Abstract
Somatic mutations are post-zygotic mutational event that leads to generation of two or more genotypes within an individual. With the recent advances in genomic technologies, there is an increasing recognition of the role of somatic mosaicism in Mendelian disease. Somatic mutation can occur at the chromosomal or the DNA sequence level and the distribution of somatic mosaicism among tissues depends on the timing of the mutation during fetal development. Certain types of somatic mutations are lethal when present in the germline and hence, are only seen in the somatic state, while there are other somatic mutations that have a milder phenotype than when present in the germline. Presence of somatic mutations can also modulate the clinical phenotype of an individual in certain diseases. In this review, we discuss the recent updates on somatic mosaicism in Mendelian diseases, types of somatic mutations, and methods to detect these somatic mutations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mendelian diseases, also known as monogenic diseases, are considered to be rare individually, but collectively occur at a rate of 40–82 per 1000 live births, with an estimated 7.9 million children being born annually with a serious birth defect of genetic or partially genetic origin [1, 2]. Mendelian diseases are disorders caused by variations at a single genetic locus and include diseases such as tuberous sclerosis complex and cystic fibrosis, among others. These variations may be inherited or occur de novo. Inherited mutations are present in all the cells of the affected individual and are present in one or both the parents. De novo mutations refer to mutations that are present only in the proband but are absent in the parents. Typically, these de novo mutations occur for the first time in a parent germ cell prior to fertilization and are inherited by all cells of the offspring. Somatic mutations, a sub-type of de novo mutations, are post-zygotic mutational events that lead to an individual having two or more populations of cells with distinct genotypes, despite developing from a single fertilized egg [3••, 4••].
Somatic mutations lead to an individual being mosaic, with only a subset of cells harboring the mutation. These mutations are absent in the parents, and depending on the timing of mutation with respect to embryonic development, may affect cells across all cell types or may be present in only a few specific cell types [3••, 5, 6•]. While the role of somatic mutation in cancer cells is well established [7], the appreciation of an analogous role for somatic mutations that occur randomly during the normal mitotic cell divisions of embryonic development, and hence present in clones of cells in one or more tissues of the body, has been relatively recent.
With advances in genomic technologies, there has been an expansion in our knowledge of types of tissues in which somatic mutations have been detected as well as the kind of mutations being detected. Somatic mutations could reflect point mutations (also known as single nucleotide variants or SNVs), insertions/deletions (indels), copy number variants (CNVs) (including chromosomal aneuploidy), short tandem repeats (STRs), and transposable element variants. Here we will review the recent literature about the emerging role of somatic mutations in Mendelian disease.
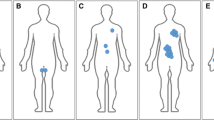
Embryology: Development and Distribution of Somatic Mutations
As mosaicism is caused by mitotic error post fertilization, we will briefly discuss the events of early fetal development as this is essential to interpreting and understanding mosaicism (Fig. 1). Post fertilization, the zygote undergoes successive mitoses to produce a ball of cells, which then produces the blastocyst. The outermost layer of the blastocyst produces the placental tissue and the inner cell mass gives rise to the embryo. Initially, the embryo consists of two different cell layers—epiblast and hypoblast. The epiblast differentiates into the ectoderm, mesoderm, and endoderm, while hypoblast gives rise to the amniotic cavity. Structures of ectodermal origin include the central nervous system, facial structures, and the extremities, including skin. The mesoderm differentiates into the cardiac, abdominal, and urogenital structures and hematopoietic cells. The endoderm gives rise to epithelial tissues, including the lining of the urinary tract and lung [8].
Early human fetal development from zygote (day 0) to the formation of embryonic mesoderm, endoderm, and ectoderm (day 16). The mesoderm differentiates into the cardiac, abdominal, and urogenital structures and hematopoietic cells. The endoderm gives rise to epithelial tissues, including the lining of the urinary tract and lung. The ectoderm differentiates into the central nervous system, facial structures, and the extremities, including skin. Timing of the mutational event determines the distribution of the somatic mutation across different tissues
Somatic mutations that develop in the early post-zygotic stage will be distributed across different tissue types. The mutations will likely be detected by analysis of more accessible tissue, such as the peripheral blood leukocytes. On the other hand, some mutations develop later in fetal development and hence, direct examination of the affected tissue would provide the best chance of detecting the mutation. In these instances, analysis of peripheral blood leukocytes would be unrevealing.
