Abstract
Introduction
Obesity decreases health-related quality of life, but bariatric surgery improves it. This study evaluates the effect of laparoscopic Roux-en-Y gastric bypass, postoperative complications, and percentage of excess body weight loss on quality of life.
Methods
SF-36v.1 questionnaires were administered preoperative (n = 505), 1 year (n = 237) and 2 years (n = 106) following laparoscopic Roux-en-Y gastric bypass. Analysis was performed using Student’s t-test and multiple logistic regression analysis. Complications were defined as requiring additional intervention or hospitalization. SF-36 responses were normalized to 1998 US norms.
Results
Bariatric patients scored significantly lower on all scales compared to the normal population. Health-related quality of life notably improves after surgery. At 1 year, scores not only improved from baseline, but were higher than those of the non-obese reference population regardless of complications. Compared to patients at 2 years without complications, patients experiencing complications reported decreased scores, but scores remained higher than preoperative scores in five scales. At 1 and 2 years, ≤50% excess body weight loss decreased scores; however, scores were significantly improved from baseline.
Conclusions
Health-related quality of life in bariatric patients is worse than in controls, but it improves 1 and 2 years after laparoscopic Roux-en-Y gastric bypass. Complications or ≤50% excess body weight loss slightly decreases this improvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity is an increasing problem in both developed and developing nations [14]. Morbid obesity (body mass index [BMI] > 40 kg/m2 or BMI > 35 kg/m2 with co-morbidities) results in health, psychosocial, and socioeconomic repercussions on an individual level, but it also adds a staggering economic burden to society as a whole. Obesity has been linked to almost 300,000 deaths yearly and $117 billion dollars in direct and indirect annual healthcare spending in the United States alone [1, 22]. The prevalence of obesity has been steadily increasing as the age-adjusted prevalence of obesity (BMI ≥ 30) in this country is now greater than 30% [9]. The primary goals of treatment are to control concomitant diseases, symptoms, and complaints, and to minimize psychosocial adverse effects by reducing weight. Bariatric surgery is the only treatment modality that results in maintained weight loss and control of medical co-morbidities related to obesity [10].
While many of the studies regarding bariatric surgery outcomes focus on percentage of excess body weight loss (%EWL) and resolution of co-morbidities, another essential measure of treatment efficacy is the effect surgery has on patients’ everyday life and well-being, the health-related quality of life (HRQL). Health-related quality of life is gaining increased attention as its importance in evaluating the effectiveness of treatment modalities is realized [4, 12]. Moreover, HRQL is a particularly relevant construct in weight-loss research because obesity has been shown to exert significant negative consequences on HRQL, which improve with adequate weight loss [7, 11, 23, 18, 19].
Studies suggest HRQL is improved after open Roux-en-Y gastric bypass [3, 6], and more recent data suggest improvement in HRQL is achieved more rapidly and is maintained after laparoscopic Roux-en-Y gastric bypass (LRYGB) [15, 16]. Although these outcomes imply overall enhancement of HRQL after LRYGB, we are unaware of outcomes studies regarding the patients who suffer postoperative complications or experience ≤50% EWL. This study aims to address HRQL in these patient groups.
Materials and methods
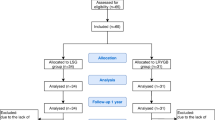
Patients (505: preoperative; 237: 1-year follow-up; 106: 2-year follow-up) who underwent LRYGB by one surgeon (R.H.C.) for morbid obesity between August 2001 and August 2005 were included in this study to assess HRQL measured by the SF-36 Health Survey version 1 [13]. Eight scales are included in this questionnaire: physical function, role—physical, bodily pain, general health, vitality, social function, role—emotional, and mental health. Patients were selected for operation using accepted National Institutes of Health (NIH) criteria.
The SF-36 was administered in person during the preoperative and postoperative clinical visits. During the preoperative clinic visit, participants were instructed that this questionnaire would be administered during this visit and at each annual postoperative visit. The participant was given a paper copy of the SF-36 to complete, and return during the same visit to the research nurse administrator (T.D.L.), who was present and able to respond to questions about the questionnaire if necessary. The participant responses were abstracted from the paper copy into a Microsoft Access database. Transformed scores and norm-based scores were obtained using the QualityMetric SF Health Outcomes Scoring Software (QualityMetric Incorporated, Lincoln, RI). The software standardized the scores using the means and standard deviations obtained from the 1998 U.S. general population. Norm-based scores range from 0 to 100, with a mean of 50 and a standard deviation of 10.
