Abstract
Hypermethylation in the CpG island promoter regions of tumor suppressors is known to play a significant role in the development of HNSCC and the detection of which can aid the classification and prognosis of HNSCC. This study aims to profile the methylation patterns in a panel of key genes including CDKN2A, CDKN2B, KLOTHO (KL), RASSF1A, RARB, SLIT2, and SFRP1, in a group of HNSCC samples from Saudi Arabia. The extent of methylation in these genes is determined using the MethyLight assay and correlated with known clinicopathological parameters in our samples of 156 formalin-fixed and paraffin-embedded HNSCC tissues. SLIT2 methylation had the highest frequency (64.6%), followed by RASSF1A (41.3%), RARB (40.7%), SFRP1 (34.9), KL (30.7%), CKDN2B (29.6%), and CKDN2A (29.1%). KL and SFRP1 methylation were more predominant in nasopharyngeal tumors (P = 0.001 and P = 0.031 respectively). Kaplan Meier analysis showed that patients with moderately differentiated tumors who display SFRP1 methylation have significantly worse overall survival in comparison with other samples. In contrast, better clinical outcomes were seen in patients with KL methylation. In conclusion, our findings suggest that the detection of frequent methylation in SFRP1 and KL genes’ promoters could serve as prognostic biomarkers for HNSCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HNSCC is characterized as a heterogeneous and molecularly complex set of cancers that are caused by a variety of genetic and epigenetic aberrations that affect important mechanisms such as signal transduction, DNA repair, apoptosis, and cell cycle regulation pathways (Scully et al. 2000; Stadler et al. 2008). DNA cytosine hypermethylation within CpG island promoter regions is a chief epigenetic modification that induces the silencing of several tumor-related genes (Jones and Baylin 2002). Aberrant DNA methylation of several tumor-related genes has been frequently found in HNSCC (Czerninski et al. 2009; Demokan 2011; Hasegawa et al. 2002; Meng et al. 2016; Rigi-Ladiz et al. 2011). Many studies show that epigenetic aberrations in the promoter area of tumor suppressor genes play an important role in the initiation and progression of HNSCC (Cai et al. 2016; Fendri et al. 2009; Worsham et al. 2012). Hypermethylation of such genes is linked with clinical outcomes such as tumor stage, tumor size, and lymph node metastasis, and worse outcomes in HNSCC (Demokan 2011; Hasegawa et al. 2002; Ren et al. 2015).
Aberrant methylation of RASSF1A is associated with HNSCC stage (Hasegawa et al. 2002) and lymph node metastasis in nasophageal carcinomas (Fendri et al. 2009), as well as overall survival of oral squamous cell carcinoma (Huang et al. 2009). The down-regulation of SFRP1 by promoter hypermethylation is linked with tumor grade and stage (Demokan 2011) and worse survival (Ren et al. 2015). Moreover, methylated SFRP1 is associated with an elevated risk of recurrence in esophageal cancer (Liu et al. 2011). Methylated RARB is also found to be associated with highly differentiated nasopharyngeal tumors, tumor stage, and lymph node metastasis of nasopharyngeal carcinomas (Fendri et al. 2009). Aberrant methylation of the CDKN2B gene is associated with early stages of carcinogenesis in HNSCC (Xie et al. 2013). CDKN2A methylation is also associated with poorly differentiated tumor (Steinmann et al. 2009), lymph node metastasis, tumor stage, and size in HNSCC (Hasegawa et al. 2002). SLIT2 promoter methylation is associated with poor patient outcome (Maiti et al. 2015).
The full extent of DNA methylation patterns in HNSCC carcinogenesis is yet to be elucidated. Understanding such patterns and the subsequent pathways affected will improve our understanding of HNSCC pathogenesis and may eventually lead to better clinical management. Current clinical management of HNSCC needs improvement as such cancers have been associated with worse prognosis compared to other types of tumors (Economopoulou et al. 2016; Esteller 2002). Overall, the five-year survival rate for HNSCC patients for all sites and stages is <50%, with significantly lowered post-treatment quality of life (Carvalho et al. 2005; Worsham et al. 2012).
