Abstract
Oleanolic acid (OA) is a naturally occurring pentacyclic triterpenoid and possesses diverse pharmacological activities, including anti-cancer effects that have been confirmed in multiple types of human cancers. However, the potential effect of natural OA on human prostate cancer is still unclear. The present study aimed to explore whether and how OA exerted anti-cancer effects in prostate cancer. Our data showed that OA inhibited cell viability and proliferation, and promoted cell apoptosis and G0/G1 phase cell cycle arrest in prostate cancer PC-3, DU145, and LNCaP cells, in a dose-dependent manner. In addition, OA was found to regulate the expression levels of apoptosis-related and cell cycle-related proteins, as well as the activity of PI3K/Akt pathway, in a dose-dependent manner. Mechanistically, our data revealed that OA exerted anti-cancer effects in vitro in PC-3 and DU145 cells by repressing the PI3K/Akt pathway. In agreement, OA also suppressed the tumor growth of PC-3 cells in vivo via inhibition of the PI3K/Akt pathway. In conclusion, our findings demonstrate the anti-cancer properties of OA in prostate cancer cells, both in vitro and in vivo, and provide the experimental evidence for the use of OA as an adjuvant agent for prostate cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oleanolic acid (OA; 3β-hydroxyolean-12-en-28-oic acid) is a biologically active pentacyclic triterpenoid that has been isolated from more than 1600 plant species ranging from edible plants to medicinal herbs [1, 2]. OA displays various beneficial pharmacological properties, such as anti-oxidant, anti-inflammatory, anti-diabetic, anti-viral, hepato-protective, anti-microbial, and anti-cancer effects [3–5]. The anti-cancer effect of OA has been verified in a wide variety of human cancers, such as breast [6], hepatocellular [7–9], lung [10, 11], colon [12, 13], pancreatic [14, 15], and gallbladder cancers [16], as well as hematological malignancies [17] and malignant glioma [18, 19]. Increasing evidence has shown that the anti-cancer properties of OA range from inhibition of cell survival and proliferation to induction of apoptosis and cell cycle arrest as well as suppression of migration and invasion.
Synthetic derivatives of OA have been found to exhibit anti-cancer properties in human prostate cancer (PCa) [20–23], but the potential effect of natural OA on PCa has not been clearly clarified. Therefore, the present study aimed to investigate whether and how OA exerted its anti-neoplastic activity against PCa. The results revealed that OA could inhibit cell viability and proliferation, and induce cell apoptosis and G0/G1 phase cell cycle arrest in human PCa PC-3, DU145, and LNCaP cells, in a dose-dependent manner in vitro. In addition, OA dose-dependently regulated the expression levels of apoptosis-related and cell cycle-related proteins as well as the activity of the phosphoinositide-3-kinase (PI3K)/Akt pathway. Our data further demonstrated that it was through the inactivation of PI3K/Akt pathway that OA exhibited its in vitro anti-cancer roles in PC-3 and DU145 cells. Moreover, OA repressed the tumorigenic capacity of PC-3 cells in nude mice through the PI3K/Akt pathway. Herein, we show the anti-cancer ability of natural OA on PCa cells, both in vitro and in vivo, and provide experimental evidence in support of OA as a potential adjuvant drug for PCa patients.
Materials and methods
Materials
OA was purchased from Sigma–Aldrich (Saint Louis, MO, USA), dissolved in dimethyl sulfoxide (DMSO; Sigma–Aldrich) at a 60 mM stock concentration and then stored at −20 °C. For final working concentrations, OA stock solution was further diluted with culture medium.
Cell culture
PC-3 (TCHu158), DU145 (TCHu222), and LNCaP (TCHu173) were directly purchased from Shanghai Cell Bank, Chinese Academy of Sciences (Shanghai, People’s Republic of China). The three cell lines were maintained in RPMI 1640 medium (Gibco, Thermo Fisher Scientific Inc., Waltham, MA, USA) supplemented with 10 % fetal bovine serum (Gibco) in a 5 % CO2 humidified incubator at 37 °C.
Cell transfection
The over-expression plasmid for Akt and the empty vector plasmid as negative control (NC) were constructed by Shanghai GeneChem Co., Ltd. (Shanghai, People’s Republic of China). Cells were seeded in 6-well plates overnight. For transfection, appropriate amount of Akt or NC plasmids and Lipofectamine 2000 transfection reagent (Invitrogen, Thermo Fisher Scientific Inc., Waltham, MA, USA) were separately diluted in Opti-MEM Reduced-Serum Medium (Gibco) for 5 min, and then co-incubated for 20 min at room temperature before being added into each well. Stably transfected cells were selected by G418 (EMD Chemicals, Inc., San Diego, CA, USA).
Cell viability assay
Cell viability assay was assessed with the Cell Counting Kit-8 (CCK-8; Dojindo, Kumamoto, Japan). Cells (1 × 104 per well) were seeded in 96-well plates overnight and treated with the indicated concentrations of OA for 24, 48, and 72 h. At each time point, 10 μl of CCK-8 solution was added into each well and incubated at 37 °C for 2 h. The absorbance at 450 nm was measured on a microplate reader (Tecan, Mannedorf, Switzerland).
Colony formation assay
Cell proliferation activity was assessed by colony formation assay. Cells were pre-treated with the indicated concentrations of OA for 48 h. Then, cells were collected and seeded into 6-well plates (1 × 103 cells per well) for 14 days. Cells were fixed with methanol and stained with 0.1 % crystal violet (Sigma–Aldrich). Colonies (˃50 cells) were counted.
Flow cytometry analysis
Cell apoptosis was detected using the Annexin V-FITC Apoptosis Detection Kit (KeyGEN Biotech, Nanjing, China) following the manufacturer’s protocols. Cells (5 × 105 per well) were seeded into 6-well plates overnight and then treated with the indicated concentrations of OA for 48 h. Cells were collected, suspended in Annexin V-FITC binding buffer, incubated with Annexin V-FITC and propidium iodide (PI) and analyzed on a FACSVerse™ flow cytometer (BD Biosciences, San Jose, CA, USA).
