Abstract
Tentorial dural arteriovenous fistulas (TDAVFs) located and occur in the (reflected) double dural layer of the tentorium and its attachments. The vast majority have leptomeningeal venous drainage and tend to cause intracranial hemorrhage or progressive neurological deficits. These lesions are often more challenging to treat than DAVFs at other locations and may require multiple treatment sessions and/or combined approaches. Because of their rarity, the number of reports describing TDAVFs and their endovascular management is limited. The introduction of the nonadhesive liquid agent ethylene-vinyl alcohol represents a paradigm shift regarding the endovascular treatment for TDAVFs. Endovascular treatment is a safe and effective therapy for TDAVFs. Transarterial embolization could be used as a primary therapeutic option for most TDAVFs. When a transarterial approach is not possible or does not result in total lesion occlusion, transvenous or combined approaches can be performed, leading to high angiographic occlusion rates.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
12.1 Introduction
Tentorial dural arteriovenous fistulas (TDAVFs) constitute 4.0–8.4% of all intracranial dural arteriovenous fistulas (DAVFs) [1, 2]. They are deeply located and occur in the (reflected) double dural layer of the tentorium and its attachments [2, 3]. Additionally, most of them are supplied by multiple, small and tortuous arteries [4]. The vast majority have leptomeningeal venous drainage and tend to cause intracranial hemorrhage or progressive neurological deficits [3, 5, 6]. These lesions are often more challenging to treat than DAVFs at other locations and may require multiple treatment sessions and/or combined approaches [3, 6,7,8,9]. Because of their rarity, the number of reports describing TDAVFs and their endovascular management is limited [3].
The introduction of the nonadhesive liquid agent ethylene-vinyl alcohol represents a paradigm shift regarding the endovascular treatment (EVT) for TDAVFs [9]. In addition to superior clinical results, occlusion rates have also improved, making EVT the current preferred therapeutic option in most cases [9].
In the following chapter, we review anatomical aspects, clinical manifestations and endovascular management of the TDAVFs.
12.2 Epidemiology
A meta-analysis involving 377 patients with DAVFs showed that tentorial fistulas occur less frequently than lesions located in the transverse-sigmoid sinus and cavernous sinus regions (8.4% versus 62.6% and 11.9%, respectively) [1]. Huang et al. [4] treated 122 DAVFs between 2005 and 2008, with 13.1% harboring DAVFs at the tentorial region [4]. Thus, tentorial lesions represent a small portion of all intracranial DAVFs.
Regarding distribution, most TDAVFs are diagnosed in middle-aged men [2, 3]. Men comprise between 61.5% and 91.9% of cases [3, 4].
12.3 Anatomical Considerations
TDAVFs are complex lesions surrounded by critical neurovascular structures located deep in the cranial cavity [7]. According to Zhou et al. [2], they represent a unique subtype of lesion because their fistulous connections are located in the tentorial dura mater and not in the sinus wall. The dura mater of the tentorium and its insertions have two layers [3], and dural arteriovenous fistulas from other topographies involve regions where the dura comprises a single layer.
Despite their proximity to the lateral and sigmoid sinuses, TDAVFs are usually considered separately from fistulas involving these sinuses. This distinction appears to be historical and is based on anatomical, clinical and therapeutic differences [3].
An arteriovenous shunt can occur in any region of the tentorium. In the anteroposterior direction, the tentorial fistulas are distributed from the region of the clinoid processes and petrous apex to the torcula [2, 10]. In the mediolateral direction, they may involve medial locations, such as the free edge of the tentorium, edges of the straight sinus and torcula, or may reach the most lateral portion of the tentorium, adjacent to the lateral sinus [2, 10].
12.4 Vascular Supply
Most TDAVFs are vascularized by several arteries that may come from different vascular axes. Several dural branches emerging from the external carotid artery (e.g., middle meningeal artery), the internal carotid artery (e.g., medial tentorial artery), and the vertebrobasilar system (e.g., posterior meningeal artery) can supply these lesions. Some TDAVFs receive recruitment from pial branches [4, 11].
Lawton et al. found that the arterial supply of TDAVFs can originate from six different sources: (a) tentorial artery; (b) middle meningeal artery; (c) posterior meningeal artery; (d) meningeal branches from the pial arteries; (e) scalp arteries; and (f) miscellaneous branches of the external carotid artery. These results demonstrate that branches of the internal carotid artery, external carotid artery, and vertebrobasilar system may be responsible for irrigating the TDAVFs [7].
Liu et al. (2014) published a series of 26 patients with TDAVFs; all lesions were supplied by multiple vessels [12]. According to Tomak et al., 90.9% of TDAVFs were supplied by more than one artery [6]. Of the 14 TDAVFs treated by Huang et al., only one (7.1%) received a contribution from a single arterial pedicle [4]. Wu et al. found that 35.3% of TDAVFs receive a pial supply [11].
12.5 Venous Drainage
TDAVFs are universally associated with leptomeningeal venous drainage. Most series reporting the results of different treatment modalities for TDAVFs highlighted that 100% of the lesions had direct leptomeningeal venous drainage [2, 6, 8, 13, 14]. However, as described by Iwamuro et al., some TDAVFs do not have direct leptomeningeal venous drainage. This review involved 86 cases and showed that only 5.8% of the lesions drained directly into the venous sinuses, including the superior petrous sinus, straight sinus and transverse sinus. The venous drainage of most (94.2%) of the TDAVFs occurred directly to the leptomeningeal veins from the thrombosed venous sinus. In these cases, the obstruction to the sinusal venous flow precipitated the redirection of venous drainage to the leptomeningeal veins, causing the phenomenon of “arterialization” and development of aneurysms in the involved veins [15].
The TDAVFS that drained into a venous sinus represented 7.1% of the cases in the study of Huang et al. [4], 16.1% in the experience of Picard et al. [10], and 23% in the investigation by Byrne and Garcia [3]. In these studies, even when the TDAVFs presented direct venous drainage into a venous sinus, there was a secondary reflux occurred toward the leptomeningeal veins. In our series, all TDAVFs had direct leptomeningeal venous drainage (Fig. 12.1) [16].