Somatic Mutations in Mendelian Diseases
“Single Hit” Somatic Mutations
For Mendelian diseases that manifest in the haploinsufficient state, damaging protein-altering mutations in one allele (single hit) can lead to disease. When these mutations develop post fertilization, it leads to somatic mosaicism. Some of the de novo somatic mutations are referred to as ‘obligatory’ somatic mutations, as they are lethal when present in the germline and have only been described in the mosaic state. These disorders tend to be sporadic with no evidence of familial clustering. These obligatory somatic mutations have traditionally been described in cancers, where the somatic mutation confers growth advantage to the tumor tissue leading to uncontrolled proliferation. A tumor tissue may have thousands of mutations—only a subset of these, referred to as “driver” mutations, have been causally implicated in oncogenesis, while the remainder, referred to as “passenger” mutations, do not directly contribute to oncogenesis [9, 10]. On the other hand, ‘obligatory’ somatic mutations in Mendelian disorders typically involve only one genetic locus and include disorders such as McCune Albright syndrome (caused by activating mutations in GNAS) [11], Proteus syndrome (caused by activating mutations in AKT1) [12], and Sturge-Weber syndrome (caused by mutations in GNAQ) [13].
Somatic mutations have also been observed in a fraction of patients with traditional Mendelian diseases such as tuberous sclerosis complex (caused by mutations in TSC1/TSC2) [14], incontinentia pigmenti (caused by mutations in NEMO) [15], double cortex (caused by mutations in DCX, LIS1) [16, 17], and periventricular nodular heterotopia (caused by mutations in FLNA) [18, 19]. Similarly, a case of sporadic, early onset Alzheimer's disease has been attributed to a somatic mosaic presenilin-1 mutation present in the brain [20] and another case of sporadic Creutzfeldt–Jakob disease was caused by an early embryonic somatic mutation identified by the presence of three alleles for the gene encoding the major prion protein PrP [21]. Somatic mutations in alpha-synuclein have been reported in association with Parkinson's disease [22]. These individuals have a milder phenotype compared to the individuals with germline mutations in the same genes [6•, 18].
“Second Hit” Mutations Produce Mosaicism
In several dominantly inherited conditions, an individual exhibits a heterozygous germline variant, present in all cells, with a somatic second mutation leading to overgrowth of specific tissues, as per the “two hit” model of Knudson [23]. This “second hit” could account for the variable expressivity in several of the dominantly inherited disorders. One of the classic examples of this form of second hit somatic mutation is neurofibromatosis type 1 (NF1), which is characterized by germline mutations in the gene NF1. These neurofibromas have been reported to develop when a second mutation develops in the other NF1 allele [24]. Similarly, in tuberous sclerosis complex (TSC), somatic second mutations have been shown in non-nervous system tumors of TSC, subependymal giant cell astrocytomas as well as non-cancerous cortical tubers in patients with TSC [14, 25].
Diseases Modulated by Somatic Mutations
In addition to directly causing disease, somatic mutations have been shown to modify the disease process in some cases. Some neurodegenerative diseases, including Huntington disease, dentatorubral-pallidoluysian atrophy, and Fragile X syndrome, are caused by inheritance of microsatellite repeats that are highly unstable and can exhibit marked somatic heterogeneity in repeat lengths across brain regions and tissues of affected individual [26–28]. DEPDC5 is a well-recognized cause of autosomal dominant focal epilepsy and imaging of individuals with mutations in DEPDC5 is typically normal. Recently, Scheffer and colleagues described a series of individuals with DEPDC5-related focal epilepsy who also had a range of brain malformations [29]. The presence of brain malformations in individuals with DEPDC5-related epilepsy could be partially explained by the “second hit” phenomenon with a somatic mutation in the other allele of DEPDC5 or another gene in the related pathway causing the malformations. Direct analysis of the brain tissues of these individuals could provide support for this hypothesis [30].
Gonadal Mosaicism—Mutation in the Parental Germline Cells
While somatic mutations are typically post-fertilization de novo events, in some instances, the de novo event occurs in the parent gonadal tissue after the germline cells have separated from the somatic cells during their embryological development. This leads to a mutation that is confined to the germline cells and may be present in only some of the germline cells. This is referred to as germline or gonadal mosaicism. In this scenario, although the parent is healthy (as his/her somatic cells are unaffected), he or she is at risk of having another affected child with the same disorder. Recurrence risk estimates due to gonadal mosaicism vary across different diseases and are typically around 2–5 % [31, 32], but may be higher in some conditions (such as Duchenne muscular dystrophy) [33, 34].
Types of Somatic Variants
Large-Scale Chromosomal Abnormalities
Chromosomal alterations such as whole chromosome aneuploidy, segmental aneuploidy, and structural alterations have been historically identified by cytogenetic analyses (Table 1). Chromosomal abnormalities are a fairly common cause of developmental disorders and affect 1 in 200 liveborn individuals and up to 50 % of spontaneous miscarriages [4••].
