Abstract
A 68-year-old male with gastric cancer was treated with tegafur/gimeracil/oteracil and oxaliplatin for 6 months. Thereafter, he was treated with paclitaxel and ramucirumab for 3 months. However, neither regimen had much effect. Thus, he was treated with nivolumab for 2 months, but he developed proteinuria, microhematuria, and an acute kidney injury. A kidney biopsy revealed occasional swollen endothelial cells and proliferating mesangial cells. Few abnormal findings were seen in the tubules or interstitial tissue. Immunofluorescent staining showed segmental immunoglobulin A and complement component 3 deposition, in the mesangial area. Electron microscopy showed a small amount of electron-dense deposits in the paramesangial area and swollen endothelial cells. Mesangial interposition, the loss of endothelial cell fenestration, and subendothelial edema were also observed. Furthermore, foot process effacement and villous transformation of epithelial cells were noted. After the discontinuation of nivolumab, the patient’s renal function gradually improved, and his proteinuria disappeared. Nivolumab treatment was restarted at that time because of cancer progression; however, it was ineffective. No occult blood was detected from 7 months after the administration of the last dose of nivolumab. This is a unique case, in which a kidney biopsy revealed evidence of nivolumab-associated glomerular endothelial injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immune checkpoint inhibitors (ICI) are increasingly being used to treat cancer, ICI are associated with a unique category of side effects, which are termed immune-related adverse events (irAE) [1].
Nivolumab is a human immunoglobulin (Ig)G4 anti-programmed cell death 1 monoclonal antibody, which is designed to augment immunological reactions against cancer cells.
Nivolumab-associated kidney injuries are less common than nivolumab-associated injuries affecting other organs, but they are very important. Kidney injuries commonly present as acute tubulointerstitial nephritis [2, 3], whereas glomerular disease is rare.
In this report, we present a case of nivolumab-associated glomerular endothelial injury in a patient with gastric cancer.
Case report
A 68-year-old male was diagnosed with stage IV gastric cancer 11 months prior to admission and was treated with tegafur/gimeracil/oteracil and oxaliplatin for 6 months. Thereafter, he was treated with paclitaxel and ramucirumab for 3 months. However, neither regimen had much effect. Thus, the patient was treated with nivolumab (3 mg/kg) every 2 weeks. At the time of the administration of the first dose of nivolumab, his serum creatinine concentration was 0.77 mg/dL, and urinalysis showed a protein value of 1+ and an occult blood value of 2+, but 1–4 red blood cells per high-power field were present in his urinary sediment. His urinary protein level was increased at 1 month after the start of nivolumab treatment, and 30–49 red blood cells per high-power field were detected in his urinary sediment a month and a half after the start of nivolumab treatment. At 2 months after the start of the nivolumab treatment, the patient had lost 3 kg in weight and developed diarrhea, and his serum creatinine concentration had risen from 0.77 to 1.96 mg/dL. His total protein excretion was 0.87 g/day, his urinary protein to creatinine ratio was 1.73 g/gCr, and his urinary sediment contained dysmorphic red blood cells and > 100 red blood cells per high-power field. His urinary sodium level was 29 mEq/L, and fractional excretion of sodium was 0.21%. He had taken lansoprazole, loperamide, and clostridium butyricum preparations.
On admission, his height was 170.5 cm, and his weight was 55.0 kg. His blood pressure was 93/62 mmHg, and he had a regular heartbeat of 83 beats/min and a temperature of 36.2 °C. A physical examination did not produce any remarkable findings.
Blood tests revealed the following (Table 1): red blood cell count: 302 × 104/μL, hemoglobin level: 9.9 g/dL, hematocrit level: 29.4%, white blood cell count: 3200/μL, platelet count: 10.8 × 104/μL, serum total protein level: 5.7 g/dL, serum albumin level: 2.1 g/dL, and blood urea nitrogen level: 19 mg/dL. Immunological examinations produced the following results: serum IgG: 1898 mg/dL, IgA: 339 mg/dL, IgM: 134 mg/dL, 50% hemolytic complement activity (CH50): 59 U/mL, complement component (C)3: 97 mg/dL, C4: 36 mg/dL, and anti-nuclear antibodies: 40× . Tests for myeloperoxidase anti-neutrophil cytoplasmic antibodies (ANCA), proteinase 3 ANCA, and anti-glomerular basement membrane antibodies produced negative results, as did tests for the hepatitis B surface antigen, and the anti-hepatitis C virus antibody. Urinary test revealed the following (Table 1): α1 microglobulin: 10.7 mg/L (normal range: < 8.3 mg/L), β2 microglobulin: 131 μg/L (normal range: < 250 μg/L).