Promoter methylation events of the CDKN2A (Cyclin-dependent kinase inhibitor-2A), CDKN2B (Cyclin-dependent kinase inhibitor-2B), KL (KLOTHO), RASSF1A (Ras association (RalGDS/AF-6) domain family member 1A), RARB (Retinoic acid receptor beta), SLIT2 (slit guidance ligand 2), and SFRP1 (soluble frizzled receptor protein-1) genes have been commonly implicated in different tumorigenesis pathways. In the present study, we aim to assess the aberrant promoter methylation of these genes in HNSCC patients from Saudi Arabia and examine their potential as biomarkers for the disease.
Material and methods
Patients’ samples
This retrospective study includes 156 formalin-fixed Paraffin-embedded (FFPE) blocks containing tissue that met the World Health Organization (WHO) criteria for squamous cell carcinoma of the head and neck. Tissues were retrieved from the department of pathology, King Abdulaziz University Hospital, and from King Abdulaziz Medical City, National Guard Health Affairs, Jeddah, Saudi Arabia, covering the period 2005 through 2014. The samples consisted primarily of tumors from nasopharyngeal tumors (n = 52, 33%), larynx (n = 20, 13%), and other oral cavity sites [tongue (n = 53, 34%), buccal site (n = 14, 9%), lip (n = 13, 8%), and undefined (n = 4, 3%)]. The relevant clinicopathological data (Table 1) (gender, age, grade, lymph node status (LN), and tumor size (T)) were obtained from the patients’ records after obtaining the relevant ethical approvals (Unit of Biomedical Ethics, King Abdulaziz University Hospital No. 1127–13 and King Abdulaziz Medical City No. RJ13/042/J). Genomic DNA was extracted from the FFPE archival tissues utilizing the Qiagen QIAMP FFPE Tissue DNA extraction kit, following the manufacturer’s protocol.
Sodium bisulfite modification and MethyLight assay
Up to 500 nanograms of extracted DNA was incubated with sodium bisulfite to convert unmethylated cytosine residues to uracil, leaving methylated cytosine unchanged, utilizing Qiagen Epitect Bisulfite Conversion Kit. The methylation pattern of the promoter regions of seven candidate genes (CDKN2A, CDKN2B, KL, RASSF1A, RARB, SLIT2, and SFRP1) was assessed using the MethyLight assay that is specific to bisulfite modified DNA, utilizing the primers and probes sequences previously described (Dallol et al. 2011; Dallol et al. 2012; Dallol et al. 2015; Feng et al. 2008; Kuroki et al. 2003). COL2A1 was used as reference gene to normalize the methylation value of the input DNA for the targeted gene to the total amount of input DNA. In order to verify the specificity of the Methylight assay, a fully methylated DNA that had been treated with SssI-methyltransferase (Qiagen) was used as a positive control and fully unmethylated DNA as a negative control (Qiagen), by which methylated and unmethylated alleles were discriminated.
The percentage of fully methylated reference (PMR) was calculated by dividing the 1) ratio of the quantity of targeted gene to COL2A1 in a sample over 2) the ratio of the targeted gene to COL2A1 in the M.SssI-methylated and bisulfite-treated control, and then 3) multiplying by 100. Samples where the PMR value was above or equal to 10% were considered positive for methylation, whereas samples with a PMR value below 10% were considered unmethylated.
Statistical analysis
All data analysis was carried out using SPSS version 24 (IBM Crop., N.Y., USA). Fischer’s exact test (two-sided) was applied to evaluate the significance of the associations between methylation events and clinical parameters. Univariate and multivariate logistic-regression models were used to study the association between methylation level and clinical variants. The results of all models are reported using the odds ratio (OR), regression coefficient (B), and P value. The Kaplan-Meier test was used to estimate the impact of methylation patterns on overall survival. Overall survival was defined as the time (in months) from the date of diagnosis to the last recorded date of being alive or death. Two-sided P values less than 0.05 were considered significant.