Aneuploidy of chromosomes 13, 18, 21 and sex chromosomes accounts for nearly all the aneuploidy-related live births. Sex chromosome mosaicism usually arises from post-zygotic mitotic non-disjunction. Aneuploidy of other chromosomes is usually lethal to the developing fetus and is only observed in the mosaic state for some of the chromosomes (including 1, 2, 5, 8, 9, 16, 17, and 22) [3••]. These individuals have a variable phenotype as the severity of the disorder is determined by the particular chromosome involved as well as by the proportion of cells in the body carrying the aneuploidy. For example, mosaic trisomy 21, affecting 1 % of the cases of Down syndrome, leads to a less severe phenotype compared to germline trisomy 21 [3••, 4••].
Mosaicism for structural abnormalities is less common than aneuploidy, but has been identified in the form of translocations, deletions, duplications, inversions, ring chromosomes, and isochromosomes [35–37]. Isochromosomes are structurally abnormal chromosomes created by the presence of two copies of one of the arms of a chromosome, while the other arm is missing. Four well-recognized isochromosome syndromes include Pallister–Killian syndrome (isochromosome 12p), cat-eye syndrome (isochromosome 22q), isochromosome 15q11, and isochromosome 18p. As the level of mosaicism in different tissue varies across individuals, all have been associated with variable degree of developmental delay and intellectual disability [4••].
Copy Number Variants
Recent advances in genomic tools such as microarray analysis have improved the resolution of cytogenomic imbalances to be detected at a submicroscopic level and, in some instances, to individual exons. These aberrations are referred to as copy number variants (CNVs). Germline CNVs have been reported in 10–15 % of patients with developmental delay and/or autism spectrum disorder [38], while mosaic CNVs have been reported in 0.5–3.74 % of patients with congenital and developmental anomalies [39•, 40, 41]. Mosaic CNV involving chromosome 1q has been well described in individuals with hemimegalencephaly [42, 43] and more recently in focal cortical dysplasia [44, 45]. Copy number variation has been noted across different tissues from the same individual [46] and mosaic CNVs have been observed in monozygotic twins with discordant phenotypes [47].
Single Nucleotide Variants
Mutations at the level of the nucleotide, either base substitutions or small insertions or deletions (indels), in the genomic DNA may lead to abnormal mRNA and consequent abnormal protein production. Single nucleotide variants (SNVs) can either lead to loss of function (missense or splicing variants), gain of function (missense), or absence of protein (nonsense, frameshift, canonical splicing variants). Mosaic SNVs have been reported in a range of disorders (Table 2), including those associated with brain malformations [16–19, 43, 48, 49], Proteus syndrome [12], CLOVES syndrome [50], Sturge–Weber syndrome [13], and verrucous venous malformation [51], among others. Mosaic SNVs in the AKT-PIK3-mTOR pathway result in overgrowth and have been hypothesized to be lethal when constitutional as they disrupt early embryonic development. On the other hand, the mosaic variants in DCX, LIS1, TSC1, FLNA, etc. present as milder phenotypes compared to when they present as germline [3••]. Mosaicism has also been described in disorders related to developmental delay and/or epilepsy syndromes such as Pitt–Hopkins syndrome (caused by mutations in TCF4) [ 52], Rett syndrome (caused by mutations in MeCP2) [53], Cornelia de Lange syndrome (caused by mutations in NIPBL, SMC1A, SMC3) [54, 55], X-linked Charcot–Marie–Tooth type 1 (caused by mutations in GJB1) [56], FOXG1 syndrome [57], benign familial neonatal seizures (KCNQ2) [58], and Temple-Baraitser syndrome (KCNH1) [59]. More recently, mosaicism has been described in X-linked Alport syndrome(COL4A5) [60], a form of nephropathy, where individuals with the mosaic variant were either asymptomatic or very mildly affected.
Recurrence Risk and Genetic Counseling
Management of individuals with Mendelian diseases is restricted to anticipation of potential complications with limited ability to intervene to alter the natural history of the disease. Hence, recurrence risk counseling is the most effective intervention in clinical genetics. Detection of somatic mutation as a cause of disease in an individual suggests a post-fertilization event and hence, the risk of recurrence in the siblings is low and similar to the general population. The risk to the offspring of the proband depends on the timing of the somatic mutation. If the mutation developed prior to separation of germinal cells and the somatic cells, then there is a 50 % risk to the proband of having an affected child. For conditions which are lethal when constitutional, the pregnancy will be non-viable if the fetus inherits the mutated allele. On the other hand, if the mutation developed after the germinal cells had separated and is confined to the somatic cells, then there is no increased risk to the offspring.
Detection of Somatic Variants
The tools required to detect somatic variants depend on the type of variant (Table 3).