A 32-year-old man with a tentorial dural arteriovenous fistula (TDAVF). (a) Coronal magnetic ressonance T2-weighted image of the brain showing a dilated and tortuous flow void signal in the tentorial incisura (white arrows) and brainstem congestion (white arrowheads). (b) An anteroposterior view of the right external carotid artery arteriogram showing a marginal TDAVF supplied by the right middle meningeal artery (MMA) (black arrows) draining to the right lateral mesencephalic vein (white arrowhead) presenting venous ectasia (double black arrowheads). (c) Lateral view of the right internal carotid arteriogram. Additional supply provided by branches from the right medial tentorial artery (white thick arrows). (d) A nondetachable tip microcatheter is navigated in the right MMA. Superselective angiography showing the microcatheter tip in the wedge position (white arrowhead), tortuous and thin distal MMA branches (black arrows) and the level of the spinosum foramen (black arrowhead). (e) Lateral unsubtracted image showing the Onyx cast, reflux along the MMA (double white arrows), anterograde progression just to the fistulous connection (black arrowheads) and filling of the proximal portion of the draining vein (white arrowheads). (f) Postembolization right external carotid artery arteriogram, anteroposterior view, demonstrating the TDAVF total occlusion
The main drainage pathways for TDAVFs are directly related to the location of the arteriovenous shunt, as described by Picard et al. [10]. Lesions located in the medial part of the tentorium drain primarily into cerebellar cortical veins, and their flow can be directed to the galenic system anteriorly or the torcula and lateral sinuses posteriorly. Some lesions can drain into the spinal venous system. The TDAVFs located in the tentorium notch region drain primarily toward the lateral mesencephalic vein and basal vein of Rosenthal, and their flow can be directed to the supratentorial or infratentorial compartment, even reaching the perimedullary veins. The lateral mesencephalic vein is critical in the drainage of lesions located adjacent to the tentorium notch. It communicates the venous system of the supra- and infratentorial compartments connecting Rosenthal’s basal vein to the petrosal system. According to Cannizzaro et al., the lateral mesencephalic vein is involved in the venous drainage of 31% of TDAVFs [9]. Lesions located in the most lateral portion of the tentorium drain into the cortical veins from the inferolateral surface of the temporal and occipital lobes.
12.6 Clinical Presentation
Several angioarchitectural features of TDAFVs have been linked to the development of aggressive clinical behavior. Among them, are leptomeningeal venous drainage, the formation of venous varices and deep drainage toward the galenic system [1,2,3,4,5,6,7,8,9,10].
Because of the effects of venous hypertension, a strong tendency exists for patients to present with intracranial hemorrhage or progressive neurological deficits. Awad et al. reported that TDAVFs have more aggressive neurological behavior than DAVFs in other locations, causing hemorrhage or progressive neurological deficits in 97% of cases [1]. The results of other studies revealed that between 79% and 92% of patients have TDAVFs that determine aggressive neurological behavior and that 38–74% of cases have hemorrhagic presentation [2].
An increasing number of TDAVFs have been diagnosed and treated before their rupture. Several factors can justify this phenomenon, such as the high availability of noninvasive imaging tests and the recognition of venous hypertension as a prominent cause of neurological morbidity. In recent decades, the proportion of patients with TDAVFs with hemorrhagic presentation has dropped from 64.4% (1980–1995) to 43.6% (2006–2014) [9]. In our series, 17 (37.8%) patients reported intracranial hemorrhage [16]. All the patients had received treatment between 2005 and 2019, a period practically similar to the second part of the meta-analysis published by Cannizzaro et al. [9]. A diagnosis before the hemorrhagic manifestation and the subsequent treatment of fistulas are certainly factors that have contributed to the better clinical results obtained in recent decades.
However, the diagnosis of asymptomatic lesions remains infrequent. None of the 19 patients reported by Jiang et al. were asymptomatic, and most (78.9%) exhibited hemorrhage [17]. In the experience of Huang et al., all 14 patients were symptomatic, and 85.7% had intracranial hemorrhage [4]. Even in studies whose hemorrhagic presentation rates were lower, the percentage of asymptomatic patients remained very low. Lawton et al. published the largest series in the literature on the microsurgical treatment of TDAVFs, with 31 patients. Although the bleeding rate found was relatively lower (55%) than that in previous reports, only two (6%) patients were asymptomatic [7].
Our experience encompasses contemporary results. Only three patients were asymptomatic (6.7%), indicating that most TDAVFs continue to be diagnosed when symptomatic [16]. These data confirm that the universal presence of leptomeningeal venous drainage, emphasized by many authors and found in 100% of our patients, determines symptomatic venous hypertension in most patients.
Neurological manifestations resulting from venous hypertension without associated hemorrhage were found in 55.5% (25) of our patients (Fig. 12.2) [16].
A 64-year-old man presenting cervical pain, dysphagia and tetraparesis. (a) Sagittal MRI T2-weighted image of the cranio-cervical junction showing a midline retro cerebellar dilated flow void signal (white thick arrow), medullary and cervical spinal cord patchy edema (white arrowheads) and vessel flow voids dorsally to the spinal cord (double white arrowheads). (b) Lateral view of the right external carotid artery angiogram, late arterial phase, demonstrating a medial type TDAVF supplied solely by the dural branch of the mastoid artery (double white arrows) draining to the ectasia (black asterisk) right inferior vermian vein (black arrowheads). (c) TAA using the DTM in the OCC mastoid branch. Onyx anterograde progression along the mastoid branch (black arrowheads), penetration into proximal portion of the drainage vein (white arrowhead) and at the venous ectasia (double white arrows). (d) Lateral unsubtracted image showing the Onyx cast filling the OCC mastoid branch (black arrowhead), the distal mastoid dural branch (double black arrows), the proximal aspect of the drainage vein (white arrows), and the venous ectasia (white asterisk). (e) Postembolization right external carotid artery arteriogram, lateral view demonstrating the TDAVF total occlusion. (f) Postoperative sagittal MRI T2-weighted image of the cranio-cervical junction showing resolution of the spinal cord congestion and flow voids disappearance
12.7 Classification
Picard et al. proposed a classification system for DAVFs located exclusively in the tentorium [10]. The tributary veins of the tentorial surface were divided into three regions and the TDAVFs were categorized as follows:
-
(a)
Marginal type: fistulas located along the free edge of the tentorium. They have venous drainage through the basilar and lateral mesencephalic veins. Consequently, they may present drainage into infra- or supratentorial leptomeningeal veins or medullary veins. In rare cases, these fistulas can drain into the cavernous sinus and superior ophthalmic vein.
-
(b)
Lateral type: the lesions are located adjacent to the lateral sinus and receive supratentorial venous drainage through veins on the lateral and inferior surface of the temporal and occipital lobes.
-
(c)
Medial type: fistulas are located adjacent to the torcula and straight sinus. Its venous drainage is infratentorial, coming from veins on the surface of the vermis or cerebellar hemispheres. They drain secondarily into the torcula, lateral sinus or straight sinus.
Anatomical grouping facilitated the radiological identification of the TDAVFs by predicting the venous drainage patterns they might develop. Picard’s classification has been the most used by most authors.
To create an algorithm for choosing the best neurosurgical access, Lawton et al. developed a classification system for TDAVFs. Lesions were categorized into six types according to their anatomical location, dural implantation base, involved venous sinus, and direction of venous drainage [7].