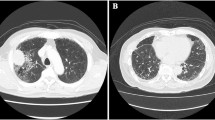
Light microscopy revealed 26 glomeruli, 1 of which exhibited global sclerosis. The remaining glomeruli showed occasional swollen endothelial cells and proliferating mesangial cells (Fig. 1a and b). Few abnormal findings were seen in the tubules or interstitial tissue (Fig. 1c). Immunofluorescent staining revealed segmental IgA (1+) and C3 (1+) deposition in the mesangial area (Fig. 2a). Staining of IgG, IgM, C4, and C1q produced negative results. Electron microscopy showed a small amount of electron-dense deposits in the paramesangial area and swollen endothelial cells (Fig. 2b). Mesangial interposition (Fig. 2c), the loss of endothelial cell fenestration, and subendothelial edema (Fig. 2d) were also observed. Furthermore, foot process effacement and villous transformation of epithelial cells were noted (Fig. 2d).
Immunofluorescent staining and electron microscopy. a Immunofluorescent staining of Immunoglobulin A deposits in the mesangial area. b A small amount of electron-dense deposits in the paramesangial area (arrow) and swollen endothelial cells. c Mesangial interposition. d Loss of fenestration of endothelial cells, subendothelial edema, foot process effacement and villous transformation of epithelial cells
The patient was not treated with steroids because it was considered that dehydration had contributed to the acute kidney injury, and his kidney function gradually improved (Fig. 3). One month and a half after the discontinuation of nivolumab, his proteinuria disappeared (Fig. 3). Nivolumab treatment was restarted at that time because of cancer progression; however, it was ineffective (Fig. 3). Therefore, irinotecan was administered instead by the oncologist (Fig. 3). No occult blood was detected from 7 months after the administration of the last dose nivolumab (Fig. 3).
Discussion
irAE are becoming more common with the increasing use of ICI. ICI block T cell inhibition and stimulate immunological responses towards cancer cells, but they can also impair the self-tolerance of the immune system. irAE are known to occur in the gastrointestinal tract, lung, liver, and endocrine system [4]. Renal irAE are less common than irAE affecting other organs. ICI-related acute kidney injuries were reported to occur in 2.2% of patients [2]. However, recent studies have suggested that renal irAE might be more common than has previously been reported [5].
As mentioned earlier, acute tubulointerstitial nephritis is the most common renal irAE induced by nivolumab [2, 3]. Cases of nivolumab-associated glomerular disease are rare, but are being reported increasingly, which include IgA nephropathy [6,7,8], focal segmental necrotizing pauci-immune glomerulonephritis [8], membranous nephropathy [8], crescentic glomerulonephritis [9], and focal segmental glomerulosclerosis [10].
The mechanisms underlying renal irAE are unknown, but several hypotheses, which are primarily based on non-renal irAE and partially based on renal irAE in mouse models, have been suggested [11]. The potential mechanisms include: (1) the formation of new or reactivated T cells that target tumor antigens but cross-react with off-target kidney tissues, (2) the loss of tolerance combined with ICI-induced reactivation of drug-specific T cells, (3) an increase in proinflammatory cytokines/chemokine levels in kidney tissue, and (4) the generation of autoantibodies (anti-kidney tissue antibodies). However, the reason why various pathological types of kidney injury are found in patients that suffer renal irAE is not well understood.
There have been some previous reports about nivolumab-associated glomerulonephritis with IgA deposition, although there were some differences in the clinical and pathological findings between the present and previous cases [6,7,8]. In the present case, the time from the administration of nivolumab until urinary abnormalities were detected was short. Moreover, the renal damage appeared to involve endothelial injuries because electron microscopy showed swollen endothelial cells, mesangial interposition, the loss of endothelial cell fenestration, and subendothelial edema. Foot process effacement and villous transformation of epithelial cells are indicative of epithelial damage. Therefore, it is possible that IgA deposition had occurred previously.
As mentioned above, the pathological findings of the present case represented endothelial injuries. Only one case of ipilimumab-associated endothelial injury has been reported previously [2]. Light microscopy showed diffusely distributed wrinkled glomerular basement membranes and ‘onion skin’ lesions of the small arteries. On electron microscopy, a swollen endothelium and subintimal widening filled with electron-lucent ‘fluffy’ material were detected. The patient’s renal function did not recover after glucocorticoids therapy. The pathogenetic mechanism responsible for the endothelial injuries in these two cases are unclear; therefore, the accumulation of the similar cases will be necessary.
The proteinuria and reduced renal function seen in the current case seemed to have been caused by the nivolumab therapy (Fig. 3), although hematuria persisted for long time after the cessation of nivolumab treatment. We frequently experience cases in which hematuria remains for a long time, even if proteinuria disappears, during steroid treatment for other types of nephritis, such as IgA nephritis or ANCA-related nephritis. Therefore, mild renal injuries might have remained for a while after the cessation of nivolumab treatment.
In the current case, we need to consider the effects of the gastric cancer and the fact that chemotherapeutic agents were administered before nivolumab. Gastric cancer might be related to membranous nephropathy, membranoproliferative nephropathy, crescentic glomerulonephritis, and thrombotic microangiopathy [12, 13], and a case of ramucirumab- associated thrombotic microangiopathy was reported previously [14]. However, urinary abnormalities developed after the discontinuation of ramucirumab, and these abnormalities were ameliorated after the cessation of nivolumab treatment, although the patient’s cancer was not cured. Therefore, renal damage in the present case was possible to associated with nivolumab administration.
