Abstract
Breast cancer is the most commonly diagnosed invasive malignancy and the second leading cause of cancer death in women. This chapter considers epidemiologic evidence regarding the association between physical activity and breast cancer risk from 73 studies conducted around the world. Across these studies there was a 25% average risk reduction amongst physically active women as compared to the least active women. The associations were strongest for recreational activity, for activity sustained over the lifetime or done after menopause, and for activity that is of moderate to vigorous intensity and performed regularly. There is also some evidence for a stronger effect of physical activity amongst postmenopausal women, women who are normal weight, have no family history of breast cancer, and are parous. It is likely that physical activity is associated with decreased breast cancer risk via multiple interrelated biologic pathways that may involve adiposity, sex hormones, insulin resistance, adipokines, and chronic inflammation. Future research should include prospective observational epidemiologic studies relating proposed biomarkers to breast cancer risk and also randomized controlled trials to examine how physical activity influences the proposed biomarkers. Exercise trials will provide more clarity regarding the appropriate type, dose, and timing of activity that relate to breast cancer risk reduction.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Physical inactivity is one of the few established breast cancer risk factors amenable to intervention. Over 90 studies conducted worldwide have investigated some aspect of this association. In this chapter, we review the epidemiologic literature on physical activity and breast cancer risk, examining the effect of the different parameters of activity and effect modification within different population subgroups. We also review the biologic mechanisms whereby physical activity may influence the risk of breast cancer.
2 Epidemiologic Evidence
2.1 Background
Breast cancer is the most common invasive malignancy diagnosed in women, with 1,151,298 new cases estimated worldwide in 2002 (Ferlay et al. 2004). Female breast cancer represents 27% of all new female cancers in developed countries: estimates project 192,370 new cases in the U.S. and 22,700 cases in Canada in 2009 (Canadian Cancer Society 2009; Jemal et al. 2009). The lifetime risk of a woman being diagnosed with breast cancer is approximately one in eight in the United States (Jemal et al. 2009), and slightly lower in other developed countries (Australian Institute of Health and Welfare and National Breast and Ovarian Cancer Centre 2009; Canadian Cancer Society 2009; Cancer Research UK 2009).
Worldwide, breast cancer is the most common cause of cancer death among women; the number of estimated deaths in 2002 was 410,712 (Ferlay et al. 2004). In developed countries breast cancer is often the second leading cause of cancer death in women, following lung cancer (Canadian Cancer Society 2009; Jemal et al. 2009; Office for National Statistics 2008). A total of 40,170 and 5,400 breast cancer deaths are projected to occur in the U.S. and Canada, respectively, in 2009 (Canadian Cancer Society 2009; Jemal et al. 2009). However, 5-year relative survival is high, approaching 90% in developed countries (Australian Institute of Health and Welfare and National Breast and Ovarian Cancer Centre 2009; Canadian Cancer Society 2009; Jemal et al. 2009; Office for National Statistics 2008).
Most of the established risk factors for breast cancer are not easily modifiable. These include: age, race, a family history of breast cancer, genetic susceptibility, benign breast disease, early age at menarche, late age at menopause, and nulliparity (Bernstein 2009; Monninkhof et al. 2007a). Physical inactivity is one of the few behavioral risk factors amenable to change, and as such represents an opportunity to reduce the burden of disease from breast cancer.
There have been a number of reviews and reports written on the topic of physical activity and breast cancer prevention. These have generally concluded that the evidence supporting this association is convincing (Friedenreich and Cust 2008; Friedenreich and Orenstein 2002; IARC Working Group 2002; Monninkhof et al. 2007a); however the World Cancer Research Fund was more cautious, labeling the association probable (World Cancer Research Fund and the American Institute for Cancer Research 2007).
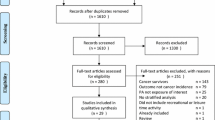
This chapter updates the review of physical activity and breast cancer risk provided by Friedenreich and Cust (2008). Here, we have incorporated the epidemiologic literature published to December 2009: 33 cohort studies and 40 case-control studies. Where multiple publications from the same study were found, the most recent publication (cohort studies), or the original publication (case-control studies), was selected for inclusion in our main results. We defined study results as null if the odds or hazard ratios fell between 0.9 and 1.1, inclusive. If the upper limit of the 95% confidence intervals (95% CI) was less than 1.05, we considered the results to be of borderline statistical significance.
2.2 Overall Associations Between Physical Activity and Breast Cancer Risk
Twenty-nine of the 73 studies reviewed (40%) found a statistically significant risk reduction for breast cancer when comparing the highest versus lowest level of physical activity (Bernstein et al. 2005; Breslow et al. 2001; Carpenter et al. 2003; Calle et al. 1998; Dallal et al. 2007; Dirx et al. 2001; Fraser and Shavlik 1997; Friedenreich et al. 2001; Kruk 2007a, b; Kruk and Aboul-Enein 2003; Levi et al. 1999; Mathew et al. 2009; Matthews et al. 2001; Mezzetti et al. 1998; Moradi et al. 2000; Peplonska et al. 2008; Peters et al. 2009a; Rintala et al. 2002; Rockhill et al. 1999; Sesso et al. 1998; Shoff et al. 2000; Suzuki et al. 2008; Thune et al. 1997; Ueji et al. 1998; Verloop et al. 2000; Wyrwich and Wolinsky 2000; Wyshak and Frisch 2000; Yang et al. 2003). An additional eight studies (11%) had a borderline, statistically significant breast cancer risk reduction (Hirose et al. 2003; John et al. 2003; Lee et al. 2001b; Leitzmann et al. 2008; Maruti et al. 2008; McTiernan et al. 1996; McTiernan et al. 2003; Patel et al. 2003), and 14 (19%) observed a statistically nonsignificant reduction (Adams-Campbell et al. 2001; Chang et al. 2006; Dey et al. 2009; Dorn et al. 2003; Dosemeci et al. 1993; Friedenreich and Rohan 1995; Gilliland et al. 2001; Hu et al. 1997; Marcus et al. 1999; Moradi et al. 2002; Rintala et al. 2003; Shin et al. 2009; Slattery et al. 2007; Sprague et al. 2007). Nineteen (26%) studies produced null effects (Bardia et al. 2006; Calle et al. 1998; Chen et al. 1997; Colditz et al. 2003; Coogan and Aschengrau 1999; Gammon et al. 1998; Gao et al. 2009; Howard et al. 2009; Lahmann et al. 2007; Lee et al. 2001a; Luoto et al. 2000; Magnusson et al. 2005; Mertens et al. 2006; Nkondjock et al. 2006; Schmidt et al. 2008; Silvera et al. 2006; Steindorf et al. 2003; Taioli et al. 1995; Tehard et al. 2006), and three (4%) studies observed a statistically nonsignificant increased risk of breast cancer among the most physically active women (Dorgan et al. 1994; Margolis et al. 2005; Schnohr et al. 2005). Statistically significant risk reductions were reported as frequently in the case-control studies (16 studies from a total of 40; 40%) as in the cohort studies (13 from 33; 39%) (Figs. 2.1 and 2.2). Across all studies there was a 25% average risk reduction, with a stronger effect found in the case-control studies (an average risk reduction of 30%) than in the cohort studies (a 20% risk reduction). Of the 51 studies that found a decreased risk of breast cancer with increased levels of physical activity, 41 examined the trend of this relationship (Adams-Campbell et al. 2001; Bernstein et al. 2005; Breslow et al. 2001; Carpenter et al. 2003; Cerhan et al. 1998; Chang et al. 2006; Dallal et al. 2007; Dey et al. 2009; Dirx et al. 2001; Dorn et al. 2003; Dosemeci et al. 1993; Friedenreich et al. 2001; Friedenreich and Rohan 1995; Gilliland et al. 2001; Hirose et al. 2003; Hu et al. 1997; Kruk 2007a; b; Lee et al. 2001b; Leitzmann et al. 2008; Levi et al. 1999; Marcus et al. 1999; Maruti et al. 2008; Mathew et al. 2009; Matthews et al. 2001; McTiernan et al. 1996, 2003; Mezzetti et al. 1998; Moradi et al. 2000, 2002; Patel et al. 2003; Peplonska et al. 2008; Rockhill et al. 1999; Sesso et al. 1998; Shin et al. 2009; Shoff et al. 2000; Slattery et al. 2007; Sprague et al. 2007; Thune et al. 1997; Ueji et al. 1998; Yang et al. 2003). Thirty-three of these studies found evidence for a dose–response relation between increasing levels of physical activity and decreasing breast cancer risks (Adams-Campbell et al. 2001; Bernstein et al. 2005; Breslow et al. 2001; Carpenter et al. 2003; Cerhan et al. 1998; Dallal et al. 2007; Dey et al. 2009; Dirx et al. 2001; Friedenreich et al. 2001; Gilliland et al. 2001; Kruk 2007a; b; Lee et al. 2001b; Levi et al. 1999; Maruti et al. 2008; Mathew et al. 2009; Matthews et al. 2001; McTiernan et al. 1996, 2003; Mezzetti et al. 1998; Moradi et al. 2000, 2002; Patel et al. 2003; Peplonska et al. 2008; Rockhill et al. 1999; Sesso et al. 1998; Shin et al. 2009; Shoff et al. 2000; Slattery et al. 2007; Sprague et al. 2007; Thune et al. 1997; Ueji et al. 1998; Yang et al. 2003).
2.3 Type, Dose, and Timing of Activity
One of the difficulties inherent in reviewing the physical activity and breast cancer literature is the heterogeneity of methods used to assess physical activity. Some studies have utilized comprehensive assessments of lifetime physical activity, whereas others have used single-item measures. Hence, we examined specific parameters of physical activity (i.e. type, dose, timing) and their association with breast cancer risk, separately.
