Abstract
Background
Contrast-enhanced magnetic resonance angiography (CE-MRA) has become a very popular imaging technique in the evaluation of the extracranial vessels pathology, while it is not commonly used to rule out intracranial vascular pathology. On the contrary, 3D time of flight MRA (TOF-MRA) has a solid role in the study of intracranial arterial vessels disease.
Materials and methods
One hundred and eight patients were consecutively included in the study. All patients were submitted to a 3 Tesla 3D CE-MRA imaging to rule out extracranial vessels pathology. A comparison was made with a 3D-TOF sequence acquired at the same time in the assessment of intracranial vessels diseases such as steno-occlusion, dissection, and aneurysms.
Results
With regard to steno-occlusive disease, Spearman’s rank correlation coefficient was of 0.56 for stenosis detection and of 0.57 for occlusive disease detection. The two techniques shared similar results in the evaluation of anterior circulation, while 3D-TOF found higher grades of stenosis for posterior circulation. With regard to dissection, Spearman’s rank correlation coefficient was of 0.7. 3D-TOF depicted more intramural hematoma (Spearman’s rank = 0.46), while CE-MRA showed more pseudo-aneurysms (Spearman’s rank = 0.56). Both the technique equally evaluated the presence of intracranial aneurysms (Spearman’s rank = 1).
Conclusion
CE-MRA can be considered a reliable tool to rule out intracranial pathology associated to supraortic steno-occlusive disease, also allowing time reduction. In the suspicion of dissection a T1-weighted sequence has to be added to detect the presence of a subacute vessel wall hematoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance angiography (MRA) plays a key role in the accurate diagnosis of steno-occlusive disease and dissection of the cervical and intracranial arteries and in the detection of intracranial aneurysms: in the last decades, it has seen a progressive increase in popularity and clinical applicability [1]. Its major advantage over CT angiography (CTA) is to be less invasive and complementary to MR study of the brain, the real gold standard to diagnose acute or chronic vascular brain pathologies.
Although digital subtraction angiography (DSA) has always been considered a diagnostic gold standard, there have been many reports showing the diagnostic accuracy of CE-MRA in the evaluation of carotid artery stenosis [2,3,4]. Coverage from the aortic arch up to the circle of Willis is the major benefit of contrast-enhanced MR angiography (CE-MRA) when compared with 3D time of flight (TOF-MRA), and its role in the evaluation of proximal high-grade stenosis and occlusion has also been widely established [5, 6]. CE-MRA has also been proven to have higher sensitivity and specificity values for extracranial carotid artery stenosis at both 1.5 T and 3 T than 3D-TOF-MRA, due to the latter greater sensitivity to saturation effect [5, 7]. Moreover CE-MRA allows a complete visualization of the vertebral arteries, a major advantage not only over 3D-TOF-MRA but also on US and CTA, and the latter impaired by vertebral bones.
There is still no consensus regarding the optimal method for diagnosing dissection of extra-intracranial arteries with MRA. CE-MRA currently represents the most popular choice for the non-invasive imaging of arterial dissection [8]. 3D TOF-MRA demonstrated excellent sensitivity (87–99%) in the diagnosis of carotid dissection [9] when compared to DSA, but this sensitivity turned out to be lower (60%) for the detection of vertebral dissection [10].
Both CTA and CE-MRA allow to study the intracranial circulation to rule out the presence of concomitant pathology, as tandem stenosis or vascular malformations. The prevalence of incidental aneurysms in imaging studies is of 0.5–2% [11], and about 1% of patients with asymptomatic ICA stenosis have an intracranial aneurysm [12], while the prevalence of intracranial stenosis in patients with extracranial steno-occlusive disease is unknown.
While CTA allows a complete high resolute coverage of both extra- and intracranial arteries, CE-MRA is limited by its coronal acquisition that may exclude part of the more distal posterior circulation and its relative low spatial resolution compared to TOF-MRA [13]. A reconstruction along the sagittal axis is the only one provided most of the times, followed by another common drawback of CE-MRA in the evaluation of the intracranial circulation, that is the presence of possible venous background in the absence of a correct timing. To allow a better coverage of the intracranial circulation at a higher spatial resolution, in our center a 3D-TOF-MRA acquisition centered on the intracranial circulation is also added to the standard CE-MRA acquisition, with multiple reconstructions and optimal background suppression.
