Abstract
Introduction: Obesity has rapidly become a global health pandemic, resulting in an increasing number of patients undergoing bariatric and metabolic surgery with a substantial impact on patient Quality of Life (QoL). The focus of this chapter will be on QoL after bariatric surgery encompassing both the physical and psychological aspects. The chapter will further examine whether post-operative QoL in bariatric surgery is influenced by the type of bariatric procedure undertaken.
Methods: A thorough search of the literature were performed using PubMed in keeping with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) guidance. All studies that reported QoL post bariatric surgery (with a minimum of 12 months follow up) were included.
Results: A total of eight studies (four of them meta-analyses) were included in this chapter, totalling 12,216 patients. The methodology of the studies included in the reviews were varied, ranging from cohort, case control studies and Randomised Control Studies (RCTs). The tools used in the assessment of QoL was highly varied, however, all the studies unanimously concluded that bariatric surgery has a significant positive impact on a patient’s physical QoL. For psychological well-being, the results were mixed with some studies reporting an improvement in mental health post bariatric surgery, whilst others reported no difference compared to a patient’s pre-operative mental health. There were also differences in QoL depending on what type of bariatric surgery was undertaken. Gastric Sleeve and Gastric Bypass tended to have better QoL scores compared to gastric band.
Discussion: Bariatric surgery (irrespective of the type) significantly improves physical QoL mainly by improving mobility, reducing musculoskeletal pain, and promoting general physical fitness. The results are less clear in mental QoL. Certain bariatric procedures (bypass and sleeve) are associated with better QoL scores compared to other procedures (gastric band).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Over the last three decades, obesity has become a global health pandemic, the worrying trajectory of which is set to worsen. The World Health Organisation (WHO) estimates around 2.8 million deaths annually worldwide as a result of being overweight or obese [1]. More recently this disease which was once thought to be affecting the rich and developed nations has made its presence worldwide. It has been predicted that more than half of the world population will be obese by the year 2030 [2]. In response, ever increasing numbers of patients are undergoing bariatric and metabolic surgery. Bariatric and Metabolic Surgery (BMS) has been shown to be effective in achieving and maintaining weight loss and potentially reversing some of the comorbidities associated with obesity and metabolic syndrome [3]. BMS has been shown in various large studies to be responsible for sustained long term weight loss as well as a decrease in overall mortality as compared to obese population that has not had this intervention [4, 5].
In particular, BMS is more effective than lifestyle interventions in reducing the risk of cardiovascular morbidity such as myocardial infarction and kidney disease in diabetic patients [6,7,8]. There is evidence to suggest a decreased risk of hormone related cancers such as breast, endometrium and prostate following BMS in obese patients [9]. BMS is also considered an effective treatment for Type II Diabetes Mellitus, Hypertension and Obstructive Sleep Apnoea in patients who are overweight [10, 11].
This has also resulted in vast amounts of medical literature exploring the Quality of Life (QoL) amongst patients who have undergone bariatric surgery. The tools used to assess QoL are perhaps as numerous as the range of issues investigated although in recent years, there has been a growing effort to use standardised QoL scoring checklists and questionnaires in the hope of obtaining meaningful comparisons between studies. Certainly, obesity comes with its own QoL impacts whether the patient is pre- or post-surgery.
Quality of Life (QoL)
The WHO defines health as “a state of complete physical, mental and social well-being, and not merely the absence of disease and infirmity”. QoL has been defined as “an overall general well-being that comprises objective descriptors and subjective evaluations of physical, material, social, and emotional well-being together with the extent of personal development and purposeful activity, all weighted by a personal set of values” [12]. From a patient’s perspective it is essentially a sensation of well-being and a judgement of satisfaction with life. Numerous definitions and interpretations of QoL are available in the literature. This has led to the development of various scales that can objectively measure a patient’s perception of their current health. Health Related Quality of Life (HRQoL) examines wellbeing in various domains such as physical, mental and social health [12]. HRQoL has been defined as “those aspects of self-perceived well- being that are related to or affected by the presence of disease or treatment” [13]. In order to be able to meaningfully compare HRQoL between two or more groups of patients various questionnaires have been developed [14, 15]. Such tools aim at assessing a combination of aspects such as physical and social functioning, pain, mental wellbeing and ability for self-care. One must acknowledge however that HRQoL should ideally be assessed from the patient’s point of view. This means that the values can fluctuate over time and that there are differences in how it is perceived and hence reported by people of various ages and cultural backgrounds. The terms QoL, health status and HRQoL have been used interchangeably in literature and various efforts have been made to underpin the subtle differences in these definitions [12].
