Abstract
Purpose of Review
An epidemic of age-associated cognitive decline, most commonly ascribed to neurodegenerative conditions such as Alzheimer’s and Parkinson’s disease, is causing healthcare costs to soar and devastating caregivers. An estimated 6.5 million Americans are living today with Alzheimer’s disease, with 13.8 million cases projected by mid-century. Although genetic mutations are known to cause neurodegeneration, autosomal dominant disease is very rare and most sporadic cases can be attributed, at least in part, to modifiable risk factors.
Recent Findings
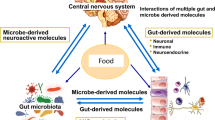
Diet is a potential modifiable risk factor in cognitive decline. Food communicates with the brain through a complex signaling web involving multiple cells, mediators and receptors. Gut-brain communication is modulated by microorganisms including bacteria, archaea, viruses, and unicellular eukaryotes, which together constitute the microbiota. Microbes not only play major roles in the digestion and fermentation of the food, providing nutrients and bioactive metabolites, but also reflect the type and amount of food consumed and food-borne toxic exposures. Food components modify the diversity and abundance of the microbial populations, maintain the integrity of the gut barrier, and regulate the passage of microbes and their metabolites into the blood stream where they modulate the immune system and communicate with body systems including the brain.
Summary
This paper will focus on selected mechanisms through which interactions between diet and the gut microbiota can modify brain integrity and cognitive function with emphasis on the pathogenesis of the most common dementia, Alzheimer’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s Disease Pathophysiology: a Model for Nutrient-Associated Neurodegeneration
Alzheimer’s disease (AD), a serious public health challenge today [1•], was first described by Alois Alzheimer over a century ago [2]. The disease was characterized by an accumulation of toxic protein aggregates in the brain as extracellular amyloid plaques (Aβ) and intracellular neurofibrillary tangles (NFT) [3]. For over 30 years, AD pathogenesis has been attributed to the “amyloid hypothesis” postulating that amyloid peptides, specifically beta amyloid 42 (Aβ42) and related peptides, accumulate in the brain due to an imbalance in amyloid production and clearance and that the degree of amyloid accumulation is the initiating factor in Alzheimer’s disease [4]. The hypothesis holds that amyloid peptides fold into structures that promote self-assembly of like molecules into neurotoxic Aβ plaques and that the accumulation of the Aβ plaques decreases the number of synapses and induces hyperphosphorylation of tau protein, destabilizing microtubules and leading to the formation of intracellular NFT. Aβ adopt ordered polymer structures with the capacity to seed into other regions of the brain in a manner virtually identical to prions [5]. The authors suggest that Aβ formation, propagation, and seeding in the brain must be considered a fundamental characteristic of AD. As the involved neurons become dysfunctional and die, the patient develops stereospecific signs and symptoms including loss of memory and cognitive decline.
The amyloid hypothesis has been supported by the finding that three gene mutations in the amyloid processing cascade are necessary and sufficient to cause toxic Aβ aggregates in autosomal dominant AD [3, 6]. Despite the fact that autosomal dominant AD occurs in less than 1% of cases, Aβ and NFT have been the primary targets of therapy for many years, unfortunately with limited clinical efficacy. Recently, persuasive arguments have been presented that while the presence of Aβ aggregates and NFT in the brain may be predictive of cognitive decline, they are not necessarily initiating factors in AD pathogenesis. Emerging research on the physiologic functions of amyloid suggests that upstream events injure brain cells and/or modify the processing of amyloid proteins, resulting in accumulation of toxic amyloid aggregates and extracellular plaques that can potentiate hyperphosphorylated tau tangles and neuronal death [7••, 8].
Amyloid Sources, Functions, Processing, and Clearance
Amyloid peptides are produced in the brain from a larger amyloid precursor protein (APP). APP participates in the formation and plasticity of synapses within the CNS as well as in neuromuscular synapses [9]. Following production, APP binds copper in a growth factor like domain; copper binding to APP is essential to induce trans-directed dimerization of purified APP. At the cell surface, APP bound to copper potently promotes synaptogenesis [10]. Membrane bound APP is cleaved sequentially by alpha- and gamma secretase enzymes into soluble amyloid fragments that do not aggregate and are cleared via the ubiquitin–proteasome degradation pathway and recycled to amino acids by autophagy-lysosomal pathways. Small amyloid peptides are also transported across the astroglial blood–brain barrier (BBB) into the cerebrospinal fluid for degradation by circulatory and lymphatic systems [11].
Alternatively, APP can be cleaved to Aβ fragments by β-site amyloid precursor protein-cleaving enzyme 1 (BACE1; β-secretase) expressed by neurons, brain endothelial cells, and astrocytes. Normally, BACE1 plays an important role in retinal homeostasis and mitochondrial function. Inhibition of BACE1 reduced mitochondrial membrane potential, augmented mitochondrial fragmentation, and increased cleaved caspase-3 expression resulting in apoptosis of cells under oxidative stress [12]. Other physiological functions of Aβ fragments include antimicrobial activity, tumor suppression, maintenance of blood–brain barrier (BBB) integrity, and synaptic functions [13]. BACE1 is upregulated when astrocytes and microglial cells are activated by inflammatory mediators and bacterial metabolites such as lipopolysaccharide [14].
Aβ fragments are also cleared by autophagy and ubiquitin–proteasome activity [15] and cross the BBB to be cleared by capillary beds in the periphery [16]. The rate of Aβ clearance by ubiquitin-dependent and independent proteasome activity is compromised in AD. Toxic Aβ fragments adopt a 3 dimensional structure that binds the proteasome, blocking its ability to degrade the toxic aggregates [17]. The misfolded proteins remain in the cell to dimerize, aggregate, and accumulate in the cores of neuritic plaques and in the walls of blood vessels resulting in amyloid angiopathy [18].
