Abstract
NF1 affects ~1/3,000 individuals, irrespective of gender or ethnic background, and as many as 30–50 % of these patients present as “sporadic” or “founder” patients. A small fraction of these “sporadic” patients present with mosaicism for a “first hit” NF1 mutation. The precise frequency of mosaicism in NF1 is unknown, but first estimates indicate it may affect ~10 % of the patients with a total gene deletion. Here, we provide an overview of the different forms of mosaicism: gonadal or germline mosaicism, gonosomal mosaicism affecting both gonads and somatic cells, and somatic mosaicism, which may be “generalized” in phenotypic appearance or “localized” with a “segmental” distribution. Revertant mosaicism is discussed as well, though it has not yet been demonstrated in NF1 patients. Molecular data reported in the literature, proving the presence of an NF1 “first hit” mutation affecting only a portion of the body cells, depending on the timing of the mutational “first hit” during development, are summarized and the mutational spectrum and phenotype identified in mosaic NF1 patients are reviewed. The implications of our current understanding of mosaicism for molecular diagnostics in NF1 are discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Malignant Peripheral Nerve Sheath Tumor
- Glomus Tumor
- Somatic Mosaicism
- Plexiform Neurofibroma
- Sporadic Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
12.1 Introduction
Neurofibromatosis type 1 (NF1, MIM 162200) is a common autosomal dominant genetic disorder affecting ~1/3,000 individuals worldwide (Huson et al. 1989). NF1 is a progressive disorder, with more symptoms typically developing with time. NF1 shows complete penetrance, although the disease presents with a high degree of phenotypic variability even within families and within monozygotic twins carrying the same mutation (Rieley et al. 2011). Patients present with multiple café-au-lait macules (CALM), skinfold freckles, iris Lisch nodules, and neurofibromas. Neurofibromas can be subdivided into dermal neurofibromas, benign tumors that increase in number and size with age but do not undergo malignant transformation, and congenital plexiform neurofibromas, tumors involving multiple fascicles which in ~5 % of cases may progress to malignant peripheral nerve sheath tumors (MPNSTs) (Korf 1999). Optic pathway gliomas and specific skeletal abnormalities of the sphenoid wing, long bones, and vertebrae are also typical clinical signs associated with NF1. In addition, macrocephaly, short stature, learning disabilities, and attention difficulties are frequently observed in NF1 patients. NF1 patients also have an increased risk of developing specific malignancies (reviewed by Brems et al. 2009).
NF1 is due to mutations in the 282-kb-long NF1 gene located on 17q11.2, comprising 57 constitutive and at least three alternatively spliced exons. The 8,454 nucleotides of the open reading frame of the NF1 transcript encode neurofibromin, which negatively regulates Ras-GTPases (Ballester et al. 1990; Xu et al. 1990). NF1 functions as a tumor suppressor, and NF1-associated neoplasias, such as neurofibromas, gastrointestinal stromal tumors, glomus tumors, juvenile myelomonocytic leukemia, astrocytomas, and pheochromocytomas, have been shown to carry 2 mutant NF1 copies (reviewed by Brems et al. 2009). NF1 inactivation of both alleles has been documented in dermal as well as in plexiform neurofibromas, but additional genetic changes, including complex karyotypes, have only been identified in MPNSTs.
In addition, somatic “second hit” NF1 mutations have also been identified in tissues from tibial pseudarthrosis (Stevenson et al. 2006) and CALMs (De Schepper et al. 2008; Maertens et al. 2007).
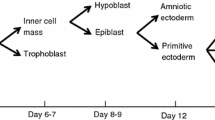
Biallelic NF1 inactivation follows the Knudson “two-hit hypothesis”. According to this model of tumorigenesis, one mutant allele (the “first hit” mutation) is inherited from an affected parent (for familial cases) or from a mutant germ cell of an otherwise unaffected parent. Alternatively, the first hit mutation results from a de novo mutation in the fertilized egg or occurs in very early stages of the developing embryo. By contrast, the “second hit” mutation affecting the other (wild-type) allele is then specifically present only in those somatic cells which represent the tumor or CALM initiating cells.
12.2 Mosaicism
NF1 affects ~1/3,000 individuals irrespective of gender or ethnic background and as many as 30–50 % of these patients present as “sporadic” or “founder” patients, that is, have no affected parent from whom the disorder was inherited (Friedman 1999; Evans et al. 2010). It follows that the NF1 gene has a new mutation rate of 3.7–26 × 10−5, that is, 10–100-fold higher to that which is observed in most other known human disease-associated genes (reviewed by Poyhonen et al. 2000 and references therein). The cause of this unusually high mutation rate is still unknown, the large size and complexity of the gene being possibly only partially contributory. Zlotogora proposed in 1993 that a proportion of the sporadic or “founder” NF1 patients may have the disease as the consequence of a somatic mutation after fertilization and the first molecularly proven somatic mosaic NF1 patient was reported in 1996: a multi-exon deletion of at least 100 kb encompassing exons 4–39 was identified in a 31-year-old patient with seven CALMs, bilateral axillary freckling, and multiple small cutaneous neurofibromas (Colman et al. 1996).