Galenic DAVFs (type 1) are located in the midline, on the posterior margin of the tentorial incisura, associated with the vein of Galen as it enters the anterior falcotentorial junction, and their venous drainage can be supratentorial, infratentorial or in both directions. Straight sinus DAVFs (type 2) are located in the midline, along the falcotentorial junction, associated with the straight sinus, with drainage into veins on the inferior surface of the tentorium. Torcular DAVFs (type 3) are located in the midline at the posterior margin of the falcotentorial junction, associated with the torcula and supratentorial venous drainage. Tentorial DAVFs (type 4) are located in the tentorium body, are associated with the tentorial sinus and drain into the occipital (supratentorial) veins. Superior petrosal sinus DAVFs (type 5) are located laterally where the tentorium connects to the middle fossa dura mater and are related to the superior petrosal sinus, draining infratentorially to the petrous vein and its tributaries. Type 6 lesions are called incisural DAVFs. They are located along the free edge of the tentorium, without clear association with a venous sinus, draining into supratentorial veins within and around the cisterna ambiens.
In 2013, Byrne and Garcia proposed a classification system for TDAVFs based on the location of arteriovenous communication [3]. The lesions were divided into two types: (a) dural arteriovenous fistulas in the midline region that could be located in the torcula or falx of the cerebellum and (b) lateral petrotentorial arteriovenous fistulas arranged along the implantation of the tentorium in the petrous bone. The venous drainage patterns found by the authors were similar to the system proposed by Picard et al. [10].
12.8 Treatment
Several therapeutic modalities have been proposed for TDAVFs, such as ligation of the feeding arteries, surgical excision of the fistula, interruption of draining veins, arterial and/or venous embolization, and radiosurgery. Available options can be performed in isolation or in various combinations [6]. However, much debate exists concerning the best treatment option.
Endovascular treatment has become the predominant therapeutic option for most DAVFs because the arterial supply from the external carotid artery can be safely embolized. Additionally, its location on the walls of the dural venous sinuses facilitates its venous access and occlusion. The combination of arterial and venous embolization results in high obliteration rates for most types of DAVFs. However, according to Lawton et al., lesions located in the tentorial region represent an exception [7].
Tentorial dural arteriovenous fistulas have a complex arterial supply. In addition to branches of the external carotid artery, multiple vessels participate in its supply, such as meningeal branches from the internal carotid artery and vertebrobasilar system [7]. These arteries, in addition to being challenging to microcatheterize, are at greater risk when embolized compared with branches originating from the external carotid artery. Because most tentorial dural arteriovenous fistulas drain exclusively into the leptomeningeal veins, venous access has limitations. Microcatheterization of the venous system located deep around the tentorium is challenging [2, 4, 7]. Thus, treatment of TDAVFs may require microsurgery, unlike most other types of DAVFs.
12.8.1 Microsurgical Treatment
Based on the existing concepts that EVT can rarely cure TDAVFs, several authors have defended microsurgery over the last decades as the treatment of choice for these lesions [2, 7, 18, 19].
In 2003, Tomak et al. reported a series of 22 patients with TDAVFs, all Borden type III lesions undergoing endovascular and/or surgical treatment, over a 12-year period. In the early part of the study (1988–1995), the surgical technique used involved disconnecting the arterial supply and draining vein associated with nidal resection. The microsurgical strategy was modified in the most recent period (1995–2000), with only the disconnection of the drainage vein performed without nidal resection. The authors consider that disconnection of the arterial supply and excision of the nidus may be associated with high rates of morbidity and mortality, deeming the procedure unnecessary [6].
More recent publications have shown different types of complications related to microsurgery. Gross and Du described the results of the microsurgical treatment of 14 TDAVFs whose technique used was the simple interruption of the drainage vein. The overall rate of neurological complications was 35.7%. In three cases, transient neurological deficits (cranial nerve palsy or hemiparesis) occurred and one patient developed permanent hemiparesis. One death due to massive intraoperative cerebral edema occurred [20].
Sugiyama et al. published a series of 39 patients with DAVFs who had undergone microsurgical treatment. Ten cases had tentorial lesions. Compared with lesions from other topographies, TDAVFs had higher rates of complications (17.2%; 95% CI 9.7–24.6%) and subtotal angiographic occlusion (8.1%; 95% CI 2.7–13.4%). Cerebral edema after surgery or excessive intraoperative blood loss were the most frequent complications [21].
Although many authors advocate microsurgery as a first-line treatment for TDAVFs, neurological complication rates are considerable [9]. Endovascular treatment, which is less invasive, could become the preferred method if its angiographic occlusion rates are satisfactory [16].
12.8.2 Endovascular Treatment
12.8.2.1 Transvenous Approach
The endovascular treatment of DAVFs using a venous approach has been an efficient option to manage lesions that present direct venous drainage into a dural sinus. In these cases, when the venous sinus is considered excluded from the venous drainage of the supra and infratentorial compartments, it can be occluded.
Most TDAVFs drain exclusively into the leptomeningeal veins. This angioarchitectural characteristic determines that venous access to the fistulous connection point is performed along very dilated, tortuous and thin veins. Venous embolization must be performed to occlude only the portion of the vein immediately adjacent to the fistula, preserving functional venous drainage. The most proximal portion of the drainage vein should be the target of the endovascular occlusion.
Few reports have investigated ETV of TDAVFs using the transvenous approach. The first case was described in 1997 by Kallmes et al. The lesion was occluded with platinum microcoils [22]. In 1999, Deasey et al. described the results of EVT of two TDAVFs using venous access. Lesions drained directly into a venous sinus, an uncommon fact, and were accessed through the internal jugular vein and straight sinus [23]. Tomak et al. reported the results of the transvenous EVT of five TDAVFs. One patient died from ischemia in the posterior fossa after the injection of n-BCA into the petrous vein [6]. Jiang et al. used venous access as a complement to arterial access to treat two TDAVFs. One patient died because of venous rupture during EVOH injection [17]. Wanjberg et al. treated eight patients with TDAVFs. In three of them (37.5%), transvenous access was performed. Two patients were treated exclusively using the venous approach, and one was subjected to combined treatment [14].
Huang et al. advised against transvenous embolization of TDAVFs because of the complex anatomy of the involved veins. Because venous varices often have thin walls, a risk of vascular perforation exists. Additionally, partial or distal occlusion of the draining veins can result in redirection of blood flow to the cortical veins, with a risk of venous hypertension or secondary hemorrhage [4].
Therefore, several authors, including Kallmes et al., do not propose transvenous embolization alone as the primary therapy for most TDAVFs. Instead, this approach should be used in combination with or as an alternative to arterial embolization, microsurgery, or radiosurgery [22].
12.8.2.2 Transarterial Approach
Since the first description of DAVF therapeutic embolization, at the beginning of the 1970s [24], several embolizing agents, such as particles [25], liquid silicone [26], cyanoacrylates [27], and EVOH [28] have been used.