Results
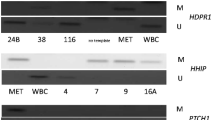
We screened 156 HNSCC patients elected on the basis of the availability of tissue block and patient data. The tumor tissue samples includes tissues that are surgically-resected from 57 females (36.5%) and 99 males (63.5%). The average age at diagnosis was 53 years (range, 11–96 years); 103 (66%) patients were under 45 years and 53 (34%) patients were above 45. Patient and tumor characteristics are detailed in Table 1. The methylation levels of the seven-gene panel used in this study was first confirmed to be tumor-specific by comparative analysis of matched non-tumorous tissues (Fig. 1). SLIT2 methylation showed the highest frequency in HNSCC tumor tissues (n = 122, 81%), followed by RASSF1A (n = 78, 52%), RARB (n = 77, 50%), CKDN2A (n = 55, 48%), SFRP1 (n = 66, 47%), KL (n = 58, 40%), and CKDN2B (n = 56, 36%). Only four cases (2.5%) exhibited significant methylation in all seven genes; interestingly, these cases were histologically classified as high grade tumors (grade 3). In contrast, three cases (2%) did not exhibit any detectable methylation for any of the seven genes and these cases were histologically classified as low grade tumors (grade 1) category. SFRP1 methylation was significantly associated with the hypermethylation of CDKN2A, KL, and SLIT2 (p < 0.001, p = 0.022, and p = 0.050, respectively). However, RARB methylation was negatively associated with CDKN2A (p = 0.046) and positively associated with KL (p = 0.045). Figure 2 illustrates the methylation frequency of the candidate genes in different tumor locations (i.e., nasopharyngeal, larynx, and oral cavity).
A multivariate logistic regression model was applied to assess the potential confounding effects of clinical variables on promoter methylation events for the seven genes in different settings. Adjusted models show that tumors originated from larynx were significantly associated with methylation events in both CDKN2A (p = 0.045) and CDKN2B (p = 0.009). In addition, tongue tumors exhibited significant levels of CDKN2B methylation (p = 0.012). Moreover, nasopharyngeal tumors were significantly associated with methylated CDKN2B (p = 0.016) and methylated SFRP1 (p = 0.018). Furthermore, methylation of both CDKN2A and SLIT2 promoters were weakly associated with moderately differentiated (grade 2) tumors originating from the larynx site (p = 0.039).
In terms of association with age, younger patients (≤ 45 years old) demonstrated more frequent, albeit not statistically significant, SFRP1 methylation compared to older patients (p = 0.053). Whereas, other methylated genes showed no significant association with age. In term of lymph node involvement, there was no significant correlation identified with the methylation of any gene. However, there was a significant association between tumor location and the methylation levels of CDKN2A, KL, SFRP, and SLIT2 (p = 0.001, p = 0.004 p = 0.00, and p = 0.001 respectively). Moreover, undifferentiated tumors (i.e., high grade tumors, grade 3) exhibited a significant association with methylation events for both KL (p = 0.002) and SFRP1 (p = 0.001).
Depending on methylation status, the data were sub-grouped by tumor location, gender, tumor grade, and age. We found that SFRP1 and CDKN2B methylation were more frequent in young nasopharyngeal cancer male patients (≤ 45 years old; p = 0.001 and p = 0.024, respectively). In contrast, KL promoter methylation was a frequent event in young female nasopharyngeal cancer patients (p = 0.033). Male patients with tumors originating from the larynx exhibit a weak correlation between moderately differentiated tumors and methylation events of SLIT2 (p = 0.039), CDKN2A (p = 0.006), and CDKN2B (p = 0.055). Tongue cancers from male patients were associated with low methylation levels of SLIT2 (p = 0.031) in poorly differentiated tumors and low methylation levels of CDKN2A in moderately or well-differentiated tumors (p = 0.025 and p = 0.027, respectively). No significant association between methylation patterns and overall survival for the seven genes were identified, as confirmed by Kaplan-Meier survival analysis. However, when stratified according to tumors grade, a significant association between SFRP1 methylation and poor survival in patients with moderately differentiated tumors (grade 2) was observed (p = 0.003). On the other hand, KL methylation correlated with favorable prognosis (p = 0.010) in nasopharyngeal cancer patients (Fig. 3).