Genetic mosaicism refers to a condition where two or more genetically distinct cell populations, derived from the same fertilized egg, coexist in the same individual. Mosaicism in genetic disorders with significant skin manifestations, such as neurofibromatosis type 1, will be more readily visible than in disorders mainly affecting, for example, internal organs. With respect to NF1, mosaicism as discussed here refers to the fact that (only) a subpopulation of the body cells in a patient carries a “first hit” NF1 mutation.
The following types of mosaicism for a “first hit” NF1 mutation may be encountered. Gonadal or germline mosaicism occurs when a fraction of the germ cells (sperm or ova) carry a mutation, which may then lead to more than one affected offspring from clinically normal parents. Pure gonadal mosaicism is likely to be extremely rare in NF1, as only two such families have been reported to date (Lázaro et al. 1994; Bottillo et al. 2010). Mutations occurring early during embryonic development, before gastrulation and the formation and separation of the primordial germ cells, may lead to gonosomal mosaicism where somatic as well as germ cells can be mosaic. If mutations arise after the primordial germ cells were formed and set apart, patients may present solely with somatic mosaicism, implying that they would not be at risk of transmitting the disorder to the next generation. Ruggieri and Huson (2001) proposed the terms mosaic-generalized NF1 and mosaic-localized NF1 (or segmental NF1), reflecting the anticipated timing of the mutational event. Patients with mosaic-generalized NF1 present with typical NF1-related symptoms such as pigmentary changes and neurofibromas, not restricted to a few body segments. It may be particularly daunting to predict, solely from clinical observation, whether a sporadic patient has constitutional NF1 (i.e., with an NF1 mutation in all body cells) versus mosaic-generalized NF1 and if in the latter patients, whether or not the gonads are involved. Patients with “mosaic-localized” or “segmental” NF1 present with NF-related symptoms confined to a limited body area. The affected area may present with pigmentary changes only, with neurofibromas only, or with both pigmentary changes and neurofibromas. Further, isolated plexiform neurofibromas also occur and recently the first patient to be described was proven to carry biallelic NF1 inactivation in this isolated lesion (Beert et al. 2012).
In segmental NF1, the causative mutational event is assumed to have occurred at a later developmental time, offering an explanation for the clinically observed phenotype restricted to a specific body segment. It is most likely to assume that the germ cells of patients with segmental NF1 do not harbour the (first hit) NF1 mutation. However, apart from the timing of the mutational event, the types of progenitor cells affected as well as the nature of the NF1 mutation (hypomorphic versus, e.g., a total NF1 gene deletion) and the age of the patient at clinical evaluation will all equally contribute to the observed widely variable phenotypic outcome in the patient at a given time point. Segmental NF1 is rare, with a frequency estimated to be at least 15 times less prevalent than NF1, between 0.0014 % and 0.002 % (Huson and Ruggieri 2000; Wolkenstein et al. 1995; Ingordo et al. 1995; Listernick et al. 2003). The first proof at the molecular level that segmental NF1 is indeed due to postzygotic NF1 mutations was provided through identification of an NF1 microdeletion in ~15–24 % of the fibroblasts cultured from the CALMs of the affected, but not in the fibroblasts from the unaffected region, from an 18-year-old male with pigmentary lesions scattered over the left upper quadrant of the body (Tinschert et al. 2000). Importantly, however, thereafter some patients have been reported who phenotypically presented as having “mosaic-localized” or “segmental” NF1 disease, yet were confirmed as being gonosomal mosaic by molecular analysis and as ascertained after birth of their affected offspring (Consoli et al. 2005; Callum et al. 2012).
In the clinical literature, a number of segmental NF1 patients have been described having offspring with segmental NF1 (Rubenstein et al. 1983; Huson and Ruggieri 2000; Oguzkan et al. 2004); such vertical transmission is very difficult to explain as a result of mosaicism for a mutation shared between parent and child. None of these reported cases had molecular analyses performed and hence the underlying cause remains obscure. In addition, apart from a number of clinical “mosaic-localized” or “segmental” NF1 cases which are very likely to carry NF1 mutations in the affected cells, though it was not molecularly investigated and hence the precise underlying cause remains unknown (e.g., Hager et al. 1997; Ruggieri and Huson 2001; Listernick et al. 2003; Morais et al. 2010), some patients have been reported in the literature as having “segmental” NF1 even though they presented with, in addition to pigmentary abnormalities, some features clearly not associated with NF1 (e.g., Castori et al. 2008; Pascual-Castroviejo et al. 2008). As these patients were not analyzed at the molecular level, and hence not proven to carry an NF1 mutation, it must be realized that their phenotype may well be due to a concurrent defect in more than one gene, including the NF1 gene, or even might be due altogether to a defect in one or more other genes, not even involving NF1. As the molecular tools to investigate the genetics associated with NF1 disease have become more widely available, clinical reports of “segmental NF1” cases should be accompanied by appropriate supportive data using state-of-the-art molecular genetic analyses to prove NF1 involvement, especially when patients present with features not associated with NF1.
