Abstract
Minimally invasive hepatectomy for benign and malignant liver lesions has gained popularity in the past decade due to improved perioperative outcomes when compared to conventional ‘open’ technique. We aim to investigate our initial experience of robotic hepatectomy undertaken in our hepatobiliary program. All patients undergoing robotic hepatectomy between 2013 and 2018 were prospectively followed. Data are presented as median (mean ± SD). A total of 80 patients underwent robotic hepatectomy within the study period. 60% of the patients were women, age of 63 (62.4 ± 14.1), body mass index of 28 (29.6 ± 9.4), ASA class of 2.5 (2.5 ± 0.6), and MELD score of 7 (8.2 ± 2.8). Size of resected lesion was 3.9 (4.6 ± 3) cm. Indications for resection were metastatic lesions (30%), hepatocellular carcinoma (28%), cholangiocarcinoma (7%), gallbladder cancer (5%), neuroendocrine tumors (4%), and benign lesions (26%). Formal hepatectomy (right or left) was performed in 30% of the patients. Operative time was 233 (267.2 ± 109.6) minutes, and estimated blood loss was 150 (265.7 ± 319.9) ml. Length of hospital stay was 3 (5.0 ± 4.6) days. One patient was converted to ‘open’ approach. 10 patients experienced postoperative complications. Readmissions within 30 days of hospital discharge were seen in eight patients. Our data support that robotic hepatectomy is safe and feasible, with favorable short-term outcomes and low conversion rate. Robotic technology extends the application of minimally invasive techniques in the field of hepatobiliary surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Minimally invasive liver surgery has gained popularity since the first-reported laparoscopic liver resection for benign tumor in 1991 [1]. Laparoscopic liver surgery has been shown to be safe with better perioperative outcomes when compared to the traditional ‘open’ approach, as it was associated with decreased intraoperative blood loss, decreased length of hospital stay, decreased morbidity, and lower mortality with no difference in long-term oncological outcomes when performed for malignant tumors [2,3,4,5,6,7]. Minimally invasive hepatobiliary surgery remains to be a challenging field that demands a high level of experience along with advanced training. In the last decade, laparoscopic liver resection pioneered the minimally invasive approach in liver surgery; however, there are inherited limitations of this technique including limited degree of motion, tremor amplification, poor ergonomics, fulcrum effect against the port, and difficulty in two-dimensional image adaptation [8, 9]. Therefore, this field has been faced with slower adoption among liver surgeons with hesitation to widely apply this technique [10].
Robotic liver surgery represents the most recent evolution in the field of minimally invasive liver surgery. It was introduced initially to overcome the aforementioned limitations of laparoscopic liver surgery, as the robotic technology provides the operating surgeon better magnified three-dimensional view, elimination of physiological tremor, improved dexterity with seven degrees of freedom, ease of suturing, and better motion scaling [11, 12]. Large studies have relatively been limited regarding the use of robotic hepatectomy in the treatment of liver tumors. Published reports in the literature mostly contain small number of patients by a single surgeon. Many hepatobiliary centers performing minimally invasive hepatectomy are still in the exploration phase of robotic technology. We designed this study to evaluate the safety of robotic hepatectomy undertaken in our hepatobiliary program. Herein, we report our experience and clinical outcomes of 80 robotic hepatectomy for benign and malignant tumors, which is to our knowledge the largest series reported to date. We hypothesize that the use of robotic hepatectomy is safe and feasible, and this technique can be universally applied for benign and malignant liver tumors.
Materials and methods
With institutional review board approval, 80 consecutive patients undergoing robotic hepatectomy between 2013 and 2018 in a single hepatobiliary center were prospectively followed. There were 10 other patients who underwent open hepatectomy and 0 patient underwent laparoscopic hepatectomy (a total of 90 patients underwent hepatectomy within the study period). Majority of the robotic hepatectomy (85%) were undertaken in 2017–2018 after the addition of first author (IS) into our hepatopancreatobiliary unit, following completion of a minimally invasive gastrointestinal surgery fellowship (Yale University School of Medicine 2015) and a hepatopancreatobiliary surgery fellowship (University of Pittsburgh Medical Center-Starzl Institute 2016). Coauthors SR and AR functioned as cosurgeons during these cases, mainly working at the bedside as a ‘wingman’. Patient demographics including body mass index (BMI), sex, age, American Society of Anesthesiologists (ASA) score, operative time, estimated blood loss (EBL), ‘open’ conversion rate, perioperative complication, blood transfusion rate, and length of hospital stay (LOS) were collected and analyzed. Data are presented as median (mean ± SD).