Preoperatively, demographic and obesity-related health information was collected. In the postoperative follow-up period, weight, BMI, %EWL, and complications requiring intervention were recorded at each visit. The two-tailed Student’s t-test was used to compare the mean values of the eight SF-36 scales preoperatively, at 1 year postoperatively, and at 2 years postoperatively. Complications and EWL variables for the two postoperative follow-up surveys were also measured. Multiple linear regression analysis (MLRA) of the full model included demographics, BMI, preoperative co-morbidities, prior abdominal procedures, operative and follow-up variables for the two postoperative surveys to test the impact of complications and EWL on HRQL at each of the eight SF-36 scales at 1 year and at 2 years after LRYGB.
Results
Each patient underwent LRYGB without conversion to an open procedure. The mean operative time was 101.7 min (range, 62–227 min). A total of 505 patients completed preoperative SF-36 questionnaires. Of 423 eligible patients, 237 (56%) completed SF-36 questionnaires at 1 year following surgery, and 106 of 332 (32%) eligible patients completed a questionnaire at 2 years. Demographic data for these groups are reported in Table 1.
Health-related quality of life results for patients preoperatively and at 1 and 2 years after LRYGB are reported in Table 2. Compared to a US normalized mean score of 50 in each scale, preoperative patients scored significantly lower on all scales of the SF-36 HRQL survey. At 1 year after LRYGB, values in each of the eight scales were significantly increased from preoperative scores and normalized controls (Table 2 and 3). Improvement from baseline remained statistically significant in all eight scales of the SF-36 at 2 years, however to a lesser extent than at 1 year. Overall scores for the 2-year population compared to patients at 1 year reported significantly lower scores in each scale except physical function (52.7 [± 7.7] versus 53.3 [± 7.5], respectively, p = 0.51; Table 2). When compared to the US normal population at 2 years after surgery, patients scale scores were significantly higher in the physical function, general health, and vitality scales (Table 3).
The overall rate of postoperative complications requiring intervention in our study group was 17.3% at 1 year and 21.7% at 2 years of follow-up (Table 4). There was one in-hospital death. Patients experiencing complications within the first year following LRYGB reported significant improvement in all 8 scales of the SF-36 over preoperative levels, and mean values were greater than normalized controls (Fig. 1). At 1 year patients with complications scored significantly lower than those without complications in only one of eight scales, vitality (58.1 [± 9.1] versus 54.2 [± 10.2], respectively, p = 0.029; Table 5). However, there was no difference in the MLRA model.
Data at the 2-year follow-up are reported in Figure 2. Patients experiencing complications had statistically significant improvement over preoperative levels in all but three scales: social function, role—emotional, and mental health. Compared to patients at 2 years without complications, patients experiencing complications reported decreased HRQL scores in six of eight scales: role—physical, bodily pain, general health, vitality, social function, and mental health (Table 5). In MLRA, all scales in patients with complications were significantly decreased except for physical function and general health.
Patients who lost ≤50% EWL reported improvement in all 8 scales of the SF-36 over preoperative levels, and mean scores were not statistically different from the scores of those who lost >50% EWL at 1 year (n = 10) or at 2 years (n = 6) after surgery (p > 0.05 for each scale). Furthermore, on MLRA, patients who lost ≤50% EWL did not demonstrate any significantly lower scale score than those who lost more weight at 1 year, except for physical function; at 2 years, none were lower.
Discussion
Patients undergoing LRYGB may expect a significant increase in HRQL, which can be sustained at 2 years, even in the settings of surgery-related complications or ≤50% EWL.
At 1 year following LRYGB, HRQL measurements were not only improved from preoperative levels but also were also quantitatively better than the non-obese reference population, even those with surgical complications. Exceeding the reference values for the HRQL measures is consistent with the “euphoria effect” commonly observed after RYGB-induced weight loss [12]. Choban et al. [3] reported that, at 1 year after obesity surgery, some scale scores exceed those of US norms. An initial increase above US norms after surgery with a subsequent decrease in scores over time was also found by Dixon et al. [5]. We confirm their findings and have also demonstrated a pattern of HRQL that is increased from controls at 1 year while mean scores were slightly lower at 2 years after LRYGB. This phenomena may also have a role in the decision bias that patients may demonstrate in defending their choice to undergo surgery. In addition, patients may report a higher level of quality of life while filling out their questionnaire than they are actually experiencing as a form of reassurance to themselves that they made the right decision.
