Abstract
Purpose
The aim of this study was to evaluate the diagnostic performance of Inhance 3D Velocity (I3DV) in intracranial venous thrombosis and investigate the possible impact of venous sinus hypoplasia/aplasia on false thrombosis diagnosis made with I3DV.
Methods
This study included 540 patients. Contrast-enhanced magnetic resonance venography combined with conventional sequences was considered the gold standard test (GST), while I3DV was considered as diagnostic test. We accessed the diagnostic success of I3DV for intracranial venous thrombosis detection, thrombosed vessel identification, and total/partial thrombus distinction. The possible relationship between false-positive thrombus diagnosed by I3DV and venous sinus hypoplasia or aplasia diagnosed by GST was investigated.
Results
The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of I3DV in the detection of intracranial venous thrombosis were 95.7%, 92.1%, 64.1%, 99.3%, and 92.6%, respectively. A significant association was observed between I3DV and GST in terms of thrombosis detection and total/partial thrombus distinction (p < 0.001). A significant relationship was observed between false-positive thrombosis diagnosis in I3DV and hypoplasia in the left transverse sinus (p < 0.001).
Conclusion
Intracranial venous thrombosis may be diagnosed faster and more accurately than traditional phase contrast magnetic resonance angiography in I3DV. This technique can be used in situations where contrast medium application is contraindicated. As in other non-contrast magnetic resonance venography techniques, left transverse sinus hypoplasia can be diagnosed as a thrombosed vessel in I3DV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance venography (MRV) is an imaging method used to evaluate the patency of venous structures. MRV is usually performed to evaluate intracranial dural venous sinuses and related venous structures. The primary pathology here is intracranial venous thrombosis [1, 2]. Furthermore, anatomic variations (hypoplasia or aplasia) may often be encountered [3].
Although digital subtraction angiography is the gold standard for evaluating intracranial venous structures, it is not frequently used owing to its invasiveness and the effect of ionizing radiation [4]. In practice, through advancements in computed tomography (CT) imaging and magnetic resonance imaging (MRI) in the last 3 decades, the correct diagnosis is usually made through non-contrast CT—MRI, CT venography, and MRV.
MRV can be performed either in non-contrast (NCMRV) or contrast-enhanced (CEMRV) modes. Luminal patency can be evaluated with high sensitivity and specificity by using CEMRV [5], but it cannot be performed in the setting of pregnancy, kidney insufficiency, or allergy history. In such situations, non-contrast MRV (NCMRV) is generally performed. The most commonly used methods for this purpose are 2- or 3-dimensional (2D/3D) time-of-flight (TOF) or 2D/3D phase-contrast (PC) imaging. All defined NCMRV methods have several advantages and disadvantages [4].
Inhance 3D Velocity (I3DV) is an advanced 3D-PC MR angiography technique that combines parallel imaging and optimized filling of the k-space [6, 7]. This technique is known to have very long scanning times and exceeded motion artifacts (considered disadvantages of traditional 3D-PC MR angiography) and an improved background suppression and contrast-to-noise ratio [6]. However, there is no information about situations such as transverse sinus hypoplasia or turbulent flow, which may be diagnosed as a false thrombus in NCMRV examinations, thereby affecting this sequence [8, 9]. Moreover, the diagnostic performance of I3DV in intracranial venous thrombosis remains unknown.
Therefore, we sought to access the diagnostic performance of I3DV in intracranial venous thrombosis and investigate the possible impact of venous sinus hypoplasia/aplasia on falsely diagnosing thrombosis using I3DV.
Methods
Ethical board consent was obtained for this study.
Patient selection
Cranial MRV examinations done for “venous thrombosis” were searched through Centricity™ RIS-İ 6 (GE Healthcare, Chicago, IL, USA) program. We noted 589 MRV examinations performed between June 2016 and November 2020. We also excluded examinations of the same patients and studies lacking one of the conventional (T1 weighted and T2 weighted), I3DV, and CEMRV sequences. We included and retrospectively reviewed 540 studies related to different patients involving conventional, I3DV, and CEMRV sequences. Before all MRV examinations, informed consent was obtained from all the patients.
