Abstract
Objective
Dural arteriovenous fistulae (DAVF) in the tentorial middle line region are uncommon with specific features and more cognitive disorders than any other region. The purpose of this study is to present clinical characteristics and our experience with endovascular treatment in this specific region.
Methods
During a 20-year period, 94.9% of patients (74/78) underwent endovascular treatment (36 in galenic, 48.6%) (12 in straight sinus, 16.2%) (26 in torcular, 35.1%). There were 63 males and 15 females with mean age of 50 (50 ± 12) years in total of 78 patients. The clinical presentation, angiographic features, treatment strategy, and clinical outcomes were recorded.
Results
Transarterial embolization (TAE) was performed in 89.2% of the 74 patients (66/74), transvenous embolization alone in one patient and mixed approach in seven. Complete obliteration of the fistulas was obtained in 87.5% of the patients (64/74). 71 patients (mean, 56 months) had phone, outpatient, or admission follow-up. The digital subtraction angiography (DSA) follow-up period (25/78, 32.1%) was 13.8 (6–21) months. Two of them (2/25, 8%) had fistula recurrences after complete embolization and were embolized again. The phone follow-up period (70/78, 89.7%) was 76.6 (40–92.3) months. Pre-embolization and post-embolization mRS ≥ 2 were in 44 patients (44/78) and 15 (15/71) patients, respectively. DAVF with internal cerebral vein drainage (OR 6.514, 95% Cl 1.201–35.317) and intracranial hemorrhage (OR 17.034, 95% Cl 1.122–258.612) during TAE were the risk factors for predicting poor outcomes (followed up mRS ≥ 2).
Conclusions
TAE is the first-line treatment for tentorial middle line region DAVF. When pial feeders’ obliteration is difficult to achieve, it should not be forced due to the poor outcomes after intracranial hemorrhage. The cognitive disorders caused by this region were not reversible as reported. It is imperative to enhance the care provided to these patients with cognitive disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tentorial dural arteriovenous fistulae (DAVF) are complex and extremely dangerous lesions. [1,2,3]. According to Lawton et al., the tentorial middle line region DAVF include galenic, straight sinus, and torcular DAVF [1]. They have summarized the pathological anatomy as well as the best surgical strategies for tentorial DAVF. However, endovascular treatment (EVT) is now a better option for DAVF [2, 4, 5] and tentorial middle line region DAVF has a deeper location, more complex angioarchitecture and more cognitive disorders than other region’s DAVF. The authors think it is necessary to summarize the treatment strategies for EVT in this region with a large sample size.
Methods
Data collection and definition
A total 78 tentorial middle line region DAVF were included in this study between 2000 and 2020 at Xuanwu Hospital in Beijing. The patient’s clinical data and follow-up outcomes were collected. All patients were evaluated using the modified Ranking score (mRS) at the preoperative, postoperative and follow-up periods. Poor outcomes were defined as follow-up mRS greater than or equal to 2. Cognitive disorders were defined as dementia, psychiatric symptoms, and hypomnesia. Ocular complaints included diplopia, hypopsia, and conjunctival congestion. A small percentage of DAVF patients were discovered by accident as a result of other diseases or routine checkup. Other diseases included intracranial aneurysms, intracranial tumors, pulsing mass in the scalp and spinal vascular malformations. Admission, outpatient and phone follow-up were all included. We investigated the outcomes and complications of each treatment modality. The local ethics committee of our organization gave its approval to this study.
Statistical analysis
SPSS 26.0 was used for statistical analysis. Means and standard deviations were used to describe continuous variables, while counts and percentages were used to present categorical variables. Fisher exact test and Chi-square test was performed to test significance of associations between categorical variables. Poor outcomes and cognitive disorders were predicted using univariate and multivariate logistic regression analyses. Significant results were defined as 2-sided P values < 0.05.