Figures 2.3, 2.4, and 2.5 present study outcomes by type of physical activity: occupational, recreational, walking/cycling, and household activity. The greatest breast cancer risk reductions were found for recreational and household activity (average 21%), followed by walking/cycling (18%), and occupational activity (13%).
Dose refers to the combination of frequency, duration, and intensity of the activity performed. Frequency describes how many times a particular physical activity is undertaken, while duration describes the amount of time physical activity is undertaken for. Intensity describes the level of exertion required to perform a particular physical activity, and is often categorized as light, moderate, or vigorous, according to energy expenditure.
Few studies reported frequency of physical activity, hence no figure is presented. Participation in moderate intensity physical activity was associated with an average decreased risk of 15%. A slightly greater risk reduction was found for vigorous intensity physical activity, 18% (Fig. 2.6). Similarly, greater decreases in breast cancer risk were observed with greater duration of activity (moderate-to-vigorous intensity or recreational activity) (Fig. 2.7). Hence, while participation in 2–3 h per week was associated with an average risk reduction of 9%, women who reported 6.5 h of activity per week or more had a decreased risk of 30%.
Studies also assessed physical activity performed during different periods of life: adolescence, early adulthood (20s), middle adulthood (30s/40s), and later adulthood (≥50 years) (Fig. 2.8). Although risk reductions were observed for physical activity performed at each age period, activity after age 50 seemed to have a slightly stronger effect than earlier periods of activity (an average risk reduction of 17%). The average decrease in breast cancer risk associated with physical activity performed during adolescence was 16%; during early adulthood it was 8%, and during middle adulthood it was 15%. Sixteen studies assessed physical activity over the adult lifetime and the average risk reduction was even greater at 27% (data not shown).
2.4 Population Subgroups
We also considered how the association between physical activity and breast cancer risk may vary between different population subgroups. There were sufficient data to examine effect modification by menopausal status, body mass index (BMI; weight/height2) race, family history of breast cancer, hormone receptor status, and parity.
A decrease in breast cancer risk was found for both pre- and postmenopausal women (Fig. 2.9); however, across all studies that reported on menopausal status, the average risk reduction was somewhat greater among postmenopausal women (31%) than among premenopausal women (27%). Twenty-five studies presented results stratified by menopausal status, i.e. both pre- and postmenopausal women in the same study population (Adams-Campbell et al. 2001; Dey et al. 2009; Dorn et al. 2003; Friedenreich et al. 2001; Friedenreich and Rohan 1995; Gammon et al. 1998; Gilliland et al. 2001; Hirose et al. 2003; Howard et al. 2009; Hu et al. 1997; John et al. 2003; Kruk 2007a, b; Lahmann et al. 2007; Mathew et al. 2009; Matthews et al. 2001; Mezzetti et al. 1998; Moradi et al. 1999; Shin et al. 2009; Silvera et al. 2006; Slattery et al. 2007; Suzuki et al. 2008; Thune et al. 1997; Ueji et al. 1998; Yang et al. 2003). Only three observed statistically significant decreases in breast cancer risk for both pre- and postmenopausal women (Kruk 2007a; Suzuki et al. 2008; Yang et al. 2003). From the 25 studies that examined breast cancer risk reductions of pre- and postmenopausal women separately, 13 studies found greater risk reductions among postmenopausal women (Adams-Campbell et al. 2001; Dey et al. 2009; Dorn et al. 2003; Friedenreich et al. 2001; Friedenreich and Rohan 1995; Gammon et al. 1998; Gilliland et al. 2001; Hirose et al. 2003; Howard et al. 2009; Hu et al. 1997; John et al. 2003; Kruk 2007a, b; Lahmann et al. 2007; Mathew et al. 2009; Matthews et al. 2001; Mezzetti et al. 1998; Moradi et al. 1999; Shin et al. 2009; Silvera et al. 2006; Slattery et al. 2007; Suzuki et al. 2008; Thune et al. 1997; Ueji et al. 1998; Yang et al. 2003), 11 studies found a stronger effect among premenopausal women (Dorn et al. 2003; Friedenreich and Rohan 1995; Hirose et al. 2003; John et al. 2003; Lahmann et al. 2007; Silvera et al. 2006; Slattery et al. 2007; Suzuki et al. 2008; Thune et al. 1997; Ueji et al. 1998; Yang et al. 2003), and one study found no difference by menopausal status (Shin et al. 2009). It is noteworthy, however, that of these 25 studies that stratified by menopausal status, 12 yielded statistically significant risk reductions in postmenopausal women, whereas for premenopausal women only three studies showed statistically significant risk reductions.
The second effect modifier, BMI, was examined in 22 studies (Breslow et al. 2001; Colditz et al. 2003; Dallal et al. 2007; Friedenreich et al. 2001; Gammon et al. 1998; Hirose et al. 2003; Kruk and Aboul-Enein 2003; Leitzmann et al. 2008; Luoto et al. 2000; Maruti et al. 2008; McTiernan et al. 2003; Moradi et al. 2002; Patel et al. 2003; Peplonska et al. 2008; Peters et al. 2009b; Schmidt et al. 2008; Sesso et al. 1998; Suzuki et al. 2008; Tehard et al. 2006; Thune et al. 1997; Verloop et al. 2000; Yang et al. 2003). Figure 2.10 presents the results of these studies categorized as low BMI (<22 kg/m2), medium BMI (22–25 kg/m2), high BMI (≥25 kg/m2), and very high BMI (≥30 kg/m2). Greater decreases in breast cancer risk for highest versus lowest categories of physical activity were observed among women with lower BMI. The average risk reduction for low BMI was 27%; for medium BMI breast cancer risk was decreased by 24%; for high BMI it decreased by 18%; and, among women with very high BMI, the average risk reduction was less than 1%.
Only four studies calculated risk estimates separately for different racial/ethnic groups within their samples (Bernstein et al. 2005; Gilliland et al. 2001; John et al. 2003; Slattery et al. 2007) (Fig. 2.11). However, most of the studies included in this review could be classified according to the main racial group of their sample. An effect of physical activity on breast cancer risk was observed across all racial groups. Each of the three studies that included black women found a reduced risk (on average a relative decrease of 41%) (Adams-Campbell et al. 2001; Bernstein et al. 2005; John et al. 2003), two of the three studies of Hispanic women observed a reduced risk (average 28%) (Gilliland et al. 2001; John et al. 2003), and a decreased risk was found in both studies of Indian women (average 38%) (Dey et al. 2009; Mathew et al. 2009) and in the eight studies that included Asian women (average 41%) (Gao et al. 2009; Hirose et al. 2003; Hu et al. 1997; Matthews et al. 2001; Shin et al. 2009; Suzuki et al. 2008; Ueji et al. 1998; Yang et al. 2003). The average risk reduction for white women was somewhat lower (20%) (Bardia et al. 2006; Bernstein et al. 2005; Chang et al. 2006; Chen et al. 1997; Coogan and Aschengrau 1999; Dallal et al. 2007; Dirx et al. 2001; Fraser and Shavlik 1997; Friedenreich et al. 2001; Gilliland et al. 2001; Hofvind and Thoresen 2001; Howard et al. 2009; John et al. 2003; Kruk 2007a; Kruk and Aboul-Enein 2003; Lahmann et al. 2007; Leitzmann et al. 2008; Levi et al. 1999; Luoto et al. 2000; Magnusson et al. 2005; Margolis et al. 2005; Maruti et al. 2008; Mezzetti et al. 1998; Moradi et al. 1999, 2000, 2002; Peplonska et al. 2008; Peters et al. 2009a; Rintala et al. 2002, 2003; Schmidt et al. 2008; Schnohr et al. 2005; Slattery et al. 2007; Steindorf et al. 2003; Tehard et al. 2006; Thune et al. 1997; Verloop et al. 2000).
Nine studies included separate risk estimates for women with and without a family history of breast cancer (Bernstein et al. 2005; Carpenter et al. 2003; Dallal et al. 2007; Hirose et al. 2003; Magnusson et al. 2005; Peplonska et al. 2008; Peters et al. 2009b; Schmidt et al. 2008; Sprague et al. 2007). A strong risk reduction, on average 21%, was observed among women without a family history of breast cancer while women with a family history experienced no breast cancer risk reduction with higher levels of physical activity (less than 1% on average). These risk decreases were statistically significant in all studies except for one that found no effect modification by family history of breast cancer (Magnusson et al. 2005).
Hormone receptor status was examined in 11 studies as a potential effect modifier (Bardia et al. 2006; Bernstein et al. 2005; Dallal et al. 2007; Dey et al. 2009; Enger et al. 2000; Lee et al. 2001b; Leitzmann et al. 2008; Maruti et al. 2008; Peplonska et al. 2008; Peters et al. 2009a; Schmidt et al. 2008). Seven studies examined the association between physical activity and breast cancer for estrogen positive (ER+) and negative (ER-) tumors (Bardia et al. 2006; Bernstein et al. 2005; Dallal et al. 2007; Dey et al. 2009; Peplonska et al. 2008; Peters et al. 2009a; Schmidt et al. 2008). Five studies observed statistically significant breast cancer risk reductions for higher levels of physical activity among women with ER+ tumors (Bardia et al. 2006; Bernstein et al. 2005; Peplonska et al. 2008; Peters et al. 2009a; Schmidt et al. 2008); two studies found significant reductions for ER- tumors (Dallal et al. 2007; Dey et al. 2009). The average risk reduction across all studies that examined the association for ER+ and ER- was the same for both groups (20%). Three studies compared the breast cancer risk reductions for highest versus lowest physical activity categories among women with progesterone positive (PR+) and negative (PR-) tumors (Bardia et al. 2006; Peplonska et al. 2008; Schmidt et al. 2008). Peplonska et al. (2008) and Schmidt et al. (2008) found statistically significant breast cancer risk reductions for higher physical activity among women with PR+ tumors, and no effect for PR- tumors. Bardia et al. (2006) observed the reciprocal – significant risk reductions for PR- and no effect for PR+. Eight studies compared women with estrogen- and progesterone- positive (ER+/PR+) tumors with women that had estrogen and progesterone negative (ER-/PR-) tumors (Bardia et al. 2006; Bernstein et al. 2005; Dallal et al. 2007; Enger et al. 2000; Lee et al. 2001b; Leitzmann et al. 2008; Maruti et al. 2008; Peters et al. 2009a; Schmidt et al. 2008), and an additional study considered women with ER-/PR- alone (Bernstein et al. 2005). Statistically significant risk reductions were found in only one ER+/PR+ study (Schmidt et al. 2008) and one ER-/PR- study (Dallal et al. 2007). Average risk reductions were greater for women with ER-/PR- tumors (27%) than for women with ER+/PR+ tumors (14%).
