Abstract
Purpose of Review
This review of central nervous system (CNS) immune-mediated disorders serves as an overview of multiple neuroinflammatory conditions. Organized by CNS site, it gives the reader up to date information on clinical presentation, diagnostic pitfalls, and treatment considerations for the acute phase of these disorders. Special attention is paid to some of the more rare CNS neuroinflammatory disorders, given the treatment and rehabilitation challenges that they present.
Recent Findings
In-depth discussion about conditions that can mimic idiopathic transverse myelitis is emphasized during this review. Also, opsoclonus-myoclonus syndrome is included as a discussion point in this review with the most recent literature cited. A general overview of the most current approaches and considerations for multiple sclerosis, neuromyelitis optica, and autoimmune encephalitis is discussed.
Summary
This review serves as a brief overview of neuroinflammatory conditions most relevant to neurologists and rehabilitation providers who see and manage these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immune-mediated central nervous system (CNS) disorders are a diverse group of overall rare but potentially devastating disorders. They occur in both children and adults, although etiologic concerns will vary depending on age. The most common of immune-mediated CNS diseases is multiple sclerosis (MS), a chronic autoimmune disease in which myelin is the target of a dysfunctional immune system, and injury can occur anywhere within the CNS. However, MS is only one of several immune-mediated disorders that can occur in children and adolescents, and, although other conditions are much more uncommon, each carries a unique set of potential treatment and rehabilitation challenges and options.
Spinal Cord
Immune-mediated disorders that affect the spinal cord are infrequent, but these disorders can be physically devastating to patients, and differences in management can have significant impacts. Recognition of such disorders remains a challenge, and there is wide variability in treatment regimens, depending on the condition.
Idiopathic Transverse Myelitis
Clinical Presentation
Idiopathic transverse myelitis (ITM) occurs in 1 in every 250,000–500,000 patients, although estimates of incidence vary. It can occur at all ages, affecting infants through adults. Generally speaking, younger patients with ITM are more likely to have a monophasic disease and, with older patients, there is likely a higher risk for ITM to be a manifestation of an underlying chronic autoimmune condition [1,2,3,4,5, 6•, 7•, 8•].
Symptoms in ITM reflect the area of spinal cord involvement; however, even with patients with apparent similarly affected cords, there can be a wide variability in symptoms. Patients will present with symptoms of upper or lower extremity sensory changes, weakness, and/or bladder or bowel changes [1,2,3,4].Occasionally, patients will have isolated symptoms that last for hours or days before other deficits evolve, such as urinary retention or even priapism [9, 10]. The symptoms can evolve from their onset to the nadir from hours to weeks, although very rapid evolution of symptoms, such as minutes to a few hours, should provoke a concern for a vascular etiology [1,2,3,4]. Conversely, slowly progressive symptoms that last more than weeks or months generally reduce concern for ITM. Careful history taking is crucial to determining etiology and planning for diagnostic imaging and treatment, although this can be difficult with younger and nonverbal patients.
Diagnosis and Etiology
ITM is a diagnosis of exclusion and is dependent on clinical features and history, examination findings, imaging, and cerebrospinal fluid findings. There is no one imaging, clinical, or laboratory feature considered pathognomonic for ITM [1,2,3,4]. The most formally accepted criteria are from the Transverse Myelitis Working Group from 2002 by Kerr and colleagues [11]. Magnetic resonance imaging (MRI) of the spinal cord is considered crucial for diagnosis, and, unless absolutely contraindicated, patients with suspected ITM should undergo a lumbar puncture. Causes of infection should be explored; however, multiple infections have been reported with ITM, but it is unclear, especially with viral causes, whether or not cord injury and inflammation is from direct viral or bacterial injury or is a secondary autoimmune response to an infectious trigger and/or a combination thereof [1,2,3,4, 12].However, recognition of a possible infectious cause may open up therapeutic options such as with Bartonella henselae or herpes simplex virus [13,14,15,16].
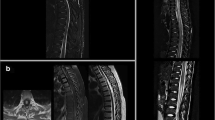
With respect to MRI findings, lesions within the spinal cord can be single or multifocal and can involve both the gray and white matter regions of the cord. Although ITM has been historically grouped with MS as a monophasic demyelinating disorder, it is being increasingly recognized that, like with MS, gray matter of the cord can be involved and greater cord gray matter involvement likely imparts a more concerning prognosis [17•]. In addition, lesions within the spinal cord are typically hyperintense on T2 imaging and can have variable degrees of gadalinium contrast enhancement; however, absence of gadalinium enhancement does not preclude a diagnosis of ITM [1,2,3,4,5, 6•, 7•, 8•, 10,11,12].
Spinal fluid findings are heterogenous across ITM cases. “Classic” ITM will have some or several markers in the spinal fluid consistent with inflammation, such as an elevation in the white blood cells in the CSF, an elevated IgG index and/or synthesis rate, and/or the presence of four or more oligoclonal bands. However, CSF protein can also be elevated and the spinal fluid can sometimes be benign-appearing [1,2,3,4,5, 6•, 7•, 8•, 10,11,12].There are some older small case series of CSF cytokines in ITM cases showing IL-1 and IL-6 elevations; however, these results have not been reproduced across larger series of ITM cases and they are not routinely used for diagnosis or management [18•, 19, 20].
A diagnosis of ITM implies that no clear etiologic factor has been found, meaning there is not thought to be an underlying diagnosis of MS or another inflammatory condition that is the explanatory factor for the myelitis presentation. In the setting where it is unclear whether or not there is an underlying cause, such as MS or another inflammatory condition, the term transverse myelitis really only describes the clinical syndrome whereas idiopathic transverse myelitis is reserved for cases where no cause is found and the disease is thought to be monophasic [1,2,3,4,5, 6•, 7•, 8•, 10,11,12].