Results
Presentation
There were 78 patients with adult DAVF in the tentorial middle line region, including galenic (39/78, 50%), straight sinus (12/78, 15.4%) and torcular DAVF (27/78, 34.6%) (Table 1). Except for hydrocephalus (P = 0.007), there were no statistically significant differences between the galenic group and the straight sinus-torcular group. The mean patient age was 50 ± 12 years and 63 were male (63/78, 80.8%). The median duration of symptoms was 3 months. 67 patients (67/78, 85.9%) presented with related symptoms and 11 patients (11/78, 14.1%) were without symptoms or found incidentally. Three patients with galenic DAVF were discovered during a routine checkup, and three others were discovered by chance due to a pulsing mass in the scalp. In straight sinus DAVF, one patient was found accidentally during a DSA examination for spinal vascular malformation, and the other was identified during a routine checkup. Torcular DAVF was found by chance in two patients as a result of intracranial aneurysms and one as a result of an intracranial tumor. The most common symptoms of the tentorial middle line region DAVF were cognitive disorders (29/78, 37.2%) (16 in galenic, 16/39, 41%) (7 in straight sinus, 7/12, 58.3%) (6 in torcular, 6/27, 22.2%) followed by headache (26/78, 33.3%) and intracranial hemorrhage (19/78, 24.4%) (7 in galenic, 7/39, 17.9%) (4 in straight sinus, 4/12, 33.3%) (8 in torcular, 8/27, 29.6%). When admitted, 41 patients’ mRS ≥ 2 (41/78, 52.6%) (22 in galenic, 22/39, 56.4%) (8 in straight sinus, 8/12, 66.7%) (11 in torcular, 11/27, 40.7%).
Straight sinus occlusion or bilateral transverse sinus occlusion (thrombus) were found in 20.5% of the patients (16/78) (7 in galenic, 7/39, 17.9%) (5 in straight sinus, 5/12, 41.7%) (4 in torcular, 14.8%). Tentorial middle line region DAVF with internal cerebral vein drainage was found to be a risk factor for the onset of cognitive disorders in a multivariate analysis (Table 2) (OR 7.189, 95% Cl 1.787–28.923).
Angioarchitecture
The majority of the DAVF had numerous arterial feeders as well as venous drainage (Table 3). The most common arterial feeds were branches from the occipital artery (OA) (71.8%), followed by branches from the middle meningeal artery (MMA) (67.8%), the posterior meningeal artery (PMA) (52.5%), tentorial branches from the superior cerebellar artery (SCA) and posterior cerebral artery (PCA) (48.7%), and the tentorial artery originating from the meningohypophyseal trunk (MHT) (47.4%). Other arterial feeders included branches from the anteroinferior cerebellar artery (AICA) and posteroinferior cerebellar artery (PICA) (11.1%), the ascending pharyngeal artery (AphA) (12.8%), the posterior auricular artery (PAA) (2.6%), the superficial temporal artery (STA) (12.8%) and branches of the anterior cerebral artery (ACA) (3.8%).
Most of the tentorial middle line region DAVF were high grade (Borden type II or III). A few torcular DAVF had direct venous drainage to the straight sinus, vein of Galen and internal cerebral vein. The drainage veins included the vein of Galen (66.7%), the internal cerebral vein (39.7%), cortical and cerebellar veins (48.7%), the transverse sinus (21.8%) and the cavernous sinus (5.1%).
Treatment and outcomes
74 patients (74/78) underwent EVT (Table 3) (36 in galenic, 12 in straight sinus, 26 in torcular). Four patients were not treated because they either refused treatment or the interventional approach was difficult. Four intracranial hemorrhages occurred during the embolization and 1 patient died due to the hemorrhage in hospital. One cranial nerve palsy (IX) and two brain infarctions occurred after the embolization. At the follow-up, they were completely symptom-free. Transarterial embolization (TAE) was the most common access route (66/74, 89.2%). Only one torcular DAVF were treated transvenously (1/26), and six torcular DAVF (6/26) were treated with mixed approach. The most common embolization materials were ONYX (61/74, 82.4%), Glubran (24/74, 32.4%), balloon (14/74, 18.9%), and coil (1/74, 1.4%). Complete obliteration of the fistulas was achieved in 87.5% (64/74) (31 in galenic, 31/36, 86.1%) (11 in straight sinus, 11/12, 91.7%) (22 in torcular, 22/26, 84.6%) of patients. Two or more embolizations were performed in 31.3% (20/64) (12 in galenic, 12/31, 38.7%) (8 in torcular, 8/11, 72.7%) of the patients who achieved complete obliteration.