MRI protocol
All MRV examinations were performed using a 1.5T MRI device (Signa Explorer®, GE Healthcare, Chicago, IL, USA). First, T1 weighted (T1W), T2 weighted (T2W), and I3DV were obtained before contrast administration. Then, a pre-contrast 3D-spoiled gradient echo-based CEMRV sequence was acquired. Thereafter, a bolus tracking sequence was started, and 0.2 mL/kg meglumine gadoterate was applied with an automated injection device through an intravenous route at a rate of 4–5 mL/s. A post-contrast CEMRV sequence was obtained (similar to the pre-contrast sequence) when opacification was seen in the superior sagittal sinus (SSS). The technical parameters of each sequence are listed in Table 1.
As soon as the post-contrast CEMRV sequence was obtained, the MRI console automatically subtracted the pre-contrast CEMRV sequence from the post-contrast sequence. In addition, maximum intensity projection (MIP) images were also obtained from the magnitude images of I3DV and subtracted images of CEMRV.
Imaging interpretation
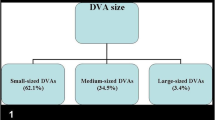
Two observers reviewed all studies: one with 19-year experience in neuroradiology and the other with 8 years in general radiology. In the first assessment, only the I3DV images were evaluated. In the second, the conventional and CEMRV sequences were analyzed. All observers were blinded to the results of the assessments. When the assessments were complete, the agreement between the analyses of both observers was investigated. In cases of disagreement, the last decision was given by a common consensus. SSS; transverse sinuses (TS); sigmoid sinuses (SS); jugular bulbs (JB); sinus rectus (SR); internal cerebral veins (IJV); Rosenthal basal veins (RBV); veins of Galen (GV), Trolard (TV), and Labbé (LV); and other cortical veins (OCV) were assessed for thrombosis. In addition, main sinuses (SSS, SR, left and right TS–SS–JB) were evaluated for total/partial thrombosis distinction in both assessments and for hypoplasia in only CEMRV. In I3DV evaluation, flow signals were assessed with magnitude, multiplanar reformation (MPR), and MIP images, while the anatomic features of the vessel were evaluated using rephased images. In CEMRV evaluation, subtraction, MPR, and MIP images were assessed for diagnosis. Total/partial thrombosis, hypoplasia, and aplasia assessment criteria used in I3DV assessments are shown in Fig. 1.
Graphical illustration of the assessment criteria used in I3DV evaluations. Normal vessel: the vessel with normal size and flow signal in transverse magnitude, transverse rephased, and longitudinal MIP images. Total thrombus: no flow signal in magnitude and MIP images, recognizable vessel structure in rephased images. Partial thrombus: decreased vessel diameter in magnitude and MIP images, in comparison with rephased images. Hypoplasia: small and similar vessel diameter in magnitude, rephased, and MIP images. Aplasia: no recognizable vessel structure in magnitude, rephased, and MIP images
Data collection
Patient age and sex were determined. Total/partial thrombosis findings of the vessels determined in both assessments and hypoplasia/aplasia findings in the second assessment were recorded.
Statistical analysis
“CEMRV combined with conventional sequences” was considered as gold standard test (GST) and I3DV as diagnostic test [10]. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy for the diagnosis of “intracranial venous thrombosis” in patients were determined. The tolerance for venous thrombosis diagnosis and total/partial thrombus distinction between I3DV and GST were also evaluated using kappa analysis. The relationship between false-positive thrombosis findings in I3DV and hypoplasia/aplasia findings of GST was assessed using the Pearson chi-square test for each main sinus. The agreement level was assessed using Cohen’s kappa coefficient (κ). κ < 0 was defined as poor agreement level, 0–0.2; slight, 0.21–0.4; fair, 0.41–0.60; moderate, 0.61–0.8; substantial, 0.81–0.99; almost perfect; and 1 is perfect. p-values less than 0.05 are considered statistically significant. All analyses were performed using the SPSS 23.0 version for windows.