HRQoL After surgery
It has been proposed that HRQoL should be the metric of choice in a clinical setting as it not only focusses on health, but also on disease [16, 17]. Traditionally the success of a surgical procedure was based on the complications and survival following surgery. With the advances in treatment modalities and surgical techniques the complications have reduced and survival has improved over time. Herein comes the importance of understanding the patients’ perception of success following an operation which is well captured by HRQoL measures [17]. However, there are also critics who are sceptical about the use of such measures at their face value. It is true that there are limitations in being able to accurately gauge QoL due to the subjectivity and perception or interpretation of health and wellbeing between different patient cohorts. Hence one must be very careful while comparing HRQoL outcomes depending on the disease process that has necessitated surgery, for example curative versus palliative surgery for cancer.
HRQoL After Bariatric and Metabolic Surgery
The effectiveness of BMS in reduction or remission of obesity related complications and overall mortality in obese population has been adequately shown [3,4,5]. In addition to the resolution of metabolic syndrome, BMS also aims at providing a significant improvement in overall QoL of the patients. This is expected to continue many years following surgery. Certainly, patients themselves would measure the success of BMS based on their own evaluation of the difference in QoL pre and postoperatively [18, 19]. On both the physical and mental fronts, studies have shown that obese patients who underwent BMS had an improvement in QoL and this was sustained for many years after surgery [20, 21].
However, it remains somewhat unclear as to whether different approaches of surgery result in different levels of satisfaction and QoL. The main aim of this chapter is to summarise the existing literature with regards to differences in QoL (both physical and mental) following bariatric surgery. The secondary objectives will be to compare different surgical operations and endoscopic procedures to determine whether there are differences in QoL depending on the procedure undertaken.
Methods
Search Study and Inclusion Criteria
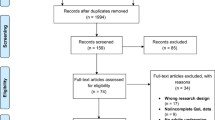
A systemic literature search was performed in Pubmed accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) [22] up to June 2021. As this is a summary of reviews, the search strategy was restricted to Review articles published in the English language only. The surgical intervention as both generic terms such as “Metabolic surgery”, “Bariatric surgery”, “Surgery for obesity”, “Surgery for weight loss” and specific procedures (Roux en y Gastric Bypass, Gastric Band, Sleeve Gastrectomy, Vertical Banded Gastroplasty, Duodenal Switch, Biliopancreatic Diversion or One Anastomosis Gastric Bypass) in combination with QoL related terms (“Health related quality of life”, “Quality of life”, “Patient reported outcomes”). Accepted variations in both the intervention and assessment were included. Manual searches of article references were carried out to ascertain additional potential studies for inclusion. Only systematic reviews and/or meta-analyses involving patients who had undergone bariatric surgery and had undergone QoL assessment were included. Narrative reviews, opinions or studies whose aim was solely to validate the QoL assessment tool were excluded from this study. Lack of baseline quality of life assessment before surgery was not an exclusion criterion.
Data Extraction and Results Reporting
Following the initial search, the abstracts were reviewed for the above criteria. The main text of subsequent studies was reviewed by the three authors independently for inclusion. Disagreement was resolved after discussion between the authors. Data were extracted by three of the authors independently and included data on the surgical intervention, the number of participants, the control intervention where relevant and length of follow up. The primary outcome of interest was the change in quality-of-life scores at specified time points after surgery according to obesity specific and non-specific QOL assessments across different procedures. Only studies with at least 12 months follow up were included in a quantitative analysis. Effect Sizes were reported as stated by the authors of the systematic reviews and/or meta-analyses, be it as an Odds Ratio (OR) or Standard Mean Difference (SMD) accompanied by their associated measure of uncertainty (i.e., 95% Confidence Interval [CI]).