Follow-up
71 patients (91%) (mean, 56 months) (34 in galenic, 34/39, 87.2%) (12 in straight sinus, 12/12, 100%) (25 in torcular, 25/27, 92.6%) had phone, outpatient, or admission follow-up. The DSA follow-up period (25/78, 32.1%) was 13.8 (6–21) months. Two of them (2/25, 8%; both in Galen; 1 month and 3 years after embolization) had fistula recurrences after complete embolization and were embolized again. The phone follow-up period (70/78, 89.7%) was 76.6 (40–92.3) months. One patient died while being treated in the hospital, and six patients were lost to follow-up. 75% (3/4) of the untreated patients remained stable but experienced cognitive disorders. 84.5% (60/71) (28 in galenic, 10 in straight sinus, 22 in torcular) of patients had related symptoms at presentation: when patients were followed up, 43.3% (26/60) (9 in galenic, 9/28, 32.1%) (4 in straight sinus, 4/10, 40%) (13 in torcular, 13/22, 59.1%) had complete symptom resolution, 8.3% (5/60) (1 in galenic, 4 in torcular) reported worsening symptoms. One of the patients’ symptoms (in torcular) deteriorated as a result of hemorrhaging during TAE. The rest of the patients (29/60) remained stable. 89.7% (26/29) (18 in galenic, 18/28, 64.3%) (6 in straight sinus, 6/10, 60%) (5 in torcular, 5/22, 22.7%) of the stable patients still had cognitive disorders. When followed up, 15 patients’ mRS was greater than or equal to 2 (15/71, 21.1%) (6 in galenic, 6/34, 17.6%) (3 in straight sinus, 3/12, 25%) (6 in torcular, 6/25, 24%). Tentorial middle line region DAVF with internal cerebral vein drainage (OR 6.514, 95% Cl 1.201–35.317) and intracranial hemorrhage (OR 17.034, 95% Cl 1.122–258.612) during embolization were the risk factors for predicting poor outcomes (Table 4).
Discussion
Treatment
In our facility, TAE is the first-line treatment for the tentorial middle line region DAVF. TAE pathways include the MMA, OA, PCA, AphA, and PMA. Transvenous embolization (TVE) is as an adjuvant treatment. The typical interventional procedures of tentorial middle line region DAVF were illustrated (Figs. 1, 2, 3, 4).
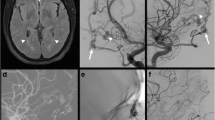
Galenic DAVF. A Sagittal high-resolution magnetic resonance imaging (HRMRI) showing the dilated vein of Galen and straight sinus. Note enlargement of the lateral ventricle. B Anteroposterior view of the right external carotid artery (ECA) angiogram demonstrating tentorial midline region DAVF with multiple artery supplies. C, D Lateral view of the left internal carotid artery (ICA) and the left ECA angiogram showing arterial supply to the fistula from the left pericallosal artery (C, yellow arrow), MMA (D, yellow arrow) and OA (D, blue arrow) converging into the mural channel with the dilated vein of Galen and straight sinus drainage. Note the mural channels (D, white arrows). E, F Super-selective injection through pericallosal artery (E). TAE via pericallosal artery using Glubran was performed. Note the glue cast (F, white arrow). G–I Super-selective injection through left falcine artery from the MMA (G). TAE via falcine artery using ONYX was performed. Note the ONYX cast in the mural channels around the vein of Galen (H, white arrows) and the ONYX not completely occluded the vein. J There is no residual shunting. 4 years after the embolization, the patient complained of mild hypomnesia, but the severe headache she had before the operation was gone. She was satisfied with the results of the treatment