The cell cycle distribution was analyzed with the Cell Cycle Detection Kit (KeyGEN Biotech) following the manufacturer’s instructions. Cells (5 × 105 per well) were seeded into 6-well plates overnight and then treated with the indicated concentrations of OA for 48 h. Cells were harvested, fixed with 70 % ethanol, incubated with RNase A, stained with PI, and then detected on a FACSVerse flow cytometer.
Mitochondrial membrane potential (MMP) assay
MMP was assessed using a Mitochondrial Membrane Potential Assay Kit with JC-1 (Beyotime Biotechnology, Jiangsu, China) as previously described [24]. Briefly, after treatment with the indicated concentrations of OA for 48 h, 5 × 104 cells were incubated with JC-1 staining working solution at 37 °C for 20 min in the dark and then washed twice with JC-1 staining buffer solution. The fluorescence intensities of mitochondrial JC-1 aggregates (red) and monomers (green) were detected using an Enspire fluorescence microplate reader (PerkinElmer, Waltham, MA, USA). The levels of MMP were calculated as the red/green fluorescence ratio.
Detection of reactive oxygen species (ROS) generation
Intracellular ROS was detected with a Reactive Oxygen Species Assay Kit (Beyotime) as previously reported [24]. Following treatment with the indicated concentrations of OA for 48 h, 5 × 104 cells were incubated with 2′,7′-dichlorofluorescein diacetate (DCFH-DA) at 37 °C for 20 min in the dark and then washed thrice with serum-free culture medium. The fluorescence intensities were measured using an Enspire fluorescence microplate reader (PerkinElmer).
Measurement of lysosomal membrane permeabilization (LMP)
Quantification of LMP was performed with LysoTracker Green (Invitrogen) and Hoechst 33342 (Invitrogen) as previously described [25]. After treatment with the indicated concentrations of OA for 48 h, 5 × 104 cells were incubated in the dark with LysoTracker Green working solution at 37 °C for 1 h and subsequently with Hoechst 33342 at 37 °C for 15 min, and washed twice with serum-free culture medium. Then, fluorescence intensities were measured on an Enspire fluorescence microplate reader (PerkinElmer). Values were calculated as fluorescence (LysoTracker Green)/fluorescence (Hoechst).
Caspase activity assay
Caspase activity was detected using Caspase 3/8/9 Activity Assay Kit (Beyotime) following the manufacturer’s instructions. After treatment with the indicated concentrations of OA for 48 h, cells were collected, lysed, and centrifuged at 12,000 × g for 20 min at 4 °C. Protein concentrations in the supernatants were measured using Bradford Protein Assay Kit (Beyotime). Equal amounts of protein from each cell lysate were incubated with reaction buffer and the respective caspase substrate, Ac-DEVD-pNA for caspase-3, Ac-IETD-pNA for caspase-8, or Ac-LEHD-pNA for caspase-9, for 2 h at 37 °C. Absorbance was measured at 405 nm on a microplate reader (Tecan).
Quantitative reverse transcription polymerase chain reaction
Quantitative reverse transcription polymerase chain reaction (qRT-PCR) was conducted as previously described [26]. Briefly, total RNA was extracted from tumor tissues with RNAiso Plus (TaKaRa, Shiga, Japan) and reversely transcribed using First Strand cDNA Synthesis Kit (TaKaRa). Quantitative PCR was then performed using the SYBR Fast qPCR Mix (TaKaRa). The primer sequences listed as follows were obtained from PrimerBank (The Center for Computational and Integrative Biology, Harvard Medical School, Boston, MA, USA) [27]: Akt, 5′-GTCATCGAACGCACCTTCCAT-3′ (forward) and 5′-AGCTTCAGGTACTCAAACTCGT-3′ (reverse) (PrimerBank I.D. No. 62241012c3); GAPDH, 5′-GGAGCGAGATCCCTCCAAAAT-3′ (forward) and 5′-GGCTGTTGTCATACTTCTCATGG-3′ (reverse) (PrimerBank I.D. No. 378404907c1). GAPDH was used as the endogenous control.
Western blotting analysis
Cells were treated with the indicated concentrations of OA for 48 h. Total proteins were extracted from cells or tissues using RIPA Lysis Buffer (Beyotime). The cytosolic and mitochondrial proteins were isolated with the Cell Mitochondrial Isolation Kit (Beyotime) following the manufacturer′s protocols. Proteins were separated by SDS-PAGE and transferred onto PVDF membranes (Merck Millipore, Billerica, MA, USA). After blocking with 5 % nonfat milk, the membranes were incubated with primary antibodies at 4 °C overnight, followed by incubation with secondary antibodies (Proteintech, Chicago, IL, USA). The immunoblots were visualized by BeyoECL Plus (Beyotime) on a BioSpectrum Imaging System (UVP, Upland, CA, USA). The primary antibodies were against cleaved PARP (Beyotime), Bax (Proteintech), Bcl-2 (Proteintech), Bcl-xL (Proteintech), cyclin-dependent kinase 4 (CDK4; Santa Cruz, Dallas, TX, USA), cyclin D1 (Santa Cruz), cytochrome c (Proteintech), COX IV (Proteintech), PI3K [Cell Signaling Technology (CST), Beverly, MA, USA], Akt (CST), phosphorylated Akt at serine 473 (p-AktSer473; CST), phosphorylated p-Bad at serine 136 (p-BadSer136; ABCAM, Cambridge, MA, USA), phosphorylated glycogen synthase kinase 3 beta at serine 9 (p-GSK-3βSer9; CST), forkhead box O1 (FOXO1; Signalway Antibody, College Park, MD, USA), phosphorylated FOXO1 at serine 256 (p-FOXO1Ser256; Signalway Antibody), and GAPDH (Proteintech). COX IV and GAPDH were used as the loading controls.
