Abstract
Purpose of Review
The use of thickened liquids has become one of the most common management strategies for individuals with dysphagia. The purpose of this paper is to review methods that can be used to measure the flow characteristics of liquids used in dysphagia management. We describe the measurement of apparent viscosity, measures of extensional flow, slump tests (specifically the line-spread test and Bostwick consistometry), gravity flow tests, and subjective methods.
Recent Findings
We discuss the relationship between different approaches to measuring flow, the 2002 American National Dysphagia Diet and the 2017 International Dysphagia Diet Standardisation Initiative (IDDSI) framework. A comparison of test results across four methods is provided.
Summary
A consistent approach is needed for the measurement of flow for thickened liquids used in dysphagia management. This review highlights differences that can be expected across different flow testing methodologies. Adherence to a common method and measurement definitions will promote patient safety and facilitate future research regarding the effectiveness of texture modification as an intervention for dysphagia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Texture modification is a widely used intervention for dysphagia [1•, 2]. Thickened liquids flow more slowly than thin liquids, and this provides extra time for a person with dysphagia to achieve airway protection during swallowing. In 2008, a landmark study by Logemann and colleagues showed that individuals with dementia or Parkinson’s disease who aspirated thin barium were less likely to aspirate thicker liquids [3•]. However, to date, the literature has not identified the degree of thickening that is required to achieve therapeutic benefit [4•].
Despite the widespread use of thickened liquids in dysphagia management, without clear definitions for different degrees of thickening, there is a high likelihood of variability in practice. A 2013 review of terminology and guidelines around the world clearly illustrated the potential for confusion across countries [1•]. In North America, liquids used in dysphagia management have been known by the labels thin, nectar-like, honey-like, and spoon- or pudding-thick since the publication of the National Dysphagia Diet (NDD) in 2002 [5]. Viscosity measurements for these categories were proposed at a shear rate of 50 reciprocal seconds (/s) as follows: thin: 1–50 cP; nectar-like: 51–350 cP; honey-like: 351–1750 cP; and spoon-thick: > 1750 cP. However, neither the equipment nor the skills necessary to perform accurate viscosity measurements at controlled shear rates are accessible to clinicians, caregivers, or patients with dysphagia. This means that individuals who are involved in purchasing or preparing thickened liquids for people with dysphagia rely on the information on product labels or on subjective measures, such as the stirring and manipulation of a liquid, observation of the liquid while being poured from a cup or analysis of the liquid by mouthfeel, or oral appraisal [6]. This dependency on subjective impressions leads to poor quality control of liquid consistency: Glassburn and Deem demonstrated that clinicians showed poor inter- and intra-individual reliability when using powdered thickeners to achieve targets of nectar- and honey-thick liquids based on subjective impression [7]. Similarly, Cichero and colleagues found significant differences in the viscosities of thickened meal-time and videofluoroscopy liquids labeled with identical names across ten different hospitals [8]. They cautioned that such variability creates the potential for patients to receive inappropriate thicknesses of liquid in their diets when transferred across facilities. In 2017, a new international framework for classifying liquids and foods used in dysphagia management was published with the goal of establishing common terminology and measurement guidelines to promote safety in the delivery of texture modified foods and thickened liquids to people with dysphagia [9•]. Implementation of this International Dysphagia Diet Standardisation Initiative (IDDSI) Framework is underway around the world.
In this manuscript, we will review methods that are available to measure the flow properties of liquids used in dysphagia. Both low- and high- technology approaches will be described. We will then illustrate comparative measures across four of these methods for a set of liquids.
Measures of Apparent Viscosity
Viscosity, in lay terms, is the appearance or perception of the “thickness” of a liquid. Technically, viscosity is the resistance of a substance to flow under an applied force. Rheometers are instruments that measure viscosity through the application of force to a liquid, which causes deformation or shearing of the liquid. The rate at which this deformation occurs is called shear rate. Viscosity remains constant across the shear rate continuum for some liquids (i.e., Newtonian liquids) but varies across different shear rates for other liquids (i.e., non-Newtonian); shear-thinning behavior, in which lower viscosities are seen at higher shear rates, is a common characteristic of liquids used in dysphagia management [10•]. For this reason, accurate measurements of viscosity require control of shear rate on the rheometer; but not all models of rheometer come with this option [11]. When viscosity is reported at specific shear rates, we use the term apparent viscosity.