The aim of this study was is to verify the correlation of CE-MRA and 3D-TOF MRA in the detection of intracranial vascular lesions. The presence of a good correlation between the two techniques would allow to rely on CE-MRA also to depict intracranial associated pathologies also shortening the acquisition time
Materials and methods
Patients
This is retrospective study approved by our institutional review board, and informed consent was waived. Patients were enrolled on the suspicious of vascular abnormality on CTA or Doppler ultrasounds, such as stenosis or dissection.
MR imaging
MR imaging was performed on a 3-T whole-body MR imaging system (Philips Medical Systems, Best, Netherlands) using a head and neck array coil. The MRI protocol comprised three axial HR images (T2-weighted [T2WI]; T1-weighted [T1WI], FLAIR), diffusion weighted images, CE-MRA for the evaluation of both extra and intracranial vessels. A 3D-TOF MRA was also performed to assess intracranial circulation.
CE-MRA
CE-MRA was performed in the coronal plane immediately after 3D-TOF-MRA. Contrast material (Gadobutrol - 0.1 mmol/kg) was injected via the ante-cubital vein at a rate of 2.5 ml/s followed by a saline (0.9%) bolus of 20 ml at 2.5 ml/s. The 3D volume was acquired with the following imaging parameters: TR, 4.3 ms; TE, 1.59 ms, field-of-view 320 × 320 × 75, matrix size 456 × 456. Parallel image acquisition using GRAPPA (Generalized Autocalibrating Partially Parallel Acquisition) algorithm was applied with an acceleration factor of 2. Voxel dimensions for reconstructions were 0.5 × 0.5 × 0.5 mm.
3D-TOF-MRA
The 3D volume was positioned in an axial orientation at the level of the internal carotid artery with the following imaging parameters: repetition time (TR) 23 ms, echo time (TE) 3.5 ms, field of view 200 × 200 × 94 mm; matrix size 500 × 399; chunk thickness 18.9. Parallel image acquisition using GRAPPA (Generalized Autocalibrating Partially Parallel Acquisition) algorithm was applied with an acceleration factor of 2.8. Voxel dimensions for reconstructions were 0.298 × 0.298 × 0.45 mm. Complete coverage included internal carotid and vertebral arteries from C1.
Imaging analysis
3D-TOF-MRA and CE-MRA were reviewed separately and in random order by two independent neuroradiologists.
The presence and location of intracranial stenosis was qualitatively determined on axial and coronal view (from C1 to the pericallosal artery). Percentage of stenosis was graded as:
-
score of 1 ( ≤ 50%);
-
score 2 (> 50% e < 70%);
-
score 3 for occlusion ( ≥ 70%).
Presence of carotid or vertebral dissection was determined (from C1 to the intracranial tracts). Arterial dissection was determined according to the presence of at least one of the following MR findings:
-
Mural hematoma;
-
Dissecting pseudo-aneurysms;
-
Stenosis.(suspected for dissection according to site and/or shape).
The presence, location, shape, and maximum diameter of intracranial aneurysms were assessed
Statistics
Stenosis grades determined by 3D-TOF and CE-MRA were compared using the Spearman rank correlation coefficient. The presence of dissection and the agreement between 3D-TOF and CE-MRA in the assessment of mural hematoma, dissecting aneurysms, and stenosis were made using Spearman rank correlation coefficient. A p value ≤ 0.05 was considered statistically significant. Cohen’s Kappa was used to evaluate interrater reliability. The analysis was carried out using IBM Statistic SPSS software, ver.20.
Results
A total number of 108 patients was enrolled in our study. There were 43 female patients (mean age 53 years old, range 27–94 years old) and 65 male patients (mean age 53 years old, range 29–76 years old). Interrater agreement was very good for both TOF MRA (κ = 0.9) and CE-MRA (κ = 0.85).