In vivo tumorigenesis
BALB/c nude male mice (4-week old) were purchased from Beijing HFK Bioscience Co. Ltd (Beijing, China), housed under specific pathogen-free conditions and maintained in a temperature- and humidity-controlled environment with a 12-h light/dark cycle. This study was carried out in strict accordance with the recommendations in the national guideline for the care and use of laboratory animals. All efforts were taken to minimize mice suffering.
The nude mice were randomized into four groups (five mice per group): NC, NC + OA, Akt, and Akt + OA. PC-3 cells (3 × 106 in 0.2 ml phosphate-buffered saline) stably transfected with or without Akt were subcutaneously inoculated into the right front axilla of each mouse in the corresponding groups. Mice were intraperitoneally administered with OA (150 mg/kg/day) in the corresponding groups [7]. On day 21, the mice were sacrificed, and isolated tumors were weighed. Then, the tumors were analyzed by qRT-PCR, western blotting, and immunohistochemistry (IHC).
IHC analysis
Following fixation in 4 % paraformaldehyde, the tumors were embedded in paraffin and then sectioned. After deparaffinization in xylene and rehydration in decreasing concentrations of ethanol, tissue sections (4 μm) were immersed in sodium citrate buffer for antigen retrieval and subsequently in 3 % hydrogen peroxide solution for quenching endogenous peroxidase activity. After blocking with 5 % bovine serum albumin solution, the sections were incubated with primary antibodies against Akt (CST), p-AktSer473 (CST), Ki-67 (Proteintech), p-BadSer136 (ABCAM), Bcl-2 (Proteintech), p-GSK-3βSer9 (CST) or cyclin D1 (Santa Cruz), respectively, at 4 °C overnight, followed by incubation with peroxidase-conjugated secondary antibodies (Proteintech). The sections were incubated with diaminobenzidine solution (Beyotime), counterstained with hematoxylin solution (Beyotime) and then visualized with an inverted microscope (Olympus, Tokyo, Japan).
Statistical analysis
All experiments were repeated at least three times. Data were expressed as the mean ± standard deviation (SD). Statistical analysis was performed with GraphPad Prism software (Version 6.01; GraphPad Software, Inc., San Diego, CA, USA). Statistical differences were considered significant at p < 0.05.
Results
OA inhibited cell viability and proliferation in human PCa cells
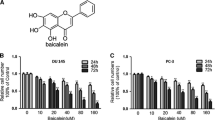
To begin, the effects of OA on cell viability and proliferation were examined in human PCa cell lines. The CCK-8 assay showed that OA treatment resulted in a remarkable decrease in cell viabilities of PC-3, DU145, and LNCaP cells in a dose- and time-dependent manner (Fig. 1a). In addition, colony formation assay revealed that OA dose-dependently reduced colony-forming rates of PC-3, DU145, and LNCaP cells (Fig. 1b).
OA inhibited cell viability and proliferation of PCa cells. a PC-3, DU145, and LNCaP cells were treated with the indicated concentrations of OA for 24, 48, and 72 h, respectively. Cell viability was analyzed by cell counting kit (CCK-8) assay. *p < 0.05 compared with the respective time point of the control group (concentration of OA = 0 μM). # p < 0.05 compared with the respective concentration of the control group (culture time = 24 h). b For colony formation assay, PC-3, DU145, and LNCaP cells, pre-treated with the indicated concentrations of OA for 48 h, were seeded in 6-well plates without OA for 14 days. *p < 0.05 compared with the control group (concentration of OA = 0 μM). DMSO (v/v, 0.1 %) was used as the vehicle control. All data were presented as mean ± SD from three independent experiments
OA induced apoptosis, loss of MMP, generation of intracellular ROS and increase of LMP in human PCa cells
Next, the apoptotic effects of OA on PC-3, DU145, and LNCaP cells were investigated by flow cytometry. As shown in Fig. 2a, OA treatment noticeably reduced the number of surviving cells and increased the number of both early and late apoptotic cells in a dose-dependent manner. Mitochondria play a critical role in cell apoptosis [28], and the loss of MMP can lead to the release of apoptotic-inducing factor and caspase activators, such as cytochrome c [29]. To determine the changes in MMP after exposure to OA, MMP in PCa cells was assessed using a Mitochondrial Membrane Potential Assay Kit with JC-1 (Beyotime). The result showed that MMP was remarkably decreased with the increase of OA concentration in PC3, DU145, and LNCaP cells (Fig. 2b).
OA induced cell apoptosis, loss of MMP, generation of intracellular ROS, and increase of LMP in PCa cells. PC-3, DU145, and LNCaP cells were treated with the indicated concentrations of OA for 48 h. a Cell apoptosis was measured by flow cytometry. b The relative levels of MMP were assessed using a Mitochondrial Membrane Potential Assay Kit with JC-1. c The relative levels of intracellular ROS were detected with a Reactive Oxygen Species Assay Kit. d the relative levels of LMP were detected with LysoTracker Green. DMSO (v/v, 0.1 %) was used as the vehicle control. *p < 0.05 versus the control group (concentration of OA = 0 μM). All data were representative of three independent experiments
Mitochondria are important sources of intracellular ROS production, which can contribute to the loss of MMP and an increase of LMP in a range of pathologies [30, 31]. Previous studies showed that OA could induce the generation of intracellular ROS and an increase of LMP [6, 9, 14]. In the present study, intracellular ROS was detected with a Reactive Oxygen Species Assay Kit (Beyotime). The results showed that the levels of ROS were dose-dependently increased with treatment of OA in the three cell lines (Fig. 2c). In addition, LMP was measured using LysoTracker Green (Invitrogen). As shown in Fig. 2d, high concentrations of OA induced a significant increase of LMP, while lower concentrations of OA seemed to have no effect on the levels of LMP.