During swallowing, a liquid bolus is first squeezed through the mouth by the tongue and then propelled into and through the pharynx [12]; the shear rates that apply during this process are likely to vary at different locations in the oropharynx. In particular, shear rates are likely to differ between the horizontally and vertically oriented planes of the oral cavity and the pharynx, as well as between zones within a fluid, depending on proximity to the walls of the oropharynx [13,14,15]. Although the NDD recommended the classification of liquids using ranges of viscosity specified at a single shear rate of 50/s, research by Shama and Sherman suggested that shear rate in the oropharynx ranges from 10/s to over 1000/s [16].
Although the measurement of apparent viscosity has been an established way of reporting flow in the field of dysphagia, this method has its limitations and should not be used as the only measure of liquid behavior [10•]. Other liquid properties fall outside the scope of rheological measurement, including fattiness, slipperiness, roughness, cohesiveness, elasticity, adhesiveness, and homogeneity (to name a few) [17]. Two recent studies illustrate that liquids with similar apparent viscosities, but prepared using different thickeners can have significantly different perceptual characteristics in the mouth [18, 19]. Stokes and colleagues suggest that further measures, including measures of extensional flow (see below), are required to fully reveal similarities and differences in liquid flow characteristics [17].
Tests of Extensional Flow
Extensional flow testing involves placing a liquid between two plates and slowly moving the plates apart, allowing the liquid to stretch, while maintaining constant volume. Upon stretching, a strand develops as the plates move in opposite directions. The area to volume ratio of the strand is much higher in extensional flow than it is in shear flow. During oral processing and pharyngeal swallowing, bolus deformation patterns include both shear and extensional flow [10, 20].
In a recent Swedish study [21], both shear-controlled and extensional viscosity testing were performed on liquids thickened with five commercial thickeners used for dysphagia management. Liquids thickened with xanthan gum had higher extensional viscosities (and were slightly more shear-thinning) than those thickened with starch [21]. This finding demonstrates the ability of extensional testing to detect additional properties of liquids that might not be measured by other available testing methods.
Slump Tests: Line-Spread Test and Bostwick Consistometer
Another method of liquid flow testing involves the observation of flow across a flat, level surface over time; these tests are called slump tests and include the line-spread test and Bostwick consistometry. Budke and colleagues [22] describe line-spread test methodology, as follows:
-
1)
A cylinder standing 3.5-cm high and 5.0 cm in diameter is placed on a flat, level clear surface, which is marked with concentric circles with ½-cm spacing;
-
2)
The test liquid is placed in the cylinder, which is then lifted, allowing the sample to flow;
-
3)
The average distance flowed across four equal quadrants of the circle template is measured at 60 s;
-
4)
High numbers represent greater spread (i.e., lower viscosity) while low numbers represent less spread (i.e., higher viscosity).
Variations across line-spread tests may include differences in cylinder height and capacity, in the spacing between the lines on the concentric circle grid, and in the number of points around the circle where measurements are taken. The line-spread test cannot be used to determine shear viscosity, but is useful for broad categorization of liquids into therapeutic groupings of similarly behaving liquids [23, 24]. Notably, this approach has been heavily used for classifying liquids for dysphagia management into different consistencies in Japan [25].
Bostwick consistometry is a second type of slump test. The Bostwick consistometer device allows a specified volume of liquid (i.e., 75 ml) to flow from a small holding chamber into a longer measurement chamber when a gate is released. The long chamber is marked with distance measurements in half centimeters, and distance flowed (at the leading edge) is measured at 30 s. Liquids that are higher in viscosity will have lower numbers on the Bostwick, while those that are lower in viscosity will flow further. Liquids with very low viscosity are likely to exhibit a floor effect while thin liquids will flow quickly to the end of the long chamber, demonstrating a ceiling effect. Such limitations are also seen with line-spread testing.
