Abstract
Programmed cell death protein-1 (PD-1) inhibitor may be therapeutic in patients with relapsed or refractory classical Hodgkin’s lymphoma (cHL). This study examined the prognostic significance of PD-1 and two PD-1 ligands (PD-L1 and PD-L2) in uniformly treated cHL. Diagnostic tissues from 109 cHL patients treated with a doxorubicin, bleomycin, vinblastine, and dacarbazine regimen were evaluated retrospectively by immunohistochemical analysis of PD-L1, PD-L2, and PD-1 expressions. The median follow-up time was 4.91 years (range, 0.17–17.33 years). Thirteen patients (11 %) expressed PD-1 protein in the peritumoral microenvironment, which was associated with poor overall survival (OS) (P = 0.017). PD-L1 or PD-L2 expression was not associated with OS. There was no correlation between PD-L1 and PD-1 expression or between PD-L2 and PD-1 expression. Multivariate analysis identified PD-1 protein as an independent prognostic factor for OS (P = 0.019). Subgroup analysis according to the Ann Arbor stage of cHL showed that PD-1 protein expression had a prognostic value in limited-stage cHL (P = 0.048). PD-1 is an independent prognostic factor in cHL and may allow the identification of a subgroup of patients with limited-stage cHL who require more intensive therapy and who may benefit from anti-PD-1 agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Standard treatment does not cure at least 20 % of patients with classical Hodgkin’s lymphoma (cHL), and they may require adapted first-line treatment [1, 2]. Although the International Prognostic Score (IPS) is a powerful tool for risk stratification, it does not fully reflect intrinsic biological features of cHL tumor cells. Furthermore, IPS does not apply to limited stages [3], and none of the published prognostic-factor systems can reliably identify patients with a worse prognosis.
Programmed cell death protein-1 (PD-1) is an immune checkpoint receptor of T, B, and natural killer (NK) cells that represses Th1 cytotoxic immune responses and contributes to the maintenance of tolerance to systemic self-antigens [4, 5]. Two ligands for PD-1, PD-L1 (B7-H1) and PD-L2 (B7-DC), have been identified as negative immune regulators via interaction with the PD-1 receptor [6]. By expressing PD-L1 or PD-L2 ligands on the tumor cell surface and engaging PD-1 receptor-positive T, B, and NK cells, tumors can promote the PD-1 pathway to evade an immune response [7]. A blockade of PD-1 or PD-L1 by anti-PD-1 or anti-PD-L1 antibody, respectively, instills remarkable antitumor activity in melanoma, renal cell cancer, non-small-cell lung cancer, and ovarian cancers. PD-1, PD-L1, and PD-L2 have prognostic significance in gastrointestinal stromal tumors [8], nasopharyngeal carcinoma [9], urothelial carcinoma [10], breast cancer [11], lung cancer [12], and colorectal cancer [13].
Nivolumab is a monoclonal antibody directed at PD-1. It has substantial therapeutic activity and an acceptable safety profile in relapsed or refractory cHL [14]. Co-expression of PD-1 and PD-L1 is associated with poor clinical outcomes in patients with cHL [15]. Although PD-1 and PD-L2 also appear to play important roles in the modulation of Th2 responses [16], no study has examined the relationship between PD-1, PD-L1, and PD-L2 and their prognostic implication in cHL patients. Our present retrospective study evaluated PD-1, PD-L1, and PD-L2 expressions in cHL patients and examined correlations between these markers and their prognostic significance.
Materials and methods
Patients
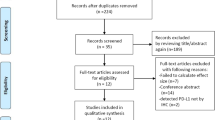
This retrospective study reviewed histological and immunohistochemical data from 109 consecutive patients diagnosed with cHL at Asan Medical Center, Seoul, South Korea, between 1995 and 2012. All patients had pathologically confirmed cHL that was treated with a doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) therapy regimen, with or without radiation. The patients were ≥15 years of age at diagnosis and had no previous treatment or history of malignancy. Paraffin-embedded tumor tissues and follow-up data were available for all patients included in the study. The median follow-up time was 4.91 years (range, 0.17–17.33 years). Response criteria were based on standard guidelines. Routine follow-up imaging analyses were performed every 3 months for the first 2 years, every 6 months for the next 3 years, and annually (or whenever clinically indicated) thereafter. This research was approved by the Internal Review Board of the Asan Medical Center.