Results
Summary of Studies
The key findings of this study have been sumamrised in Fig. 7.1. Searches using the above terms returned a total of 26 studies, of which eight met the inclusion criteria and all were published between 2012 and 2020. Of these eight, four were meta-analyses [23,24,25,26] (Table 7.1). A total of 12,216 patients were included across all the reviews. The number of articles included in each study ranged from 7 [24] to 36 [27]. The methodology of the studies included in the reviews were varied, ranging from cohort, case control studies and Randomised Control Studies (RCTs). Follow up was equally heterogenous across the different reviews, with average lengths of follow up ranging from 3 months to 25 years.
Quality of Life (QoL) Assessments Tools
A wide variety of different assessment tools were used across the different reviews (Table 7.2), including questionnaires on both physical and mental well-being. In total, across the eight systematic reviews, 26 separate QoL assessment tools were used post bariatric procedures. Some of the assessment tools used such as the Bariatric Analysis and Reporting Outcome System (BAROS), Quality of Life, Obesity and Dietics (QoLOD) and Obesity and Weight-loss Quality of Life (OWQoL) were specific to bariatrics and obesity whilst others such as the SF-36, Hospital Anxiety and Depression Scale (HADS) and European Quality of Life Measurement questionnaire (EQ-5D) are more generalised measures of QoL. Similarly, some of the assessment tools were specific to physical or mental health, whilst others assessed both.
Study Heterogeneity
There was considerable clinical and mathematical heterogeneity amongst the studies in the reviews and meta-analyses largely due the differences in the study populations as well as the varying QoL assessment tools employed. In some of the meta-analyses, mathematical heterogeneity was up to 90%.
Physical QoL Changes
All the included reviews reported on physical QoL changes and unanimously reported a significant improvement in QoL irrespective of the questionnaires used in the studies. The four meta-analyses [23,24,25,26] all demonstrated effect sizes in favour of the surgical group with regards to the biggest difference in improvement of physical QoL (Table 7.3). Driscoll and colleagues reported a 17-fold improvement in physical QoL post bariatric surgery (OR: 17.54, 95% CI 6.60–28.48). Similarly The meta-analysis by Gadd an colleagues focussed on endoscopic therapies, and similar to the bariatric procedures such as LAGB, SG and GB, reported a significant improvement in quality of life [24].
Mental QoL Changes
The evidence for improvement in mental well-being was less clear. Three of the four meta-analyses [23, 25, 26] reviews included in this current review measured mental QoL. One of which, by Driscoll and colleagues, demonstrated a clear improvement in certain aspects of mental QoL post bariatric surgery but not others. The 2016 study used SF-36 scores to demonstrate an improvement in all aspects of mental health including vitality (OR: 15.33, 95% CI: 6.98–23.68, P = 0.0003), social functioning (OR: 14.35, 95% CI: 3.49–25.21, P = 0.010) and emotional well-being (OR: 11.48, 95% CI: 3.04–19.92) and overall mental health [23]. In contrast however, Szmulewicz and colleagues did not find a substantial improvement in mental health QoL in their meta-analyses between the surgical and non-surgical bariatric groups [26]. Similarly, Jumbe and colleagues also found no difference in mental health QoL between surgical and non-surgical groups at up to 10 years follow up.
QoL Post Different Procedures
A systematic review by Hachem and colleagues [28] compared bariatric surgery with other operative strategies. Overall, the review reported a significantly improved physical QoL following bariatric surgery irrespective of the surgical procedure. Interestingly however, it also found that whilst there were no differences in QoL post-surgery based on surgical access i.e. laparoscopic sleeve gastrectomy vs. open sleeve gastrectomy; there were differences in the type of procedure performed, i.e. gastric band vs. gastric sleeve The review included two studies which compared LAGB to SG and found that QoL was significantly higher in the SG group in the first 6 months post-operatively, but by 12 months, there were no differences between the two groups. The same review reported that an RCT which compared GB to VBG, found that whilst both groups reported a higher QoL post-operatively, the GB group had a significantly larger increase in QoL compared with the VBG group [29]. Others have also reported a greater increase in QoL post GB compared to LAGB [30].
Discussion
The main findings of this review of systematic reviews is that post bariatric surgery, patients generally report a significantly positive change in their QoL irrespective of the procedure taken. This change however is more appreciable in physical rather than mental well-being. Interestingly, even after endoscopic bariatric procedures that are traditionally associated with lesser weight loss (such as gastric balloon), the reported QoL post procedure is still largely positive [24].