Gut-Brain Axis Signaling, Barrier Function, and Metabolite Production
The gut-brain axis includes bidirectional neurohormonal communication through the hypothalamic-pituitary axis and the immune system, as well as the enteric nervous system that conveys signals from gastrointestinal neuropod cells and specific receptors in the gut through neural tracts to the brain [19] Non-neuronal signaling from the gut depends in part on the gut barrier that regulates passage of luminal contents through the intestinal epithelial cell (IEC) monolayer into the circulation. Barrier integrity is maintained by interactions among at least four redundant systems. The IEC monolayer is joined by tight junctions between adjacent cells; tight junction (TJ) proteins such as zonulin-1 span the intracellular space and link to cytoskeletal components, strengthening the monolayer. TJ proteins restrict transport across the IEC monolayer to molecules that bind transporter proteins on the apical surface and shuttle selected molecules into the cell by a transcellular route. A second component of the gut barrier is the thick blanket of viscous mucus that overlies the monolayer and separates the IECs from luminal bacteria [20]. The mucus layer is maintained by goblet cells in the IEC monolayer and is stratified into two distinct layers. An inner layer, adherent to the IECs, is largely devoid of bacteria. The outer, porous layer, provides nutrients and binding sites for beneficial (commensal) microbes [21]. Innate immune cells (dendritic cells) project across the IEC monolayer, sample luminal microbial content, and generate tolerance signals that prevent the innate immune system from responding to commensal bacteria or food antigens [22, 23].
Receptors on the IECs constitute a third component of the gut barrier. IECs sense microbial metabolites in the gut lumen using pattern recognition receptors (PRR) that detect microbial ligands and secrete a variety of antimicrobial mediators [24]. Prominent among the PRR is the family of Toll-like receptors (TLR) expressed on the IEC apical surface. TLR recognize microbe-derived ligands such as pro-inflammatory lipopolysaccharide (LPS). In the healthy gut, the inner mucus layer shields IEC bound TLR from luminal microbes, thereby preventing TLR binding and activation. This protection is subverted by microbial pathogens that utilize several alternative strategies to invade the IEC cytoplasm; tactics include bacterial secretion systems, biofilm formation, and pore-forming toxins that insert their ligands into the IEC cytosol. Pathogen invasion upregulates an inflammatory cascade that culminates in the formation of large intracellular multiprotein complexes (inflammasomes) that activate pro-inflammatory interleukins 1β (IL-1β) and 18 (IL-18), stimulate host inflammatory cascades including nuclear factor-kappa beta (NF-κB), and recruit neutrophils and other immune cells to the area. In response to pathogens, host defenses are activated. Antimicrobial peptide secretion by the IEC monolayer is stimulated and mucus secretion enhanced [25, 26]. Innate and adaptive arms of the immune system constitute a fourth line of barrier defense. In response to threat, a robust cellular immune response includes cytotoxic, regulatory, and memory T-cell activation and B-cell differentiation into plasma cells that secrete antibodies to detected antigens [27]. The immune system transmits signals to the brain through T-lymphocytes and cytokine mediators.
Commensal bacteria provide a variety of beneficial products for their host. They produce neurotransmitters such as dopamine, norepinephrine, serotonin, acetylcholine, gamma amino butyric acid (GABA), and histamine [28] that reach the brain through circulatory and neural tracts and modulate brain cell physiology [29]. Saccharolytic bacteria (e.g., Bifidobacteria) ferment dietary fiber and produce short chain fatty acids (SCFA) and other substrates that provide energy and essential nutrients to the diverse microbe populations [30], the IECs, and to the host. Microbial metabolism converts dietary chemicals such as polyphenols into metabolites that can activate the transcription factor, nuclear factor erythroid 2-related factor 2 (Nrf2). Nrf2 binds to the DNA and stimulates expression of multiple cytoprotective enzymes [19]. Dietary sulfur donors (garlic, broccoli) are metabolized to the gasotransmitter, hydrogen sulfide (H2S) that enhances barrier function and reduces inflammation [31•]. Many microbial metabolites can cross the BBB and regulate gene expression in the brain, for example, by inhibiting histone deacetylase [32]. A healthy microbial population can also potentially provide 37% of the daily requirement of folate, together with substantial amounts of B vitamins such as biotin, cobalamin, niacin, pantothenate, pyridoxine, riboflavin, and thiamin [33].
Gut microbes produce amyloid that polymerizes into large, complex biofilms that contribute to mucus attachment and protect microbes against host defenses. In response to infection, commensal gut microbes secrete soluble amyloid A that binds specific retinoids with high affinity in a 4:1 ratio and acts as a systemic transport vehicle. Retinoids taken up by the microglia reduce brain inflammation [34]. Pathogens such as Escherichia coli produce a microbial amyloid (curli) that differs from brain amyloid in primary structure, but is similar in tertiary structure. In vitro and in vivo evidence suggest that this molecular mimicry can elicit cross-seeding in host amyloid, stimulating brain proteins to adopt a pathogenic amyloid β structure [35], and possibly compromise Aβ clearance by inhibiting proteasome activity [17].
Dysbiosis: Cause or Effect of AD?
Gut dysbiosis is commonly observed in AD patients. A cross-sectional study revealed higher odds of AD pathology with lower abundance of microbial SCFA producers in the gut [36]. There are many mechanisms through which a dysbiotic gut could elicit AD pathology. Microbes and their products can translocate through a compromised gut barrier and bind to tissue TLR, stimulating systemic inflammatory mediators that transmit their signals to the brain. Alternatively, TLR on microglia and supporting brain cells can be directly activated by LPS binding through the TLR4/MyD88 pathway with subsequent inflammasome formation and de novo synthesis of effector molecules [37]. LPS bound to TLR elicits inflammation that compromises the BBB [38], allowing entry of noxious metabolites into the brain [39]. While a causal relationship remains to be determined, strong evidence suggests that diet modulation to achieve a healthy gut microbiome may reduce AD risk and/or progression.
Targeted Diet Modification to Reduce Risk for Neurodegeneration
Modify Food Intake to Prevent Dysbiosis
Experimental trials suggest that microbial populations adapt rapidly to diet [40] and that probiotic administration can reduce AD damage in experimental animals [41]. Fermented foods such as yogurt, cheese, and vegetables are major sources of probiotics, defined as living members of microbial species that introduce microbes into the gut [42]. Prebiotics are food components that supply substrate and augment growth of existing gut microbes [43]. Undigested oligosaccharides (fermentable fiber) such as inulin increase the abundance of beneficial Bifidobacteria in the distal human gut [44]. Microbial adaptation studied by introducing human microbiota into a mouse model (gnotobiotic model) [45] and in human subjects [46] occurred within 1 day of undigested carbohydrate reaching the distal gut. These studies also revealed that meat-based diets fostered the growth of bile-tolerant microorganisms (e.g., Bacteroides) and decreased the levels of oligosaccharide-metabolizing organisms.
