qureshi ZA, Hittle LE, O’Hara JA, Rivera JI, Syed A, Shields RK, et al. Colistin-resistant Acinetobacter baumannii: beyond carbapenem resistance. Clin Infect Dis. 2015;60(9):1295–303.
Sopirala MM, Pope-Harman A, Nunley DR, Moffatt-Bruce S, Ross P, Martin SI. Multidrug-resistant Acinetobacter baumannii pneumonia in lung transplant recipients. J Heart Lung Transplant. 2008;27(7):804–7.
Lagana P, Melcarne L, Delia S. Acinetobacter baumannii and endocarditis, rare complication but important clinical relevance. Int J Cardiol. 2015;187:678–9.
Lenhard JR, Thamlikitkul V, Silveira FP, Garonzik SM, Tao X, Forrest A, et al. Polymyxin-resistant, carbapenem-resistant Acinetobacter baumannii is eradicated by a triple combination of agents that lack individual activity. J Antimicrob Chemother. 2017;72(5):1415–20.
Menegucci TC, Fedrigo NH, Lodi FG, Albiero J, Nishiyama SAB, Mazucheli J, et al. Pharmacodynamic effects of sulbactam/meropenem/polymyxin-B combination against extremely drug resistant Acinetobacter baumannii using checkerboard information. Microb Drug Resist. 2019;25(9):1266–74.
Ooi MH, Ngu SJ, Chor YK, Li J, Landersdorfer CB, Nation RL. Population pharmacokinetics of intravenous colistin in pediatric patients: implications for the selection of dosage regimens. Clin Infect Dis. 2019;69(11):1962–8.
Blumer JL, Reed MD, Kearns GL, Jacobs RF, Gooch WM 3rd, Yogev R, et al. Sequential, single-dose pharmacokinetic evaluation of meropenem in hospitalized infants and children. Antimicrob Agents Chemother. 1995;39(8):1721–5.
Schaad UB, Guenin K, Straehl P. Single-dose pharmacokinetics of intravenous sulbactam in pediatric patients. Rev Infect Dis. 1986;8(Suppl. 5):S512–7.
US FDA. Coly-Mycin® M parenteral colistimethate for injection, USP. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/050108s033lbl.pdf. Accessed 29 Jul 2022.
US FDA. Merrem® IV (meropenem for injection), for intravenous use. 1996. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/050706s037lbl.pdf. Accessed 29 Jul 2022.
Nahata MC, Vashi VI, Swanson RN, Messig MA, Chung M. Pharmacokinetics of ampicillin and sulbactam in pediatric patients. Antimicrob Agents Chemother. 1999;43(5):1225–9.
Jones H, Rowland-Yeo K. Basic concepts in physiologically based pharmacokinetic modeling in drug discovery and development. CPT Pharmacomet Syst Pharmacol. 2013;14(2): e63.
Sy SK, Wang X, Derendorf H. Introduction to pharmacometrics and quantitative pharmacology with an emphasis on physiologically based pharmacokinetics. In: Derendorf H, Schmidt S, editors. Applied pharmacometrics. New York: Springer; 2014. p. 1–64.
Rodgers T, Rowland M. Physiologically based pharmacokinetic modelling 2: predicting the tissue distribution of acids, very weak bases, neutrals and zwitterions. J Pharm Sci. 2006;95(6):1238–57.
Rodgers T, Leahy D, Rowland M. Physiologically based pharmacokinetic modeling 1: predicting the tissue distribution of moderate-to-strong bases. J Pharm Sci. 2005;94(6):1259–76.
Kitzis MD, Acar JF, Gutmann L. Antibacterial activity of meropenem against Gram-negative bacteria with a permeability defect and against staphylococci. J Antimicrob Chemother. 1989;24(Suppl. A):125–32.
Park SW, We JS, Kim GW, Choi SH, Park HS. Stability of new carbapenem DA-1131 to renal dipeptidase (dehydropeptidase I). Antimicrob Agents Chemother. 2002;46(2):575–7.
