Abstract
As prevalence of obesity continues to rise in the United States, we are beginning to elucidate the complex role of obesity-associated chronic inflammation, endocrine dysfunction, and hormone production as a driver for increased breast cancer risk. Epidemiological data suggest that obesity (BMI > 30) is associated with increased breast cancer incidence, worse prognosis, and higher mortality rates. Mechanistically, obesity and excess fat mass represent a state of chronic inflammation, insulin resistance, adipokine imbalance, and increased estrogen signaling. This pro-tumorigenic environment stimulates cancer development through abnormal growth, proliferation, and survival of mammary tissue. Importantly, obesity is a modifiable risk factor; alterations in cell proliferation, apoptosis, circulating estrogen, and insulin sensitivity are observed in response to weight loss attainable through behavior modification including dietary and exercise changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the second leading cause of cancer-related death in US women; approximately, 1 in 8 women (12 %) in the US will develop invasive breast cancer over the course of her lifetime. According to the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) data [1], over 231,000 new cases of invasive breast cancer will have been diagnosed in women in 2015, with breast cancer incidence continuing to rise. Despite advances in diagnostic screening and cancer treatment, over 40,000 women in the US will have died from breast cancer in 2015 [2].
Breast cancer is a heterogeneous disease that varies based on molecular subtype, clinical-pathological presentation, prognosis, and treatment. Tumor characteristics and response to treatment vary based on tumor stage, tumor grade, and expression of various receptors. Tumors are histologically classified by receptor positivity, which includes estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor-2 (HER2). A variety of factors have been shown to impact an individual’s risk of developing breast cancer and their ultimate prognosis. Some of the more well-established risk factors include age, family history, and estrogen exposure (nulliparity, hormone replacement therapy, and age at menarche, first full-term pregnancy, and menopause) [3]; more recently, obesity has been identified as a modifiable, lifestyle-associated risk factor. Obesity and weight gain tends to be associated with ER receptor positivity [4, 5], especially among the obese postmenopausal population [6]. Prior to menopause, ovarian synthesis is the main source of estrogen production. Circulating estradiol levels after menopause are proportional to fat mass and are directly related to breast cancer risk [7, 8]. The relationship between obesity and postmenopausal breast cancer appears to be causal especially with evidence documenting a 50 % reduction in risk of breast cancer seen among women who lost and maintained more than 10 kg after menopause [7].
In this review, we will first discuss the controversial definition of obesity. Then we will focus on the evidence derived from population studies that link obesity to increased risk of breast cancer and worse breast cancer outcomes. We will summarize our current understanding of the pathophysiology and molecular mechanisms of how obesity can promote tumorigenesis. Finally, we will review several obesity reduction methods as cost-effective strategies to reduce breast cancer risk and improve breast cancer outcomes.
Obesity—Definition
Obesity can be defined multiple ways, including body weight, fat distribution (central vs. peripheral), and body mass index (BMI [kg/m2]; body weight relative to height). BMI 25–29.9 is considered overweight and greater than 30 is classified as obese (Table 1). While we have adopted the BMI classification system for our definition of obesity, it is important to note that body fat distribution has a significant impact on health and hormone signaling.
Central adiposity has been found to be an independent predictor of postmenopausal breast cancer risk and is an important risk factor to consider as waist circumferences continue to expand in the United States [8, 9]. Based on BMI criteria, approximately 78.6 million adults in the U.S. (35 %) are considered obese [10]. Specifically, the prevalence of obesity among women aged 60 and older has increased from 31.5 to 42 % over the past decade [9, 11]. Central adiposity, defined by waist-to-hip ratio greater than 0.80 in women and 0.95 in men, represents metabolically active visceral fat that is associated with multiple health risks, such as metabolic syndrome, coronary artery disease, and many cancers [12]. BMI, however, is not an accurate measure of adipose versus lean mass and does not take into account fat distribution. As such, BMI is prone to overestimating fat mass in physically active people and underestimating fat mass in sarcopenic older patients [13••]. Compared to BMI, body composition more accurately reflects metabolically active adipose tissue, with visceral fat contributing significantly to metabolic changes [14, 15]. Nonetheless, BMI remains the most practical and widely used parameter for defining obesity in populations.
Obesity is Linked to Increased Risk of Cancer and Poor Cancer Outcomes
As presented by Wolin et al., historical data reveal that obesity is a cause of cancer death in approximately 20 % of women, which is especially significant considering the prevalence of obesity and overweight had increased from 15 % in 1980 to 35 % in 2005. Further, they purport that approximately 20 % of all cancer cases are attributed to overweight and obesity [16].
Obesity has been linked to increased risk of breast cancer and other epithelial malignancies [17••, 18]. Multiple studies have reported an increased relative risk ranging from 1.5 to 2.5 for breast cancer among women with BMI > 30 [19–21]. Research has suggested that central adiposity [9] as a measure of visceral fat may be a better surrogate for increased risk of postmenopausal breast cancer than other anthropometric qualifiers like BMI and body weight [17, 22]. The Sister Study, a large, prospective study found that waist circumference is independently associated with both pre- and postmenopausal breast cancer risk [9]. Body fat distribution, lifetime weight history, and weight fluctuations later in life also impact the disease. Weight gain in adulthood is an established risk factor for postmenopausal breast cancer [23]. Interestingly, when looking at breast cancer risk factors, weight gain in adulthood (20 to 50 years old) and BMI fall just below Gail Model parameters (free estradiol, parity, age of menopause, and quantitative breast density) in influence [24].