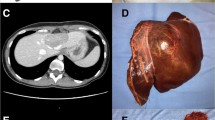
All of the robotic hepatectomies were undertaken in a 475-bed tertiary non-university teaching hospital using the da Vinci Xi® system (Intuitive Surgical, Sunnyvale, CA, USA). Our hepatopancreaticobiliary unit was established in 2013 with capability of undertaking major open and minimally invasive hepatopancreaticobiliary resections. Indications and preoperative evaluation for robotic hepatectomy are similar to those of ‘open’ liver resection, according to the International Hepato-Pancreato-Biliary Association. Imaging of the liver is obtained with triphasic liver computed tomography (CT) scan or magnetic resonance imaging (MRI). Biopsy is generally reserved only in cases of diagnostic uncertainty. Evaluation of future liver remnant volume and patient general health performance is similar to those of ‘open’ operation. All patients who require resection of a liver tumor(s) in our program are subjected to the robotic approach, unless it is considered technically unsafe or unfeasible. Robotic hepatectomy is not attempted in patients with obvious main portal vein, hepatic artery, hepatic vein trifurcation, or inferior vena cava tumor invasion, or in whom complex vasculobiliary resection/reconstruction might be necessary such as in Klatskin tumor. Direct tumor invasion into right hemidiaphragm, large tumor size, cirrhotic liver, prior open abdominal operation, and prior open liver resection(s)/ablation(s) are not considered contraindication for the robotic hepatectomy.
Major complications are defined as bleeding, leak, internal organ injury, or others which require deviation from routine procedure. Nearly all of our postoperative hepatobiliary patients are managed on a regular surgical floor, unless major issues are observed intraoperatively or anticipated postoperatively. In those unusual circumstances, the patients are managed in the intensive care unit.
Results
A total of 80 patients underwent robotic hepatectomy within the study period. 60% of the patients were women, age of 63 (62.4 ± 14.1) years old, body mass index of 28 (29.6 ± 9.4) kg/m2, ASA class of 2.5 (2.5 ± 0.6), and MELD score of 7 (8.2 ± 2.8). Size of resected lesion was 3.9 (4.6 ± 3) cm (Table 1). Indications for the hepatectomy were hepatocellular carcinoma (27.5%), intrahepatic cholangiocarcinoma (7.5%), gallbladder cancer (5%), colorectal cancer (26.3%), neuroendocrine tumors (3.8%), and benign tumors (26.3%) (Table 2). 41% of patients underwent left liver resection, 43% underwent right liver resection, while the remaining 16% underwent central liver resection. Formal hemihepatectomy (right or left) was performed in 25% of the patients (Table 3). Operative time was 233 (267.2 ± 109.6) min, and estimated blood loss was 150 (265.7 ± 319.9) ml. Length of hospital stay was 3 (5.0 ± 4.6) days [Table 3]. One patient was converted to the conventional ‘open’ approach due to difficulty in accessing a tumor located in posteromedial segment 8. While major intraoperative complications were not seen, ten (12.5%) patients experienced postoperative complications including bile leak, respiratory failure, wound complications at the specimen extraction port site, enterocutaneous fistula, urinary retention, and atrial fibrillation. Readmissions within 30 days of hospital discharge were seen in eight (10%) patients (Table 3). Three patients returned to the hospital due to liver specific complications (two bile leaks and one transient jaundice). None of them required reoperation. One patient had positive resection margin following a left extended hepatectomy for hepatocellular carcinoma involving beyond the secondary biliary duct of the future liver remnant. Mortality within 30 days after operation was seen in one patient who developed postoperative respiratory failure.
Discussion
Hepatobiliary surgery has been always recognized as a challenging field of surgery, which is associated with delicate works around the complex vascular and biliary structures, necessitating meticulous and precise dissections [13]. Therefore, majority of hepatobiliary operations are performed with the traditional ‘open’ approach. A large ‘open’ incision is associated with significant postoperative pain, high narcotic requirement, increased length of hospital stay, and significant wound complications. Minimally invasive surgery has proven its advantages over the traditional ‘open’ approach, including shorter hospital stay, decreased postoperative pain, better cosmesis, and rapid return to preoperative activity [14]. Multiple studies comparing the outcomes of laparoscopic and ‘open’ liver operations had confirmed similar results [3, 15]. In a meta-analysis comparing laparoscopic to ‘open’ liver surgery, it was found that the laparoscopic liver operations were associated with lower blood loss, decreased need for blood transfusion, shorter hospital stay, and lower 30-day mortality rate compared to the traditional ‘open’ approach. This meta-analysis demonstrated the superiority of laparoscopic liver resection [16].