Results
The mean age of the patients was 36.26 ± 17.7 years. We observed that 35.7% of the study population were male. The sensitivity of I3DV in diagnosing venous thrombosis was 95.7%, specificity; 92.1%, PPV; 64.1%, NPV; 99.3%, and accuracy; 92.6% (Table 2). We observed a substantial agreement between I3DV and GST in the setting of venous thrombosis (κ = 0.725, p < 0.001).
In the thrombosed vessel evaluation (Table 2), SSS, SR, ISV, RBV, and left TV were assessed with 100% sensitivity, specificity, PPV, NPV, accuracy, and perfect accordance (κ=1, p<0.001). The right SS, right JB, right TV, right LV, and OCV were evaluated with a sensitivity of 100%, specificity of 99.2–99.8%, PPV of 80–91.7%, NPV of 100%, and accuracy of 99.3–99.8%, with an almost perfect accordance (κ = 0.888–0.955, p < 0.001). The left SS was evaluated with a sensitivity of 95.7%, specificity of 99.4%, PPV of 88%, NPV of 99.8%, and accuracy of 96.1%, with an almost perfect agreement (κ = 0.913, p < 0.001). Left TS and left JB were evaluated with a sensitivity of 95.5%, specificity of 96.1–98.1%, PPV of 51.2–67.7%, NPV of 99.8%, accuracy of 96.1–98.0%, and a moderate agreement (κ = 0.648–0.782, p < 0.001). The right TS was accessed with a sensitivity of 90.9%, specificity of 98.8%, PPV of 76.9%, NPV of 99.6%, accuracy of 98.6%, and substantial agreement (κ = 0.826, p < 0.001).
We evaluated 4320 main venous sinuses of 540 patients for total/partial thrombus distinction. The accuracy of I3DV was 98.5%. GST was substantial (κ = 0.783, p < 0.001). Right and left TS and left JB were assessed with a substantial agreement (κ = 0.619–0.785, p < 0.001) and with an accuracy of 95.7–98.7%. Right and left SS, right JB, and SSS were assessed with almost perfect agreement (κ = 0.963–0.849, p < 0.001) and with an accuracy of 98.7–99.6%. SR was accessed with a perfect accordance (κ = 1, p < 0.001) and 100% accuracy (Table 3).
ICVT was diagnosed in four patients. Right TV was thrombosed in two patients, right LV in one patient, and bilateral posterior-superior superficial cortical veins in one patient. ICVT was diagnosed in I3DV with 100% sensitivity, specificity, PPV, NPV, accuracy, and perfect accordance (κ = 1, p < 0.001).
Venous thrombosis cases are displayed in Figs. 2, 3, and 4.