Ikawa K, Nakashima A, Morikawa N, Ikeda K, Murakami Y, Ohge H, et al. Clinical pharmacokinetics of meropenem and biapenem in bile and dosing considerations for biliary tract infections based on site-specific pharmacodynamic target attainment. Antimicrob Agents Chemother. 2011;55(12):5609–15.
Ganguly S, Edginton AN, Gerhart JG, Cohen-Wolkowiez M, Greenberg RG, Gonzalez D, et al. Physiologically based pharmacokinetic modeling of meropenem in preterm and term infants. Clin Pharmacokinet. 2021;60(12):1591–604.
Bax RP, Bastain W, Featherstone A, Wilkinson DM, Hutchison M, Haworth SJ. The pharmacokinetics of meropenem in volunteers. J Antimicrob Chemother. 1989;24(Suppl. A):311–20.
Fawaz S, Barton S, Whitney L, Swinden J, Nabhani-Gebara S. Stability of meropenem after reconstitution for administration by prolonged infusion. Hosp Pharm. 2019;54(3):190–6.
Nakwan N, Usaha S, Chokephaibulkit K, Villani P, Regazzi M, Imberti R. Pharmacokinetics of colistin following a single dose of intravenous colistimethate sodium in critically ill neonates. Pediatr Infect Dis J. 2016;35(11):1211–4.
Michalopoulos AS, Falagas ME. Colistin: recent data on pharmacodynamics properties and clinical efficacy in critically ill patients. Ann Intensive Care. 2011;1(1):30.
Falagas ME, Kasiakou SK. Colistin: the revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clin Infect Dis. 2005;40(9):1333–41.
Honore PM, Jacobs R, Joannes-Boyau O, Lochy S, Boer W, De Waele E, et al. Continuous renal replacement therapy-related strategies to avoid colistin toxicity: a clinically orientated review. Blood Purif. 2014;37(4):291–5.
Ma Z, Wang J, Nation RL, Li J, Turnidge JD, Coulthard K, et al. Renal disposition of colistin in the isolated perfused rat kidney. Antimicrob Agents Chemother. 2009;53(7):2857–64.
Bouchene S, Marchand S, Couet W, Friberg LE, Gobin P, Lamarche I, et al. A whole-body physiologically based pharmacokinetic model for colistin and colistin methanesulfonate in rat. Basic Clin Pharmacol Toxicol. 2018;123(4):407–22.
Viel A, Henri J, Bouchene S, Laroche J, Rolland JG, Manceau J, et al. A population WB-PBPK model of colistin and its prodrug CMS in pigs: focus on the renal distribution and excretion. Pharm Res. 2018;35(5):92.
Plachouras D, Karvanen M, Friberg LE, Papadomichelakis E, Antoniadou A, Tsangaris I, et al. Population pharmacokinetic analysis of colistin methanesulfonate and colistin after intravenous administration in critically ill patients with infections caused by gram-negative bacteria. Antimicrob Agents Chemother. 2009;53(8):3430–6.
Sharma VD, Singla A, Chaudhary M, Taneja M. Population pharmacokinetics of fixed dose combination of ceftriaxone and sulbactam in healthy and infected subjects. AAPS PharmSciTech. 2016;17(5):1192–203.
Jaruratanasirikul S, Wongpoowarak W, Wattanavijitkul T, Sukarnjanaset W, Samaeng M, Nawakitrangsan M, et al. Population pharmacokinetics and pharmacodynamics modeling to optimize dosage regimens of sulbactam in critically ill patients with severe sepsis caused by Acinetobacter baumannii. Antimicrob Agents Chemother. 2016;60(12):7236–44.
Foulds G, Stankewich JP, Marshall DC, O’Brien MM, Hayes SL, Weidler DJ, et al. Pharmacokinetics of sulbactam in humans. Antimicrob Agents Chemother. 1983;23(5):692–9.
Biesdorf C, Martins FS, Sy SKB, Diniz A. Physiologically-based pharmacokinetics of ziprasidone in pregnant women. Br J Clin Pharmacol. 2019;85(5):914–23.