Epidemiological studies have suggested that obesity worsens breast cancer prognosis, specifically via increased incidence of recurrence, metastases, and mortality [25]. In a prospective study of over 500,000 women, each successive increase in BMI was associated in a step-wise fashion with worse breast cancer prognosis and increased mortality in both pre- and postmenopausal women [26]. Obese women tend to be diagnosed at later stages with larger primary tumors and greater likelihood of lymph node involvement [27]. Obesity is associated with greater tumor burden and higher grade of tumors at diagnosis [28, 29], and has detrimental impact on mortality among breast cancer patients regardless of menopausal status [30, 31]. It is purported that nearly 50 % of deaths in postmenopausal breast cancer patients can be linked to obesity [18]. Overweight and obesity has been estimated to directly account for approximately 15–30 % of cancer deaths in the US [26]. This is in stark contrast to the projected 90,000 cancer deaths per year that are avoided by maintaining a healthy weight (BMI < 25). Further, a positive correlation exists between obesity and breast cancer recurrence. Likewise, shorter disease-free survival and lower overall survival has been demonstrated in obese patients, independent of tumor stage at diagnosis [32–35].
In addition to affecting development and prognosis, obesity has been shown to negatively impact response to chemotherapy treatment [36•, 37] and increased BMI is associated with increased incidence of metastatic disease and decreased disease-free survival, regardless of subtype. Obesity complicates medical management of breast cancer and makes chemotherapy dosing more difficult. Chemotherapy dosing is often weight-based, so to avoid increased toxicity at higher doses, some obese women may not receive adequate therapeutic regimens. Obesity is related to increased risk of complications associated with all treatment modalities (surgery, radiation, chemotherapy).
The Molecular Mechanisms Underlying the Pro-tumorigenic Effects of Obesity
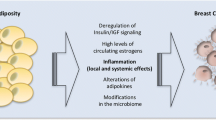
Originally, the pro-tumorigenic effects of obesity on breast cancer were mainly attributed to higher circulating estrogen levels due to increased aromatase expression by adipocytes [38]. However, there is a synergistic oncogenic effect of adipokine derangements, hyperglycemia with insulin resistance, and increased circulating estrogen that contributes to breast cancer development [39•]. The role of obesity is multifactorial and multiple estrogen-independent mechanisms exist. At present, there are at least three different hypotheses to explain the effect of obesity on cancer development, progression, and prognosis: (1) Obesity and its related metabolic syndrome create an environment of elevated insulin and IGF-1, which are potent epithelial mitogenic factors [22]; (2) Obesity promotes a chronic inflammatory state where by local cytokine secretion (IL-6, IL-1B, TNF-a) supports a pro-inflammatory tumor promoting microenvironment independent of hormonal mediators [40]; and (3) Increased estrogen secondary to enhanced aromatase activity in adipocytes can stimulate abnormal growth of ER + mammary cells [41–43].
Role of Obesity and Its Related Metabolic Syndrome on Tumorigenesis
Endocrine dysfunction plays a role in breast carcinogenesis and tumor growth. High BMI is associated with chronic hyperglycemia, elevated circulating insulin, insulin resistance, and ultimate development of metabolic syndrome. Hallmarks of the insulin resistant state include aberrant glucose metabolism, chronic inflammation, and altered production of hormones (IGF-1, leptin, adiponectin) [44, 45]. Hyperinsulinemia and type 2 Diabetes represent independent risk factors for colorectal, kidney, breast, endometrial, and pancreatic cancer, regardless of BMI [46].
Insulin and IGF-1
Insulin is a peptide hormone produced by beta cells of the pancreas that is released in response to circulating glucose levels. Insulin resistance impacts breast cancer progression via inflammation and growth factor signaling [47]. The role of insulin is multifold; insulin and its related insulin-like growth factor-1 (IGF-1) upregulate the PI3 K/Akt and Ras/Raf/MAPK systems, which are responsible for cell proliferation and inhibition of apoptosis [48, 49]. Downstream signaling pathways integrate intra- and extracellular conditions that regulate cell growth, survival, and metabolism [49, 50].
Hyperglycemia and hyperinsulinemia have been associated with increased hepatic IGF-1 production irrespective of growth hormone signaling [51]. Typically, IGF-1 binding proteins tightly regulate bioavailable IGF-1. However, in the obese, hyperglycemia leads to suppression of IGF-1 binding protein synthesis and hyperinsulinemia increases expression of hepatic GH receptor with consequent IGF-1 synthesis [51, 52]. Normally, IGF-1 interacts with circulating estrogen during normal mammary gland growth and differentiation [53]. Insulin and IGF-1 impact estrogen signaling via decreased hepatic synthesis of sex-hormone binding globulin (SHBG), which ultimately increases bioavailable estrogens [18] and enhances aromatase activity [54] thereby stimulating proliferation of ER + tumors. The IGF-1 receptor regulates proliferation, survival, differentiation, transformation, cell-substrate, and cell–cell interactions [55, 56]. IGF-1 receptor has been implicated in regulation of tumor microenvironment, epithelial-mesenchymal transition, and in development and maintenance of cancer stem cells [57]. Activation of the insulin and IGF-1 receptors has downstream effects that ultimately upregulate mammalian target of rapamycin (mTOR) [58], thereby inducing cell proliferation and survival.
Adipokines–Leptin and Adiponectin
In the healthy adult, leptin is an energy-sensing peptide hormone produced by adipocytes that is positively correlated with nutritional status and adipose stores [59]; as such, leptin signals the brain to reduce appetite. In the obese state, leptin overproduction by adipose tissue leads to resistance to this anorexigenic signal. Release of leptin is stimulated by insulin, estrogens, TNF-a, and glucocorticoids, which point to the complex interplay between fat storage and inflammation [59, 60]. Leptin has an impact on immune function, cytokine production, angiogenesis, and carcinogenesis. Furthermore, leptin exerts a tumorigenic effect on ER + tumors through upregulation of aromatase gene expression and estrogen synthesis [61]. The leptin receptor has been identified on many ER + tumors suggesting a potentiating effect of leptin on hormone receptor breast cancer development.