Copy Number Variants
Karyotype and Fluorescence In Situ Hybridization
Cytogenetic analysis is the study of banded pattern of the chromosomes during metaphase of the cell cycle. It is carried out on a cell-by-cell basis and hence, mosaicism is easily recognized when only a few cells carry the chromosomal abnormality. The cytogenetic detection of low-level mosaicism is a challenge as adequate number of cells must be counted. This analysis can detect large-scale chromosomal abnormalities, most commonly, aneuploidy. However, the limit of detection of chromosomal aberration is around 5 Mb and CNVs below 5 Mb will be missed on routine cytogenetic analysis [4••].
Fluorescence in situ hybridization (FISH), on the other hand, utilizes tagged probes that bind to specific chromosome of interest and allows for detection of numeric and structural abnormalities, including submicroscopic (below 5 Mb) copy number changes. An advantage of FISH over chromosome analysis is that FISH does not require actively dividing cells and hence, can be performed in both the interphase and metaphase of the cell cycle. However, hybridization-related artifacts are common, and the high rates of mosaic aneuploidy reported with the use of karyotyping and FISH [61] have not been replicated in recent single-cell studies [42, 62••].
Chromosome Microarray Analysis
Microarray-based techniques have replaced conventional cytogenetic analysis in many instances as they are able to detect submicroscopic genomic imbalances or CNVs and, unlike FISH, allow for interrogation of CNVs across the entire genome. In addition, samples do not require culturing and cells in all cell cycle phases are analyzed and hence, the technique is less prone to artifacts [4••]. Types of microarray analyses include array comparative genomic hybridization (aCGH) which detects copy number aberrations, genome-wide single nucleotide polymorphism (SNP) arrays, which can analyze both SNPs and CNVs, and targeted high-density arrays focusing on a few known and candidate regions. aCGH is able to detect somatic CNVs when variant cells constitute >10 % of the total cell population [40]. SNP arrays are much more sensitive for mosaicism detection and mosaicism involving <5 % of cells has been detected using these arrays [41, 63, 64]. As SNP arrays are able to analyze the zygosity of the SNPs, they aid in understanding the genetic mechanism by which mosaicism has occurred. Targeted high-density arrays allow for greater precision in detection and quantification of mosaicism [65•].
Single-Cell Copy Number Analyses
Single-cell analysis allows one to isolate single nuclei [66•] that can then be subjected to amplification followed either by microarray or low-coverage whole-genome sequencing for CNV analysis. Single-cell genomic analyses have demonstrated that somatic aneuploidy in adult neurons is less common than previously estimated, while somatic CNVs are not that rare [67].
Digital Droplet PCR
Digital droplet PCR (ddPCR) provides the ability to quantify nucleic acids with high precision and sensitivity [68]. This method has been used successfully to reproducibly and reliably detect the presence of trisomy 21 down to 2 % mosaicism [69]. ddPCR was used to confirm the presence of low-frequency mosaic CNVs in the induced pluripotent stem cells derived from fibroblasts, when standard techniques were unable to detect these CNVs [70].
Single Nucleotide Variants, Including Insertions and Deletions
Sanger Sequencing
Sanger sequencing is the most widely used method for detection of SNVs but is unable to detect mosaic alleles below a threshold of 15–20 % [71] and can miss a significant proportion of low-level mosaic mutations [6•]. In addition, mosaic mutations at higher allele fractions are miscalled as germline, highlighting the limitations of Sanger sequencing in detecting mosaicism on both ends of the spectrum [6•].
Next-Generation Sequencing
Next-generation sequencing (NGS) is a high-throughput technique that allows parallel analysis of the multiple regions of the genome [72, 73]. Whole exome and genome sequencing (WES/WGS) technologies have allowed an exponential increase in our understanding of human genetic disorders and have been reported to detect somatic mutations in rare instances [74–76]. However, due to inhomogeneities in library preparation and an average depth of 40–80×, WES/WGS may miss somatic mutations, especially when the read depth is low. On the other hand, deep-targeted sequencing allows one to interrogate a smaller portion of the genome to much greater depths and has been used successfully to detect low-level mosaicism as low as 5 % [6•, 49]. In addition, as many as 30 % of the mutations associated with unexplained brain malformations are somatic, the majority of which would be missed on Sanger sequencing and even on routine WES [6•, 77]. An alternative to performing deep sequencing is bioinformatic alteration of exome sequencing pipelines or performing next-generation sequencing on paired samples (affected and unaffected tissue), both of which have been used successfully to detect somatic mutations in cancerous [7] as well as non-cancerous disorders [12, 48].
Subcloning Followed by Sanger Sequencing
Subcloning of the amplified PCR products into a vector followed by transformation into a bacterium such as E. coli leads to formation of multiple colonies of the bacteria, each containing either the wild type or the mutant allele. Sanger sequencing of multiple individual colonies not only allows for confirmation of the presence of the mosaic variant, but also allows for quantification of the level of mosaicism [6•, 43].