Straight sinus DAVF. A Axial T2 MRI showing increased signal in the bilateral basal ganglia. B Anteroposterior view of the vertebral artery (VA) angiogram demonstrating tentorial midline region DAVF. C–E Lateral view of the right VA (C) and left ECA (D, E) angiogram demonstrating arterial supply to the fistula (C, yellow arrow) from the PCA, the SCA, the meningeal branches of OA (D, yellow arrow) and posterior branches of the MMA (E, yellow arrow and white arrows) with the reflux to the straight sinus, inferior sagittal sinus and internal cerebral vein (D, white arrows). Note the occlusion of the straight sinus. F Super-selective injection through posterior branches of the MMA. G TAE via MMA using ONYX was performed. Be careful not to allow ONYX reflux to vein of Galen. H Posterior angiogram showing no residual fistula. I, J The angiograms 1 year after the embolization showing no recurrence. The patient still complains of hypomnesia and becomes agitated, but his condition has significantly improved since the operation
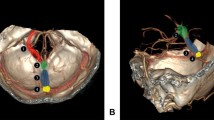
Torcular DAVF. A Axial computer tomography (CT) showing the left temporal lobe hemorrhage. B Anteroposterior view of the right ECA angiogram demonstrating tentorial midline region DAVF. Note the bilateral transverse sinuses occlusion (late venous phase). C, D Lateral view of the left ECA angiogram showing arterial supply to the fistula from the MMA (C, yellow arrows), the AphA (D, yellow arrow) with the straight sinus, vein of Galen (C, white arrow), the superior sagittal sinus (C, black arrow) and vein of Trolard (C, blue arrow) drainage. The left MHT, PMA, SCA also supplied the fistula (not shown). E Balloon-dilated occluded right transverse sinus was performed. F–H Transvenous balloon (F, location of the torcular herophili, white arrow)-assisted ONYX embolization was performed via MMA (G) and AphA (H). I After complete embolization of the fistula, DSA on late venous phase showing patency of right transverse-sigmoid sinus drainage. J–L The angiograms 2 years after the treatment showing no residual shunting. Related headache and tinnitus completely disappeared
Torcular DAVF. A Anteroposterior view of the right ECA angiogram demonstrating tentorial midline region DAVF. Note the right transverse sinuses occlusion. B, C Lateral view of the right ECA and VA angiogram showing arterial supply to the fistula from the MMA, the OA, the PAA and the PCA. D Super-selective injection through pial branches from PCA. TAE via PCA using Glubran was performed. E–H Transvenous balloon (E, lateral view)-assisted ONYX embolization was performed via MMA (F, G) and no residual shunt was left (H). Related ocular complaints almost disappeared 3 years after the embolization
Tentorial DAVF are often with pial arterial supply [1, 2]. Before fistula embolization through dural feeders, Wu et al. recommended obliterating the pial feeding arteries to reduce the risk of hemorrhage [6]. However, four intracranial hemorrhages happened when obliterating the pial feeding arteries and the patients had bad outcome (OR 17.034, 95% Cl 1.122–258.612). When pial feeders’ obliteration is difficult to achieve, it should not be forced. The second choice is to reduce the blood flow reflux to the deep venous system and cortical veins.
In general, we were able to achieve Cognard degradation in the partially embolized patients (Cognard III or IV to Cognard I or IIa). Following that, we recommend that patients be readmitted to the hospital for DSA after 1 to 3 months to see if they can be re-intervened to complete embolization. If the intervention still fails, the patient is advised to have gamma knife therapy [7].
Galenic DAVF
Early on, combined endovascular and surgical treatment was the first-line treatment for DAVF involving the deep venous system [1, 8, 9]. At present, TAE has the most effective treatment modality for galenic DAVF [10,11,12]. Only one case of galenic DAVF was treated with mix approach in our center. In this case, TVE was performed via straight sinus, with a coil placed in the dilated vein of Galen to reduce blood flow. The embolization was then achieved with TAE via MMA using ONYX.