Finally, revertant mosaicism refers to the situation where a mutant cellular phenotype is reversed back to normal in some somatic cells by, for example, true reverse point mutation, gene conversion, nondisjunction, or mitotic recombination. Revertant mosaicism has been demonstrated in many genetic conditions involving the skin, including epidermolysis bullosa, Bloom syndrome, and Fanconi anemia amongst others (reviewed by Lai-Cheong et al. 2011), yet has never been demonstrated so far in NF1. To date, only three cases have been specifically investigated for the presence/absence of revertant mosaicism: a woman with NF1 signs throughout the entire body with a few sharply delineated segments of the skin unaffected, suggestive of revertant mosaicism (Vandenbroucke et al. 2004), and two pairs of monozygotic twins discordant for neurofibromatosis type 1 (Kaplan et al. 2010; Vogt et al. 2011).
All cases with molecular data supporting mosaicism for a “first hit” NF1 mutation, reported as of May 2012, are summarized in Table 12.1. Highlights from these studies and case reports include the following:
-
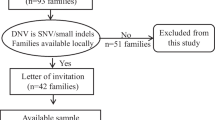
The frequency of mosaicism in sporadically affected NF1 patients is currently still largely unknown. A first estimate was obtained for patients carrying specifically a total gene deletion (TGD) interphase FISH analysis in 146 patients carrying a TGD showed mosaicism in blood in 9.6 % (14/146) (Messiaen et al. 2011). At least 10/14 carried a 1.2-Mb NF1 type 2 or atypical TGD deletion (see Chap. 14).
-
The typical 1.4-Mb type 1 TGD, previously uniquely found as a result of nonallelic homologous recombination during maternal meiosis between the paralogous recombination sites 1 and 2 (PRS 1 and 2), may also rarely result from recombination during mitotic post-zygotic cell divisions, as now proven in three patients carrying a mosaic TGD type 1 in blood (Messiaen et al. 2011).
-
Mosaicism in sporadic patients carrying a TGD type 2 is very high, estimated to occur at least in 70 % of founders (Messiaen et al. 2011). There seems to be a clear preponderance of females amongst mosaic founder patients with a TGD type 2 (Kehrer-Sawatzki et al. 2004; Steinmann et al. 2007).
-
Several studies found the percentage of hematopoietic cells carrying an NF1 mutation, especially when carrying a TGD type 2, to be higher as compared to urine and buccal epithelial cells or fibroblasts from affected as well as unaffected regions in patients with generalized-mosaic NF1 (Kehrer-Sawatzki et al. 2004, 2012; Vandenbroucke et al. 2004; Steinmann et al. 2007; Kehrer-Sawatzki and Cooper 2008; Roehl et al. 2012). Two mosaic patients were, however, found by FISH analysis in blood to carry the deletion in all cells, whereas a lower percentage was found in the buccal cells (Steinmann et al. 2007; Roehl et al. 2012). These tissue-specific differences suggest a selective growth advantage of hematopoietic stem cells carrying an NF1 deletion (Roehl et al. 2012).
-
Patients with mosaic type 2 TGD have milder disease manifestations, with a significantly lower external and internal plexiform neurofibroma burden, no facial dysmorphisms, and no delayed cognitive development compared to patients with a type 1 TGD (which typically is constitutional) (Kehrer-Sawatzki et al. 2012). This can probably be attributed to the presence of normal cells in the mosaic patients. However, since the risk of malignant transformation remains in any plexiform lesions present, special clinical management to allow early detection is still required.
-
The line separating generalized mosaic NF1 from segmental NF1 may not always be clear. In general, a mutation in blood is not detected in patients with clear segmental presentation. Gonosomal mosaicism has, however, been proven in an adult male with four pigmentary lesions on the midline of his back as the sole NF1-related manifestation (Callum et al. 2012). This intragenic multi-exon deletion, present in <20 % of the blood cells and in ~20 % of the sperm, was detected because of the preferential amplification of the shorter transcript by reverse-transcriptase PCR as part of a comprehensive NF1 testing (Callum et al. 2012). Low-level mosaic mutations typically escape detection by Sanger sequencing and array comparative genome hybridization (aCGH) or multiplex ligation-dependent probe amplification (MLPA).
-
The aggregated data obtained from all patients with mosaic NF1 (“generalized” or “segmental”) clearly indicate that the percentage of cells carrying the NF1 “first hit” mutation often is too low to be reliably detected in blood (or even is absent) and hence may be missed (Tinschert et al. 2000; Consoli et al. 2005; Maertens et al. 2007; Callum et al. 2012).
