Abstract
Purpose of Review
Evidence from observational studies suggests that obesity is associated with low vitamin D. As both obesity and hypovitaminosis D present an alarmingly increased prevalence worldwide, there is an intense research interest to clarify all aspects of this association. This review summarizes current evidence from meta-analyses investigating vitamin D status in obesity, including the effects of weight loss and bariatric surgery on vitamin D status and the outcomes of vitamin D supplementation on body weight. We also discuss potential pathophysiologic mechanisms and important controversies.
Recent Findings
Data from meta-analyses consistently support an inverse association of vitamin D levels with body weight. However, the impact of weight loss on improving vitamin D status is small, while studies on the supplementation with vitamin D after bariatric surgery have shown conflicting results regarding vitamin D status. Moreover, interventional studies do not support a beneficial effect of vitamin D supplementation on body weight. These findings warrant a cautious interpretation due to important methodological limitations and confounding factors, such as high heterogeneity of studies, variable methods of determination of vitamin D and definition of deficiency/insufficiency, use of various adiposity measures and definitions of obesity, and inadequate adjustment for confounding variables influencing vitamin D levels. The underlying pathogenetic mechanisms associating low vitamin D in obesity include volumetric dilution, sequestration into adipose tissue, limited sunlight exposure, and decreased vitamin D synthesis in the adipose tissue and liver. Experimental studies have demonstrated that low vitamin D may be implicated in adipose tissue differentiation and growth leading to obesity either by regulation of gene expression or through modulation of parathyroid hormone, calcium, and leptin.
Summary
Obesity is associated with low vitamin D status but weight loss has little effect on improving this; vitamin D supplementation is also not associated with weight loss. Evidence regarding vitamin D status after bariatric surgery is contradicting. The link between vitamin D and obesity remains controversial due to important limitations and confounding of studies. More research is needed to clarify the complex interplay between vitamin D and adiposity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a multifactorial chronic state of positive energy balance and excessive fat accumulation, associated with decreased life expectancy [1]. During the last 50 years, obesity rates have increased worldwide, with major implications to public health and the economy. It has been estimated that over 650 million adults (approximately 13% of the world’s adult population) have obesity, while over 340 million children and adolescents aged 5–19 years presented overweight or obesity in 2016 [2]. Evidence from the National Health and Nutrition Examination Survey (NHANES) has indicated that the age-adjusted prevalence of obesity among US adults was 42.4% in 2017–2018 [3].
Somewhat paradoxically, given that overconsumption of food is an important driver of positive energy balance leading to obesity, patients with obesity often present with micronutrient deficiencies, with hypovitaminosis D being one of them [4]. Vitamin D is naturally present in few foods (i.e., oily fish, cod liver oil, sun-dried mushrooms, as well as fortified foods including milk, orange juice, margarine, and cooking oil); in large part, it is endogenously synthesized when solar ultraviolet rays (290–315 nm) enhance vitamin D synthesis in the skin that is then mostly stored in adipose tissue [5]. As adipose tissue constitutes quantitatively the most important storing compartment, it is possible that the global obesity epidemic could partly explain the high prevalence of hypovitaminosis D worldwide. Despite the plentiful sunshine, hypovitaminosis D is observed at high rates in Africa, India, Australia, Asia, South America, and, surprisingly, the Middle East [6]. Serum 25-hydroxyvitamin D (25(OH)D) is often used as an index of vitamin D nutritional status and, besides obesity, risk factors for low 25(OH)D levels include extremes of age, female sex, malnutrition, dark skin phototype, winter season, low socioeconomic status, and covered clothing style [6]. Vitamin D receptors (VDRs) are expressed in a plethora of tissues and cells, while the pleiotropic actions of vitamin D in non-skeletal outcomes have become increasingly recognized [7].
While there is consensus that serum 25(OH)D concentrations should be used to assess vitamin D status, because it reflects the contribution of both diet and endogenous synthesis, there has been a debate on the suggested thresholds to define low vitamin D status or hypovitaminosis D (deficiency and insufficiency) [8]. Previous guidelines define vitamin D deficiency as 25(OH)D values below 50 nmol/L (20 ng/mL) and vitamin D insufficiency as 25(OH)D values of 50–75 nmol/L (20–30 ng/mL) [9]. However, in a most recent consensus statement, vitamin D deficiency is defined as 25(OH)D values below 30 nmol/L (12 ng/mL) and vitamin D insufficiency as 25(OH)D values between 30 and 50 nmol/L (12–20 ng/mL), while levels between 50–125 nmol/L (20–50 ng/mL) are considered safe and sufficient regarding skeletal health in the general population [10]. These definitions are endorsed by the US Institute of Medicine, while a concentration above 75 nmol/L (30ng/mL) is recommended by the US Endocrine Society for optimal health benefit particularly in elderly subjects with augmented risk of fractures as well as osseous, renal and digestive disorders [9, 11].
Data from large observational studies (NHANES III and Framingham) suggest that obesity is associated with an increased risk of hypovitaminosis D [12, 13]. Although vitamin D is mostly known for its role in calcium homeostasis and bone health, this multifaceted hormone exerts pleiotropic actions regarding metabolism, immunity and cellular proliferation and differentiation, with anti-inflammatory, anti-atherogenic, cardioprotective and neuroprotective effects, among others [14, 15]. Besides obesity, hypovitaminosis D is strongly associated with risk factors of metabolic syndrome, such as dyslipidemia, insulin resistance, and arterial hypertension, with serious implications in cardiometabolic risk and morbidity [16, 17]. Hypovitaminosis D is growing into a worldwide epidemic, with prevalence rates as high as 13% for deficiency and 40% for insufficiency in the North American and the European population and even higher rates in the Asian populations [18].
Apparently, obesity and hypovitaminosis D represent two concurrent pandemics undermining public health globally. Therefore, there has been significant interest in investigating this association and the underlying pathophysiologic mechanisms. Numerous observational studies have explored vitamin D status in relation to body weight [19]. Additionally, many important questions and considerations have arisen regarding the direction of this relationship: is obesity the cause of low vitamin D, or is low vitamin D responsible for the increasing rates of obesity? To address these questions, many interventional studies aimed at exploring the effect of weight loss on vitamin D levels and, conversely, the effect of vitamin D supplementation on body weight; however with inconsistent results. Furthermore, recent experimental studies aimed at investigating molecular mechanisms and genetic factors linking vitamin D to obesity [20,21,22].
Herein, we present evidence from meta-analyses regarding vitamin D status in obesity, the effect of weight loss and bariatric surgery on vitamin D levels, as well as the effect of vitamin D supplementation on body weight homeostasis. We also discuss important controversies stemming from methodological limitations and inconsistencies among studies. Finally, we highlight potential pathophysiologic mechanisms that may explain the bi-directional link between obesity and low vitamin D.
Literature Search
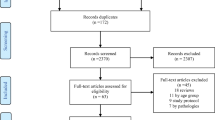
A search of the literature was performed in reliable biomedical databases (PubMed/MEDLINE, Scopus and Google Scholar) to identify articles published through November 2020. The search terms “vitamin D” or “25-hydroxyvitamin D” or “25OHD” or “vitamin D deficiency” or “vitamin D insufficiency” or “hypovitaminosis D” or “vitamin D supplementation” and “obesity” or “overweight” or “body weight” or “body mass index” or “BMI” or “body fat” or “adiposity” or “ adipose tissue” or “weight loss” or “bariatric surgery” were used. No restrictions in publication date, language or age of study participants were applied. We selectively included only meta-analyses in our review. Observational studies, clinical studies, randomized controlled trials (RCTs), and reviews without a meta-analysis were excluded. We also reviewed the references of included articles to identify any additional meta-analyses.
Evidence from Meta-analyses
Table 1 summarizes the characteristics and main findings of meta-analyses regarding vitamin D and obesity. These meta-analyses have investigated various aspects of the association between vitamin D and obesity: (1) the association between obesity and vitamin D status; (2) the effect of weight loss on vitamin D levels; (3) the effect of bariatric surgery on vitamin D status; and (4) the effect of vitamin D supplementation on various adiposity outcomes.
Is Obesity Associated with Vitamin D Status?
Seven meta-analyses, published between 2013 and 2018, have addressed the association between obesity and vitamin D status. Thirty-four cross-sectional studies were analyzed by Saneei et al. and a weak but significant inverse association between vitamin D levels and body mass index (BMI) was found [23]. The association was observed in both genders in developed countries and only in males in developing ones. A large meta-analysis of 21 population-based studies used information from 42,024 adults to explore any causal association between obesity and vitamin D status [24••]. A bi-directional Mendelian randomization analysis of large cohorts was performed showing that obesity may lead to low vitamin D and not vice versa. Specifically, every unit increase in BMI (1 kg/m2) was associated with a decrease in 25(OH)D by 1.15%, after adjusting for age, gender and other confounders.
A subsequent meta-analysis of 12 observational studies concluded that obesity, defined as BMI >30 kg/m2, was associated with an increased risk for vitamin D insufficiency/deficiency (< 50 nmol/L) (RR 1.52, 95% CI: 1.33–1.73) in subjects of all ages [25]. Another meta-analysis of 23 observational studies reporting vitamin D levels in subjects with normal weight, overweight and obesity (excluding severe obesity) demonstrated that vitamin D deficiency (defined as 25(OH)D < 50 nmol/L) was 24% and 35% more prevalent in subjects with overweight and obesity, respectively, compared to those with normal weight [26••]. The association of vitamin D deficiency with obesity was found to be independent of age, latitude, vitamin D deficiency definition and the developmental status of the country where studies were conducted.