According to Kim et al., mural channels were described as tubular structures that were isolated from the sinus’s main lumen and into which feeders converged [13]. We discovered a number of DAVF near the vein of Galen with similar angioarchitecture (Fig. 1D, white arrows) [14]. Several arterial feeders converged into the channel. TAE administered through the arterial feeders to embolize the channels could result in complete embolization. There is no need to obstruct the entire non-functional vein of Galen (Fig. 1H, white arrows).
Straight sinus DAVF
Straight sinus DAVF is sometimes associated with straight sinus occlusion [15] and often with fragile pial vein drainage [1, 12] which prevents TVE. TAE is still the first-line treatment.
We believe there are two types of straight sinus DAVF, which resembles the DAVF in the sinus region: sinus type and sinus wall type. The feeders directly converging into the sinus, with or without reflux, are referred to as sinus type. Sinus wall type refers to feeders that are isolated from the sinus's main lumen and reflux to an adjacent cortical vein, such as the superior vermian vein in straight sinus region, due to the clot of the main sinus. [1]
In the illustrated case (sinus type), several arterial feeders directly converged into the straight sinus and refluxed into the deep venous with obstruction of the straight sinus (Fig. 2). In this particular type of straight sinus DAVF, complete occlusion of the fistula could be easily achieved by completely occluding the non-functional straight sinus.
Torcular DAVF
TAE, TVE, and mixed approach are all used to treat torcular herophili DAVF [12, 16, 17]. TAE alone cannot always achieve complete occlusion of the fistula. TVE may be performed as an adjuvant method. In the illustrated case (Fig. 3), a balloon was used to recanalize the occluded right transverse sinuse, and transvenous balloon-assisted ONYX embolization was performed via MMA and AphA. It is not recommended to occlude the entire straight sinus in order to achieve complete occlusion. Although in this case, the patient’s outcome was good. However, without the high blood flow, the recanalized transverse sinus is more likely to occlude again. In this case, we recommend partial embolization of the fistula rather than occluding the venous structure, which still functions normally.
For torcular DAVF in which the artery feeders confluence at one point of the sinuses or a venous lake next to the sinuses, ONYX embolization can be performed by positioning the balloon directly at the torcular herophili via the TVE alone.
Prognosis
Tentorial middle line region DAVF induces a higher rate of thalamic dementia because of thalamic venous congestion (Table 3) [1, 10, 18,19,20]. In our study, the most common symptoms of the tentorial middle line region DAVF were cognitive disorders (29/78, 37.2%) (16 in galenic, 16/39, 41%) (7 in straight sinus, 7/12, 58.3%) (6 in torcular, 6/27, 22.2%). Although it is reported that related symptoms are potentially reversible [10, 18], when patients were followed up, 89.7% (26/29) (18 in galenic, 18/28, 64.3%) (6 in straight sinus, 6/10, 60%%) (5 in torcular, 5/22, 22.7%) still had cognitive disorders. Since the follow-up period is long enough, we believe the neurological deficits caused by DAVF are permanent. When we followed up with phone calls, we discovered that 5 patients (5/29, 17.2%) died as a result of a car accident when driving. We believe the tragedy was caused by cognitive disorders. Family members should pay more attention to the patients.
Limitations
This is a non-randomized retrospective single-center study. Many patients or family members described the patient’s symptoms over the phone during the most recent follow-up. It may have an effect on the accuracy with which doctors evaluate patients. Regular follow-up procedures included both MRI and DSA. Peng Zhang, the chief physician, reviewed the MRIs that were typically done in the outpatient clinic. DSA reviews were only performed as necessary. Annual MRIs are advised for follow-up, and angiography is still the gold standard for a precise diagnosis of complete dAVF obliteration [7, 21]. However, only 32.1% of all patients have an DSA re-examination. In this study, a number of patients were followed up using MRI [22,23,24], which may reduce the detection of recurrence fistulas.
Conclusion
Most patients with tentorial middle region DAVF are symptomatic at presentation. Most of them have cortical venous drainage. Drainage to the internal cerebral vein is associated with cognitive disorders. TAE is the first-line treatment for this region. When pial feeders’ obliteration is difficult to achieve, it should not be forced due to the poor outcomes after intracranial hemorrhage.
