Abstract
Recently, time-of-flight (TOF) and gadolinium-enhanced MR angiography (MRA) imaging have been used to demonstrate subacute intramural hematoma in cervical artery dissection and to detect intraplaque haemorrhage. Our aim was to perform an exploratory study to analyse if venous thrombus-related signal changes (potentially showing iso- or hyperintensity) in cerebral venous sinus thrombosis (CVST) could be observed on 3D-TOF MRA imaging. We analysed retrospectively MRIs of CVST patients in whom both contrast-enhanced MR venography (CEMRV) and 3D-TOF sequences were performed in the acute/subacute phase (i.e. < 31 days after symptom onset). The occluded sinus segments were defined on CEMRV. First, analyses of signal changes in occluded venous sinuses segments (defined by and unblinded to CEMRV) on native 3D-TOF images and morphological MRI sequences were performed. Second, a blinded (to CEMRV and other morphological MRI sequences) analysis was performed on 3D-TOF imaging assessing signal changes on 3D-TOF considering all sinus segments. Twenty-five CVST patients were included. 3D-TOF imaging showed signal changes (most often hyperintensity and less often isointensity) in 84% of the occluded sinus segments. Signal changes were observed in 91% of the occluded sinus segments on T1-weighted imaging, in 69% on T2-weighted imaging, in 68% on FLAIR, in 32% on DWI, and in 55% on T2*-weighted imaging. On blinded analysis, sensitivity of 3D-TOF sequences decreased to 80%, whereas specificity was only 65%. Abnormal signal in the venous sinuses on 3D-TOF may possibly help to suspect CVST, especially when CEMRV sequences lack.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebral venous sinus thrombosis (CVST) can be often well visualised on MRI. Contrast-enhanced MR venography (CEMRV) is probably the most reliable sequence to diagnose CVST, while other morphological MRI sequences are also useful [1,2,3,4,5,6,7,8].
Recently, 3D time-of-flight (3D-TOF) and gadolinium-enhanced MR angiography (MRA) imaging, classically used to study extra- and intracranial cerebral arteries, has been also used to demonstrate subacute intramural hematoma in cervical artery dissection and to detect intraplaque haemorrhage (both seen as hyperintensity) [9,10,11,12,13,14]. Our aim was to perform an exploratory study to analyse if venous thrombus-related signal changes (potentially showing iso- or hyperintensity) in CVST could be observed on 3D-TOF MRA imaging.
Methods
We retrospectively analysed MRIs of CVST patients performed in the acute/subacute phase (< 31 days between symptom onset and MRI) between 2006 and 2016. Only MRIs including both CEMRV and 3D-TOF sequences performed in the same acquisition were included. In both participating centres, a total number of 112 MRIs of CVST patients were screened for the presence of CEMRV and 3D-TOF sequences. Both sequences were performed in 37 patients. Of these patients, 12 were excluded because of CVST localisation out of the field of TOF acquisition (most often in case of isolated involvement of anterior/superior portions of the superior sagittal sinus or inferior portions of the sigmoid sinus) or because of an associated vascular malformation, leaving 25 patients for analysis. 3D-TOF imaging was performed before gadolinium injection for CEMRV sequences in all patients. 3D-TOF imaging was performed on four different MRI scanners, including 23 patients on a 1.5T magnet (Avanto, Siemens, Erlangen, Germany; Intera, Philips, The Netherlands; Ingenia, Philips, The Netherlands) and two patients on a 3T magnet (Signa HDxt, GE Medical Systems, Milwaukee, Wis), using different MRI parameters. Slice thickness varied between 0.41 and 0.7 mm (the most commonly used slice thickness was 0.5 mm, used in 12/25 patients), isotropic pixel size varied between 0.26 and 0.62 mm side (with a dimension of 0.35 mm side as most frequently used in nearly half of the patients), flip angle RF pulse was 20° in all patients except two with 18° and four with 25°, bandwidth varied between 95 and 200 Hz/pixel, TE echo time from 1.399 to 7.15, and TR repetition time from 20 to 25 (with TR of 23 used in 19/25 patients). Analysis of signal changes on TOF was performed using axial 3D TOF native images covering the entire Willis polygon for an average number of 180 slices.
Initially, we analysed the different sinus segments (superior sagittal sinus [SSS], left transverse sinus [LTS], right transverse sinus [RTS], left sigmoid sinus [LSS], right sigmoid sinus [RSS], straight sinus [SS], deep venous system [DVS: vein of Galen, internal cerebral veins]) on CEMRV, used as the gold standard for CVST diagnosis on MRI. Sinus segments were defined as occluded when partial or complete thrombosis was observed.