In the province of Québec (Canada), Bostwick flow distances are used to categorize thickened liquids for clinical purposes as follows: “clair”/thin: 16–24 cm; “nectar”: 13–15 cm; “miel”/honey: 7–9 cm; and “pudding”: 3–5 cm [26, 27]. While the Bostwick test provides results on a continuous scale, clinicians may experience difficulty when attempting to categorize liquids that fall in the gaps between these ranges.
Gravity Flow Tests: Posthumus Funnel, Zahn Cups, and IDDSI Flow Test
Similar to slump tests, gravity flow tests involve observation of liquid flow, but oriented in a vertical direction. A variety of testing methods fall under the gravity flow test category. Historically, the posthumus funnel was used to measure the viscosity of yogurt [28]; a predetermined amount of liquid was allowed to flow through the funnel and the time to exit the funnel was measured as an index of apparent viscosity. Studies have found similarities between funnel flow time and oral examination of viscosity [29]. The Zahn cup is a similar method of liquid flow testing, based on time [30]. The stainless-steel Zahn cup comes in various sizes and has a small hole in the bottom. Generally, large cup sizes are used for liquids with low flow and small cup sizes are used when the liquid is fast-flowing (low viscosity). To determine the flow of the liquid, the cup is dipped into the liquid, filled and pulled out of the body of liquid [31]. Once the Zahn cup has surfaced and the fluid is allowed to flow out of the bottom, the time until the stream of liquid breaks is measured. This “breaking” of the liquid stream is known as efflux time [32]. Some gravity flow testing methods also provide a measure of kinematic viscosity, in centistokes (cSt). Kinematic viscosity can be derived from efflux time using equations provided by Zahn cup manufacturers.
Other gravity flow tests are based on residual volume in the testing device after flow has occurred for a set amount of time; this is analogous to slump test methodology. IDDSI has selected this type of gravity flow test as their primary recommended method of liquid flow characterization. The IDDSI Flow Test involves the observation of liquid flow through a standard 10-ml slip-tip syringe [10]. Instructions can be found at www.iddsi.org. After 10 s of flow, the height of the residual column of liquid is used to categorize the liquid, as follows: Level 0, Thin: no liquid left in the syringe; Level 1, Slightly Thick: 1–4 ml of liquid left in the syringe; Level 2, Mildly Thick: 4–8 ml of liquid left in the syringe; Level 3, Moderately Thick: 8–10 ml of liquid left in the syringe; Level 4, Extremely Thick: 10 ml liquid left, no drips observed.
Drip Tests
As mentioned above, the IDDSI Flow Test reaches a point of saturation, such that extremely thick liquids do not display any flow through the syringe in the 10-s test period. At this point, the IDDSI testing guidelines recommend further testing using more subjective methods of observing the manner in which a bolus drops or drips from a utensil. Both forks and spoons are used in these tests.
Fork-drip tests aim to classify thick drinks and fluid foods based on whether they flow through the prongs of a fork. This type of testing is sensitive to differences in viscosity, both in a descriptive approach and with more objective measurements of time-to-first-drip of the liquid through the fork [33, 34]. Historically, the Australian guidelines for dysphagia diet classification included fork drip testing to describe distinct categories of liquid flow as follows: regular liquids will run through the prongs of a fork quickly, leaving no coating behind; mildly thick liquids still run fairly quickly through the prongs of a fork but leave a visible coating behind; moderately thick liquids coat the fork and drop slowly (in dollops) through the prongs; extremely thick liquids remain on the fork with no dripping and hold together well [35]. Similarly, the 2011 British guidelines incorporated fork testing to differentiate levels of thickness, based on whether or not an item could be eaten with a fork. Thin purees were described as not being possible to eat with a fork, because they drip (albeit slowly) through the prongs [36]. By contrast, thick purees can be eaten with a fork, because they do not drop through the prongs.