Polyvinyl alcohol (PVA) particles were used for preoperative embolization in several microsurgical series of TDAVFs, decreasing their vascularization [2, 7]. However, the occlusion of a TDAVF after isolated PVA injection is uncommon [6].
Tomak et al. treated 11 patients harboring TDAVFs using the transarterial approach (TAA) with glue injection and reported 45% total angiographic occlusion. The TAA with n-BCA injection led to an increase in the rates of angiographic occlusion in the EVT of TDAVFs. However, less than half of the patients were cured alone using this strategy. Many cases still required complementary microsurgical treatment during the cyanoacrylate era [6].
The shift from polyvinyl alcohol particles to adhesive liquid agents has slightly improved the occlusion rates [6], but the introduction of ethylene-vinyl alcohol has offered a new perspective.
The first cases of TDAVFs treated using EVOH were described from 2006 onward, and the angiographic occlusion rates proved to be encouraging [29]. Huang et al., using only EVOH injection, obtained 85.7% angiographic occlusion in 14 TDAVFs [4]. Onyx injection through the posterior branch of the MMA has become the first therapeutic option for most TDAVFs [3, 4, 8, 9, 11,12,13,14, 17].
12.8.3 Endovascular Treatment Results
The use of EVOH has resulted in a substantial increase in angiographic occlusion rates and has caused changes in treatment strategies for TDAVFs. The proportion of patients treated with microsurgery alone decreased from 38.7% (period 1980–1995) to 20.4% (period 2006–2014). During the same period, the proportion of patients treated using the endovascular route alone has increased from 16.1% to 48.0%. Cannizzaro et al. observed a sustained deviation from the therapeutic option that occurred in the last two decades [9].
The endovascular approach has become the preferred technique to treat TADVFs. In most series, even during the Onyx era, occlusion rates with exclusive EVT rarely exceed 80% [3, 4, 8, 9, 11,12,13, 17]. In a review of 72 TDAVFs subjected to EVT, 86.1% were occluded at the end of the procedure, but patients who required combined surgery were excluded from the analysis [30].
In 2021, we published the largest series reporting the results for patients with TDAVFs who were treated using an endovascular approach and the TAA as a first-line strategy. An isolated TAA was sufficient to occlude 39 (86.7%) TDAVFs (Fig. 12.3). Some factors contributed to the high rate of total occlusion obtained using the TAA.
Hemorrhagic presentation. (a) Axial cranial computed tomography revealing intraparenchymal hemorrhage (black asterisk). (b) An anteroposterior (AP) and (c) lateral view of the left external carotid artery arteriogram showing a lateral TDAVF (white asterisk) supplied by the left middle meningeal artery (MMA) (double black arrows) and the left occipital artery (white arrowhead) draining to the left occiptobasal vein (white arrowhead) presenting venous ectasia (black arrowhead) and the ipsilateral lateral sinus (white arrow). (d) AP unsubtracted image showing the Onyx cast after isolated left MMA embolization. (e) Postembolization left external carotid artery arteriogram, AP view and (f) lateral view demonstrating the TDAVF total occlusion
12.8.4 Importance of the Preferential Use of the Middle Meningeal Artery
The choice of the middle meningeal artery as the preferred access was a determining factor for the high rate of occlusion obtained in several series [3, 4, 8, 9, 11,12,13,14, 17]. This artery has unique characteristics, and even when it does not represent the major vascular supply to the TDAVF, it is recognized as a favorable conduit for EVOH injection.
The MMA is the largest meningeal branch and, consequently, participates in the vascular supply of most DAVFs. Because of the hemodynamic stress caused by the arteriovenous shunt, the MMA often becomes larger than normal [31]. The posterior branch of the middle meningeal artery supplies most TDAVFs and provides direct access to its collecting venous system [9]. Puffer et al. reported that the posterior branch of the MMA has a relatively straight course and is dilated in most TDAVFs [13]. These features allow for selective distal catheterization adjacent to the point of fistulous connection. The distal positioning of the microcatheter, almost always in a wedged position, allows the progression of the EVOH, limiting the amount of reflux.
Even when the MMA has a smaller caliber than other pedicles, it should be chosen as the first option for EVOH injection. The main justification for this option is based on anatomical grounds. The MMA and its branches have a relatively straight course along their dural implantation, making their microcatheterization easier relative to the other branches. The extent of reflux does not determine high risks, such as those existing for arteries located in the subdural space. Even in the presence of extensive reflux, the microcatheter can be safely removed because the MMA has a dural anchor. When difficulty exists in removing the microcatheter, the chances of arterial rupture are still much lower when this meningeal branch is chosen. The risks of occlusion of the normal vessels due to reflux are also much lower. The preference to access the TDAVFs by the MMA (66.7%) was one factor that contributed to the high rate of total occlusion obtained in our series [16].
12.8.5 Middle Meningeal Artery Limitations
The middle meningeal artery has unique characteristics, even when it is not the major supplier for the fistula, it is recognized as a favorable conduit [3, 9, 13, 17]. In most series, the MMA was the preferred and most accessed artery [3, 13, 17, 32].
However, there are some limitations in the use of the MMA. First, there is a risk of complications such as microcatheter retention or cranial nerve palsy due to excessive reflux of Onyx [4, 13, 17, 32]. Additionally, in some cases, the injection must be stopped even if occlusion of the fistula has not occurred. In recent years, new tools, such as detachable tip microcatheters (DTMs) and double-lumen balloons (DLBs), have been used for the EVT of TDAVFs [8, 32, 33]. DTMs can be retrieved, even after prolonged injections in distal branch pedicles, often with significant reflux [32, 33]. The use of DTMs can reduce the risks of microcatheter retention, allowing longer and controlled Onyx injections. The rationale for using DLBs is to block reflux and to favor the anterograde migration of Onyx [8, 34], but the size of the MMA should allow a DLB to be insufflated beyond the level of the spinosum foramen.
Second, many TDAVFs are not vascularized by the MMA. In our experience, most fistulas were supplied by the MMA (39/86.7%) [16]. However, according to some authors, its contribution to the TDAVF supply may vary from 33.3% to 88.8% [3, 4, 7, 8, 13].
Third, some anatomical factors, such as the absence of a “sizable” MMA [13] or an exclusive supply from an excessively tortuous artery [4, 8, 13, 17], sometimes make MMA embolization challenging.
12.8.6 Use of an Alternative Arterial Access
Because some TDAVFs are not nourished by the MMA [3, 7, 8], other arterial feeders, such as the occipital artery (OCC) and posterior meningeal artery (PMA), should be considered. However, due to their excessive tortuosity, distal catheterization can be complicated or even impossible [8, 13]. The OCC is surrounded by loose connective tissue and may be very tortuous and dilated, particularly when it accommodates high flow [8]. Although the intracranial segment of the PMA demonstrates a relatively straight configuration, its extracranial portion is tortuous, likely to accommodate the motility of the neck [35].