-
A subpopulation of the Schwann cells within the neurofibromas carries the second NF1 hit, in accordance with the two-hit tumor-suppressor hypothesis (Serra et al. 2000; Maertens et al. 2006). In the CALMs of NF1 patients, melanocytes, but not keratinocytes or fibroblasts, carry a first and second hit in the NF1 gene (De Schepper et al. 2008). Maertens et al. (2007) demonstrated that accurate diagnosis of mosaic or segmental NF1 necessitates comprehensive mutation analysis specifically of those neural-crest derived cells that are relevant, that is, the Schwann cells in the neurofibromas and the melanocytes in the CALMs. In these specific cells, but not (or only at too low a level) in blood, fibroblasts, or keratinocytes, a common first NF1 hit can be found in the different lesions (neurofibromas or CALMs) of segmental NF1 patients. This may also explain why no mutations were found in the fibroblasts of the patient described by Schultz et al. (2002).
-
In total, 49 unrelated patients, mosaic for a “first hit” post-zygotic NF1 mutation in the gonads and/or somatic cells, were reported and only 6/49 carried a minor lesion mutation affecting 1 nucleotide, all resulting in a premature stop codon. This probably reflects the technical difficulties associated with the detection of mosaic point mutations.
-
In 43/49 of these cases, the mutation was either an intragenic multi-exon deletion or a large deletion. At least 17 of these deletions were type 2 TGD spanning 1.2-Mb.
-
Finally, one pair of discordant twins was reported by Kaplan et al. (2010), with a woman carrying an NF1 nonsense mutation in both the Epstein–Barr virus-transformed lymphoblastoid cells propagated from her B-lymphocytes and her buccal epithelial cells, but not in her skin fibroblasts, yet being asymptomatic as of the age of 57 years. In another pair of discordant twins (Vogt et al. 2011), the affected 3-year-old twin was shown to be mosaic in blood and buccal cells for a nonsense mutation p.Gln1370*, which was not found in the unaffected twin. This can be explained by a post-zygotic mutation occurring after the twinning event took place, that is, after day 3–4 of embryonic life.
12.3 Molecular Diagnosis of NF1
Molecular diagnosis of NF1 is challenging owing to the large size of the gene, the existence of multiple highly homologous non-processed pseudogenes, the lack of mutational hotspots, and the complex mutational spectrum including a significant fraction of unusual splice mutations such as deep-intronic splice mutations or mutations affecting exonic splice enhancers, mimicking nonsense, missense, or even silent mutations at the genomic level (Messiaen and Wimmer 2008). The highest sensitivity and specificity are obtained using a multistep approach including an RNA-based center assay (Messiaen et al. 2000; Wimmer et al. 2006; Valero et al. 2011).
Clinical applications of mutational analysis have increased in relevance since some clear genotype–phenotype correlations have unfolded, with large deletions resulting in a more severe clinical phenotype (Upadhyaya et al. 1998; Riva et al. 2000; Mautner et al. 2010) and with the 3-bp in-frame deletion of 1 amino acid in exon 17 resulting in a milder phenotype without cutaneous or superficial plexiform neurofibromas (Upadhyaya et al. 2007). Further, limited genetic heterogeneity has been found by identification of a novel disorder, Legius syndrome, caused by mutations in the SPRED1 gene (Brems et al. 2007). Patients with Legius syndrome have multiple CALMs with or without skinfold freckling and macrocephaly, but do not develop the typical NF1-associated tumors (Brems et al. 2012). In patients presenting solely with CALMs with/without freckling, a correct diagnosis of constitutional NF1 versus mosaic NF1 (for sporadic patients) versus Legius syndrome cannot be made exclusively based on the clinical manifestation.
In ∼95% of patients presenting with “classic NF1”, including CALMs, skinfold freckling and neurofibromas, the NF1 mutation is identified if a comprehensive approach including RNA-based sequencing is applied (Messiaen et al. 2009). However, the detection rate in the blood lymphocytes drops in sporadic patients, even if they present with CALMs, skinfold freckling and neurofibromas probably because some of them present with mosaicism for an NF1 mutation undetectable/absent in the blood.
The majority of generalized mosaic patients reported to date present with a type 2 or atypical TGD, apparently detectable in a higher percentage of blood lymphocytes compared to urine-derived or buccal epithelial cells (Kehrer-Sawatzki et al. 2004, 2012; Vandenbroucke et al. 2004; Steinmann et al. 2007; Kehrer-Sawatzki and Cooper 2008; Roehl et al. 2012). Hence, blood represents a good sample from which to start analyses. In order to ascertain mosaicism, it seems to be sensible to pursue quantitative testing such as FISH in urine-derived epithelial cells in sporadic patients carrying a type 2 or atypical TGD identified in blood. Establishing a diagnosis of mosaic versus constitutional NF1 has important repercussions for counseling the patients and family with regard to recurrence risk.