Parity was considered by seven studies (Bernstein et al. 2005; Dallal et al. 2007; Friedenreich et al. 2001; Magnusson et al. 2005; Maruti et al. 2008; Moradi et al. 2000; Tehard et al. 2006). A greater risk reduction was found for parous women (average decrease in breast cancer risk 38%) than for nulliparous women (average decrease 18%).
2.5 Summary of Epidemiologic Findings
In this review of 73 observational epidemiologic studies of physical activity and breast cancer risk, we found an average decrease in breast cancer risk of 25% when comparing the most physically active to the least active women. The risk reductions observed in studies assessing recreational and household activities were greater than for walking/cycling or occupational activity. Greater risk reductions were also observed for physical activity of longer than shorter duration. In terms of physical activity intensity, slightly stronger risk reductions were observed for women reporting participation in vigorous-intensity activities, in comparison with participation in moderate-intensity activities. We did not consider the associations of light-intensity activities or sedentary behavior separately in this review. Activity done after menopause appeared to have the greatest impact on the risk of breast cancer. However, risk reductions were apparent for physical activity performed across the lifespan. Within those studies that stratified by menopausal status, statistically significant risk reductions occurred more commonly amongst postmenopausal women than among premenopausal women. Physical activity reduced the risk of breast cancer within each BMI category except in obese women (≥30 kg/m2) with a clear dose–response in the breast cancer risk reduction across BMI categories with the greatest decrease risk among lean women (<22 kg/m2). Effect modification was also observed between race, family history of breast cancer, and parity subgroups with a stronger effect of physical activity observed amongst women of non-Caucasian backgrounds, without a family history of breast cancer and who were parous. Clear effect modification of the association between physical activity and breast cancer risk by hormone receptor status was not elucidated.
This review of the epidemiologic findings is limited, first and foremost, by the heterogeneity of methods used to assess physical activity. The vast majority of studies in our review used physical activity questionnaires, with some assessing lifetime physical activity and others using a single-item measure. Study quality also varied because of differences across these studies in sampling procedures and in reporting the results regarding the association between physical activity and breast cancer. Hence, direct comparisons across studies regarding these associations are difficult to interpret. We have presented average risk reductions, calculated as the mean of the point estimates, to allow comparisons between subgroups. However, average risk reduction is a crude measure that does not account for differences in study methods or the precision of the risk estimates. All risk reductions presented in this review represent the highest versus lowest category of physical activity assessed within a particular study. Physical activity categories may differ significantly between studies, and hence the strength of associations may be dependent somewhat on cutoffs used to define the most and least active participants.
Another factor for consideration is the validity of the physical activity questionnaires that were used. It is well recognized that physical activity questionnaires are prone to recall error and social desirability and other biases. In addition, many questionnaires focus on moderate- to vigorous-intensity activity, as it is difficult to capture light-intensity activities accurately by questionnaire. Hence, only a small fraction of an individual’s total physical activity may be measured in a given study. Physical activity questionnaires are frequently validated against other criterion measures, but these validation studies are limited by the lack of a true gold standard criterion method for measuring habitual activity over the long term.
Finally observational studies, whilst providing etiological insights, are not able to establish a direct, causal link between physical activity and breast cancer risk (Friedenreich 2001). Three randomized, controlled trials (RCTs) that were specifically designed to examine the etiologic pathways between physical activity and postmenopausal breast cancer risk have been conducted (Friedenreich et al. 2010a; McTiernan et al. 1999; Monninkhof et al. 2007b). These studies have involved supervised, controlled exercise interventions in which several proposed breast cancer biomarkers were measured and compared between the exercise and control groups to assess the impact of exercise on these biomarkers. The Physical Activity for Total Health (PATH) study (n = 173) and the Alberta Physical Activity and Breast Cancer Prevention (ALPHA) trial (n = 320) administered a moderate- to vigorous-intensity physical activity intervention of approximately 225 min per week over 12 months (Friedenreich et al. 2010a; McTiernan et al. 1999); the Sex Hormones and Physical Exercise (SHAPE) study prescribed a combined strength and aerobic training program of approximately 150 min per week to 189 sedentary postmenopausal women over 12 months (Monninkhof et al. 2007b). The effects of exercise on a variety of proposed biomarkers of risk have been reported, with more published results anticipated in the future. Current findings are described in the sections below.
3 Biologic Mechanisms
Various biologic pathways relating physical activity to breast cancer risk have been proposed (McTiernan 2008; Neilson et al. 2009; Rogers et al. 2008; Thompson et al. 2009; Wetmore and Ulrich 2006), but these pathways are still not well understood. It is likely that multiple interrelated pathways act cooperatively to decrease breast cancer risk. It is also possible that certain mechanisms predominate with specific doses or types of physical activity or perhaps in select subgroups of women, as implied earlier in this chapter.
One common theme of many hypotheses explaining the relation between physical activity and breast cancer risk is a mediation of the effect through body weight. Adiposity, frequently measured in terms of BMI, is now convincingly associated with increased breast cancer risk in postmenopausal women, and weight gain and abdominal fatness are probably also causally related (Renehan et al. 2008; World Cancer Research Fund and the American Institute for Cancer Research 2007). In premenopausal women there is no such association; in fact an inverse relation with BMI is probable (World Cancer Research Fund and the American Institute for Cancer Research 2007). Physical activity is recommended as a means for achieving modest weight loss in overweight and obese adults and also for weight maintenance (Donnelly et al. 2009; Lau et al. 2007). However, there is only limited evidence supporting the effectiveness of physical activity for abdominal fat loss (Lau et al. 2007; Ross and Janssen 1999). It remains plausible, however, that postmenopausal women could be amenable to significant abdominal fat loss given the right exercise prescription (e.g., Cuff et al. 2003; Giannopoulou et al. 2005; Irwin et al. 2003). The PATH and ALPHA trials demonstrated a clear exercise effect in a range of body composition measures (Friedenreich et al. 2010b; Irwin et al. 2003) including abdominal fat, whereas the SHAPE trial found that exercisers decreased body fat and waist circumference, but not weight, in comparison with controls (Velthuis et al. 2009). Therefore, fat loss is a logical explanation for the association between exercise and postmenopausal breast cancer risk.
One currently hypothesized biologic model for breast cancer risk, focusing mainly on the promotion and progression of initiated cells, implicates sex hormones, insulin resistance, adipokines, and chronic inflammation as possible mediators of physical activity (Neilson et al. 2009) (Fig. 2.12). While all of the proposed biomarkers in this model are associated with adiposity, and specifically abdominal fat, many of them are also influenced by exercise irrespective of body fat changes. Hence, the extent to which fat loss is necessary to derive a significant risk benefit from exercise remains a matter of controversy. Below we discuss these hypothesized mechanisms in more detail.
Hypothesized biologic model relating proposed biomarkers of risk to long-term exercise in pre- and postmenopausal women (Adapted from Neilson et al. 2009)
3.1 Sex Hormones
Endogenous estrogen status has been the predominant hypothesized mechanism relating physical activity to breast cancer risk for both pre- and postmenopausal women. Estrogens can inhibit apoptosis and act as mitogens in the breast, stimulating mammary cell proliferation through estrogen receptor-mediated transcriptional activity and by activation of intracellular signaling pathways (Lorincz and Sukumar 2006; Yager and Davidson 2006). In addition, oxidative estrogen metabolites with genotoxic and mutagenic potential could contribute to breast cancer initiation (Coyle 2008; Yager and Davidson 2006). The successful use of antiestrogenic drugs for reducing breast cancer risk serves as very strong evidence of the causal role for estrogens in women with ER+ breast tumors (Uray and Brown 2006).
Compelling evidence from observational studies supports a positive association between breast cancer risk and estrogens in postmenopausal women. In a pooled analysis of nine prospective studies in postmenopausal women (Key et al. 2002), the odds ratio for breast cancer was 2.00 (95% CI: 1.47–2.71) for the highest versus the lowest quintiles of total estradiol while for estrone the odds ratio was 2.19 (95% CI: 1.48–3.22). Given these findings and others (Cleary and Grossmann 2009), it is now widely accepted that estrogen status is associated with postmenopausal breast cancer. Fewer studies have examined this association in premenopausal women given the complexities of studying circulating hormone levels amidst menstrual cycles, and findings in general have been less consistent than for postmenopausal women (Eliassen and Hankinson 2008). Interestingly, one large cohort study conducted within the Nurses’ Health Study II showed that estradiol levels collected in the follicular phase of the menstrual cycle (but not the luteal phase) were significantly associated with an increased risk of premenopausal breast cancer, both overall and for ER+/PR+ tumors (Eliassen et al. 2006).