-
1.
Assessment of intracranial stenosis
CE-MRA detected 38 stenosis: 42% of them were grade 1 (16/38), 42% of them were grade 2 (16/38), 16% of them were grade 3 (6/38). 3D-TOF-MRA detected 55 stenosis: 40% of them were grade 1 (22/55), 40% were grade 2 (22/55), and 20% were grade 3 (11/55). Table 1 shows the regional distributions of stenosis for both the techniques. Spearman’s rank correlation coefficient for stenosis detection was calculated to be 0.56 (p = 0.01). Spearman’s rank correlation coefficient for Grade 3 (occlusion) detection was calculated to be 0.57 (p = 0.01). ICA (internal carotid artery from C1) stenosis were all the same identified by both CE-MRA and 3D-TOF-MR. CMA (cerebral middle artery) stenosis were equally identified by CE-MRA and 3D-TOF for grade 1 and grade 2; TOF-MRA detected more grade 3 stenosis. CAA (cerebral anterior artery) stenosis were all the same identified by CE-MRA and 3D-TOF, but a higher number of stenosis was ranked by CE-MRA for grade 2 and by TOF-MRA for grade 3 respectively. With regard to posterior circulation, 3D-TOF ranked a higher number of severe stenosis compared to CE-MRA.
-
2.
Evaluation of dissections
CE-MRA detected 22 findings consistent with dissection (17/22 internal carotid arteries, 5/22 vertebral arteries). 3D-TOF-MRA detected 37 findings consistent with dissections (28/37 internal carotid arteries, 8/37 vertebral arteries, 1/37 basilar artery); they were all detected from C1 all along their intra-cranial course. Spearman’s rank correlation coefficient for the detection of dissection was calculated to be 0.7 (p = 0.01). Spearman’s rank correlation coefficients for the detection of intramural hematoma was of 0.45 (p = 0.036), for the presence of pseudo aneurysm was of 0.56 (p = 0.006), and for the presence of stenosis was of 0.42 (p = 0.049). Table 2 shows the distribution of the different MR findings that were used to identify the presence of dissection at both techniques.
-
3.
Detection of aneurysms
Both CE-MRA and 3D TOF-MRA detected the presence of a total number of 6 aneurysms, of small and large sizes: two of the right middle cerebral artery, one of the left anterior communicating artery, three of the internal carotid artery. They were all saccular aneurysms. All the aneurysms identified at CE-MRA were detected at 3D-TOF-MRA (100%). Spearman’s rank correlation coefficient for aneurysms detection was calculated to be 1 (p = .001).
Discussion
CE-MRA is an established technique for the visualization of the vessels of the supra-aortic vasculature, and has progressively replaced 3D-TOF-MRA as the method of choice in the clinical practice for the imaging of the extracranial carotid circulation [14, 15]. CE-MRA has the ability to produce higher quality images of the entire carotid and vertebro-basilar circulations in a single acquisition and in a much shorter acquisition time [16, 17]. Recent advances in gradient subsystems provided superior temporal resolution by shorter repetition time, thus resulting in greater anatomic coverage. However, this excellent technique carries with itself some early limitations, including a fundamental image-quality-related metric of inadequate spatial resolution as well as undesirable venous enhancement, related to mismatch timing of the MR data acquisition to the arterial contrast bolus passage [18]. The post-processing technique is fast and works extremely well with CE-MRA, since vascular signal is typically much greater than background signal, providing projection images that are quite similar in appearance to conventional angiograms. However, if not properly timed, this algorithm depicts veins and arteries in the same acquisition.
3D TOF-MRA produces high-resolution images, especially when 3D: the 3D acquisitions give high-spatial resolution isotropic imaging and sufficient signal-to-noise ratio, allowing for better visualization of the main arterial and small peripheral intracranial vessels. One of the most known shortcomings of TOF is the saturation of protons in vessels within the imaging section or slab, especially for 3D-TOF, where flow lies within the plane of imaging, limiting the maximum slab thickness of each acquisition, reducing the signal within vessels with consequent stenosis overestimation [19]. Imaging acquisition times are also longer, and motion artifacts may affect the entire exam, not only the single slice [20]. However, the use of a 3-Tesla scan helps improve image quality without an increase in scan time.