Conversely, adiponectin is a hormone secreted mainly by visceral white adipose tissue (WAT) that is negatively correlated with fat mass [62]. Its role is to modulate glucose metabolism, increase insulin sensitivity and lipolysis, and exert anti-inflammatory effects by downregulating obesity-associated inflammatory cytokines [63]. Studies have now implicated decreased circulating adiponectin levels—as seen in obesity—as a risk factor for cardiovascular disease, type 2 Diabetes, and several types of cancers [64]. As expected, there is an inverse relationship between breast cancer risk and systemic levels of adiponectin [63]. Specifically, adiponectin exhibits multiple anticancer effects: increased insulin sensitivity, activation of AMPK, and inhibition of NF-kB [65–67]. AMPK serves as a cellular energy sensor that increases skeletal muscle glucose uptake, reduces gluconeogenesis in the liver, increases insulin sensitivity, and promotes glucose utilization leading to increased fatty acid oxidation [68]. NF-kB activation is commonly observed in many tumors and is associated with elevated serum insulin, IGF-1, and leptin levels [49, 69–71]. Recent studies have identified a correlation between women with low circulating adiponectin levels and more aggressive breast cancer phenotypes (larger size, higher grade, ER negative, metastasis) [64].
Obesity and Chronic Inflammation
Obesity constitutes a chronic, low-grade systemic inflammatory state characterized by increased levels of cytokines known to potentiate tumor development and growth [18, 69, 72]. Local in-breast inflammation of WAT produces pro-inflammatory mediators (TNFα, IL-1β, IL-6) and increases expression of aromatase within breast adipocytes [39, 73]. In response to infiltration by activated macrophages, visceral WAT secretes inflammatory cytokines that stimulate gluconeogenesis in the liver leading to increased serum glucose levels and subsequent increased pancreatic insulin secretion that further contribute to development of insulin resistance [59]. This microenvironment establishes a positive feedback loop, whereby stromal fat cells secrete adipokines, which attract macrophages that once activated further secrete pro-inflammatory cytokines (IL-1B, IL-6, TNF-a) that ultimately contribute to insulin resistance and breast cancer development [41].
Obesity Effects on Adipocyte–Macrophage Interaction
Obesity has been associated with adipocyte hypertrophy in mammary tissue [74•], which provides evidence for a causal relationship between obesity, inflammation of WAT in breast tissue, and tumor development [74]. Adipose tissue is metabolically and immunologically active and has the ability to transdifferentiate in vivo [75]. As fat mass increases and adipocytes hypertrophy, cell wall stretch results in release of pro-inflammatory cytokines and increased lipolysis with release of free fatty acids. Within WAT, the activated macrophage acts as key mediator in inflammation. Macrophages are able to infiltrate tumors and amplify the pro-inflammatory tumorigenic milieu through production of cytokines, prostaglandins, and angiogenic factors [69, 76]. Histologically, this has been observed by the formation of crown-like structures (CLS) that represent macrophages surrounding dead adipocytes. CLS are observed in subcutaneous and visceral fat of patients with metabolic syndrome [77] and have been found in mammary tissue of obese mice and WAT of human breast [74, 78]. Adipocyte cell death—represented by CLS—leads to release of free fatty acids that further stimulate the inflammatory response via toll-like receptor-4, increased cytokines (IL-1B, IL-6, TNF-α, PGE-2), and NF-kB signaling. NF-kB upregulates cell proliferation, apoptosis, inflammation, metastasis, and angiogenesis; additionally, it is associated with insulin resistance, increased aromatase activity, and is implicated in many cancers [39, 49].
Obesity Effects on Tumor Microenvironment
As detailed above, the tumor microenvironment in obese patients is characterized by elevated growth factors and pro-inflammatory mediators, including fatty acids, inflammatory cytokines, and influx of immune cells [18, 69, 72]. Beyond these mechanisms, the tumor microenvironment and interaction between tumor cells with stroma, soluble factors, signaling molecules, and the extracellular matrix can all promote tumorigenesis and impact response to treatment. Similar to immune cell function in wound healing, inflammation is involved in tissue remodeling and angiogenesis in tumors [79]. The pro-inflammatory milieu enables tumor cells to hijack the proliferative state and utilize it for tumor growth, invasion, and metastasis [80, 81].
Elevations in circulating pro-inflammatory mediators are associated with poor prognosis in obese breast cancer patients [82, 83]. Driven by stromal components, chemokines, cytokines, and growth factors, the tumor microenvironment has been postulated to have at least three different effects on tumor phenotype and presentation, including (1) increased genetic instability of tumor cells, (2) regulation of gene expression via induction of signaling cascades in tumor cells, and (3) exerting selective pressure on cells [84]. This implies that tumor phenotype involves complex interplay between cancer cells and surrounding host stromal cells. Thus, the microenvironment and locally secreted adipokines are capable of influencing mammary epithelial cell growth and differentiation [85].
Obesity Effects on Estrogen Homeostasis and Aromatase Signaling
The link between body weight and estrogen is well documented; with increasing body fat, there are significant increases in circulating estrogens, especially among postmenopausal women [86]. In premenopausal women, ovarian production of estrogens drives serum levels and the effect of peripheral androgen conversion to estrogen does not significantly alter the overall serum concentration of estrogen; as such, estradiol levels are similar in obese and lean premenopausal women. This relationship is complicated in obese premenopausal women; increased adiposity and metabolic dysfunction can contribute to anovulatory cycles that may lead to decreased estrogen exposure.