Histopathological analysis and immunohistochemistry
All histological and immunophenotypic data were reviewed by two pathologists (JH and YWK). The cHL cases were subtyped according to World Health Organization (WHO) criteria as nodular sclerosis (NS), lymphocyte-rich (LR), mixed cellularity (MC), lymphocyte-depleted (LD), or not-otherwise-specified cHL. A tissue microarray (TMA) was constructed with three 1-mm-diameter tumor cores from selected areas of formalin-fixed, paraffin-embedded tumor samples. TMA sections were stained using a BenchMark XT automatic immunohistochemistry staining device (Ventana Medical System, Tucson, AZ). An anti-PD-L1 monoclonal antibody (mAb) (dilution 1:100, clone E1L3N; Cell Signaling Technology, Danvers, MA), a mouse anti-PD-L2 mAb (dilution 1:3000, clone #176611; R&D systems, Minneapolis, MN), and a mouse anti-PD-1 mAb (dilution 1:100, clone MRQ-22; Cell Marque, Rocklin, CA) were used. In the TMA, each case was represented by three tissue cores. At least 10 CD30-positive Hodgkin/Reed-Sternberg (HRS) cells in at least one of the three core cylinders from each patient were read. Various cutoff points for PD-L1, PD-L2, and PD-1 expressions were examined by the Kaplan-Meier method, with comparisons performed by log-rank testing from the 10th to the 25th percentile in 5 % increments, i.e., 10, 15, 20, and 25 % (Supplementary Table 1). The most significant differences in OS were observed at a cutoff point of 20 % for PD-L1, PD-L2, and PD-1. A sample was considered PD-L1- or PD-L2-positive if the expression of these markers was detected in ≥20 % of HRS cells. A sample was considered PD-1-positive if PD-1 expression was detected in ≥20 % of the peritumoral microenvironment. In situ hybridization (ISH) analysis of Epstein-Barr Virus (EBV)-encoded RNA-1 and RNA-2 (EBER) was performed and scored as previously described [17].
Statistical analyses
Overall survival (OS) was defined as the interval between the date of diagnosis and death from any cause. The follow-up of living patients was censored at their last follow-up date. Cumulative OS was analyzed by the Kaplan-Meier method, and comparisons were performed by log-rank testing. Multivariate prognostic analyses of OS were performed with the Cox proportional hazard regression model using the enter method. Categorical variables were compared using the chi-square test. All statistical analyses were performed using the SPSS statistical software program version 18.0 (SPSS, Chicago, IL) or R 2.15.2. All P values are two-sided associations, and P < 0.05 was considered statistically significant.
Results
Patient characteristics
The clinical characteristics of the 109 patients are summarized in Table 1. The median age of the patients was 36 years (range, 15–77 years). Twenty patients died. The median OS was not reached. The estimated 5-year OS was 83 %.
PD-L1, PD-L2, and PD-1 expressions in cHL tissues
The correlations between PD-L1, PD-L2, PD-1, and clinical variables are summarized in Table 2. Eighty-two patients (75 %) showed cytoplasmic and/or membranous positivity for PD-L1 (Fig. 1a). Patients with PD-L1 expression were more likely to have a low level of lactate dehydrogenase (49 % vs. 22 %, P = 0.024) than PD-L1-negative patients. Thirteen patients (11 %) revealed cytoplasmic and/or membranous positivity for PD-L2 (Fig. 1b) or membranous positivity for PD-1 (Fig. 1c). PD-L2 or PD-1 expression was not associated with clinical variables. All PD-L2-positive cases showed PD-L1 positivity. According to the expressions of PD-L1 and PD-1, 23 cases were negative for both PD-L1 and PD-1, 73 cases were positive for PD-L1 and negative for PD-1, 4 cases were positive for PD-1 and negative for PD-L1, and 9 cases were positive for both PD-L1 and PD-1. There was no correlation between PD-L1 and PD-1 expressions (P = 0.732). There was also no correlation between PD-L2 and PD-1 expressions (P = 0.706).