In many other surgical subspecialties, minimally invasive approach had been widely adopted and has even become the standard of care. Laparoscopic liver surgery despite its clear superiority has not been widely adopted by many liver surgeons due to its technical complexity and challenging nature, more specifically the steep learning curve associated with laparoscopic liver resection. Difficulty in mastering this technique partly stems from the inherited limitations of laparoscopic techniques, including the fulcrum effect and the limited degree of instruments movement [17]. The robotic system overcomes these limitations by providing the surgeon three-dimensional high-definition surgical vision, better motion scaling, and internal articulated endowrist motion. These benefits can be clearly appreciated when performing a meticulous dissection around the liver hilum and near the major vascular structures, including the inferior vena cava and the portal vein [17]. The robotic system also allows the operating surgeon to use three robotic arms. The third arm can be locked in place while operating with other two arms, which provides a great advantage in certain situations such as when performing intracorporeal suturing or vascular clamping in difficult locations [18].
Studies evaluating the safety and feasibility of using the robotic approach for hepatobiliary surgery have been relatively limited. Most case series are single institutional with low number of patients (< 50 patients). It has only been a decade since the robotic technology was introduced to the field of liver surgery. As mentioned above, robotic technology offers solutions to the inherited limitations of laparoscopic approach; however, robotic surgical system comes with higher costs, which can be prohibitive to many programs and places. Consequently, the exploration of the safety and the outcomes of robotic liver surgery has been limited to high-volume academic/transplant centers.
In this series, most of the patients were middle-aged overweight women; majority of them had normal preoperative bilirubin with low MELD score. The majority of the resections were undertaken for malignant lesions, with hepatocellular carcinoma and colorectal liver metastasis being the most common. Few had metastatic tumors from other origins such as ovarian, stomach and renal cell cancer. Resections for liver metastases were considered only in the absence of peritoneal carcinomatosis or unresectable extrahepatic disease. All patients except one had negative margins after the resection. The single R1 case was seen in a patient who underwent extended left hepatectomy for a 17-cm left-sided hepatocellular carcinoma involving a deep intrahepatic portion of the right posterior hepatic duct, beyond the secondary biliary radicles. Further, more aggressive bile duct resection followed by Roux-en-Y hepaticojejunostomy reconstruction was deemed unsafe. A quarter of the patients had benign indications for liver resections. Those lesions were resected because of severe symptoms (pain, fullness, and early satiety) associated with the large tumors or in the presence of diagnostic uncertainty despite multiple preoperative core needle biopsies.
More complex resections were performed in this series than any other reported series in the literature, as 30% of the patients underwent formal or extended left/right hepatectomies [14, 19]. Our median length of hospital stay was only 3 days, which was difficult to simulate with ‘open’ liver resection. The short hospital stay is contributed by minimal postoperative pain, lower narcotic requirement, earlier resumption of oral intake (postoperative day 0), and shorter in-hospital recovery after robotic hepatectomy. The median estimated blood loss for the entire cohort was 150 ml, with only one patient required intraoperative blood transfusion. Bleeding control is one of the most challenging aspects of minimally invasive hepatectomy. Robotic system facilitates meticulous dissection of the inflow vascular structures, which is the key factor of performing anatomical liver resection. Anatomical liver resection is associated with lower blood loss [20, 21]. Bleeding from the hepatic veins during parenchymal transection is also frequently the source of significant blood loss. We routinely lower the central venous pressure to < 5 mmHg and remove the positive end expiratory pressure (PEEP) during the parenchymal transection, in addition to detail mapping of the intrahepatic vascular structures prior to starting the transection. While several different energy device options exist for open and laparoscopic hepatectomy, the choice is rather limited with the robotic technique. We utilize robotic monopolar electrocautery for < 2 cm superficial liver parenchymal transection, followed by a robotic vessel sealer™ (Intuitive Surgical, Sunnyvale, CA, USA) for the deeper parenchymal transection. The robotic vessel sealer is capable of handling/sealing intraparenchymal blood vessels ≤ 7 mm in diameter. To achieve bloodless liver parenchymal transection, we activate the jaws while gradually closing them. Two applications of coagulation were done prior to cutting. For the crossing intrahepatic vascular structures ≥ 8 mm, we prefer to use either a linear vascular stapler or Hemolock clips™ (Intuitive Surgical, Sunnyvale, CA, USA). The robotic approach provides the surgeon with superior three-dimensional visualization, better depth perception, increased dexterity, increased degree of freedom, and ease of suturing. All of these advantages facilitate precise parenchymal transection and further minimize blood loss.