Dysbiosis has been reported following exposure to environmental pollutants including non-food dietary additives and agents used in food production [47]. Antibiotic drugs, medically prescribed or prophylactically administered to animals, caused microbial dysbiosis in mice and humans [48, 49]. Non-antibiotic drugs have also been implicated in dysbiosis [50]. Industrial additives and antimicrobial baths used to extend shelf life of processed foods are increasingly implicated in gut dysbiosis and/or translocation of gut bacterial metabolites into the blood stream [51•, 52]. Emulsifiers such as polysorbate 80 and carboxymethylcellulose, commonly added during food processing, increased the population of mucolytic bacteria and thinned the protective mucosal gut barrier in mice [53]. Maltodextrin, a polysaccharide chemically derived from starch, increased the adhesiveness of E. coli, stressed goblet cells, and thinned the protective mucus layer, causing bacterial translocation and colonic inflammation in mice [54]. A prospective cohort study that analyzed the 24-h diet recalls of 118,528 non-demented participants at baseline reported that participants who consumed ultra-processed food had greater risk for dementia than those who consumed minimally processed foods [55].
Aggressive food processing methods such as milling, extruding, and extraction modify the chemical structure of whole food and reduce the fiber content. These changes have been implicated in compromised gut barrier function [56]. A fiber-poor diet reduced the saccharolytic bacterial population and promoted the growth of mucus-degrading bacteria in a gnotobiotic mouse model, increasing bacterial translocation across the gut barrier [57]. Non-nutritive sweeteners (NNS) also potentiate dysbiosis. Human microbiota exposed to selected NNS in an in vitro simulation system reduced the fermentative response and microbial diversity [58] and have been implicated in development glucose intolerance [59] and antibiotic resistance in gut microbes [60].
These data suggest that a diet composed of minimally processed, fiber-rich foods will enhance the abundance and diversity of commensal microbes, stimulate mucus protection, and strengthen the IEC barrier to prevent translocation of pathogens and their metabolites into systemic circulation. Since gut dysbiosis and inflammatory mediators can increase blood–brain barrier permeability to neurotoxins, diet modification has potential to prevent inflammatory processes in the brain known to increase risk for AD and cognitive decline [61]. Agricultural antibiotics represent ~ 80% of US antibiotic usage [62]. These drugs have potential to leave residue in animal products and flesh; thus, animal products should be sourced, as much as possible from facilities that practice sustainable agriculture and do not rely on prophylactic antibiotics and high-grain diets to rapidly bring their animals to market weight.
Optimize Consumption of Foods That Induce Neurohormesis
Paracelsus (1493–1541) wrote that “all substances are poison … the right dose differentiates a poison from a remedy.” The concept of hormesis states that chronic sublethal stress can protect against larger, more lethal stresses. A xenohormesis hypothesis has been proposed to describe the ability of animals (heterotrophs) to use chemical cues from other species (fungi, plants) to mount a preemptive defense that improves its survival by upregulating detoxifying mechanisms and adaptive signaling pathways [63]. Neurohormesis describes memory, learning, and performance as well as adaptive detoxifying and signaling systems altered by chemical cues from other species [64•].
Hormetic phytochemicals (HP) act in a biphasic dose–response manner; in low amounts they exert a positive/beneficial effect, while at higher doses, they become progressively more toxic [65]. Low doses of HP counter neurodegeneration due to oxidative stress by upregulating antioxidant enzymes such as superoxide dismutase (SOD), glutathione peroxidase, heme oxygenase, and redox enzymes including NAD(P)H quinone oxidoreductase 1 [66]. Adaptive stress responses such as the cytoprotective Nrf2 transcription factor, hypoxia inducible factor 1 (HIF 1), and peroxisome proliferator-activated receptor (PPAR) activities are upregulated while the pro-inflammatory cascade, NFκβ, is moderated. In addition, HP impact signaling pathways that regulate outgrowth of axons and dendrites, synapse formation and maintenance, and cell survival. Cytoprotective pathways include neurotrophic factors such as brain-derived neurotrophic factor (BDNF), silent information regulator deacetylases (sirtuins; SIRT), and AMP-activated protein kinase (AMPK), a master regulator of cellular energy homeostasis [66].
Low-dose chemicals such as polyphenols, terpenoids, flavonoids, and sulfur-rich compounds in brassica and allium vegetables generate ROS that act as cues to upregulate multiple survival systems. This explains the difficulty in translating in vitro experimental results using antioxidants in the clinical setting [67]. Excess use of antioxidant drugs can minimize the hormetic impact of these cues. Additionally, many HP chemicals (curcumin, catechin, resveratrol) are poorly absorbed intact, but microbial-derived metabolites not only can have dramatically different actions, but many cross the BBB to exert beneficial effects on neuronal systems as reviewed [19]. Thus, in contrast to the large single doses required to detect activity in experimental trials, chronic consumption of small doses of HP chemicals can have a synergistic effect to maximize defense mechanisms [68].
Optimize Mitochondrial Biogenesis and Energy Utilization
The brain utilizes approximately 20% of the mammalian oxygen requirement [69]; glucose is the primary substrate of mitochondrial oxidation. Decreased energy production in the AD brain has been attributed to insulin resistance and impaired insulin signaling resulting in failure to transport glucose across the BBB. However, glucose transport may not be the primary defect in AD, since intracerebral glucose, sorbitol, and fructose levels were 3–fivefold higher in AD patients than in normal subjects [70]. The authors proposed that glucose entering the brain is not effectively oxidized due to mitochondrial dysfunction. Excess intracellular glucose is shunted through the polyol pathway, reduced to sorbitol, and subsequently oxidized to fructose. Fructose is metabolized to uric acid by fructokinase-C (KHK-C), an ATP-requiring enzyme. KHK-C has been located in the brain and is upregulated by dietary and endogenous fructose, high-salt intake, and intermittent glycemia. Central fructose metabolism is implicated in mitochondrial dysfunction, neuroinflammation, impaired glycolysis, reduced ATP, and cerebral insulin resistance [71].
Other causes of mitochondrial dysfunction include downregulation or reduced activity of key mitochondrial enzymes and decreased mitochondrial biogenesis [72]. The gut microbiota provides cofactors and amino acids essential for mitochondrial maintenance [33]. For example, diet and gut-derived thiamin is phosphorylated (TPP) and functions as a cofactor for the mitochondrial enzyme complexes, pyruvate dehydrogenase and alpha-ketoglutarate dehydrogenase, that facilitate glucose oxidation in the mitochondria. TPP deficiency compromises mitochondrial oxidation of glucose, reduces energy production, increases endoplasmic reticulum (ER) stress, and leads to neurodegeneration [73]. Thiamin deficiency is widespread among elderly and diabetic populations but often under-reported [74].