Prognostic significance of PD-L1, PD-L2, and PD-1 expressions
Patients with PD-1 expression had lower 5-year OS rates (59 vs. 86 %, P = 0.017; Fig. 2a) than patients without PD-1 expression. PD-L1 or PD-L2 expression was not significantly associated with OS rates (P = 0.477, Fig. 2b, and P = 0.676, Fig. 2c, respectively). To evaluate the relationship between PD-L1 and PD-1, we combined the dichotomized PD-L1 and PD-1 data and stratified patients into three risk groups (PD-L1-/PD-1-, PD-L1+ or PD-1+, PD-L1+/PD-1+). PD-L1+/PD-1+ patients showed worse OS compared to other groups, although this difference was not statistically significant (P = 0.598; Fig. 2d). OS was analyzed for two groups (PD-1+ and PD-L1+ vs. PD-1- and/or PD-L1-). However, OS was not significantly different between two groups (P = 0.33) in all patients. Analysis of patients with a limited stage showed no significant difference between two groups, either (P = 0.604).
Comparison of survival rates according to PD-L1, PD-L2, and PD-1 expressions. Overall survival (OS) was significantly worse in PD-1-positive cases (a). PD-L1 (b) or PD-L2 (c) expression was not significantly associated with OS. Patients with PD-L1+ and PD-1+ status showed a poorer OS compared to other groups, although this difference was not statistically significant (d)
Univariate analysis revealed that OS was associated with IPS (≥3). Multivariate analysis identified the PD-1 expression as an independent prognostic marker for OS (P = 0.019, Table 3) along with high-risk IPS (≥3). As the prognostic significance of IPS was limited to the advanced-stage disease [3], we performed subgroup analysis according to the disease stage to determine if PD-1 expression outperforms IPS as a prognostic marker. In limited-stage cHL cases, PD-1-positive patients had a worse OS compared with PD-1-negative patients, (P = 0.048; Fig. 3a). In contrast, IPS was not significantly associated with OS in limited-stage cHL (P = 0.784). In advanced-stage cHL cases, PD-1-positive status was not associated with OS (P = 0.13; Fig. 3b), whereas IPS was significantly associated with OS (P = 0.012).
Discussion
In our present study, the expression of PD-1 was independently associated with OS, supporting the hypothesis that a PD-1-related signaling pathway plays an important role in the progression of cHL. Although IPS was not significantly associated with OS in limited-stage cHL, PD-1 expression did have prognostic value in limited-stage cHL. However, PD-L1 or PD-L2 expression was not associated with OS rate.
Two studies previously assessed the prognostic significance of the PD-1 expression in patients with cHL and yielded mixed results [15, 18]. Muenst et al. found a significantly negative prognostic effect of PD-1 expression [18]. Paydas et al. reported that cases with co-expression of PD-1 and PD-L1 correlated with inferior OS, but PD-1 or PD-L1 alone did not [15]. Our study identified significant adverse prognostic effects of PD-1 expression but not co-expression of PD-1 and PD-L1, PD-L1 alone, or PD-L2 alone. Although the PD-1-blocking antibody nivolumab has been evaluated in patients with cHL, that study did not report on PD-1 expression [14]. Further studies are needed to confirm the precise mechanism of the PD-1-blocking antibody in relation to PD-1 expression in cHL patients.
We used 20 % as a cutoff in analysis of PD-L1, PD-L2, and PD-1. We found a negative prognostic effect of PD-1 expression. Various cutoffs were used in previous studies. In the pioneering study by Ansell et al., all cases were PD-L1- and PD-L2-positive [14]. However, that study included relapsed or refractory cHL alone, and the number of cases was relatively small. Muenst et al. used 23 PD-1 cells/mm2 as the cutoff for PD-1 [18]. Forty-five percent of patients in that study had more than 23 PD-1 cells/mm2. Paydas et al. used 20 % as the cutoff for PD-1 and 5 % as the cutoff for PD-L1 [15]. Twenty percent of patients in that study were positive for PD-1 and PD-L1 expressions. Possible causes for the discrepancies between previous studies and our current results include ethnic differences and technical differences such as different antibody clones and the use of tissue microarray vs. whole sections.