Discussion
Epigenetic aberrations of several tumor-related genes have been reported recently as one of the common inactivation mechanisms in head and neck cancers (Meng et al. 2016). In this study, we analyzed DNA hypermethylation of seven genes in 156 cases of HNSCC. Methylation of six genes (CDKN2A, CDKN2B, RASSF1A, RARB, SLIT2, and SFRP1) was previously reported in head and neck cancers (Fendri et al. 2009; Gröbe et al. 2013; Maiti et al. 2015; Marsit et al. 2006; Maruya et al. 2004). Frequent hypermethylation of KL has been recently reported in breast and cervical cancer (Dallol et al. 2015; Lee et al. 2010). To our knowledge, this is the first study to show a significant association between the presence of methylation of the KL promoter and young female with nasopharyngeal cancer patients (≤ 45 years old; p = 0.033). It is interesting to hypothesize that KL hypermethylation may be connected with the female physiology and thus more frequent in female cancer patients (Dallol et al. 2015; Rubinek et al. 2012). Wolf et al. (2008) reported an association between women with breast cancer with BRCA1 mutations and lower KL expression (Wolf et al. 2008). Lee et al. (2010) reported that epigenetic silencing of KL was associated with aberrant activation of the Wnt pathway in invasive cervical carcinoma (Lee et al. 2010). KL is a hormone that plays important roles in longevity and cellular homeostasis (Dallol et al. 2015; Kurosu et al. 2005). Moreover, several studies have reported that KL displays a tumor suppressive role in many cancers by inhibiting the growth factor receptor signaling (IGF-1R signaling) pathway that stimulate cell proliferation and migration (Lee et al. 2010). Taken together, these data and the literature suggest that KL methylation is a potential tumor suppressor gene for HNSCC progression.
Previously, it was reported that inactivation of SLIT2 by methylation had prognostic value in HNSCC as it was one of the early events in the development of neoplasm in head and neck (Maiti et al. 2015). In the current study, SLIT2 was the most frequently methylated gene, occurring in about (n = 122, 80.8%) of all cases, which suggest that SLIT2 methylation status might be an early event in HNSCC tumorigenesis. The SLIT2 gene encodes a small non-coding RNA called microRNA-218 (miRNA-218) within one of its introns (Zhang et al. 2013). It has been shown that miRNA-218 functions as a tumor suppressor that inhibits the expression of oncogenes (Kinoshita et al. 2012). miRNA-218 specifically targets the pro-migration and invasion candidate oncogene LAMB3 in HNSCC cells (Kinoshita et al. 2012). MicroRNA-218 is epigenetically regulated by SLIT2 gene as miRNA-218 was shown recently to be suppressed by SLIT2 hypermethylation in oral SCC (Rodriguez et al. 2004). Therefore, aberrant promoter methylation of SLIT2 is likely to lead to transcriptional silencing of miRNA-218 in several cancer tissues, thus reducing its tumor suppressor activities.
In line with other studies, CDKN2A, CDKN2B, RARB, and RASSF1A were frequently methylated in our samples. However, our results failed to find a significant correlation between such genes and age, gender, tumor size, and lymph node involvement. This could indicate a different underlying mechanism(s) of HNSCC carcinogenesis in our samples.