Spoon drop or tilt testing is used to measure the adhesiveness of a liquid, and the ability for the sample to remain cohesive. The behavior of the liquid is observed after being loaded onto a spoon and then tipping or tilting the spoon. IDDSI recommends use of the Spoon Tilt Test to distinguish between levels 4 and 5 in the framework. At Level 4 (extremely thick liquids), a sample should: be cohesive enough to hold its shape while on the spoon (but may spread or slump once on a plate); slide/drop-off of the spoon as a single bolus when tilted, or with a slight shake or flick; leave very little residue behind on the spoon. In particular, this test is useful for identifying items that are sticky and likely to be challenging for individuals with dysphagia to move efficiently through the mouth.
Illustration
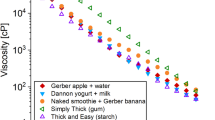
In order to illustrate the differences that may be seen across different methods of flow measurement, we will share results of shear-controlled rheometry, line-spread testing, Bostwick consistometry, and gravity flow testing using the IDDSI Flow Test for two arrays of liquids spanning the thin to extremely thick continuum. One array was prepared using a starch-based thickener (Nestlé® Resource® ThickenUp®) in concentrations of 0, 4.15, 4.77, 5.85, and 7.8 g/100 ml of flavored water (Nestlé® Lemon Splash); the second array was prepared using a xanthan gum-based thickener (Nestlé® Resource® ThickenUp® Clear) in concentrations of 0, 0.65, 1.25, 2.1, and 7.5 g/100 ml of the same flavored water. Table 1 provides comparison results for the four types of testing for both arrays. The values shown represent the mean test result obtained across three repeated tests at room temperature, 1 h after mixing. A few of the results are worth highlighting. First, it is obvious that much larger amounts of starch thickener were required (compared to xanthan gum-based thickener) to achieve target flow within each of the IDDSI liquid flow levels. Notice also that the apparent viscosities of the starch thickened liquids are substantially higher than those of the gum-thickened liquids, despite the fact that these liquids display similar gravity flow. Notably, a large jump can be seen in the amount of xanthan gum thickener required to achieve an extremely thick (Level 4) IDDSI flow test result, compared to Level 3. This reflects the fact that a small number of drips from the syringe may be seen as the IDDSI Flow Test reaches its saturation point. This fact also illustrates the fact that switching to fork drip and spoon tilt testing is appropriate and important to confirm the characteristics of extremely thick liquids. Furthermore, the results in Table 1 clearly illustrate both floor and ceiling effects for the line-spread and Bostwick methods. In fact, the slightly thick liquids reached saturation (i.e., 24 cm of flow) on the Bostwick test in approximately 7 s, well in advance of the 30-s time frame specified for reading flow results.
Figure 1 expands upon the data in Table 1 by plotting flow test, line-spread, and Bostwick test results, and clearly illustrates the inverse relationship that can be expected between the IDDSI Flow Test and slump test methods. The different degrees of test saturation can also be appreciated in a comparison of the three methods. For the slightly thick and mildly thick liquids, both the line-spread and Bostwick results display test saturation, whereas differences between these levels and between the starch and gum-thickened liquids within the mildly thick level can be seen using the IDDSI Flow Test. Conversely, the extremely thick liquids show saturation on the IDDSI Flow Test. Slight differences between the starch and gum-thickened stimuli can be appreciated in the Bostwick results, while the line-spread test was sensitive to differences between thickeners at all consistency levels. At this point, it remains unknown whether small differences either in slump test results or in gravity flow measures (i.e., those that fall within the boundaries of the IDDSI flow levels) have clinical significance, either with respect to eliciting differences in swallowing physiology or in the frequency of airway invasion.