OA induced G0/G1 phase cell cycle arrest in human PCa cells
The effects of OA on cell cycle progression were assessed by flow cytometry in PC-3, DU145, and LNCaP cells. Consistently in the three cell lines, treatment of OA dose-dependently suppressed cell cycle progression with an increased percentage of cells in the G0/G1 phase and a decreased percentage of cells in the S phase (Fig. 3).
OA induced G0/G1 phase cell cycle arrest in PCa cells. PC-3, DU145, and LNCaP cells were treated with the indicated concentrations of OA for 48 h and then cell cycle distribution was detected by flow cytometry. DMSO (v/v, 0.1 %) was used as the vehicle control. *p < 0.05 versus the control group (concentration of OA = 0 μM). All data were representative of three independent experiments
OA regulated the expression levels of apoptosis-related and cell cycle-related proteins as well as the activity of the PI3K/Akt pathway in PCa cells
To investigate the underlying molecular mechanisms of OA on cell apoptosis and G0/G1 phase arrest in PCa cells, caspase activity assay and western blotting analysis were applied to assess the expression levels of apoptosis-related and cell cycle-related proteins in PC-3, DU145, and LNCaP cells treated with OA for 48 h. Our data revealed that OA upregulated the activities of caspase-8, caspase-9, and caspase-3, increased the expression levels of cleaved PARP and Bax, and decreased the expression levels of Bcl-2, Bcl-xL, CDK4, and cyclin D1, in a generally dose-dependent manner (Fig. 4a and b). In addition, OA promoted the release of cytochrome c from the mitochondria into the cytoplasm (Fig. 4c).
OA regulated the expression levels of apoptosis-related and cell cycle-related proteins in PCa cells. PC-3, DU145, and LNCaP cells were treated with the indicated concentrations of OA for 48 h. a Caspase activities were detected in PC-3, DU145, and LNCaP cells. *p < 0.05 versus the control group (concentration of OA = 0 μM). All data represented three independent experiments. b Expression levels of cleaved PARP, Bax, Bcl-2, Bcl-xL, CDK4, and cyclin D1 were detected by western blotting. c The levels of cytochrome c in mitochondria and cytoplasm were detected by western blotting. DMSO (v/v, 0.1 %) was used as the vehicle control
PI3K is known to induce the phosphorylation and activation of Akt, and a growing body of evidence demonstrates that the PI3K/Akt pathway is one of the most frequently activated signaling pathways in human cancers, including PCa [32, 33]. Hyperactivity of the PI3K/Akt pathway promotes cell survival and proliferation through phosphorylation of downstream targets, such as Bad, GSK-3β, and FOXO1 [34–37]. Therefore, we investigated whether OA affected the PI3K/Akt pathway and its downstream targets in PC-3, DU145, and LNCaP cells. Western blotting showed that OA obviously decreased the expression levels of PI3K, p-AktSer473, p-BadSer136, and p-GSK-3βSer9 in a dose-dependent manner, while no significant differences in total Akt, total FOXO1, or p-FOXO1Ser256 were observed (Fig. 5).
OA repressed the PI3K/Akt pathway in PCa cells. PC-3, DU145, and LNCaP cells were treated with the indicated concentrations of OA for 48 h. The expression levels of PI3K, Akt, p-AktSer473, p-BadSer136, p-GSK-3βSer9, FOXO1, and p-FOXO1Ser256 were detected by western blotting. DMSO (v/v, 0.1 %) was used as the vehicle control
Akt over-expression reversed the effects of OA on cell viability, proliferation, cell apoptosis, and G0/G1 phase cell cycle arrest in PCa cells
To investigate whether OA inhibited cell viability and proliferation of PCa cells through the PI3K/Akt pathway, we over-expressed Akt in PC-3 and DU145 cells. Western blotting demonstrated that expression and activity of Akt were both elevated in PC-3 and DU145 cells (Fig. 6a). CCK-8 and colony formation assays showed that over-expression of Akt obviously reversed the inhibitory effects of OA on cell viability and proliferation of PC-3 and DU145 cells in the Akt + OA group compared with the NC + OA group (Fig. 6b and c). Furthermore, flow cytometry revealed that Akt over-expression relieved the effects of OA on cell apoptosis and G0/G1 phase arrest in the two cell lines in the Akt + OA group versus the NC + OA group (Fig. 7a and b).
Akt over-expression reversed the inhibitory effects of OA on cell viability and proliferation in PCa cells. a Over-expression and activity of Akt in PC-3 and DU145 cells were verified by western blotting. Mock, untransfected control. b PC-3 and DU145 cells transfected with or without Akt were treated with or without OA (30 μM) for 24, 48, and 72 h. Cell viability was analyzed by CCK-8 assay. *p < 0.05 versus the respective time point of the NC + OA group. c For colony formation assay, PC-3 and DU145 cells transfected with or without Akt were pre-treated with or without OA (30 μM) for 48 h, and then seeded in 6-well plates without OA for 14 days. All data were presented as mean ± SD from three independent experiments. *p < 0.05 versus the NC + OA group
Akt over-expression reversed the effects of OA on apoptosis and G0/G1 phase arrest in PCa cells. PC-3 and DU145 cells transfected with or without Akt were treated with or without OA for 48 h. a, b Cell apoptosis and distribution of cell cycle were analyzed by flow cytometry, respectively. *p < 0.05 versus the NC + OA group. Data were expressed as mean ± SD from three independent experiments
Akt over-expression reversed the effects of OA on apoptosis-related and cell cycle-related proteins in PCa cells
Caspase activity assay and western blotting analysis indicated that Akt over-expression decreased the activities of caspase-9 and caspase-3, and elevated the expression levels of p-BadSer136, Bcl-2, p-GSK-3βSer9, and cyclin D1 in PC-3 and DU145 cells in the Akt + OA group versus the NC + OA group (Fig. 8a and b).