Multiple mechanisms could explain associations between postmenopausal breast cancer, estrogen levels, and physical activity. The first relates to BMI, which increases breast cancer risk specifically in postmenopausal women (World Cancer Research Fund and the American Institute for Cancer Research 2007). This relation might exist in part because after menopause, ovarian estrogen production ceases and adipose tissue becomes a key endogenous source of circulating estrogens (Kendall et al. 2007; Lorincz and Sukumar 2006). Hence, by reducing body fat through exercise, estrogen levels may decrease resulting in a lower risk of breast cancer. Levels of adipokines that influence estrogen biosynthesis can also be altered with weight loss (Cleary and Grossmann 2009). Furthermore, physical activity can lower blood insulin levels thereby increasing circulating sex hormone binding globulin (SHBG) (Kaaks 1996; Pugeat et al. 1991) which binds reversibly to estrogens to affect their bioavailability.
In premenopausal women these biologic mechanisms are less well understood. Exercise has been linked to delayed menarche and menstrual dysfunction implying lower cumulative exposure to sex hormones and presumably lower risk of breast cancer; however, the level of activity needed to achieve these effects is probably high (reviewed in Bernstein 2009; Campbell and McTiernan 2007) and an energy deficit, rather than exercise per se, may be the predominant mechanism (Loucks 2003). In observational studies of highly active premenopausal women, blood estrogen levels have generally been inversely related to activity but in cross-sectional studies of nonathletes, the relation is more equivocal (Coyle 2008).
Breast cancer risk may also be affected by androgen levels. Androgens can act directly on breast cells by binding to the androgen receptor to influence cell growth (Nicolas Diaz-Chico et al. 2007) and/or they may act indirectly via estrogen production: the aromatase enzyme converts testosterone to estradiol, and androstenedione to estrone, within adipose and other tissues in postmenopausal women and principally in the ovaries of premenopausal women (Kendall et al. 2007). Testosterone, which is one of the most powerful natural forms of androgen, is derived from androstenedione in the ovaries and also in peripheral tissues such as adipose and breast (Nicolas Diaz-Chico et al. 2007). In a pooled analysis of prospective studies in postmenopausal women (Key et al. 2002) and in at least one other cohort study (Kaaks et al. 2005), adjustment for estradiol levels only slightly attenuated the relative risk associated with testosterone, thus supporting an independent mechanism for androgens. Physical activity might lower testosterone levels by decreasing adiposity, or possibly by increasing SHBG levels (and decreasing the bioavailability of testosterone) on account of lowered blood insulin levels (Kaaks 1996; Pugeat et al. 1991).
Epidemiologic evidence supports a positive association between serum androgen levels and postmenopausal (Key et al. 2002; Neilson et al. 2009) and, to a lesser extent, premenopausal breast cancer risk (Eliassen and Hankinson 2008). In a pooled analysis of prospective studies, postmenopausal women in the highest quintiles of serum testosterone and androstenedione concentrations, respectively, had more than double the risk of developing breast cancer compared to women in the lowest quintiles (RR = 2.22, 95% CI: 1.59–3.10 for testosterone; RR = 2.15, 95% CI: 1.44–3.21 for androstenedione) (Key et al. 2002). In premenopausal women, fewer studies have been conducted but findings have been fairly consistent, showing nonsignificantly and significantly increased risks for those with higher blood levels of testosterone (Eliassen and Hankinson 2008).
The effect of physical activity on sex hormones may vary according to hormone receptor status (Sieri et al. 2009), across the menopausal transition (Schmitz et al. 2007), and also with body fat (McTiernan et al. 2004a; McTiernan et al. 2004b). Three RCTs have examined the effect of exercise on sex hormone levels and weight change in postmenopausal women. In the PATH trial, women assigned to the exercise group who lost more than 2% body fat experienced significantly lower blood estrogen and androgen levels relative to controls after 12 months of exercise (McTiernan et al. 2004a; McTiernan et al. 2004b). Likewise, the SHAPE trial showed that relative to controls, androgen (but not estrogen) levels decreased significantly in exercisers who lost >2% body fat after 4 months of exercise (Monninkhof et al. 2009). In the ALPHA trial, estrogen levels decreased significantly more in exercisers than in controls after 12 months, even after adjusting for weight change, whereas androgen levels did not change significantly (Friedenreich et al. 2010a). Unlike the first two trials, the ALPHA trial findings for estrogen suggest an independent role for physical activity. Similarly, some cross-sectional studies (but not all, Bertone-Johnson et al. 2009; Van Gils et al. 2009) in postmenopausal women have found significant inverse associations between physical activity and sex hormone levels even after controlling for BMI or adiposity (Cauley et al. 1989; Chan et al. 2007; Madigan et al. 1998; Verkasalo et al. 2001). Therefore, it remains unclear whether or not fat loss is needed to induce changes in sex hormones.
3.2 Insulin-Related Factors
A causal link between insulin resistance and breast cancer risk is biologically plausible. Insulin exerts mitotic, anti-apoptotic effects in breast cancer cells (Lann and LeRoith 2008; Osborne et al. 1976) and hyperinsulinemia increases the bioavailability of sex hormones by decreasing SHBG levels (Kaaks 1996; Pugeat et al. 1991). Insulin resistance and hyperinsulinemia are also strongly related to obesity (Haslam and James 2005) and particularly intraabdominal fat (Kaaks 1996), as well as various adipokines and inflammatory factors (Rose et al. 2004; Vona-Davis et al. 2007) that individually have been linked to breast cancer. Therefore, insulin may alter breast cancer risk independently or indirectly through other biomarkers of risk.
The epidemiologic evidence surrounding the role of insulin in breast cancer risk is growing but remains inconclusive. A modest causal association with breast cancer risk appears to exist with type 2 diabetes, specifically in postmenopausal women (Larsson et al. 2007; Xue and Michels 2007). Yet, while findings from retrospective studies have generally also shown positive associations between breast cancer risk and insulin and C-peptide (a marker of pancreatic insulin secretion (Bonser and Garcia-Webb 1984)) levels, cohort studies have typically produced null results (Pisani 2008). The effect may vary according to menopausal status. Yet within pre- and postmenopausal women, relations between breast cancer risk and insulin or C-peptide have been inconsistent (Neilson et al. 2009; Xue and Michels 2007). Recently, however, one cohort study of 5,450 postmenopausal women that employed serial measurements of glucose and insulin found a statistically significant positive association between breast cancer risk and insulin levels (Kabat et al. 2009) and a case-cohort study found the same association but only amongst nonusers of hormone therapy (Gunter et al. 2009). Another recent prospective study (Cust et al. 2009) found no association with C-peptide in postmenopausal women but did observe decreased risk with increasing HbA1C levels, a measure of long-term blood glucose (Gabbay 1982).
Exercise combined with weight loss is generally accepted as an effective means for improving insulin sensitivity and preventing diabetes (Ivy 1997; Klein et al. 2004; Ryan 2000; Warburton et al. 2007). The effect of exercise may be strongest for those with impaired (versus normal) glucose tolerance (Ivy 1997), when as combined aerobic/resistance exercise versus aerobic exercise alone (Cuff et al. 2003), or at higher intensity (Gill 2007). In terms of abdominal fat loss (which correlates with insulin sensitivity), however, one 20-week exercise RCT in postmenopausal women on a calorie-restricted diet showed no difference whether moderate or vigorous aerobic exercise was undertaken (Nicklas et al. 2009). In the PATH trial, insulin levels decreased with moderate exercise and this change was significantly different from that of controls (Frank et al. 2005). Moreover, insulin change was modified by change in total fat mass: exercisers who lost >2 kg body fat over the year had a significantly larger decrease in insulin levels than those who gained fat mass. In addition, among those women who gained fat over the year, exercise prevented an increase in insulin levels. Hence, exercise appears to alter insulin levels through weight change but also independently of fat loss.
Higher levels of circulating insulin-like growth factor-1 (IGF) have also been hypothesized to increase breast cancer risk. IGF-1 may impact breast tissue directly by acting as a potent mitogen which increases cell proliferation and decreases apoptosis within the breast (Yu and Rohan 2000). The epidemiologic evidence for a positive association with breast cancer is stronger in pre- than in postmenopausal women (Fletcher et al. 2005), but is generally inconsistent (Eliassen and Hankinson 2008; Lann and LeRoith 2008). Furthermore, the evidence relating IGF-1 and IGF binding protein-3 (IGFBP-3) levels to physical activity in women has been inconsistent and generally unconvincing (McTiernan et al. 2005; Orenstein and Friedenreich 2004; Tworoger et al. 2007b). Thus, IGF-1 may not be an important intermediate factor in the proposed physical activity–breast cancer pathway.
3.3 Adipokines and Inflammation
Adipokines (adipocytokines) are a group of biologically active polypeptides produced by adipocytes or adipose tissue; they include leptin (Cirillo et al. 2008; Surmacz 2007), adiponectin (Barb et al. 2007; Wang et al. 2007), tumor necrosis factor-α (TNF-α) (Balkwill 2006; Szlosarek et al. 2006), and interleukin-6 (IL-6) (Knupfer and Preiss 2007). C-reactive protein (CRP) is not an adipokine, but an acute phase protein produced in the liver in response to TNF-α and IL-6 levels (Heikkila et al. 2007; Lee and Pratley 2005); all three are considered inflammatory markers. Obesity represents a chronic low-grade, systemic inflammatory state with elevated levels of inflammatory markers (Lee and Pratley 2005). Perpetual cell proliferation, microenvironmental changes and oxidative stress resulting from chronic inflammation could deregulate normal cell growth to promote initiated cells toward malignancy (Coussens and Werb 2002). Adipokines may also increase risk on account of their strong positive correlations with hyperinsulinemia, insulin resistance, and type 2 diabetes, by affecting estrogen biosynthesis and estrogen activity, or by directly altering cell growth and promoting metastases (reviewed in, Neilson et al. 2009).
