Abstract
Duplications of Yq arm (and AZF) seems to be tolerated by fertile males, while mutations, deletions, duplications or haploinsufficiency of SHOX can originate a wide range of phenotypes, including short stature and skeletal abnormalities. We report a case of non-obstructive azoospermia in a young man with short stature, skeletal anomalies, normal intelligence and hormonal parameters. This male showed a very singular Y-chromosome aberration, consisting of a duplication of Yq and proximal regions of Yp, with a deletion of almost all PAR1 in Yptel, including SHOX. CBA- and RBA-banding and FISH-mapping with telomeric, centromeric, AZF and SHOX probes were used. These results were confirmed by array CGH, which revealed the following karyotype constitution: arr [hg19] Xp22.33 or Yp11.32p11.31 (310,932–2,646,815 or 260,932–2,596,815) ×1, Yp11.2q12 (8,641,183–59,335,913) ×2. We conclude that the haploinsufficience of SHOX may be the cause of short stature and skeletal defects in the patient, while the non-obstructive azoospermia could be related to the lack of X–Y pairing during meiosis originated by the anomalous configuration of this chromosome abnormality and large deletion which occurred in Yp-PAR1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In nature, both numerical and structural chromosomal aberrations can have deleterious effects on fertility and, in the general population, their frequency is approximately 0.6% (Berger 1975), reaching, in males with infertility problems, higher values, varying between 2% and 14% (Shi and Martin 2000). The Y-chromosome aberrations may be both structural and numerical, and they may occur together and separately in the same subject. With the exception of sterility, no relevant physical abnormalities have been found so far, in consideration of the few genes present in this chromosome. What follows are the main structural anomalies on the Y chromosome. Dicentrism, the most frequent aberration of this chromosome, occurs in the case of transversal and not longitudinal division of chromatids. The result is an isochromosome with duplication of short or long arm. Microdeletion, mainly involving the AZF cluster or SRY gene (Hofherr et al. 2011). Ring, an aberration where losses of terminal p- or q-arms occur (Guilherme et al. 2013). Translocation X/Y or Y/autosomal (Dobek et al. 2015; Bispo et al. 2014; Gunel et al. 2008), Yp or Yq isochromosomes (Hemmat et al. 2013): these abnormalities occur very rarely.
Among the Y-chromosome numerical aberrations, the most common is the XXY syndrome (Klinefelter) form of hypogonadism and chromosome aneuploidy (0.15%) in the general male population (Bojesen et al. 2003), followed by the XYY syndrome, occurring in 0.1% of live male births. Although the karyotype 47,XYY is relatively common, this syndrome and its phenotypes are not yet well understood. The diagnosis of an XYY karyotype generally occurs late (around 17.1 years of age, on average) and only 15% of patients are diagnosed with this syndrome (Jo et al. 2015). The XYY phenotype is often correlated with short stature, increased head circumference (Geerts et al. 2003), and behavioural and psychiatric problems, such as attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) (Margari et al. 2014). Generally, XYY males have normal fertility, although azoospermic cases have been reported (for a review, see Bardsley et al. 2013); hyperdiploidy cases, such as 2n = 48,XYYY, have also been reported (Hunter and Quaife 1973). The duplication of Yq arms (and AZF) seems to be well tolerated by fertile males (Hsu et al. 2014), while mutations, deletions, duplications or haploinsufficiency of SHOX can originate a wide range of phenotypes, such as Léri–Weill dyschondrosteosis (LWD), Turner syndrome, disproportionate short stature (DSS) and Langer mesomelic dysplasia (LS) (Vinasco Sandoval et al. 2014; Gatta et al. 2014; Valetto et al. 2016).