Akt over-expression reversed the effects of OA on apoptosis-related and cell cycle-related proteins in PCa cells. PC-3 and DU145 cells transfected with or without Akt were treated with or without OA for 48 h. a Caspase activities were detected in PC-3 and DU145 cells using a Caspase Activity Assay Kit. *p < 0.05 compared with the NC + OA group. Data were presented as mean ± SD (n = 3). b Expression levels of p-AktSer473, p-BadSer136, Bcl-2, p-GSK-3βSer9, and cyclin D1 were detected by western blotting
OA inhibited tumorigenesis of PC-3 cells in vivo by repressing the PI3K/Akt pathway
To further explore whether OA affected tumorigenesis of PCa cells in vivo, we subcutaneously inoculated PC-3 cells stably transfected with or without Akt into nude mice. Then, OA (150 mg/kg/day) was intraperitoneally administered in the NC + OA and the Akt + OA groups. Consistent with the in vitro experiments, OA remarkably repressed the tumor growth of PC-3 cells in nude mice in the NC + OA group versus the NC group, while the inhibitory effect of OA was reversed by over-expression of Akt in the Akt + OA group versus the NC + OA group (Fig. 9a and b). Meanwhile, qRT-PCR and western blotting confirmed that Akt was upregulated in the Akt group (Fig. 9c and d). Moreover, IHC analysis revealed that OA downregulated expression levels of p-AktSer473, Ki-67, p-BadSer136, Bcl-2, p-GSK-3βSer9, and cyclin D1 in tumor tissues of the NC + OA group versus the NC group, which was also reversed by over-expression of Akt in the Akt + OA group versus the NC + OA group (Fig. 10).
OA inhibited tumorigenesis of PC-3 cells in vivo through repressing PI3K/Akt pathway. PC-3 transfected with or without Akt were subcutaneously injected into the right front axilla of BALB/c nude mice and grow for 21 days. a Isolated tumors from nude mice were photographed on day 21. b Isolated tumors from nude mice were weighed. *p < 0.05 versus the NC + OA group. c The mRNA levels of Akt in tumor tissues were assessed by qRT-PCR. *p < 0.05 versus the NC + OA group. All data were presented as mean ± SD (n = 3). d The expression of Akt protein in tumor tissues was assessed by western blotting
OA regulated the expression levels of p-AktSer473, Ki-67, p-BadSer136, Bcl-2, p-GSK-3βSer9, and cyclin D1 in vivo. The expression levels of Akt, p-AktSer473, Ki-67, p-BadSer136, Bcl-2, p-GSK-3βSer9, and cyclin D1 in tumor tissues from nude mice were assessed by IHC analysis. Representative data were shown. Original magnification, ×200
Discussion
Previous studies have demonstrated that OA can suppress cell survival and proliferation in various human cancers. In the present study, CCK-8 and colony formation assays showed that OA could dose-dependently repress cell viability and proliferation in human PCa PC-3, DU145, and LNCaP cells. Consistent with a previous report in gallbladder cancer [16], OA also induced cell apoptosis and G0/G1 phase arrest in PC-3, DU145, and LNCaP cells.
Apoptosis is a genetically controlled cell-death process that maintains tissue homeostasis [38]. Deregulated apoptosis can result in various pathological conditions including cancers [39]. However, like a double-edged sword, apoptosis may also serve as a helpful target of cancer treatment; In fact, anti-cancer agents or other therapeutic strategies can eliminate cancer cells by restoring defective apoptosis [40, 41]. Activation of caspases, a family of cysteinyl aspartate-specific proteinases, triggers apoptosis by cleaving cellular proteins critical for cell survival, such as PARP [42–44]. The members of the Bcl-2 family play a vital role in regulation of apoptosis [45, 46]. In the current study, we found that treatment of OA induced mitochondrial depolarization and then release of cytochrome c from the mitochondria to the cytoplasm in PC-3, DU145, and LNCaP cells. Moreover, western blotting revealed that OA reduced the activities of caspase-8, caspase-9, and caspase-3, increased the expression levels of cleaved PARP and Bax, and downregulated the expression levels of Bcl-2 and Bcl-xL. These data suggested that OA induced cell death in PCa cells through the mitochondrial apoptotic pathway. In addition, our data revealed that OA could induce the generation of intracellular ROS and that a high-dose of OA could increase LMP, which is consistent with a previous report [14].
Eukaryotic cell proliferation is controlled by cell cycle checkpoints, which ensure the proper timing of cellular events. Uncontrolled cell proliferation can contribute to genomic instability and tumorigenesis [47]. Targeting the cell cycle is regarded as an effective strategy for cancer therapy [48–50]. Transition of G1 into S phase is one of the cell cycle checkpoints, and it is mainly driven by the CDK4/6-cyclin D complexes, which are actively being explored as therapeutic targets for cancer treatment [51–53]. Our data indicated that OA downregulated the expression levels of CDK4 and cyclin D1 in PC-3, DU145, and LNCaP cells.