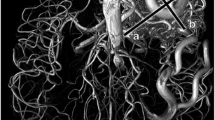
Our results showed that CE-MRA and 3D-TOF-MRA have a good agreement in the detection of intracranial stenosis, especially for the intracranial carotid arteries. For the posterior vertebral circulation, 3D-TOF MRA detected a higher number of vertebral stenosis compared to CE-MRA (Fig. 1). This resulted particularly true when imaging vertebral artery where 3D-TOF MRA estimated more sever grades of stenosis. Previous studies investigated the difference between CE-MRA and 3D TOF-MRA in the evaluation of intracranial stenosis, the latter showing a tendency of stenosis overestimations [7, 21, 22]. Evaluation of posterior circulation with MRA imaging is of outmost importance as both ultrasound and CTA can be invalidated by the presence of an inadequate acoustic window or bone artifacts respectively. It is known that accelerated flow through stenotic areas may lead to overestimate the degree of stenosis [19]. Studies at 3-Tesla imaging for the external and proximal carotid arteries reported that 3D-TOF-MRA might miss classify pseudo-occlusion as complete occlusion (Fig. 2) [5, 7]. The disagreement showed between the two techniques could be explained by this tendency towards overestimation of the 3D-TOF: the absence of a gold standard such DSA to compare our results does not allow to establish the correct evaluation of the degrees of stenosis, but it seems reasonable to think in favor of more false positives obtained by 3D-TOF. The results stress the importance of acquiring CE-MRA in the suspicion of vertebral arteries stenosis due to the great number of false positive occlusion at 3D-TOF MRA.
MRA represents a non-invasive and valuable approach in the diagnosis and evaluation of spontaneous cerebral artery dissection (CAD), and among all sequences contrast-enhanced MRA in combination with fat-suppressed T1w images at 3-Tesla are the most widely used in the current clinical scenario [8]. However, CE-MRA might underestimate the presence of CAD due to the limited spatial resolution, adjacent veins and the tortuous course of the arteries, and may underestimate the presence of intramural hematoma, due to the very short repetition time used for first-pass CE-MRA (Figs. 3 and 4) [23]. On the other hand, 3D-TOF-MRA provides T1 contrast and angiographic information at the same time. It has been proven to have a good sensitivity in the detection of spontaneous CAD, with very good agreement in the detection of stenosis, occlusions, and aneurysms compared to the standard MR protocol [13]. Our results supported these findings: 3D-TOF-MRA detected all the dissections identified by CE-MRA, but, compared to the latter, it is able to depict a higher rate of intramural hematoma, thus resulting in a more accurate diagnosis of dissection. This resulted to be of particular relevance in the absence of stenosis at CE-MRA. The rate of stenosis associated to the presence of dissection detected by the two techniques was different between the two techniques: it may be referred to the already discussed overestimation of arterial stenosis and occlusion related to the 3D-TOF technique, and this is consistent to what previously published [13]. On the other hand, CE-MRA should be the technique of choice in the follow-up of dissections, due to the more accurate assessment of associated pseudo-aneurysm.
Vertebral artery dissection. a, b 3D-TOF source and MIP images show the presence of intramural dissective hematoma at the level of the left verterbral artery, resulting in a moderate stenosis (white arrow). c CE-MRA MIP image shows the presence of a moderate stenosis at the level of the left vertebral artery, without clearly depicting the intramural hematoma but only a moderate stenosis
Vertebral artery dissection. (a, b) Axial 3D-TOF source and MIP images show intramural hematoma in the presence of dissection at the level of the right internal carotid artery. c 3D-TOF MIP images at 2-month follow-up shows the persistence of intramural hematoma that is not clearly detectable on the CE-MRA MIP image (d)
A good consensus was obtained for both the technique in the assessment and evaluation of intracranial aneurysms. Even though our sample was small, our results are in agreement with the literature (Fig. 5). Anzalone et al. previously showed that 3D-TOF-MRA and CE-MRA have both similar accuracy in detecting intracranial aneurysms with a higher accuracy for CE-MRA in larger aneurysms and coiled treated aneurysms. [14].
