Abstract
The classification of ameloblastoma in multicystic or unicystic variants is associated with its clinical behaviour. Recently, BRAF and SMO mutations have been reported in ameloblastomas. However, it is not clear if such mutations are shared by the multi- and unicystic variants of ameloblastoma or by odontogenic carcinomas. We assessed BRAFV600E and SMOF412E in multicystic, unicystic and desmoplastic ameloblastomas. In addition, we investigated whether the BRAFV600E mutation occurs in odontogenic carcinomas. A total of 28 formalin-fixed paraffin-embedded samples, comprising 17 ameloblastomas and 11 odontogenic carcinomas, were included. The BRAFV600E mutation was assessed by real-time PCR with a specific TaqMan probe and confirmed by Sanger sequencing. The SMOF412E mutation was assessed by Sanger sequencing. Fourteen out of 17 (82 %) ameloblastomas showed the BRAFV600E mutation, specifically, 5/6 (83 %) unicystic, 7/9 (78 %) multicystic and 2/2 desmoplastic ameloblastomas. BRAFV600E mutation was detected in 4/11 (36 %) malignant tumours, specifically, 3/8 (38 %) ameloblastic carcinomas and 1/1 clear cell odontogenic carcinoma, while the two ghost cell odontogenic carcinomas did not harbour this mutation. The SMOF412E mutation was not detected in ameloblastoma. The BRAFV600E-activating mutation is a common event in ameloblastomas, occurring regardless of site or histological type. This mutation is also detected in odontogenic carcinomas. SMO somatic mutation is a secondary genetic event in the ameloblastoma pathogenesis. Our findings support the possibility for personalised, molecular-targeted therapy for ameloblastomas and odontogenic carcinomas harbouring the BRAFV600E mutation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Odontogenic tumours comprise a group of heterogeneous lesions ranging from hamartomatous or non-neoplastic tissue proliferation to benign or malignant neoplasms with metastatic potential. The ameloblastoma is the most common odontogenic neoplasm, comprising almost 50 % of the group [1], but to date, only a few studies elucidating its mutations and others hallmarks have been described in literature.
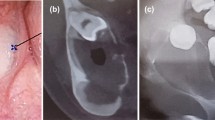
Ameloblastoma is a locally aggressive, benign odontogenic neoplasm that is classified by the World Health Organization (WHO) into the following variants: solid/multicystic, unicystic, desmoplastic or peripheral types [1]. While solid/multicystic lesions tend to be more infiltrative, unicystic tumours are usually encapsulated. Resection with a 1.5- to 2-cm margin beyond the radiological limits is suggested for the treatment of the solid/multicystic type, but a more conservative approach has been advocated by some authors for the unicystic variant [2]. Surgical resection is associated with significant facial deformity and morbidity.
Ameloblastic carcinoma (AC) is a rare odontogenic malignant neoplasm that combines the histological features of ameloblastoma with cytological atypia, such as cellular pleomorphism, mitoses, nuclear hyperchromatism, focal necrosis and perineural invasion [3, 4]. AC exhibits local aggressiveness and a propensity for metastasis, and currently, no potential molecular target for personalised molecular therapy has been described for this entity. According to the WHO, AC may arise de novo or from a long-standing ameloblastoma [1, 3]. However, there is no unequivocal evidence to prove the transition from the benign to the malignant ameloblastoma phenotype.
Mitogen-activated protein kinase (MAPK) pathways are evolutionarily highly conserved kinase modules that link extracellular signals to the machinery that coordinates a broad spectrum of cellular processes, such as growth, proliferation, differentiation, migration and apoptosis. The Ras/Raf/MEK/ERK pathway is an extensively studied mammalian MAPK pathway and is deregulated in several human cancers [5]. Among the Raf kinase family members, BRAF is the most potent activator of the MAPK pathway [6]. BRAF-activating transversion (T > A) in the kinase domain at exon 15 (position c.1799) is the most frequent BRAF mutation, and it results in a valine (V) to glutamic acid (E) substitution at codon 600. The mutated protein, BRAFV600E, is thought to mimic the phosphorylation of the activation segment and constitutively activates the MAK kinase pathway [5].
The BRAFV600E mutation was recently reported in ameloblastomas [7–9]. In vitro experiments demonstrated that BRAF-mutated ameloblastoma cells had constitutive MAPK pathway activation, which was inhibited by the BRAF inhibitor vemurafenib [7, 9].
The identification of this BRAF mutation in ameloblastomas is an important step towards personalised therapy for this disease [10]. Nevertheless, it is important to further refine these analyses and to evaluate whether the BRAFV600E mutation is a signature of multicystic ameloblastomas or if it is also found in unicystic tumours. Is this mutation present in desmoplastic ameloblastomas? We aimed to answer this question. In addition, it is important to investigate whether maxillary ameloblastomas present this mutation in the same frequency as has been reported for the mandibular cases. Considering that AC is the malignant counterpart of ameloblastomas, we assessed the BRAFV600E mutation in AC samples, as well as in other malignant epithelial odontogenic tumours (ghost cell odontogenic carcinomas and clear cell odontogenic carcinoma). Because activating SMO mutations (mostly SMOL412F) have been suggested to be a carcinogenic event underling the pathogenesis of maxillary ameloblastomas [9], we also assessed SMO mutations at codon 412 in the same cohort of ameloblastomas.