In the present study, a young male was found to be affected by non-obstructive azoospermia during a pilot study (EcoFoodFertility initiative) to investigate biomarkers of early pollution damage on human semen. This study was conducted on healthy males living in various areas of different environmental impact in Italy (Bergamo et al. 2016). Subsequent cytogenetic and array CGH investigations revealed a very singular Y-chromosome aberration, showing the duplication of both Yq and proximal regions of Yp and the deletion of almost all PAR1 (including SHOX) in Yptel. Phenotypic, clinical and skeletal X-graph analyses have revealed that the patient showed short stature, skeletal defects and normal hormonal parameters. A similar structural chromosomal abnormality has been reported by Wiland et al. (2015).
Patient and methods
Clinical observations
A 23-year-old infertile male, in whom non-obstructive azoospermia was revealed, underwent cytogenetic analysis. He was the only son of healthy and non-consanguineous parents. The patient has no dysmorphic face, normal psychomotor development, short stature (25th centile) and weight of 69 kg (Fig. 1a). Skeletal X-graph revealed right dorsal and left lumbar scoliosis, asymmetric pelvis, short femoral necks and bilateral radial bowing. There were no other defects of the organs and apparatus. The case was found during a preliminary screening project (EcoFoodFertility initiative, http://www.ecofoodfertility.it/the-project.html), a multicentre, multidisciplinary research connecting human lifestyle and dietary habits to the environmental consequences of exposure to toxicants, with the aim to increase our knowledge of the environmental impact on human health using several biomarkers in both blood and semen of males living in areas with different environmental impacts (Bergamo et al. 2016).
Laboratory analyses and scrotal echography
The following clinical analyses were performed: testosterone, free testosterone, 17-alpha hydroxyprogesterone, dihydrotestosterone (DHT), 17-beta-2-estradiol, FSH, LH, prolactin and DHEA-S. Scrotal echography was also performed.
Cell cultures, chromosome banding and FISH-mapping techniques
Peripheral blood samples of both the young male and his father were cultured to obtain normal cultures (without addition of any base analogue) and cultures were treated with BrdU (15 μg/mL) and Hoechst33258 (30 μg/mL) 6 h before harvesting, to obtain late-BrdU incorporation and enhanced R-banding patterns. CBA-, RBA- and GTG-banding, as well as the FISH-mapping techniques, followed the protocols reported in Iannuzzi and Di Berardino (2008). For FISH-mapping analyses, the following BAC clones were used: PLAY5.5 (Y-centromere), RP11-800 K15 (containing SHOX), RP11-458F2 (containing AZF) and PNA telomeric probe. At least 100 cells were studied for both CBA- and RBA-banding with 10 karyotypes arranged, while 30 metaphases were studied for each probe used during FISH-mapping analyses.
Array CGH
For array CGH, we used the array platform SurePrintG3 CGH ISCA v2 8x60K with a real average resolution of about 250 kb in backbone. The detailed analysis was performed on 500 genomic regions associated with pathologies selected by the International Standards for Cytogenomic Arrays (ISCA) Consortium (http://www.iscaconsortium.org) for the application of array CGH technology. The reference database was: https://decipher.sanger.ac.uk, Genome Assembly hg19 (build 37), http://omim.org/. Finally, Agilent CytoGenomics 3.0.6.6 software was used for the analysis.
Results
Clinical analyses and echography
Hormonal concentrations were normal for testosterone (751.93 ng/dL), free testosterone (22.1 pg/mL), 17-alpha hydroxyprogesterone (1.3 ng/mL), dihydrotestosterone (DHT) (681 pg/mL), 17-beta-2-estradiol (E2) (25.0 pg/mL), FSH (6.4 mIU/mL, 6.4 mIU/mL, 5.7 mIU/mL at 0, 20 and 40 min, respectively), LH (3.3 mIU/mL, 3.0 mIU/mL and 2.9 mIU/mL at 0, 20 and 40 min, respectively), prolactin (15.6 ng/mL) and DHEA-S (436 μg/dL). Furthermore, scrotal echography did not reveal any abnormality.