In our series, all TDAVFs were supplied by at least one of these arteries: the MMA, OCC or PMA [16]. Consequently, in all patients, one of them could be catheterized. Nine (20%) TDAVFs were treated by exclusive OCC embolization (Fig. 12.4), and the PMA was accessed in four patients (Fig. 12.5). In our experience, when necessary, with the aid of a distal flexible intracranial catheter, positioning the microcatheter or DLB tip inside the OCC mastoid branch or catheterizing the PMA is possible [16, 34]. The introduction of DTMs and DLBs is another factor that has further facilitated TAA execution in arteries other than the MMA [8, 32,33,34].
TAA Onyx injection using DLB. (a) Lateral right occipital artery selective angiogram demonstrating a tentorial TDAVF supplied solely by dural feeders (black arrowheads) from the OCC mastoid branch (black arrow). (b) Tip of the DLB into the mastoid branch (white arrowhead) and anterograde Onyx progression just to the fistulous point and to the “foot” of the drainage vein (black arrowhead). (c) Postoperative lateral right OCC angiogram showing total obliteration of the TDAVF and the OCC patency (black arrows)
TDAVF supplied by the posterior meningeal artery. (a) Oblique left vertebral artery (white arrowhead) selective angiogram demonstrating a medial type tentorial TDAVF (black arrowhead) supplied solely by the posterior meningeal artery (black arrows) draining to the declival vein (white arrow). (b) A nondetachable tip microcatheter is navigated in the left PMA (black arrows). Superselective angiography showing the microcatheter tip in the wedge position, the fistulous point (black arrowhead) and the tortuous drainage vein (white arrow). (c) Oblique unsubtracted image showing the Onyx cast filling the PMA (black arrows), the fistulous connection (black arrowhead) and the proximal aspect of the drainage vein. (d) Postoperative oblique left vertebral angiogram showing total obliteration of the TDAVF and the PMA patency (white arrowhead)
12.8.7 Transvenous and Combined Approaches
A reduced arterial size or excessive tortuosity sometimes make the TAA challenging [4, 8, 13]. These limitations explain why in most EVT series, even in the Onyx era, some TDAVFs are not occluded or treated using the arterial route. The rate of using the TAA in the EVT series varies from 75% to 100% [4, 8, 13, 17, 30]. Puffer et al. obtained 67% of total angiographic occlusion using an isolated TAA with Onyx [13]. Huang et al. described a series of 14 patients harboring TDAVFs treated by transarterial Onyx injection with a 85.7% total angiographic occlusion. They considered the TVA too risky and did not use it for their patients [4]. Until 2020, no series of exclusive TAAs could achieve more than 90% angiographic occlusion [3, 4, 8, 12,13,14, 17].
Despite some successful outcomes [6, 13, 17, 22, 23], the TVA has been avoided because microcatheter navigation along tortuous, dilated, and potentially fragile leptomeningeal veins is considered challenging and risky [4, 6, 17]. However, to achieve higher occlusion rates solely with EVT, in our opinion, the domain of venous access is fundamental. Wanjberg et al. reported that eight TDAVFs were completely occluded after exclusive EVT. Five patients were treated using the TAA with Onyx injection. Two patients were treated using the TVA, and another was treated with combined endovascular access [14].
Isolated transvenous or combined approaches were performed in four (8.8%) patients in our experience, and all controlled TDAVFs presented with occlusion at the 6-month follow-up. Two TDAVFs were treated by TVA as the primary intention because their arterial supply was judged as inaccessible. Incomplete angiographic occlusion after the TAA occurred in two patients, and both required the TVA. Depending on the leptomeningeal vein involved, the positioning of a hyperflexible distal intracranial catheter into the straight or lateral sinus was crucial to provide support for microcatheter navigation just to the “foot of the vein.” We consider that the TVA is a feasible alternative access to treat TDAVFs and should be reserved for situations when arterial access is not possible or insufficient to completely occlude the TDAVF [16].
Only one patient was not treated by an exclusive endovascular approach in our experience. In this patient, a very tortuous MMA originated from the ophthalmic artery (Fig. 12.6). There was no other supply to the TDAVF, and the drainage vein was very dilated and tortuous. Temporal craniectomy followed by direct MMA puncture and Onyx embolization was performed [16]. According to some authors, combined surgical-endovascular techniques can be an alternative for DAVFs that are complicated by a lack of accessibility to an MMA approach [36, 37]. When the TAA is not possible and the TVA is considered high risk, direct MMA puncture should be considered as an alternative approach [16, 36, 37].
Combined surgical-endovascular approach. (a) Oblique right internal carotid artery selective angiogram demonstrating a lateral type tentorial TDAVF supplied solely by the middle meningeal artery (black arrowheads) originating from the ophthalmic artery (black arrows). (b) MMA direct puncture. (c) Oblique unsubtracted image showing the craniectomy and percutaneous MMA access. (d) Superselective angiography showing the microcatheter tip in the wedge position, the fistulous point and the tortuous and dilated drainage vein. (e) Unsubtracted image showing the Onyx cast. (f) Postembolization right internal carotid artery arteriogram, lateral view demonstrating the TDAVF total occlusion
12.8.8 Nonadhesive Liquids as the Preferred Embolic Agent
Tomak et al. treated eleven patients harboring TDAVFs using the TAA with glue injection and reported 45% total angiographic occlusion [6]. However, since the first reports on EVT of TDAVFs with Onyx, angiographic occlusion rates have increased [3, 4, 8, 12,13,14, 16, 17]. Nonadhesive liquids have been the most common material (78.4%) used to treat TDAVFs in the last decade [30], and their advantages over adhesive liquid agents are well established [4, 13, 30, 38]. Recently, other nonadhesive liquid agents, such as Squid (Emboflu, Gland, Switzerland) and Phil (Microvention, Tustin, CA, USA), have been used successfully [8, 30].
We systematically used Onyx as the preferred embolic agent [16]. It was used alone or combined with other agents in all patients except one, who was treated by two sessions with transvenous access. In this patient, the TDAVF was embolized with coils leading to incomplete angiographic occlusion. In the second session, a microcatheter not compatible with dimethyl sulfoxide was used, after subtotal occlusion with coils, glue was injected.