Recently, programmed cell death ligand-1 (PD-L1) immunohistochemical findings in kidney biopsy specimens from patients on anti-PD-1 therapy was reported [15]. Positive PD-L1 staining of tubular epithelial cell membranes and inflammatory cells was seen in patients with anti-PD-1 therapy-associated acute interstitial nephritis (AIN), but not in patients with anti-PD-1 therapy-associated acute tubular necrosis or those with AIN secondary to other medications. In the present case, anti-PD-L1 was partially detected on tubular epithelial cell membranes and inflammatory cells, not on glomeruli (Supplementary Figs. 1a–d).
irAE can be managed via treatment interruption and occasional corticosteroid treatment. We did not treat our patient with steroids because his pathological findings were not severe, and the acute kidney injury was also considered to have been caused by dehydration. His kidney function gradually improved after the cessation of nivolumab treatment.
In conclusion, we reported a newly diagnosed case of nivolumab-associated glomerular endothelial injury. Renal biopsies should be performed to obtain an adequate diagnosis and ensure appropriate treatment in such cases.
References
Champiat S, Lambotte O, Barreau E, Belkhir R, Berdelou A, Carbonnel F, et al. Management of immune checkpoint blockade dysimmune toxicities: a collaborative position paper. Ann Oncol. 2016;27(4):559–74.
Cortazar FB, Marrone KA, Troxell ML, Ralto KM, Hoenig MP, Brahmer JR, et al. Clinicopathological features of acute kidney injury associated with immune checkpoint inhibitors. Kidney Int. 2016;90(3):638–47.
Shirali AC, Perazella MA, Gettinger S. Association of acute interstitial nephritis with programmed cell death 1 inhibitor therapy in lung cancer patients. Am J Kidney Dis. 2016;68(2):287–91.
Spain L, Diem S, Larkin J. Management of toxicities of immune checkpoint inhibitors. Cancer Treat Rev. 2016;44:51–60.
Wanchoo R, Karam S, Uppal NN, Barta VS, Deray G, Devoe C, et al. Adverse renal effects of immune checkpoint inhibitors: a narrative review. Am J Nephrol. 2017;45(2):160–9.
Jung K, Zeng X, Bilusic M. Nivolumab-associated acute glomerulonephritis: a case report and literature review. BMC Nephrol. 2016;17(1):188.
Kishi S, Minato M, Saijo A, Murakami N, Tamaki M, Matsuura M, et al. IgA nephropathy after nivolumab therapy for postoperative recurrence of lung squamous cell carcinoma. Intern Med. 2018;57(9):1259–63.
Mamlouk O, Selamet U, Machado S, Abdelrahim M, Glass WF, Tchakarov A, et al. Nephrotoxicity of immune checkpoint inhibitors beyond tubulointerstitial nephritis: single-center experience. J Immunother Cancer. 2019;7(1):2.
Takahashi N, Tsuji K, Tamiya H, Shinohara T, Kuroda N, Takeuchi E. Goodpasture’s disease in a patient with advanced lung cancer treated with nivolumab: an autopsy case report. Lung Cancer. 2018;122:22–4.
Daanen RA, Maas RJH, Koornstra RHT, Steenbergen EJ, van Herpen CML, Willemsen A. Nivolumab-associated nephrotic syndrome in a patient with renal cell carcinoma: a case report. J Immunother. 2017;40(9):345–8.
Perazella MA, Shirali AC. Nephrotoxicity of cancer immunotherapies: past, present and future. J Am Soc Nephrol. 2018;29(8):2039–52.
Lien YH, Lai LW. Pathogenesis, diagnosis and management of paraneoplastic glomerulonephritis. Nat Rev Nephrol. 2011;7(2):85–95.
Jhaveri KD, Shah HH, Calderon K, Campenot ES, Radhakrishnan J. Glomerular diseases seen with cancer and chemotherapy: a narrative review. Kidney Int. 2013;84(1):34–44.
Yamada R, Okawa T, Matsuo K, Suzuki M, Mori N, Mori K. Renal-limited thrombotic microangiopathy after switching from bevacizumab to ramucirumab: a case report. BMC Nephrol. 2019;20(1):14.
Cassol C, Satoskar A, Lozanski G, Rovin B, Hebert L, Nadasdy T, et al. Anti-PD-1 immunotherapy may induce interstitial nephritis with increased tubular epithelial expression of PD-L1. Kidney Int Rep. 2019;4(8):1152–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have declared that no conflicts of interest exist.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patient in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
13730_2021_610_MOESM1_ESM.png
Supplementary Fig. 1 Immunohistochemistry performed with PD-L1 antibodies. a: PD-L1 staining of the tubular epithelial cell membrane (PNG 902 kb)
About this article
Cite this article
Shim, J., Tochio, A., Ueda, N. et al. Nivolumab-associated glomerular endothelial injury in a patient with gastric cancer. CEN Case Rep 10, 576–581 (2021). https://doi.org/10.1007/s13730-021-00610-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13730-021-00610-0