A recent meta-analysis of 55 studies confirmed the inverse association of vitamin D with BMI [27]. Interestingly, the study showed that this association is stronger in patients with type 2 diabetes mellitus (DM2) and is affected by BMI. Notably, in non-diabetic subjects, the association was weak among those in the normal BMI range and became gradually stronger with increasing BMI. In patients with DM2, there was an abrupt increase in the strength of this association in subjects with BMI >30 kg/m2 [27]. The association of fat mass (FM) and percentage of fat mass (PFM) with vitamin D status was investigated by Golzarand et al. based on 35 observational studies [28]. An inverse association was found which was independent of age, latitude or longitude. Finally, a meta-analysis of vitamin D in female subjects with or without polycystic ovary syndrome (PCOS) has shown that waist-hip ratio (WHR) was a negative predictor of vitamin D status, independent of BMI [29]. This study analyzed data from 14 case-controlled studies with 2262 participants. However, most of these studies were not randomized and did not adjust for confounding factors, limiting the value of this finding.
Overall, results from meta-analyses support an inverse relationship between measures of adiposity and vitamin D levels, with a stronger association in subjects with obesity than those with a normal weight. Additionally, there is some evidence to suggest a causal role of obesity in low vitamin D levels.
Does Weight Loss Affect Vitamin D Levels?
The effect of weight loss on vitamin D levels was examined in 2 meta-analyses. Mallard et al included 4 randomized and 11 non-randomized controlled trials aiming at investigating whether weight loss after dietary and/or exercise interventions results in an increase in serum 25(OH)D compared to weight maintenance, under similar supplemental vitamin D intake [30•]. The authors concluded that weight loss is associated with a small but significant increase in serum 25(OH)D, but they did not find any evidence of a dose-response effect between weight loss and 25(OH)D increase.
A recent meta-analysis of 23 studies in subjects with overweight and obesity found that weight and PFM loss after caloric restriction and/or exercise were associated with marginally significant increases in 25(OH)D (p=0.05 and p=0.06, respectively [31]. However, this meta-analysis acknowledged a number of important limitations such as a possible seasonal effect on vitamin D status and a wide variation in methodology of the included studies regarding vitamin D determination as well as body composition measurements.
Collectively, these results suggest that weight loss presents little beneficial effect on vitamin D status. Given the small number and the heterogeneity of the studies analyzed as well as various methodological issues, more studies are needed to elucidate this issue.
Does Bariatric Surgery Affect Vitamin D Levels?
Bariatric surgery included a variety of surgical procedures in the treatment of obesity, showing greater efficacy regarding weight loss than any other approach [42]. However, it is associated with a higher risk of vitamin and mineral deficiencies, including vitamin D and calcium, due to limited dietary intake and reduced gut absorption [43]. Meta-analyses on bariatric surgery have focused on the effects of vitamin D supplementation on vitamin D status after surgery as well as implications in bone metabolism.
A meta-analysis of 10 prospective observational studies, including 344 patients with severe obesity who underwent bariatric surgery (Roux-en-Y gastric bypass), demonstrated that 25(OH)D did not change significantly after surgery, while calcium decreased and parathyroid hormone (PTH) increased [32]. Of note, vitamin D and calcium supplementation postoperatively was reported in all studies, while duration of follow-up was 6–36 months. However, bone mineral density was significantly decreased, indicating bone loss after surgery, despite vitamin D and calcium supplementation. There was a high heterogeneity between studies regarding the doses and the duration of supplemental vitamin D.
Another meta-analysis investigated the change in vitamin D status after bariatric surgery compared to non-surgical controls with obesity [33•]. It included 7 controlled studies (2 RCTs), but only 3 assessed 25(OH)D levels. There were no significant differences in percent change of 25(OH)D from baseline between the bariatric surgery group and controls at 12 and 24 months after inclusion to the study, although there was a trend for a higher increase in vitamin D in the control group. However, data on vitamin D supplementation were not reported. Also, there were no data on weight loss after surgery or on weight loss interventions-if any-in the control group. The limited number of studies, the small sample size, and the high heterogeneity are the most important limitations of the above meta-analysis.
Vitamin D deficiency was investigated in a meta-analysis of 12 prospective studies (6 RCTs) of 1285 subjects with obesity after bariatric surgery, who received vitamin D supplementation [34]. Vitamin D supplementation was associated with significant improvement in 25(OH)D levels 1 year after bariatric surgery, independently of study design, baseline levels, weight loss and vitamin D dosage. Also, vitamin D deficiency decreased from 54% preoperatively to 31% 1 year postoperatively. The difference in the prevalence of vitamin D deficiency was significant only in RCTs and with vitamin D daily doses above 800 IU. The greater improvement in 25(OH)D was observed in patients with a normal baseline 25(OH)D and those who were submitted to Roux-en-Y gastric bypass, compared to those with vitamin D deficiency at baseline and to laparoscopic gastric bypass.
Finally, a recent meta-analysis of 13 studies published between 2010 and 2018 compared gastric bypass to sleeve gastrectomy regarding bone metabolism and related complications [35]. This meta-analysis showed that circulating 25(OH)D and calcium were significantly lower after gastric bypass compared to sleeve gastrectomy. Interestingly, BMI and bone mineral density after these procedures were similar. The doses of supplemental vitamin D and calcium were not reported and the duration of postoperative follow-up was 12 months in most of the included studies. Sleeve gastrectomy is a restricted procedure, while gastric bypass is both restricted and malabsorptive. These findings suggest that current vitamin D supplementation strategies after malabsorptive bariatric surgery are insufficient and they should be reconsidered.
Overall, the above meta-analyses are inconclusive regarding vitamin D status after bariatric surgery. Besides the high heterogeneity and the small number of selected studies, the variable vitamin D supplementation strategies present the most important confounding factor. However, Li et al suggested that vitamin D supplementation with a daily dosage of more than 800 IU may be effective in preventing postoperative vitamin D deficiency and enhancing serum 25(OH)D levels [34].
Does Vitamin D Supplementation Affect Adiposity Measures?
The effect of vitamin D supplementation on obesity has been the subject of a large number of interventional clinical studies, most of them being RCTs. Eight meta-analyses published in the last few years have focused on this particular topic. A meta-analysis of 12 RCTs investigated the effect of vitamin D supplementation on various measures of adiposity, namely BMI, FM, and PFM, in the absence of caloric restriction [36]. The intervention group received vitamin D3 (calcitriol) in various doses ranging from 20 to 7000 IU/day, or 20,000 to 40,000 IU/week, or 50,000 IU every 20 days or 120,000 IU three times fortnightly. Most subjects were adults with obesity or overweight, but adolescents and children above 10 years of age were included in 2 studies. The duration of the studies ranged from 1 month to 3 years. The meta-analysis showed that vitamin D supplementation did not decrease any measure of adiposity. Furthermore, body weight was not influenced by either the absolute vitamin D status achieved or its change from baseline. However, 8 of 12 RCTs favored a reduction in BMI following vitamin D supplementation albeit this did not reach statistical significance. Age and gender emerged as potential confounding factors, with younger people and females being more likely to experience a decrease in FM following vitamin D supplementation.
Another meta-analysis of 26 RCTs (including 8 of the 12 RCTs of the meta-analysis by Pathak et al.) with 42,430 adult participants and a median treatment duration of 12 months failed to demonstrate any significant effects on body weight, BMI or FM following vitamin D supplementation (daily dose range 300–12,695 IU D3) with or without calcium [37•]. Only 3 studies included dietary weight loss interventions with caloric restriction. Furthermore, this meta-analysis found no evidence to support a dose-response relationship between vitamin D3 and any measure of adiposity. Manousopoulou et al. performed a meta-analysis of 9 RCTs including 1586 otherwise healthy adults with overweight or obesity and found that vitamin D supplementation had no effect on body weight or BMI [38]. The duration of the intervention ranged from 6 weeks to 4 years with doses of vitamin D ranging from 1000 IU/day to 120,000 IU fortnightly. The small number of studies and the lack of adjustment for age and other confounding factors limit the value of this meta-analysis.
The meta-analysis of Mallard et al. included 15 randomized and non-randomized controlled trials and demonstrated that vitamin D supplementation (median daily dose of 350 IU) combined with caloric restriction and/or exercise had no effect on weight loss [30•]. Golzarand et al. also showed that vitamin D supplementation had no effect on PFM in adults based on results from 10 RCTs [28]. A meta-analysis of 11 RCTs investigating the effect of vitamin D3 supplementation (dose range 25,000–600,000 IU/month) on weight loss in subjects with overweight or obesity yielded contradicting results, in that weight loss was not affected by vitamin D, but waist circumference (WC) was significantly reduced [39]. The mixed results may be attributed to the fact that vitamin D supplementation was combined with weight-loss interventions, such as exercise and caloric restriction, in 3 of the RCTs analyzed. Likewise, a recent meta-analysis of 20 RCTs and 1,146 participants of all ages explored the effect of vitamin D fortified diet on various anthropometric indices and concluded this diet significantly decreased WC and WHR, but had no effect on body weight, BMI, FM and lean mass [40]. Interestingly, a subgroup analysis demonstrated that duration of the vitamin D fortified diet for up to 6 months was associated with non-significant reduction in body weight, but the same intervention for more than 6 months was associated with a significant increase in body weight. Also, no beneficial effect on anthropometric indices was detected from the addition of calcium to vitamin D supplementation
Finally, the most recent meta-analysis of 20 RCTs and 3153 participants investigated the effect of vitamin D supplementation on measures of adiposity (BMI, WC, WHR) in healthy adults [41]. The vitamin D doses ranged from 100 to 8571 IU/day and the duration of the interventions ranged from 1.5 to 36 months. This meta-analysis showed that vitamin D had no significant effect on BMI, WC, or WHR. However, subgroup analysis demonstrated a beneficial effect on BMI only in females, subjects of Asian origin, and duration of intervention ≥ 6 months.
Overall, the majority of available meta-analyses do not support any beneficial effect of vitamin D supplementation on various measures of adiposity such as body weight, BMI, FM, and PFM. However, two meta-analyses reported contradicting results of reduced WC and WHR in the absence of changes in BMI, FM, and lean mass. This finding warrants further investigation. Since WC and WHR are better indices of body fat distribution than BMI or FM, any potentially favorable effect of vitamin D supplementation would have important implications in metabolic health of subjects with obesity.