Patients who developed complications within 2 years after LRYGB reported lower scores in the role—physical section, which categorizes perceived level of accomplishment, limitations in types of activities performed, and level of difficulty of work or other activities. They did not report any difference in the physical function scale, however, which addresses specific tasks such as getting dressed, walking, and climbing stairs. Postoperative complications may lead to a general perception of lower functioning, whereas in actuality these patients perform specific activities of daily living at the same level as patients without complications.
Patients with complications at 2 years also reported a lower mental health score, which is based on questions relating to mood. When asked about the effect their emotions had on activities of daily living, work, and relationships in the role—emotional subscale, however, these patients reported no difference than those who had not experienced complications. Because of the complications, this phenomenon may also be explained by an overall perception of mental and physical function as worse than they actually are. Although complications negatively affected bodily pain, general health, vitality, and social function scores compared to patients without complications, all eight scales were either no different or significantly improved compared to preoperative scores. Results of the present study offer valuable information for preoperative patient education to reassure the morbidly obese individual that HRQL after surgery will likely be improved compared to preoperative levels, even if postoperative complications occur.
The results of loss of body weight lie within the experience of most groups reporting on this type of surgery with median values for %EWL at 72.4 (± 15.1) 1 year after surgery and 78.5 (±16.5) at 2 years after surgery. Complication rates were also consistent with outcomes of other large studies [5, 15, 16, 20]. However, because complication rates were low, the number of patients experiencing an adverse event was low, with only 41 patients at 1 year and 23 at 2 years available for comparison. These low numbers limited power to analyze the extent each complication had on the HRQL score. Demographic data were also similar to those of other large published studies [5, 16, 20]; however, the present study may have limited applicability to populations other than Caucasian.
The definition of successful weight loss after bariatric surgery has been widely accepted as 50% or more EWL. This degree of weight loss consistently provides resolution of co-morbidities [2]. However, in our study, patients with ≤50% EWL at 1 year did not suffer any significant detrimental effect on HRQL compared to those losing >50%, except in the physical function scale, and at 2 years there was no difference in any scale. This demonstrates that our definition of success after bariatric surgery may not be the same as the patient’s definition. These outcomes have to be considered in the setting of low numbers of patients in the ≤50% EWL group. There were 10 patients at 1 year and only 6 patients at 2 years with ≤50% EWL that were eligible for comparison. A larger group of subjects with ≤50% EWL weight loss would help validate these findings.
Long-term follow-up for bariatric patients is essential, and we strongly urge each patient to return for annual assessments. We contact patients by e-mail, telephone, letter, and postcard to encourage return for follow-up. Despite these efforts, we were only able to achieve 56% follow-up at 1 year and 32% follow-up at 2 years for patients included in this study. This may be due in part to the wide geographical area from which we drew our population. In addition, it may be that patients feel well and do not think it necessary to return to the doctor’s office, or perhaps the opposite is true, and patients feel embarrassed if they have not lost enough weight or if they are not complying with dietary and lifestyle recommendations. These factors, and possibly others, raise the specter of bias in our comparisons. These results can be helpful, however, in that they reflect a real-world bariatric practice where compliance with instructions cannot always be enforced.
Consideration of the HRQL outcomes after bariatric procedures has been accepted into clinical practice, and the data that support improvement after surgery are reassuring for both patients and physicians. As in the present review of LRYGB patients, several other reports have demonstrated improved HRQL despite complications following different bariatric procedures such as gastric banding [8, 22] and ileogastrostomy [17]. One study of 18 patients who underwent open Roux-en-Y gastric bypass also reported improved HRQL in patients with postoperative complications [22]. Such studies highlight the severe adverse effect obesity has on HRQL and show that even when bariatric surgery results in significant adverse events, the improvement in HRQL is significant enough to overshadow most complications of the operation. Our data reinforces the idea that despite the risks of complications, LRYGB results in improved quality of patients’ lives in terms of their health.