A case of total thrombosis. Sagittal rephased image of I3DV (a), recognizable left TS lumen (black arrow). Magnitude image in the same plane (b) and coronal MIP image (c) of I3DV, no flow signal in left TS. T2-weighted image (d), hyperintense left TS (white arrow). Sagittal post-contrast CEMRV image (e) in the same plane with sagittal I3DV images above, a complete filling defect in left TS. MIP image reconstructed from subtracted CEMRV images (f), no signal in left TS
A case of partial thrombosis. Coronal rephased image of I3DV (a), identifiable round lumen of SSS (black arrowheads). Magnitude image of I3DV (b) in the same plane with (a), only a small flow signal in the left corner of SSS (white arrowhead) and no signal in other parts. MIP I3DV image (c), a heterogeneous flow signal and decreased calibration in the convexity part of SSS (thin white arrows). Sagittal rephased image of I3DV (d) same plane with (c), hyperintense low compartment of SSS convexity part (thin black arrows), showing no flow signal in (c). Coronal post-contrast CEMRV image (e) in the same plane with coronal I3DV images above, a central filling defect and peripheral enhancement (white arrowheads with black inside). MIP image of CEMRV (f), a partial filling defect in convexity segment
The case diagnosed as a total thrombus using I3DV and as partial thrombus using GST. Sagittal rephased image of I3DV (a), detectable lumen of right TS–SS junction (arrows). Magnitude (b) and MIP (c) I3DV images in the same plane with (a), no flow signal in the junction. Post-contrast (d), subtraction (e), and MIP (f) images of CEMRV in a same plane with I3DV images above, partial filling defects in the junction and nearby parts of TS–SS, which are compatible with partial thrombus
From GST evaluations, hypoplasia/aplasia was observed in 184 left SS, 181 left TS, 177 left JB, 112 right TS, 105 right SS, 94 right JB, 3 SSS, and 1 SR (Table 4). In the evaluation of hypoplastic and aplastic sinuses with I3DV, a very high significant relationship was observed between left TS hypoplasia in GST and false-positive-left TS thrombosis in I3DV (p < 0.001). Hypoplasia was more frequently observed in patients with false-positive TS thrombosis than the others (Table 5). No significant relationship was observed between false-positive thrombosis diagnosed by I3DV and the presence of hypoplasia/aplasia on GST for SSS, SS, right and left SS, right and left JB, and right TS (p > 0.05).
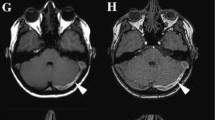
A left TS hypoplasia case interpreted as left TS thrombosis with I3DV is shown in Fig. 5.
The left TS hypoplasia case interpreted as left TS thrombosis with I3DV. Sagittal rephased (a), magnitude (b), and MIP (c) images belong to I3DV from the middle of the left TS, recognizable TS contour (black arrow) on (a), but no flow signal in (b) and (c) (white arrowheads), findings considered as total thrombus. T2-weighted image (d), hyperintensity of the left TS (white arrow), can be due to slow flow or thrombus. Post-contrast CEMRV image (e) in the same plane with sagittal I3DV images above, normal opacification of the left TS lumen (empty white arrow). Axial MIP image of CEMRV, hypoplastic left TS
Discussion
I3DV is an improved 3D-PC sequence with many advantages over traditional 3D-PC imaging such as using parallel imaging with the ASSET technique, decreased repetition and echo times, T1-weighted rephased images different from proton density weighted-like images obtained using the traditional technique, and advances in k-space filling. Reports reveal that all the improvements above resulted in improved scanning time, vascular contrast, and background suppression [6, 7]. The sensitivity, specificity, NPV, and accuracy of I3DV were very high for intracranial venous thrombosis in our study. However, the PPV was lower than the other parameters (64.1% versus > 92%). In studies evaluating the diagnostic performance of traditional 3D-PC MRV for venous thrombosis, sensitivity levels ranged from 90 to 100%, specificity from 50 to 92%, PPV from 63 to 76%, and NPV from 86 to 97% [11,12,13]. Our study shows that I3DV offers a very high-level diagnostic performance with shorter examination times than traditional 3D-PC MRV.
In clinical practice, the most commonly used technique for NCMRV is 2D-TOF MRV [14]. It has a sensitivity of 51–100% for cerebral venous thrombosis, specificity of 48–93%, PPV of 39–64%, and NPV of 65–100% [13, 15,16,17]. 2D-TOF is beneficial over 3D-TOF in that it is sensitive to slow flow [14, 18]. 2D-TOF imaging is also superior to traditional 3D-PC MRV in terms of shorter acquisition times (5–8 min vs. 15 min approx.) and lack of knowledge regarding the flow rate of the vessels in interest [1, 18]. However, 2D-TOF MRV has several disadvantages. These include signal gaps that may simulate thrombosis, saturation of in-plane flow signals, and false-negative diagnoses resulting from T1-shortening situations (subacute thrombus and adjacent subacute hemorrhage) [18, 19]. 3D-PC MRV is not affected by T1 shortening, though having long image acquisition times; thus, severe motion artifacts can occur [18]. However, in I3DV, acquisition time shorter than 3D-PC and at a similar length as 2D-TOF can be obtained, and it is still independent of T1-shortening effects because of its PC-based nature. Hence, I3DV could be used as the primary NCMRV method in all routine clinical and emergency conditions, even in the setting of intracranial hemorrhage. Further investigations may focus on the comparison of I3DV and 2D-TOF efficiency for venous thrombosis diagnosis.