This study also showed that a number (n = 66, 46.8%) of patients with HNSCC exhibited significant hypermethylation in the SFRP1 promoter. This finding is lower than the percentage of SFRP1 promoter hypermethylation reported in HNSCC previously (Marsit et al. 2006). However, this study reports that SFRP1 methylation is more frequent in young male nasopharyngeal cancer patients (n = 15, 29%), (p = 0.001). Abnormal methylation of SFRP1 is likely to result in an aberrant Wnt/β-catenin signaling pathway, which is required for cell differentiation, proliferation, and adhesion (Ren et al. 2015). Compared with other head and neck tumors, early distant metastasis and high rates of local invasion have been observed in patients with nasopharyngeal cancer (Kinoshita et al. 2012; Lee et al. 1992). Our finding shows the close association of SFRP1 methylation with clinical outcomes in HNSCC patients. Kaplan–Meier analysis showed that patients with moderately differentiated tumors who display SFRP1 methylation have significantly worse overall survival. A similar finding between SFRP1 promoter methylation and unfavorable prognosis has been demonstrated for brain tumors (Majchrzak-Celińska et al. 2016), bladder cancers (Marsit et al. 2005), and breast cancer (Veeck et al. 2006). Conversely, a better clinical outcome was seen in patients with KL methylation, unlike the previous report by Xie et al., whose study linked KL methylation with poor prognosis in hepatocellular carcinoma (Xie et al. 2013).
Our findings show that by examining the methylation frequency of the seven genes, HNSCC tumors can be stratified accordingly. Therefore, the methylome of this group of tumors is likely to reveal interesting biomarkers that can help provide a better understanding of this disease and its progression.
References
Cai F, Xiao X, Niu X, Shi H, Zhong Y (2016) Aberrant Methylation of MGMT promoter in HNSCC: a meta-analysis. PLoS One 11:e0163534. doi:10.1371/journal.pone.0163534
Carvalho AL, Nishimoto IN, Califano JA, Kowalski LP (2005) Trends in incidence and prognosis for head and neck cancer in the United States: a site-specific analysis of the SEER database. Int J Cancer 114:806–816. doi:10.1002/ijc.20740
Czerninski R, Krichevsky S, Ashhab Y, Gazit D, Patel V, Ben-Yehuda D (2009) Promoter hypermethylation of mismatch repair genes, hMLH1 and hMSH2 in oral squamous cell carcinoma. Oral Dis 15:206–213. doi:10.1111/j.1601-0825.2008.01510.x
Dallol A, Al-Ali W, Al-Shaibani A, Al-Mulla F (2011) Analysis of DNA methylation in FFPE tissues using the MethyLight technology. Methods Mol Biol 724:191–204. doi:10.1007/978-1-61779-055-3_13
Dallol A et al (2012) Methylation of the polycomb group target genes is a possible biomarker for favorable prognosis in colorectal cancer cancer epidemiology, biomarkers & prevention. Oncology 21:2069–2075. doi:10.1158/1055-9965.epi-12-0755
Dallol A et al (2015) Frequent methylation of the KLOTHO gene and overexpression of the FGFR4 receptor in invasive ductal carcinoma of the breast. Tumour Biol 36:9677–9683. doi:10.1007/s13277-015-3733-3
Demokan S, Dalay N (2011) Role of DNA methylation in head and neck cancer. Clin Epigenetics 2:123–150. doi:10.1007/s13148-011-0045-3
Economopoulou P, Perisanidis C, Giotakis EI, Psyrri A (2016) The emerging role of immunotherapy in head and neck squamous cell carcinoma (HNSCC): anti-tumor immunity and clinical applications. Ann Transl Med 4, 173. doi:10.21037/atm.2016.03.34