Data availability
The data are available from the corresponding author on reasonable request.
Abbreviations
- DAVF:
-
Dural arteriovenous fistulae
- DSA:
-
Digital subtraction angiography
- EVT:
-
Endovascular treatment
- mRS:
-
Modified Ranking score
- OA:
-
Occipital artery
- MMA:
-
Middle meningeal artery
- PMA:
-
Posterior meningeal artery
- SCA:
-
Superior cerebellar artery
- PCA:
-
Posterior cerebral artery
- MHT:
-
Meningohypophyseal trunk
- AICA:
-
Anteroinferior cerebellar artery
- PICA:
-
Posteroinferior cerebellar artery
- AphA:
-
Ascending pharyngeal artery
- PAA:
-
Posterior auricular artery
- STA:
-
Superficial temporal artery
- ACA:
-
Anterior cerebral artery
- TAE:
-
Transarterial embolization
- TVE:
-
Transvenous embolization
References
Lawton MT, Sanchez-Mejia RO, Pham D, Tan J, Halbach VV (2008) Tentorial dural arteriovenous fistulae: operative strategies and microsurgical results for six types. Neurosurgery 62(3 Suppl 1):110–124. https://doi.org/10.1227/01.neu.0000317381.68561.b0
Su X, Fan X, Ma Y, Wang J, Wang Y, Zhang H (2022) Diagnosis and treatment of a dural arteriovenous fistula involving the superior petrosal vein. World Neurosurg. https://doi.org/10.1016/j.wneu.2022.08.065
Lewis AI, Tomsick TA, Tew JM Jr (1994) Management of tentorial dural arteriovenous malformations: transarterial embolization combined with stereotactic radiation or surgery. J Neurosurg 81(6):851–859. https://doi.org/10.3171/jns.1994.81.6.0851
Puffer RC, Daniels DJ, Kallmes DF, Cloft HJ, Lanzino G (2012) Curative Onyx embolization of tentorial dural arteriovenous fistulas. Neurosurg Focus 32(5):E4. https://doi.org/10.3171/2011.12.Focus11323
Baharvahdat H, Ooi YC, Kim WJ, Mowla A, Coon AL, Colby GP (2020) Updates in the management of cranial dural arteriovenous fistula. Stroke Vasc Neurol 5(1):50–58. https://doi.org/10.1136/svn-2019-000269
Wu Q, Zhang XS, Wang HD et al (2016) Onyx embolization for tentorial dural arteriovenous fistula with pial arterial supply: case series and analysis of complications. World Neurosurg 92:58–64. https://doi.org/10.1016/j.wneu.2016.04.033
Cifarelli CP, Kaptain G, Yen CP, Schlesinger D, Sheehan JP (2010) Gamma knife radiosurgery for dural arteriovenous fistulas. Neurosurgery 67(5):1230–1235. https://doi.org/10.1227/NEU.0b013e3181eff6f7
Barnwell SL, Halbach VV, Higashida RT, Hieshima G, Wilson CB (1989) Complex dural arteriovenous fistulas. Results of combined endovascular and neurosurgical treatment in 16 patients. J Neurosurg 71(3):352–358. https://doi.org/10.3171/jns.1989.71.3.0352
Halbach VV, Higashida RT, Hieshima GB, Wilson CB, Hardin CW, Kwan E (1989) Treatment of dural fistulas involving the deep cerebral venous system. Am J Neuroradiol Mar-Apr 10(2):393–399
Holekamp TF, Mollman ME, Murphy RK et al (2016) Dural arteriovenous fistula-induced thalamic dementia: report of 4 cases. J Neurosurg 124(6):1752–1765. https://doi.org/10.3171/2015.5.Jns15473
Guedin P, Gaillard S, Boulin A et al (2010) Therapeutic management of intracranial dural arteriovenous shunts with leptomeningeal venous drainage: report of 53 consecutive patients with emphasis on transarterial embolization with acrylic glue. J Neurosurg 112(3):603–610. https://doi.org/10.3171/2009.7.Jns08490
Tong D, Chen X, Lv X, Li K, Xu K, Yu J (2019) Current status of endovascular treatment for dural arteriovenous fistulae in the tentorial middle region: a literature review. Acta Neurol Belg 119(1):5–14. https://doi.org/10.1007/s13760-018-1044-3