Single-Cell Sequencing
Isolation, genome amplification, and sequencing of single cells allows for quantification of the level of mosaicism as well as to determine which cell lineage is affected. In an individual with hemimegalencephaly, bulk tissue analysis showed somatic point mutation in AKT3 at ~35 % mosaicism, while single-cell sequencing revealed the mutation in 39 % of neuronal nuclei and 27 % of non-neuronal nuclei. This suggests that the mutational event occurred in an early neocortical progenitor cell [66•]. This was consistent with the radiological phenotype of the individual that showed involvement of both gray and white matter [43].
Mass Spectrometry
Using mass spectrometry, Sequenom MassARRAY iPLEX platform allows a high-throughput method of validating and quantifying somatic point mutations in a given sample [78, 79].
Conclusion
The role of somatic mutations in Mendelian disease is still under appreciated. Somatic mutations can cause diseases by ‘single hit’ mechanism, ‘two hit’ mechanism, and by disease process modulation. The mutations can be in large chromosomal regions, copy number variants or single nucleotide variants. The disease presentations are wide ranging but the phenotype tends to be less severe compared to when the mutation is constitutional. Newer genomic technologies such as single-cell sequencing and deep next-generation sequencing will allow systematic measurement of somatic mutation rates in different Mendelian diseases. This will allow us to estimate the prevalence of somatic mutations as a cause of Mendelian disorders, and to understand to what extent somatic mutations modify the pathogenesis of Mendelian diseases. With this knowledge, we can counsel families more precisely.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
MoDBD Foundation. Global report on birth defects: the hidden toll of dying and disabled children. White Plains: March of Dimes; 2006.
Baird PA, Anderson TW, Newcombe HB, Lowry RB. Genetic disorders in children and young adults: a population study. Am J Hum Genet. 1988;42(5):677–93.
•• Poduri A, Evrony GD, Cai X, Walsh CA. Somatic mutation, genomic variation, and neurological disease. Science. 2013;341(6141):1237758. This reference reviews the literature around somatic mosaicism in neurological disorders.
•• Biesecker LG, Spinner NB. A genomic view of mosaicism and human disease. Nat Rev Genet. 2013;14(5):307–20. This reference reviews the literature around somatic mosaicism in Mendelian disorders.
Kennedy SR, Loeb LA, Herr AJ. Somatic mutations in aging, cancer and neurodegeneration. Mech Ageing Dev. 2012;133(4):118–26.
• Jamuar SS, Lam AT, Kircher M, et al. Somatic mutations in cerebral cortical malformations. N Engl J Med. 2014;371(8):733–43. A systematic approach to quantifying the prevalence of somatic mosaicism in undiagnosed brain malformation using deep sequencing.
Watson IR, Takahashi K, Futreal PA, Chin L. Emerging patterns of somatic mutations in cancer. Nat Rev Genet. 2013;14(10):703–18.
Gardner RJS, G.R.; Shaffer, L.G. Chromosome abnormalities and Genetic Counseling. Chromosome abnormalities and Genetic Counseling. Oxford: Oxford University Press; 2011.
Greenman C, Stephens P, Smith R, et al. Patterns of somatic mutation in human cancer genomes. Nature. 2007;446(7132):153–8.
Pleasance ED, Cheetham RK, Stephens PJ, et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nature. 2010;463(7278):191–6.
Weinstein LS, Shenker A, Gejman PV, Merino MJ, Friedman E, Spiegel AM. Activating mutations of the stimulatory G protein in the McCune-Albright syndrome. N Engl J Med. 1991;325(24):1688–95.
Lindhurst MJ, Sapp JC, Teer JK, et al. A mosaic activating mutation in AKT1 associated with the Proteus syndrome. N Engl J Med. 2011;365(7):611–9.
Shirley MD, Tang H, Gallione CJ, et al. Sturge-Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. N Engl J Med. 2013;368(21):1971–9.
Niida Y, Stemmer-Rachamimov AO, Logrip M, et al. Survey of somatic mutations in tuberous sclerosis complex (TSC) hamartomas suggests different genetic mechanisms for pathogenesis of TSC lesions. Am J Hum Genet. 2001;69(3):493–503.
Smahi A, Courtois G, Vabres P, et al. Genomic rearrangement in NEMO impairs NF-kappaB activation and is a cause of incontinentia pigmenti. The International Incontinentia Pigmenti (IP) Consortium. Nature. 2000;405(6785):466–72.
Gleeson JG, Minnerath S, Kuzniecky RI, et al. Somatic and germline mosaic mutations in the doublecortin gene are associated with variable phenotypes. Am J Hum Genet. 2000;67(3):574–81.
Sicca F, Kelemen A, Genton P, et al. Mosaic mutations of the LIS1 gene cause subcortical band heterotopia. Neurology. 2003;61(8):1042–6.