Ketone bodies (acetate, beta-hydroxybutyrate, and acetoacetate) are short-chain organic acids formed in the liver by beta oxidation of fatty acids during periods of fasting or consumption of a high-fat, low-carbohydrate (ketogenic) diet; under these conditions, low insulin secretion permits lipolysis of fat stores as substrate for ketone production. Ketones are also produced directly from dietary medium chain (C6:0–C12:0) fatty acids found in coconut oil and fermented dairy fat [75]. Ketones easily cross the BBB through proton-linked organic acid-based transporters [76], are converted in the mitochondria to acetyl CoA, and provide an alternative substrate for ATP synthesis. Ketone metabolism has also been reported to increase oxidative stress (ROS) and signal survival mechanisms, as described for neurohormesis effects above. Survival mechanisms include activation of the cytoprotective Nrf2 transcription factor, increased sirtuin activation, and increased AMPK. AMPK activation inhibits anabolic activity by inhibiting its regulator, mammalian target of rapamycin (mTOR), a major growth regulator. This action activates autophagy and protects protein reserves. Ketone metabolism decreases the action of the pro-inflammatory NFκβ cascade and subsequent inflammasome activity. Mitochondrial biogenesis, DNA repair, and antioxidant systems including glutathione biosynthesis are also increased [77•] by ketone metabolism.
Minimize Copper Dyshomeostasis and Maximize Sulfur Availability
Copper (Cu) transport is a double-edged sword in AD pathogenesis. The “metal hypothesis” holds that copper metabolism is perturbed in AD and that extracellular copper bound to Aβ stimulates oxidative stress and is causal in neurodegeneration [78]. However, it has also been observed that while neurotoxic amyloid plaques are studded with copper, adjacent brain cells appear severely copper depleted [79], raising the possibility that the pathogenesis of AD may also be linked to inadequate intracellular Cu content [80]. The potential for diet modulations to optimize copper homeostasis is suggested by observations that AD patients have elevated homocysteine levels with reduced vitamins B12 and B6 and folate levels [81, 82]. Impaired transport through the transsulfuration pathway and reduced neuronal glutathione (GSH) are also considered risk factors for AD [83].
Copper accepts and donates single electrons as it transitions between its two redox states, Cu+ and Cu2+. Extracellular oxidized Cu2+ bound to a tripeptide (gly-his-lys) and complexed with glutathione (GSH) is purported to provide reduced copper (Cu+) to the human copper transporter (hCTR1) for entry into the cell [84]. Once in the cell, Cu+ is bound to an array of chaperones, storage and transport proteins to maintain optimal copper for oxidative phosphorylation, antioxidant protection by superoxide dismutase, and other essential activities [85]. Thus, inadequate intracellular Cu+ compromises mitochondrial function and increases oxidative stress.
GSH, consisting of three amino acids, glutamate, glycine, and cysteine, is an essential antioxidant, redox buffer, and neuromodulator. Cysteine is the limiting amino acid for GSH biosynthesis. Astrocytes take up oxidized cystine from the extracellular space via the cystine/glutamate exchanger (Xc−) and export GSH for uptake by other brain cells [86]. Cysteine is produced via the transsulfuration pathway (Fig. 1) that irreversibly converts homocysteine (Hcy) to cysteine via the pyridoxal phosphate-dependent (B6-dependent) enzymes, cystathionine β-synthase (CBS) and cystathionine γ-lyase [87]. Oxidative stress inhibits CBS and increases Hcy accumulation [85].
Methionine and transsulfuration pathways. Vitamins B12, B6, and methyl tetrahydrofolate are required for the homeostasis of homocysteine, methylation capacity, and the conversion of homocysteine to cysteine by the transsulfuration pathway. Cysteine is rate limiting for glutathione biosynthesis, as well as taurine and hydrogen sulfide availability. Together the methionine and transsulfuration pathways maintain optimal sulfur-containing amino acids (methionine, cystine) for protein synthesis and folate cofactors for nucleotide biosynthesis. Reproduced from [92], which is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Hcy can also be methylated to methionine (Met) in a pathway (Fig. 1) requiring vitamin B12 and 5-methyl tetrahydrofolate (MTHF). Met is subsequently bound to adenosyl creating S-adenosylmethionine (SAM) a universal methyl donor. Demethylated SAM is recycled to Hcy, maintaining optimal tissue levels of Hcy and Met. Inadequate availability of folate and B12 in brain cells interrupts Hcy methylation [88] and results in its intracellular Hcy accumulation. Hcy exerts oxidative stress, oxidizes Cu+, and creates tightly bound, neurotoxic Cu-Hcy complexes [89] that exit the cell [90]. Extracellular oxidized copper inhibits hCTR1 activity and inhibits copper uptake, further depleting intracellular Cu+. A yeast model of extracellular Hcy crystal structure has demonstrated its ability to self-assembly into amyloid-like toxic fibrils and seed the aggregation of AD-associated Aβ polypeptides. While this model did not describe copper in the fibrils, the presence of copper bound to Aβ fibrils is well described [91•].
Methionine and transsulfuration pathways depend on B vitamin (B12, B6, and 5-methyl tetrahydrofolate) availability. These nutrients are produced by the gut microbiota [33] and supplied by diet. Vitamin B12 deficiency is more common with aging and mechanistically linked to AD [92]; subclinical deficiency was found in 10 to 15% of individuals older than 60 years and in 25 to 35% of individuals aged over 80 years. Since plants do not produce vitamin B12, it must be obtained by gut microbial action and from animal or fermented products.
Folate deficiency has also been linked to AD pathogenesis. Mechanisms include reduced SAM production with subsequent hypomethylation of the secretase genes, upregulating gene products that increase Aβ accumulation with toxic downstream effects. SAM is also required for synthesis of phosphatidylcholine, a precursor for choline and production of acetylcholine, the neurotransmitter severely diminished in AD [93]. Methyl tetrahydrofolate (MTHF) is produced in green leafy vegetables, but also by microbial action. Stabile, non-reduced folic acid is used therapeutically, but humans have a very low and variable ability to reduce it to the MTHF cofactor [94]. MTHF enters the brain by binding to its receptor on the choroid plexus creating a cerebrospinal fluid (CSF) concentration 3–fourfold that in the serum. CSF folate concentrations were lower in late-onset AD patients [95] despite serum concentrations in the normal range, suggesting a transport defect. Alteration in choroid plexus morphology and function have been identified in AD and linked to dysbiosis and gut permeability to LPS and inflammatory mediators [96].