All eight systematic reviews and meta-analyses unanimously reported an improvement in overall QoL post-surgery. Some of the meta-analyses reported quite substantial and dramatic improvements in physical QoL including increased mobility, reduced musculo-skeletal pain, and general physical fitness. However, this improvement appears to be more pronounced in physical QoL factors compared to mental. The 2015 meta-analysis by Lindekilde and colleagues found an overall improved QoL in both physical and mental domains, however, the mental QoL scores in the surgical group was only marginally better than the non-surgical group. In the meta analyses of RCTs by Szmulewicz and colleagues, no difference was found in mental QoL between the surgical and non-surgical group at all [26]. A systematic review by Hachem and colleagues appears to confirm this lack of (or at best, mildly improved) change in quality of life [28]. This raises the question as to whether weight loss alone is adequate a change in a patient’s life to alter one’s mental well-being and whether we should move beyond such a crude metric as a marker of mental well-being.
Certainly, there is evidence that a substantial proportion of patients continue to suffer from self-esteem and body image issues post bariatric surgery, even in those who have achieved adequate or even excellent weight loss [31]. This appears to be particularly problematic in those with a pre-existing eating disorder diagnosed prior to bariatric surgery [32]. The assumption, therefore, that substantial weight loss post bariatric surgery automatically translates into mental well-being is somewhat naïve and extrapolation or expectation that weight loss will guarantee mental well-being is dangerous. Clinicians need to be mindful that post-operative mental well-being is multi-factorial and not just related to waist size. This may explain why body contouring surgery post bariatric 1surgery has been associated with an improved QoL and mental well-being as demonstrated in a meta-analysis of 13 studies [33].
Some of the key threats that may explain this difference in physical and mental QoL were presented in a systematic review by Mazer and colleagues [34]. The review specifically highlighted social stigma associated with undergoing bariatric surgery was an important contributor to low satisfaction and HRQOL post-surgery. The same review also reported that satisfaction was in part dependent on the type of bariatric surgery patients undergo but surprisingly did not find an association with the degree of weight loss and an improvement in HRQOL. This finding is somewhat in conflict with results from meta-analyses which have reported a link between weight loss and an improvement in HRQOL post bariatric surgery [25]. This was more evident with the physical rather than the mental domains of the QOL assessments.
These findings have been corroborated by Sarwer and colleagues, who reported a relationship between post-surgery weight stigmatisation and depression in bariatric patients [35]. Consistently patients with pre-existing mental health conditions, in particular depression, have described poorer weight loss and separately worse HRQOL post-surgery [36]. The same study reported that certain comorbidities such as cardiovascular disease and dyslipidaemia are associated with poorer HRQOL scores post-operatively, although others such as hypertension, diabetes, gender, and age did not seem to impact HRQOL significantly.
Ironically, one of the most common reported reasons for a poor HRQOL following bariatric surgery may well be due to a side effect of the surgery’s success. Excess skin occurs readily after rapid weight loss and following a successful bariatric procedure whereby a patient may lose anything up to 60–70% of their excess weight, the amount of excess skin may be considerable. This has significant negative body image connotations and recurrent skin related complications. It is therefore not unsurprising that patients who undergo body contour surgery (abdominoplasty etc.) following bariatric surgery are most likely to report an improvement in both physical and mental HRQOL [36]. A summary of the factors which influence HRQOL post bariatric surgery is presented in Fig. 7.2.
Part of the difficulty in assessing QoL post-surgery is the various assessment tools that are utilised, making it difficult to make direct comparisons between studies. Furthermore, different QoL questionnaires have varying sensitivity for different aspects of measuring QoL [37, 38]. To complicate matters further, there is evidence that QoL as reported by patients is not only affected by personality traits, cultural and environmental surroundings [39, 40], but is also temporally sensitive. That is, QoL scores can change in the same person, depending on the events/stage of one’s life at that particular point in time and interpreting these changes over time can be challenging [41].