Esteller M (2002) CpG island hypermethylation and tumor suppressor genes: a booming present, a brighter future. Oncogene 21:5427–5440. doi:10.1038/sj.onc.1205600
Fendri A et al (2009) Inactivation of RASSF1A, RARbeta2 and DAP-kinase by promoter methylation correlates with lymph node metastasis in nasopharyngeal carcinoma. Cancer Biol Ther 8:444–451
Feng Q et al (2008) DNA methylation in tumor and matched normal tissues from non-small cell lung cancer patients. Cancer epidemiology, biomarkers & prevention. Oncology 17:645–654. doi:10.1158/1055-9965.EPI-07-2518
Gröbe A et al (2013) Immunohistochemical analysis of p16 expression, HPV infection and its prognostic utility in oral squamous cell carcinoma. J Oral Pathol Med 42:676–681. doi:10.1111/jop.12086
Hasegawa M, Nelson HH, Peters E, Ringstrom E, Posner M, Kelsey KT (2002) Patterns of gene promoter methylation in squamous cell cancer of the head and neck. Oncogene 21:4231–4236. doi:10.1038/sj.onc.1205528
Huang KH, Huang SF, Chen IH, Liao CT, Wang HM, Hsieh LL (2009) Methylation of RASSF1A, RASSF2A, and HIN-1 is associated with poor outcome after radiotherapy, but not surgery, in oral squamous cell carcinoma. Clin Cancer Res 15:4174–4180. doi:10.1158/1078-0432.CCR-08-2929
Jones PA, Baylin SB (2002) The fundamental role of epigenetic events in cancer. Nat Rev Genet 3:415–428. doi:10.1038/nrg816
Kinoshita T et al (2012) Tumor suppressive microRNA-218 inhibits cancer cell migration and invasion through targeting laminin-332 in head and neck squamous cell carcinoma. Oncotarget 3:1386–1400. doi:10.18632/oncotarget.709
Kuroki T, Trapasso F, Yendamuri S, Matsuyama A, Alder H, Mori M, Croce CM (2003) Allele loss and promoter hypermethylation of VHL, RAR-beta, RASSF1A, and FHIT tumor suppressor genes on chromosome 3p in esophageal squamous cell carcinoma. Cancer Res 63:3724–3728
Kurosu H et al (2005) Suppression of aging in mice by the hormone. Klotho Science 309:1829–1833. doi:10.1126/science.1112766
Lee AW et al (1992) Retrospective analysis of 5037 patients with nasopharyngeal carcinoma treated during 1976-1985: overall survival and patterns of failure. Int J Radiat Oncol Biol Phys 23:261–270
Lee J et al (2010) The anti-aging gene KLOTHO is a novel target for epigenetic silencing in human cervical carcinoma. Mol Cancer 9:109. doi:10.1186/1476-4598-9-109
Liu JB et al (2011) Plasma DNA methylation of Wnt antagonists predicts recurrence of esophageal squamous cell carcinoma. World J Gastroenterol 17:4917–4921. doi:10.3748/wjg.v17.i44.4917
Maiti GP et al (2015) Frequent inactivation of SLIT2 and ROBO1 signaling in head and neck lesions: clinical and prognostic implications. Oral Surg Oral Med Oral Pathol Oral Radiol 119:202–212. doi:10.1016/j.oooo.2014.09.029
Majchrzak-Celińska A, Słocińska M, Barciszewska AM, Nowak S, Baer-Dubowska W (2016) Wnt pathway antagonists, SFRP1, SFRP2, SOX17, and PPP2R2B, are methylated in gliomas and SFRP1 methylation predicts shorter survival. J Appl Genet 57:189–197. doi:10.1007/s13353-015-0312-7
Marsit CJ et al (2005) Epigenetic inactivation of SFRP genes and TP53 alteration act jointly as markers of invasive bladder cancer. Cancer Res 65:7081–7085. doi:10.1158/0008-5472.CAN-05-0267
Marsit CJ, McClean MD, Furniss CS, Kelsey KT (2006) Epigenetic inactivation of the SFRP genes is associated with drinking, smoking and HPV in head and neck squamous cell carcinoma. Int J Cancer 119:1761–1766. doi:10.1002/ijc.22051