After menopause, peripheral adipocyte synthesis of estrogens takes over for ovarian hormone biosynthesis. Adipocytes produce aromatase—a cytochrome P450 enzyme encoded by the CYP19 gene—that is responsible for greater estrogen biosynthesis and upregulation of progesterone receptor, an ER target gene [74, 82, 83]. Significantly, activation of specific promoters by elevated pro-inflammatory cytokines in breast tissue leads to increased transcription of CYP19 [87]. Aromatase in adipose and breast tissue is responsible for the conversion of circulating androgens originating from the adrenal cortex and postmenopausal ovary into estrogens [88]. Consequently, increased fat mass impacts both serum estrogen concentration and locally secreted estrogen levels in breast tumors. Circulating estrogens support proliferation of breast epithelial cells and greater aromatase activity raises the risk of hormone receptor positive breast cancer in postmenopausal women [89]. Aromatase is mediated in an autocrine/paracrine manner by adipocyte production of inflammatory mediators like IL-6 and TNF-a, forming a positive feedback loop that increases estrogen synthesis [90].
Weight Loss Interventions as a Potentially Cost Effective Strategy to Reduce Breast Cancer Risk and Improve Outcomes—A “Low Hanging” Fruit?
Obesity is one of the known modifiable risk factors for breast cancer that can impact prognosis in newly diagnosed patients. Lifestyle modification guidelines have been identified to help individuals with weight control and cancer prevention. Weight reduction in postmenopausal women decreases circulating estrogen levels and increases serum sex-hormone binding globulins.
The obese state is signified by both increased size of pre-existing fat mass and synthesis of new adipocytes via de novo cell differentiation (hypertrophy and hyperplasia, respectively) [91]. It is now appreciated, that adipocytes are not merely fat repositories, but also act as an endocrine organ by secreting bioactive molecules called adipokines (i.e., adiponectin and leptin) that act in an autocrine, paracrine, and endocrine fashion [92] Obese individuals typically have increased circulating levels of insulin, IGF-1, leptin, and inflammatory cytokines [93, 94]. It is well established that obesity is associated with metabolic syndrome, chronic inflammation, diabetes, and cardiovascular disease. The prevalence of metabolic syndrome (insulin resistance, hypertension, hypertriglyceridemia, low HDL, and central obesity [95]) is estimated at 34 % of the adult population in the US and largely correlates with obese individuals. Metabolic syndrome is now known to impact growth signaling, inflammatory processes, vascular integrity, and hormonal signaling that is associated with cancer development, recurrence, and prognosis [96•, 97, 98].
In a study by Eliassen et al., history of weight change in adulthood among postmenopausal women was associated with increased risk of breast cancer (p < 0.001); women who had gained 25 kg by menopause had an increased risk (RR 1.45, 95 % CI 1.27–1.66) compared to those who maintained a stable weight. Weight gain after menopause of 10 kg was associated with increased risk of breast cancer (RR 1.18, 95 % CI 1.03–1.35) compared to those who maintained a healthy weight [23]. Significantly, weight gain after breast cancer treatment is associated with worse outcomes regardless of menopausal status [99]. In the same study, weight loss of 10 kg or more after menopause was associated with a suggested decreased risk of breast cancer (RR 0.77, 95 % CI 0.56–1.08). Weight loss—by diet or exercise—has been associated with normalization of inflammatory markers and adipokines [100–102]. Further, exercise with or without change in weight, has been shown to have beneficial effects on inflammation and insulin sensitivity [101, 103].
There are a number of ways to combat obesity, the most common being via physical activity and nutrition. It has been shown that habitual physical activity among postmenopausal women can reduce breast cancer occurrence by up to 25 % [104]. A significantly lower risk of recurrence and an improved overall survival among breast cancer patients is observed in those who engage in aerobic exercise equal to 9 metabolic equivalent-hours (MET-h) for 120–180 min per week compared to less active women [105, 106]. The mitigating effects of exercise are thought to be via pathways affecting insulin sensitivity, anti-inflammatory mechanisms, and improvements in visceral adipose stores [38, 107]. Levels of circulating estrogens are also influenced by physical activity, with higher levels of activity leading to decreases in serum estrogen concentrations [40].
Several mechanisms have been identified as potential mediators of exercise on cancer development. These include alterations in cell proliferation, apoptosis, circulating sex hormone levels, decreased IGF-1 concentration, increased insulin sensitivity, and changes in bodyweight and composition [108]. Exercise may garner its protective effects by tempering the synthesis of mitogenic pro-inflammatory cytokines, hormones, and growth factors. Further studies are needed to identify which factors have more impact on carcinogenesis.
Physical activity and dietary habits have both been correlated with breast cancer survival, possibly via regulation of circulating sex hormone concentrations. Fortunately, weight reduction via dietary changes with caloric restriction or through bariatric surgery has been shown to result in decreased circulating estrogens. Fat loss with reduction in aromatase-derived estrogen can impact ER + breast tumor growth. Supporting this idea, a recent study found that breast cancer incidence was decreased by 85 % status post gastric bypass surgery [109].
Epidemiologic studies report that only half of breast cancer survivors meet recommendations for activity or servings of fruits and vegetables. For cancer survivors aged 70–90 years old, the European Healthy Aging study reported a 60 % reduction in disease-specific and all-cause mortality among participants that adhered to a Mediterranean diet, were physically active, and did not use tobacco [110]. Pierce et al. described an increase in 10-year survival rate among breast cancer survivors who engaged in weekly physical activity (30 min of walking, 6 days per week) and whose diet included at least 5 servings of fruits and vegetables daily. Further, these two practices were associated with a 50 % reduction in mortality during the subsequent follow-up period; however, the mortality benefit was only observed in women who engaged in both lifestyle modifications, implying a synergistic protective effect of diet, and activity modifications for overall breast cancer survival [111].