12.8.9 Influence of the Number of Arterial Feeders
TDAVFs are often nourished by multiple vascular groups [4, 7, 8], and only 6.7% of our cases were supplied by a single artery [16]. Liu et al. reported the influence of the number of feeding arteries on the occlusion rates of TDAVFs. According to them, the total occlusion rates using the TAA with Onyx were 85.7%, 53.8%, and 66.7% in the tentorial marginal, lateral, and medial subtypes, respectively. Marginal TDAVFs had fewer feeding arteries and presented higher occlusion rates after the TAA [12]. In our series, all TDAVFs, except one, were completely occluded. The presence of more than four arterial feeders was a predictor of failure for total occlusion after the first treatment session. Other factors, such as bilateral supply and Picard type, were not predictors for occlusion after the first procedure. The high flow secondary to the multiple arterial supply likely causes an increased pressure in the leptomeningeal drainage vein, making it challenging for Onyx to penetrate the shunt during injection into a single arterial pedicle.
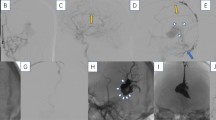
To increase the complete occlusion rates using a single procedure, inspired by the concept of double catheterization to treat pial arteriovenous malformations [39], we have adopted a new strategy in recent years. If a TDAVF was supplied by the MMA and OCC, we performed double catheterization [16, 34]. Depending on the caliber and tortuosity of the MMA, a DTM or a DLB was chosen. Inside the mastoid branch of the OCC, another DLB was positioned. Both arteries were blocked, reducing the flow to the shunt and the pressure inside the vein. Simultaneous Onyx injection occluded these lesions in a single session (Fig. 12.7) [16].
TDAVF supplied by multiple arterial feeders and double catheterization technique. (a, b) An anteroposterior (AP) and lateral view of the right external carotid artery and (c, d) left external carotid artery angiogram. TDAVF (white asterisk) supplied by the middle meningeal (black arrows) and the occipital arteries (black arrowheads) from both sides draining directly to a dilated leptomeningeal vein (white arrowhead). (e) Lateral right external carotid roadmapping image demonstrating the position of the double lumen balloon (DLB) tip into the mastoid branch of the occipital artery. To obtain support for the DLB navigation, the proximal guiding catheter is positioned in the external carotid artery (white arrowhead), the flexible distal access catheter is navigated along a very tortuous and dilated occipital artery as close as possible to the origin of the mastoid branch (white arrow) and the DLB is inflated (double black arrows). (f) Lateral unsubtracted image revealing the position of the flexible distal access catheters in the left middle meningeal artery (black arrowhead) and in the right occipital artery (white arrow). A compatible DSMO microcatheter is positioned distally in the middle meningeal artery (double white arrowheads) and a double lumen balloon is placed inside the mastoid branch (double black arrows). (g) Simultaneous superselective angiography showing the microcatheter position in the middle meningeal artery (white arrowheads) and the DLB in the occipital artery (double black arrows). (h) Unsubtracted image showing the Onyx cast. (i, j) Postoperative bilateral common carotid artery angiogram, AP view, arterial and venous phase demonstrating the TDAVF total occlusion
12.8.10 Clinical Outcomes
Compared with other therapeutic modalities, EVT resulted in lower perioperative morbidity (6%) and greater resolution of symptoms (82%). In addition, the good long-term neurological outcomes were significantly superior (89%). Due to these clinical results, in recent decades, the endovascular approach has become the standard treatment for most TDAVFs [9].
Despite our aggressive endovascular strategy, where no patient needed complementary direct microsurgical treatment, 41 patients (91.1%) presented good neurological outcomes at 6 months. Most patients with symptomatic unruptured TDAVFs improved [16].
12.8.11 Complications
The reported complication rates of EVT varied from 0% to 13.5% [3, 4, 8, 9, 13, 17, 30, 32]. One of the major challenges related to the intra-arterial injection of liquid agents during the embolization of TDAVFs is the possibility of excessive reflux. Several complications have been described resulting from this phenomenon, such as microcatheter retention and/or rupture, cranial nerve palsy and cerebral ischemia. The force required for microcatheter extraction after the injection of liquid agents is variable and depends on factors such as vascular tortuosity, extent of reflux and proximal access support [33].
Anatomical factors influence microcatheter navigation along dural and pial arteries [4, 6, 8, 13]. Tortuosity and reduced caliber can limit distal catheterization [13]. Depending on the microcatheter tip position, forward Onyx progression is limited, increasing the risk of complications related to excessive reflux [4]. Total occlusion of the TDAVF may not occur after injection in a single artery, requiring additional arterial access and increased risks [16].
In our series, seven (15.6%) patients showed clinical complications after EVT. Five of them experienced transient complications. In most of these cases, multiple arteries were catheterized. In multivariable analysis, clinical complications were related to the number of accessed arteries [16].
12.8.12 Cranial Nerve Deficits After Arterial Embolization
Some arteries that supply the tentorial region also participate in the vascular supply of some cranial nerves [35]. Cranial nerve palsy during the arterial injection of EVOH occurs when the embolic agent migrates toward the vascular supply of the nerve called the vasa nervorum [32]. According to Gioppo et al., the rate of cranial neuropathy associated with endovascular treatment of TDAVFs is 1.2% [30].
12.8.13 Middle Meningeal Artery
Immediately adjacent to the spinous foramen, the middle meningeal artery gives rise to a short arterial trunk that divides into a lateral branch (petrosal artery) and a medial branch (cavernous branch to the trigeminal ganglion). The cavernous branch contributes to the supply of the second and third portions of the trigeminal nerve. The petrous branch penetrates the temporal bone and supplies the tympanic segment and geniculate ganglion of the facial nerve [32, 35]. The occlusion of these branches, resulting from the reflux of EVOH during the injection, can cause deficits of the trigeminal and facial nerves (Fig. 12.8) [32, 40, 41].
Marginal TDAVF. Facial palsy due to Onyx reflux. (a) Lateral view of the right external carotid artery angiography showing a marginal TDAVF supplied by the middle meningeal artery (double white arrows) and accessory meningeal artery (white arrowhead). (b) Lateral unsubtracted image demonstrating the Onyx reflux filling retrogradely the middle meningeal artery trunk below the spinosum foramen level (double white arrows) and the accessory meningeal artery trunk (white arrowhead)
To prevent this complication, avoiding Onyx reflux into the petrosal branch is critical [13]. An alternative, is the positioning of a DLB beyond the spinosum foramen level, but the size of the MMA sometimes limits this approach [16].
12.8.14 Medial Tentorial Artery
Despite contributing to the vascular supply in many TDAVFs (50–72%) [4, 7, 8, 42], the medial tentorial artery (MTA) has not been used as a frequent access for the injection of liquid agents. A risk of reflux exists toward the internal carotid artery. Additionally, because the oculomotor and trochlear nerves may derive their blood supply from the MTA, complications such as diplopia may occur [32, 35]. In our series, the MTA supplied 42.2% of the TDAFVs. In only one patient, the MTA was used for Onyx injection, since all fistulas had additional feeding arteries. Transitory diplopia occurred after MMA and MTA Onyx embolization. The MTA was embolized after subtotal occlusion using MMA access. No reflux to the spinosum foramen occurred, and no ischemia was identified on MRI [16]. We recommend that the MTA should be embolized only for TDAVFs for which it is the only feeding artery or if residual filling after embolization occurs by other arterial pedicles. A balloon should be positioned in the internal carotid artery in front of the origin of the MTA. Rooij et al. treated six patients with TDAVFs that were mainly supplied by the tentorial artery. In four patients, the MTA was the only arterial feeder to the fistulas. Three TDAVFs were embolized by glue injection into the MTA with balloon occlusion of the internal carotid artery without complications [42].