Conclusion
The existence of multiple labelling conventions for thickened liquids, without an accessible and valid method of confirming flow properties is a patient safety risk [1•]. There are numerous examples in coronial literature of choking deaths due to the provision of inappropriate food textures to patients with dysphagia. For example, the Ontario Office of the Coroner has recently identified inconsistencies in diet texture labelling as a contributing factor in a death due to choking [37]. With respect to liquids, current evidence regarding the effectiveness of thickened liquids for reducing aspiration and preventing negative sequela is hampered by a lack of consistent use of clear terminology and measurement [3, 4]. One example of the confusion that can arise in this respect is seen in a randomized control trial which involved the observation of pneumonia and other outcomes in older adults with dementia or Parkinson’s disease over a 3-month time frame [38•]. Two levels of thickened liquid were studied, along with consumption of thin liquids using a chin-down technique. The thickened liquids were labeled “nectar” and “honey”; however, the apparent viscosity of the honey-thick liquids was twice as thick as the NDD guideline for honey-thick liquids. Participants in that study showed unexpected negative outcomes with this honey-thick consistency, including higher rates of pneumonia, dehydration, and death. It would, however, be incorrect to generalize these results to liquids with a viscosity within the NDD category of honey-thick because the “honey” thick liquid used in the study actually belonged to the “pudding” thick consistency class.
The standard definitions and measurement methods recommended by the IDDSI provide a path out of the confusion that has dominated the clinical use of thickened liquids. The low-technology testing methods developed by IDDSI are accessible not only to hospitals, food service providers, and clinicians, but importantly also to caregivers. As such, they empower end users to check the consistency of liquids for people with dysphagia at the point of service, and facilitate risk reduction through improved adherence to diet texture recommendations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Cichero JAY, Steele CM, Duivestein J, Clave P, Chen J, Kayashita J, et al. The need for international terminology and definitions for texture modified foods and thickened liquids used in dysphagia management: foundations of a global initiative. Curr Phys Med Rehabil Rep. 2013;1(4):280–91. https://doi.org/10.1007/s40141-013-0024-z. http://springerlink.bibliotecabuap.elogim.com/article/10.1007%2Fs40141-013-0024-z Paper describing variation in terminology around the world used to describe categories of food texture and liquid consistency for use in dysphagia management, illustrating the need for standard terms and measurement.
Garcia JM, Chambers E, Molander M. Thickened liquids: practice patterns of speech-language pathologists. Am J Speech Lang Pathol. 2005;14(1):4–13.
• Logemann JA, Gensler G, Robbins J, Lindblad AS, Brandt D, Hind JA, et al. A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson’s disease. J Speech Lang Hear Res. 2008;51(1):173–83. Largest known randomized trial of the effect of liquid consistency on aspiration rates in people with dysphagia (dementia or Parkinson’s Disease), compared directly within a videofluoroscopy exam. Efficacy of thickened liquids for eliminating aspiration in this population was determined.
• Steele CM, Alsanei WA, Ayanikalath S, Barbon CE, Chen J, Cichero JA, et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30(1):2–26. https://doi.org/10.1007/s00455-014-9578-x. http://bit.ly/1wvZydp Systematic review of > 10,000 references from the medical and engineering scientific literature regarding the influence of liquid consistency and food texture on swallowing function and physiology. Findings include evidence that thicker liquids do help to decrease aspiration. However, evidence was also found that residue begins to accumulate when liquids are too thick.
American Dietetic Association National Dysphagia Diet Task Force. National Dysphagia Diet: standardization for optimal care. Chicago: Faulhaber, D; 2002.
Steele CM, Van Lieshout PHHM, Goff D. The rheology of liquids: a comparison of clinicians? Subjective impressions and objective measurement. Dysphagia. 2003;18(3):182–95.
Glassburn DL, Deem JF. Thickener viscosity in dysphagia management: variability among speech-language pathologists. Dysphagia. 1998;13(4):218–22.
Cichero JA, Jackson O, Halley PJ, Murdoch BE. How thick is thick? Multicenter study of the rheological and material property characteristics of mealtime fluids and videofluoroscopy fluids. Dysphagia. 2000;15(4):188–200.