Martins FS, Zhu P, Heinrichs MT, Sy SKB. Physiologically based pharmacokinetic-pharmacodynamic evaluation of meropenem plus fosfomycin in paediatrics. Br J Clin Pharmacol. 2020;87(3):1012–23.
Sy SK, Asin-Prieto E, Derendorf H, Samara E. Predicting pediatric age-matched weight and body mass index. AAPS J. 2014;16(6):1372–9.
Valentin J. Basic anatomical and physiological data for use in radiological protection: reference values: ICRP publication 89. Ann ICRP. 2002;32(3–4):1–277.
Ince I, Solodenko J, Frechen S, Dallmann A, Niederalt C, Schlender J, et al. Predictive pediatric modeling and simulation using ontogeny information. J Clin Pharmacol. 2019;59(Suppl. 1):S95-103.
Open Systems Pharmacology. PK-Sim® Ontogeny Database, version 7.3. https://github.com/Open-Systems-Pharmacology/OSPSuite.Documentation/blob/master/PK-Sim Ontogeny Database Version 7.3.pdf. Accessed 28 May 2022.
McNamara PJ, Alcorn J. Protein binding predictions in infants. AAPS PharmSci. 2002;4(1):E4.
Wacharachaisurapol N, Sukkummee W, Anunsittichai O, Srisan P, Sangkhamal S, Chantharit P, et al. Dose recommendations for intravenous colistin in pediatric patients from a prospective, multicenter, population pharmacokinetic study. Int J Infect Dis. 2021;109:230–7.
Jansson B, Karvanen M, Cars O, Plachouras D, Friberg LE. Quantitative analysis of colistin A and colistin B in plasma and culture medium using a simple precipitation step followed by LC/MS/MS. J Pharm Biomed Anal. 2009;49(3):760–7.
Heffernan AJ, Roberts JA. Dose optimisation of antibiotics used for meningitis. Curr Opin Infect Dis. 2021;34(6):581–90.
Yokoyama Y, Matsumoto K, Ikawa K, Watanabe E, Morikawa N, Takeda Y. Population pharmacokinetic-pharmacodynamic target attainment analysis of sulbactam in patients with impaired renal function: dosing considerations for Acinetobacter baumannii infections. J Infect Chemother. 2015;21(4):284–9.
Delattre IK, Taccone FS, Jacobs F, Hites M, Dugernier T, Spapen H, et al. Optimizing beta-lactams treatment in critically-ill patients using pharmacokinetics/pharmacodynamics targets: are first conventional doses effective? Expert Rev Anti Infect Ther. 2017;15(7):677–88.
Cheah SE, Wang J, Nguyen VT, Turnidge JD, Li J, Nation RL. New pharmacokinetic/pharmacodynamic studies of systemically administered colistin against Pseudomonas aeruginosa and Acinetobacter baumannii in mouse thigh and lung infection models: smaller response in lung infection. J Antimicrob Chemother. 2015;70(12):3291–7.
Tomaselli F, Maier A, Matzi V, Smolle-Juttner FM, Dittrich P. Penetration of meropenem into pneumonic human lung tissue as measured by in vivo microdialysis. Antimicrob Agents Chemother. 2004;48(6):2228–32.
Maglio D, Teng R, Thyrum PT, Nightingale CH, Nicolau DP. Pharmacokinetic profile of meropenem, administered at 500 milligrams every 8 hours, in plasma and cantharidin-induced skin blister fluid. Antimicrob Agents Chemother. 2003;47(5):1771–3.
Markantonis SL, Markou N, Fousteri M, Sakellaridis N, Karatzas S, Alamanos I, et al. Penetration of colistin into cerebrospinal fluid. Antimicrob Agents Chemother. 2009;53(11):4907–10.
Rodvold KA, Gotfried MH, Isaacs RD, O’Donnell JP, Stone E. Plasma and intrapulmonary concentrations of ETX2514 and sulbactam following Intravenous administration of ETX2514SUL to healthy adult subjects. Antimicrob Agents Chemother. 2018;62(11):e01089-e1118.