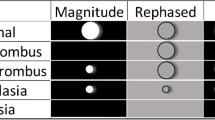
First, an unblinded (to CEMRV) analysis was performed, assessing MRI signal on 3D-TOF and morphological MRI sequences (T1-weighted, T2-weighted, FLAIR, DWI, T2*-weighted, and SWI), only in the occluded sinus segments defined by CEMRV. We analysed the sensitivity of these different MRI sequences. For the 3D-TOF analysis, the sinus segment was considered abnormal when homogeneous or peripheral hyperintensity was observed or in case of isointensity associated with hypointensity in the non-involved (on CEMRV) sinus segments. On T1-weighted, T2-weighted, FLAIR, and DWI, we searched for iso- or hyperintensity inside the sinus segments. For T2*-weighted and SWI imaging, the sinus was called abnormal only when a clear magnetic susceptibility effect was noted. For 3D-TOF imaging, analyses were performed independently by two reviewers (D.R. and I.M.), and Cohen’s kappa (κ) coefficient was calculated to assess the agreement between both raters. The morphological MRI sequences were only reviewed by one reviewer (D.R.). A two-tailed Fisher’s exact test was used to compare 3D-TOF sequences with the other MRI sequences.
Second, a blinded (to CEMRV and other MRI sequences) analysis was performed 2 months later by one reviewer (D.R.) for 3D-TOF imaging considering all sinus segments.
To analyse potential change over time of the signal on 3D-TOF sequences, we compared data (using Fisher’s exact test) between patients with time between symptom onset and MRI < 7 versus ≥ 7 days and < 14 versus ≥ 14 days.
Results
Twenty-five MRIs of 25 acute/subacute CVST patients (18 women and seven men; median age 42, range 18–80; median time between symptom onset and MRI 8 days, range 1–30) were analysed. A total of 64 sinus segments (mean 2.5 segments per patient, range 1–6) were occluded on CEMRV: 10 SSS, 15 LTS, 10 RTS, 14 LSS, 7 RSS, 6 SS, and 2 DVS.
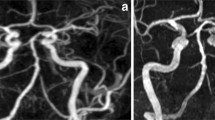
On unblinded analysis, 3D-TOF sequences showed signal changes in 54 sinus segments, corresponding to a sensitivity of 84%. When 3D-TOF showed signal changes, hyperintensity (i.e. hyperintensity in all sinus segments called abnormal) was seen in 82% and mixed iso- and hyperintensity (i.e. isointensity in certain sinus segments and hyperintensity in other segments) was observed in 18%. On 3D-TOF, hyperintensity in occluded sinus segments was homogeneous in 29%, limited to the peripheral sinus borders in 42%, and mixed (homogeneous in certain sinus segments and peripheral in other segments) in 29% of the patients. The interrater reliability for 3D-TOF analyses of the different sinus segments with κ statistics was good, with κ values of 1 for SSS, 1 for RTS, 0.747 for RSS, 0.840 for LTS, 0.913 for LSS, 0.832 for SS, and 0.646 for DVS. T1-weighted imaging was performed in 21/25 patients (84%), T2-weighted imaging in 23/25 patients (92%), FLAIR in 23/25 patients (92%), DWI in 24/25 patients (96%), T2*-weighted imaging in 24/25 patients (96%), and SWI in 3/25 patients (12%). Because of the low number of SWI sequences, this sequence was not further analysed. Sensitivity was 91% for T1-weighted, 69% for T2-weighted, 68% for FLAIR, 32% for DWI, and 55% for T2*-weighted imaging. When comparing directly different MRI sequences (i.e. in patients where all these sequences were performed) sensitivity was 81% for 3D-TOF, 91% for T1-weighted, 69% for T2-weighted, 69% for FLAIR, 32% for DWI, and 58% for T2*-weighted imaging. Differences in sensitivity were statistical significant only between 3D-TOF and FLAIR (p = 0.044), 3D-TOF and DWI (p < 0.001), and 3D-TOF and T2*-weighted imaging (p < 0.001). The Figure shows 3D-TOF and T1-weighted imaging of seven CVST patients (Fig. 1).
MRI T1-weighted and 3D-TOF imaging in seven CVST patients. MRI axial unenhanced T1-weighted (a, c, e, g, i, k, and m) and 3D-TOF (b, d, f, h, j, l and n) imaging in seven different CVST patients (each horizontal row corresponds to a different patient) showing the presence of hyperintensity in the involved venous sinuses and the concordance of signal changes on both sequences
On analysis blinded to CEMRV, sensitivity of 3D-TOF sequences decreased to 80%, whereas specificity was only 65% (essentially due to the false positive isointense sinus signal or slightly hyperintense signal in the peripheral borders of sinus segments).
The difference between MRI scans of different field strengths was not analysed because of the very low number of patients with a 3T MRI (n = 2).
The presence/absence of hyperintensity on 3D-TOF sequences did not differ significantly between patients with time between symptom onset and MRI < 7 versus ≥ 7 days and < 14 versus ≥ 14 days.
Discussion
Based on our study, CVST was frequently seen as hyperintensity on 3D-TOF. On analysis unblinded to CEMRV, sensitivity of 3D-TOF sequences to detect signal changes in occluded sinus segments was slightly lower compared with T1-weighted imaging but higher than other sequences. However, on analysis blinded to CEMRV and morphological sequences, specificity of 3D-TOF was relatively low.
When CVST is suspected, adequate MRI sequences (including CEMRV) will be performed and probably detect CVST. However, a minority of CVST patients lack typical symptoms. When no specific neurological disorder is suspected or sometimes also because of time saving reasons in acute care management, shorter MRI protocols are proposed. In this kind of situations, abnormal signal in the venous sinuses on 3D-TOF (when performed) may possibly help to suspect CVST and incite to perform other sequences including CEMRV in order to confirm CVST diagnosis.