• Cichero JAY, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017;32(2):293–314. https://doi.org/10.1007/s00455-016-9758-y. http://springerlink.bibliotecabuap.elogim.com/article/10.1007/s00455-016-9758-y. Paper describing the process followed by the International Dysphagia Diet Standardisation Initiative to develop a new framework of terminology, definitions and measurement techniques to classify texture modified foods and thickened liquids used in dysphagia management.
• Hanson B. A review of diet standardization and bolus rheology in the management of dysphagia. Curr Opin Otolaryngol Head Neck Surg. 2016;24(3):183–90. Review paper regarding rheology and measurement of fluid characteristics relevant to dysphagia.
Cichero JAY, Jackson O, Halley PJ, Murdoch BE. How thick is thick? Multicenter study of the rheological and material property characteristics of mealtime fluids and videofluoroscopy fluids. Dysphagia. 2000;15(4):188–200.
Hiiemae KM, Palmer JB. Food transport and bolus formation during complete feeding sequences on foods of different initial consistency. Dysphagia. 1999;14(1):31–42.
Burbidge AS, Cichero JAY, Engmann J, Steele CM. “A day in the life of the fluid bolus”: an introduction to fluid mechanics of the oropharyngeal phase of swallowing with particular focus on dysphagia. Appl Rheol. 2016;26:1–10.
Nicosia MA. Theoretical estimation of shear rate during the oral phase of swallowing: effect of partial slip. J Texture Stud. 2013;44(2):132–9.
Nicosia MA, Robbins JA. The fluid mechanics of bolus ejection from the oral cavity. J Biomech. 2001;34(12):1537–44. Epub 2001/11/22
Shama F, Sherman P. Identification of stimuli controlling the sensory evaluation of viscosity II. J Texture Stud. 1973;4(1):111–8.
Stokes JR, Boehm MW, Baier SK. Oral processing, texture and mouthfeel: from rheology to tribology and beyond. Curr Opin Colloid Interface Sci. 2013;18(4):349–59.
Vickers Z, Damodhar H, Grummer C, Mendenhall H, Banaszynski K, Hartel R, et al. Relationships among rheological, sensory texture, and swallowing pressure measurements of hydrocolloid-thickened fluids. Dysphagia. 2015;30(6):702–13.
Ong J, Steele CM, Duizer LM. Sensory characteristics of liquids thickened with commercial thickeners to levels specified in the International Dysphagia Diet Standardisation Initiative (IDDSI) framework. Food Hydrocoll. 2018;79:208–17.
Nyström M, Stading M, Qazi W, Bulow M, Ekberg O. Effects of rheological factors on perceived ease of swallowing. Appl Rheol. 2015;25:63876.
Waqas MQ, Wiklund J, Altskär A, Ekberg O, Stading M. Shear and extensional rheology of commercial thickeners used for dysphagia management. J Texture Stud. 2017;48(6):507–17.
Budke J, Garcia JM, Chambers EIV. Comparisons of thickened beverages using line spread measurements. J Acad Nutr Diet. 2008;108(9):1532–5.
Lund AM, Garcia JM, Chambers IVE. Line spread as a visual clinical tool for thickened liquids. Am J Speech Lang Pathol. 2013;22(3):566–71.
Nicosia MA, Robbins J. The usefulness of the line spread test as a measure of liquid consistency. Dysphagia. 2007;22(4):306–11. Epub 2007/06/22
Watanabe E, Yamagata Y, Fujitani J, Fujishima I, Takahashi K, Uyama R, et al. The criteria of thickened liquid for dysphagia management in Japan. Dysphagia. 2018;33(1):26–32.
Association professionelle des nutritionnistes experts en dysphagie. Énoncé de position. https://opdq.org/wp-content/uploads/2013/07/APNED_EnonceDePosition_IDDSI_Francais.pdf Accessed April 18, 2018.