Identification of the cell of origin in the CALMs and neurofibromas, that is, the melanocyte (De Schepper et al. 2008) and Schwann cell (Serra et al. 2000; Maertens et al. 2006), can now be applied to the precise identification of the common “first hit” NF1 mutation in the melanocytes or Schwann cells cultured from the affected regions of segmental patients (Maertens et al. 2007) or suspected mosaic patients in whom no mutation could be identified in the blood after comprehensive testing. Identification of such a common “first hit” establishes the unambiguous diagnosis of segmental or mosaic NF1. Moreover, it provides a marker that can be used for family planning, if desired, as the mutation may be at risk of being transmitted to the next generation and, if so, would result in constitutional NF1 (with all body cells carrying the inherited mutation). Refinement of the risk for transmission can be pursued in mosaic/segmental male patients, through analysis of the sperm, but cannot be provided in female patients, given the inaccessibility of the eggs for screening.
Future progress in diagnosis of founder patients is likely to come from novel technologies such as deep sequencing and may provide a means to detect low-level mosaicism in a reliable and sensitive way.
References
Ainsworth P, Chakraborty P, Weksberg R (1997) Example of somatic mosaicism in a series of de novo neurofibromatosis type 1 cases due to a maternally derived deletion. Hum Mutat 9:452–459.
Ballester R, Marchuk D, Boguski M, Saulino A, Letcher R, Wigler M, Collins F (1990) The NF1 locus encodes a protein functionally related to mammalian GAP and yeast IRA proteins. Cell 63:851–860
Beert E, Brems H, Renard M, Ferreiro J, Melotte C, Thoelen R, De Wever I, Sciot R, Legius E, Debiec-Rychter M (2012) Biallelic inactivation of NF1 in a sporadic plexiform neurofibroma. Genes Chromosomes Cancer 51:852–857
Bottillo I, Torrente I, Lanari V, Pinna V, Giustini S, Divona L, De Luca A, Dallapiccola B (2010) Germline mosaicism in neurofibromatosis type 1 due to a paternally derived multi-exon deletion. Am J Med Genet A 152A:1467–1540.
Brems H, Chmara M, Sahbatou M, Denayer E, Taniguchi K, Kato R, Somers R, Messiaen L, De Schepper S, Fryns J-P, Cools J, Marynen P, Thomas G, Yoshimura A, Legius E (2007) Germline loss-of-function mutations in SPRED1 cause a neurofibromatosis 1-like phenotype. Nat Genet 39:1120–1126.
Brems H, Beert E, de Ravel T, Legius E (2009) Mechanisms in the pathogenesis of malignant tumours in neurofibromatosis type 1. Lancet Oncol 10:508–523.
Brems H, Pasmant E, Van Minkelen R, Wimmer K, Upadhyaya M, Legius E, Messiaen L (2012) Review and update of SPRED1 mutations causing Legius syndrome. Hum Mutat 33(11):1538–1546.
Callum P, Messiaen L, Bower P, Skovby F, Iger J, Timshel S, Sims C, Falk R (2012) Gonosomal mosaicism for an NF1 deletion in a sperm donor: evidence of the need for coordinated, long-term communication of health information among relevant parties. Hum Reprod 27:1223–1229.
Castori M, Majore S, Romanelli F, Didona B, Grammatico P, Zambruno G (2008) Association of segmental neurofibromatosis 1 and oculo-auriculo-vertebral spectrum in a 24-year-old female. Eur J Dermatol 18:22–27.
Colman S, Rasmussen S, Ho V, Abernathy C, Wallace M (1996) Somatic mosaicism in a patient with neurofibromatosis type 1. Am J Hum Genet 58:484–574
Consoli C, Moss C, Green S, Balderson D, Cooper DN, Upadhyaya M (2005) Gonosomal mosaicism for a nonsense mutation (R1947X) in the NF1 gene in segmental neurofibromatosis type 1. J Invest Dermatol 125:463–469.
De Schepper S, Maertens O, Callens T, Naeyaert J-M, Lambert J, Messiaen L (2008) Somatic mutation analysis in NF1 café au lait spots reveals two NF1 hits in the melanocytes. J Invest Dermatol 128:1050–1053.
Evans D, Howard E, Giblin C, Clancy T, Spencer H, Huson S, Lalloo F (2010) Birth incidence and prevalence of tumor-prone syndromes: estimates from a UK family genetic register service. Am J Med Genet A 152A:327–359.
Fernández-Rodríguez J, Castellsagué J, Benito L, Benavente Y, Capellá G, Blanco I, Serra E, Lázaro C (2011) A mild neurofibromatosis type 1 phenotype produced by the combination of the benign nature of a leaky NF1-splice mutation and the presence of a complex mosaicism. Hum Mutat 32:705–714.