The most thrombosed vessel according to GST was SSS. Bilateral TS–SS–JB were frequently thrombosed as well. Reports show that 62–63% of venous sinus thromboses are observed in SSS and 41.7–49.0% in TS [20, 21]. The very high sensitivity and specificity observed for venous sinus thrombosis in I3DV could be related to the diagnosis of SSS thrombosis, which is the most frequent vessel thrombosis with 100% accuracy.
There is no information about the efficiency of NCMRV for total and partial thrombus distinction in the literature. This differentiation was made in I3DV, with very high accuracy levels and significant accordance with GST. Total thromboses were diagnosed with almost perfect accuracy. However, false diagnoses were made using I3DV in some of cases with partial thrombus or with no thrombus (Table 3). I3DV may generally provide the correct idea for total and partial thrombosis. However, care must be taken when a low level of false diagnoses can be made.
Hypoplasia–aplasia findings were most frequently observed in the left SS and left TS by GST examination (Table 4). Similarly, hypoplasia has been most commonly seen in the left TS in previous studies [22, 23]. Although a similar frequency of hypoplasia was observed in the left SS and left TS, a significant relationship was noted only between left TS hypoplasia and false-positive left TS diagnosed with I3DV. This relationship has been described for traditional PC-MRV sequences, and it seems that I3DV does not bring any solution to this situation [24, 25]. This may originate from the PC basis of I3DV, which is sensitive to the flow rate. Major anastomotic veins such as the LV or superior petrosal vein ordinarily drain to the TS-SS junctions. Therefore, the flow rate could increase from this level towards SS, even in the case of hypoplasia, and hypoplastic SS may be seen in I3DV. However, there is no generally draining vessel to hypoplastic TS; the flow rate in hypoplastic TS may be slow. Consequently, flow signal may not be observed in it, and diagnosis of thrombosis can be performed using I3DV, similar to other PC-MRV methods. CEMRV may correctly diagnose in these cases. However, in cases where contrast medium is contraindicated, a hyperintense signal of the sinus in diffused-weighted imaging or blooming artifacts in the sinus lumen may be useful in differentiating thrombus from hypoplasia [26]. In addition, I3DV could be repeated with at least a halved encoding velocity value, and a very slow flow in these sinuses may be demonstrated. However, further investigations need to be explored to verify this hypothesis.
There are some other imaging techniques and modalities for the detection of intracranial venous thrombosis. Venous sinus thrombosis and ICVT can be suspected in non-contrast CT by searching dense vessel sign examples, such as delta sign for SSS thrombosis or cord sign for ICVT [18]. A filling defect can be observed in venous sinuses or superficial and deep cerebral veins in CT venography. Flow void loss of venous sinuses or veins in conventional MRI is the most related finding for cerebral venous sinus thrombosis, but in the acute stage, the signal in T1W and T2W may mimic flow void and cause a false-negative result [4]. All NCMRV techniques are flow-dependent, and hypoplastic/aplastic TS or slow flows may be diagnosed as thrombosis [18]. 3D-CEMRV overcomes these situations well, but it requires the timing experience for the optimal opacification of venous sinuses. The timing issue can be solved using 4D-CEMRV (time-resolved) techniques, but both CEMRV methods are performed with a gadolinium-based contrast agent [18]. A current imaging technique used for venous thrombosis detection is 3D-T1 Black-Blood Imaging, which is based on nulling the signal in the vessel lumen. It is very sensitive for detecting subacute thrombosis due to T1 shortening but not much for acute and chronic forms, in which T1 is not hyperintense [27]. Optimal imaging protocol must be selected considering the clinical condition of the patient.