Transverse Myelitis vs Acute Myelopathies from Other Causes
With ITM being a diagnosis of exclusion, it should be noted that there are other conditions that can mimic ITM but are not inflammatory in origin. A vascular myelopathy is one of the more common mimickers, and diagnosis can be challenging. In one large series of patients undergoing angiography, misdiagnosis of vascular myelopathies as ITM was approximately 30%. Arterial myelopathies typically present with an extremely rapid onset of symptoms, but myelopathies that are venous in origin or due to a vascular malformation can have presentations indistinguishable from an inflammatory myelitis. In addition, there is also data to suggest that myelopathies that are vascular in origin may include markers typically thought to be exclusive to inflammatory myelopathies, such as pleocytosis and gadalinium contrast enhancement. Unfortunately, magnetic resonance angiography (MRA) is insensitive for identifying vascular abnormalities, and the gold standard for diagnosis of a vascular myelopathy depends on catheter angiography [21•, 22•]
Another mimicker is a fibrocartilaginous embolus, a condition in which there is herniation of intervertebral disk material into the vasculature surrounding the cord and subsequent secondary cord injury. This condition can be provoked by seemingly minor trauma or benign movements, and patients will often report feeling a “pop” sensation or unusual sensation prior to a rapid onset of symptoms. Symptoms typically progress rapidly over minutes to several hours, and imaging and laboratory and clinical features can also be indistinguishable from an ITM. There are some imaging findings thought to suggest the diagnosis, but they are not ubiquitous across all cases [23•, 24•].
In the past few years, there has been a surge in cases being now referred to as acute flaccid myelitis (AFM). The initial data implicated an enterovirus as the culprit, and it was also noted that typical immunotherapy regimens, such as intravenous high-dose steroids, intravenous immunoglobulin (IVIg), or plasma exchange/plasmapheresis (PLEX) were not particularly efficacious. However, later cases have not definitively confirmed this link, and the investigations for these cases are ongoing. Patients with AFM can present with a fairly rapid onset and tend to have more gray matter spinal cord involvement, specifically anterior horn involvement, and affected limbs will exhibit persistent flaccid paralysis and often atrophy in muscle groups in affected limbs over time, consistent with a phenotype that mirrors poliomyelitis [25•, 26•, 27•]. Of note, although there has been focus on AFM in the past few years, previous papers have noted that patients with ITM with nerve conduction study/electromyography changes and/or persistent flaccid paralysis tended to have a poorer prognosis [28, 29]. This author feels that at least some of these aforementioned cases likely had a phenotype not dissimilar from AFM cases today. Although considered distinct by some researchers from a more classic ITM, it is likely that AFM represents a subtype of ITM cases.
Another potential important confounding condition with ITM is a pre-syrinx with Arnold-Chiari malformations [30]. There is some concern in the ITM community that the presence of an Arnold-Chiari malformation may be a risk factor for ITM, and there are a few cases of a Chiari malformation presenting in such a way as to suggest the diagnosis of ITM [31•].Unfortunately, there are no clear guidelines as to how to best manage a potentially symptomatic Chiari malformation in the setting of an acute presentation, but, if a patient has profound weakness, then surgical correction can be considered.
The importance of these mimickers is due to the fact that the above conditions may have a poor response to traditional treatments used for ITM. This author recommends consideration of any of the above with a history atypical for ITM, persistent flaccid paralysis, a rapid onset and clinical deterioration, and/or in the absence of factors supportive of an inflammatory cause such as the absence of gadalinium contrast enhancement and the absence of CSF findings consistent with inflammation.
Treatment for ITM
Typical treatment for the acute phase of ITM are 3–7 days of high-dose intravenous (IV) steroids, typically methylprednisolone, 1000 mg IV every 24 h for patients >35 kg or 30 mg/kg/day IV for patients <35 kg. In patients that do not respond to steroids, either IVIg (0.4 g/kg IV daily for 3–5 days) or PLEX, with a minimum of five exchanges and possibly up to ten exchanges, could be considered [1,2,3,4,5, 6•, 7•, 8•, 10,11,12].Other more aggressive therapies that have been considered in more refractory cases of ITM have been cyclophosphamide, dosed at 750–1000 mg/m2, or high-dose IV methotrexate, dosed at 2500 mg/m2 with leucovorin rescue [32–33, 34•]. Rituximab, dosed at 375 mg/m2 for 4 doses over 4 weeks or 2 doses over 4 weeks, or 1000 mg IV dosed once or 2 doses over 4 weeks, has been used for ITM cases in select circumstances, although it is typically employed more so when an underlying chronic inflammatory disorder such as NMO-SD is suspected [35, 36]. The latter three therapies should be initiated with neurologists familiar with these medications and/or rheumatologists or oncologists. In addition, cyclophosphamide, methotrexate, or rituximab generally take a few days to weeks before reaching peak effect.
With respect to timing of escalation of immunotherapy in ITM cases, the duration of the inflammatory phase in ITM is likely variable across different patients but likely only lasts a few weeks to 2–3 months [1,2,3,4,5, 6•, 7•, 8•, 10,11,12].Due to the fact that all the therapies act on the inflammatory phase of the disease process, patients that have a suboptimal response to initial therapies should be escalated to the next therapy sooner rather than later. In this author’s experience, therapies that show little benefit in the first few days or within 1–2 days following completion should be considered non-responders to that treatment. In addition, patients that have responded poorly or have worsened following treatment should be considered for further investigation, such as vascular imaging of the spine, with concern that misdiagnosis is the reason for the inadequate response [21•, 22•, 23•, 24•]. Furthermore, escalation of immunotherapy should be based on the clinical status of the patient in the acute phase of the disease rather than radiologic or laboratory findings.
Following completion of immunotherapy, rehabilitation is dependent on the patient’s deficit. However, activity-based rehabilitation therapy is generally considered the gold standard to aid recovery, although data is gleaned from studies of traumatic spinal cord injuries [37•, 38]. In addition, recovery from ITM can occur over several months or even years. In patients with concomitant peripheral nerve injury with their ITM, nerve transfer can be considered that might provide functional benefit with select activities or muscle groups [39, 40].
Neuromyelitis Optica-Spectrum Disorders and Multiple Sclerosis
Both neuromyelitis optica-spectrum disorders (NMO) and multiple sclerosis (MS) are relapsing neuroinflammatory diseases. NMO can cause an inflammatory myelitis, typically involving long segments of the spinal cord (three or more vertebral segments) and optic neuritis, but brain lesions causing a hemispheric syndrome and brainstem syndromes have been described leading to revision of the diagnostic criteria for NMO. About 80% of cases will be anti-aquaporin4 antibody positive, but the absence of antibody positivity does not exclude the diagnosis. Flare-ups, exacerbations, or attacks (all those terms used relatively interchangeably) are typically treated with high-dose steroids or PLEX. Acute exacerbations refractory to those treatments have been treated with IVIg, cyclophosphamide, and high-dose IV methotrexate. Maintenance immunotherapy used to reduce the risk for further attacks includes azathioprine, mycophenolate mofetil, oral weekly methotrexate, or IV rituximab. Refractory NMO cases that have failed one or more of these treatments have been treated with IV tocilizumab with some success. None of these above treatments are FDA-approved for NMO. Although NMO is much less prevalent than MS, consideration of this diagnosis is important in atypical MS cases as certain MS disease-modifying therapies (DMT) such as the interferons, and possibly, natalizumab, have been associated with clinical worsening of certain NMO cases [41•, 42, 43•].