Currently, there is no consensus as to which QoL reporting tool should be used largely since there is a lack of guidelines for measuring or reporting psychosocial outcomes. In 2015, the American Society of Metabolic and Bariatric Surgery (ASMBS) published a consensus document entitled Standardized Outcomes Reporting in Metabolic and Bariatric Surgery [36]. In this report they classified QoL outcome measures into generic, system/condition specific and obesity specific instruments. They evaluated various tools for validity and reliability and concluded that no single tool is ideal for measuring QoL post bariatric surgery. There is compromise within the scope of the questionnaire, administration logistics (viz. ease of administration or associated costs) and the statistical properties of these measures. This consensus statement concluded that although there was no single recommended measure of QoL, all studies involving post-operative outcomes should ideally use one of the validated tools to report QoL.
Bariatric surgery is associated with not only substantial weight loss and the improvement of many physiological and physical parameters but also overall QoL, particularly physical QoL. It’s effect on mental QoL is less clear as this is a metric that is likely to be affected by a variety of personality types, culture, and environmental factors. There is also some evidence that whilst nearly all bariatric procedures resulting in weight loss are associated with a positive change in QoL scores, there does appear to be differences between the various procedures as to how big a change in QoL they cause. Finally, dizzying array of assessment tools has also made it challenging in making any meaningful comparisons between the different studies.
References
World Health Organization. Obesity. https://www.who.int/news-room/facts-in-pictures/detail/6-facts-on-obesity
Finkelstein EA, Khavjou OA, Thompson H, et al. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42:563–70.
O’Brien PE, Hindle A, Brennan L, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29:3–14.
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34.
Romeo S, Maglio C, Burza MA, et al. Cardiovascular events after bariatric surgery in obese subjects with type 2 diabetes. Diabetes Care. 2012;35:2613–7.
Jonsson S, Hedblad B, Engström G, Nilsson P, Berglund G, Janzon L. Influence of obesity on cardiovascular risk. Twenty-three-year follow-up of 22,025 men from an urban Swedish population. Int J Obes Relat Metab Disord. 2002;26:1046–53.
Wong CKH, Wu T, Wong SKH, et al. Effects of bariatric surgery on kidney diseases, cardiovascular diseases, mortality and severe hypoglycaemia among patients with Type 2 diabetes mellitus. Nephrol Dial Transplant. 2021;36:1440–51.
Mackenzie H, Markar SR, Askari A, et al. Obesity surgery and risk of cancer. Br J Surg. 2018;105:1650–7.
Bhandari V, Kosta S, Bhandari M, Bhandari M, Mathur W, Fobi M. Bariatric metabolic surgery: an effective treatment of type 2 diabetes. J Minim Access Surg. 2021;18(3):396–400. https://doi.org/10.4103/jmas.JMAS_325_20.
Seki Y, Kasama K, Yokoyama R, et al. Bariatric surgery versus medical treatment in mildly obese patients with type 2 diabetes mellitus in Japan: propensity score-matched analysis on real-world data. J Diabetes Investig. 2021;13(1):74–84. https://doi.org/10.1111/jdi.13631.
Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? PharmacoEconomics. 2016;34:645–9.
Ebrahim S. Clinical and public health perspectives and applications of health-related quality of life measurement. Soc Sci Med. 1995;41:1383–94.
Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21:271–92.
Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–43.
Apolone G, De Carli G, Brunetti M, Garattini S. Health-related quality of life (HR-QOL) and regulatory issues. An assessment of the European Agency for the Evaluation of Medicinal Products (EMEA) recommendations on the use of HR-QOL measures in drug approval. PharmacoEconomics. 2001;19:187–95.
Scarpa M. Quality of life after surgery of the alimentary tract. World J Gastroenterol. 2010;16:5020–3.
Major P, Stefura T, Dziurowicz B, et al. Quality of life 10 Years after bariatric surgery. Obes Surg. 2020;30:3675–84.
Urbach DR. Measuring quality of life after surgery. Surg Innov. 2005;12:161–5.
Raaijmakers LCH, Pouwels S, Thomassen SEM, Nienhuijs SW. Quality of life and bariatric surgery: a systematic review of short- and long-term results and comparison with community norms. Eur J Clin Nutr. 2017;71:441–9.