Finally, for women in whom medical weight loss strategy has failed, surgical weight loss strategy may be of benefit. However, very few studies have addressed the role of weight loss surgery in mitigating breast cancer risk and improving breast cancer outcome.
Conclusions
Abundant data are now available to clarify the relationship between obesity and breast cancer as not merely due to fatness or increased BMI. It is now widely accepted that the obese state creates a hostile environment that is associated with a chronic systemic inflammatory state, metabolic syndrome, and altered production of estrogens and adipokines. The mitogenic milieu created by obesity supports breast tumor growth through increased circulating estrogens, hyperinsulinemia and insulin resistance, elevated insulin-like growth factor 1 (IGF-a) activity, inflammatory cytokine secretion, adipokine overproduction, and imbalance due to excess adipocytes. As such, it is reasonable to focus on each of these pathways as possible areas to manipulate the physiological response to fatness and develop interventions to prevent and treat breast cancer.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;. doi:10.1093/jnci/dju055.
DeSantis CE, Fedewa SA, Goding Sauer A, et al. Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin. 2016;66:31–42. doi:10.3322/caac.21320.
McPherson K, Steel CM, Dixon JM. ABC of breast diseases. Breast cancer-epidemiology, risk factors, and genetics. BMJ. 2000;321:624–8.
Ahn J, Schatzkin A, Lacey JV, et al. Adiposity, adult weight change, and postmenopausal breast cancer risk. Arch Intern Med. 2007;167:2091–102. doi:10.1001/archinte.167.19.2091.
Maehle BO, Tretli S, Skjaerven R, Thorsen T. Premorbid body weight and its relations to primary tumour diameter in breast cancer patients; its dependence on estrogen and progesteron receptor status. Breast Cancer Res Treat. 2001;68:159–69.
Rose DP, Komninou D, Stephenson GD. Obesity, adipocytokines, and insulin resistance in breast cancer. Obes Rev. 2004;5:153–65. doi:10.1111/j.1467-789X.2004.00142.x.
Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med. 2009;361:2252–60. doi:10.1056/NEJMsa0900459.
Lovegrove JA. Obesity, body fat distribution and breast cancer. Nutr Res Rev. 2002;15:389–412. doi:10.1079/NRR200245.
White AJ, Nichols HB, Bradshaw PT, Sandler DP. Overall and central adiposity and breast cancer risk in the Sister Study. Cancer. 2015;121:3700–8. doi:10.1002/cncr.29552.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–7.
Ogden CL, Carroll MD, Flegal KM. Prevalence of obesity in the United States. JAMA. 2014;312(2):189–90.
Han TS, van Leer EM, Seidell JC, Lean ME. Waist circumference action levels in the identification of cardiovascular risk factors: prevalence study in a random sample. BMJ. 1995;311:1401–5.
••Goodwin PJ, Stambolic V. Impact of the obesity epidemic on cancer. Annu Rev Med. 2015;66:281–96. Thorough review of the relationship between the obesity epidemic and cancer incidence. Review covers biological plausibility of obesity as a driver and disease modifier of cancer.
Tchernof A, Després JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359–404. doi:10.1152/physrev.00033.2011.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285:2486–97.
Wolin KY, Carson K, Colditz GA. Obesity and cancer. Oncologist. 2010;15:556–65. doi:10.1634/theoncologist.2009-0285.
••Renehan AG, Tyson M, Egger M, et al. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008;371:569–78. doi: 10.1016/S0140-6736(08)60269-X This article provides an in-depth report of the epidemiological association between obesity and cancer. Explores biological mechanisms that link obesity with cancer.
van Kruijsdijk RCM, van der Wall E, Visseren FLJ. Obesity and cancer: the role of dysfunctional adipose tissue. Cancer Epidemiol Biomark Prev. 2009;18:2569–78. doi:10.1158/1055-9965.EPI-09-0372.
Huang Z, Hankinson SE, Colditz GA, et al. Dual effects of weight and weight gain on breast cancer risk. JAMA. 1997;278:1407–11.
Morimoto LM, White E, Chen Z, et al. Obesity, body size, and risk of postmenopausal breast cancer: the Women’s Health Initiative (United States). Cancer Causes Control. 2002;13(8):741–51.
Sellers TA, Kushi LH, Potter JD, et al. Effect of family history, body-fat distribution, and reproductive factors on the risk of postmenopausal breast cancer. N Engl J Med. 1992;326:1323–9. doi:10.1056/NEJM199205143262004.
Stephenson GD, Rose DP. Breast cancer and obesity: an update. Nutr Cancer. 2003;45:1–16. doi:10.1207/S15327914NC4501_1.
Eliassen AH, Colditz GA, Rosner B, et al. Adult weight change and risk of postmenopausal breast cancer. JAMA. 2006;296(2):193–201. doi:10.1001/jama/296.2.193.
Santen RJ, Boyd NF, Chlebowski RT, et al. Critical assessment of new risk factors for breast cancer: considerations for development of an improved risk prediction model. Endocr Relat Cancer. 2007;14:169–87. doi:10.1677/ERC-06-0045.
Strong AL, Ohlstein JF, Biagas BA, et al. Leptin produced by obese adipose stromal/stem cells enhances proliferation and metastasis of estrogen receptor positive breast cancers. Breast Cancer Res. 2015;17:112. doi:10.1186/s13058-015-0622-z.
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–38. doi:10.1056/NEJMoa021423.