Our study has several limitations and strengths. The large sample size and the applicability of the standard examination protocol to all cases are the main strengths. However, we encountered limitations which include the fact that it was a single-center and retrospective study design and that GST is not considered as DSA.
In conclusion, intracranial venous thrombosis can be diagnosed in I3DV with high accuracy and shorter acquisition times compared to traditional PC MRV. This sequence can be used as the main NCMRV sequence for routine clinical practice and emergency cases. However, like other NCMRV sequences, some left TS hypoplasia may be diagnosed by mistake as TS thrombosis.
References
Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF (2006) Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 26(Suppl 1):S19–S43
Morris PP, Black DF, Port J, Campeau N (2017) Transverse sinus stenosis is the most sensitive mr imaging correlate of idiopathic intracranial hypertension. AJNR Am J Neuroradiol 38:471–477
Mas JL, Meder JF, Meary E, Bousser MG (1990) Magnetic resonance imaging in lateral sinus hypoplasia and thrombosis. Stroke. 21:1350–1356
Ghoneim A, Straiton J, Pollard C, Macdonald K, Jampana R (2020) Imaging of cerebral venous thrombosis. Clin Radiol 75:254–264
Dmytriw AA, Song JSA, Yu E, Poon CS (2018) Cerebral venous thrombosis: state of the art diagnosis and management. Neuroradiology. 60:669–685
Shigenaga Y, Sasaki M, Ishimoto T, Ama K (2018) Simultaneous visualization of vessels and brain tumor with contrast-enhanced three-dimensional phase-contrast MR imaging. Magn Reson Med Sci 17:184–188
Lummel N, Boeckh-Behrens T, Lutz J, Burke M, Linn J (2012) Evaluation of the supraaortic arteries using non-contrast-enhanced velocity MR angiography “Inhance”. Neuroradiology. 54:1215–1219
Provenzale JM, Kranz PG (2011) Dural sinus thrombosis: sources of error in image interpretation. AJR Am J Roentgenol 196:23–31
Higgins JN, Gillard JH, Owler BK, Harkness K, Pickard JD (2004) MR venography in idiopathic intracranial hypertension: unappreciated and misunderstood. J Neurol Neurosurg Psychiatry 75:621–625
Bousser MG, Ferro JM (2007) Cerebral venous thrombosis: an update. Lancet Neurol 6:162–170
Ozturk K, Soylu E, Parlak M (2018) Dural venous sinus thrombosis: the combination of noncontrast CT, MRI and PC-MR venography to enhance accuracy. Neuroradiol J 31:473–481
Sari S, Verim S, Hamcan S, Battal B, Akgun V, Akgun H, Celikkanat S, Tasar M (2015) MRI diagnosis of dural sinus - cortical venous thrombosis: tmmediate post-contrast 3D GRE T1-weighted imaging versus unenhanced MR venography and conventional MR sequences. Clin Neurol Neurosurg 134:44–54
Jalli R, Zarei F, Farahangiz S, Khaleghi F, Petramfar P, Borhani-Haghighi A, Yadollahikhales G (2016) The sensitivity, specificity, and accuracy of contrast-enhanced T1-weighted image, T2*-weighted image, and magnetic resonance venography in diagnosis of cerebral venous sinus thrombosis. J Stroke Cerebrovasc Dis 25:2083–2086
Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, deVeber G, Ferro JM, Tsai FY (2011) Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 42:1158–1192
Liang L, Korogi Y, Sugahara T, Onomichi M, Shigematsu Y, Yang D, Kitajima M, Hiai Y, Takahashi M (2001) Evaluation of the intracranial dural sinuses with a 3D contrast-enhanced MP-RAGE sequence: prospective comparison with 2D-TOF MR venography and digital subtraction angiography. AJNR Am J Neuroradiol 22:481–492