Cytogenetic and array CGH analyses
While the karyotype of the father was normal, that of the son (Fig. 1b) showed an anomalous Y chromosome in all studied metaphases, as revealed by various chromosome banding techniques and FISH-mapping applications (Fig. 2). In particular, CBA-banding revealed two HC blocks in both Y-chromosome arms (Fig. 2a), while centromeric probe revealed one single centromere (Fig. 2c). Telomeric PNA probes revealed normal telomeres on both Y-arms (Fig. 2d). The presence of a duplication of the entire q-arm was confirmed by the AZF-specific probe, which revealed two clear and strong signals in both arms of the Y chromosome (Fig. 2e). These results were confirmed by array CGH, which showed the following result:
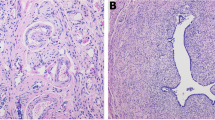
Composite figure showing details of the abnormal Y chromosome drawn from different cells (a–d) and treated for CBA-banding (a), RBA-banding (b), centromeric probe (c) and centromeric-telomeric probes (d). Note the strong HC blocks present in both Y-chromosome arms (a), only one centromeric FITC signal (c) and telomeric FITC signals on both Y-chromosome arms (d). Details of FISH-mapping with probes containing AZF and SHOX are also shown (e and f, respectively). Note the strong FITC signals with a probe containing AZF in both Y-chromosome arms (e, arrows) and the presence of FITC signals with a probe containing SHOX only at the telomeres of Xp (PAR1, large arrow), being absent in the abnormal Y chromosome (small arrow)
arr [hg19] Xp22.33 or Yp11.32p11.31 (310,932–2,646,815 or 260,932–2,596,815) ×1, Yp11.2q12 (8,641,183–59,335,913) ×2. Essentially, the array analysis evidenced the presence of an increased signal (duplication) in a large region of the Y chromosome of about 50 MB from Yp11.2 band to the band Yq12 (terminal end). Furthermore, a loss of signal (deletion) of about 2.3 MB on the X chromosome at the Xp22.33 band (PAR1) was also observed. Since PAR1 and PAR2 are homologous regions present on both X and Y chromosomes, these regions are present in a single copy on the array platform, and it is possible that the deletion observed on Xpter (PAR1) really occurred on Yp (PAR1 region). In fact, an FISH analysis with a probe containing SHOX (PAR1) has demonstrated that the deletion of the PAR1 region occurred in Ypter, being clear signals present only in Xpter (Fig. 2f). In addition, a PCR analysis with the marker DXY (Yp11.22q12, PAR1) (not shown) revealed its mono-allelic presence. Idiogrammatic representations of normal and abnormal G-banded Y chromosomes, with FISH-mapped loci in our study, are shown in Fig. 3.
Discussion
As mentioned above, the only similar case to our observation has been reported by Wiland et al. (2015). By matching the two observations, the following basic differences have been noted concerning the structural aberration. In the study of Wiland et al. (2015), the region covering the duplication is from qter → q11.22.1::p11.31 → qter, while in our case, it is from qter → q11.22.1::p11.2 → qter. In addition, in our case, the deletion which occurred in PAR1 (2.3 MB on the total 2.7 MB of PAR1) is larger than that which occurred in the case reported by Wiland et al. (2015). Indeed, while SHOX (PAR1) was present in the abnormal Y chromosome of the study by Wiland et al. (2015), it was absent in the abnormal Y chromosome of our case (Fig. 2f).
In Wiland et al.’s observation, the testis biopsy showed inhibited spermatogenesis at the spermatocyte level and tubular hyalinisation of lamina propria. The authors believe that this defect may have perturbed the conjugation of sex chromosomes during first meiotic division and could have led to spermatogenic arrest. Unfortunately, we could not perform histological analyses of seminiferous tubules of our patient, as done in the study of Wiland et al. (2015), to further support an abnormal spermatogenesis. However, the anomalous configuration of this chromosome abnormality and the deletion of almost all PAR1 could be the cause of the lack of sex chromosome pairing, thus explaining the azoospermia in the young man.