While this paper was not designed to compare the results of robotic versus open and laparoscopic hepatectomy, our results compared favorably to other reported series [20]. Internally within our program, we do not have a laparoscopic group for comparison since we mainly utilize robotic approach for all our minimally invasive hepatectomies. On the contrary, patients who underwent open hepatectomy typically require major vessel resection and reconstruction, which make this an “apple to orange” comparison. In this current series, ten (13%) patients experienced postoperative complications, which is lower than those reported in the literature. Ho et al. conducted a systemic review of 19 case series including a total of 217 liver resections, where they reported 20% postoperative complication rate [20]. Choi et al. [17] from a modern Asian liver cancer center in Korea reported 43.3% postoperative complication rate. The most common complication in our series was bile leak (3.8%). All of these patients were managed with computed tomography (CT)-guided percutaneous drainage, and the drain was removed within 1–3 weeks after the placement. One patient developed respiratory insufficiency triggered by pneumonia and pleural effusions after a robotic right partial hepatectomy for hepatocellular carcinoma. His respiratory insufficiency was further complicated by multiorgan failure and the patient eventually died on postoperative day 16. One patient developed an enterocutaneous fistula, most likely from an unrecognized bowel injury during extensive lysis of adhesions. This patient had several prior incisional hernia repairs with synthetic mesh placement.
The rate of ‘open’ conversion in our series was 1% due to difficult access to the posteromedially located segment 8 tumor. Most series reported ‘open’ conversion rate between 6.7% and 20% [13, 17,18,19,20,21,22,23,24]. Despite the true advantage of robotic approach over the conventional laparoscopic method in liver surgery has not been validated in a randomized clinical trial, we as strong proponents of robotic hepatectomy believe that robot enables more complex liver resections to be done safely. Because the robotic technique overcomes many of the technical limitations of laparoscopic liver resection, a greater percentage of major hepatectomy can be completed in a truly minimally invasive fashion, without the need of a handport or a minilaparotomy incision [19]. Tsung et al. reported a matched comparison study comparing robotic to laparoscopic hepatectomies. In that study, 93% of robotic hepatectomies were completed in purely minimally invasive fashion compared to only 49.1% of those that were performed laparoscopically [19]. Specifically for robotic liver surgery, it is vital to have an adequately trained surgeon at the patient’s bedside as a ‘wingman’ who helps managing the installation and the exchange of the robotic arms along with suctioning and optimal retraction to help providing the best exposure to the operating surgeon, and also to perform safe stapling of major vessels during parenchymal transection when needed [25,26,27].
Readmissions within 30 days of hospital discharge were seen in eight (10%) patients. Two patients were readmitted for bile leak which was managed by percutaneous drain placement. One patient presented to the emergency department for jaundice without any other systemic symptoms. CT scan did not show any evidence of biliary leak or obstruction. He was readmitted to the surgical floor for fluid resuscitation and the jaundice gradually resolved within 48 h. No patients required reoperation in this series.
Conclusion
Our serious support that robotic hepatectomy is safe and feasible, with favorable short-term outcomes for both benign and malignant tumors and with a low ‘open’ conversion rate. Robotic technology extends the application of minimally invasive techniques in the field of hepatobiliary surgery.