Klingebiel R, Bauknecht HC, Bohner G, Kirsch R, Berger J, Masuhr F (2007) Comparative evaluation of 2D time-of-flight and 3D elliptic centric contrast-enhanced MR venography in patients with presumptive cerebral venous and sinus thrombosis. Eur J Neurol 14:139–143
Fu JH, Lai PH, Hsiao CC, Li SC, Weng MJ, Wang PC, Chen CKH (2010) Comparison of real-time three-dimensional gadolinium-enhanced elliptic centric-ordered MR venography and two-dimensional time-of-flight MR venography of the intracranial venous system. J Chin Med Assoc 73:131–138
van Dam LF, van Walderveen MAA, Kroft LJM, Kruyt ND, Wermer MJH, van Osch M, Huisman MV, Klok FA (2020) Current imaging modalities for diagnosing cerebral vein thrombosis - a critical review. Thromb Res 189:132–139
Canedo-Antelo M, Baleato-González S, Mosqueira AJ, Casas-Martínez J, Oleaga L, Vilanova JC, Luna-Alcalá A, García-Figueiras R (2019) Radiologic clues to cerebral venous thrombosis. Radiographics. 39:1611–1628
Ferro JM, Canhão P, Bousser MG, Stam J, Barinagarrementeria F, Stolz E, ISCVT Investigators (2010) Cerebral venous thrombosis with nonhemorrhagic lesions: clinical correlates and prognosis. Cerebrovasc Dis 29:440–445
Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F, ISCVT Investigators (2004) Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 35:664–670
Tantawy HF, Morsy MM, Basha MA, Nageeb RS (2020) Different normal anatomical variations of the transverse dural sinus in magnetic resonance venography (MRV): do age and sex matter? Eur J Anat 24:49–56
Goyal G, Singh R, Bansal N, Paliwal VK (2016) Anatomical variations of cerebral MR venography: is gender matter? Neurointervention. 11:92–98
Ayanzen RH, Bird CR, Keller PJ, McCully F, Theobald MR, Heiserman JE (2000) Cerebral MR venography: normal anatomy and potential diagnostic pitfalls. AJNR Am J Neuroradiol 21:74–78
Han K, Chao AC, Chang FC et al (2016) Diagnosis of transverse sinus hypoplasia in magnetic resonance venography: new insights based on magnetic resonance imaging in combined dataset of venous outflow impairment case-control studies: post hoc case-control study. Medicine (Baltimore) 95:e2862
Chang YM, Kuhn AL, Porbandarwala N, Rojas R, Ivanovic V, Bhadelia RA (2020) Unilateral nonvisualization of a transverse dural sinus on phase-contrast MRV: frequency and differentiation from sinus thrombosis on noncontrast MRI. AJNR Am J Neuroradiol 41:115–121
Wang G, Yang X, Duan J, Zhang N, Maya MM, Xie Y, Bi X, Ji X, Li D, Yang Q, Fan Z (2019) Cerebral venous thrombosis: MR black-blood thrombus imaging with enhanced blood signal suppression. AJNR Am J Neuroradiol 40:1725–1730
Author information
Authors and Affiliations
Contributions
Ozpar R – Data curation, conceptualization
Tonkaz M – Investigation, methodology
Erkal D – Resources, investigation
Ongen G – Resources, data curation
Hakyemez B – Supervision, validation
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of Bursa Uludag University Faculty of Medicine.
Consent to participate (include appropriate statements)
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozpar, R., Tonkaz, M., Erkal, D. et al. Non-contrast magnetic resonance venography with Inhance 3D Velocity: diagnostic performance for intracranial venous thrombosis. Neuroradiology 63, 1853–1861 (2021). https://doi.org/10.1007/s00234-021-02710-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02710-1