MS is the most common neuroinflammatory disease, with estimates of prevalence affecting approximately 1 in 1000 adults, with 90% of cases occurring in ages greater than 18 years of age. Presenting symptoms vary widely, but an inflammatory sensory myelitis, especially when involving the dorsal columns, or an optic neuritis should provoke concern for MS. Cord lesions are typically short segment lesions and involve mostly the white matter of the cord or are mixed gray-white matter. Attacks, flares, or exacerbations of MS typically will exhibit gadalinium-enhancing lesions and are treated with high-dose IV steroids or PLEX in steroid-refractory cases. Most cases of MS in younger patients are relapsing, remitting MS (RRMS), and there are now 12 FDA-approved DMTs for MS. There are two subtypes of progressive MS, where the clinical course is one of slow, gradual clinical deterioration rather than discrete neurologic attacks. These are secondary progressive MS, a later phase of RRMS, and primary progressive MS. Recently, ocrelizumab has become the first FDA-approved DMT for progressive MS [44, 45].
For MS and NMO, rehabilitation is crucial in order to facilitate recovery from attacks and to reduce the likelihood of long-term disability. Beyond physical therapy and occupational therapy to aid recovery following an acute neurologic attack, there are multiple long-term rehabilitation needs often needed by NMO and MS patients. Spasticity, pain, and bladder and bowel dysfunction management can have a significant impact on quality of life and day-to-day functioning [46].
Systemic Inflammatory Disorders
Sarcoidosis, an inflammatory syndrome that primarily affects the lungs, involves the CNS in about 10% of patients. Neurosarcoidosis can present with a longitudinally extensive inflammatory myelitis but it can also involve other CNS regions. It is unusual for sarcoidosis to present with neurologic manifestations first, but it does happen infrequently. In patients that present with a long segment myelitis, neurosarcoidosis should be considered. Typical screening tests include an angiotensin-converting enzyme level, although somewhat insensitive as a screening test, and either chest radiograph or a CT chest to look for mediastinal lymphadenopathy, present in about 80–90% of cases [47•, 48•, 49].
Systemic lupus erythematosus and Sjogren’s disease can also involve the CNS. Both conditions can rarely cause a myelitis or an optic neuritis [50,51,52,53]. In addition, systemic lupus erythematosus (SLE) patients can have neuropsychiatric SLE with various psychiatric and neurologic manifestations. These patients typically require more aggressive immunotherapy treatment than SLE patients without neurologic involvement [54].
Brainstem and Cerebellum
Opsoclonus-Myoclonus/Ataxia Syndrome
Opsoclonus-myoclonus/ataxia syndrome (OMS) is a poorly understood neuroinflammatory syndrome. It is rare, with an incidence of about 1 in 500,000–1,000,000 patients. It typically affects infants and younger children; however, presentations in adults have been reported. In infants and children, it has a strong association with neuroblastoma, and a diagnosis of OMS should include a thorough assessment for this malignancy [55•, 56•].However, like with ITM, various infectious etiologies have been implicated in tumor-negative cases [57•, 58].
Patients typically present clinically over days to weeks with a progressive ataxia with myoclonic movements and often opsoclonus. In younger ambulatory children, it can manifest as a regression of motor milestones. Imaging is often benign-appearing, although there are rare reports of some findings on advanced neuroimaging techniques. The localization of the cause of these symptoms is thought to be due to lesions within the brainstem, cerebellum, or both and/or the connections between the two structures, with possible secondary effects on the cortex [59•]. CSF findings sometimes show nonspecific markers of inflammation in the acute phase, such as a pleocytosis or elevated oligoclonal bands or IgG index or synthesis rate. Flow cytometry is not routinely done, but an abnormal expansion of B cells in the CSF has also been reported [60].
For the acute phase, IV steroids, ACTH, and IVIg are the most routinely used treatment modalities [61, 62•]. PLEX has been described with anecdotal success [63, 64].More recently, initiation of IV rituximab as an adjunctive treatment has been described [65•]. In general, the symptoms tend to be highly steroid/ACTH-responsive, and this author recommends a prolonged steroid taper following the acute phase for 12–16 weeks if the patient proves to respond well to steroids. In patients that do not respond well to steroids, IVIg or PLEX should be considered [66, 67].
Following the acute phase of the disease, the risk for residual sequelae is high even in patients with a seemingly good clinical response. The ataxia, myoclonus, and opsoclonus do tend to improve with treatment, but the risk for chronic neurobehavioral deficits has been reported to be as high as 80% of patients. Patients can have cognitive problems, sleep difficulties, and unusual anger outbursts described as “rage” episodes [68]. Occasionally, patients can have deficits related to residual myoclonic movements or ataxia affecting their ability to walk or perform tasks, such as writing and eating. For the cognitive concerns, patients should be assessed and followed with formal neuropsychological testing. Rehabilitation should focus on improving gross and fine motor control and medications to manage the behavioral symptoms [69, 70].
With respect to relapses in OMS, it has been described as a relapsing neuroinflammatory syndrome; however, there is no clear imaging or laboratory marker for relapses [71•]. It is not clear whether or not long-term immunosuppressive medication usage reduces the risk for relapses or neurologic morbidity; however, re-exacerbation of previous symptoms, typically identical to the initial acute phase but less severe, tends to respond well to brief high-dose steroid or ACTH pulses. Medications that have been used long-term include mycophenolate mofetil, IV rituximab, IV-pulsed cyclophosphamide, and azathioprine [72,73,74]. There is no clear consensus, beyond aggressive treatment in the acute phase, about long-term immunotherapy management for OMS.