It is important to underline that the SHOX gene is involved in stature determination. The haploinsufficiency (as in our case) is responsible for the short stature of some genetic diseases, such as Léri–Weill syndrome. There is reason to believe that the short stature and skeletal defects of the patient are due to the presence of SHOX only in the Xpter, being deleted in Ypter. On the contrary, in the study of Wiland et al. (2015), where SHOX was present on the abnormal Y chromosome, the patient shoved normal stature and absence of skeletal defects. Since treatments with GH, during the development of patients affected by these genetic pathologies, seem to have some beneficial effect to increase stature (Valetto et al. 2016), an early discovery of these defects by both cytogenetic and genetic analyses is essential to reduce the worst effects of these pathologies on male carriers.
No single explanation can be supposed for the origin of the anomalous chromosome. One plausible explanation may be the following: the genotype might arise from the fertilisation of normal oocyte by a YY sperm. In one of the Y chromosomes occurred a separation between p and q and, later, an inverse interchromosomal translocation of only the long arm on the other entire Y chromosome. Another more likely possibility is that an entire q-arm duplication occurred with subsequent intrachromosomal inverse translocation. A third different acceptable understanding of this chromosome event has been reported by Wiland et al. (2015): an incorrect repair of DNA breaks in homologous chromatids of chromosome Y that led to the formation of the two abnormal rearranged chromatids, which segregated to two different spermatids after second meiotic division.
In conclusion, while the short stature and skeletal defects can be due to the SHOX haploinsufficiency, no complete explanation can be found for the non-obstructive azoospermia. As hypothesised above, the azoospermia could be due to the lack of X–Y pairing during meiosis due to both abnormal Y chromosome and deletion of almost all PAR1.
References
Bardsley MZ, Kowal K, Levy C, Gosek A, Ayari N, Tartaglia N, Lahlou N, Winder B, Grimes S, Ross JL (2013) 47,XYY syndrome: clinical phenotype and timing of ascertainment. J Pediatr 163(4):1085–1094
Bergamo P, Volpe MG, Lorenzetti S, Mantovani A, Notari T, Cocca E, Cerullo S, Di Stasio M, Cerino P, Montano L (2016) Human semen as an early, sensitive biomarker of highly polluted living environment in healthy men: a pilot biomonitoring study on trace elements in blood and semen and their relationship with sperm quality and RedOx status. Reprod Toxicol 66:1–9
Berger R (1975) The incidence of constitutional chromosome aberrations. J Genet Hum 23:42–49
Bispo AV, Burégio-Frota P, Oliveira dos Santos L, Leal GF, Duarte AR, Araújo J, Cavalcante da Silva V, Muniz MT, Liehr T, Santos N (2014) Y chromosome in Turner syndrome: detection of hidden mosaicism and the report of a rare X;Y translocation case. Reprod Fertil Dev 26(8):1176–1182
Bojesen A, Juul S, Gravholt CH (2003) Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. J Clin Endocrinol Metab 88:622–626
Dobek WA, Kim HG, Walls CA, Chorich LP, Tho SP, Wang ZX, McDonough PG, Layman LC (2015) Long-term follow-up of females with unbalanced X;Y translocations-reproductive and nonreproductive consequences. Mol Cytogenet 8:13
Gatta V, Palka C, Chiavaroli V, Franchi S, Cannataro G, Savastano M, Cotroneo AR, Chiarelli F, Mohn A, Stuppia L (2014) Spectrum of phenotypic anomalies in four families with deletion of the SHOX enhancer region. BMC Med Genet 15:87
Geerts M, Steyaert J, Fryns JP (2003) The XYY syndrome: a follow-up study on 38 boys. Genet Couns 14:267–279
Guilherme RS, Klein E, Hamid AB, Bhatt S, Volleth M, Polityko A, Kulpanovich A, Dufke A, Albrecht B, Morlot S, Brecevic L, Petersen MB, Manolakos E, Kosyakova N, Liehr T (2013) Human ring chromosomes—new insights for their clinical significance. Balkan J Med Genet 16(1):13–20