Newsom SW, Palsingh J, Wells FC, Kelly HC. Penetration of meropenem into heart valve tissue. J Antimicrob Chemother. 1995;36(Suppl. A):57–62.
Shetty AK, Zanirati G. The interstitial system of the brain in health and disease. Aging Dis. 2020;11(1):200–11.
Aoki N, Tateda K, Kikuchi Y, Kimura S, Miyazaki C, Ishii Y, et al. Efficacy of colistin combination therapy in a mouse model of pneumonia caused by multidrug-resistant Pseudomonas aeruginosa. J Antimicrob Chemother. 2009;63(3):534–42.
Albiero J, Mazucheli J, Barros J, Szczerepa M, Nishiyama SAB, Carrara-Marroni FE, et al. Pharmacodynamic attainment of the synergism of meropenem and fosfomycin combination against Pseudomonas aeruginosa producing metallo-beta-lactamase. Antimicrob Agents Chemother. 2019;63(6):e00126-e219.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. 2020. www.clsi.org. Accessed 29 Jul 2022.
Tsuji BT, Pogue JM, Zavascki AP, Paul M, Daikos GL, Forrest A, et al. International consensus guidelines for the optimal use of the polymyxins: endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy. 2019;39(1):10–39.
Huang JX, Blaskovich MA, Pelingon R, Ramu S, Kavanagh A, Elliott AG, et al. Mucin binding reduces colistin antimicrobial activity. Antimicrob Agents Chemother. 2015;59(10):5925–31.
Abodakpi H, Gohlke J, Chang KT, Chow DS, Tam VH. Analytical and functional determination of polymyxin B protein binding in serum. Antimicrob Agents Chemother. 2015;59(11):7121–3.
Yokoyama Y, Matsumoto K, Ikawa K, Watanabe E, Shigemi A, Umezaki Y, et al. Pharmacokinetic/pharmacodynamic evaluation of sulbactam against Acinetobacter baumannii in in vitro and murine thigh and lung infection models. Int J Antimicrob Agents. 2014;43(6):547–52.
Fish DN. Meropenem in the treatment of complicated skin and soft tissue infections. Ther Clin Risk Manag. 2006;2(4):401–15.
Zobell JT, Young DC, Waters CD, Ampofo K, Cash J, Marshall BC, et al. A survey of the utilization of anti-pseudomonal beta-lactam therapy in cystic fibrosis patients. Pediatr Pulmonol. 2011;46(10):987–90.
Kanra G. Experience with ampicillin/sulbactam in severe infections. J Int Med Res. 2002;30(Suppl. 1):20A-30A.
Fotakopoulos G, Makris D, Chatzi M, Tsimitrea E, Zakynthinos E, Fountas K. Outcomes in meningitis/ventriculitis treated with intravenous or intraventricular plus intravenous colistin. Acta Neurochir. 2016;158(3):603–10 (discussion 10).
Florescu DF, Qiu F, McCartan MA, Mindru C, Fey PD, Kalil AC. What is the efficacy and safety of colistin for the treatment of ventilator-associated pneumonia? A systematic review and meta-regression. Clin Infect Dis. 2012;54(5):670–80.
Bian X, Liu X, Feng M, Bergen PJ, Li J, Chen Y, et al. Enhanced bacterial killing with colistin/sulbactam combination against carbapenem-resistant Acinetobacter baumannii. Int J Antimicrob Agents. 2021;57(2): 106271.
Shi H, Lee JS, Park SY, Ko Y, Eom JS. Colistin plus carbapenem versus colistin monotherapy in the treatment of carbapenem-resistant Acinetobacter baumannii pneumonia. Infect Drug Resist. 2019;12:3925–34.
Maifiah MH, Creek DJ, Nation RL, Forrest A, Tsuji BT, Velkov T, et al. Untargeted metabolomics analysis reveals key pathways responsible for the synergistic killing of colistin and doripenem combination against Acinetobacter baumannii. Sci Rep. 2017;30(7):45527.
Pettit RS, Neu N, Cies JJ, Lapin C, Muhlebach MS, Novak KJ, et al. Population pharmacokinetics of meropenem administered as a prolonged infusion in children with cystic fibrosis. J Antimicrob Chemother. 2016;71(1):189–95.