Fortino S, Andre M, Sudish M, Nicholas MB (2005) Thoracoscopically guided transaxillary resection of adjoining intercostal plexiform neurofibromas: review of mosaicism in neurofibromatosis: technical note. Neurosurgery 57 (4 Suppl):E407
Friedman J (1999) Vascular and endocrine abnormalities. In: Friedman JM, Gutmann DH, AmcCollin M, Riccardi VM (eds) Neurofibromatosis. Phenotype, natural history, and pathogenesis. Johns Hopkins University Press, Baltimore, MD, pp 274–296
Hager C, Cohen P, Tschen J (1997) Segmental neurofibromatosis: case reports and review. J Am Acad Dermatol 37:864–873
Havlovicova M, Novotna D, Kocarek E, Novotna K, Bendova S, Petrak B, Hrdlicka M, Sedlacek Z (2007) A girl with neurofibromatosis type 1, atypical autism and mosaic ring chromosome 17. Am J Med Genet A 143:76–157.
Huson SM, Ruggieri M (2000) The neurofibromatosis. In: Harper J, Oranje JM, Rose M (eds) Textbook of pediatric dermatology, vol 2. Blackwell, Oxford, pp 1204–1224
Huson S, Compston D, Harper P (1989) A genetic study of von Recklinghausen neurofibromatosis in south east Wales II. Guidelines for genetic counselling. J Med Genet 26:712–733
Ingordo V, D’Andria G, Mendicini S, Grecucci M, Baglivo A (1995) Segmental neurofibromatosis: is it uncommon or underdiagnosed? Arch Dermatol 131:959–1019
Kaplan L, Foster R, Shen Y, Parry D, McMaster M, O’Leary M, Gusella J (2010) Monozygotic twins discordant for neurofibromatosis 1. Am J Med Genet A 152A:601–607.
Kehrer-Sawatzki H, Cooper DN (2008) Mosaicism in sporadic neurofibromatosis type 1: variations on a theme common to other hereditary cancer syndromes? J Med Genet 45:622–653.
Kehrer-Sawatzki H, Kluwe L, Sandig C, Kohn M, Wimmer K, Krammer U, Peyrl A, Jenne D, Hansmann I, Mautner VF (2004) High frequency of mosaicism among patients with neurofibromatosis type 1 (NF1) with microdeletions caused by somatic recombination of the JJAZ1 gene. Am J Hum Genet 75:410–433.
Kehrer-Sawatzki H, Vogt J, Mußotter T, Kluwe L, Cooper DN, Mautner V-F (2012) Dissecting the clinical phenotype associated with mosaic type-2 NF1 microdeletions. Neurogenetics 13:229–236
Korf B (1999) Plexiform neurofibromas. Am J Med Genet 89:31–38
Lai-Cheong J, McGrath J, Uitto J (2011) Revertant mosaicism in skin: natural gene therapy. Trends Mol Med 17:140–148.
Lázaro C, Gaona A, Lynch M, Kruyer H, Ravella A, Estivill X (1995) Molecular characterization of the breakpoints of a 12-kb deletion in the NF1 gene in a family showing germ-line mosaicism. Am J Hum Genet 57:1044–1053
Lázaro C, Ravella A, Gaona A, Volpini V, Estivill X (1994) Neurofibromatosis type 1 due to germ-line mosaicism in a clinically normal father. New Engl J Med 331:1403–1410.
Listernick R, Mancini A, Charrow J (2003) Segmental neurofibromatosis in childhood. Am J Med Genet A 121A:132–137.
Maertens O, Brems H, Vandesompele J, De Raedt T, Heyns I, Rosenbaum T, De Schepper S, De Paepe A, Mortier G, Janssens S, Speleman F, Legius E, Messiaen L (2006) Comprehensive NF1 screening on cultured Schwann cells from neurofibromas. Hum Mutat 27:1030–1070.
Maertens O, De Schepper S, Vandesompele J, Brems H, Heyns I, Janssens S, Speleman F, Legius E, Messiaen L (2007) Molecular dissection of isolated disease features in mosaic neurofibromatosis type 1. Am J Hum Genet 81:243–294.
Mautner VF, Kluwe L, Friedrich RE, Roehl AC, Bammert S, Hogel J, Spori H, Cooper DN, Kehrer-Sawatzki H (2010) Clinical characterization of 29 neurofibromatosis type 1 patients with molecularly ascertained 1.4 Mb type-1 deletions. J Med Genet 47:623–630
Messiaen L, Callens T, Mortier G, Beysen D, Vandenbroucke I, Van Roy N, Speleman F, Paepe A (2000) Exhaustive mutation analysis of the NF1 gene allows identification of 95% of mutations and reveals a high frequency of unusual splicing defects. Hum Mutat 15:541–596.