Limitations of our study were the relative small sample size, the different MRI scans and parameters used, the retrospective character of the MRI analyses, and the exclusion of patients with CVST involving only sinus portions out of the field of 3D-TOF acquisition. In addition, by including only patients with both 3D-TOF and CEMRV sequences, a potential selection bias might have been created (where for instance only both sequences were performed in CVST cases difficult to diagnose). This study was only preliminary, performed in order to assess the potential presence of signal changes on 3D-TOF imaging in occluded venous sinuses. The principal aim was not to compare 3D-TOF and morphological MRI sequences directly blinded to CEMRV imaging to calculate positive and negative predictive values and accuracy of these sequences. Therefore, analysis by (and comparison between) two different reviewers was only performed for 3D-TOF sequences unblinded to CEMRV and blinded analysis of 3D-TOF was only performed to have an idea of the specificity of signal changes in the venous sinuses on 3D-TOF compared with what was observed on CEMRV. In order to better assess the diagnostic value of 3D-TOF signal changes in CVST, larger CVST patient groups (taking into account also the difference in time from onset and the different sinus segments) have to be studied by 3D-TOF and morphological MRI sequences and these different sequences have to be compared directly and blinded for each of the sequences.
References
Bonneville F (2014) Imaging of cerebral venous thrombosis. Diagn Interv Imaging 95:1145–1150
Patel D, Machnowska M, Symons S, Yeung R, Fox AJ, Aviv RI et al (2016) Diagnostic performance of routine brain MRI sequences for dural venous sinus thrombosis. AJNR Am J Neuroradiol 37:2026–2032
Sadigh G, Mullins ME, Saindane AM (2016) Diagnostic performance of mri sequences for evaluation of dural venous sinus thrombosis. AJR Am J Roentgenol 206:1298–1306
Lövblad KO, Bassetti C, Schneider J, Guzman R, El-Koussy M, Remonda L et al (2001) Diffusion-weighted mr in cerebral venous thrombosis. Cerebrovasc Dis 11:169–176
Chu K, Kang DW, Yoon BW, Roh JK (2001) Diffusion-weighted magnetic resonance in cerebral venous thrombosis. Arch Neurol 58:1569–1576
Idbaih A, Boukobza M, Crassard I, Porcher R, Bousser MG, Chabriat H (2006) MRI of clot in cerebral venous thrombosis: high diagnostic value of susceptibility-weighted images. Stroke 37:991–995
Ihn YK, Jung WS, Hwang SS (2013) The value of T2*-weighted gradient-echo MRI for the diagnosis of cerebral venous sinus thrombosis. Clin Imaging 37:446–450
Bidar F, Faeghi F, Ghorbani A (2016) Assessment of cerebral venous sinus thrombosis using T2 (*)-weighted gradient echo magnetic resonance imaging sequences. Iran J Neurol 15:96–99
Habs M, Pfefferkorn T, Cyran CC, Grimm J, Rominger A, Hacker M et al (2011) Age determination of vessel wall hematoma in spontaneous cervical artery dissection: a multi-sequence 3T cardiovascular magnetic resonance study. J Cardiovasc Magn Reson 13:76
Kirsch E, Kaim A, Engelter S, Lyrer P, Stock KW, Bongartz G et al (1998) MR angiography in internal carotid artery dissection: improvement of diagnosis by selective demonstration of the intramural haematoma. Neuroradiology 40:704–709
Li Q, Wang J, Chen H, Gong X, Ma N, Gao K et al (2015) Characterization of craniocervical artery dissection by simultaneous MR noncontrast angiography and intraplaque hemorrhage imaging at 3T. AJNR Am J Neuroradiol 36:1769–1775
Qiao Y, Etesami M, Malhotra S, Astor BC, Virmani R, Kolodgie FD et al (2011) Identification of intraplaque hemorrhage on MR angiography images: a comparison of contrast-enhanced mask and time-of-flight techniques. AJNR Am J Neuroradiol 32:454–459
Yoshimura S, Yamada K, Kawasaki M, Asano T, Kanematsu M, Takamatsu M et al (2011) High-intensity signal on time-of-flight magnetic resonance angiography indicates carotid plaques at high risk for cerebral embolism during stenting. Stroke 42:3132–3137
Yamada K, Song Y, Hippe DS, Sun J, Dong L, Xu D et al (2012) Quantitative evaluation of high intensity signal on MIP images of carotid atherosclerotic plaques from routine TOF-MRA reveals elevated volumes of intraplaque hemorrhage and lipid rich necrotic core. J Cardiovasc Magn Reson 14:81
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
It was obtained from the study participants.
Rights and permissions
About this article
Cite this article
Renard, D., Le Bars, E., Arquizan, C. et al. Time-of-flight MR angiography in cerebral venous sinus thrombosis. Acta Neurol Belg 117, 837–840 (2017). https://doi.org/10.1007/s13760-017-0835-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-017-0835-2