Acute Cerebellar Ataxia
Acute cerebellar ataxia is an acute syndrome presenting with ataxia of gait or extremities often evolving over days to weeks. It is a disease almost universally of young children. It is routinely considered post-infectious in etiology, although numerous pathogens have been described. In patients that are functionally impacted, MRI brain and lumbar puncture are typically recommended. Patients often show lesions within the cerebellum, although MRI-negative cases have been described. CSF findings such as a pleocytosis or elevated protein have been described but are not universal [75].
In patients that are significantly affected, especially if ambulatory patients that cannot walk, a course of high-dose IV steroids, methylprednisolone 30 mg/kg/day for 3–5 days (max dose of 1000 mg) is not unreasonable. In patients with a severe course, those with a suboptimal steroid response, and/or those that present with deterioration after initial improvement, OMS should be considered as an alternative diagnosis. If there are clear imaging findings, malignancies may need to be considered depending on the features of the cerebellar lesion(s) [62•].
Rehabilitation should be akin to patients that have suffered a cerebellar stroke with a focus on motor planning and techniques to retrain the patient’s vestibular system, although patients can also recover spontaneously [76].Overall prognosis is typically excellent.
Other Brainstem Syndromes
Although NMO typically presents with a myelitis or optic neuritis, a common prodrome in approximately a third of presenting relapses involves the area postrema in the medulla. Patients can have refractory vomiting or hiccoughs that can last for days. This often delays diagnosis in patients not previously diagnosed. In established NMO patients or patients with an initial demyelinating event suspicious for NMO but has not met full diagnostic criteria, a syndrome >24 h of persistent vomiting or hiccoughing should be considered as highly suspicious for a relapse [77•, 78, 79]. Other neurologic attacks in NMO referable to the brainstem have been described but are not as common [80, 81•].
MS can involve any aspect of the CNS, and any brainstem syndrome can occur with it. One syndrome that has a high predilection for occurring in MS more so than other neuroinflammatory disorders is an internuclear ophthalmoplegia (INO). Presence of an INO on examination should be regarded as highly suspicious for MS [82]. Bell’s palsy can also be seen with MS patients where a lesion may be present in the brainstem at the entry zone of CN VII [83]. Virtually, all other cranial neuropathies have been reported with MS [84]. MS patients can also present with various forms of ataxia, and lesions can occur throughout the cerebellum and the cerebellar peduncles. Middle cerebellar peduncular lesions tend to be quite common in MS patients [85].
As described above, acute exacerbations of either MS or NMO are best initially treated with IV high-dose steroids and PLEX in refractory cases.
Neurosarcoidosis can also present with brainstem involvement and has been associated with various cranial neuropathies [49, 86].
Brain
Acute Disseminated Encephalomyelitis and Autoimmune Encephalitis
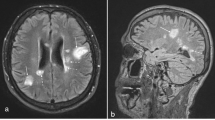
Acute disseminated encephalomyelitis (ADEM) and autoimmune encephalitis (AE) are two separate diseases that primarily affect the brain. ADEM can present with both brain and cord lesions, and it is similar to ITM in that it is thought to be due to a secondary autoimmune response to a potential viral trigger and generally requires imaging findings, CSF results, and exclusion of other causes to establish the diagnosis. Typically, patients present over several hours to days with a progressive neurologic syndrome of weakness, numbness, altered mental status, and seizures amongst other symptoms. Unlike with an MS patient presenting with an initial demyelinating event, patients typically have some degree of an encephalopathy. The patients are usually children, although adolescents and adults can acquire ADEM. The incidence mirrors that of ITM. Unlike ITM, the prognosis is generally more favorable. Typical treatments are high-dose IV steroids for 3–5 days, 30 mg/kg/day (max dose 1000 mg), IVIg (0.4 g/kg/day) for 3–5 days, or PLEX (minimum of five exchanges) [87, 88•].
AE is becoming a more recognized neurologic disease that is really a set of disorders based on diagnostic testing. The most common and well-recognized is anti-NMDA receptor antibody encephalitis (NMDAR). The typical patients present with seizures, encephalopathy, and often have a movement disorder; however, psychiatric manifestations can occur and patients will sometimes exhibit very bizarre behaviors. NMDAR diagnosis is made with the test for anti-NMDA antibodies, and suspected cases should be tested in the blood and CSF, as some patients will only be positive in the CSF. Typical acute treatments are steroids, IVIg, and PLEX; however, patients are more likely than ADEM patients to need more long-term immunotherapy such as cyclophosphamide, dosed at 750–1000 mg/m2 monthly for 3–6 months, or IV rituximab, dosed at 375 mg/m2 or 1000 mg 1–2 times over 4 weeks. Prognosis is generally favorable, but recovery can require months to years. Due to the cognitive and psychiatric impacts, formal neuropsychological testing is recommended [89, 90•, 91•, 92•, 93•, 94•, 95•].
Rehabilitation for ADEM (for those patients with significant sequelae) and AE often more closely mirrors rehabilitation for traumatic brain injury (TBI) patients [96]. When recovery is incomplete, treatment is based on managing ongoing symptoms.
Conclusion
Immune-mediated CNS disorders present unique challenges in diagnosis, treatment, and long-term management. Underlying diagnostic considerations are crucial, and aggressive treatment during the acute phase of these disorders can have significant impact on prognosis.
References
Papers of particular interest, published recently have been highlighted as: • Of importance
Krishnan C, Kaplin AI, Pardo CA, Kerr DA, Keswani SC. Demyelinating disorders: update on transverse myelitis. Curr Neurol Neurosci Rep. 2006;6(3):236–43.
Krishnan C, Kaplin AI, Deshpande DM, Pardo CA, Kerr DA. Transverse myelitis: pathogenesis, diagnosis and treatment. Front Biosci. 2004;9:1483–99.
Harzheim M, Schlegel U, Urbach H, Klockgether T, Schmidt S. Discriminatory features of acute transverse myelitis: a retrospective analysis of 45 patients. J Neurol Sci. 2004;217(2):217–23.
Scott TF. Nosology of idiopathic transverse myelitis syndromes. Acta Neurol Scand. 2007;115(6):371–6.
Kuo SC, Cho WH, Shih HI, Tu YF. Idiopathic acute transverse myelitis in children: a retrospective series. Neuropediatrics. 2015;46(5):307–12.