Kim J, Kim BM, Park KY et al (2022) Angioarchitectural analysis of arteriovenous shunts in dural arteriovenous fistulas and its clinical implications. Neurosurgery 91(5):782–789. https://doi.org/10.1227/neu.0000000000002121
Fournier D, Rodesch G, Terbrugge K, Flodmark O, Lasjaunias P (1991) Acquired mural (dural) arteriovenous shunts of the vein of Galen Report of 4 cases. Neuroradiology 33(1):52–55. https://doi.org/10.1007/bf00593335
Pu J, Si X, Ye R, Zhang B (2017) Straight sinus dural arteriovenous fistula presenting with reversible parkinsonism: A case report and literature review. Medicine (Baltimore) 96(49):e9005. https://doi.org/10.1097/md.0000000000009005
Takada S, Isaka F, Nakakuki T, Mitsuno Y, Kaneko T (2015) Torcular dural arteriovenous fistula treated via stent placement and angioplasty in the affected straight and transverse sinuses: case report. J Neurosurg 122(5):1208–1213. https://doi.org/10.3171/2014.12.Jns141374
Koutsouras GW, Rahmani R, Schmidt T, Silberstein H, Bhalla T (2018) Coil and Onyx embolization of a torcular herophili dural arteriovenous fistula in a full-term neonate with advanced heart failure using a transumbilical approach. J Neurosurg Pediatr 23(1):80–85. https://doi.org/10.3171/2018.6.Peds1819
Carrasco R, Pascual JM (2017) Letter to the Editor: Dural arteriovenous fistula: a clinical model of thalamic dementia? J Neurosurg 126(3):1020–1022. https://doi.org/10.3171/2016.7.Jns161826
Chen PM, Olson SE, Handwerker J (2020) Bithalamic lesions: cranial dural arteriovenous fistula manifesting as thalamic dementia. Stroke 51(12):e355–e358. https://doi.org/10.1161/strokeaha.120.030576
Cascio Rizzo A, Bonaffini N, Bove R et al (2021) Clinical reasoning: rapidly progressive thalamic dementia. Neurology 96(5):e809–e813. https://doi.org/10.1212/wnl.0000000000011161
Yang HC, Kano H, Kondziolka D et al (2010) Stereotactic radiosurgery with or without embolization for intracranial dural arteriovenous fistulas. Neurosurgery 67(5):1276–1283. https://doi.org/10.1227/NEU.0b013e3181ef3f22
Meckel S, Maier M, Ruiz DS et al (2007) MR angiography of dural arteriovenous fistulas: diagnosis and follow-up after treatment using a time-resolved 3D contrast-enhanced technique. AJNR Am J Neuroradiol 28(5):877–884
Ferro JM, Coutinho JM, Jansen O et al (2020) Dural arteriovenous fistulae after cerebral venous thrombosis. Stroke 51(11):3344–3347. https://doi.org/10.1161/strokeaha.120.031235
Lindgren E, Rentzos A, Hiltunen S et al (2022) Dural arteriovenous fistulas in cerebral venous thrombosis: data from the international cerebral venous thrombosis consortium: data from the international cerebral venous thrombosis consortium. Eur J Neurol 29(3):761–770. https://doi.org/10.1111/ene.15192
Funding
This study was funded by the National Natural Science Foundation of China (No.82101460). The role of the funding body: collection of the data.
Author information
Authors and Affiliations
Contributions
Conception and design: XS, YM. Acquisition of data: XS, ZS, TT, YF, XM, QG. Drafting the article: XS. Critically revising the article: YM, PZ, HZ. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interests
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Su, X., Song, Z., Tu, T. et al. A retrospective study of 78 adult tentorial middle line region dural arteriovenous fistulae. Acta Neurol Belg 123, 1395–1404 (2023). https://doi.org/10.1007/s13760-023-02237-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-023-02237-7