EBV, a common herpes virus that infects more than 90 % of humans, is categorized as a group 1 human carcinogen by the International Agency for Research on Cancer due to its etiologic role in cHL [19]. Our present study found no correlation between EBV status and PD-L1 expression, PD-L2 expression, or PD-1 expression. A prior study also failed to identify a correlation between EBV and PD-1 or EBV and PD-L1 [15]. We performed subgroup analyses in PD-1- or PD-L1-positive patients according to EBER status. However, EBER status was not significantly associated with OS in PD-1- or PD-L1-positive patients (P = 0.573 and P = 0.407, respectively). These results suggest that PD-1 expression is associated with survival outcomes independently of EBV status.
In our current study, PD-1 expression was significantly associated with poor prognosis, especially for patients with limited-stage disease. Although IPS remains a valid predictor of outcome for patients with advanced-stage disease, it is unsuccessful in stratifying subgroups with a poorer prognosis in patients with limited-stage cHL [3]. Our present results also revealed that IPS was associated with prognosis only in advanced-stage cHL. Therefore, PD-1 expression is a viable prognostic factor alternative to IPS in limited-stage cHL.
In our present series, 75 % of cases were positive for PD-L1 and 11 % were positive for PD-1. Four cases were positive for PD-1 and negative for PD-L1. Three out of four patients died. Besides its interaction with PD-1, PD-L1 also binds CD80 molecules expressed on activated T cells, mediating T cell inhibition [20, 21]. To the best of our knowledge, ligands for PD-1 beside PD-L1 and PD-L2 have not been identified. Further studies are needed to determine the precise mechanisms for the poor prognosis of PD-L1-negative/PD-1-positive cases.
Engagement of PD-1 might directly inhibit T cell receptor (TCR)-mediated effector functions by recruiting phosphatases such as Src homology 2 domain-containing tyrosine phosphatase 2 (SHP-2) [22]. Phosphorylation of the TCR CD3zeta chains and Zap-70, early steps following TCR engagement, is also inhibited by PD-1 [22, 23]. PD-1 inhibits T cell activation by attenuating TCR signaling (SHP-2) and promoting the expression of genes that impair T cell function. PD-1 enhances the expression of transcription factor ATF-like (BATF), which is sufficient to inhibit T cell proliferation and cytokine secretion [24]. Activation of PD-1 impairs T cell expansion and function by promoting IL-10 production [25]. PD-1 inhibits T cell responses by promoting the induction and maintenance of iT reg cells via the downregulation of phospho-Akt, mTOR, S6, and ERK2 and the concomitant upregulation of PTEN [26]. PD-1 regulates T cell metabolism by inhibiting glycolysis and promoting lipolysis and fatty acid oxidation [27].
The most common approach to blocking the PD-1, PD-L1, and PD-L2 pathways is to use mAbs against the receptor. These antibodies inhibit ligand binding and downregulate the receptor. Anti-PD-L1 mAbs, including MEDI4736, and MPDL3280A, have significant antitumor activity in non-small-cell lung cancer [28, 29], melanoma [28], bladder cancer [30], and renal cancer [28]. PD-1-targeting mAbs such as nivolumab and pembrolizumab have shown remarkable success by generating durable clinical responses in melanoma [31–33], non-small-cell lung cancer [34, 35], renal cancer [36], and cHL [14]. Previous studies revealed a strong correlation of the PD-L1 expression to the treatment efficacy of anti-PD-1 agents in non-small-cell lung cancer, melanoma, and head and neck cancer [37–39]. A significant correlation between the PD-L1 expression to treatment efficacy of anti-PD-L1 agents was also reported in melanoma, non-small-cell lung cancer, and bladder cancer [39]. In Ansell’s study, the association between the PD-L1 expression in HRS cells of cHL patients and the response to nivolumab was not examined [14]. We suggest that PD-1 may be a possible predictive marker for anti-PD-1 agents because PD-1 alone was significantly associated with OS rates in our study.