Haakinson DJ, Leeds SG, Dueck AC, et al. The impact of obesity on breast cancer: a retrospective review. Ann Surg Oncol. 2012;19:3012–8. doi:10.1245/s10434-012-2320-8.
Cleveland RJ, Eng SM, Abrahamson PE, et al. Weight gain prior to diagnosis and survival from breast cancer. Cancer Epidemiol Biomark Prev. 2007;16:1803–11. doi:10.1158/1055-9965.EPI-06-0889.
Feigelson HS, Patel AV, Teras LR, et al. Adult weight gain and histopathologic characteristics of breast cancer among postmenopausal women. Cancer. 2006;107:12–21. doi:10.1002/cncr.21965.
Dal Maso L, Zucchetto A, Talamini R, et al. Effect of obesity and other lifestyle factors on mortality in women with breast cancer. Int J Cancer. 2008;123:2188–94. doi:10.1002/ijc.23747.
Reeves KW, Faulkner K, Modugno F, et al. Body mass index and mortality among older breast cancer survivors in the study of osteoporotic fractures. Cancer Epidemiol Biomark Prev. 2007;16:1468–73. doi:10.1158/1055-9965.EPI-07-0051.
Senie RT, Rosen PP, Rhodes P, et al. Obesity at diagnosis of breast carcinoma influences duration of disease-free survival. Ann Intern Med. 1992;116:26–32.
Majed B, Moreau T, Senouci K, et al. Is obesity an independent prognosis factor in woman breast cancer? Breast Cancer Res Treat. 2008;111:329–42. doi:10.1007/s10549-007-9785-3.
Chlebowski RT, Aiello E. Weight loss in breast cancer patient management. J Clin Oncol. 2002;20(4):1128–43.
Protani M, Coory M, Martin JH. Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat. 2010;123:627–35. doi:10.1007/s10549-010-0990-0.
•Berger NA. Obesity and cancer pathogenesis. Ann N Y Acad Sci. 2014;1311:57–76. doi:10.1111/nyas.12416.
Del Fabbro E, Parsons H, Warneke CL, et al. The relationship between body composition and response to neoadjuvant chemotherapy in women with operable breast cancer. Oncologist. 2012;17:1240–5. doi:10.1634/theoncologist.2012-0169.
McTiernan A, Rajan KB, Tworoger SS, et al. Adiposity and sex hormones in postmenopausal breast cancer survivors. J Clin Oncol. 2003;21:1961–6. doi:10.1200/JCO.2003.07.057.
•Iyengar NM, Hudis CA, Dannenberg AJ. Obesity and inflammation: new insights into breast cancer development and progression. Am Soc Clin Oncol Educ Book 2013. p. 46–51. doi: 10.1200/EdBook_AM.2013.33.46 Description of mechanistic relationship between obesity related inflammation and breast cancer progression.
Lorincz AM, Sukumar S. Molecular links between obesity and breast cancer. Endocr Relat Cancer. 2006;13:279–92. doi:10.1677/erc.1.00729.
Vona-Davis L, Rose DP. Adipokines as endocrine, paracrine, and autocrine factors in breast cancer risk and progression. Endocr Relat Cancer. 2007;14:189–206. doi:10.1677/ERC-06-0068.
Schäffler A, Schölmerich J, Buechler C. Mechanisms of disease: adipokines and breast cancer - endocrine and paracrine mechanisms that connect adiposity and breast cancer. Nat Clin Pract Endocrinol Metab. 2007;3:345–54. doi:10.1038/ncpendmet0456.
Bulun SE, Chen D, Moy I, et al. Aromatase, breast cancer and obesity: a complex interaction. Trends Endocrinol Metab. 2012;23:83–9. doi:10.1016/j.tem.2011.10.003.
Braun S, Bitton-Worms K, LeRoith D. The link between the metabolic syndrome and cancer. Int J Biol Sci. 2011;7:1003–15.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6. doi:10.1038/nature05482.
Kaaks R. Nutrition, hormones, and breast cancer: is insulin the missing link? Cancer Causes Control. 1996;7:605–25.
Goodwin PJ, Ennis M, Pritchard KI, et al. Fasting insulin and outcome in early-stage breast cancer: results of a prospective cohort study. J Clin Oncol. 2002;20:42–51.
Pollak MN, Schernhammer ES. Insulin-like growth factors and neoplasia. Nat Rev Cancer. 2004;4:505–18. doi:10.1038/nrc1387.
Renehan AG, Roberts DL, Dive C. Obesity and cancer: pathophysiological and biological mechanisms. Arch Physiol Biochem. 2008;114:71–83. doi:10.1080/13813450801954303.
Moore T, Beltran L, Carbajal S, et al. Dietary energy balance modulates signaling through the Akt/mammalian target of rapamycin pathways in multiple epithelial tissues. Cancer Prev Res (Phila). 2008;1:65–76. doi:10.1158/1940-6207.CAPR-08-0022.
Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008;8:915–28. doi:10.1038/nrc2536.
Hursting SD, Smith SM, Lashinger LM, et al. Calories and carcinogenesis: lessons learned from 30 years of calorie restriction research. Carcinogenesis. 2010;31:83–9. doi:10.1093/carcin/bgp280.
Hawsawi Y, El-Gendy R, Twelves C, et al. Insulin-like growth factor–oestradiol crosstalk and mammary gland tumourigenesis. Biochim Biophys Acta. 2013;1836:345–53. doi:10.1016/j.bbcan.2013.10.005.
Su B, Wong C, Hong Y, Chen S. Growth factor signaling enhances aromatase activity of breast cancer cells via post-transcriptional mechanisms. J Steroid Biochem Mol Biol. 2011;123:101–8. doi:10.1016/j.jsbmb.2010.11.012.