While biologic plausibility exists, relatively little epidemiologic evidence has related elevated adipokines and inflammatory markers to a significantly increased risk of breast cancer in postmenopausal women (Neilson et al. 2009), for whom risk is most clearly associated with body fat. Among those studies that have examined these markers, most focused on leptin and adiponectin. Evidence was generally conflicting in the case of leptin and somewhat stronger for adiponectin (Barb et al. 2007), but for both of these proposed biomarkers only a few studies were of prospective design (Cust et al. 2009; Stattin et al. 2004; Tworoger et al. 2007a). The etiologic relevance of the adiponectin:leptin ratio also is now being considered (Cleary et al. 2009).
Exercise trials across various study populations have generally supported the absence of an effect of exercise on inflammatory markers, but differing study designs and study populations makes this overall finding difficult to interpret (Wetmore and Ulrich 2006). In fact recent RCT evidence from older type 2 diabetics implied that greater decreases in leptin, IL-6, TNF-α, and CRP and enhanced increases in adiponectin might be achieved with exercise of high intensity (versus low) and preferably using a combination of aerobic and resistance training (versus aerobic) (Balducci et al. 2009). In addition, the PATH trial in postmenopausal women demonstrated lowered leptin (Frank et al. 2005) and CRP (Campbell et al. 2009) levels after 12 months of exercise, but CRP was decreased only among women who were obese or had abdominal obesity.
Sustained physical activity probably lowers adipokine and CRP levels through several mechanisms. In one prospective cohort study, adipokine and inflammatory marker changes correlated significantly with changes in intraabdominal fat in women transitioning to menopause (Lee et al. 2009), implying that biomarker decreases can be achieved through weight loss. Similarly, the PATH trial demonstrated significant decreases in CRP specifically in those who lost body fat (Campbell et al. 2009). Yet exercise RCTs have also shown decreases in adipokine and CRP levels that occurred independently of fat loss (Balducci et al. 2009; You et al. 2004). Such fat-independent mechanisms are generally not well understood, but hypotheses have been suggested (e.g., Mathur and Pedersen 2008).
3.4 Other Mechanisms
Other pathways relating physical activity to breast cancer almost certainly exist. Biologic pathways causing DNA damage, cancer initiation, or cancer promotion and progression (Rundle 2005) may interact with the mechanisms already discussed to increase breast cancer risk even further. With improved understanding regarding these interrelated mechanisms and their role in the causal pathways between physical activity and breast cancer risk, the biologic model depicted in Fig. 2.12 could be modified or expanded. Mammographic density was not included in this model since exercise has not been proven to lower the dense area or dense volume of the breast, which are positively associated with breast cancer risk (Woolcott et al. 2010). Likewise, the ratio of estrogen metabolites 2-hydroxyestrone:16α-hydroxyestrone has been hypothesized to increase breast cancer risk, but relatively strong epidemiologic evidence suggests no effect of physical activity on this ratio (Atkinson et al. 2004; Campbell et al. 2007; Schmitz et al. 2008). Other proposed mechanisms that might relate physical activity to breast cancer risk include the ability of exercise to decrease oxidative stress (e.g., as measured by F2-isoprostanes (Dai et al. 2009; Schmitz et al. 2008)) and enhance resting immune function (Campbell et al. 2008; Wetmore and Ulrich 2006). Moreover, by altering estrogen levels, exercise may reduce promoter hypermethylation of tumor suppressor genes (i.e., gene silencing by estrogens) and also genotoxicity from estrogen metabolite–DNA adducts formed in breast tissue (Coyle 2008). Other hypotheses suggest that certain intracellular signaling pathways are affected favorably by exercise, whereby procarcinogenic pathways are suppressed and anticarcinogenic pathways are promoted within the breast (Thompson et al. 2009). Across many proposed mechanisms, effect modification by genetic subtype might better our understanding of the etiologic importance of proposed biomarkers (Han et al. 2008; Kendall et al. 2007) and their responses to exercise (Gill 2007).
4 Conclusion
The criteria for causality for the association between physical activity and breast cancer risk are largely met with the evidence that has accumulated thus far from observational epidemiologic studies. There is consistent evidence from studies conducted around the world for a 25% risk reduction amongst physically active women as compared to the least active women. There is also evidence of a dose–response effect of decreasing risk with increasing levels of activity as well as mechanistic data from randomized exercise intervention trials that have examined intermediate biomarkers hypothesized to be part of the pathway between physical activity and breast cancer risk. The associations are strongest for recreational activity that is sustained over lifetime or at least after menopause, that is of moderate to vigorous intensity, and performed regularly. There is also emerging evidence that physical activity may have a differential effect amongst population subgroups with stronger effects found in postmenopausal women, normal weight women, non-Caucasians, parous women, and women without a family history of breast cancer.
Several areas for future research can be considered. These would include examining how sedentary behavior and light-intensity activity additionally contribute to breast cancer risk or risk reduction. More precision is needed in the assessment of physical activity including the type, dose, and timing of activity over the lifetime for these studies. Research that focuses on effect modification by factors such as menopausal status, tumor subtype, and other components of type, timing, and dose of activity would improve our understanding of the nature of the association between physical activity and breast cancer risk. Investigations of the related biologic mechanisms would also inform future epidemiologic research. There is a need for prospective observational epidemiologic studies relating new and proposed biomarkers to breast cancer risk (particularly pertaining to insulin resistance and inflammation). As well, additional randomized, controlled exercise intervention trials that evaluate biomarker changes with different types and doses of physical activity are needed to further elucidate how activity influences breast cancer risk.
References
Adams-Campbell LL, Rosenberg L, Rao RS et al (2001) Strenuous physical activity and breast cancer risk in African-American women. J Natl Med Assoc 93:267–275
Atkinson C, Lampe JW, Tworoger SS et al (2004) Effects of a moderate intensity exercise intervention on estrogen metabolism in postmenopausal women. Cancer Epidemiol Biomark Prev 13:868–874
Australian Institute of Health and Welfare, National Breast and Ovarian Cancer Centre (2009) Breast cancer in Australia: An overview. Cancer series no. 50, Cat. no. CAN 46, Canberra (in press)
Balducci S, Zanuso S, Nicolucci A et al (2009) Anti-inflammatory effect of exercise training in subjects with type 2 diabetes and the metabolic syndrome is dependent on exercise modalities and independent of weight loss. Nutr Metab Cardiovasc Dis DOI:10.1016/j.numecd.2009.04.015
Balkwill F (2006) TNF-alpha in promotion and progression of cancer. Cancer Metastasis Rev 25:409–416
Barb D, Williams CJ, Neuwirth AK et al (2007) Adiponectin in relation to malignancies: A review of existing basic research and clinical evidence. Am J Clin Nutr 86:s858–s866
Bardia A, Hartmann LC, Vachon CM et al (2006) Recreational physical activity and risk of postmenopausal breast cancer based on hormone receptor status. Arch Intern Med 166: 2478–2483
Bernstein L (2009) Exercise and breast cancer prevention. Curr Oncol Rep 11:490–496
Bernstein L, Patel AV, Ursin G et al (2005) Lifetime recreational exercise activity and breast cancer risk among black women and white women. J Natl Cancer Inst 97:1671–1679
Bertone-Johnson ER, Tworoger SS, Hankinson SE (2009) Recreational physical activity and steroid hormone levels in postmenopausal women. Am J Epidemiol 170:1095–1104
Bonser AM, Garcia-Webb P (1984) C-peptide measurement: Methods and clinical utility. Crit Rev Clin Lab Sci 19:297–352
Breslow RA, Ballard-Barbash R, Munoz K et al (2001) Long-term recreational physical activity and breast cancer in the National Health and Nutrition Examination Survey I epidemiologic follow-up study. Cancer Epidemiol Biomark Prev 10:805–808
Calle EE, Murphy TK, Rodriguez C et al (1998) Occupation and breast cancer mortality in a prospective cohort of US women. Am J Epidemiol 148:191–197
Campbell KL, McTiernan A (2007) Exercise and biomarkers for cancer prevention studies. J Nutr 137:161S–169S
Campbell KL, Westerlind KC, Harber VJ et al (2007) Effects of aerobic exercise training on estrogen metabolism in premenopausal women: A randomized controlled trial. Cancer Epidemiol Biomark Prev 16:731–739