Some limitations of our present study include its retrospective design, short follow-up period for some recent cases, and small sample size. Furthermore, TMA does not reflect the entire protein expression profile due to tumor heterogeneity.
In summary, our current results suggest that PD-1 is an independent prognostic factor in cHL and may be useful for identifying a subgroup of patients with limited-stage cHL at high risk for recurrence or progression that might benefit from anti-PD-1 agents.
References
Bjorkholm M, Axdorph U, Grimfors G, Merk K, Johansson B, Landgren O, et al. Fixed versus response-adapted MOPP/ABVD chemotherapy in Hodgkin’s disease. A prospective randomized trial. Annals Oncol. 1995;6:895–9.
Quddus F, Armitage JO. Salvage therapy for Hodgkin’s lymphoma. Cancer J. 2009;15:161–3.
Hasenclever D, Diehl V. A prognostic score for advanced Hodgkin’s disease. International prognostic factors project on advanced Hodgkin’s disease. N Engl J Med. 1998;339:1506–14.
Freeman GJ, Long AJ, Iwai Y, Bourque K, Chernova T, Nishimura H, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192:1027–34.
Okazaki T, Honjo T. PD-1 and PD-1 ligands: from discovery to clinical application. Int Immunol. 2007;19:813–24.
Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol. 2008;26:677–704.
Weber J. Immune checkpoint proteins: a new therapeutic paradigm for cancer--preclinical background: CTLA-4 and PD-1 blockade. Semin Oncol. 2010;37:430–9.
Bertucci F, Finetti P, Mamessier E, Pantaleo MA, Astolfi A, Ostrowski J, et al. PDL1 expression is an independent prognostic factor in localized gist. Oncoimmunology. 2015;4:e1002729.
Zhang J, Fang W, Qin T, Yang Y, Hong S, Liang W, et al. Co-expression of PD-1 and PD-L1 predicts poor outcome in nasopharyngeal carcinoma. Med Oncol. 2015;32:86.
Bellmunt J, Mullane SA, Werner L, Fay AP, Callea M, Leow JJ, et al. Association of PD-L1 expression on tumor-infiltrating mononuclear cells and overall survival in patients with urothelial carcinoma. Ann Oncol. 2015;26:812–7.
Muenst S, Schaerli AR, Gao F, Daster S, Trella E, Droeser RA, et al. Expression of programmed death ligand 1 (PD-L1) is associated with poor prognosis in human breast cancer. Breast Cancer Res Treat. 2014;146:15–24.
Zhang Y, Wang L, Li Y, Pan Y, Wang R, Hu H, et al. Protein expression of programmed death 1 ligand 1 and ligand 2 independently predict poor prognosis in surgically resected lung adenocarcinoma. OncoTargets Ther. 2014;7:567–73.
Droeser RA, Hirt C, Viehl CT, Frey DM, Nebiker C, Huber X, et al. Clinical impact of programmed cell death ligand 1 expression in colorectal cancer. Eur J Cancer. 2013;49:2233–42.
Ansell SM, Lesokhin AM, Borrello I, Halwani A, Scott EC, Gutierrez M, et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphoma. N Engl J Med. 2015;372:311–9.
Paydas S, Bagir E, Seydaoglu G, Ercolak V, Ergin M (2015) Programmed death-1 (PD-1), programmed death-ligand 1 (PD-L1), and EBV-encoded RNA (EBER) expression in Hodgkin lymphoma. Ann Hematol
Rozali EN, Hato SV, Robinson BW, Lake RA, Lesterhuis WJ. Programmed death ligand 2 in cancer-induced immune suppression. Clin Dev Immunol. 2012;2012:656340.
Huh J, Cho K, Heo DS, Kim JE, Kim CW. Detection of Epstein-Barr virus in Korean peripheral T-cell lymphoma. Am J Hematol. 1999;60:205–14.
Muenst S, Hoeller S, Dirnhofer S, Tzankov A. Increased programmed death-1+ tumor-infiltrating lymphocytes in classical Hodgkin lymphoma substantiate reduced overall survival. Hum Pathol. 2009;40:1715–22.
Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, et al. A review of human carcinogens--part b: biological agents. Lancet Oncol. 2009;10:321–2.