12.8.15 Distal Onyx Migration
Onyx migration has been reported during transarterial and transvenous high-flow DAVF embolization [43]. In our experience, this complication occurred in one patient with a lateral TDAVF supplied by six different arterial branches that was embolized by the MMA. During Onyx injection, distal migration occurred. We attribute this complication to the high-flow condition and washout effect related to the multiple arterial feeders. An alternative to avoid this complication is to use Onyx-34 during the initial phases of the injection [44]. During the embolization of pial arteriovenous malformations, double catheterization of the main afferents may decrease flow to the arteriovenous shunt and the risk of Onyx migration [39]. In recent years, when possible, we started to perform double catheterization, and distal venous Onyx migration did not occur [16].
12.8.16 Hemorrhage
Hemorrhagic complications are related to vessel perforation [3, 4], the presence of a pial supply [11], extensive thrombosis of the drainage vein [40], and distal venous occlusion with a residual fistula [17].
Vascular perforation can occur during arterial or venous access. Huang et al. [4] described a series of 14 TDAVFs treated with transarterial injection of EVOH. In one case, arterial perforation occurred during microcatheterization, causing subarachnoid hemorrhage. After embolization through the same artery, subtotal devascularization of the lesion was obtained. The patient evolved uneventfully.
Jiang et al. warned that the migration of liquid embolic agents toward the distal segment of the draining vein can cause venous rupture if there is residual flow in the fistulous connection. These authors reported a fatal complication related to rupture of the draining vein during transvenous injection of EVOH [17].
DAVFs with a pial arterial supply are also called acquired or mixed duropial fistulas. There are rare reports of these lesions [45]. Wu et al. described the results of transarterial injection of EVOH in 17 patients with TDAVFs [11]. Six TDAVFs (35.3%) received an arterial supply from the pial branches. In this series, no DAVF from other topographies received pial vascularization, only tentorial lesions. During embolization, two patients with TDAVFs with a pial supply had hemorrhage. The authors believed that high-flow TDAVF induces the development of pial arteriovenous fistulas. During EVOH injection through a meningeal branch, occlusion of the draining vein and dural arterial supply of the TDAV without involvement of the pial fistula can be observed. Restriction of venous drainage from the pial fistula may lead to hemorrhage. It is postulated that the pial arterial supply may be a risk factor for intraoperative hemorrhage during the embolization of meningeal branches with EVOH. To avoid this complication, endovascular occlusion of the pial supply is suggested before embolization of the dural branches.
After total or subtotal occlusion of a TDAVF with direct leptomeningeal venous drainage, a severe complication may arise. Extensive thrombosis of the arterialized draining vein can cause venous infarction or hemorrhage [40, 46]. Borha et al. reported a bleeding complication attributed to massive thrombosis of the draining vein that occurred 4 days after embolization of a lateral type TDAVF using EVOH and n-BCA [46]. To prevent this type of complication, Cognard et al. recommended the postoperative use of intravenous heparin for 48 h and then low molecular weight heparin at a preventive dose for 15–30 days to prevent venous drainage thrombosis. However, in their series, one TDAVF had postembolization hemorrhage secondary to extensive venous thrombosis [40]. This issue remains controversial, and we do not use routine anticoagulation after treatment [16].
12.9 Conclusions
Endovascular treatment is a safe and effective therapy for TDAVFs. A TAA could be used as a primary therapeutic option for most TDAVFs. When a TAA is not possible or does not result in total lesion occlusion, transvenous or combined approaches can be performed, leading to high angiographic occlusion rates.
References
Awad IA, Little JR, Akarawi WP, Ahl J. Intracranial dural arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg. 1990;72:839–50.
Zhou LF, Chen L, Song DL, et al. Tentorial dural arteriovenous fistulas. Surg Neurol. 2007;67:472–82.
Byrne JV, Garcia M. Tentorial dural fistulas: endovascular management and description of the medial dural-tentorial branch of the superior cerebellar artery. AJNR Am J Neuroradiol. 2013;34:1798–804.
Huang Q, Xu Y, Hong B, et al. Use of Onyx in the management of tentorial dural arteriovenous fistulae. Neurosurgery. 2009;65:287–92.
Davies MA, ter Brugge K, Willinsky R, Wallace MC. The natural history and management of intracranial dural arteriovenous fistulae. Part 2: aggressive lesions. Interv Neuroradiol. 1997;3:303–11.
Tomak PR, Cloft HJ, Kaga A, et al. Evolution of the management of tentorial dural arteriovenous malformations. Neurosurgery. 2003;52:750–60.
Lawton MT, Sanchez-Mejia RO, Pham D, et al. Tentorial dural arteriovenous fistulae: operative strategies and microsurgical results for six types. Neurosurgery. 2008;62(3 Suppl 1):110–24.
Kortman HG, Boukrab I, Bloemsma G, et al. Tentorial dural arteriovenous fistulas: a single-center cohort of 12 patients. J Cerebrovasc Endovasc Neurosurg. 2017;19:284–90.
Cannizzaro D, Brinjikji W, Rammos S, et al. Changing clinical and therapeutic trends in tentorial dural arteriovenous fistulas: a systematic review. AJNR Am J Neuroradiol. 2015;36:1905–11.
Picard L, Bracard S, Islak C, et al. Dural fistulae of the tentorium cerebelli. Radioanatomical, clinical and therapeutic considerations. J Neuroradiol. 1990;17(3):161–81.
Wu Q, Zhang XS, Wang HD, et al. Onyx embolization for tentorial dural arteriovenous fistula with pial arterial supply: case series and analysis of complications. World Neurosurg. 2016;92:58–64.
Liu C, Xu B, Song D, et al. Clinical approach of using Onyx via transarterial access in treating tentorial dural arteriovenous fistula. Neurol Res. 2014;36(11):983–91.
Puffer RC, Daniels DJ, Kallmes DF, et al. Curative Onyx embolization of tentorial dural arteriovenous fistulas. Neurosurg Focus. 2012;32(5):E4.
Wajnberg E, Spilberg G, Rezende MT, et al. Endovascular treatment of tentorial dural arteriovenous fistulae. Interv Neuroradiol. 2012;18:60–8.
Iwamuro Y, et al. Tentorial dural arteriovenous fistula presenting symptoms due to mass effect on the dilated draining vein: case report. Surg Neurol. 2006;65:511–5.