Parrini E, Mei D, Wright M, Dorn T, Guerrini R. Mosaic mutations of the FLN1 gene cause a mild phenotype in patients with periventricular heterotopia. Neurogenetics. 2004;5(3):191–6.
Guerrini R, Mei D, Sisodiya S, et al. Germline and mosaic mutations of FLN1 in men with periventricular heterotopia. Neurology. 2004;63(1):51–6.
Beck JA, Poulter M, Campbell TA, et al. Somatic and germline mosaicism in sporadic early-onset Alzheimer’s disease. Hum Mol Genet. 2004;13(12):1219–24.
Alzualde A, Moreno F, Martinez-Lage P, et al. Somatic mosaicism in a case of apparently sporadic Creutzfeldt-Jakob disease carrying a de novo D178 N mutation in the PRNP gene. Am J Med Genet B Neuropsychiatr Genet. 2010;153B(7):1283–91.
Proukakis C, Houlden H, Schapira AH. Somatic alpha-synuclein mutations in Parkinson’s disease: hypothesis and preliminary data. Mov Disord. 2013;28(6):705–12.
Knudson AG Jr. Mutation and cancer: statistical study of retinoblastoma. Proc Natl Acad Sci U S A. 1971;68(4):820–3.
Garcia-Linares C, Fernandez-Rodriguez J, Terribas E, et al. Dissecting loss of heterozygosity (LOH) in neurofibromatosis type 1-associated neurofibromas: importance of copy neutral LOH. Hum Mutat. 2011;32(1):78–90.
Qin W, Chan JA, Vinters HV, et al. Analysis of TSC cortical tubers by deep sequencing of TSC1, TSC2 and KRAS demonstrates that small second-hit mutations in these genes are rare events. Brain Pathol. 2010;20(6):1096–105.
Hashida H, Goto J, Suzuki T, et al. Single cell analysis of CAG repeat in brains of dentatorubral-pallidoluysian atrophy (DRPLA). J Neurol Sci. 2001;190(1–2):87–93.
Hellenbroich Y, Schwinger E, Zuhlke C. Limited somatic mosaicism for Friedreich’s ataxia GAA triplet repeat expansions identified by small pool PCR in blood leukocytes. Acta Neurol Scand. 2001;103(3):188–92.
Ito Y, Tanaka F, Yamamoto M, et al. Somatic mosaicism of the expanded CAG trinucleotide repeat in mRNAs for the responsible gene of Machado-Joseph disease (MJD), dentatorubral-pallidoluysian atrophy (DRPLA), and spinal and bulbar muscular atrophy (SBMA). Neurochem Res. 1998;23(1):25–32.
Scheffer IE, Heron SE, Regan BM, et al. Mutations in mammalian target of rapamycin regulator DEPDC5 cause focal epilepsy with brain malformations. Ann Neurol. 2014;75(5):782–7.
Poduri A. DEPDC5 does it all: shared genetics for diverse epilepsy syndromes. Ann Neurol. 2014;75(5):631–3.
van der Meulen MA, van der Meulen MJ, te Meerman GJ. Recurrence risk for germinal mosaics revisited. J Med Genet. 1995;32(2):102–4.
Campbell IM, Yuan B, Robberecht C, et al. Parental somatic mosaicism is underrecognized and influences recurrence risk of genomic disorders. Am J Hum Genet. 2014;95(2):173–82.
Bakker E, Veenema H, Den Dunnen JT, et al. Germinal mosaicism increases the recurrence risk for ‘new’ Duchenne muscular dystrophy mutations. J Med Genet. 1989;26(9):553–9.
Helderman-van den Enden AT, de Jong R, den Dunnen JT, et al. Recurrence risk due to germ line mosaicism: Duchenne and Becker muscular dystrophy. Clin Genet. 2009;75(5):465–72.
Conlin LK, Kramer W, Hutchinson AL, et al. Molecular analysis of ring chromosome 20 syndrome reveals two distinct groups of patients. J Med Genet. 2011;48(1):1–9.
Hsu LY, Yu MT, Richkind KE, et al. Incidence and significance of chromosome mosaicism involving an autosomal structural abnormality diagnosed prenatally through amniocentesis: a collaborative study. Prenat Diagn. 1996;16(1):1–28.
Gijsbers AC, Dauwerse JG, Bosch CA, et al. Three new cases with a mosaicism involving a normal cell line and a cryptic unbalanced autosomal reciprocal translocation. Eur J Med Genet. Jul-Aug. 2011;54(4):e409–12.
Miller DT, Adam MP, Aradhya S, et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet. 2010;86(5):749–64.
• Cheung SW, Shaw CA, Scott DA, et al. Microarray-based CGH detects chromosomal mosaicism not revealed by conventional cytogenetics. Am J Med Genet A. 2007;143A(15):1679–86. Important in demonstrating role of microarray to detect mosaic copy number variants.