Controversies in the Association Between Vitamin D and Obesity
The critical appraisal of the abovementioned meta-analyses raises a number of important issues that warrant consideration, as they constitute a source of potential bias and confounding. Notable limitations comprise the heterogeneity of the included studies in terms of participant characteristics, the diverse methods of vitamin D determination and the analytical challenges, the variable definitions of hypovitaminosis D used, the lack of adjustment for various confounding factors influencing vitamin D levels, and the reliability of the various adiposity measures used to characterize obesity (Fig. 1).
Graphic presentation of the various parameters, confounding factors, and potential pathophysiologic mechanisms of the association between obesity and vitamin D. PTH, parathyroid hormone; VDR, vitamin D receptor. Image of woman with obesity is derived from the free medical site http://smart.servier.com/ by Servier licensed under a Creative Commons Attribution 3.0 Unported License
Methodological Considerations
The majority (11 of 15) of the meta-analyses presented herein reported that the high heterogeneity or the small number of the included studies may have impacted their findings (Table 1). Specifically, the dissimilarity in study design and methodology is a critical factor when diverse studies are considered together in meta-analyses, for example when pulling together observational studies and RCTs. The inclusion of mixed population may have influenced the results in multiple ways, as there is considerable variation of FM and body fat distribution between different genders and age groups. Also, according to data from the NHANES surveys on the US population, 25(OH)D is decreasing with age, while women present lower levels compared to men [44]. It has been shown that the inverse association of vitamin D and body adiposity is weaker in younger and stronger in older adults [19], and weaker in subjects with normal body weight, being gradually stronger in individuals with increasing BMI [27]. Therefore, studying populations with a wide range of BMI and age may modify any observed associations. Additionally, the definition of vitamin D insufficiency/deficiency used is another methodological difference between studies. Definitions for vitamin D sufficiency, insufficiency and deficiency were previously established after a consensus reached in 2011 [9]. However, in the following years, there has been some debate about the thresholds to define low vitamin D status, leading to significant heterogeneity between studies [8].
Some controversy also exists regarding the analytical challenges and the best laboratory methodology for determining 25(OH)D levels. Total serum 25(OH)D concentration, which is the sum of D3 and D2 forms, is considered the best single biomarker of vitamin D status [45]. When vitamin D synthesis and/or ingestion is below 2000 IU per day, there is nearly complete conversion of vitamin D to 25(OH)D [46]. Moreover, 25(OH)D has a long half-life (~3 weeks) in the blood circulation. The circulating 25(OH)D concentration also reflects the availability of substrate for local tissue synthesis and autocrine/paracrine action of 1,25(OH)2D. In contrast to 25(OH)D, 1,25(OH)2D is tightly regulated by multiple physiologic pathways and its concentrations may not diminish until late into vitamin D deficiency. Furthermore, 1,25(OH)2D has a short half-life of approximately 4 h [9], while its concentrations are modulated by hormones, such as estradiol, testosterone, prolactin, and prostaglandins, as well as several medications, such as corticosteroids, ketoconazole, bisphosphonates, heparin, and thiazide diuretics [47]. Interestingly, circulating 25(OH)D determination presents a number of analytical challenges, for example its highly lipophilic nature and strong binding affinity for vitamin D binding protein (DBP). Noteworthy, 25(OH)D assays should specifically target the molecule of 25(OH)D in the presence of a plethora of structurally related precursor and degradation products as well as products of alternative vitamin D metabolic pathways, such as C3-epimers. Assays must also detect 25(OH)D3 and 25(OH)D2 separately or, in the case of determination of total 25(OH)D assays, should recover them equally [48].
The laboratory methods used to determine serum 25(OH)D comprise competitive protein-binding assays (CPBA), immunoassays (radioimmunoassay/RIA,enzyme-linked immunosorbent assay/ELISA, chemiluminescence immunoassay/CLIA) as well as chromatographic assays, which include high-performance liquid chromatography (HPLC) and liquid chromatography-tandem mass spectrometry (LC-MS/MS). RIA has been the most frequently reported method in the literature, used also in some of the large-scale population studies studying vitamin D, such as the NHANES and the Women’s Health Initiative (WHI) in the U.S. The accuracy of determination varies widely between different laboratory methods and between individual laboratories [48]. CPBA, CLIA, and RIA assays may overestimate 25(OH)D levels [48, 49]. Although the gold standard method is LC-MS/MS because of its high sensitivity and specificity, the elevated equipment costs have limited its widespread clinical use [50]. Immunoassays present the advantage of automation with substantially higher throughput and lower cost than LC-MS/MS methods [50, 51]. Interestingly, many studies have reported poor agreement between different automated platforms and RIA, HPLC, and LC-MS/MS [52]. Even mass spectrometric methodology may not produce comparable results [52]. In order to overcome these limitations, great efforts have been concentrated on promoting standardization of laboratory assays, which is pivotal to achieve comparable results across different methodologies and manufacturers.
Differences in baseline total 25(OH)D between genders comprise another potential confounder [53]. Sexual dimorphism in adipose and muscle tissue as well as differences in adiposity between pre- and postmenopausal women may account for differences regarding vitamin D that should be considered [54, 55]. Moreover, differences in BMI could account for inter-individual variation in vitamin D supplementation response, which should be considered in interventional studies [56]. Obesity has been shown to reduce the effect of vitamin D supplementation on vitamin D levels in adults [57, 58]. Race may also influence vitamin D levels through the attenuated sunlight effect on vitamin D synthesis in subjects with darker skin [53]. Likewise, the location of the study is an important confounding factor as differences in latitude affect the extent of sunlight exposure [59]. Of note, only 2 meta-analyses examined the effect of latitude and reported that the inverse association of vitamin D with obesity was independent of differences in latitude [27, 28].
Vitamin D levels present a known seasonal variation with higher levels in the summer and autumn and lower levels in the winter and early spring [59, 60]. Thus, the timing of vitamin D determination is an important confounding factor, not accounted for in many studies. In the case of a meta-analysis, it is very difficult to select homogenous studies regarding the season of vitamin D measurement, especially with longitudinal studies that last several months.
Many other characteristics of the studied population may influence the results of relevant studies, such as cultural and religious factors related to dietary habits, dressing codes that dictate covering most of the body surface, and behavioral (obesity may limit outdoor activities) as well as lifestyle (diet and exercise) differences [61]. Also, differences in socioeconomic and developmental status may be a source of heterogeneity between studies affecting both nutrition and lifestyle. The prevalence of obesity and vitamin D status differs substantially according to social, economic and developmental status [62, 63]. Such differences have led in contradicting results regarding the association of vitamin D status and obesity in one meta-analysis [23], but did not affect the association in another [26••].
An important environmental parameter that may influence vitamin D status is atmospheric pollution, which is more prevalent in urban areas and may block type B ultraviolet (UVB) wavelength of sunlight [64]. Additionally, vitamin D intake may substantially differ between countries owing to variations in health policies regarding vitamin D fortification of foods such as milk, juices, cereals and fat spreads in European countries and the US, and in national recommendations regarding vitamin D supplement use [65].
Besides environmental factors, genetic factors also influence vitamin D levels, but the degree of this effect is difficult to quantify without population-based genetic analyses. Thirty five genes and a number of functional variants and SNPs associated with vitamin D levels have been recognized [66]. The genetic determinants of vitamin D status and the response to supplementation may confound the findings of clinical studies with unpredictable results.
The effect of bariatric surgery on vitamin D status is extremely difficult to be evaluated, due to the great variability in vitamin D supplementation strategy after surgery. Nutritional deficiency is a well-known long-term complication of bariatric surgery and varies according to the type of procedure [43]. Restrictive procedures (gastric bypass, sleeve gastrectomy, gastroplasty, gastric banding) limit food intake due to early satiety. Malabsorptive procedures (jejunoileal bypass) hinder the absorption of macronutrients by altering the flow of food and its contact with bile acids and pancreatic enzymes. However, the most widely used procedure nowadays is Roux-en-Y-gastric bypass, with both restrictive and malabsorptive effects [42]. Besides macronutrients, there is substantial micronutrient malabsorption after bariatric surgery, including B vitamins, fat-soluble vitamins (A, D and K) and minerals (calcium, iron, zinc and copper) [43, 67]. Therefore, supplementation with vitamin D and calcium is always recommended after surgery according to consensus guidelines [68]. Studies on vitamin D after bariatric surgery mainly focus on evaluating supplementation strategies to prevent vitamin D deficiency and complications related to bone metabolism. However, vitamin D supplementation dosing, other weigh loss interventions and the effect of weight loss on vitamin D were not taken into consideration.
Evidence from meta-analyses suggests that changes in calcium and PTH are associated with bone loss after surgery, despite preservation of vitamin D levels [32, 35]. 25(OH)D is inversely associated with PTH. It has been suggested that the 25(OH)D threshold for maximum suppression of PTH may be a better index of the optimal vitamin D status [69]. A recent study showed that the 25(OH)D threshold for PTH suppression was lower in patients with BMI ≥ 30kg/m2 1 year after surgery, compared to those with BMI < 30kg/m2 (5 vs 10 ng/mL), suggesting that very low 25(OH)D levels are required to activate PTH axis and result in secondary hyperparathyroidism and bone loss [70]. However, this study also demonstrated that, when obesity is maintained after surgery, PTH and 25(OH)D do not correlate significantly. Therefore, the evaluation of vitamin D status indirectly through PTH assessment has important limitations.
Regarding interventional studies examining the effect of vitamin D supplementation on body weight, a remarkable variability of doses and types of vitamin D (D2 and D3) with or without supplemental calcium were used for various periods of time, contributing to the high heterogeneity between studies. The absolute vitamin D status achieved or its change from baseline values might be a more appropriate outcome measure in these studies [36]. Also, subgroup analysis based on the duration of vitamin D supplementation might lead to safer conclusions [41]. However, there is great difficulty in conducting robust subgroup analyses in homogenous populations (in terms of age, gender, race, latitude, BMI, dosing of vitamin D and duration) due to the small number of studies.