Maruya S, Issa JP, Weber RS, Rosenthal DI, Haviland JC, Lotan R, El-Naggar AK (2004) Differential methylation status of tumor-associated genes in head and neck squamous carcinoma: incidence and potential implications. Clin Cancer Res 10:3825–3830. doi:10.1158/1078-0432.CCR-03-0370
Meng RW et al (2016) Aberrant Methylation of RASSF1A closely associated with HNSCC, a meta-analysis. Sci Rep 6:20756. doi:10.1038/srep20756
Ren XY et al (2015) Low SFRP1 expression correlates with poor prognosis and promotes cell invasion by activating the Wnt/β-catenin signaling pathway in NPC. Cancer Prev Res (Phila) 8:968–977. doi:10.1158/1940-6207.CAPR-14-0369
Rigi-Ladiz MA, Kordi-Tamandani DM, Torkamanzehi A (2011) Analysis of hypermethylation and expression profiles of APC and ATM genes in patients with oral squamous cell carcinoma. Clin Epigenetics 3:6. doi:10.1186/1868-7083-3-6
Rodriguez A, Griffiths-Jones S, Ashurst JL, Bradley A (2004) Identification of mammalian microRNA host genes and transcription units. Genome Res 14:1902–1910. doi:10.1101/gr.2722704
Rubinek T et al (2012) Epigenetic silencing of the tumor suppressor klotho in human breast cancer breast. Cancer Res Treat 133:649–657. doi:10.1007/s10549-011-1824-4
Scully C, Field JK, Tanzawa H (2000) Genetic aberrations in oral or head and neck squamous cell carcinoma (SCCHN): 1. Carcinogen metabolism, DNA repair and cell cycle control. Oral Oncol 36:256–263
Stadler ME, Patel MR, Couch ME, Hayes DN (2008) Molecular biology of head and neck cancer: risks and pathways. Hematol Oncol Clin North Am 22:1099–1124, vii. doi:10.1016/j.hoc.2008.08.007
Steinmann K, Sandner A, Schagdarsurengin U, Dammann RH (2009) Frequent promoter hypermethylation of tumor-related genes in head and neck squamous cell carcinoma. Oncol Rep 22:1519–1526
Veeck J et al (2006) Aberrant methylation of the Wnt antagonist SFRP1 in breast cancer is associated with unfavourable prognosis. Oncogene 25:3479–3488. doi:10.1038/sj.onc.1209386
Wolf I et al (2008) Klotho: a tumor suppressor and a modulator of the IGF-1 and FGF pathways in human breast cancer. Oncogene 27:7094–7105. doi:10.1038/onc.2008.292
Worsham MJ, Ali H, Dragovic J, Schweitzer VP (2012) Molecular characterization of head and neck cancer: how close to personalized targeted therapy? Mol Diagn Ther 16:209–222. doi:10.2165/11635330-000000000-00000
Xie B, Zhou J, Yuan L, Ren F, Liu DC, Li Q, Shu G (2013) Epigenetic silencing of Klotho expression correlates with poor prognosis of human hepatocellular carcinoma. Hum Pathol 44:795–801. doi:10.1016/j.humpath.2012.07.023
Zhang C, Ge S, Hu C, Yang N, Zhang J (2013) MiRNA-218, a new regulator of HMGB1, suppresses cell migration and invasion in non-small cell lung cancer. Acta Biochim Biophys Sin Shanghai 45:1055–1061. doi:10.1093/abbs/gmt109
Acknowledgements
The authors would like to thank the Ministry of Education and King Abdulaziz City for Science and Technology (KACST) for their financial support. Special thanks are extended to Maram Amin, Najla Filimban, and Fatma Gazzaz for their valuable technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Communicated by: Michal Witt
Rights and permissions
About this article
Cite this article
Alsofyani, A.A., Alsiary, R.A., Samkari, A. et al. Prognostic potential of KLOTHO and SFRP1 promoter methylation in head and neck squamous cell carcinoma. J Appl Genetics 58, 459–465 (2017). https://doi.org/10.1007/s13353-017-0404-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13353-017-0404-7