Campbell PT, Wener MH, Sorensen B et al (2008) Effect of exercise on in vitro immune function: A 12-month randomized, controlled trial among postmenopausal women. J Appl Physiol 104: 1648–1655
Campbell PT, Campbell KL, Wener MH et al (2009) A yearlong exercise intervention decreases CRP among obese postmenopausal women. Med Sci Sports Exerc 41:1533–1539
Canadian Cancer Society (2009) Canadian Cancer Statistics 2009. Toronto
Cancer Research UK (2009) Breast cancer – UK incidence statistics. CancerStats http://info.cancerresearchuk.org/cancerstats/types/breast/incidence/index.htm#source5
Carpenter CL, Ross RK, Paganini-Hill A et al (2003) Effect of family history, obesity and exercise on breast cancer risk among postmenopausal women. Int J Cancer 106:96–102
Cauley JA, Gutai JP, Kuller LH et al (1989) The epidemiology of serum sex hormones in postmenopausal women. Am J Epidemiol 129:1120–1131
Cerhan JR, Chiu BC et al (1998) Physical activity, physical function, and the risk of breast cancer in a prospective study among elderly women. J Gerontol A Biol Sci Med Sci 53A:M251–M256
Chan MF, Dowsett M, Folkerd E et al (2007) Usual physical activity and endogenous sex hormones in postmenopausal women: The European Prospective Investigation into Cancer-Norfolk population study. Cancer Epidemiol Biomark Prev 16:900–905
Chang SC, Ziegler RG, Dunn B et al (2006) Association of energy intake and energy balance with postmenopausal breast cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Epidemiol Biomark Prev 15: 334–341
Chen CL, White E, Malone KE et al (1997) Leisure-time physical activity in relation to breast cancer among young women (Washington, United States). Cancer Causes Control 8:77–84
Cirillo D, Rachiglio AM, la MR et al (2008) Leptin signaling in breast cancer: An overview. J Cell Biochem 105:956–964
Cleary MP, Grossmann ME (2009) Minireview: Obesity and breast cancer: the estrogen connection. Endocrinology 150:2537–2542
Cleary MP, Ray A, Rogozina OP et al (2009) Targeting the adiponectin:leptin ratio for postmenopausal breast cancer prevention. Front Biosci (Schol Ed) 1:329–357
Colditz GA, Feskanich D, Chen WY et al (2003) Physical activity and risk of breast cancer in premenopausal women. Br J Cancer 89:847–851
Coogan PF, Aschengrau A (1999) Occupational physical activity and breast cancer risk in the upper Cape Cod cancer incidence study. Am J Ind Med 36:279–285
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Coyle YM (2008) Physical activity as a negative modulator of estrogen-induced breast cancer. Cancer Causes Control 19:1021–1029
Cuff DJ, Meneilly GS, Martin A et al (2003) Effective exercise modality to reduce insulin resistance in women with type 2 diabetes. Diab Care 26:2977–2982
Cust AE, Stocks T, Lukanova A et al (2009) The influence of overweight and insulin resistance on breast cancer risk and tumour stage at diagnosis: A prospective study. Breast Cancer Res Treat 113:567–576
Dai Q, Gao YT, Shu XO et al (2009) Oxidative stress, obesity, and breast cancer risk: Results from the Shanghai Women’s Health Study. J Clin Oncol 27:2482–2488
Dallal CM, Sullivan-Halley J, Ross RK et al (2007) Long-term recreational physical activity and risk of invasive and in situ breast cancer: The California teachers study. Arch Intern Med 167: 408–415
Dey S, Boffetta P, Mathews A et al (2009) Risk factors according to estrogen receptor status of breast cancer patients in Trivandrum, South India. Int J Cancer 125:1663–1670
Dirx MJ, Voorrips LE, Goldbohm RA et al (2001) Baseline recreational physical activity, history of sports participation, and postmenopausal breast carcinoma risk in the Netherlands Cohort Study. Cancer 92:1638–1649
Donnelly JE, Blair SN, Jakicic JM et al (2009) American College of Sports Medicine Position Stand Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 41:459–471
Dorgan JF, Brown C, Barrett M et al (1994) Physical activity and risk of breast cancer in the Framingham Heart Study. Am J Epidemiol 139: 662–669
Dorn J, Vena J, Brasure J et al (2003) Lifetime physical activity and breast cancer risk in pre- and postmenopausal women. Med Sci Sports Exerc 35:278–285
Dosemeci M, Hayes RB, Vetter R et al (1993) Occupational physical activity, socioeconomic status, and risks of 15 cancer sites in Turkey. Cancer Causes Control 4:313–321
Eliassen AH, Hankinson SE (2008) Endogenous hormone levels and risk of breast, endometrial and ovarian cancers: Prospective studies. Adv Exp Med Biol 630:148–165
Eliassen AH, Missmer SA, Tworoger SS et al (2006) Endogenous steroid hormone concentrations and risk of breast cancer among premenopausal women. J Natl Cancer Inst 98:1406–1415
Enger SM, Ross RK, Paganini-Hill A et al (2000) Body size, physical activity, and breast cancer hormone receptor status: Results from two case-control studies. Cancer Epidemiol Biomark Prev 9:681–687
Ferlay J, Bray F, Pisani P et al (2004) GLOBOCAN 2002: Cancer incidence, mortality and prevalence worldwide cancerbase no. 5. version 2.0. IARC Press, Lyon http://www-dep.iarc.fr
Fletcher O, Gibson L, Johnson N et al (2005) Polymorphisms and circulating levels in the insulin-like growth factor system and risk of breast cancer: A systematic review. Cancer Epidemiol Biomark Prev 14:2–19
Frank LL, Sorensen BE, Yasui Y et al (2005) Effects of exercise on metabolic risk variables in overweight postmenopausal women: A randomized clinical trial. Obes Res 13:615–625
Fraser GE, Shavlik D (1997) Risk factors, lifetime risk, and age at onset of breast cancer. Ann Epidemiol 7:375–382
Friedenreich CM (2001) Physical activity and cancer prevention: From observational to intervention research. Cancer Epidemiol Biomark Prev 10:287–301
Friedenreich CM, Cust AE (2008) Physical activity and breast cancer risk: Impact of timing, type and dose of activity and population subgroup effects. Brit J Sports Med 42:636–647
Friedenreich CM, Orenstein MR (2002) Physical activity and cancer prevention: Etiologic evidence and biological mechanisms. J Nutr 132: 3456S–3464S
Friedenreich CM, Rohan TE (1995) Physical activity and risk of breast cancer. Eur J Cancer Prev 4:145–151
Friedenreich CM, Bryant HE, Courneya KS (2001) Case-control study of lifetime physical activity and breast cancer risk. Am J Epidemiol 154: 336–347
Friedenreich CM, Woolcott CG, McTieman A et al (2010a) Alberta Physical Activity and Breast Cancer Prevention Trial: sex hormone changes in a year-long exercise intervention among postmenopausal women. J Clin Oncol 28:1458–1466
Friedenreich C, Woolcott CG, McTiernan A et al (2010b) Adiposity changes after a one year aerobic exercise intervention among postmenopausal women: randomized controlled trial. Int J Obes (in press)
Gabbay KH (1982) Glycosylated hemoglobin and diabetes mellitus. Med Clin North Am 66: 1309–1315
Gammon MD, Schoenberg JB, Britton JA et al (1998) Recreational physical activity and breast cancer risk among women under age 45 years. Am J Epidemiol 147:273–280
Gao CM, Tajima K, Ding JH et al (2009) Body size, physical activity and risk of breast cancer. A case control study in Jangsu Province of China. Asian Pac J Cancer Prev 10:877–881
Giannopoulou I, Ploutz-Snyder LL, Carhart R et al (2005) Exercise is required for visceral fat loss in postmenopausal women with type 2 diabetes. J Clin Endocrinol Metab 90:1511–1518
Gill JM (2007) Physical activity, cardiorespiratory fitness and insulin resistance: A short update. Curr Opin Lipidol 18:47–52
Gilliland FD, Li YF, Baumgartner K et al (2001) Physical activity and breast cancer risk in hispanic and non-hispanic white women. Am J Epidemiol 154:442–450
Gunter MJ, Hoover DR, Yu H et al (2009) Insulin, insulin-like growth factor-I, and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 101:48–60
Han CZ, Du LL, Jing JX et al (2008) Associations among lipids, leptin, and leptin receptor gene Gin223Arg polymorphisms and breast cancer in China. Biol Trace Elem Res 126:38–48
Haslam DW, James WP (2005) Obesity. Lancet 366:1197–1209
Heikkila K, Ebrahim S, Lawlor DA (2007) A systematic review of the association between circulating concentrations of C reactive protein and cancer. J Epidemiol Community Health 61: 824–833
Hirose K, Hamajima N, Takezaki T et al (2003) Physical exercise reduces risk of breast cancer in Japanese women. Cancer Sci 94:193–199
Hofvind SS, Thoresen SO (2001) Physical activity and breast cancer. Tidsskr Nor Laegeforen 121: 1892–1895
Howard RA, Leitzmann MF, Linet MS et al (2009) Physical activity and breast cancer risk among pre- and postmenopausal women in the U.S. Radiologic Technologists cohort. Cancer Causes Control 20:323–333
Hu YH, Nagata C, Shimizu H et al (1997) Association of body mass index, physical activity, and reproductive histories with breast cancer: A case-control study in Gifu, Japan. Breast Cancer Res Treat 43: 65–72
IARC Working Group (2002) IARC Handbook of Cancer Prevention, Volume 6: Weight control and physical activity. IARC, Lyon
Irwin ML, Yasui Y, Ulrich CM et al (2003) Effect of exercise on total and intra-abdominal body fat in postmenopausal women: A randomized controlled trial. JAMA 289:323–330
Ivy JL (1997) Role of exercise training in the prevention and treatment of insulin resistance and non-insulin-dependent diabetes mellitus. Sports Med 24:321–336
Jemal A, Siegel R, Ward E et al (2009) Cancer Statistics, 2009. Ca-A Cancer J Clin 59:225–249