Ballif BC, Rorem EA, Sundin K, et al. Detection of low-level mosaicism by array CGH in routine diagnostic specimens. Am J Med Genet A. 2006;140(24):2757–67.
Conlin LK, Thiel BD, Bonnemann CG, et al. Mechanisms of mosaicism, chimerism and uniparental disomy identified by single nucleotide polymorphism array analysis. Hum Mol Genet. 2010;19(7):1263–75.
Cai X, Evrony GD, Lehmann HS, et al. Single-cell, genome-wide sequencing identifies clonal somatic copy-number variation in the human brain. Cell Rep. 2014;8(5):1280–9.
Poduri A, Evrony GD, Cai X, et al. Somatic activation of AKT3 causes hemispheric developmental brain malformations. Neuron. 2012;74(1):41–8.
Conti V, Pantaleo M, Barba C, et al. Focal dysplasia of the cerebral cortex and infantile spasms associated with somatic 1q21.1-q44 duplication including the AKT3 gene. Clin Genet. 2014. doi:10.1111/cge.12476.
Liu J, Reeves C, Michalak Z, et al. Evidence for mTOR pathway activation in a spectrum of epilepsy-associated pathologies. Acta Neuropathol Commun. 2014;2:71.
Piotrowski A, Bruder CE, Andersson R, et al. Somatic mosaicism for copy number variation in differentiated human tissues. Hum Mutat. 2008;29(9):1118–24.
Bruder CE, Piotrowski A, Gijsbers AA, et al. Phenotypically concordant and discordant monozygotic twins display different DNA copy-number-variation profiles. Am J Hum Genet. 2008;82(3):763–71.
Lee JH, Huynh M, Silhavy JL, et al. De novo somatic mutations in components of the PI3K-AKT3-mTOR pathway cause hemimegalencephaly. Nat Genet. 2012;44(8):941–5.
Riviere JB, Mirzaa GM, O’Roak BJ, et al. De novo germline and postzygotic mutations in AKT3, PIK3R2 and PIK3CA cause a spectrum of related megalencephaly syndromes. Nat Genet. 2012;44(8):934–40.
Kurek KC, Luks VL, Ayturk UM, et al. Somatic mosaic activating mutations in PIK3CA cause CLOVES syndrome. Am J Hum Genet. 2012;90(6):1108–15.
Couto JA, Vivero MP, Kozakewich HP, et al. A somatic MAP3K3 mutation is associated with verrucous venous malformation. Am J Hum Genet. 2015;96(3):480–6.
Kousoulidou L, Tanteles G, Moutafi M, Sismani C, Patsalis PC, Anastasiadou V. 263.4 kb deletion within the TCF4 gene consistent with Pitt–Hopkins syndrome, inherited from a mosaic parent with normal phenotype. Eur J Med Genet. 2013;56(6):314–8.
Topcu M, Akyerli C, Sayi A, et al. Somatic mosaicism for a MECP2 mutation associated with classic Rett syndrome in a boy. Eur J Hum Genet. Jan 2002;10(1):77–81.
Huisman SA, Redeker EJ, Maas SM, Mannens MM, Hennekam RC. High rate of mosaicism in individuals with Cornelia de Lange syndrome. J Med Genet. May 2013;50(5):339–44.
Ansari M, Poke G, Ferry Q, et al. Genetic heterogeneity in Cornelia de Lange syndrome (CdLS) and CdLS-like phenotypes with observed and predicted levels of mosaicism. J Med Genet. Oct 2014;51(10):659–68.
Borgulova I, Mazanec R, Sakmaryova I, Havlova M, Safka Brozkova D, Seeman P. Mosaicism for GJB1 mutation causes milder Charcot–Marie–Tooth X1 phenotype in a heterozygous man than in a manifesting heterozygous woman. Neurogenetics. 2013;14(3–4):189–95.
Diebold B, Delepine C, Nectoux J, Bahi-Buisson N, Parent P, Bienvenu T. Somatic mosaicism for a FOXG1 mutation: diagnostic implication. Clin Genet. 2014;85(6):589–91.
Milh M, Lacoste C, Cacciagli P, et al. Variable clinical expression in patients with mosaicism for KCNQ2 mutations. Am J Med Genet A. 2015. doi:10.1002/ajmg.a.37152.
Simons C, Rash LD, Crawford J, et al. Mutations in the voltage-gated potassium channel gene KCNH1 cause Temple-Baraitser syndrome and epilepsy. Nat Genet. 2015;47(1):73–7.
Fu XJ, Nozu K, Kaito H, et al. Somatic mosaicism and variant frequency detected by next-generation sequencing in X-linked Alport syndrome. Eur J Hum Genet. 2015. doi:10.1038/ejhg.2015.113.