The serine/threonine kinase Akt, also known as protein kinase B, comprises three highly homologous isoforms (Akt1/PKBα, Akt2/PKBβ, and Akt3/PKBγ) and plays a critical role in a wide range of key cellular processes, such as cell survival, proliferation, apoptosis, cell cycle, metabolism, migration, and invasion [54, 55]. Increasing evidence has indicated that aberrant hyper-activation of the PI3K/Akt pathway is one of the most common molecular alterations in human malignancies, including PCa, while re-programming the altered the PI3K/Akt pathway represents a powerful strategy for rational cancer therapy [56, 57]. The growth factor receptor-associated PI3K activates Akt by promoting its phosphorylation at threonine 308 and serine 473, which triggers a signaling cascade that results in the inhibition of apoptosis and cell cycle arrest. Specifically, Akt affects the phosphorylation status of certain pro-apoptotic molecules and thus inhibits apoptosis [58, 59]. For example, Akt phosphorylates the pro-apoptotic factor Bad at Ser136, thereby promoting the interaction of Bad with 14-3-3 proteins and inhibiting the association of Bad with Bcl-2 and Bcl-xL, which inhibits cell apoptosis [59]. In parallel, human caspase-9 is also reported to be phosphorylated at serine 196 by Akt, which inhibits the caspase cascade and promotes cell survival [60]. In addition, Akt contributes to cell proliferation via influencing cell cycle progression. For example, Akt phosphorylates GSK-3β at serine 9, resulting in its inactivation and the stabilization of cyclin D1, a key player in the transition of the G1 to S phase [61]. Akt-mediated inactivation of GSK-3β not only regulate cyclin D1 gene transcription through decreased phosphorylation of β-catenin but it can also induce cyclin D1 stability by preventing GSK-3β from promoting cyclin D1 proteolysis [62]. In addition, Akt can phosphorylate and directly inhibit the function of FOXO1, a member of the forkhead family that regulates diverse cellular processes, such as apoptosis and cell cycle arrest. [37, 63–67] In the present study, we evaluated the effects of OA on the PI3K/Akt pathway in PCa cells. Our data indicated that OA treatment did not significantly change the expression levels of total Akt, total FOXO1, or p-FOXO1Ser256, but noticeably reduced the expression levels of PI3K, p-AktSer473, p-BadSer136 and p-GSK-3βSer9 in PC-3, DU145, and LNCaP cells.
Based on the above findings, we posed the hypothesis that OA might repress cell survival and proliferation in PCa cells through the PI3K/Akt pathway. To further verify the hypothesis, we over-expressed Akt in PC-3 and DU145 cells. Our results showed that over-expression of Akt reversed the effects of OA on cell viability, colony-forming capacity, apoptosis, and G0/G1 phase arrest in the two cell lines in the Akt + OA group versus the NC + OA group. Furthermore, our data showed that Akt over-expression restored the protease activity of caspase-9 and the expression levels of p-BadSer136, p-GSK-3βSer9, and cyclin D1 in PC-3 and DU145 in the Akt + OA group versus the NC + OA group. In agreement with a previous report indicating that Akt could up-regulate Bcl-2 expression via cAMP-response element-binding protein [68], our results showed that Akt over-expression also restored Bcl-2 expression. However, it is necessary to further confirm whether Akt can up-regulate Bcl-2 in PCa.
Importantly, the anti-cancer effects of OA in vivo were assessed. Our results indicated that OA obviously inhibited the tumor growth of PC-3 cells in nude mice, compared with the control group, and that this effect was reversed by over-expression of Akt, which was in accordance with our in vitro study. Additionally, IHC analysis suggested that OA downregulated Ki-67, p-BadSer136, Bcl-2, p-GSK-3βSer9, and cyclin D1 through repressing Akt activity.
Collectively, our present study reveals that OA can inhibit cell survival and proliferation of PCa cells, both in vitro and in vivo, through the induction of apoptosis and G0/G1 phase cell cycle arrest, which is realized by regulating the PI3K/Akt pathway. In effect, our study indicates that OA can serve as a potential adjuvant agent for the treatment of PCa.
References
Liu J. Pharmacology of oleanolic acid and ursolic acid. J Ethnopharmacol. 1995;49:57–68.
Pollier J, Goossens A. Oleanolic acid. Phytochemistry. 2012;77:10–5.
Castellano JM, Guinda A, Delgado T, Rada M, Cayuela JA. Biochemical basis of the antidiabetic activity of oleanolic acid and related pentacyclic triterpenes. Diabetes. 2013;62:1791–9.
Sultana N, Ata A. Oleanolic acid and related derivatives as medicinally important compounds. J Enzyme Inhib Med Chem. 2008;23:739–56.
Dzubak P, Hajduch M, Vydra D, Hustova A, Kvasnica M, Biedermann D, et al. Pharmacological activities of natural triterpenoids and their therapeutic implications. Nat Prod Rep. 2006;23:394–411.
Allouche Y, Warleta F, Campos M, Sanchez-Quesada C, Uceda M, Beltran G, et al. Antioxidant, antiproliferative, and pro-apoptotic capacities of pentacyclic triterpenes found in the skin of olives on MCF-7 human breast cancer cells and their effects on DNA damage. J Agric Food Chem. 2011;59:121–30.
Wang X, Bai H, Zhang X, Liu J, Cao P, Liao N, et al. Inhibitory effect of oleanolic acid on hepatocellular carcinoma via ERK-p53-mediated cell cycle arrest and mitochondrial-dependent apoptosis. Carcinogenesis. 2013;34:1323–30.
Shyu MH, Kao TC, Yen GC. Oleanolic acid and ursolic acid induce apoptosis in HuH7 human hepatocellular carcinoma cells through a mitochondrial-dependent pathway and downregulation of XIAP. J Agric Food Chem. 2010;58:6110–8.
Liese J, Abhari BA, Fulda S. Smac mimetic and oleanolic acid synergize to induce cell death in human hepatocellular carcinoma cells. Cancer Lett. 2015;365:47–56.
Lucio KA, Rocha Gda G, Moncao-Ribeiro LC, Fernandes J, Takiya CM, Gattass CR. Oleanolic acid initiates apoptosis in non-small cell lung cancer cell lines and reduces metastasis of a B16F10 melanoma model in vivo. PLoS ONE. 2011;6:e28596.
Zhao X, Liu M, Li D. Oleanolic acid suppresses the proliferation of lung carcinoma cells by miR-122/Cyclin G1/MEF2D axis. Mol Cell Biochem. 2015;400:1–7.