• Huh Y, Park EJ, Jung JW, Oh S, Choi SC. Clinical insights for early detection of acute transverse myelitis in the emergency department. Clin Exp Emerg Med. 2015;2(1):44–50. This citation was flagged due to it being a larger case series (N = 46) and is a more recent study and highlights the potential for misdiagnosis with a myelitis event.
• Greenberg BM, Frohman EM. Immune-mediated myelopathies. Continuum (Minneap Minn). 2015;21(1 Spinal Cord Disorders):121–31. This citation was flagged due to it being a newer comprehensive review of myelopathies and the importance of diagnostic category and aggressive treatment where appropriate.
• Goh C, Desmond PM, Phal PM. MRI in transverse myelitis. J Magn Reson Imaging. 2014;40(6):1267–79. This citation was flagged due to it highlighting the importance of location of lesions within the spinal cord with a three-dimensional approach in a diagnosis of myelitis and considerations of how location of a lesion within the spinal cord has clear diagnostic implications.
Hiraga A, Sakakibara R, Mori M, Yamanaka Y, Ito S, Hattori T. Urinary retention can be the sole initial manifestation of acute myelitis. J Neurol Sci. 2006;251(1–2):110–2.
Hammond ER, Kerr DA. Priapism in infantile transverse myelitis. Arch Neurol. 2009 Jul;66(7):894–7.
Transverse Myelitis Consortium Working Group. Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology. 2002;59(4):499–505. Review
West TW, Hess C, Cree BA. Acute transverse myelitis: demyelinating, inflammatory, and infectious myelopathies. Semin Neurol. 2012 Apr;32(2):97–113.
Nardone R, Versace V, Brigo F, Tezzon F, Zuccoli G, Pikija S, et al. Herpes simplex virus type 2 myelitis: case report and review of the literature. Front Neurol. 2017;8:199.
Figueroa D, Isache C, Sands M, Guzman N. An unusual case of acute transverse myelitis caused by HSV-1 infection. IDCases. 2016;5:29–31.
Sendi P, Hirzel C, Bloch A, Fischer U, Jeannet N, Berlinger L, et al. Bartonella-associated transverse myelitis. Emerg Infect Dis. 2017;23(4):712–3.
Baylor P, Garoufi A, Karpathios T, Lutz J, Mogelof J, Moseley D. Transverse myelitis in 2 patients with Bartonella henselae infection (cat scratch disease). Clin Infect Dis. 2007;45(4):e42–5.
• Absoud M, Greenberg BM, Lim M, Lotze T, Thomas T, Deiva K. Pediatric transverse myelitis. Neurology. 2016;87(9 Suppl 2):S46–52. This citation was flagged due to it being one of the more recent comprehensive reviews of myelitis in children.
• Dixit P, Garg RK, Malhotra HS, Jain A, Verma R, Sharma PK, et al. Cytokines and matrix metalloproteinases in the cerebrospinal fluid of patients with acute transverse myelitis: an outcome analysis. Inflamm Res. 2016;65(2):125–32. This citation was flagged due to it being one of the few studies that looked at CSF cytokines in patients with myelitis with a control group.
Kaplin AI, Deshpande DM, Scott E, Krishnan C, Carmen JS, Shats I, et al. IL-6 induces regionally selective spinal cord injury in patients with the neuroinflammatory disorder transverse myelitis. J Clin Invest. 2005;115(10):2731–41.
Uzawa A, Mori M, Arai K, Sato Y, Hayakawa S, Masuda S, et al. Cytokine and chemokine profiles in neuromyelitis optica: significance of interleukin-6. Mult Scler. 2010;16(12):1443–52.
• El Mekabaty A, Pardo CA, Gailloud P. The yield of initial conventional MRI in 115 cases of angiographically confirmed spinal vascular malformations. J Neurol. 2017;264(4):733–9 This citation was flagged due to it highlighting the low potential yield of MRI with respect to the diagnosis of vascular myelopathies.
• Chen J, Gailloud P. Safety of spinal angiography: complication rate analysis in 302 diagnostic angiograms. Neurology. 2011;77(13):1235–40. This citation was flagged to highlight the importance of spinal catheter angiography in diagnosis of vascular myelopathies and also notes a significant rate of misdiagnosis of transverse myelitis that were actually vascular in origin.
• Rengarajan B, Venkateswaran S, McMillan HJ. Acute asymmetrical spinal infarct secondary to fibrocartilaginous embolism. Childs Nerv Syst. 2015;31(3):487–91 This citation was flagged (N = 2) as one of the few newer studies noting that fibrocartilaginous embolus is a known mimicker of idiopathic transverse myelitis and it needs to be considered in any patient with an acute myelopathy.
• Koch MJ, Stapleton CJ, Agarwalla PK, Torok C, Shin JH, Coumans JV, et al. Open and endovascular treatment of spinal dural arteriovenous fistulas: a 10-year experience. J Neurosurg Spine. 2017;26(4):519–23. This citation was flagged due to it highlighting the importance of consideration of the fact that certain vascular myelopathies are potentially treatable as with dural AV fistulas in this case series (N = 47).
• Yoder JA, Lloyd M, Zabrocki L, Auten J. Pediatric acute flaccid paralysis: enterovirus D68-associated anterior myelitis. J Emerg Med. 2017. This case report was flagged to highlight the perspective of Emergency room physicians with respect to a potential myelitis case and to note that cases of acute flaccid myelitis are still occurring outside of the initial outbreak in 2014.
• Esposito S, Chidini G, Cinnante C, Napolitano L, Giannini A, Terranova L, et al. Acute flaccid myelitis associated with enterovirus-D68 infection in an otherwise healthy child. Virol J. 2017;14(1):4. This case report was flagged to note the suspected viral link with acute flaccid myelitis.
• Messacar K, Schreiner TL, Van Haren K, Yang M, Glaser CA, Tyler KL, et al. Acute flaccid myelitis: a clinical review of US cases 2012–2015. Ann Neurol. 2016;80(3):326–38. This study was flagged as the most comprehensive review of the most recent U.S. data on acute flaccid myelitis.
Kalita J, Misra UK, Mandal SK. Prognostic predictors of acute transverse myelitis. Acta Neurol Scand. 1998;98(1):60–3.
Misra UK, Kalita J. Can electromyography predict the prognosis of transverse myelitis? J Neurol. 1998;245(11):741–4.