Surmacz E. Function of the IGF-I receptor in breast cancer. J Mammary Gland Biol Neoplas. 2000;5(1):95–105.
Le Roith D. Regulation of proliferation and apoptosis by the insulin-like growth factor I receptor. Growth Hormone IGF Res. 2000;10:S12–3.
Seccareccia E, Brodt P. The role of the insulin-like growth factor-I receptor in malignancy: an update. Growth Hormone IGF Res. 2012;22(6):193–9.
Stewart AJ, Johnson MD, May FE, Westley BR. Role of insulin-like growth factors and the type I insulin-like growth factor receptor in the estrogen-stimulated proliferation of human breast cancer cells. J Biol Chem. 1990;265:21172–8.
Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548–56. doi:10.1210/jc.2004-0395.
Gautron L, Elmquist JK. Sixteen years and counting: an update on leptin in energy balance. J Clin Invest. 2011;121:2087–93. doi:10.1172/JCI45888.
Catalano S, Marsico S, Giordano C, et al. Leptin enhances, via AP-1, expression of aromatase in the MCF-7 cell line. J Biol Chem. 2003;278:28668–76. doi:10.1074/jbc.M301695200.
Galic S, Oakhill JS, Steinberg GR. Adipose tissue as an endocrine organ. Mol Cell Endocrinol. 2010;316:129–39. doi:10.1016/j.mce.2009.08.018.
Tian YF, Chu CH, Wu MH, Chang CL. Anthropometric measures, plasma adiponectin, and breast cancer risk. Endocr Relat Cancer. 2007;14:669–77.
Mantzoros C, Petridou E, Dessypris N. Adiponectin and breast cancer risk. J Clin Endocr Metab. 2004;89(3):1102–7.
Vaiopoulos AG, Marinou K, Christodoulides C. The role of adiponectin in human vascular physiology. Int J Cardiol. 2012;155(2):188–93.
Barb D, Williams CJ, Neuwirth AK, Mantzoros CS. Adiponectin in relation to malignancies: a review of existing basic research and clinical evidence. Am J Clin Nutr. 2007;86:s858–66.
Stofkova A. Leptin and adiponectin: from energy and metabolic dysbalance to inflammation and autoimmunity. Endocr Regul. 2009;43:157–68.
Dalamaga M, Diakopoulos KN, Mantzoros CS. The role of adiponectin in cancer: a review of current evidence. Endocr Rev. 2012;33:547–94. doi:10.1210/er.2011-1015.
Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol. 2010;72:219–46. doi:10.1146/annurev-physiol-021909-135846.
O’Rourke RW. Inflammation in obesity-related disease. Surgery. 2009;145(3):255–9.
Karin M. Nuclear factor-κB in cancer development and progression. Nature. 2006;441:431–6. doi:10.1038/nature04870.
Pierce BL, Ballard-Barbash R, Bernstein L, et al. Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J Clin Oncol. 2009;27:3437–44. doi:10.1200/JCO.2008.18.9068.
Osborn O, Olefsky JM. The cellular and signaling networks linking the immune system and metabolism in disease. Nat Med. 2012;18:363–74. doi:10.1038/nm.2627.
•Morris PG, Hudis CA, Giri D, Morrow M. Inflammation and increased aromatase expression occur in the breast tissue of obese women with breast cancer. Cancer Prev Res. 2011;4:1021–9. Description of in-breast inflammation underscoring how obesity-related inflammation promotes development of cancer, especially in mammary tissue.
Charrière G, Cousin B, Arnaud E, André M. Preadipocyte conversion to macrophage Evidence of plasticity. J Biol Chem. 2003;278:9850–5.
Allavena P, Sica A, Garlanda C. The Yin-Yang of tumor-associated macrophages in neoplastic progression and immune surveillance. Immunol Rev. 2008;222:155–61.
Cinti S, Mitchell G, Barbatelli G, et al. Adipocyte death defines macrophage localization and function in adipose tissue of obese mice and humans. J Lipid Res. 2005;46:2347–55. doi:10.1194/jlr.M500294-JLR200.
Subbaramaiah K, Howe LR, Bhardwaj P, et al. Obesity is associated with inflammation and elevated aromatase expression in the mouse mammary gland. Cancer Prev Res (Phila). 2011;4:329–46. doi:10.1158/1940-6207.CAPR-10-0381.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–44. doi:10.1038/nature07205.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7. doi:10.1038/nature01322.
Balkwill F, Charles KA, Mantovani A. Smoldering and polarized inflammation in the initiation and promotion of malignant disease. Cancer Cell. 2005;7:211–7. doi:10.1016/j.ccr.2005.02.013.
Bachelot T, Ray-Coquard I, Menetrier-Caux C. Prognostic value of serum levels of interleukin 6 and of serum and plasma levels of vascular endothelial growth factor in hormone-refractory metastatic breast cancer patients. Br J Cancer. 2003;88:1721–6.
Dandona P, Weinstock R, Thusu K, et al. Tumor necrosis factor-alpha in sera of obese patients: fall with weight loss. J Clin Endocrinol Metab. 1998;83:2907–10. doi:10.1210/jcem.83.8.5026.
Korkaya H, Liu S, Wicha MS. Breast cancer stem cells, cytokine networks, and the tumor microenvironment. J Clin Invest. 2011;121:3804–9. doi:10.1172/JCI57099.
Andò S, Catalano S. The multifactorial role of leptin in driving the breast cancer microenvironment. Nat Rev Endocrinol. 2012;8:263–75. doi:10.1038/nrendo.2011.184.