Rehen SK, Yung YC, McCreight MP, et al. Constitutional aneuploidy in the normal human brain. J Neurosci. 2005;25(9):2176–80.
•• Knouse KA, Wu J, Whittaker CA, Amon A. Single cell sequencing reveals low levels of aneuploidy across mammalian tissues. Proc Natl Acad Sci USA. 2014;111(37):13409–14. Review on structural mosaic variants and techniques to detect mosaicism.
Dumanski JP, Piotrowski A. Structural genetic variation in the context of somatic mosaicism. Methods Mol Biol. 2012;838:249–72.
Rodriguez-Santiago B, Malats N, Rothman N, et al. Mosaic uniparental disomies and aneuploidies as large structural variants of the human genome. Am J Hum Genet. 2010;87(1):129–38.
• Pham J, Shaw C, Pursley A, et al. Somatic mosaicism detected by exon-targeted, high-resolution aCGH in 10,362 consecutive cases. Eur J Hum Genet. 2014;22(8):969–78. Used single cell sequencing to demonstrate that L1 retrotransposition is a rare event in human brain, unlike what was considered previously.
• Evrony GD, Cai X, Lee E, et al. Single-neuron sequencing analysis of L1 retrotransposition and somatic mutation in the human brain. Cell. 2012;151(3):483–96. Used single cell sequencing to demonstrate somatic CNVs in “normal” human brain.
Cai X, Evrony GD, Lehmann HS, et al. Single-cell, genome-wide sequencing identifies clonal somatic copy-number variation in the human brain. Cell Rep. 2014;8(5):1280–9.
Pinheiro LB, Coleman VA, Hindson CM, et al. Evaluation of a droplet digital polymerase chain reaction format for DNA copy number quantification. Anal Chem. 2012;84(2):1003–11.
Heyries KA, Tropini C, Vaninsberghe M, et al. Megapixel digital PCR. Nat Methods. 2011;8(8):649–51.
Abyzov A, Mariani J, Palejev D, et al. Somatic copy number mosaicism in human skin revealed by induced pluripotent stem cells. Nature. 2012;492(7429):438–42.
Rohlin A, Wernersson J, Engwall Y, Wiklund L, Bjork J, Nordling M. Parallel sequencing used in detection of mosaic mutations: comparison with four diagnostic DNA screening techniques. Hum Mutat. 2009;30(6):1012–20.
Ng SB, Turner EH, Robertson PD, et al. Targeted capture and massively parallel sequencing of 12 human exomes. Nature. 2009;461(7261):272–6.
Ng SB, Buckingham KJ, Lee C, et al. Exome sequencing identifies the cause of a mendelian disorder. Nat Genet. 2010;42(1):30–5.
Pagnamenta AT, Lise S, Harrison V, et al. Exome sequencing can detect pathogenic mosaic mutations present at low allele frequencies. J Hum Genet. 2012;57(1):70–2.
Pritchard CC, Smith C, Marushchak T, et al. A mosaic PTEN mutation causing Cowden syndrome identified by deep sequencing. Genet Med. 2013;15(12):1004–7.
Gilissen C, Hehir-Kwa JY, Thung DT, et al. Genome sequencing identifies major causes of severe intellectual disability. Nature. 2014;511(7509):344–7.
Tapper WJ, Foulds N, Cross NC, et al. Megalencephaly syndromes: exome pipeline strategies for detecting low-level mosaic mutations. PLoS ONE. 2014;9(1):e86940.
Gabriel S, Ziaugra L, Tabbaa D. SNP genotyping using the Sequenom MassARRAY iPLEX platform. Curr Protoc Hum Genet. 2009;Chapter 2:Unit 2 12.
Lee JH, Huynh M, Silhavy JL, et al. De novo somatic mutations in components of the PI3K-AKT3-mTOR pathway cause hemimegalencephaly. Nat Genet. 2012;44(8):941–5.
Acknowledgments
Dr Saumya Shekhar Jamuar is supported by the Nurturing Clinician Scientist Scheme, Paediatrics Academic Clinical Programme, Singhealth Duke-NUS Graduate Medical School, Singapore.
Disclosure
TW Ting, R Shahdadpuri, and SS Jamuar all declare no conflicts of interest.
Human and Animal Rights and Informed Consent
All studies by Saumya Shekhar Jamuar involving animal and/or human subjects were performed after approval by the appropriate institutional review boards. When required, written informed consent was obtained from all participants.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Clinical Genetics.
Rights and permissions
About this article
Cite this article
Ting, T.W., Shahdadpuri, R. & Jamuar, S.S. Mosaicism in Traditional Mendelian Diseases. Curr Genet Med Rep 3, 101–109 (2015). https://doi.org/10.1007/s40142-015-0071-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40142-015-0071-0