Ravaglia S, Moglia A, Bogdanov EI. Presyrinx in children with Chiari malformations. Neurology. 2009;72(22):1966–7.
• Vadivelu S, Vadivelu S, Mealy M, Patel S, Kosnik-Infinger L, Becker D. Chiari I malformation in children with transverse myelitis. Dev Neurorehabil. 2017;24:1–6. This study was flagged due to it being one of the newest articles to demonstrate a concern for a link between Chiari malformations and the diagnosis of idiopathic transverse myelitis.
Greenberg BM, Thomas KP, Krishnan C, Kaplin AI, Calabresi PA, Kerr DA. Idiopathic transverse myelitis: corticosteroids, plasma exchange, or cyclophosphamide. Neurology. 2007;68(19):1614–7.
Scott TF, Frohman EM, De Seze J, Gronseth GS, Weinshenker BG, Therapeutics and Technology Assessment Subcommittee of American Academy of Neurology. Evidence-based guideline: clinical evaluation and treatment of transverse myelitis: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2011;77(24):2128–34.
• Beh SC, Kildebeck E, Narayan R, Desena A, Schell D, Rowe ES, et al. High-dose methotrexate with leucovorin rescue: for monumentally severe CNS inflammatory syndromes. J Neurol Sci. 2017;372:187–95. This citation was flagged due to it highlighting the importance of high-dose IV methotrexate as a therapeutic option for severe CNS inflammatory diseases (N =10).
Chiganer EH, Hryb JP, Carnero Contentti E. Myelitis and lupus: clinical manifestations, diagnosis and treatment. Review. Reumatol Clin. 2016.
Greenberg BM, Graves D, Remington G, Hardeman P, Mann M, Karandikar N, et al. Rituximab dosing and monitoring strategies in neuromyelitis optica patients: creating strategies for therapeutic success. Mult Scler. 2012;18(7):1022–6.
• Jones ML, Evans N, Tefertiller C, Backus D, Sweatman M, Tansey K, et al. Activity-based therapy for recovery of walking in individuals with chronic spinal cord injury: results from a randomized clinical trial. Arch Phys Med Rehabil. 2014;95(12):2239–46. This study was flagged as a newer clinical trial that supports the importance of activity-based rehabilitation for patients with spinal cord injuries, even outside of the acute phase.
Sadowsky CL, Hammond ER, Strohl AB, Commean PK, Eby SA, Damiano DL, et al. Lower extremity functional electrical stimulation cycling promotes physical and functional recovery in chronic spinal cord injury. J Spinal Cord Med. 2013;36(6):623–31.
Dorsi MJ, Belzberg AJ. Nerve transfers for restoration of upper extremity motor function in a child with upper extremity motor deficits due to transverse myelitis: case report. Microsurgery. 2012;32(1):64–7.
Hattori Y, Doi K, Baliarsing AS. A part of the ulnar nerve as an alternative donor nerve for functioning free muscle transfer: a case report. J Hand Surg Am. 2002;27(1):150–3.
• Marignier R, Cobo Calvo A, Vukusic S. Neuromyelitis optica and neuromyelitis optica spectrum disorders. Curr Opin Neurol. 2017;30(3):208–15. This citation was flagged due to it being a newer comprehensive review of NMO-SD with the new criteria and recognition of the anti-MOG phenotype considerations.
Tenembaum S, Chitnis T, Nakashima I, Collongues N, McKeon A, Levy M, et al. Neuromyelitis optica spectrum disorders in children and adolescents. Neurology. 2016;87(9 Suppl 2):S59–66.
• Kitley J, Palace J. Therapeutic options in neuromyelitis optica spectrum disorders. Expert Rev Neurother. 2016;16(3):319–29. This citation was flagged due to it being a newer and comprehensive review of best available options for long-term NMO disease management.
English C, Aloi JJ. New FDA-approved disease-modifying therapies for multiple sclerosis. Clin Ther. 2015;37(4):691–715.
Menge T, Dubey D, Warnke C, Hartung HP, Stüve O. Ocrelizumab for the treatment of relapsing-remitting multiple sclerosis. Expert Rev Neurother. 2016;16(10):1131–9.
Newsome SD, Aliotta PJ, Bainbridge J, Bennett SE, Cutter G, Fenton K, et al. A framework of care in multiple sclerosis, part 2: symptomatic care and beyond. Int J MS Care. 2017;19(1):42–56.
• Radwan W, Lucke-Wold B, Robadi IA, Gyure K, Roberts T, Bhatia S. Neurosarcoidosis: unusual presentations and considerations for diagnosis and management. Postgrad Med J. 2016;5. This case series (N= 3) was flagged due to a good demonstration of the heterogeneity of neurosarcoidosis presentation.
• Ibitoye RT, Wilkins A, Scolding NJ. Neurosarcoidosis: a clinical approach to diagnosis and management. J Neurol. 2017;264(5):1023–8. This study was flagged due to it being a newer comprehensive review of the diagnostic approach and pitfalls and the options for management for neurosarcoidosis.
Fritz D, van de Beek D, Brouwer MC. Clinical features, treatment and outcome in neurosarcoidosis: systematic review and meta-analysis. BMC Neurol. 2016;16(1):220.
Costallat BL, Ferreira DM, Costallat LT, Appenzeller S. Myelopathy in systemic lupus erythematosus: clinical, laboratory, radiological and progression findings in a cohort of 1,193 patients. Rev Bras Reumatol Engl Ed. 2016;56(3):240–51.
Carvajal Alegria G, Guellec D, Mariette X, Gottenberg JE, Dernis E, Dubost JJ, et al. Epidemiology of neurological manifestations in Sjögren's syndrome: data from the French ASSESS cohort. RMD Open. 2016;2(1)
Man BL, Mok CC, Fu YP. Neuro-ophthalmologic manifestations of systemic lupus erythematosus: a systematic review. Int J Rheum Dis. 2014;17(5):494–501.
Bak E, Yang HK, Hwang JM. Optic neuropathy associated with primary Sjögren's syndrome: a case series. Optom Vis Sci. 2017;94(4):519–26.
Garrett G, Ambrose N, Davids Z, Bindman D. Course of neuropsychiatric symptoms during flares of systemic lupus erythematosus (SLE). Case Rep Psychiatry. 2017;2017:2890436. doi:10.1155/2017/2890436.