The transsulfuration pathway requires vitamin B6 as cofactor for the two enzymes that convert homocysteine to cysteine. In addition to its requirement for GSH biosynthesis, cysteine is also substrate for the gasotransmitter, hydrogen sulfide (H2S). H2S has several physiological and pathological actions in the brain. In addition to its function as an endothelial-derived relaxation factor, H2S protects neurons from oxidative stress and glutamate-mediated excitotoxicity. H2S has also been shown to elevate intracellular calcium concentration in neurons and glia, facilitate long-term potentiation, and optimize synaptic remodeling [97•]. H2S and transsulfuration pathways are compromised in AD brains. Recently, chemical H2S donors were shown to prevent hyperphosphorylation of tau by sulfhydrating its kinase (glycogen synthase kinase 3β) and ameliorating motor and cognitive defects in a mouse model [97•]. Dietary sulfur donors including brassica (cabbage) and allium (garlic) vegetables have been shown to act as sulfur donors in vitro and were metabolized to H2S by gut microbes in experimental models. Two pathways have been proposed for the ability of donors generate H2S in cells: they may react with cellular thiols such as GSH, or they may upregulate transsulfuration enzymes that produce H2S [31•]. Whether H2S produced by dietary sulfur donors impact brain function is unclear.
Make NAD Available
Nicotine adenine dinucleotide (NAD) transports high energy electrons from the citric acid cycle to complex 1 of the electron transport chain. It is also essential for a wide variety of activities critical to cell metabolism, gene expression, DNA repair, redox reactions, immune defense, intracellular trafficking, aging, and cell death. In short, NAD is essential for life [98•]. Abundant evidence from animal models and humans has demonstrated that declining NAD availability is a hallmark of senescence [72, 99]. The age-associated fall in NAD has been attributed to its increased utilization by the NAD-dependent enzyme, poly (ADP-ribose)polymerase 1, activated in response to injury and DNA damage. Sirtuin activation in response to hormetic cues also requires NAD [99]. Decreased availability of NAD can compromise sirtuin activity, leading to mitochondrial dysfunction and, since sirtuins are deacetylases, hyperacetylated mitochondrial proteins [72]. Depletion of NAD also causes translocation of the apoptosis inducing factor (AIF) from the mitochondrial membrane to the nucleus, resulting in cell death.
Niacin is found in both animal and plant sources; however, bioavailability may be limited for some plants. For example, the niacin deficiency disease, pellagra, occurred in patients who consumed low-protein and high-maize diets; populations who consumed maize treated with alkali (nixtamalization) did not develop pellagra because the alkali released niacin from the maize. NAD can be synthesized de novo from amino acids including L-tryptophan, or by salvage of precursors including nicotinic acid (NA), nicotinamide mono-nucleotide (NMN), and derivatives such as nicotinamide riboside (NR); NAD precursors are collectively termed, vitamin B3. NAD is also essential for microbial life; however, dietary B3 precursors are absorbed in the proximal gut and do not reach the colonic microbes. To determine the source of NAD precursors for gut microbes, isotopic tracers were used to identify a cycle through which NMN in the host circulation entered the gut lumen and was used by microbes for NA biosynthesis [100••]. Colonic microbes obtained approximately 50% of substrate for NA biosynthesis from fermentable fiber. The NA produced was used by gut microbes and by the host intestinal cells; NA was also absorbed and used by the host for NAD biosynthesis. These data suggest that NAD precursors obtained from the diet are complemented by NA synthesized by a healthy gut microbiome. This unique metabolic cycle between microbe and host ensures that both organisms maintain optimal NAD levels. Since a large fraction of substrate for microbial NA biosynthesis depends on host consumption of fermentable carbohydrate, it is likely that a diet high in ultra-processed foods devoid of dietary fiber may compromise NAD homeostasis.
Conclusion
Age-associated cognitive decline, especially due to Alzheimer’s disease (AD), is reaching epidemic proportions. Despite abundant research into the pathogenesis and treatment of AD, for many patients, cognitive decline is inexorable. This review explores mechanisms through which diet modification can modulate risk factors for AD. Strategies include optimizing gut microbiome health, reducing oxidative stress and inflammation, and supporting mitochondrial abundance and function. A healthy and diverse microbiota not only promotes innate immune protection by strengthening the gut barrier, but it also provides nutrient cofactors and metabolites that stimulate adaptive detoxifying and signaling systems that promote survival of cells, tissues, and host.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Association A. 2022 Alzheimer’s disease facts and figures. Alzheimers Dement. 2022;18(4):700–89. Comprehensive review of the public health impact of Alzheimer’s disease (AD).
Alzheimer A. Über eine eigenartige Erkrankung der Hirnrinde Allgemeine Zeitschrift fur Psychiatrie und Psychisch-gerichtliche Medizin. Psychiatry (Edgmont). 1907;64:146–8.
Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E. Alzheimer’s disease. Lancet. 2011;377(9770):1019–31.
Selkoe DJ, Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med. 2016;8(6):595–608.
Walker LC, Schelle J, Jucker M. The prion-like properties of amyloid-β assemblies: implications for Alzheimer’s disease. Cold Spring Harb Perspect Med. 2016;6(7).
Van Cauwenberghe C, Van Broeckhoven C, Sleegers K. The genetic landscape of Alzheimer disease: clinical implications and perspectives. Genet Med. 2016;18(5):421–30.
•• Frisoni GB, Altomare D, Thal DR, Ribaldi F, van der Kant R, Ossenkoppele R, et al. The probabilistic model of Alzheimer disease: the amyloid hypothesis revised. Nat Rev Neurosci. 2022;23(1):53–66. Current understanding about the pathogenesis and potential treatment strategies for AD.
Clifford JJ, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14(4):535–62.
Klevanski M, Herrmann U, Weyer SW, Fol R, Cartier N, Wolfer DP, et al. The APP intracellular domain is required for normal synaptic morphology, synaptic plasticity, and hippocampus-dependent behavior. J Neurosci. 2015;35(49):16018–33.
Baumkötter F, Schmidt N, Vargas C, Schilling S, Weber R, Wagner K, et al. Amyloid precursor protein dimerization and synaptogenic function depend on copper binding to the growth factor-like domain. J Neurosci. 2014;34(33):11159–72.