John EM, Horn-Ross PL, Koo J (2003) Lifetime physical activity and breast cancer risk in a multiethnic population: The San Francisco Bay area breast cancer study. Cancer Epidemiol Biomark Prev 12:1143–1152
Kaaks R (1996) Nutrition, hormones, and breast cancer: Is insulin the missing link? Cancer Causes Control 7:605–625
Kaaks R, Rinaldi S, Key TJ et al (2005) Postmenopausal serum androgens, oestrogens and breast cancer risk: The European prospective investigation into cancer and nutrition. Endocr Relat Cancer 12:1071–1082
Kabat GC, Kim M, Caan BJ et al (2009) Repeated measures of serum glucose and insulin in relation to postmenopausal breast cancer. Int J Cancer 125:2704–2710
Kendall A, Folkerd EJ, Dowsett M (2007) Influences on circulating oestrogens in postmenopausal women: Relationship with breast cancer. J Steroid Biochem Mol Biol 103:99–109
Key T, Appleby P, Barnes I et al (2002) Endogenous sex hormones and breast cancer in postmenopausal women: Reanalysis of nine prospective studies. J Natl Cancer Inst 94:606–616
Klein S, Sheard NF, Pi-Sunyer X et al (2004) Weight management through lifestyle modification for the prevention and management of type 2 diabetes: Rationale and strategies: a statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. Diab Care 27:2067–2073
Knupfer H, Preiss R (2007) Significance of interleukin-6 (IL-6) in breast cancer (review). Breast Cancer Res Treat 102:129–135
Kruk J (2007a) Lifetime physical activity and the risk of breast cancer: A case-control study. Cancer Detect Prev 31:18–28
Kruk J (2007b) Association of lifestyle and other risk factors with breast cancer according to menopausal status: A case-control study in the region of Western Pomerania (Poland). Asian Pacific J Cancer Prev 8:513–524
Kruk J, Aboul-Enein HY (2003) Occupational physical activity and the risk of breast cancer. Cancer Detect Prev 27:187–192
Lahmann PH, Friedenreich C, Schuit AJ et al (2007) Physical activity and breast cancer risk: The European prospective investigation into cancer and nutrition. Cancer Epidemiol Biomark Prev 16:36–42
Lann D, LeRoith D (2008) The role of endocrine insulin-like growth factor-I and insulin in breast cancer. J Mammary Gland Biol Neoplasia 13: 371–379
Larsson SC, Mantzoros CS, Wolk A (2007) Diabetes mellitus and risk of breast cancer: A meta-analysis. Int J Cancer 121:856–862
Lau DC, Douketis JD, Morrison KM et al (2007) 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 176: S1–S13
Lee YH, Pratley RE (2005) The evolving role of inflammation in obesity and the metabolic syndrome. Curr Diab Rep 5:70–75
Lee IM, Cook NR, Rexrode KM et al (2001a) Lifetime physical activity and risk of breast cancer. Br J Cancer 85:962–965
Lee IM, Rexrode KM, Cook NR et al (2001b) Physical activity and breast cancer risk: The Women’s Health Study (United States). Cancer Causes Control 12:137–145
Lee CG, Carr MC, Murdoch SJ et al (2009) Adipokines, inflammation, and visceral adiposity across the menopausal transition: A prospective study. J Clin Endocrinol Metab 94: 1104–1110
Leitzmann MF, Moore SC, Peters TM et al (2008) Prospective study of physical activity and risk of postmenopausal breast cancer. Breast Cancer Res 10:R92
Levi F, Pasche C, Lucchini F et al (1999) Occupational and leisure time physical activity and the risk of breast cancer. Eur J Cancer 35: 775–778
Lorincz AM, Sukumar S (2006) Molecular links between obesity and breast cancer. Endocr Relat Cancer 13:279–292
Loucks, AB (2003) Energy availability, not body fatness, regulates reproductive function in women. Exerc Sport Sci Rev 31:144–148.
Luoto R, Latikka P, Pukkala E et al (2000) The effect of physical activity on breast cancer risk: A cohort study of 30, 548 women. Eur J Epidemiol 16:973–980
Madigan MP, Troisi R, Potischman N et al (1998) Serum hormone levels in relation to reproductive and lifestyle factors in postmenopausal women (United States). Cancer Causes Control 9:199–207
Magnusson CM, Roddam AW, Pike MC et al (2005) Body fatness and physical activity at young ages and the risk of breast cancer in premenopausal women. Br J Cancer 93:817–824
Marcus PM, Newman B, Moorman PG et al (1999) Physical activity at age 12 and adult breast cancer risk (United States). Cancer Causes Control 10:293–302
Margolis KL, Mucci L, Braaten T et al (2005) Physical activity in different periods of life and the risk of breast cancer: The Norwegian-Swedish Women’s Lifestyle and Health Cohort Study. Cancer Epidemiol Biomark Prev 14:27–32
Maruti SS, Willett WC, Feskanich D et al (2008) A prospective study of age-specific physical activity and premenopausal breast cancer. J Natl Cancer Inst 100:728–737
Mathew A, Gajalakshmi V, Rajan B et al (2009) Physical activity levels among urban and rural women in south India and the risk of breast cancer: A case-control study. Eur J Cancer Prev 18:368–376
Mathur N, Pedersen BK (2008) Exercise as a mean to control low-grade systemic inflammation. Mediat Inflamm 2008:1–6
Matthews CE, Shu XO, Jin F et al (2001) Lifetime physical activity and breast cancer risk in the Shanghai Breast Cancer Study. Br J Cancer 84:994–1001
McTiernan A (2008) Mechanisms linking physical activity with cancer. Nat Rev Cancer 8:205–211
McTiernan A, Stanford JL, Weiss NS et al (1996) Occurrence of breast cancer in relation to recreational exercise in women age 50-64 years. Epidemiology 7:598–604
McTiernan A, Ulrich CM, Yancey D et al (1999) The Physical Activity for Total Health (PATH) Study: Rationale and design. Med Sci Sports Exerc 31:1307–1312
McTiernan A, Kooperberg C, White E et al (2003) Recreational physical activity and the risk of breast cancer in postmenopausal women: The Women’s Health Initiative Cohort Study. JAMA 290:1331–1336
McTiernan A, Tworoger SS, Rajan KB et al (2004a) Effect of exercise on serum androgens in postmenopausal women: A 12-month randomized clinical trial. Cancer Epidemiol Biomark Prev 13:1099–1105
McTiernan A, Tworoger SS, Ulrich CM et al (2004b) Effect of exercise on serum estrogens in postmenopausal women: A 12-month randomized clinical trial. Cancer Res 64:2923–2928
McTiernan A, Sorensen B, Yasui Y et al (2005) No effect of exercise on insulin-like growth factor 1 and insulin-like growth factor binding protein 3 in postmenopausal women: A 12-month randomized clinical trial. Cancer Epidemiol Biomark Prev 14:1020–1021
Mertens AJ, Sweeney C, Shahar E et al (2006) Physical activity and breast cancer incidence in middle-aged women: A prospective cohort study. Breast Cancer Res Treat 97:209–214
Mezzetti M, La Vecchia C, Decarli A et al (1998) Population attributable risk for breast cancer: Diet, nutrition, and physical exercise. J Natl Cancer Inst 90:389–394
Monninkhof EM, Elias SG, Vlems FA et al (2007a) Physical activity and breast cancer: A systematic review. Epidemiology 18:137–157
Monninkhof EM, Peeters PH, Schuit AJ (2007b) Design of the sex hormones and physical exercise (SHAPE) study. BMC Public Health 7
Monninkhof EM, Velthuis MJ, Peeters PH et al (2009) Effect of exercise on postmenopausal sex hormone levels and role of body fat: A randomized controlled trial. J Clin Oncol 27: 4492–4499
Moradi T, Adami HO, Bergstrom R et al (1999) Occupational physical activity and risk for breast cancer in a nationwide cohort study in Sweden. Cancer Causes Control 10:423–430
Moradi T, Nyren O, Zack M et al (2000) Breast cancer risk and lifetime leisure-time and occupational physical activity (Sweden). Cancer Causes Control 11:523–531
Moradi T, Adami HO, Ekbom A et al (2002) Physical activity and risk for breast cancer: A prospective cohort study among Swedish twins. Int J Cancer 100:76–81
Neilson HK, Friedenreich CM, Brockton NT et al (2009) Physical activity and postmenopausal breast cancer: Proposed biologic mechanisms and areas for future research. Cancer Epidemiol Biomark Prev 18:11–27
Nicklas BJ, Wang X, You T et al (2009) Effect of exercise intensity on abdominal fat loss during calorie restriction in overweight and obese postmenopausal women: A randomized, controlled trial. Am J Clin Nutr 89:1043–1052
Nicolas Diaz-Chico B, German RF, Gonzalez A et al (2007) Androgens and androgen receptors in breast cancer. J Steroid Biochem Mol Biol 105:1–15
Nkondjock A, Robidoux A, Paredes Y et al (2006) Diet, lifestyle and BRCA-related breast cancer risk among French-Canadians. Breast Cancer Res Treat 98:285–294
Office for National Statistics (2008) Annual Update: Cancer incidence and mortality in the United Kingdom and constituent countries, 2003–05. Health Stat Quart 40:91–97
Orenstein MR, Friedenreich CM (2004) Review of physical activity and the IGF family. J Phys Activ Health 1:291–320
Osborne CK, Bolan G, Monaco ME et al (1976) Hormone responsive human breast cancer in long-term tissue culture: Effect of insulin. Proc Natl Acad Sci USA 73:4536–4540
Patel AV, Callel EE, Bernstein L et al (2003) Recreational physical activity and risk of postmenopausal breast cancer in a large cohort of US women. Cancer Causes Control 14:519–529
Peplonska B, Lissowska J, Hartman TJ et al (2008) Adulthood lifetime physical activity and breast cancer. Epidemiology 19:226–236
Peters TM, Moore SC, Gierach GL et al (2009a) Intensity and timing of physical activity in relation to postmenopausal breast cancer risk: The prospective NIH-AARP Diet and Health Study. BMC Cancer 9(1):349