Our study is a valid proof of the usefulness of CE-MRA not only in the well-known evaluation of the supra-aortic vessels, but also for the intracranial circulation at 3 T imaging. The added benefit is also the chance to shorten the acquisition time. Both radiologists and clinicians have to be aware of the more comprehensive role of CE-MRA in excluding intracranial disease while assessing extracranial pathology.
With regard to limitations, the assessment of intracranial stenosis would have benefit of a comparison with DSA data as it represents the ultimate gold-standard technique for the detection and description of the grade of stenosis. However, data from the literature have already separately established the accuracy of both techniques. In relation to dissections, it is not clear which is the ideal reference technique that shows both vessels stenosis and wall hematoma. As for aneurysms, the aim was to detect the presence, not to specifically evaluate morphology and size description.
Conclusions
In conclusion, our study suggests that CE-MRA of the supraortic vessels can depict the presence of possible associated intracranial aneurysms and stenosis of both anterior and posterior circulation, allowing a consistence examination time reduction. Nevertheless, in case of a suspicious of dissection the acquisition of CE-MRA alone may underestimate the presence of pathology, especially in the absence of vessel stenosis. In this case, a 3D T1-weighted black-blood acquisition should be added to rule out the presence of dissecting hematoma.
References
Campeau NG, Huston J 3rd. (2012 May) Vascular disorders--magnetic resonance angiography: brain vessels. Neuroimaging Clin N Am. 22(2):207–233
Randoux B, Marro B, Koskas F et al (2001) Carotid artery stenosis: prospective comparison of 0ct, three-dimensional gadolinium-enhanced mr, and conventional angiography. Radiology 220(2):179–185
Sundgren PC, Sunden P, Lindgren A et al (2002) Carotid artery stenosis: contrast-enhanced mr angiography with two different scan times compared with digital subtraction angiography. Neuroradiology 44(3):592–599
Alvarez-Linera J, Benito-Leon J, Escribano J et al (2003 May) Prospective evaluation of carotid artery stenosis: elliptic centric contrast-enhanced mr angiography and spiral ct angiography compared with digital. AJNR Am J Neuroradiol. 24(5):1012–1019
Weber J, Veith P, Jung B, Ihorst G, Moske-Eick O, Meckel S, Urbach H, Taschner CA (2015 Mar) MR angiography at 3 Tesla to assess proximal internal carotid artery stenoses: contrast-enhanced or 3D time-of-flight MR angiography? Clin Neuroradiol. 25(1):41–48
Anzalone N, Scotti R, Iadanza A (2006 Apr) MR angiography of the carotid arteries and intracranial circulation: advantage of a high relaxivity contrast agent. Neuroradiology. 48(Suppl 1):9–17
Platzek I, Sieron D, Wiggermann P et al (2014) Carotid artery stenosis: comparison of 3D time-of-flight MR angiography and contrast-enhanced MR angiography at 3T. Radiol Res Pract. 2014:508–715
Bachmann R, Nassenstein I, Kooijman H (2006) Spontaneous acute dissection of the internal carotid artery: high resolution magnetic resonance imaging at 3.0 tesla with a dedicated surface coil. Invest Radiol 41:105–111
Mehdi E, Aralasmak A, Toprak H (2018 Apr) Craniocervical dissections: radiologic findings, pitfalls, mimicking diseases: a pictorial review. Curr Med Imaging Rev. 14(2):207–222
Kidoh M, Nakaura T, Takashima H (2013 Feb) MR diagnosis of vertebral artery dissection: value of 3D time-of-flight and true fast imaging with steady-state precession fusion imaging. Insights Imaging. 4(1):135–142
Winn HR, Jane JA Sr, Taylor J et al (2002) Prevalence of asymptomatic incidental aneurysms: review of 4568 arteriograms. J Neurosurg 96:43–49