Tarasoff-Conway JM, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, et al. Clearance systems in the brain—implications for Alzheimer disease. Nat Rev Neurol. 2015;11(8):457–70.
Francelin C, Mitter SK, Qian Q, Barodia SK, Ip C, Qi X, et al. BACE1 inhibition increases susceptibility to oxidative stress by promoting mitochondrial damage. Antioxidants (Basel). 2021;10(10).
Brothers HM, Gosztyla ML, Robinson SR. The physiological roles of amyloid-β peptide hint at new ways to treat Alzheimer’s disease. Front Aging Neurosci. 2018;10.
Chacón-Quintero MV, Pineda-López LG, Villegas-Lanau CA, Posada-Duque R, Cardona-Gómez GP. Beta-secretase 1 underlies reactive astrocytes and endothelial disruption in neurodegeneration. Front Cell Neurosci. 2021;15.
Tecalco–Cruz AC, Pedraza-Chaverri J, Briones-Herrera A, Cruz-Ramos E, López–Canovas L, Zepeda–Cervantes J. Protein degradation-associated mechanisms that are affected in Alzheimer’s disease. Mol Cell Biochem. 2022.
Xiang Y, Bu X-L, Liu Y-H, Zhu C, Shen L-L, Jiao S-S, et al. Physiological amyloid-beta clearance in the periphery and its therapeutic potential for Alzheimer’s disease. Acta Neuropathol. 2015;130(4):487–99.
Thibaudeau TA, Anderson RT, Smith DM. A common mechanism of proteasome impairment by neurodegenerative disease-associated oligomers. Nat Commun. 2018;9(1):1097.
Yan R. Physiological functions of the β-site amyloid precursor protein cleaving enzyme 1 and 2. Front Mol Neurosci. 2017;10.
Nargeh H, Aliabadi F, Ajami M, Pazoki-Toroudi H. Role of polyphenols on gut microbiota and the ubiquitin-proteasome system in neurodegenerative diseases. J Agric Food Chem. 2021;69(22):6119–44.
Chen GY, Stappenbeck TS. Mucus, it is not just a static barrier. Sci Signal. 2014;7(323):pe11-pe.
Johansson MEV, Larsson JMH, Hansson GC. The two mucus layers of colon are organized by the MUC2 mucin, whereas the outer layer is a legislator of host–microbial interactions. Proc Natl Acad Sci. 2011;108(Supplement 1):4659–65.
McDole JR, Wheeler LW, McDonald KG, Wang B, Konjufca V, Knoop KA, et al. Goblet cells deliver luminal antigen to CD103+ dendritic cells in the small intestine. Nature. 2012;483(7389):345–9.
Shan M, Gentile M, Yeiser JR, Walland AC, Bornstein VU, Chen K, et al. Mucus enhances gut homeostasis and oral tolerance by delivering immunoregulatory signals. Science. 2013;342(6157):447–53.
Franchi L, Muñoz-Planillo R, Núñez G. Sensing and reacting to microbes through the inflammasomes. Nat Immunol. 2012;13(4):325–32.
Benjamin Jamaal L, Sumpter R, Levine B, Hooper LV. Intestinal epithelial autophagy is essential for host defense against invasive bacteria. Cell Host Microbe. 2013;13(6):723–34.
Philpott DJ, Sorbara MT, Robertson SJ, Croitoru K, Girardin SE. NOD proteins: regulators of inflammation in health and disease. Nat Rev Immunol. 2014;14(1):9–23.
Mowat AM. Anatomical basis of tolerance and immunity to intestinal antigens. Nat Rev Immunol. 2003;3(4):331–41.
Strandwitz P. Neurotransmitter modulation by the gut microbiota. Brain Res. 2018;1693:128–33.
Rutsch A, Kantsjö JB, Ronchi F. The gut-brain axis: how microbiota and host inflammasome influence brain physiology and pathology. Front Immunol. 2020;11.
Soto-Martin EC, Warnke I, Farquharson FM, Christodoulou M, Horgan G, Derrien M, et al. Vitamin biosynthesis by human gut butyrate-producing bacteria and cross-feeding in synthetic microbial communities. mBio. 2020;11(4).
• Rose P, Moore PK, Whiteman M, Kirk C, Zhu Y-Z. Diet and hydrogen sulfide production in mammals. Antioxidants Redox Signal. 2021;34(17):1378–93. Current understanding of the processes of hydrogen sulfide production and possible value of dietary sulfur donors.
Kasubuchi M, Hasegawa S, Hiramatsu T, Ichimura A, Kimura I. Dietary gut microbial metabolites, short-chain fatty acids, and host metabolic regulation. Nutrients. 2015;7(4):2839–49.
Magnúsdóttir S, Ravcheev D, de Crécy-Lagard V, Thiele I. Systematic genome assessment of B-vitamin biosynthesis suggests co-operation among gut microbes. Front Genetics. 2015;6:148.
Esterházy D, Mucida D. Serum amyloid A proteins take retinol for a ride. Trends Immunol. 2014;35(11):505–6.
Wang C, Lau CY, Ma F, Zheng C. Genome-wide screen identifies curli amyloid fibril as a bacterial component promoting host neurodegeneration. Proc Natl Acad Sci. 2021;118(34): e2106504118.
Verhaar BJH, Hendriksen HMA, de Leeuw FA, Doorduijn AS, van Leeuwenstijn M, Teunissen CE, et al. Gut microbiota composition is related to AD pathology. Front Immunol. 2022;12.
Heneka MT, McManus RM, Latz E. Inflammasome signalling in brain function and neurodegenerative disease. Nat Rev Neurosci. 2018;19(10):610–21.
Shigemoto-Mogami Y, Hoshikawa K, Sato K. Activated microglia disrupt the blood-brain barrier and induce chemokines and cytokines in a rat in vitro model. Front Cell Neurosci. 2018;12(494).
Serlin Y, Shelef I, Knyazer B, Friedman A. Anatomy and physiology of the blood–brain barrier. Semin Cell Dev Biol. 2015;38:2–6.
Sandhu KV, Sherwin E, Schellekens H, Stanton C, Dinan TG, Cryan JF. Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry. Transl Res. 2017;179:223–44.
Bonfili L, Cecarini V, Berardi S, Scarpona S, Suchodolski JS, Nasuti C, et al. Microbiota modulation counteracts Alzheimer’s disease progression influencing neuronal proteolysis and gut hormones plasma levels. Sci Rep. 2017;7(1):2426.