Furtado RA, Rodrigues EP, Araujo FR, Oliveira WL, Furtado MA, Castro MB, et al. Ursolic acid and oleanolic acid suppress preneoplastic lesions induced by 1,2-dimethylhydrazine in rat colon. Toxicol Pathol. 2008;36:576–80.
Janakiram NB, Indranie C, Malisetty SV, Jagan P, Steele VE, Rao CV. Chemoprevention of colon carcinogenesis by oleanolic acid and its analog in male F344 rats and modulation of COX-2 and apoptosis in human colon HT-29 cancer cells. Pharm Res. 2008;25:2151–7.
Wei J, Liu M, Liu H, Wang H, Wang F, Zhang Y, et al. Oleanolic acid arrests cell cycle and induces apoptosis via ROS-mediated mitochondrial depolarization and lysosomal membrane permeabilization in human pancreatic cancer cells. J Appl Toxicol. 2013;33:756–65.
Wei J, Liu H, Liu M, Wu N, Zhao J, Xiao L, et al. Oleanolic acid potentiates the antitumor activity of 5-fluorouracil in pancreatic cancer cells. Oncol Rep. 2012;28:1339–45.
Li HF, Wang XA, Xiang SS, Hu YP, Jiang L, Shu YJ, et al. Oleanolic acid induces mitochondrial-dependent apoptosis and G0/G1 phase arrest in gallbladder cancer cells. Drug Des Devel Ther. 2015;9:3017–30.
Zhang P, Li H, Chen D, Ni J, Kang Y, Wang S. Oleanolic acid induces apoptosis in human leukemia cells through caspase activation and poly(ADP-ribose) polymerase cleavage. Acta Biochim Biophys Sin (Shanghai). 2007;39:803–9.
Fujiwara Y, Komohara Y, Kudo R, Tsurushima K, Ohnishi K, Ikeda T, et al. Oleanolic acid inhibits macrophage differentiation into the M2 phenotype and glioblastoma cell proliferation by suppressing the activation of STAT3. Oncol Rep. 2011;26:1533–7.
Guo G, Yao W, Zhang Q, Bo Y. Oleanolic acid suppresses migration and invasion of malignant glioma cells by inactivating MAPK/ERK signaling pathway. PLoS ONE. 2013;8:e72079.
Deeb D, Gao X, Dulchavsky SA, Gautam SC. CDDO-me induces apoptosis and inhibits Akt, mTOR and NF-kappaB signaling proteins in prostate cancer cells. Anticancer Res. 2007;27:3035–44.
Deeb D, Gao X, Jiang H, Janic B, Arbab AS, Rojanasakul Y, et al. Oleanane triterpenoid CDDO-Me inhibits growth and induces apoptosis in prostate cancer cells through a ROS-dependent mechanism. Biochem Pharmacol. 2010;79:350–60.
Deeb D, Gao X, Liu Y, Jiang D, Divine GW, Arbab AS, et al. Synthetic triterpenoid CDDO prevents the progression and metastasis of prostate cancer in TRAMP mice by inhibiting survival signaling. Carcinogenesis. 2011;32:757–64.
Gao X, Deeb D, Liu Y, Arbab AS, Divine GW, Dulchavsky SA, et al. Prevention of prostate cancer with oleanane synthetic triterpenoid CDDO-Me in the TRAMP mouse model of prostate cancer. Cancer. 2011;3:3353–69.
Guo P, Pi H, Xu S, Zhang L, Li Y, Li M, et al. Melatonin improves mitochondrial function by promoting MT1/SIRT1/PGC-1 alpha-dependent mitochondrial biogenesis in cadmium-induced hepatotoxicity in vitro. Toxicol Sci. 2014;142:182–95.
Goldman A, Chen H, Khan MR, Roesly H, Hill KA, Shahidullah M, et al. The Na+/H+ exchanger controls deoxycholic acid-induced apoptosis by a H + −activated, Na + −dependent ionic shift in esophageal cells. PLoS ONE. 2011;6, e23835.
Li X, Li T, Chen D, Zhang P, Song Y, Zhu H, Xiao Y, Xing Y (2015) Overexpression of lysine-specific demethylase 1 promotes androgen-independent transition of human prostate cancer LNCaP cells through activation of the AR signaling pathway and suppression of the p53 signaling pathway. Oncol Rep
Wang X, Spandidos A, Wang H, Seed B. PrimerBank: a PCR primer database for quantitative gene expression analysis, 2012 update. Nucleic Acids Res. 2012;40:D1144–9.
Green DR, Reed JC. Mitochondria and apoptosis. Science. 1998;281:1309–12.
Kroemer G, Reed JC. Mitochondrial control of cell death. Nat Med. 2000;6:513–9.
Murphy MP. How mitochondria produce reactive oxygen species. Biochem J. 2009;417:1–13.
Reiners Jr JJ, Kleinman M, Kessel D, Mathieu PA, Caruso JA. Nonesterified cholesterol content of lysosomes modulates susceptibility to oxidant-induced permeabilization. Free Radic Biol Med. 2011;50:281–94.
Franke TF. PI3K/Akt: getting it right matters. Oncogene. 2008;27:6473–88.
Altomare DA, Testa JR. Perturbations of the AKT signaling pathway in human cancer. Oncogene. 2005;24:7455–64.
Chan CH, Jo U, Kohrman A, Rezaeian AH, Chou PC, Logothetis C, et al. Posttranslational regulation of Akt in human cancer. Cell Biosci. 2014;4:59.
Martini M, De Santis MC, Braccini L, Gulluni F, Hirsch E. PI3K/AKT signaling pathway and cancer: an updated review. Ann Med. 2014;46:372–83.