Butte MJ, Keir ME, Phamduy TB, Sharpe AH, Freeman GJ. Programmed death-1 ligand 1 interacts specifically with the B7-1 costimulatory molecule to inhibit T cell responses. Immunity. 2007;27:111–22.
Park JJ, Omiya R, Matsumura Y, Sakoda Y, Kuramasu A, Augustine MM, et al. B7-H1/CD80 interaction is required for the induction and maintenance of peripheral T-cell tolerance. Blood. 2010;116:1291–8.
Yokosuka T, Takamatsu M, Kobayashi-Imanishi W, Hashimoto-Tane A, Azuma M, Saito T. Programmed cell death 1 forms negative costimulatory microclusters that directly inhibit T cell receptor signaling by recruiting phosphatase SHP2. J Exp Med. 2012;209:1201–17.
Sheppard KA, Fitz LJ, Lee JM, Benander C, George JA, Wooters J, et al. Pd-1 inhibits T-cell receptor induced phosphorylation of the ZAP70/CD3zeta signalosome and downstream signaling to PKCtheta. FEBS Lett. 2004;574:37–41.
Quigley M, Pereyra F, Nilsson B, Porichis F, Fonseca C, Eichbaum Q, et al. Transcriptional analysis of HIV-specific CD8+ T cells shows that PD-1 inhibits T cell function by upregulating BATF. Nat Med. 2010;16:1147–51.
Said EA, Dupuy FP, Trautmann L, Zhang Y, Shi Y, El-Far M, et al. Programmed death-1-induced interleukin-10 production by monocytes impairs CD4+ T cell activation during HIV infection. Nat Med. 2010;16:452–9.
Francisco LM, Salinas VH, Brown KE, Vanguri VK, Freeman GJ, Kuchroo VK, et al. PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med. 2009;206:3015–29.
Patsoukis N, Bardhan K, Chatterjee P, Sari D, Liu B, Bell LN, et al. PD-1 alters T-cell metabolic reprogramming by inhibiting glycolysis and promoting lipolysis and fatty acid oxidation. Nat Commun. 2015;6:6692.
Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366:2455–65.
Brahmer JR, Rizvi NA, Lutzky J (2014b) Clinical activity and biomarkers of MEDI4736, an anti-PD-L1 antibody, in patients with NSCLC. ASCO Meet Abstr 32:8021
Powles T, Eder JP, Fine GD, Braiteh FS, Loriot Y, Cruz C, et al. MPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancer. Nature. 2014;515:558–62.
Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH, et al. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J Clin Oncol. 2014;32:1020–30.
Robert C, Long GV, Brady B, Dutriaux C, Maio M, Mortier L, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372:320–30.
Robert C, Ribas A, Wolchok JD, Hodi FS, Hamid O, Kefford R, et al. Anti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: a randomised dose-comparison cohort of a phase 1 trial. Lancet. 2014;384:1109–17.
Brahmer J, Reckamp KL, Baas P, Crino L, Eberhardt WE, Poddubskaya E, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373:123–35.
Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372:2018–28.
Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–54.
Gettinger SN, Shepherd FA, Antonia SJ. First-line nivolumab (anti-PD-1; BMS-936558, ONO-4538) monotherapy in advanced NSCLC: safety, efficacy, and correlation of outcomes with PD-L1 status. ASCO Meet Abstr. 2014;32:8024.
Gandhi L (2014) MK-3475 (anti-PD-1 monoclonal antibody) for non-small cell lung cancer (NSCLC): antitumor activity and association with tumor PD-L1 expression [abstract]. Proc Ann Meet AACR CT105
Sunshine J, Taube JM. PD-1/PD-L1 inhibitors. Curr Opin Pharmacol. 2015;23:32.
Acknowledgments
This study was supported by a grant (2011-090) from the Asan Institute for Life Sciences, Seoul, Korea.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Koh, Y.W., Jeon, Y.K., Yoon, D.H. et al. Programmed death 1 expression in the peritumoral microenvironment is associated with a poorer prognosis in classical Hodgkin lymphoma. Tumor Biol. 37, 7507–7514 (2016). https://doi.org/10.1007/s13277-015-4622-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4622-5