Gibson GR, Roberfroid MB. Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J Nutr. 1995;125(6):1401–12.
Walker AW, Ince J, Duncan SH, Webster LM, Holtrop G, Ze X, et al. Dominant and diet-responsive groups of bacteria within the human colonic microbiota. ISME J. 2011;5(2):220–30.
Gibson GR. Dietary modulation of the human gut microflora using the prebiotics oligofructose and inulin. J Nutr. 1999;129:1438S-S1441.
Turnbaugh PJ, Ridaura VK, Faith JJ, Rey FE, Knight R, Gordon JI. The effect of diet on the human gut microbiome: a metagenomic analysis in humanized gnotobiotic mice. Sci Transl Med. 2009;1(6):6ra14.
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484):559–63.
Jin Y, Wu S, Zeng Z, Fu Z. Effects of environmental pollutants on gut microbiota. Environ Pollut. 2017;222:1–9.
Cho I, Yamanishi S, Cox L, Methé BA, Zavadil J, Li K, et al. Antibiotics in early life alter the murine colonic microbiome and adiposity. Nature. 2012;488(7413):621–6.
Trasande L, Blustein J, Liu M, Corwin E, Cox LM, Blaser MJ. Infant antibiotic exposures and early-life body mass. Int J Obes. 2013;37(1):16–23.
Vich Vila A, Collij V, Sanna S, Sinha T, Imhann F, Bourgonje AR, et al. Impact of commonly used drugs on the composition and metabolic function of the gut microbiota. Nat Commun. 2020;11(1):362.
• Laudisi F, Stolfi C, Monteleone G. Impact of food additives on gut homeostasis. Nutrients. 2019;11(10):2334. Review of the impact of food production agents and additives and their potential to cause gut dysbiosis.
Lerner A, Matthias T. Changes in intestinal tight junction permeability associated with industrial food additives explain the rising incidence of autoimmune disease. Autoimmun Rev. 2015;14(6):479–89.
Chassaing B, Van de Wiele T, De Bodt J, Marzorati M, Gewirtz AT. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut. 2017;66(8):1414–27.
Laudisi F, Di Fusco D, Dinallo V, Stolfi C, Di Grazia A, Marafini I, et al. The food additive maltodextrin promotes endoplasmic reticulum stress-driven mucus depletion and exacerbates intestinal inflammation. Cell Mol Gastroenterol Hepatol. 2019;7(2):457–73.
Li H, Li S, Yang H, Zhang Y, Zhang S, Ma Y, et al. Association of ultra-processed food consumption with risk of dementia: a prospective cohort study. Available at SSRN 3978652. 2021.
Fardet A. Wheat-based foods and non celiac gluten/wheat sensitivity: is drastic processing the main key issue? Med Hypotheses. 2015;85(6):934–9.
Desai Mahesh S, Seekatz Anna M, Koropatkin Nicole M, Kamada N, Hickey Christina A, Wolter M, et al. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell. 2016;167(5):1339-53.e21.
Vamanu E, Pelinescu D, Gatea F, Sârbu I. Altered in vitro metabolomic response of the human microbiota to sweeteners. Genes. 2019;10(7):535.
Suez J, Korem T, Zeevi D, Zilberman-Schapira G, Thaiss CA, Maza O, et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature. 2014;514:181.
Yu Z, Guo J. Non-caloric artificial sweeteners exhibit antimicrobial activity against bacteria and promote bacterial evolution of antibiotic tolerance. J Hazard Mater. 2022;433: 128840.
Roe K. An alternative explanation for Alzheimer’s disease and Parkinson’s disease initiation from specific antibiotics, gut microbiota dysbiosis and neurotoxins. Neurochem Res. 2022;47(3):517–30.
Boeckel TPV, Brower C, Gilbert M, Grenfell BT, Levin SA, Robinson TP, et al. Global trends in antimicrobial use in food animals. Proc Natl Acad Sci. 2015;112(18):5649–54.
Howitz KT, Sinclair DA. Xenohormesis: sensing the chemical cues of other species. Cell. 2008;133(3):387–91.
• Trovato Salinaro A, Pennisi M, Di Paola R, Scuto M, Crupi R, Cambria MT, et al. Neuroinflammation and neurohormesis in the pathogenesis of Alzheimer’s disease and Alzheimer-linked pathologies: modulation by nutritional mushrooms. Immun Ageing. 2018;15:8-. Background on neurohormesis and neuroinflammation and data on the ability of nutritional mushrooms to elicit survival systems in humans.
Murugaiyah V, Mattson MP. Neurohormetic phytochemicals: an evolutionary–bioenergetic perspective. Neurochem Int. 2015;89:271–80.
Lee J, Jo D-G, Park D, Chung HY, Mattson MP. Adaptive cellular stress pathways as therapeutic targets of dietary phytochemicals: focus on the nervous system. Pharmacol Rev. 2014;66(3):815–68.
Ristow M. Unraveling the truth about antioxidants: mitohormesis explains ROS-induced health benefits. Nat Med. 2014;20(7):709–11.
Calabrese EJ, Agathokleous E, Kozumbo WJ, Stanek EJ, Leonard D. Estimating the range of the maximum hormetic stimulatory response. Environ Res. 2019;170:337–43.
Özugur S, Kunz L, Straka H. Relationship between oxygen consumption and neuronal activity in a defined neural circuit. BMC Biol. 2020;18(1):76.
Xu J, Begley P, Church SJ, Patassini S, McHarg S, Kureishy N, et al. Elevation of brain glucose and polyol-pathway intermediates with accompanying brain-copper deficiency in patients with Alzheimer’s disease: metabolic basis for dementia. Sci Rep. 2016;6(1):27524.
Johnson RJ, Gomez-Pinilla F, Nagel M, Nakagawa T, Rodriguez-Iturbe B, Sanchez-Lozada LG, et al. Cerebral fructose metabolism as a potential mechanism driving Alzheimer’s disease. Front Aging Neurosc. 2020;12.
Visioli F, Ingram A, Beckman JS, Magnusson KR, Hagen TM. Strategies to protect against age-related mitochondrial decay: do natural products and their derivatives help? Free Radical Biol Med. 2022;178:330–46.
Liu D, Ke Z, Luo J. Thiamine deficiency and neurodegeneration: the interplay among oxidative stress, endoplasmic reticulum stress, and autophagy. Mol Neurobiol. 2017;54(7):5440–8.