Cassinelli G, Zuco V, Gatti L, Lanzi C, Zaffaroni N, Colombo D, et al. Targeting the Akt kinase to modulate survival, invasiveness and drug resistance of cancer cells. Curr Med Chem. 2013;20:1923–45.
Greer EL, Brunet A. FOXO transcription factors at the interface between longevity and tumor suppression. Oncogene. 2005;24:7410–25.
Lowe SW, Lin AW. Apoptosis in cancer. Carcinogenesis. 2000;21:485–95.
Thompson CB. Apoptosis in the pathogenesis and treatment of disease. Science. 1995;267:1456–62.
Kang MH, Reynolds CP. Bcl-2 inhibitors: targeting mitochondrial apoptotic pathways in cancer therapy. Clin Cancer Res. 2009;15:1126–32.
Wong RS. Apoptosis in cancer: from pathogenesis to treatment. J Exp Clin Cancer Res. 2011;30:87.
Nicholson DW. Caspase structure, proteolytic substrates, and function during apoptotic cell death. Cell Death Differ. 1999;6:1028–42.
Thornberry NA, Lazebnik Y. Caspases: enemies within. Science. 1998;281:1312–6.
Salvesen GS, Dixit VM. Caspases: intracellular signaling by proteolysis. Cell. 1997;91:443–6.
Adams JM, Cory S. Life-or-death decisions by the Bcl-2 protein family. Trends Biochem Sci. 2001;26:61–6.
Martinou JC, Youle RJ. Mitochondria in apoptosis: Bcl-2 family members and mitochondrial dynamics. Dev Cell. 2011;21:92–101.
Evan GI, Vousden KH. Proliferation, cell cycle and apoptosis in cancer. Nature. 2001;411:342–8.
Diaz-Moralli S, Tarrado-Castellarnau M, Miranda A, Cascante M. Targeting cell cycle regulation in cancer therapy. Pharmacol Ther. 2013;138:255–71.
Carnero A. Targeting the cell cycle for cancer therapy. Br J Cancer. 2002;87:129–33.
Malumbres M, Barbacid M. Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer. 2009;9:153–66.
Nurse P. Ordering S phase and M phase in the cell cycle. Cell. 1994;79:547–50.
Besson A, Dowdy SF, Roberts JM. CDK inhibitors: cell cycle regulators and beyond. Dev Cell. 2008;14:159–69.
Musgrove EA, Caldon CE, Barraclough J, Stone A, Sutherland RL. Cyclin D as a therapeutic target in cancer. Nat Rev Cancer. 2011;11:558–72.
Manning BD, Cantley LC. AKT/PKB signaling: navigating downstream. Cell. 2007;129:1261–74.
Hers I, Vincent EE, Tavare JM. Akt signalling in health and disease. Cell Signal. 2011;23:1515–27.
Bellacosa A, Kumar CC, Di Cristofano A, Testa JR. Activation of AKT kinases in cancer: implications for therapeutic targeting. Adv Cancer Res. 2005;94:29–86.
Testa JR, Bellacosa A. AKT plays a central role in tumorigenesis. Proc Natl Acad Sci U S A. 2001;98:10983–5.
Downward J. PI 3-kinase, Akt and cell survival. Semin Cell Dev Biol. 2004;15:177–82.
Datta SR, Dudek H, Tao X, Masters S, Fu H, Gotoh Y, et al. Akt phosphorylation of BAD couples survival signals to the cell-intrinsic death machinery. Cell. 1997;91:231–41.
Cardone MH, Roy N, Stennicke HR, Salvesen GS, Franke TF, Stanbridge E, et al. Regulation of cell death protease caspase-9 by phosphorylation. Science. 1998;282:1318–21.
Liang J, Slingerland JM. Multiple roles of the PI3K/PKB (Akt) pathway in cell cycle progression. Cell Cycle. 2003;2:339–45.
Takahashi-Yanaga F, Sasaguri T. GSK-3beta regulates cyclin D1 expression: a new target for chemotherapy. Cell Signal. 2008;20:581–9.
Maiese K, Chong ZZ, Shang YC, Hou J. Clever cancer strategies with FoxO transcription factors. Cell Cycle. 2008;7:3829–39.
Lei H, Quelle FW. FOXO transcription factors enforce cell cycle checkpoints and promote survival of hematopoietic cells after DNA damage. Mol Cancer Res. 2009;7:1294–303.
van der Horst A, Burgering BM. Stressing the role of FoxO proteins in lifespan and disease. Nat Rev Mol Cell Biol. 2007;8:440–50.
Zhang X, Tang N, Hadden TJ, Rishi AK. Akt, FoxO and regulation of apoptosis. Biochim Biophys Acta. 1813;2011:1978–86.
Kloet DE, Burgering BM. The PKB/FOXO switch in aging and cancer. Biochim Biophys Acta. 1813;2011:1926–37.
Pugazhenthi S, Nesterova A, Sable C, Heidenreich KA, Boxer LM, Heasley LE, et al. Akt/protein kinase B up-regulates Bcl-2 expression through cAMP-response element-binding protein. J Biol Chem. 2000;275:10761–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the National Natural Science Foundation of China (Nos. 81272847 and 30973008) and the Program for New Century Excellent Talents in University (NCET-13-0239).
Conflicts of interest
None
Statement of human right
This article does not contain any studies with human participants performed by any of the authors.
Ethical approval
This article contains studies with animals. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. This study was approved by the Institutional Animal Care and Use Committee of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s. Republic of China (IACUC Number: S430). All procedures performed in studies involving animals were in accordance with the ethical standards of the institution at which the studies were conducted.
Additional information
Xuechao Li and Yarong Song contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, X., Song, Y., Zhang, P. et al. Oleanolic acid inhibits cell survival and proliferation of prostate cancer cells in vitro and in vivo through the PI3K/Akt pathway. Tumor Biol. 37, 7599–7613 (2016). https://doi.org/10.1007/s13277-015-4655-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4655-9