Most meta-analyses examining vitamin D status and obesity included studies that used the WHO classification for obesity based on the BMI. Indeed, the BMI is the most widely accepted measure to define obesity, but it does not accurately reflect fat mass and body fat distribution. It has been shown that for the same BMI value, excess visceral fat confers a higher risk for metabolic and cardiovascular disease compared to subcutaneous fat [71,72,73,74]. To address this methodological issue, other more meaningful measures of adiposity, which better reflect body composition and fat distribution, have also been used, including fat mass, PFM, WC, and WHR. However, only half of the meta-analyses presented in Table 1 reported on these adiposity measures. The inconsistency in adiposity outcomes between studies possibly accounts for the contradicting associations reported in some meta-analyses regarding the effects of vitamin D supplementation on obesity [39, 40]. Of note, evidence has suggested that vitamin D supplementation is associated with a reduction in visceral fat and omental adipocyte size [75, 76]. There are many methods for the objective assessment of total and regional fat mass such as densitometry, bioelectrical impedance analysis (BIA), and dual-energy X-ray absorptiometry (DEXA). In contrast to classical densitometric methods and BIA, DEXA can also provide measures of body fat distribution throughout the body with high precision and accuracy, in addition to direct measurements of fat mass and lean mass [77]. Therefore, using DEXA for determining adiposity outcomes could provide more reliable data regarding the role of vitamin D in obesity.
A Causal Relationship or Reverse Causality?
Since the inverse association between vitamin D and obesity has been established in the literature, there is growing interest and intense scientific debate regarding whether this reflects a causal relationship (obesity causes low vitamin D) or instead a reverse causation (low vitamin D causes obesity). Observational studies per se cannot provide any causal inferences. However, one large meta-analysis explored the direction and causality of this link by using genetic markers in a bi-directional Mendelian randomization (MR) analysis [24••]. Data were drawn from a large Caucasian population comprising over 42,000 participants from 21 adult cohorts from 6 European and North American countries. Genetic variants associated with BMI (12 SNPs) and vitamin D levels (2 SNPs) were used as genetic markers. The meta-analysis has shown that BMI-related genetic variants were associated with both BMI and vitamin D levels, while vitamin D-related genetic variants were only associated with vitamin D status but not BMI. This finding was confirmed in a large population of more than 120,000 subjects participating in 46 studies as part of the GIANT consortium [78]. Furthermore, a recent large-scale MR study in 401,460 white British individuals from the UK Biobank and 42,274 individuals of European ancestry explored the possible causal association of 138 conditionally independent SNPs in 69 vitamin D-associated loci with a large number of human complex traits and diseases and failed to reveal any causal role of 25(OH)D in obesity-related traits [79••]. Overall, these results support the hypothesis that obesity may lead to low vitamin D levels, while any reverse effect is probably small.
A previous study examining potential interactions between polymorphisms in the VDR gene and vitamin D status on BMI, WC, and WHR found no evidence for VDR polymorphisms being major modifiers of the association between 25(OH)D concentrations and adiposity outcomes [80]. A recent meta-analysis also found no association between VDR polymorphisms and risk for obesity [81•]. However, a subgroup analysis stratified by ethnicity has highlighted that specific VDR alleles may have a potentially protective effect against obesity, while others may present risk factors for obesity in Asian, but not European subjects. This latter study gives ground to the hypothesis that variation in vitamin D status and VDR due to genetic polymorphisms might contribute to the development of obesity, at least in some populations. Nevertheless, most of the studies on vitamin D-related genes and their relation to obesity do not support this hypothesis, suggesting that their role in obesity is small, if any.
Due to the immunometabolic properties of vitamin D and the close association of hypovitaminosis D with obesity, it has been suggested that vitamin D may be the missing link between obesity and chronic inflammation as well as metabolic disorders. However, a recent large MR study in 337,199 white British individuals from the UK Biobank did not find evidence that circulating 25(OH)D mediated the association of BMI with inflammatory biomarkers. In addition, after combining data from an observational study in 3586 individuals of the Northern Finland Birth Cohort 1966, the MR analysis and RCTs, there was no evidence of a beneficial role of vitamin D supplementation in obesity-related inflammation [82]. Another MR study exploring the effect of hypovitaminosis D-related genetic variants on diabetes mellitus in 96,423 white Danes aged 20–100 years, showed that there is an association of these variants with DM2, and that hypovitaminosis D might be a modest mediator between obesity and elevated risk for DM2 [83]. However, more large-scale RCTs are needed to clarify any possible role of vitamin D in obesity-related disorders.
Finally, epigenetic factors should not be overlooked, as they may influence vitamin D metabolism and actions as well as obesity phenotypes. For example, glutathione deficiency was reported to epigenetically alter vitamin D regulatory genes in an experimental study in obese mice [84]. Similarly, epigenetic regulation of numerous genes may contribute to obesity [85]. Therefore, epigenetic factors may confound the results of genetic studies exploring the link between vitamin D and obesity and may account for some of the inconsistency among findings.
Mechanisms Underlying the Association Between Vitamin D and Obesity
A substantial amount of research has focused in unraveling pathophysiologic pathways that could substantiate any causal link between obesity and vitamin D deficiency. Experimental studies have reported a number of potential pathophysiologic mechanisms supporting a bidirectional association between obesity and low vitamin D levels (Fig. 1).
Obesity as a Cause of Low Vitamin D Levels
UVB wavelengths of sunlight contribute to more than 80% of the production of vitamin D in humans. Thus, low concentrations of 25(OH)D observed in individuals with obesity could be explained by lower sunlight exposure due to a sedentary lifestyle, decreased participation in outdoor activities, or more clothe covering compared to normal weight subjects [19]. In line with this, studies have revealed that people with obesity have lower sunlight exposure than people with normal body weight, and that outdoor exercise may protect individuals with excess body weight from hypovitaminosis D [86, 87]. However, other studies have reported that sunlight exposure did not vary with BMI [88, 89]. As measurement of sunlight exposure is technically difficult, most findings were based on self-reported data, bearing inherent limitations. Moreover, outdoor activities do not confer exposure to the desired beneficial sunlight radiation spectrum, as this is highly dependent on the geographic location (latitude and altitude), the season of the year, the time of the day and the quality of air (stratospheric ozone and air pollution). Additionally, dressing codes as well as sunscreen use may further limit exposure of the skin to the beneficial effects of UVB [90]. Finally, aging decreases significantly the ability of the skin to produce pre-vitamin D after sunlight exposure [91].
In a landmark study, Wortsman et al. explored the effect of obesity in the cutaneous production of vitamin D3 after whole-body ultraviolet irradiation of subjects with obesity (BMI≥30kg/m2) compared to age-matched lean subjects [92••]. Subjects with obesity presented a 57% lower increase in vitamin D3 compared to lean subjects, 24 hours after irradiation, despite the fact that the precursor of vitamin D3 (7-dehydrocholesterol) in the skin was not significantly different between groups. Moreover, Osmancevic et al. found that BMI was inversely associated with the increase of serum vitamin D3 after UVB exposure, after adjustment for other factors [93]. These studies revealed that other mechanisms, rather than skin sunlight exposure, are more significant for the low vitamin D levels in obesity.
Another hypothesis is based on the potential of adipose tissue to store and retain vitamin D, preventing uncontrolled synthesis of 25(OH)D in the liver and protecting against potential toxicity [94]. The study by Wortsman et al. demonstrated that although skin biosynthesis of vitamin D did not differ between subjects with normal weight and obesity, serum 25(OH)D concentrations were lower in those with obesity [92••]. Also, this study showed that peak vitamin D2 concentrations were inversely correlated with BMI after oral administration of vitamin D2. Thus, the authors concluded that obesity-associated vitamin D insufficiency was likely due to decreased bioavailability of vitamin D from subcutaneous adipose tissue and dietary sources, because of its deposition in various body fat compartments. Furthermore, determination of vitamin D3 in subcutaneous adipose tissue from subjects with obesity by LC-MS/MS demonstrated that vitamin D3 concentrations in adipose tissue were more than 10fold higher compared to serum [95]. These findings suggest that, vitamin D, as a fat-soluble vitamin, is possibly accumulated and sequestered into adipose tissue and is unable to enter the circulation to produce 25(OH)D in the liver. This can lead to lower plasma levels of 25(OH)D in subjects with excess accumulation of adipose tissue.
Nevertheless, the hypothesis that vitamin D is sequestered into adipose tissue has been questioned by recent studies, which attributed low vitamin D levels in obesity to simple volumetric dilution of vitamin D into a greater tissue volume due to the increased body weight and size. Vitamin D, as a fat soluble molecule, is distributed in fat, muscle, liver, and serum, possibly by simple diffusion. Since all of these compartments present an increased volume in obesity, this results in lower serum vitamin D concentrations compared to lean subjects [96]. In support of this hypothesis, Drincic et al. demonstrated that there is no difference in circulating vitamin D between subjects with normal and increased body weight after adjustment for body size [97]. Furthermore, in a controlled study involving age- and race-matched women with normal weight or severe obesity, it was demonstrated that although serum vitamin D did not differ between groups, total vitamin D stores were significantly higher in severe obesity compared to normal weight [98]. It was also shown that the pattern of distribution of vitamin D in the subcutaneous and omental adipose tissues was similar, reflecting the close relationship between serum and adipose tissue vitamin D in both groups. However, based on the results of the meta-analyses discussed earlier, the effect of weight loss on vitamin D levels is rather small, suggesting that volumetric dilution may not be the only responsible mechanism [30, 31].
Interestingly, new evidence has implicated adipose tissue in vitamin D metabolism, suggesting that the metabolic activity of adipose tissue is responsible for lower vitamin D in subjects with obesity. Specifically, recent clinical and experimental studies have demonstrated that obesity is associated with decreased expression of specific genes that regulate metabolism of vitamin D, by coding synthesis of the enzymes 25-hydroxylase and 1α-hydroxylase [99,100,101]. The activity of these enzymes has been determined in human adipose tissue samples, as well as in the liver and extrahepatic tissues of high-fat diet-fed mice. The reduced synthesis of the enzymes responsible for the production of 25(OH)D in adipose tissue, the liver, and probably also other tissues in subjects with obesity may contribute to the low circulating vitamin D levels.