Beltramo E, Mazzeo A, Porta M. Thiamine and diabetes: back to the future? Acta Diabetol. 2021;58(11):1433–9.
Sun Y, Peng C, Wang J, Sun H, Guo S, Zhang H. Metabolic footprint analysis of volatile metabolites to discriminate between different key time points in the fermentation and storage of starter cultures and probiotic Lactobacillus casei Zhang milk. J Dairy Sci. 2021;104(3):2553–63.
Morris AAM. Cerebral ketone body metabolism. J Inherit Metab Dis. 2005;28(2):109–21.
• Kolb H, Kempf K, Röhling M, Lenzen-Schulte M, Schloot NC, Martin S. Ketone bodies: from enemy to friend and guardian angel. BMC Med. 2021;19(1):313. Comprehensive discussion of the multiple actions of ketones.
Hung YH, Bush AI, Cherny RA. Copper in the brain and Alzheimer’s disease. J Biol Inorg Chem. 2010;15(1):61–76.
Xu J, Church SJ, Patassini S, Begley P, Waldvogel HJ, Curtis MA, et al. Evidence for widespread, severe brain copper deficiency in Alzheimer’s dementia†. Metallomics. 2017;9(8):1106–19.
Bagheri S, Squitti R, Haertlé T, Siotto M, Saboury AA. Role of copper in the onset of Alzheimer’s disease compared to other metals. Front Aging Neurosci. 2018;9.
Liu X-X, Wu P-F, Liu Y-Z, Jiang Y-L, Wan M-D, Xiao X-W, et al. Association between serum vitamins and the risk of Alzheimer’s disease in chinese population. J Alzheimer’s Dis. 2022;85:829–36.
Wang Q, Zhao J, Chang H, Liu X, Zhu R. Homocysteine and folic acid: risk factors for Alzheimer’s disease—an updated meta-analysis. Front Aging Neurosci. 2021;13:225.
Yin G, Gan Y, Jiang H, Yu T, Liu M, Zhang Y, et al. Direct quantification and visualization of homocysteine, cysteine, and glutathione in Alzheimer’s and Parkinson’s disease model tissues. Anal Chem. 2021;93(28):9878–86.
Ufnalska I, Drew SC, Zhukov I, Szutkowski K, Wawrzyniak UE, Wróblewski W, et al. Intermediate Cu(II)-thiolate species in the reduction of Cu(II)GHK by glutathione: a handy chelate for biological Cu(II) reduction. Inorg Chem. 2021;60(23):18048–57.
Zheng L, Han P, Liu J, Li R, Yin W, Wang T, et al. Role of copper in regression of cardiac hypertrophy. Pharmacol Ther. 2015;148:66–84.
Dringen R, Pfeiffer B, Hamprecht B. Synthesis of the antioxidant glutathione in neurons: supply by astrocytes of CysGly as precursor for neuronal glutathione. J Neurosci. 1999;19(2):562–9.
McBean GJ. The transsulfuration pathway: a source of cysteine for glutathione in astrocytes. Amino Acids. 2012;42(1):199–205.
Fenech M. Folate, DNA damage and the aging brain. Mech Ageing Dev. 2010;131(4):236–41.
Linnebank M, Lutz H, Jarre E, Vielhaber S, Noelker C, Struys E, et al. Binding of copper is a mechanism of homocysteine toxicity leading to COX deficiency and apoptosis in primary neurons, PC12 and SHSY-5Y cells. Neurobiol Dis. 2006;23(3):725–30.
Dong D, Wang B, Yin W, Ding X, Yu J, Kang YJ. Disturbance of copper homeostasis is a mechanism for homocysteine-induced vascular endothelial cell injury. PLoS One. 2013;8(10).
• Bagheri S, Saboury AA, Haertlé T, Rongioletti M, Saso L. Probable reasons for neuron copper deficiency in the brain of patients with Alzheimer’s disease: the complex role of amyloid. Inorganics. 2022;10(1):6. Discussion of the role of inadequate intracellular copper concentrations in the brain of AD patients.
Lauer AA, Grimm HS, Apel B, Golobrodska N, Kruse L, Ratanski E, et al. Mechanistic link between vitamin B12 and Alzheimer’s disease. Biomolecules. 2022;12(1):129.
Robinson N, Grabowski P, Rehman I. Alzheimer’s disease pathogenesis: is there a role for folate? Mech Ageing Dev. 2018;174:86–94. Current understanding of the role of folate in the pathogenesis of AD.
Scaglione F, Panzavolta G. Folate, folic acid and 5-methyltetrahydrofolate are not the same thing. Xenobiotica. 2014;44(5):480–8.
Serot JM, Christmann D, Dubost T, Béné MC, Faure GC. CSF-folate levels are decreased in late-onset AD patients. J Neural Transm. 2001;108(1):93–9.
Johanson CE, Johanson NL. Choroid plexus blood-CSF barrier: major player in brain disease modeling and neuromedicine. J Neurol Neuromed. 2018;3(4).
• Giovinazzo D, Bursac B, Sbodio JI, Nalluru S, Vignane T, Snowman AM, et al. Hydrogen sulfide is neuroprotective in Alzheimer’s disease by sulfhydrating GSK3β and inhibiting Tau hyperphosphorylation. Proc Natl Acad Sci. 2021;118(4): e2017225118. Discussion of hydrogen sulfide actions in protecting the brain.
• Chu X, Raju RP. Regulation of NAD+ metabolism in aging and disease. Metabolism. 2022;126: 154923. Excellent review of NAD metabolism in aging and disease.
Cantó C, Menzies KJ, Auwerx J. NAD(+) metabolism and the control of energy homeostasis: a balancing act between mitochondria and the nucleus. Cell Metab. 2015;22(1):31–53.
•• Chellappa K, McReynolds MR, Lu W, Zeng X, Makarov M, Hayat F, et al. NAD precursors cycle between host tissues and the gut microbiome. bioRxiv. 2021. Careful analysis of the microbe-host cycle in which NAD from precursors and fermented carbohydrates is made available to both participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
Studies cited in this article were in compliance with human informed consent and animal rights requirements.
Conflict of Interest
The authors declare they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nutrition and the Brain
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ettinger, S. Diet, Gut Microbiome, and Cognitive Decline. Curr Nutr Rep 11, 643–652 (2022). https://doi.org/10.1007/s13668-022-00435-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-022-00435-y