Conclusions
Health-related quality of life in patients seeking bariatric surgery is significantly lower than the general population; however, after LRYGB, HRQL is dramatically improved and sustained at 2 years. Patients experiencing a complication or ≤50% EWL also report improved HRQL from baseline; however, to a lesser extent.
References
Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB (1999) Annual deaths attributable to obesity in the United States. JAMA 282:1530–1538
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Choban PS, Onyejekwe J, Burge JC, Flancbaum L (1999) A health status assessment of the impact of weight loss following Roux-en-Y gastric bypass for clinically severe obesity. J Am Coll Surg 188:491–497
Committee on Quality of Health Care in America (2001) Crossing the Quality Chasm: A New Health Care System for the 21st Century. National Academy Press, Washington, DC
Dixon JB, Dixon ME, O’Brien PE (2001) Quality of life after lap-band placement: influence of time, weight loss, and comorbidities. Obes Res 9:713–721
Dymek MP, LeGrange D, Neven K, Alverdy J (2002) Quality of life after gastric bypass surgery: a cross-sectional study. Obes Res 10:1135–1142
Fontaine KR, Barofsky I, Anderson RE (1999) Impact of weight loss on health-related quality of life. Qual Life Res 8:275–277
Freys SM, Tigges H, Heimbucher J, Fuchs KH, Fein M, Thiede A (2001) Quality of life following laparoscopic gastric banding in patients with morbid obesity. J Gastrointest Surg 5:401–407
Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM (2004) Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA 291:2847–2850
Karlsson J, Rydén A, Taft C, Sullivan M (2001) Health-related Quality of Life and Obesity. HRQL Newsletter 26:10–11
Kolotkin RL, Crosby RD, Williams GR, Hartley GG, Nicol S (2001) The relationship between health related quality of life and weight loss. Obes Res 9:564–571
Livingston EH (2002) Obesity and its surgical management. Am J Surg 184:103–113
McHorney CA, Ware JE Jr, Raczek AE (1993) The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31:247–263
Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP (1999) The spread of the obesity epidemic in the United States, 1991–1998. JAMA 282:1519–1522
Nguyen NT, Goldman C, Rosenquist J, Arango A, Cole CJ, Lee SJ, Wolfe BM (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 234:279–289
Puzziferri N, Austrheim-Smith IT, Wolfe BM, Wilson SE, Nguyen NT (2006) Three-year follow-up of a prospective randomized trial comparing laparoscopic versus open gastric bypass. Ann Surg 243:181–188
Rippe JM, Price JM, Hess SA, Kline G, DeMers KA, Damitz S, Kreidieh I, Freedson P (1998) Improved psychological well being, quality of life, and health practices in moderately overweight women participating in a 12-week structured weight loss program. Obes Res 6:208–218
Rae AJ, Cleator IGM (1993) Quality of life assessment of ileogastrosotmy. Obes Surg 3:360–364
Samsa GP, Kolotkin RL, Williams GR, Nguyen MH, Mendel CM (2001) Effects of moderate weight loss on health related quality of life: an analysis of combined data from 4 randomized trials of sibutramine vs. placebo. Am J Manag Care 7:875–883
Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J (2000) Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg 232:515–529
Stein CJ, Colditz GA (2004) The epidemic of obesity. J Clin Endocrinol Metab 89:2522–2525
van Gemert WG, Adang EM, Greve JW, Soeters PB (1998) Quality of life assessment of morbidly obese patients: effect of weight-reducing surgery. Am J Clin Nutr 67:197–201
Wadden TA, Sarwer DB, Womble LG, Foster GD, McGuckin BG, Schimmel A (2001) Psychosocial aspects of obesity and obesity surgery. Surg Clin North Am 81:1001–1024
Acknowledgments
Dr. Yarbrough is funded in part by a fellowship grant from Tyco Healthcare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a Poster at the Society of American Gastrointestinal and Endoscopic Surgeons Annual Meeting, April 2006, Dallas, Texas
Rights and permissions
About this article
Cite this article
Rea, J.D., Yarbrough, D.E., Leeth, R.R. et al. Influence of complications and extent of weight loss on quality of life after laparoscopic Roux-en-Y gastric bypass. Surg Endosc 21, 1095–1100 (2007). https://doi.org/10.1007/s00464-007-9257-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9257-1