Finally, another possible mechanism is the negative feedback exerted by1,25(OH)2D on serum 25(OH)D levels. Based on small studies, 1,25(OH)2D was found to be increased in subjects with obesity compared to normal-weight subjects [102]. The negative feedback of this active metabolite on the hepatic synthesis of its precursor was suggested to be the cause of the lower vitamin D levels in obesity. However, this finding was not confirmed in recent studies showing lower 1,25(OH)2D in obesity and a similar inverse association with BMI as for 25(OH)D [103, 104]. Furthermore, a large study in subjects with overweight or obesity demonstrated that serum 25(OH)D was closely associated with—and was also the stronger predictor for—serum 1,25(OH)2D [105]. Thus, current evidence is conflicting regarding this potential mechanism.
Low Vitamin D as a Cause of Obesity
The possible causal role of hypovitaminosis D in the pathogenesis of obesity has been under investigation, based on the fact that adipose tissue comprises a direct target for the actions of vitamin D. This is inferred from the expression of both VDR and 25-hydroxyvitamin D 1α-hydroxylase genes in adipocytes, suggesting that adipocytes may be involved in the local synthesis of biologically active 1,25(OH)2D, which may subsequently bind VDR exerting endocrine, autocrine, or paracrine actions on the adipose tissue [106].
Vitamin D is a multifaceted hormone that regulates gene expression and acts in multiple signaling pathways exerting a plethora of complex effects on adipocytes. Evidence suggests that vitamin D regulates adipose tissue differentiation and growth by multiple mechanisms: (1) inhibition of preadipocyte differentiation by suppressing the expression of adipogenic transcription factor genes; (2) inhibition of fatty acid synthesis by increasing the expression of insulin-induced gene-2; (3) reduction of lipid accumulation in vacuoles by suppressing gene expression of fatty acid synthase; and (4) induction of apoptosis of maturing preadipocytes [107,108,109]. Moreover, there is evidence from experimental studies that VDR overexpression may also inhibit preadipocyte differentiation even without binding of 1,25(OH)2D [107]. Therefore, deficiency of the anti-adipogenic vitamin D has been implicated in the expansion of adipose tissue leading to obesity.
However, recent experimental studies have shown that vitamin D may also promote adipose tissue growth. In vitro studies in animal and human adipose tissue have demonstrated that vitamin D exerts both inhibitory and promoting effects on adipogenesis through transcriptional factors and modulation of gene expression, with significant variation between species [110]. Specifically, in human preadipocytes, vitamin D may upregulate the expression of adipogenic marker genes, promoting adipogenesis [110]. Thus, the current evidence regarding this issue is contradicting and the pathophysiologic role of vitamin D in adipose tissue differentiation and growth is far from clear.
Another possible mechanism implicates the actions of PTH, which is increased in low vitamin D states. PTH enhances the production of the active vitamin D metabolite 1,25(OH)2D, but also enhances lipogenesis through increased calcium influx to adipocytes leading to excess fat and increased body weight [103, 111]. Additionally, vitamin D is a key regulator of calcium metabolism, which is important for intracellular processes affecting adipose tissue as well. It has been shown that increasing dietary calcium modulates adipose tissue growth by inhibiting lipogenesis through suppression of adipocyte fatty acid synthase expression and by stimulating lipolysis [112]. Moreover, calcium has been linked to increased fat oxidation and also to a modest increase in fecal fat excretion through decreased lipid absorption, both contributing to negative energy balance [113, 114]. Therefore, vitamin D deficiency may be implicated to weight gain and excess fat accumulation through its effects on PTH and calcium.
The direct actions of vitamin D in gene expression are responsible for the modulation of various components of the adipocyte secretome, also involving the adipokines- main hormones secreted by the adipose tissue [106, 115]. Among these, leptin regulates energy homeostasis and its role in the pathogenesis of obesity has long been established [116]. Experimental animal studies have demonstrated that 1,25(OH)2D increases leptin production through a VDR-mediated upregulation of leptin’s mRNA expression [117]. On the contrary, in vitro studies in human adipose tissue samples have shown that vitamin D3 inhibits leptin secretion [118]. Similarly, evidence from clinical studies is inconclusive regarding the association between serum 25(OH)D and leptin and the effect of vitamin D supplementation on leptin. While observational studies support an inverse association between vitamin D and leptin, interventional studies provide heterogeneous results reporting either an increase or no significant change on leptin after vitamin D supplementation [119,120,121]. Furthermore, it has been suggested that leptin may be implicated in the increased PTH associated with low vitamin D, as both leptin and PTH present similar patterns of association with vitamin D [122].
Whether vitamin D deficiency is promoting obesity by acting directly through gene regulation or indirectly through modulation of PTH, calcium, and leptin is unclear. More research on the molecular mechanisms of vitamin D metabolism, homeostasis, and action is needed before any conclusions can be drawn regarding the implication and the importance of vitamin D in the pathogenesis of obesity.
Conclusions
Evidence from meta-analyses has consistently shown an association between increased body weight (overweight or obesity) and decreased vitamin D status (insufficiency/deficiency) across all age groups. However, evidence supporting a beneficial effect of weight loss on vitamin D levels is either weak or marginally significant, while evidence is inconsistent regarding the effects of bariatric surgery and vitamin D supplementation. Additionally, all meta-analyses agree on the absence of any effect of vitamin D supplementation on most adiposity measures, particularly body weight and BMI, but a few have pointed out a potential beneficial effect on body fat distribution (WC or WHR). Nevertheless, important methodological limitations and a plethora of confounding factors may create substantial doubt regarding the robustness and clarity of this evidence. To further elucidate this issue, there is a need for carefully designed, adequately powered randomized interventional studies in selected homogenous populations, as well as comparative data on different groups of people. Finally, experimental studies have demonstrated that obesity may negatively influence vitamin D levels, but also that vitamin D deficiency may be responsible for adipose tissue growth and body fat accumulation. The underlying pathophysiologic mechanisms are complex and more research is needed to shed light on the interplay between vitamin D and adipose tissue. As hypovitaminosis D and obesity have evolved into pandemics, definite answers are urgently needed to inform public health policies and clinical nutrition guidelines.
Abbreviations
- BIA:
-
bioelectrical impedance analysis
- BMI:
-
body mass index
- CLIA:
-
chemiluminescence immunoassay
- CPBA:
-
competitive protein-binding assays
- CVD:
-
cardiovascular disease
- DBP:
-
vitamin D binding protein
- DEXA:
-
dual-energy X-ray absorptiometry
- DM2:
-
type 2 diabetes mellitus
- ELISA:
-
enzyme-linked immunosorbent assay
- FM:
-
fat mass
- HPLC:
-
high-performance liquid chromatography
- LC-MS/MS:
-
liquid chromatography tandem mass spectrometry
- MR:
-
Mendelian randomization
- mRNA:
-
messenger RNA
- NHANES:
-
National Health and Nutrition Examination Survey
- OR:
-
odds ratio
- PFM:
-
percentage of fat mass
- PCOS:
-
polycystic ovary syndrome
- PTH:
-
parathyroid hormone
- RCT:
-
randomized controlled trial
- RIA:
-
radioimmunoassay
- RR:
-
relative risk
- SNPs:
-
single nucleotide polymorphisms
- UVB:
-
type B ultraviolet
- VAT:
-
visceral adipose tissue
- VDR:
-
vitamin D receptor
- WC:
-
waist circumference
- WHI:
-
Women’s Health Initiative
- WHR:
-
waist-hip ratio
- 1,25(OH)2D:
-
1,25-dihydroxyvitamin D
- 25(OH)D:
-
25-hydroxyvitamin D
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–98. https://doi.org/10.1038/s41574-019-0176-8.
WHO – Obesity and overweight. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight Accessed 5 Jan 2021.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics. 2020
Via M. The malnutrition of obesity: micronutrient deficiencies that promote diabetes. ISRN Endocrinol. 2012;2012:103472–8. https://doi.org/10.5402/2012/103472.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. https://doi.org/10.1056/NEJMra070553.
Arabi A, El Rassi R, El-Hajj Fuleihan G. Hypovitaminosis D in developing countries-prevalence, risk factors and outcomes. Nat Rev Endocrinol. 2010;6:550–61. https://doi.org/10.1038/nrendo.2010.146.
Rojas-Rivera J, De La Piedra C, Ramos A, Ortiz A, Egido J. The expanding spectrum of biological actions of vitamin D. Nephrol Dial Transplant. 2010;25:2850–65. https://doi.org/10.1093/ndt/gfq313.
Holick MF. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017;18:153–65. https://doi.org/10.1007/s11154-017-9424-1.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. https://doi.org/10.1210/jc.2011-0385.
Giustina A, Adler RA, Binkley N, Bollerslev J, Bouillon R, Dawson-Hughes B, et al. Consensus statement from 2nd International Conference on Controversies in Vitamin D. Rev Endocr Metab Disord. 2020;2:89–116. https://doi.org/10.1007/s11154-019-09532-w.
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. Dietary Reference Intakes for Calcium and Vitamin D. Ross AC, Taylor CL, Yaktine AL, Del Valle HB, editors. Washington (DC): National Academies Press (US); 2011.
Yetley EA. Assessing the vitamin D status of the US population. Am J Clin Nutr. 2008;88:558S–64S. https://doi.org/10.1093/ajcn/88.2.558S.
Cheng S, Massaro JM, Fox CS, Larson MG, Keyes MJ, McCabe EL, et al. Adiposity, cardiometabolic risk, and vitamin D status: the Framingham Heart Study. Diabetes. 2010;59:242–8. https://doi.org/10.2337/db09-1011.
Prietl B, Treiber G, Pieber TR, Amrein K. Vitamin D and immune function. Nutrients. 2013;5:2502–21. https://doi.org/10.3390/nu5072502.