Peters TM, Schatzkin A, Gierach GL et al (2009b) Physical Activity and Postmenopausal Breast Cancer Risk in the NIH-AARP Diet and Health Study. Cancer Epidemiol Biomark Prev 18:289–296
Pisani P (2008) Hyper-insulinaemia and cancer, meta-analyses of epidemiological studies. Arch Physiol Biochem 114:63–70
Pugeat M, Crave JC, Elmidani M et al (1991) Pathophysiology of sex hormone binding globulin (SHBG): Relation to insulin. J Steroid Biochem Mol Biol 40:841–849
Renehan AG, Tyson M, Egger M et al (2008) Body-mass index and incidence of cancer: A systematic review and meta-analysis of prospective observational studies. Lancet 371:569–578
Rintala PE, Pukkala E, Paakkulainen HT et al (2002) Self-experienced physical workload and risk of breast cancer. Scand J Work Environ Health 28:158–162
Rintala P, Pukkala E, Laara E et al (2003) Physical activity and breast cancer risk among female physical education and language teachers: A 34-year follow-up. Int J Cancer 107:268–270
Rockhill B, Willett WC, Hunter DJ et al (1999) A prospective study of recreational physical activity and breast cancer risk. Arch Intern Med 159:2290–2296
Rogers CJ, Colbert LH, Greiner JW et al (2008) Physical activity and cancer prevention: Pathways and targets for intervention. Sports Med 38:271–296
Rose DP, Komninou D, Stephenson GD (2004) Obesity, adipocytokines, and insulin resistance in breast cancer. Obes Rev 5:153–165
Ross R, Janssen I (1999) Is abdominal fat preferentially reduced in response to exercise-induced weight loss? Med Sci Sports Exerc 31:S568–S572
Rundle A (2005) Molecular epidemiology of physical activity and cancer. Cancer Epidemiol Biomark Prev 14:227–236
Ryan AS (2000) Insulin resistance with aging: Effects of diet and exercise. Sports Med 30:327–346
Schmidt ME, Steindorf K, Mutschelknauss E et al (2008) Physical activity and postmenopausal breast cancer: Effect modification by breast cancer subtypes and effective periods in life. Cancer Epidemiol Biomark Prev 17:3402–3410
Schmitz KH, Lin H, Sammel MD et al (2007) Association of physical activity with reproductive hormones: The Penn Ovarian Aging Study. Cancer Epidemiol Biomark Prev 16:2042–2047
Schmitz KH, Warren M, Rundle AG et al (2008) Exercise effect on oxidative stress is independent of change in estrogen metabolism. Cancer Epidemiol Biomark Prev 17:220–223
Schnohr P, Gronbaek M, Petersen L et al (2005) Physical activity in leisure-time and risk of cancer: 14-year follow-up of 28, 000 Danish men and women. Scand J Public Health 33:244–249
Sesso HD, Paffenbarger RS Jr, Lee IM (1998) Physical activity and breast cancer risk in the College Alumni Health Study (United States). Cancer Causes Control 9:433–439
Shin A, Matthews CE, Shu XO et al (2009) Joint effects of body size, energy intake, and physical activity on breast cancer risk. Breast Cancer Res Treat 113:153–161
Shoff SM, Newcomb PA, Trentham-Dietz A et al (2000) Early-life physical activity and postmenopausal breast cancer: Effect of body size and weight change. Cancer Epidemiol Biomark Prev 9:591–595
Sieri S, Krogh V, Bolelli G et al (2009) Sex hormone levels, breast cancer risk, and cancer receptor status in postmenopausal women: The ORDET cohort. Cancer Epidemiol Biomark Prev 18:169–176
Silvera SA, Jain M, Howe GR et al (2006) Energy balance and breast cancer risk: A prospective cohort study. Breast Cancer Res Treat 97:97–106
Slattery ML, Edwards S, Murtaugh MA et al (2007) Physical activity and breast cancer risk among women in the southwestern United States. Ann Epidemiol 17:342–353
Sprague BL, Trentham-Dietz A, Newcomb PA et al (2007) Lifetime recreational and occupational physical activity and risk of in situ and invasive breast cancer. Cancer Epidemiol Biomark Prev 16:236–243
Stattin P, Soderberg S, Biessy C et al (2004) Plasma leptin and breast cancer risk: A prospective study in northern Sweden. Breast Cancer Res Treat 86:191–196
Steindorf K, Schmidt M, Kropp S et al (2003) Case-control study of physical activity and breast cancer risk among premenopausal women in Germany. Am J Epidemiol 157:121–130
Surmacz E (2007) Obesity hormone leptin: A new target in breast cancer? Breast Cancer Res 9(1):301
Suzuki S, Kojima S, Tokudome S et al (2008) Effect of physical activity on breast cancer risk: Findings of the Japan collaborative cohort study. Cancer Epidemiol Biomark Prev 17:3396–3401
Szlosarek P, Charles KA, Balkwill FR (2006) Tumour necrosis factor-alpha as a tumour promoter. Eur J Cancer 42:745–750
Taioli E, Barone J, Wynder EL (1995) A case-control study on breast cancer and body mass. Eur J Cancer 31A:723–728
Tehard B, Friedenreich CM, Oppert JM et al (2006) Effect of physical activity on women at increased risk of breast cancer: Results from the E3N cohort study. Cancer Epidemiol Biomark Prev 15:57–64
Thompson HJ, Jiang W, Zhu Z (2009) Candidate mechanisms accounting for effects of physical activity on breast carcinogenesis. IUBMB Life 61:895–901
Thune I, Brenn T, Lund E et al (1997) Physical activity and the risk of breast cancer. NEJM 336:1269–1275
Tworoger SS, Eliassen AH, Kelesidis T et al (2007a) Plasma adiponectin concentrations and risk of incident breast cancer. J Clin Endocrinol Metab 92:1510–1516
Tworoger SS, Missmer SA, Eliassen AH et al (2007b) Physical activity and inactivity in relation to sex hormone, prolactin, and insulin-like growth factor concentrations in premenopausal women - exercise and premenopausal hormones. Cancer Causes Control 18:743–752
Ueji M, Ueno E, Osei-Hyiaman D et al (1998) Physical activity and the risk of breast cancer: A case-control study of Japanese women. J Epidemiol 8:116–122
Uray IP, Brown PH (2006) Prevention of breast cancer: Current state of the science and future opportunities. Expert Opin Investig Drugs 15:1583–1600
Van Gils CH, Peeters PH, Schoenmakers MC et al (2009) Physical activity and endogenous sex hormone levels in postmenopausal women: A cross-sectional study in the Prospect-EPIC Cohort. Cancer Epidemiol Biomark Prev 18:377–383
Velthuis MJ, Schuit AJ, Peeters PH et al (2009) Exercise program affects body composition but not weight in postmenopausal women. Menopause 16:777–784
Verkasalo PK, Thomas HV, Appleby PN et al (2001) Circulating levels of sex hormones and their relation to risk factors for breast cancer: A cross-sectional study in 1092 pre- and postmenopausal women (United Kingdom). Cancer Causes Control 12:47–59
Verloop J, Rookus MA, van der Kooy K et al (2000) Physical activity and breast cancer risk in women aged 20-54 years. J Natl Cancer Inst 92:128–135
Vona-Davis L, Howard-McNatt M, Rose DP (2007) Adiposity, type 2 diabetes and the metabolic syndrome in breast cancer. Obes Rev 8: 395–408
Wang Y, Lam KS, Xu A (2007) Adiponectin as a negative regulator in obesity-related mammary carcinogenesis. Cell Res 17:280–282
Warburton DE, Katzmarzyk PT, Rhodes RE et al (2007) Evidence-informed physical activity guidelines for Canadian adults. Can J Public Health 98(Suppl 2):S16–S68
Wetmore CM, Ulrich CM (2006) Mechanisms associating physical activity with cancer incidence: Exercise and immune function. In: McTiernan A (ed) Cancer prevention and management through exercise and weight control. CRC Press Taylor & Francis, Boca Raton, FL
Woolcott CG, Courneya KS, Boyd NF et al (2010) Mammographic density change with one year of aerobic exercise among postmenopausal women: a randomized controlled trial. Cancer Epidemiol Biomark Prev 19:1112–1121
World Cancer Research Fund and the American Institute for Cancer Research (2007) Food, nutrition, physical activity, and the prevention of cancer: A Global perspective. American Institute for Cancer Research, Washington, DC
Wyrwich KW, Wolinsky FD (2000) Physical activity, disability, and the risk of hospitalization for breast cancer among older women. J Gerontol A Biol Sci Med Sci 55:M418–M421
Wyshak G, Frisch RE (2000) Breast cancer among former college athletes compared to non-athletes: A 15-year follow-up. Br J Cancer 82: 726–730
Xue F, Michels KB (2007) Diabetes, metabolic syndrome, and breast cancer: A review of the current evidence. Am J Clin Nutr 86:s823–s835
Yager JD, Davidson NE (2006) Estrogen carcinogenesis in breast cancer. N Engl J Med 354:270–282
Yang D, Bernstein L, Wu AH (2003) Physical activity and breast cancer risk among Asian-American women in Los Angeles: A case-control study. Cancer 97:2565–2575
You T, Berman DM, Ryan AS et al (2004) Effects of hypocaloric diet and exercise training on inflammation and adipocyte lipolysis in obese postmenopausal women. J Clin Endocrinol Metab 89:1739–1746
Yu H, Rohan T (2000) Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst 92:1472–1489
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Berlin Heidelberg
About this chapter
Cite this chapter
Lynch, B.M., Neilson, H.K., Friedenreich, C.M. (2010). Physical Activity and Breast Cancer Prevention. In: Courneya, K., Friedenreich, C. (eds) Physical Activity and Cancer. Recent Results in Cancer Research, vol 186. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-04231-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-642-04231-7_2
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-04230-0
Online ISBN: 978-3-642-04231-7
eBook Packages: MedicineMedicine (R0)