Madigan MP, Troisi R, Potischman N, et al. Serum hormone levels in relation to reproductive and lifestyle factors in postmenopausal women (United States). Cancer Causes Control. 1998;9:199–207.
Zhao Y, Agarwal VR, Mendelson CR, Simpson ER. Estrogen biosynthesis proximal to a breast tumor is stimulated by PGE2 via cyclic AMP, leading to activation of promoter II of the CYP19 (aromatase) gene. Endocrinology. 1996;137:5739–42. doi:10.1210/endo.137.12.8940410.
Judd HL, Judd GE, Lucas WE. Endocrine function of the postmenopausal ovary: concentration of androgens and estrogens in ovarian and peripheral vein blood. J Clin Endocr Metab. 1974;39(6):1020–4.
Cleary MP, Grossmann ME. Obesity and breast cancer: the estrogen connection. Endocrinology. 2009;150(6):2537–42.
Purohit A, Newman SP, Reed MJ. The role of cytokines in regulating estrogen synthesis: implications for the etiology of breast cancer. Breast Cancer Res. 2002;4:65–9.
Mauro L, Naimo GD, Ricchio E, Panno ML. Cross-talk between adiponectin and IGF-IR in breast cancer. Front Oncol. 2015;5:157.
Surmacz E. Leptin and adiponectin: emerging therapeutic targets in breast cancer. J Mammary Gland Biol Neoplas. 2013;18(3):321–32.
Hursting SD, Berger NA. Energy balance, host-related factors, and cancer progression. J Clin Oncol. 2010;28:4058–65. doi:10.1200/JCO.2010.27.9935.
Carter JC, Church FC. Obesity and breast cancer: the roles of peroxisome proliferator-Activated receptor-and plasminogen activator inhibitor-1. PPAR Res. 2009;4:1–13.
Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Report; 2009. p. 1–7.
•Hursting SD, Dunlap SM. Obesity, metabolic dysregulation, and cancer: a growing concern and an inflammatory (and microenvironmental) issue. Ann N Y Acad Sci. 2012;1271:82–7. doi: 10.1111/j.1749-6632.2012.06737.x Extensive review on metabolic and inflammatory change associated with increased adiposity and its role in cancer development.
Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss. Arterioscler Thromb Vasc Biol. 2006;26:968–76. doi:10.1161/01.ATV.0000216787.85457.f3.
Dunlap SM, Chiao LJ, Nogueira L, et al. Obesity enhances epithelial-to-mesenchymal transition and tumor progression in murine claudin-low and basal-like mammary tumor models. Cancer Prev Res. 2012;5:930–42.
Thivat E, Thérondel S, Lapirot O, et al. Weight change during chemotherapy changes the prognosis in non metastatic breast cancer for the worse. BMC Cancer. 2010;10:648. doi:10.1186/1471-2407-10-648.
Byers T, Sedjo RL. Does intentional weight loss reduce cancer risk? Diabetes Obes Metab. 2011;13(12):1063–72.
Friedenreich CM, Neilson HK, Lynch BM. State of the epidemiological evidence on physical activity and cancer prevention. Eur J Cancer. 2010;46:2593–604. doi:10.1016/j.ejca.2010.07.028.
van Gemert WA, May AM, Schuit AJ, et al. Effect of weight loss with or without exercise on inflammatory markers and adipokines in postmenopausal women: the SHAPE-2 trial A Randomized Controlled Trial. Cancer Epidemiol Biomark Prev. 2016;. doi:10.1158/1055-9965.EPI-15-1065.
King B, Jiang Y, Su X, et al. Weight control, endocrine hormones and cancer prevention. Exp Biol Med (Maywood). 2013;238:502–8. doi:10.1177/1535370213480695.
Lynch BM, Neilson HK, Friedenreich CM. Physical activity and breast cancer prevention. Physl Activity Cancer. 2010;186:13–42.
Holmes MD, Chen WY, Feskanich D, Kroenke CH. Physical activity and survival after breast cancer diagnosis. JAMA. 2005;293(20):2479–86. doi:10.1001/jama.293.20.2479.
Irwin ML, McTiernan A, Manson J. Physical activity and survival in postmenopausal women with breast cancer: results from the women’s health initiative. Cancer Prev Res. 2011;4(4):522–9.
Neilson HK, Friedenreich CM, Brockton NT, Millikan RC. Physical activity and postmenopausal breast cancer: proposed biologic mechanisms and areas for future research. Cancer Epidemiol Biomark Prev. 2009;18:11–27. doi:10.1158/1055-9965.EPI-08-0756.
Rogers CJ, Colbert LH, Greiner JW, et al. Physical activity and cancer prevention: pathways and targets for intervention. Sports Med. 2008;38:271–96.
Christou NV, Lieberman M, Sampalis F, Sampalis JS. Bariatric surgery reduces cancer risk in morbidly obese patients. Surg Obes Relat Dis. 2008;4:691–5. doi:10.1016/j.soard.2008.08.025.
Knoops KTB, de Groot LCPGM, Kromhout D, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292:1433–9. doi:10.1001/jama.292.12.1433.
Pierce JP, Stefanick ML, Flatt SW, et al. Greater survival after breast cancer in physically active women with high vegetable-fruit intake regardless of obesity. J Clin Oncol. 2007;25:2345–51. doi:10.1200/JCO.2006.08.6819.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical collection on Breast Cancer Surgery.
Rights and permissions
About this article
Cite this article
Gershuni, V.M., Ahima, R.S. & Tchou, J. Obesity and Breast Cancer: A Complex Relationship. Curr Surg Rep 4, 14 (2016). https://doi.org/10.1007/s40137-016-0134-5
Published:
DOI: https://doi.org/10.1007/s40137-016-0134-5