Iosifidis E, Antachopoulos C, Ioannidou M, Mitroudi M, Sdougka M, Drossou-Agakidou V, et al. Colistin administration to pediatric and neonatal patients. Eur J Pediatr. 2010;169(7):867–74.
Goverman J, Weber JM, Keaney TJ, Sheridan RL. Intravenous colistin for the treatment of multi-drug resistant, gram-negative infection in the pediatric burn population. J Burn Care Res. 2007;28(3):421–6.
Lee CH, Tang YF, Su LH, Chien CC, Liu JW. Antimicrobial effects of varied combinations of meropenem, sulbactam, and colistin on a multidrug-resistant Acinetobacter baumannii isolate that caused meningitis and bacteremia. Microb Drug Resist. 2008;14(3):233–7.
Fan B, Guan J, Wang X, Cong Y. Activity of colistin in combination with meropenem, tigecycline, fosfomycin, fusidic acid, rifampin or sulbactam against extensively drug-resistant Acinetobacter baumannii in a murine thigh-infection model. PLoS One. 2016;11(6): e0157757.
Liu X, Zhao M, Chen Y, Bian X, Li Y, Shi J, et al. Synergistic killing by meropenem and colistin combination of carbapenem-resistant Acinetobacter baumannii isolates from Chinese patients in an in vitro pharmacokinetic/pharmacodynamic model. Int J Antimicrob Agents. 2016;48(5):559–63.
Saelim W, Changpradub D, Thunyaharn S, Juntanawiwat P, Nulsopapon P, Santimaleeworagun W. Colistin plus sulbactam or fosfomycin against carbapenem-resistant Acinetobacter baumannii: improved efficacy or decreased risk of nephrotoxicity? Infect Chemother. 2021;53(1):128–40.
Lim SMS, Heffernan AJ, Zowawi HM, Roberts JA, Sime FB. Semi-mechanistic PK/PD modelling of meropenem and sulbactam combination against carbapenem-resistant strains of Acinetobacter baumannii. Eur J Clin Microbiol Infect Dis. 2021;40(9):1943–52.
Paul M, Daikos GL, Durante-Mangoni E, Yahav D, Carmeli Y, Benattar YD, et al. Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: an open-label, randomised controlled trial. Lancet Infect Dis. 2018;18(4):391–400.
Rayner CR, Smith PF, Andes D, Andrews K, Derendorf H, Friberg LE, et al. Model-informed drug development for anti-Iifectives: state of the art and future. Clin Pharmacol Ther. 2021;109(4):867–91.
Thorsted A, Bouchene S, Tano E, Castegren M, Lipcsey M, Sjolin J, et al. A non-linear mixed effect model for innate immune response: In vivo kinetics of endotoxin and its induction of the cytokines tumor necrosis factor alpha and interleukin-6. PLoS ONE. 2019;14(2): e0211981.
Couet W, Gregoire N, Marchand S, Mimoz O. Colistin pharmacokinetics: the fog is lifting. Clin Microbiol Infect. 2012;18(1):30–9.
Martins FS, Zhu P, Heinrichs MT, Sy SKB. Physiologically based pharmacokinetic-pharmacodynamic evaluation of meropenem plus fosfomycin in paediatrics. Br J Clin Pharmacol. 2021;87(3):1012–23.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by a grant from Shandong Provincial Natural Science Foundation (ZR2019BC025).
Conflict of interest
CO is the owner of SunLife Biopharma, which is a private consulting firm. All other authors have nothing to disclose.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
All authors (1) contributed to the design of the study, acquisition, or analysis of data, (2) drafted or revised the article for intellectual content, and (3) approved the final version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, S., Zhang, J., Lv, Z. et al. Prediction of Tissue Exposures of Meropenem, Colistin, and Sulbactam in Pediatrics Using Physiologically Based Pharmacokinetic Modeling. Clin Pharmacokinet 61, 1427–1441 (2022). https://doi.org/10.1007/s40262-022-01161-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01161-y