• Meena JP, Seth R, Chakrabarty B, Gulati S, Agrawala S, Naranje P. Neuroblastoma presenting as opsoclonus-myoclonus: a series of six cases and review of literature. J Pediatr Neurosci. 2016;11(4):373–7. This study was flagged as a newer study of Opsoclonus-myoclonus patients (N=6) and demonstrated a newer finding of a low relapse rate with patients treated appropriately in the acute phase
• Blaes F, Dharmalingam B. Childhood opsoclonus-myoclonus syndrome: diagnosis and treatment. Expert Rev Neurother. 2016;16(6):641–8. This study was flagged as a more recent thorough review of diagnostic approach and management options for opsoclonus-myoclonus.
• Armangué T, Sabater L, Torres-Vega E, Martínez-Hernández E, Ariño H, Petit-Pedrol M, et al. Clinical and immunological features of opsoclonus-myoclonus syndrome in the era of neuronal cell surface antibodies. JAMA Neurol. 2016;73(4):417–24. This study was cited as one of the largest studies (N =114) of adults with opsoclonus-myoclonus syndrome.
Hasegawa S, Matsushige T, Kajimoto M, Inoue H, Momonaka H, Japanese Society for Pediatric Immune-Mediated Brain Diseases, et al. A nationwide survey of opsoclonus-myoclonus syndrome in Japanese children. Brain Dev. 2015;37(7):656–60.
• Anand G, Bridge H, Rackstraw P, Chekroud AM, Yong J, Stagg CJ, et al. Cerebellar and cortical abnormalities in paediatric opsoclonus-myoclonus syndrome. Dev Med Child Neurol. 2015;57(3):265–72. This study was cited as one of the few studies that demonstrates a clear imaging abnormality in patients with a history of opsoclonus-myoclonus syndrome as compared to a control group (N = 9).
Pranzatelli MR, Travelstead AL, Tate ED, Allison TJ, Verhulst SJ. CSF B-cell expansion in opsoclonus-myoclonus syndrome: a biomarker of disease activity. Mov Disord. 2004;19(7):770–7.
Nosadini M, Mohammad SS, Suppiej A, Sartori S, Dale RC, IVIG in neurology study group. Intravenous immunoglobulin in paediatric neurology: safety, adherence to guidelines, and long-term outcome. Dev Med Child Neurol. 2016;58(11):1180–92.
• Mitchell WG, Wooten AA, O'Neil SH, Rodriguez JG, Cruz RE, Wittern R. Effect of increased immunosuppression on developmental outcome of opsoclonus myoclonus syndrome (OMS). J Child Neurol. 2015;30(8):976–82. This citation was flagged to demonstrate that more aggressive treatment for opsoclonus-myoclonus syndrome earlier in the disease course may be associated with better outcomes.
Cooper CJ, Said S. West nile virus encephalitis induced opsoclonus-myoclonus syndrome. Neurol Int. 2014;6(2):5359.
Karaca S, Kozanoğlu İ, Karakurum Göksel B, Karataş M, Tan M, Yerdelen VD, et al. Therapeutic plasma exchange in neurologic diseases: an experience with 91 patients in seven years. Noro Psikiyatr Ars. 2014;51(1):63–8.
• Toyoshima D, Morisada N, Takami Y, Kidokoro H, Nishiyama M, Nakagawa T, et al. Rituximab treatment for relapsed opsoclonus-myoclonus syndrome. Brain Dev. 2016;38(3):346–9. This study was cited highlighting the importance of consideration of rituximab for opsoclonus-myoclonus syndrome.
Gadian J, Kirk E, Holliday K, Lim M, Absoud M. Systematic review of immunoglobulin use in paediatric neurological and neurodevelopmental disorders. Dev Med Child Neurol. 2017;59(2):136–44.
Mesraoua B, Abbas M, D'Souza A, Miyares FR, Hashem M, Osman Y, et al. Adult opsoclonus-myoclonus syndrome following mycoplasma pneumoniae infection with dramatic response to plasmapheresis. Acta Neurol Belg. 2011;111(2):136–8.
Pranzatelli MR, Tate ED, Dukart WS, Flint MJ, Hoffman MT, Oksa AE. Sleep disturbance and rage attacks in opsoclonus-myoclonus syndrome: response to trazodone. J Pediatr. 2005;147(3):372–8.
De Grandis E, Parodi S, Conte M, Angelini P, Battaglia F, Gandolfo C, et al. Long-term follow-up of neuroblastoma-associated opsoclonus-myoclonus-ataxia syndrome. Neuropediatrics. 2009;40(3):103–11.
Catsman-Berrevoets CE, Aarsen FK, van Hemsbergen ML, van Noesel MM, Hakvoort-Cammel FG, van den Heuvel-Eibrink MM. Improvement of neurological status and quality of life in children with opsoclonus myoclonus syndrome at long-term follow-up. Pediatr Blood Cancer. 2009;53(6):1048–53.
• Pranzatelli MR, Tate ED. Trends and tenets in relapsing and progressive opsoclonus-myoclonus syndrome. Brain Dev. 2016;38(5):439–48. This citation was flagged as a comprehensive review of the theory of opsoclonusmyoclonus syndrome as a relapsing and progressive neuroimmunologic disease.
Pranzatelli MR, Tate ED, Travelstead AL, Baumgardner CA, Gowda NV, Halthore SN, et al. Insights on chronic-relapsing opsoclonus-myoclonus from a pilot study of mycophenolate mofetil. J Child Neurol. 2009;24(3):316–22.
Pike M. Opsoclonus-myoclonus syndrome. Handb Clin Neurol. 2013;112:1209–11.
Tate ED, Pranzatelli MR, Verhulst SJ, Markwell SJ, Franz DN, Graf WD, et al. Active comparator-controlled, rater-blinded study of corticotropin-based immunotherapies for opsoclonus-myoclonus syndrome. J Child Neurol. 2012;27(7):875–84.
Desai J, Mitchell WG. Acute cerebellar ataxia, acute cerebellitis, and opsoclonus-myoclonus syndrome. J Child Neurol. 2012;27(11):1482–8.
Bultmann U, Pierscianek D, Gizewski ER, Schoch B, Fritsche N, Timmann D, et al. Functional recovery and rehabilitation of postural impairment and gait ataxia in patients with acute cerebellar stroke. Gait Posture. 2014;39(1):563–9.