Park JE, Pichiah PBT, Cha YS. Vitamin D and Metabolic Diseases: Growing Roles of Vitamin D. J Obes Metab Syndr. 2018;27:223–32. https://doi.org/10.7570/jomes.2018.27.4.223.
Prasad P, Kochhar A. Interplay of vitamin D and metabolic syndrome: A review. Diabetes Metab Syndr. 2016;10:105–12. https://doi.org/10.1016/j.dsx.2015.02.014.
Wimalawansa SJ. Associations of vitamin D with insulin resistance, obesity, type 2 diabetes, and metabolic syndrome. J Steroid Biochem Mol Biol. 2018;175:177–89. https://doi.org/10.1016/j.jsbmb.2016.09.017.
Cashman KD, Vitamin D. Deficiency: Defining, Prevalence, Causes, and Strategies of Addressing. Calcif Tissue Int. 2020;106:14–29. https://doi.org/10.1007/s00223-019-00559-4.
Pourshahidi LK. Vitamin D and obesity: current perspectives and future directions. Proc Nutr Soc. 2015;74:115–24. https://doi.org/10.1017/S0029665114001578.
Abbas MA. Physiological functions of Vitamin D in adipose tissue. J Steroid Biochem Mol Biol. 2017;165:369–81. https://doi.org/10.1016/j.jsbmb.2016.08.004.
Ruiz-Ojeda FJ, Anguita-Ruiz A, Leis R, Aguilera CM. Genetic Factors and Molecular Mechanisms of Vitamin D and Obesity Relationship. Ann Nutr Metab. 2018;73:89–99. https://doi.org/10.1159/000490669.
Migliaccio S, Di Nisio A, Mele C, Scappaticcio L, Savastano S, Colao A. Obesity Programs of nutrition, Education, Research and Assessment (OPERA) Group. Obesity and hypovitaminosis D: causality or casualty? Int J Obes Suppl. 2019;9:20–31. https://doi.org/10.1038/s41367-019-0010-8.
Saneei P, Salehi-Abargouei A, Esmaillzadeh A. Serum 25-hydroxy vitamin D levels in relation to body mass index: a systematic review and meta-analysis. Obes Rev. 2013;14:393–404. https://doi.org/10.1111/obr.12016.
•• Vimaleswaran KS, Berry DJ, Lu C, Tikkanen E, Pilz S, Hiraki LT, et al. Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. PLoS Med. 2013;10:e1001383. https://doi.org/10.1371/journal.pmed.1001383In this large meta-analysis, the causality and direction of the relationship between vitamin D and BMI was explored, by using genetic markers in a bi-directional Mendelian randomization analysis of a large Caucasian population of over 42,000 participants. The study showed that obesity may lead to low vitamin D levels, while any reverse effect is probably small.
Shanmugalingam T, Crawley D, Bosco C, Melvin J, Rohrmann S, Chowdhury S, et al. Obesity and cancer: the role of vitamin D. BMC Cancer. 2014;14:712. https://doi.org/10.1186/1471-2407-14-712.
•• Pereira-Santos M, Costa PR, Assis AM, Santos CA, Santos DB. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes Rev. 2015;16:341–9. https://doi.org/10.1111/obr.12239This large meta-analysis of 23 studies and more than 65,000 participants demonstrated that the prevalence of vitamin D deficiency is significantly higher in overweight and obesity compared to normal body weight, independently from age, latitude and developmental status of the country.
Rafiq S, Jeppesen PB. Body Mass Index, Vitamin D, and Type 2 Diabetes: A Systematic Review and Meta-Analysis. Nutrients. 2018;10:1182. https://doi.org/10.3390/nu10091182.
Golzarand M, Hollis BW, Mirmiran P, Wagner CL, Shab-Bidar S. Vitamin D supplementation and body fat mass: a systematic review and meta-analysis. Eur J Clin Nutr. 2018;72:1345–57. https://doi.org/10.1038/s41430-018-0132-z.
Bacopoulou F, Kolias E, Efthymiou V, Antonopoulos CN, Charmandari E. Vitamin D predictors in polycystic ovary syndrome: a meta-analysis. Eur J Clin Investig. 2017;47:746–55. https://doi.org/10.1111/eci.12800.
• Mallard SR, Howe AS, Houghton LA. Vitamin D status and weight loss: a systematic review and meta-analysis of randomized and nonrandomized controlled weight-loss trials. Am J Clin Nutr. 2016;104:1151–9. https://doi.org/10.3945/ajcn.116.136879This meta-analysis evaluated the effect of weight loss after caloric restriction and/or exercise on vitamin D levels compared to weight maintenance, under similar supplemental vitamin D intake and showed that weight loss is associated with a small but significant increase in serum 25(OH)D levels.
Pannu PK, Zhao Y, Soares MJ. Reductions in body weight and percent fat mass increase the vitamin D status of obese subjects: a systematic review and metaregression analysis. Nutr Res. 2016;36:201–13. https://doi.org/10.1016/j.nutres.2015.11.013.
Liu C, Wu D, Zhang JF, Xu D, Xu WF, Chen Y, et al. Changes in Bone Metabolism in Morbidly Obese Patients After Bariatric Surgery: A Meta-Analysis. Obes Surg. 2016;26:91–7. https://doi.org/10.1007/s11695-015-1724-5.
• Kalani A, Bami H, Tiboni M, Jaeschke R, Adachi JD, Lau AN. The effect of bariatric surgery on serum 25-OH vitamin D levels: a systematic review and meta-analysis. Obes Sci Pract. 2017;3:319–32. https://doi.org/10.1002/osp4.113This meta-analysis assessed the effect of bariatric surgery on 25(OH)D by comparing adults with obesity undergone bariatric surgery to non-surgical controls and showed no significant difference in 25(OH)D change compared to baseline 12 and 24 months post surgery between cases and controls.
Li Z, Zhou X, Fu W. Vitamin D supplementation for the prevention of vitamin D deficiency after bariatric surgery: a systematic review and meta-analysis. Eur J Clin Nutr. 2018;72:1061–70. https://doi.org/10.1038/s41430-017-0059-9.
Tian Z, Fan XT, Li SZ, Zhai T, Dong J. Changes in Bone Metabolism After Sleeve Gastrectomy Versus Gastric Bypass: a Meta-Analysis. Obes Surg. 2020;30:77–86. https://doi.org/10.1007/s11695-019-04119-5.
Pathak K, Soares MJ, Calton EK, Zhao Y, Hallett J. Vitamin D supplementation and body weight status: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2014;15:528–37. https://doi.org/10.1111/obr.12162.
• Chandler PD, Wang L, Zhang X, Sesso HD, Moorthy MV, Obi O, et al. Effect of vitamin D supplementation alone or with calcium on adiposity measures: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2015;73:577–93. https://doi.org/10.1093/nutrit/nuv012This is a large meta-analysis of more than 42,000 adults that demonstrated that supplementation with vitamin D with or without calcium for more than 12 months, had no effect on adiposity measures (BMI, body weight and fat mass).
Manousopoulou A, Al-Daghri NM, Garbis SD, Chrousos GP. Vitamin D and cardiovascular risk among adults with obesity: a systematic review and meta-analysis. Eur J Clin Investig. 2015;45:1113–26. https://doi.org/10.1111/eci.12510.
Is PS, Vitamin D. Supplementation Useful for Weight Loss Programs? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Medicina (Kaunas). 2019;55:368. https://doi.org/10.3390/medicina55070368.
Emadzadeh M, Rashidmayvan M, Sahebi R, Sadeghi R, Ferns GA, Ghayour-Mobarhan M. The effect of vitamin D fortified products on anthropometric indices: A systematic review and meta-analysis. Complement Ther Clin Pract. 2020;41:101242. https://doi.org/10.1016/j.ctcp.2020.101242.
Duan L, Han L, Liu Q, Zhao Y, Wang L, Wang Y. Effects of Vitamin D Supplementation on General and Central Obesity: Results from 20 Randomized Controlled Trials Involving Apparently Healthy Populations. Ann Nutr Metab. 2020;76:153–64. https://doi.org/10.1159/000507418.
Arterburn DE, Courcoulas AP. Bariatric surgery for obesity and metabolic conditions in adults. BMJ. 2014;349:g3961. https://doi.org/10.1136/bmj.g3961.
Gletsu-Miller N, Wright BN. Mineral malnutrition following bariatric surgery. Adv Nutr. 2013;4:506–17. https://doi.org/10.3945/an.113.004341.
Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988-1994 compared with 2000-2004. Am J Clin Nutr. 2008;88:1519–27. https://doi.org/10.3945/ajcn.2008.26182.
Zerwekh JE. Blood biomarkers of vitamin D status. Am J Clin Nutr. 2008;87:1087S–91S. https://doi.org/10.1093/ajcn/87.4.1087S.
Heaney RP, Armas LA, Shary JR, Bell NH, Binkley N, Hollis BW. 25-Hydroxylation of vitamin D3: relation to circulating vitamin D3 under various input conditions. Am J Clin Nutr. 2008;87:1738–42. https://doi.org/10.1093/ajcn/87.6.1738.
Farrell CJ, Herrmann M. Determination of vitamin D and its metabolites. Best Pract Res Clin Endocrinol Metab. 2013;27:675–88. https://doi.org/10.1016/j.beem.2013.06.001.
Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86:50–60. https://doi.org/10.4065/mcp.2010.0567.
Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19:73–8. https://doi.org/10.1016/j.annepidem.2007.12.001.
Black LJ, Anderson D, Clarke MW, Ponsonby AL, Lucas RM. Ausimmune Investigator Group. Analytical Bias in the Measurement of Serum 25-Hydroxyvitamin D Concentrations Impairs Assessment of Vitamin D Status in Clinical and Research Settings. PLoS One. 2015;10:e0135478. https://doi.org/10.1371/journal.pone.0135478.