Héman LM (2009 Apr) Incidental intracranial aneurysms in patients with internal carotid artery stenosis: a CT angiography study and a metaanalysis. Stroke. 40(4):1341–1346
Coppenrath EM, Lummel N, Linn J (2013) Time-of-flight angiography: a viable alternative to contrast-enhanced MR angiography and fat-suppressed T1w images for the diagnosis of cervical artery dissection? Eur Radiol 23(10):2784–2792
Cirillo M, Scomazzoni F, Cirillo L (2013 Dec) Comparison of 3D TOF-MRA and 3D CE-MRA at 3T for imaging of intracranial aneurysms. Eur J Radiol. 82(12):e853–e859
Scarabino T, Carriero A, Giannatempo GM et al (1999) Contrast-enhanced MR angiography (CE MRA) in the study of carotid stenosis: comparison with digital subtraction angiography (DSA). J Neuroradiol 25:87–91
Aoki S, Nakajima H, Kumagai H, Araki T (2000) Dynamic contrast- enhanced MR angiography and MR imaging of the carotid artery: high-resolution sequences in different acquisition planes. AJNR Am J Neuroradiol 21:381–385
Ersoy H, Watts R, Sanelli P et al (2003) Atherosclerotic disease distri-bution in carotid and vertebrobasilar arteries: clinical experience in 100 patients undergoing fluoro-triggered 3D Gd-MRA. J Magn Reson Imaging 17:545–558
Riederer SJ, Stinson EG, Weavers PT (2018 Jan 10) Technical Aspects of Contrast-enhanced MR angiography: current status and new applications. Magn Reson Med Sci. 17(1):3–12
Korogi Y, Takahashi M, Nakagawa T et al (1997) Intracranial vas-cular stenosis and occlusion: MR angiographic findings. AJNR Am J Neuroradiol 18:135–143
Miyazaki M, Lee VS (2008 Jul) Nonenhanced MR angiography. Radiology. 248(1):20–43
Sadikin C, Teng MM, Chen TY (2007 Sep) The current role of 1.5 T non-contrast 3D time-of-flight magnetic resonance angiography to detect intracranial steno-occlusive disease. J Formos Med Assoc. 106(9):691–699
Hirai T, Korogi Y, Ono K, Nagano M, Maruoka K, Uemura S, Takahashi M (2002) Prospective evaluation of suspected steno-occlusive disease of the intracranial artery:combined MR angiography and CT angiography compared with digital subtraction angiography. AJNR Am J Neuroradiol 23:93–101
Oppenheim C, Naggara O, Touzé E (2009 Sep-Oct) High-resolution MR imaging of the cervical arterial wall: what the radiologist needs to know. Radiographics. 29(5):1413–1431
Author information
Authors and Affiliations
Contributions
Calloni Sonia Francesca: Contributed substantially to the acquisition of data, the analysis and interpretation- Drafted the manuscript.
Perrotta Marianna: conributed to the acquisition of data and the analysis.
Roveri Luisa: provided critical revision of the article. Provided final approval of the version to publish.
Panni Pietro: provided critical revision of the article and made a great contributions to the statistical analysis.
Del Poggio Anna: provided critical revision of the article.
Vezzulli Paolo Quintiliano: provided critical revision of the article.
Filippi Massimo: provided final approval of the version to publish.
Falini Andrea: Provided final approval of the version to publish.
Anzalone Nicoletta: Contributed substantially to the conception and design of the study, the acquisition of data, the analysis, and interpretation. Provided critical revision of the article. Provided final approval of the version to publish.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no compeing interests.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calloni, S.F., Perrotta, M., Roveri, L. et al. The role of CE-MRA of the supraortic vessels in the detection of associated intracranial pathology. Neurol Sci 42, 5131–5137 (2021). https://doi.org/10.1007/s10072-021-05222-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05222-1