Rezende MTS, Trivelato FP, de Castro-Afonso LH, et al. Endovascular treatment of tentorial dural arteriovenous fistulas using the transarterial approach as a first-line strategy. Oper Neurosurg. 2021;20(5):484–92.
Jiang C, Lv X, Li Y, et al. Endovascular treatment of high-risk tentorial dural arteriovenous fistulas: clinical outcomes. Neuroradiology. 2009;51(2):103–11.
Collice M, et al. Surgical treatment of intracranial dural arteriovenous fistulae: role of venous drainage. Neurosurgery. 2000;47:56–67.
Grisoli F, et al. Surgical treatment of tentorial arteriovenous malformations draining into the subarachnoid space. Report of four cases. J Neurosurg. 1984;60:1059–66.
Gross BA, Du R. Surgical treatment of high grade dural arteriovenous fistulae. J Clin Neurosci. 2013;20:1527–32.
Sugiyama T, et al. Complication rate, cure rate, and long-term outcomes of microsurgery for intracranial dural arteriovenous fistulae: a multicenter series and systematic review. Neurosurg Rev. 2021;44(1):435–50.
Kallmes DF, Jensen ME, Cloft HJ, et al. Percutaneous transvenous coil embolization of a Djindjian type 4 tentorial dural arteriovenous malformation. AJNR Am J Neuroradiol. 1997;18(4):673–6.
Deasey NP, Gholkar AR, Cox TCS, Jeffree MA. Tentorial dural arteriovenous fistulae: Endovascular treatment with transvenous coil embolization. Neuroradiology. 1999;41:308–12.
Djindjian R, Cophignon J, Theron J. Embolization by superselective arteriography from the femoral route; review of 60 cases: technique, indications, complications. Neuroradiology. 1973;6:20–6.
Grossman RI, et al. Dural malformations with ophthalmic manifestations: results of particulate embolization in seven patients. AJNR Am J Neuroradiol. 1985;6:809–13.
Berestein A. Flow controlled silicone fluid embolization. AJR Am J Roentgenol. 1980;134:1213–8.
Nelson PK, Russell SM, Woo HH, et al. Use of a wedged microcatheter for curative transarterial embolization of complex intracranial dural arteriovenous fistulas: indications, endovascular technique, and outcome in 21 patients. J Neurosurg. 2003;98(3):498–506.
Rezende MT, Piotin M, Mounayer C, et al. Dural arteriovenous fistula of the lesser sphenoid wing region treated with Onyx: technical note. Neuroradiology. 2006;48(2):130–4.
Toulgoat F, Mounayer C, Túlio Salles Rezende M, et al. Transarterial embolisation of intracranial dural arteriovenous malformations with ethylene vinyl alcohol copolymer (Onyx18). J Neuroradiol. 2006;33(2):105–14.
Gioppo A, Faragò G, Caldiera V, et al. Medial tentorial dural arteriovenous fistula embolization: single experience with embolic liquid polymer SQUID and review of the literature. World Neurosurg. 2017;107:1050.e1–7.
Yu J, et al. Clinical importance of the middle meningeal artery: a review of the literature. Int J Med Sci. 2016;13(10):790–9.
Tong D, Chen X, Lv X, et al. Current status of endovascular treatment for dural arteriovenous fistulae in the tentorial middle region: a literature review. Act Neurol Belg. 2019;119(1):5–14.
Flores BC, See AP, Weiner GM, et al. Use of the Apollo detachable-tip microcatheter for endovascular embolization of arteriovenous malformations and arteriovenous fistulas. J Neurosurg. 2018;130(3):963–71.
Zamponi JO Jr, Trivelato FP, Rezende MTS, et al. Transarterial treatment of cranial dural arteriovenous fistulas: the role of transarterial and transvenous balloon-assisted embolization. AJNR Am J Neuroradiol. 2020;41(11):2100–6.
Martins C, Yasuda A, Campero A, et al. Microsurgical anatomy of the dural arteries. Neurosurgery. 2005;56(ONS 2):211–51.
Lin N, Brouillard AM, Mokin M, et al. Direct access to the middle meningeal artery for embolization of complex dural arteriovenous fistula: a hybrid treatment approach. J Neurointerv Surg. 2015;7(7):e24.
Oh JS, Yoon SM, Shim JJ, Bae HG. Transcranial direct middle meningeal artery puncture for the onyx embolization of dural arteriovenous fistula involving the superior sagittal sinus. J Korean Neurosurg Soc. 2015;57:54–7.
Rabinov JD, Yoo AJ, Ogilvy CS, et al. ONYX versus n-BCA for embolization of cranial dural arteriovenous fistulas. J Neurointerv Surg. 2013;5:306–10.
Abud DG, Riva R, Nakiri GS, et al. Treatment of brain arteriovenous malformations by double arterial catheterization with simultaneous Onyx injection: retrospective series of 17 patients. AJNR Am J Neuroradiol. 2011;32(1):152–8.
Cognard C, Januel AC, Silva NA Jr, Tall P. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using Onyx. AJNR Am J Neuroradiol. 2008;29:235–41.
Lv X, Jiang C, Li Y, Wu Z. Results and complications of transarterial embolization of intracranial dural arteriovenous fistulas using Onyx-18. J Neurosurg. 2008;109(6):1083–90.
van Rooij WJ, Sluzewski M, Beute GN. Tentorial artery embolization in tentorial dural arteriovenous fistulas. Neuroradiology. 2006;48:737–43.
Wang H, Lv X, Jiang C, et al. Onyx migration in the endovascular management of intracranial dural arteriovenous fistulas. Interv Neuroradiol. 2009;15(3):301–8.
Nogueira RG, Dabus G, Rabinov JD, et al. Preliminary experience with onyx embolization for the treatment of intracranial dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2008;29(1):91–7.
Lai CW, et al. Cerebral arteriovenous fistulas induced by dural arteriovenous shunts. AJNR Am J Neuroradiol. 2005;26:1259–62.
Borha A, et al. Tentorial dural fistula with giant venous ampulae treated with embolisation and surgery. A case report. Acta Neurochir (Wien). 2010;152(10):1745–53.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Rezende, M.T.S., Trivelato, F.P., Ulhôa, A.C., Abud, D.G. (2022). Tentorial Dural Arteriovenous Fistulas: Anatomy, Clinical Presentation and Endovascular Treatment. In: Lv, X. (eds) Intracranial and Spinal Dural Arteriovenous Fistulas. Springer, Singapore. https://doi.org/10.1007/978-981-19-5767-3_12
Download citation
DOI: https://doi.org/10.1007/978-981-19-5767-3_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-5766-6
Online ISBN: 978-981-19-5767-3
eBook Packages: MedicineMedicine (R0)