Dalamaga M, Muscogiuri G, Paganitsa G, Parvouleskou G, Syriou V, Karagkoynis P, et al. Adherence to the Mediterranean diet is an independent predictor of circulating vitamin D levels in normal weight and non-smoker adults: an observational cross-sectional study. Int J Food Sci Nutr. 2021:1–13. https://doi.org/10.1080/09637486.2021.1878488.
Altieri B, Cavalier E, Bhattoa HP, Pérez-López FR, López-Baena MT, Pérez-Roncero GR, et al. Vitamin D testing: advantages and limits of the current assays. Eur J Clin Nutr. 2020;74:231–47. https://doi.org/10.1038/s41430-019-0553-3.
Luttmann-Gibson H, Mora S, Camargo CA, Cook NR, Demler OV, Ghoshal A, et al. Serum 25-hydroxyvitamin D in the VITamin D and OmegA-3 TriaL (VITAL): Clinical and demographic characteristics associated with baseline and change with randomized vitamin D treatment. Contemp Clin Trials. 2019;87:105854. https://doi.org/10.1016/j.cct.2019.105854.
Ambikairajah A, Walsh E, Tabatabaei-Jafari H, Cherbuin N. Fat mass changes during menopause: a metaanalysis. Am J Obstet Gynecol. 2019;221:393–409.e50. https://doi.org/10.1016/j.ajog.2019.04.023.
Goossens GH, Jocken JWE, Blaak EE. Sexual dimorphism in cardiometabolic health: the role of adipose tissue, muscle and liver. Nat Rev Endocrinol. 2021;17:47–66. https://doi.org/10.1038/s41574-020-00431-8.
Sollid ST, Hutchinson MY, Fuskevåg OM, Joakimsen RM, Jorde R. Large Individual Differences in Serum 25-Hydroxyvitamin D Response to Vitamin D Supplementation: Effects of Genetic Factors, Body Mass Index, and Baseline Concentration. Results from a Randomized Controlled Trial. Horm Metab Res. 2016;48:27–34. https://doi.org/10.1055/s-0034-1398617.
de Oliveira LF, de Azevedo LG, da Mota Santana J, de Sales LPC, Pereira-Santos M. Obesity and overweight decreases the effect of vitamin D supplementation in adults: systematic review and meta-analysis of randomized controlled trials. Rev Endocr Metab Disord. 2020;21:67–76. https://doi.org/10.1007/s11154-019-09527-7.
Bassatne A, Chakhtoura M, Saad R, Fuleihan GE. Vitamin D supplementation in obesity and during weight loss: A review of randomized controlled trials. Metabolism. 2019;92:193–205. https://doi.org/10.1016/j.metabol.2018.12.010.
O'Neill CM, Kazantzidis A, Ryan MJ, Barber N, Sempos CT, Durazo-Arvizu RA, et al. Seasonal Changes in Vitamin D-Effective UVB Availability in Europe and Associations with Population Serum 25-Hydroxyvitamin D. Nutrients. 2016;8:533. https://doi.org/10.3390/nu8090533.
Farrokhyar F, Tabasinejad R, Dao D, Peterson D, Ayeni OR, Hadioonzadeh R, et al. Prevalence of vitamin D inadequacy in athletes: a systematic-review and meta-analysis. Sports Med. 2015;45:365–78. https://doi.org/10.1007/s40279-014-0267-6.
Chouraqui JP, Turck D, Briend A, Darmaun D, Bocquet A, Feillet F, et al. Religious dietary rules and their potential nutritional and health consequences. Int J Epidemiol. 2020;dyaa182. https://doi.org/10.1093/ije/dyaa182
Drewnowski A. Obesity, diets, and social inequalities. Nutr Rev. 2009;67:S36–9. https://doi.org/10.1111/j.1753-4887.2009.00157.x.
Lips P. Worldwide status of vitamin D nutrition. J Steroid Biochem Mol Biol. 2010;121:297–300. https://doi.org/10.1016/j.jsbmb.2010.02.021.
Agarwal KS, Mughal MZ, Upadhyay P, Berry JL, Mawer EB, Puliyel JM. The impact of atmospheric pollution on vitamin D status of infants and toddlers in Delhi, India. Arch Dis Child. 2002;87:111–3. https://doi.org/10.1136/adc.87.2.111.
Prentice A. Vitamin D deficiency: a global perspective. Nutr Rev. 2008;66:S153–64. https://doi.org/10.1111/j.1753-4887.2008.00100.x.
Sepulveda-Villegas M, Elizondo-Montemayor L, Trevino V. Identification and analysis of 35 genes associated with vitamin D deficiency: A systematic review to identify genetic variants. J Steroid Biochem Mol Biol. 2020;196:105516. https://doi.org/10.1016/j.jsbmb.2019.105516.
Chakhtoura MT, Nakhoul NN, Shawwa K, Mantzoros C, El Hajj Fuleihan GA. Hypovitaminosis D in bariatric surgery: A systematic review of observational studies. Metabolism. 2016;65:574–85. https://doi.org/10.1016/j.metabol.2015.12.004.
Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon MM, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21:S1–27. https://doi.org/10.1002/oby.20461.
Lotito A, Teramoto M, Cheung M, Becker K, Sukumar D. Serum Parathyroid Hormone Responses to Vitamin D Supplementation in Overweight/Obese Adults: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrients. 2017;9:241. https://doi.org/10.3390/nu9030241.
Salazar DA, Ferreira MJS, Neves JS, Pedro JMP, Guerreiro VA, E Silva Viana S, et al. Variable Thresholds of Vitamin D Plasma Levels to Suppress PTH: the Effect of Weight and Bariatric Surgery. Obes Surg. 2020;30:1551–9. https://doi.org/10.1007/s11695-019-04351-z.
Kissebah AH, Vydelingum N, Murray R, Evans DJ, Hartz AJ, Kalkhoff RK, et al. Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab. 1982;54(2):254–60. https://doi.org/10.1210/jcem-54-2-254.
Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr. 2005;81(3):555–63. https://doi.org/10.1093/ajcn/81.3.555.
St-Pierre J, Lemieux I, Vohl MC, Perron P, Tremblay G, Després JP, et al. Contribution of abdominal obesity and hypertriglyceridemia to impaired fasting glucose and coronary artery disease. Am J Cardiol. 2002;90(1):15–8. https://doi.org/10.1016/s0002-9149(02)02378-0.
Chait A, den Hartigh LJ. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front Cardiovasc Med. 2020;7:22. https://doi.org/10.3389/fcvm.2020.00022.
Caron-Jobin M, Morisset AS, Tremblay A, Huot C, Légaré D, Tchernof A. Elevated serum 25(OH)D concentrations, vitamin D, and calcium intakes are associated with reduced adipocyte size in women. Obesity (Silver Spring). 2011;19:1335–41. https://doi.org/10.1038/oby.2011.90.
Rosenblum JL, Castro VM, Moore CE, Kaplan LM. Calcium and vitamin D supplementation is associated with decreased abdominal visceral adipose tissue in overweight and obese adults. Am J Clin Nutr. 2012;95:101–8. https://doi.org/10.3945/ajcn.111.019489.
Messina C, Albano D, Gitto S, Tofanelli L, Bazzocchi A, Ulivieri FM, et al. Body composition with dual energy X-ray absorptiometry: from basics to new tools. Quant Imaging Med Surg. 2020;10(8):1687–98. https://doi.org/10.21037/qims.2020.03.02.
Speliotes EK, Willer CJ, Berndt SI, Monda KL, Thorleifsson G, Jackson AU, et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet. 2010;42:937–48. https://doi.org/10.1038/ng.686.
•• Jiang X, Ge T, Chen CY. The causal role of circulating vitamin D concentrations in human complex traits and diseases: a large-scale Mendelian randomization study. Sci Rep. 2021;11(1):184. https://doi.org/10.1038/s41598-020-80655-wThis study is the first to explore the association between a large number of vitamin D associated SNPs with a wide range of human complex traits and diseases and showed limited evidence of the causal effects of vitamin D on obesity.
Vimaleswaran KS, Cavadino A, Berry DJ, Mangino M, Andrews P, Moore JH, et al. Interaction between allelic variations in vitamin D receptor and retinoid X receptor genes on metabolic traits. BMC Genet. 2014;15:37. https://doi.org/10.1186/1471-2156-15-37.
• Chen X, Wang W, Wang Y, Han X, Gao L. Vitamin D Receptor Polymorphisms Associated with Susceptibility to Obesity: A Meta-Analysis. Med Sci Monit. 2019;25:8297–305. https://doi.org/10.12659/MSM.915678This meta-analysis explored the association between VDR polymorphisms and obesity and found no association. However, subgroup analysis highlighted that specific VDR alleles may have a potentially protective effect against obesity, while others may present risk factors for obesity in Asian, but not European subjects.
Palaniswamy S, Gill D, De Silva NM, Lowry E, Jokelainen J, Karhu T, et al. Could vitamin D reduce obesity-associated inflammation? Observational and Mendelian randomization study. Am J Clin Nutr. 2020;111(5):1036–47. https://doi.org/10.1093/ajcn/nqaa056.
Afzal S, Brøndum-Jacobsen P, Bojesen SE, Nordestgaard BG. Vitamin D concentration, obesity, and risk of diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol. 2014;2(4):298–306. https://doi.org/10.1016/S2213-8587(13)70200-6.
Parsanathan R, Jain SK. Glutathione deficiency induces epigenetic alterations of vitamin D metabolism genes in the livers of high-fat diet-fed obese mice. Sci Rep. 2019;9:14784. https://doi.org/10.1038/s41598-019-51377-5.
Lima RPA, Hayashi DN, Lima KQDF, Gomes NIG, Ribeiro MR, et al. The Role of Epigenetics in the Etiology of Obesity: A Review. J Clin Epigenet. 2017;3:41. https://doi.org/10.21767/2472-1158.100075.
Kull M, Kallikorm R, Lember M. Body mass index determines sunbathing habits: implications on vitamin D levels. Intern Med J. 2009;39:256–8. https://doi.org/10.1111/j.1445-5994.2009.01900.x.