Driscoll S, Gregory DM, Fardy JM, Twells LK. Long-term health-related quality of life in bariatric surgery patients: a systematic review and meta-analysis. Obesity (Silver Spring). 2016;24:60–70.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Driscoll S, Gregory DM, Fardy JM, Twells LK. Long-term health-related quality of life in bariatric surgery patients: a systematic review and meta-analysis. Obesity. 2016;24:60–70.
Gadd N, McIntosh A, Fear-Keen B, Hoult J, Maimone IR, Marshall S. Do endoscopic bariatric procedures improve postprocedural quality of life and mental health? A systematic review and meta-analysis. Obes Surg. 2020;30:4091–100.
Lindekilde N, Gladstone BP, Lübeck M, et al. The impact of bariatric surgery on quality of life: a systematic review and meta-analysis. Obes Rev. 2015;16:639–51.
Szmulewicz A, Wanis KN, Gripper A, et al. Mental health quality of life after bariatric surgery: a systematic review and meta-analysis of randomized clinical trials. Clin Obes. 2019;9:e12290.
Jumbe S, Bartlett C, Jumbe SL, Meyrick J. The effectiveness of bariatric surgery on long term psychosocial quality of life—a systematic review. Obes Res Clin Pract. 2016;10:225–42.
Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg. 2016;26:395–409.
Lee W-J, Huang M-T, Yu P-J, Wang W, Chen T-C. Laparoscopic vertical banded gastroplasty and laparoscopic gastric bypass: a comparison. Obes Surg. 2004;14:626–34.
Campos GM, Rabl C, Roll GR, et al. Better weight loss, resolution of diabetes, and quality of life for laparoscopic gastric bypass vs banding: results of a 2-cohort pair-matched study. Arch Surg. 2011;146:149–55.
Kubik JF, Gill RS, Laffin M, Karmali S. The impact of bariatric surgery on psychological health. J Obes. 2013;2013:837989.
van Hout GCM, Boekestein P, Fortuin FAM, Pelle AJM, van Heck GL. Psychosocial functioning following bariatric surgery. Obes Surg. 2006;16:787–94.
Toma T, Harling L, Athanasiou T, Darzi A, Ashrafian H. Does body contouring after bariatric weight loss enhance quality of life? A systematic review of QOL studies. Obes Surg. 2018;28:3333–41.
Mazer LM, Azagury DE, Morton JM. Quality of life after bariatric surgery. Curr Obes Rep. 2017;6:204–10.
Sarwer DB, Fabricatore AN, Eisenberg MH, Sywulak LA, Wadden TA. Self-reported stigmatization among candidates for bariatric surgery. Obesity (Silver Spring). 2008;16(Suppl 2):S75–9.
Batsis JA, Lopez-Jimenez F, Collazo-Clavell ML, Clark MM, Somers VK, Sarr MG. Quality of life after bariatric surgery: a population-based cohort study. Am J Med. 2009;122(1055):e1–1055.e10.
Ribas SA, Mendes SD, Pires LB, et al. Sensitivity and specificity of assessment instruments of quality of life in rheumatoid arthritis. Rev Bras Reumatol. 2016;56:406–13.
Burckhardt CS, Anderson KL. The Quality of Life Scale (QOLS): reliability, validity, and utilization. Health Qual Life Outcomes. 2003;1:60.
Schmidt S, Bullinger M. Current issues in cross-cultural quality of life instrument development. Arch Phys Med Rehabil. 2003;84:S29–34.
Scott NW, Fayers PM, Aaronson NK, et al. The relationship between overall quality of life and its subdimensions was influenced by culture: analysis of an international database. J Clin Epidemiol. 2008;61:788–95.
Sprangers MAG, Moinpour CM, Moynihan TJ, Patrick DL, Revicki DA, Clinical Significance Consensus Meeting Group. Assessing meaningful change in quality of life over time: a users’ guide for clinicians. Mayo Clin Proc. 2002;77:561–71.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Askari, A., Arhi, C., Mamidanna, R. (2023). Quality of Life Following Bariatric and Metabolic Surgery. In: Athanasiou, T., Patel, V., Darzi, A. (eds) Patient Reported Outcomes and Quality of Life in Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-27597-5_7
Download citation
DOI: https://doi.org/10.1007/978-3-031-27597-5_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-27596-8
Online ISBN: 978-3-031-27597-5
eBook Packages: MedicineMedicine (R0)