References
Reich H, McGlynn F, DeCaprio J, Budin R (1991) Laparoscopic excision of benign liver lesions. Obstet Gynecol 78:956–958
Pilgrim CH, To H, Usatoff V, Evans PM (2009) Laparoscopic hepatectomy is a safe procedure for cancer patients. HPB (Oxf) 11:247–251
Simillis C, Constantinides VA, Tekkis PP et al (2007) Laparoscopic versus open hepatic resections for benign and malignant neoplasms—a meta-analysis. Surgery 141(2):203–211
Morino M, Morra I, Rosso E, Miglietta C et al (2003) Laparoscopic vs open hepatic resection: a comparative study. Surg Endosc 17:1914–1918
Polignano FM, Quyn AJ, de Figueiredo RS, Henderson NA, Kulli C, Tait IS (2008) Laparoscopic versus open liver segmentectomy: prospective, case-matched, intention-to-treat analysis of clinical outcomes and cost effectiveness. Surg Endosc 22(12):2564–2570
Dagher I, Di Giuro G, Dubrez J, Lainas P, Smadja C, Franco D (2009) Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg 198:173–177
Khan S, Beard RE, Kingham PT et al (2018) Long-Term oncologic outcomes following robotic liver resections for primary hepatobiliary malignancies: a multicenter study. Ann Surg Oncol 25(9):2652–2660
Kitisin K, Packiam V, Bartlett DL, Tsung A (2011) A current update on the evolution of robotic liver surgery. Minerva Chir 66(4):281–293
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2, 804 patients. Ann Surg 250(5):831–841
Milone L, Daskalaki D, Fernandes E, Damoli I, Giulianotti PC (2013) State of the art in robotic hepatobiliary surgery. World J Surg World J Surg 37(12):2747–2755
Giulianotti PC, Coratti A, Angelini M et al (2003) Robotics in general surgery: personal experience in a large community hospital. Arch Surg 138(7):777–784
Lanfranco AR, Castellanos AE, Desai JP, Meyers WC (2004) Robotic surgery: a current perspective. Ann Surg 239(1):14–21
Goja S, Singh MK, Soin AS (2017) Robotics in hepatobiliary surgery-initial experience, first reported case series from India. Int J Surg Case Rep 33:16–20
Reddy SK, Tsung A, Geller DA (2011) Laparoscopic liver resection. World J Surg 35(7):1478–1486
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 246:463–468
Sotiropoulos GC, Prodromidou A, Machairas N (2017) Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma: the European experience. J Buon 22(5):1160–1171
Choi GH, Chong JU, Han DH, Choi JS, Lee WJ (2017) Robotic hepatectomy: the Korean experience and perspective. Hepatobil Surg Nutr 6(4):230–238
Idrees K, Bartlett DL (2010) Robotic liver surgery. Surg Clin North Am 90:761–774
Tsung A, Geller DA, Sukato DC et al (2014) Robotic vs laparoscopic hepatectomy: a matched comparison. Ann Surg 259(3):549–555
Ho CM, Wakabayashi G, Nitta H, Ito N, Hasegawa Y, Takahara T (2013) Systematic review of robotic liver resection. Surg Endosc 27(3):732–739
Boggi U, Moretto C, Vistoli F, D’Imporzano S, Mosca F (2009) Robotic suture of a large caval injury caused by endo-GIA stapler malfunction during laparoscopic wedge resection of liver segments VII and VIII en-bloc with the right hepatic vein. Minim Invasive Ther Allied Technol 18:306–310
Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J (2010) Robotic versus laparoscopic resection of liver tumours. HPB (Oxf) 12(8):58
Ji WB, Wang HG, Zhao ZM, Duan WD, Lu F, Dong JH (2011) Robotic-assisted laparoscopic anatomic hepatectomy in China: initial experience. Ann Surg 253(2):342–348
Choi SB, Park JS, Kim JK et al (2008) Early experiences of robotic-assisted laparoscopic liver resection. Yonsei Med J 49(4):632–638
Sgarbura O, Vasilescu C (2010) The decisive role of the patient-side surgeon in robotic surgery. Surg Endosc 24(12):3149–3155
Giulianotti PC, Coratti A, Sbrana F et al (2011) Robotic liver surgery: results for 70 resections. Surgery 149(1):29–39
Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D (2009) The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg 250(5):772–782
Funding
This paper was not funded in part or in whole by any organization.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Sucandy, Author Schlosser, Author Bourdeau, Author Attili declare that they have no conflict of interest. Author Ross and Author Rosemurgy declare that they have educational and consulting relationships with Intuitive Surgical Corp.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Written informed consent was obtained from the patient for publication of this study. A copy of the written consent is available for review upon request.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sucandy, I., Schlosser, S., Bourdeau, T. et al. Robotic hepatectomy for benign and malignant liver tumors. J Robotic Surg 14, 75–80 (2020). https://doi.org/10.1007/s11701-019-00935-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-019-00935-0