Messiaen L, Wimmer K (2008) NF1 mutational spectrum. In: Kaufmann D (ed) Monographs in human genetics, vol 16. Karger, Basel, pp 63–77
Messiaen L, Yao S, Brems H, Callens T, Sathienkijkanchai A, Denayer E, Spencer E, Arn P, Babovic-Vuksanovic D, Bay C, Bobele G, Cohen B, Escobar L, Eunpu D, Grebe T, Greenstein R, Hachen R, Irons M, Kronn D, Lemire E, Leppig K, Lim C, McDonald M, Narayanan V, Pearn A, Pedersen R, Powell B, Shapiro L, Skidmore D, Tegay D, Thiese H, Zackai E, Vijzelaar R, Taniguchi K, Ayada T, Okamoto F, Yoshimura A, Parret A, Korf B, Legius E (2009) Clinical and mutational spectrum of neurofibromatosis type 1-like syndrome. JAMA 302:2111–2119.
Messiaen L, Vogt J, Bengesser K, Fu C, Mikhail F, Serra E, Garcia-Linares C, Cooper DN, Lazaro C, Kehrer-Sawatzki H (2011) Mosaic type-1 NF1 microdeletions as a cause of both generalized and segmental neurofibromatosis type-1 (NF1). Hum Mutat 32:213–222.
Morais P, Ferreira O, Bettencourt H, Azevedo F (2010) Segmental neurofibromatosis: a rare variant of a common genodermatosis. Acta Dermatovenerol Alp Panonica Adriat 19:27–36
Muram-Zborovski T, Vaughn C, Viskochil D, Hanson H, Mao R, Stevenson D (2010) NF1 exon 22 analysis of individuals with the clinical diagnosis of neurofibromatosis type 1. Am J Med Genet A 152A:1973–1981.
Oguzkan S, Cinbis M, Ayter S, Anlar B, Aysun S (2004) Familial segmental neurofibromatosis. J Child Neurol 19:392–396
Pascual-Castroviejo I, Pascual-Pascual SI, Viaño J (2008) Segmental neurofibromatosis type 1 (NF1) associated with Cobb syndrome: case report. Neuropediatrics 39:341–343
Petek E, Jenne D, Smolle J, Binder B, Lasinger W, Windpassinger C, Wagner K, Kroisel P, Kehrer-Sawatzki H (2003) Mitotic recombination mediated by the JJAZF1 (KIAA0160) gene causing somatic mosaicism and a new type of constitutional NF1 microdeletion in two children of a mosaic female with only few manifestations. J Med Genet 40:520–525
Poyhonen M, Kytölä S, Leisti J (2000) Epidemiology of neurofibromatosis type 1 (NF1) in northern Finland. J Med Genet 37:632–638
Rasmussen S, Colman S, Ho V, Abernathy C, Arn P, Weiss L, Schwartz C, Saul R, Wallace M (1998) Constitutional and mosaic large NF1 gene deletions in neurofibromatosis type 1. J Med Genet 35:468–539
Rieley M, Stevenson D, Viskochil D, Tinkle B, Martin L, Schorry E (2011) Variable expression of neurofibromatosis 1 in monozygotic twins. Am J Med Genet A 155A:478–563.
Riva P, Corrado L, Natacci F, Castorina P, Wu B, Schneider G, Clementi M, Tenconi R, Korf B, Larizza L (2000) NF1 microdeletion syndrome: refined FISH characterization of sporadic and familial deletions with locus-specific probes. Am J Hum Genet 66:100–109.
Roehl A, Mussotter T, Cooper DN, Kluwe L, Wimmer K, Högel J, Zetzmann M, Vogt J, Mautner V-F, Kehrer-Sawatzki H (2012) Tissue-specific differences in the proportion of mosaic large NF1 deletions are suggestive of a selective growth advantage of hematopoietic del(+/−) stem cells. Hum Mutat 33:541–591.
Rubenstein A, Bader J, Aron A, Wallace S (1983) Familial transmission of segmental neurofibromatosis. Neurology 33:76
Ruggieri M, Huson S (2001) The clinical and diagnostic implications of mosaicism in the neurofibromatoses. Neurology 56:1433–1476
Schultz E, Kaufmann D, Tinschert S, Schell H, von den Driesch P, Schuler G (2002) Segmental neurofibromatosis. Dermatology 204:296–303
Serra E, Rosenbaum T, Winner U, Aledo R, Ars E, Estivill X, Lenard H, Lázaro C (2000) Schwann cells harbor the somatic NF1 mutation in neurofibromas: evidence of two different Schwann cell subpopulations. Hum Mol Genet 9:3055–3119
Steinmann K, Cooper DN, Kluwe L, Chuzhanova N, Senger C, Serra E, Lazaro C, Gilaberte M, Wimmer K, Mautner V-F, Kehrer-Sawatzki H (2007) Type 2 NF1 deletions are highly unusual by virtue of the absence of nonallelic homologous recombination hotspots and an apparent preference for female mitotic recombination. Am J Hum Genet 81:1201–1221.