Allain A-FL, M. Desrosiers, T. Évaluation de la dysphagie: Après l'ajout de sulfate de baryum aux ailments, peut-on faire les recommandations appropriées quant aux textures et consistances pour les personnes dysphagiques? : Ordre professionel des diététistes du Québec; 2010. p. 19-20. https://www.opdq.org/wp-content/uploads/2013/08/NSE_Vol8no1_printemps_2010.pdf. Accessed April 18, 2018.
van Vliet T. On the relation between texture perception and fundamental mechanical parameters for liquids and time dependent solids. Food Qual Prefer. 2002;13(4):227–36.
Skriver A, Holstborg J, Qvist KB. Relation between sensory texture analysis and rheological properties of stirred yogurt. J Dairy Res. 1999;66(4):609–18.
Garcia JM, Chambers EIV, Molander M. Thickened liquids: practice patterns of speech-language pathologists. Am J Speech Lang Pathol. 2005;14(1):4–13.
Abbas KA, Abdulkarim SM, Saleh AM, Ebrahimian M. Suitability of viscosity measurement methods for liquid food variety and applicability in food industry - a review. J Food Agric Environ. 2010;8(3&4):100–7.
Kim CH, Lipták BG. Viscometer-laboratory. In Lipták BG, editor. Instrument Engineers’ Handbook, 4th edition, Vol. 1: Process Measurement and Analysis. CRC Press; 2003. pp 1708–22.
Park JW, Kim IJ, Lee HJ. Fork test: a new simple and reliable consistency measurement for the dysphagia diet. Geriatr Nurs. 2016;37(4):292–5.
Tsang C, Hori SE, Peladeau-Pigeon M, Steele CM. The fork-test: a simple table-top test of viscosity? Dysphagia. 2012;27(4):572. https://doi.org/10.1007/s00455-012-9428-7.
Dieticians Association of Australia and The Speech Pathology Association of Australia Limited. Texture-modified foods and thickened fluids as used for individuals with dysphagia: Australian standardised labels and definitions. 2007; 64: 553–576.
National Patient Safety Agency, Royal College Speech and Language Therapists, British Dietetic Association, National Nurses Nutrition Group, Hospital Caterers Association. Dysphagia diet food texture descriptions. 2011. http://www.thenacc.co.uk/assets/downloads/170/Food%20Descriptors%20for%20Industry%20Final%20-%20USE.pdf. Accessed on: April 18, 2018.
Office of the Chief Coroner, Province of Ontario. Geriatric and Long Term Care Review Committee 2016 Annual Report. http://www.mcscs.jus.gov.on.ca/sites/default/files/content/mcscs/docs/GLTRC%202016%20English.pdf. Accessed on: April 18, 2018.
• Robbins J, Gensler G, Hind J, et al. Comparison of 2 interventions for liquid aspiration on pneumonia incidence: a randomized trial. Ann Intern Med. 2008;148(7):509–18. Follow up to Logemann’s randomized trial of the effect of liquid consistency on in people with dysphagia, looking at 3 month health status outcomes including pneumonia. Extremely thick liquids resulted in poorer outcomes for adults with dementia or Parkinson’s disease who were confirmed to aspirate on thin liquids; these outcomes included a higher incidence of pneumonia as well as higher rates of dehydration and mortality.
Acknowledgments
The authors would like to thank Steve Pong for his assistance with line-spread testing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Carly E. A. Barbon declares no conflicts of interest.Catriona M. Steele serves as a board member for the International Dysphagia Diet Standardisation Initiative and has received speaker fees/travel expense support from International Dysphagia Diet Standardisation Initiative.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Swallowing Disorders
Rights and permissions
About this article
Cite this article
Barbon, C.E.A., Steele, C.M. Thickened Liquids for Dysphagia Management: a Current Review of the Measurement of Liquid Flow. Curr Phys Med Rehabil Rep 6, 220–226 (2018). https://doi.org/10.1007/s40141-018-0197-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-018-0197-6