Florez H, Martinez R, Chacra W, Strickman-Stein N, Levis S. Outdoor exercise reduces the risk of hypovitaminosis D in the obese. J Steroid Biochem Mol Biol. 2007;103:679–81. https://doi.org/10.1016/j.jsbmb.2006.12.032.
Walsh JS, Evans AL, Bowles S, Naylor KE, Jones KS, Schoenmakers I, et al. Free 25-hydroxyvitamin D is low in obesity, but there are no adverse associations with bone health. Am J Clin Nutr. 2016;103:1465–71. https://doi.org/10.3945/ajcn.115.120139.
Macdonald HM, Mavroeidi A, Aucott LA, Diffey BL, Fraser WD, Ormerod AD, et al. Skin color change in Caucasian postmenopausal women predicts summer-winter change in 25-hydroxyvitamin D: findings from the ANSAViD cohort study. J Clin Endocrinol Metab. 2011;96:1677–86. https://doi.org/10.1210/jc.2010-2032.
Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64:1165–8. https://doi.org/10.1210/jcem-64-6-1165.
MacLaughlin J, Holick MF. Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest. 1985;76:1536–8. https://doi.org/10.1172/JCI112134.
•• Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72:690–3. https://doi.org/10.1093/ajcn/72.3.690This landmark study demonstrated that obesity-associated vitamin D insufficiency was likely due to decreased bioavailability of vitamin D from subcutaneous adipose tissue and dietary sources, because of its deposition in various body fat compartments.
Osmancevic A, Gillstedt M, Landin-Wilhelmsen K, Wennberg Larkö AM, Larkö O, Holick MF, et al. Size of the exposed body surface area, skin erythema and body mass index predict skin production of vitamin D. J Photochem Photobiol B. 2015;149:224–9. https://doi.org/10.1016/j.jphotobiol.2015.06.008.
Savastano S, Barrea L, Savanelli MC, Nappi F, Di Somma C, Orio F, et al. Low vitamin D status and obesity: Role of nutritionist. Rev Endocr Metab Disord. 2017;18:215–25. https://doi.org/10.1007/s11154-017-9410-7.
Blum M, Dolnikowski G, Seyoum E, Harris SS, Booth SL, Peterson J, et al. Vitamin D(3) in fat tissue. Endocrine. 2008;33:90–4. https://doi.org/10.1007/s12020-008-9051-4.
Walsh JS, Bowles S, Evans AL. Vitamin D in obesity. Curr Opin Endocrinol Diabetes Obes. 2017;24:389–94. https://doi.org/10.1097/MED.0000000000000371.
Drincic AT, Armas LA, Van Diest EE, Heaney RP. Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity (Silver Spring). 2012;20:1444–8. https://doi.org/10.1038/oby.2011.404.
Carrelli A, Bucovsky M, Horst R, Cremers S, Zhang C, Bessler M, et al. Vitamin D Storage in Adipose Tissue of Obese and Normal Weight Women. J Bone Miner Res. 2017;32:237–42. https://doi.org/10.1002/jbmr.2979.
Wamberg L, Christiansen T, Paulsen SK, Fisker S, Rask P, Rejnmark L, et al. Expression of vitamin D-metabolizing enzymes in human adipose tissue -- the effect of obesity and diet-induced weight loss. Int J Obes. 2013;37:651–7. https://doi.org/10.1038/ijo.2012.112.
Roizen JD, Long C, Casella A, O'Lear L, Caplan I, Lai M, et al. Obesity Decreases Hepatic 25-Hydroxylase Activity Causing Low Serum 25-Hydroxyvitamin D. J Bone Miner Res. 2019;34:1068–73. https://doi.org/10.1002/jbmr.3686.
Elkhwanky MS, Kummu O, Piltonen TT, Laru J, Morin-Papunen L, Mutikainen M, et al. Obesity Represses CYP2R1, the Vitamin D 25-Hydroxylase, in the Liver and Extrahepatic Tissues. JBMR Plus. 2020;4:e10397. https://doi.org/10.1002/jbm4.10397.
Bell NH, Epstein S, Greene A, Shary J, Oexmann MJ, Shaw S. Evidence for alteration of the vitamin D-endocrine system in obese subjects. J Clin Invest. 1985;76:370–3. https://doi.org/10.1172/JCI111971.
Parikh SJ, Edelman M, Uwaifo GI, Freedman RJ, Semega-Janneh M, Reynolds J, et al. The relationship between obesity and serum 1,25-dihydroxy vitamin D concentrations in healthy adults. J Clin Endocrinol Metab. 2004;89:1196–9. https://doi.org/10.1210/jc.2003-031398.
Konradsen S, Ag H, Lindberg F, Hexeberg S, Jorde R. Serum 1,25-dihydroxy vitamin D is inversely associated with body mass index. Eur J Nutr. 2008;47:87–91. https://doi.org/10.1007/s00394-008-0700-4.
Lagunova Z, Porojnicu AC, Vieth R, Lindberg FA, Hexeberg S, Moan J. Serum 25-hydroxyvitamin D is a predictor of serum 1,25-dihydroxyvitamin D in overweight and obese patients. J Nutr. 2011;141:112–7. https://doi.org/10.3945/jn.109.119495.
Ding C, Gao D, Wilding J, Trayhurn P, Bing C. Vitamin D signalling in adipose tissue. Br J Nutr. 2012;108:1915–23. https://doi.org/10.1017/S0007114512003285.
Kong J, Li YC. Molecular mechanism of 1,25-dihydroxyvitamin D3 inhibition of adipogenesis in 3T3-L1 cells. Am J Physiol Endocrinol Metab. 2006;290:E916–24. https://doi.org/10.1152/ajpendo.00410.2005.
Rayalam S, Della-Fera MA, Ambati S, Yang JY, Park HJ, Baile CA. Enhanced effects of 1,25(OH)(2)D(3) plus genistein on adipogenesis and apoptosis in 3T3-L1 adipocytes. Obesity (Silver Spring). 2008;16:539–46. https://doi.org/10.1038/oby.2007.90.
Earthman CP, Beckman LM, Masodkar K, Sibley SD. The link between obesity and low circulating 25-hydroxyvitamin D concentrations: considerations and implications. Int J Obes. 2012;36:387–96. https://doi.org/10.1038/ijo.2011.119.
Mutt SJ, Hyppönen E, Saarnio J, Järvelin MR, Herzig KH. Vitamin D and adipose tissue - more than storage. Front Physiol. 2014;5:228. https://doi.org/10.3389/fphys.2014.00228.
Querfeld U, Hoffmann MM, Klaus G, Eifinger F, Ackerschott M, Michalk D, et al. Antagonistic effects of vitamin D and parathyroid hormone on lipoprotein lipase in cultured adipocytes. J Am Soc Nephrol. 1999;10:2158–64.
Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. Regulation of adiposity by dietary calcium. FASEB J. 2000;14:1132–8.
Soares MJ, Murhadi LL, Kurpad AV, Chan She Ping-Delfos WL, Piers LS. Mechanistic roles for calcium and vitamin D in the regulation of body weight. Obes Rev. 2012;13:592–605. https://doi.org/10.1111/j.1467-789X.2012.00986.x.
Gonzalez JT, Rumbold PL, Stevenson EJ. Effect of calcium intake on fat oxidation in adults: a meta-analysis of randomized, controlled trials. Obes Rev. 2012;13:848–57. https://doi.org/10.1111/j.1467-789X.2012.01013.x.
Karampela I, Christodoulatos GS, Dalamaga M. The Role of Adipose Tissue and Adipokines in Sepsis: Inflammatory and Metabolic Considerations, and the Obesity Paradox. Curr Obes Rep. 2019;8:434–57. https://doi.org/10.1007/s13679-019-00360-2.
Dalamaga M, Chou SH, Shields K, Papageorgiou P, Polyzos SA, Mantzoros CS. Leptin at the intersection of neuroendocrinology and metabolism: current evidence and therapeutic perspectives. Cell Metab. 2013;18:29–42. https://doi.org/10.1016/j.cmet.2013.05.010.
Kong J, Chen Y, Zhu G, Zhao Q, Li YC. 1,25-Dihydroxyvitamin D3 upregulates leptin expression in mouse adipose tissue. J Endocrinol. 2013;216:265–71. https://doi.org/10.1530/JOE-12-0344.
Menendez C, Lage M, Peino R, Baldelli R, Concheiro P, Diéguez C, et al. Retinoic acid and vitamin D(3) powerfully inhibit in vitro leptin secretion by human adipose tissue. J Endocrinol. 2001;170:425–31. https://doi.org/10.1677/joe.0.1700425.
Hajimohammadi M, Shab-Bidar S, Neyestani TR. Vitamin D and serum leptin: a systematic review and meta-analysis of observational studies and randomized controlled trials. Eur J Clin Nutr. 2017;71:1144–53. https://doi.org/10.1038/ejcn.2016.245.
Mousa A, Naderpoor N, Wilson K, Plebanski M, de Courten MPJ, Scragg R, et al. Vitamin D supplementation increases adipokine concentrations in overweight or obese adults. Eur J Nutr. 2020;59:195–204. https://doi.org/10.1007/s00394-019-01899-5.
Dinca M, Serban MC, Sahebkar A, Mikhailidis DP, Toth PP, Martin SS, et al. Does vitamin D supplementation alter plasma adipokines concentrations? A systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2016;107:360–71. https://doi.org/10.1016/j.phrs.2016.03.035.
Maetani M, Maskarinec G, Franke AA, Cooney RV. Association of leptin, 25-hydroxyvitamin D, and parathyroid hormone in women. Nutr Cancer. 2009;61:225–31. https://doi.org/10.1080/01635580802455149.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Metabolism
Rights and permissions
About this article
Cite this article
Karampela, I., Sakelliou, A., Vallianou, N. et al. Vitamin D and Obesity: Current Evidence and Controversies. Curr Obes Rep 10, 162–180 (2021). https://doi.org/10.1007/s13679-021-00433-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-021-00433-1