Gunel M, Cavkaytar S, Ceylaner G, Batioglu S (2008) Azoospermia and cryptorchidism in a male with a de novo reciprocal t(Y;16) translocation. Genet Couns 19(3):277–280
Hemmat M, Hemmat O, Boyar FZ (2013) Isochromosome Yp and jumping translocation of Yq resulting in five cell lines in an infertile male: a case report and review of the literature. Mol Cytogenet 6:36
Hofherr SE, Wiktor AE, Kipp BR, Dawson DB, Van Dyke DL (2011) Clinical diagnostic testing for the cytogenetic and molecular causes of male infertility: the Mayo Clinic experience. J Assist Reprod Genet 28:1091–1098
Hsu H-K, Su M-T, Chen M, Yen P, Kuo P-L (2014) Two Y chromosomes with duplication of the distal long arm including the entire AZFc region. Gene 536:444–448
Hunter H, Quaife R (1973) A 48,XYYY male: a somatic and psychiatric description. J Med Genet Mar 10(1):80–83
Iannuzzi L, Di Berardino D (2008) Tools of the trade: diagnostics and research in domestic animal cytogenetics. J Appl Genet 49(4):357–366
Jo WH, Jung MK, Kim KE, Chae HW, Kim DH, Kwon AR, Kim H-S (2015) XYY syndrome: a 13-year-old boy with tall stature. Ann Pediatr Endocrinol Metab 20:170–173
Margari L, Lamanna AL, Craig F, Simone M, Gentile M (2014) Autism spectrum disorders in XYY syndrome: two new cases and systematic review of the literature. Eur J Pediatr 173:277–283
Shi Q, Martin RH (2000) Aneuploidy in human sperm: a review of the frequency and distribution of aneuploidy, effects of donor age and lifestyle factors. Cytogenet Cell Genet 90:219–226
Valetto A, Bertini V, Michelucci A, Toschi B, Dati E, Baroncelli GI, Bertelloni S (2016) Short stature in isodicentric Y chromosome and three copies of the SHOX gene: clinical report and review of literature. Mol Syndromol 7:19–25
Vinasco Sandoval GT, Jaimes GC, Coll Barrios M, Cespedes C, Velasco HM (2014) SHOX gene and conserved noncoding element deletions/duplications in Colombian patients with idiopathic short stature. Mol Genet Genomic Med 2(2):95–102
Wiland E, Yatsenko AN, Kishore A, Stanczak H, Zdarta A, Ligaj M, Olszewska M, Wolski JK, Kurpisz M (2015) FISH and array CGH characterization of de novo derivative Y chromosome (Yq duplication and partial Yp deletion) in an azoospermic male. Reprod Biomed Online 31(2):217–224
Acknowledgements
The study has been partially supported by the “EcoFoodFertility” project. The authors wish to thank Mr. Domenico Incarnato, CNR-ISPAAM of Naples for his excellent technical assistance.
Author information
Authors and Affiliations
Contributions
DC performed array CGH and GTG-banding karyotypes and contributed to the data interpretation; AI and AP performed CBA- and RBA-banding karyotypes, all FISH-mapping analyses and contributed to the data interpretation; LM recruited the subject and performed the sperm analysis; OC provided the BAC clones; CS acquired some data and contributed to the data interpretation; MLV performed hormonal analyses, skeletal X-graph and contributed to the data interpretation; MU revised critically the manuscript for important intellectual content; LI and VV conceived the study and wrote the paper. All authors revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
We have the informed consent from the patient for this publication.
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. In particular, all studies conducted under the EcoFoodFertility project have been approved by the Ethical Committee, Coordination Service of the ASL Napoli 3, Naples, Italy, as reported in the Directive Determination N. 56 of July 15, 2015.
Additional information
Communicated by: Michal Witt
Rights and permissions
About this article
Cite this article
Cancemi, D., Iannuzzi, A., Perucatti, A. et al. Duplication of Yq- and proximal Yp-arms with deletion of almost all PAR1 (including SHOX) in a young man with non-obstructive azoospermia, short stature and skeletal defects. J Appl Genetics 58, 481–486 (2017). https://doi.org/10.1007/s13353-017-0412-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13353-017-0412-7