• Garg P, Rajasekaran M, Pandey S, Gurusamy G, Balalakshmoji D, Rathinasamy R. Magnetic resonance imaging brain findings in a case of aquaporin-4 antibody-positive neuromyelitis optica spectrum disorder, presenting with intractable vomiting and hiccups. J Neurosci Rural Pract. 2017;8(1):135–8. This citation was flagged as an excellent example of the imaging findings that correlate with the vomiting and hiccupping syndrome in NMO patients.
Popescu BF, Lennon VA, Parisi JE, Howe CL, Weigand SD, Cabrera-Gómez JA, et al. Neuromyelitis optica unique area postrema lesions: nausea, vomiting, and pathogenic implications. Neurology. 2011;76(14):1229–37.
Cheng C, Jiang Y, Lu X, Gu F, Kang Z, Dai Y, et al. The role of anti-aquaporin 4 antibody in the conversion of acute brainstem syndrome to neuromyelitis optica. BMC Neurol. 2016;16(1):203.
Li Y, Jiang B, Chen B, Zhao M, Zhou C, Wang S, et al. Neuromyelitis optica spectrum disorders with multiple brainstem manifestations: a case report. Neurol Sci. 2016;37(2):309–13.
• Kremer L, Mealy M, Jacob A, Nakashima I, Cabre P, Bigi S, et al. Brainstem manifestations in neuromyelitis optica: a multicenter study of 258 patients. Mult Scler. 2014;20(7):843–7. This citation was flagged as one of the larger studies (N = 258) of brainstem manifestations in NMO patients.
Nerrant E, Tilikete C. Ocular motor manifestations of multiple sclerosis. J Neuroophthalmol. 2017;13
Saleh C, Patsi O, Mataigne F, Beyenburg S. Peripheral (seventh) nerve palsy and multiple sclerosis: a diagnostic dilemma—a case report. Case Rep Neurol. 2016;8(1):27–33.
Evlice A, Demir T, Kaleağası C, Özcan F, Demirkıran M. Rare onset symptoms in multiple sclerosis. Acta Clin Belg. 2016;71(3):154–7.
Preziosa P, Rocca MA, Mesaros S, Pagani E, Drulovic J, Stosic-Opincal T, et al. Relationship between damage to the cerebellar peduncles and clinical disability in multiple sclerosis. Radiology. 2014;271(3):822–30.
Shimizu K, Yuki K, Sadatomo T, Kurisu K. Isolated neurosarcoidosis presenting with multiple cranial nerve palsies. Surg Neurol Int. 2016;7:44.
Pohl D, Alper G, Van Haren K, Kornberg AJ, Lucchinetti CF, Tenembaum S, et al. Acute disseminated encephalomyelitis: updates on an inflammatory CNS syndrome. Neurology. 2016;87(9 Suppl 2):S38–45.
• Brenton JN, Banwell BL. Therapeutic approach to the management of pediatric demyelinating disease: multiple sclerosis and acute disseminated encephalomyelitis. Neurotherapeutics. 2016;13(1):84–95. This citation was flagged as one of the most comprehensive and thorough reviews of the treatment and management for ADEM.
Gable M, Glaser C. Anti-N-methyl-D-aspartate receptor encephalitis appearing as a new-onset psychosis: disease course in children and adolescents within the California Encephalitis Project. Pediatr Neurol. 2017; doi:10.1016/j.pediatrneurol.2017.01.023.
• Hallowell S, Tebedge E, Oates M, Hand E. Rituximab for treatment of refractory anti-NMDA receptor encephalitis in a pediatric patient. J Pediatr Pharmacol Ther. 2017;22(2):118–23. This citation was flagged as a newer example of the importance of rituximab for treatment for anti-NMDA receptor antibody encephalitis.
• Dale RC, Gorman MP, Lim M. Autoimmune encephalitis in children: clinical phenomenology, therapeutics, and emerging challenges. Curr Opin Neurol. 2017;30(3):334–44. This citation was flagged as one of the newer and more comprehensive reviews of autoimmune encephalitis in children and considerations for management.
• Nagappa M, Parayil SB, Mahadevan A, Sinha S, Mathuranath PS, Taly AB. Management of Anti- N-methyl-D-aspartate (NMDA) receptor encephalitis in children. J Child Neurol. 2017;32(5):513–4. This citation was flagged as one of the most recent reviews of management for anti- NMDA receptor antibody encephalitis.
• Zhang L, Wu MQ, Hao ZL, Chiang SM, Shuang K, Lin MT, et al. Clinical characteristics, treatments, and outcomes of patients with anti-N-methyl-D-aspartate receptor encephalitis: a systematic review of reported cases. Epilepsy Behav. 2017;68:57–65. This citation was cited as one of the larger series of anti-NMDA receptor antibody encephalitis (N =412) and noted equivalence in efficacy between steroids and IVIg therapy.
• McKeon GL, Scott JG, Spooner DM, Ryan AE, Blum S, Gillis D, et al. Cognitive and social functioning deficits after anti-N-methyl-D-aspartate receptor encephalitis: an exploratory case series. J Int Neuropsychol Soc. 2016;22(8):828–38. This citation was flagged exploring the impacts on cognitive function with patients with known anti-NMDA receptor antibody encephalitis.
• DeSena AD, Noland DK, Matevosyan K, King K, Phillips L, Qureshi SS, et al. Intravenous methylprednisolone versus therapeutic plasma exchange for treatment of anti-N-methyl-D-aspartate receptor antibody encephalitis: a retrospective review. J Clin Apher. 2015;30(4):212–6. This citation was flagged highlighting a study that demonstrated that plasma exchange may be the most superior first-line therapy for anti-NMDA receptor antibody encephalitis.
Beis JM, Renard M. Adult anti-NMDA receptor encephalitis: which physical and rehabilitation medicine program? Case reports and literature review. Ann Phys Rehabil Med. 2016;59S:e153–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Allen D. DeSena declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Spinal Cord Injury Rehabilitation
Rights and permissions
About this article
Cite this article
DeSena, A.D. Immune-Mediated CNS Diseases: a Review. Curr Phys Med Rehabil Rep 5, 134–142 (2017). https://doi.org/10.1007/s40141-017-0160-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-017-0160-y