Steinmann K, Kluwe L, Cooper DN, Brems H, De Raedt T, Legius E, Mautner V-F, Kehrer-Sawatzki H (2008) Copy number variations in the NF1 gene region are infrequent and do not predispose to recurrent type-1 deletions. Eur J Hum Genet 16:572–652.
Stevenson D, Zhou H, Ashrafi S, Messiaen L, Carey J, D’Astous J, Santora S, Viskochil D (2006) Double inactivation of NF1 in tibial pseudarthrosis. Am J Hum Genet 79:143–151.
Streubel B, Latta E, Kehrer-Sawatzki H, Hoffmann G, Fonatsch C, Rehder H (1999) Somatic mosaicism of a greater than 1.7-Mb deletion of genomic DNA involving the entire NF1 gene as verified by FISH: further evidence for a contiguous gene syndrome in 17q11.2. Am J Med Genet 87:12–18
Tinschert S, Naumann I, Stegmann E, Buske A, Kaufmann D, Thiel G, Jenne D (2000) Segmental neurofibromatosis is caused by somatic mutation of the neurofibromatosis type 1 (NF1) gene. Eur J Hum Genet 8:455–464.
Tonsgard J, Yelavarthi K, Cushner S, Short M, Lindgren V (1997) Do NF1 gene deletions result in a characteristic phenotype? Am J Med Genet 73:80–86.
Upadhyaya M, Ruggieri M, Maynard J, Osborn M, Hartog C, Mudd S, Pentinnen M, Cordeiro I, Ponder M, Ponder BA, Krwaczak M, Cooper DN (1998) Gross deletions of the neurofibromatosis type 1 (NF1) gene are predominantly of maternal origin and commonly associated with a learning disability, dysmorphic features and developmental delay. Hum Genet 102:591–597
Upadhyaya M, Huson S, Davies M, Thomas N, Chuzhanova N, Giovannini S, Evans D, Howard E, Kerr B, Griffiths S, Consoli C, Side L, Adams D, Pierpont M, Hachen R, Barnicoat A, Li H, Wallace P, Van Biervliet J, Stevenson D, Viskochil D, Baralle D, Haan E, Riccardi V, Turnpenny P, Lazaro C, Messiaen L (2007) An absence of cutaneous neurofibromas associated with a 3-bp inframe deletion in exon 17 of the NF1 gene (c.2970-2972 delAAT): evidence of a clinically significant NF1 genotype-phenotype correlation. Am J Hum Genet 80:140–191.
Valero MC, Martin Y, Hernandez-Imaz E, Hernandez AM, Melean G, Valero AM, Rodriguez-Alvaraez FJ, Telleria D, Hernandez-Chico C (2011) A highly sensitive genetic protocol to detect NF1 mutations. J Mol Diagn 13:113–122
Vandenbroucke I, van Doorn R, Callens T, Cobben J, Starink T, Messiaen L (2004) Genetic and clinical mosaicism in a patient with neurofibromatosis type 1. Hum Genet 114:284–374.
Vogt J, Kohlhase J, Morlot S, Kluwe L, Mautner V-F, Cooper D, Kehrer-Sawatzki H (2011) Monozygotic twins discordant for neurofibromatosis type 1 due to a postzygotic NF1 gene mutation. Hum Mutat 32:47.
Wimmer K, Yao S, Claes K, Kehrer-Sawatzki H, Tinschert S, De Raedt T, Legius E, Callens T, Beiglböck H, Maertens O, Messiaen L (2006) Spectrum of single- and multiexon NF1 copy number changes in a cohort of 1,100 unselected NF1 patients. Genes Chromosomes Cancer 45:265–276.
Wolkenstein P, Mahmoudi A, Zeller J, Revuz J (1995) More on the frequency of segmental neurofibromatosis. Arch Dermatol 131:1465
Wu B, Boles R, Yaari H, Weremowicz S, Schneider G, Korf B (1997) Somatic mosaicism for deletion of the entire NF1 gene identified by FISH. Hum Genet 99:209–222
Xu G, Lin B, Tanaka K, Dunn D, Wood D, Gesteland R, White R, Weiss R, Tamanoi F (1990) The catalytic domain of the neurofibromatosis type 1 gene product stimulates ras GTPase and complements ira mutants of S. cerevisiae. Cell 63:835–876
Zlotogora J (1993) Mutations in von Recklinghausen neurofibromatosis: a hypothesis. Am J Med Genet 46:182–186.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Messiaen, L., Xie, J. (2012). NF1 Germline and Somatic Mosaicism. In: Upadhyaya, M., Cooper, D. (eds) Neurofibromatosis Type 1. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-32864-0_12
Download citation
DOI: https://doi.org/10.1007/978-3-642-32864-0_12
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-32863-3
Online ISBN: 978-3-642-32864-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)