Materials and methods
Samples
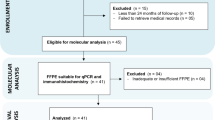
A total of 28 formalin-fixed paraffin-embedded (FFPE) tissue samples, comprising 17 ameloblastomas and 11 odontogenic carcinomas, were included in this study. These ameloblastoma samples comprised six unicystic, nine solid multicystic and two desmoplastic tumours, while the malignant tumours consisted of eight AC, one clear cell odontogenic carcinoma and two ghost cell odontogenic carcinoma samples (Table 1). The diagnostic criteria used for unicystic ameloblastoma were published by Ackerman et al. [11]. The samples were obtained from the files of the Oral Pathology Services at Universidade Federal de Minas Gerais, Universidade Federal de Uberlândia and from Instituto Nacional de Cancer, Brazil. All diagnoses were reviewed by two oral pathologists (RSG and AML). The local ethics committee approved this study (number CAAE 30405514.5.0000.5149).
DNA extraction and mutation detection
Genomic DNA was extracted from manually (ameloblastoma) or laser-microdissected (malignant tumours) FFPE tissue samples using a QIAamp DNA FFPE Tissue Kit (QIAGEN, Germany) according to the manufacturer’s instructions. To assess BRAF mutations encoding V600E, real-time PCR was performed with a specific TaqMan probe (BRAF_476_mu) (Life Technologies, CA, USA) to detect the T > A transversion at position c.1799. Data files containing cycle threshold (CT) values were imported into Mutation Detector™ Software (Life Technologies). The difference between the CT value of each mutant allele assay and the CT value of the gene reference assay was calculated, and the mutation status was determined for each sample. To confirm the BRAF mutation, Sanger sequencing was performed using the following primers: forward 3′ TCATAATGCTTGCTCTGATAGGA 5′ and reverse 3′ CCAAAAATTTAATCAGTGGA 5′. To detect the SMO mutation at codon 412, Sanger sequencing was performed with the following primer pair: forward 3′ GATGGGGACTCTGTGAGTGG 5′ and reverse 3′ TGTTGCCCAACTGGTCCT 5′. The SMO mutation was only assessed in the ameloblastomas, due to lack of DNA quantity of the malignant samples.
Results
All the results are summarised in Table 1 and Fig. 1. Fourteen of 17 ameloblastomas (82 %) showed the BRAFV600E mutation. These BRAF mutant samples represented 83 and 78 % of unicystic and multicystic samples, respectively, and both samples of desmoplastic ameloblastoma. The BRAF mutation occurred regardless of plexiform, follicular or granular cell histology. SMO mutations at codon 412 were not observed in any of the 17 ameloblastoma samples analysed.
The BRAFV600E mutation was detected in 4/11 (36 %) malignant tumours, specifically, in 3/8 (38 %) ameloblastic carcinomas and in 1/1 clear cell odontogenic carcinoma, while the two ghost cell odontogenic carcinomas did not harbour this mutation (Fig. 1, Table 1).
Discussion
According to a recently published comment by Marino-Enriquez and Fletcher [12], although the contemporary understanding of tumorigenesis is largely based on the study of malignant tumours, studies on benign tumours provide complementary and perhaps equally relevant perspectives on the mechanisms of tumour invasion and metastasis. Our molecular approach of assessing the benign and malignant counterparts of odontogenic tumours is in line with this notion, thus providing better insights into the evolution and molecular pathogenesis of neoplasia.
In 2014, the oncogenic BRAFV600E mutation was reported to be present at a high prevalence (above 60 %) in ameloblastoma [7–9]. Although these first reports described this oncogenic mutation with clinical implications for the treatment of aggressive and recurrent ameloblastoma cases, it is now of high importance to further refine this discovery. Currently, the most important information associated with ameloblastoma clinical behaviour is the classification in solid multicystic or unicystic (or desmoplastic, although rare) variants. On this basis, we aimed to investigate whether this BRAF mutation occurs in these three variants at similar proportions. In our series, 5/6 unicystic, 7/9 multicystic and 2/2 desmoplastic ameloblastomas showed the BRAFV600E mutation. This finding indicates that encapsulated (unicystic), infiltrative (multicystic) and desmoplastic ameloblastomas share the same molecular alterations, comprising 82 % of our benign samples. In addition, this mutation occurred regardless of plexiform, follicular or granular cell histology.
AC is an uncommon tumour type, with poor prognosis and frequent metastases, which indicates the requirement for systemic therapy. We showed that the BRAFV600E mutation occurs in some cases of AC, the malignant counterpart of ameloblastoma. We also report a clear cell odontogenic carcinoma harbouring the BRAFV600E mutation, revealing the MAPK pathway as a new and important target for personalised therapy for the treatment of AC and a subset of malignant odontogenic tumours.
While the BRAFV600E mutation occurred in approximately 82 % (14/17) of our benign ameloblastoma samples, a lower BRAFV600E mutation frequency was noted in AC (3/8, 38 %). Our results raise the following questions: Is BRAFV600E an oncogenic event underlying the pathogenesis of only a subset of AC and ameloblastomas? Is BRAFV600E important for the early stages of ameloblastoma tumorigenesis, and does this mutation tend to disappear with tumour progression in cases where malignant transformation occurs? Alternatively, distinct molecular pathways may underlie the pathogenesis of tumours with/without the mutation, and further studies are necessary to clarify these questions. In the case of the malignant transformation of an ameloblastoma, it is also possible to consider that some AC tumours may arise in a pre-existing, benign BRAFV600E mutant ameloblastoma after the acquisition of further oncogenic events. In animal models, the transgenic expression of human BRAFV600E has been shown to be sufficient to form nevi. However, the lesion was prone to evolve into a melanoma-like malignancy, only in a p53−/− (zebra fish model) or PTEN-silencing (mice model) background [13, 14]. Next-generation sequencing approaches, such as the single cell whole genome of serial and spatially distinct regions of AC and ameloblastomas, may enrich the debate on the existence of a biological continuum from benign to malignant ameloblastic lesions.
In a recent paper, a controversial existence of site-specific mutations in ameloblastomas was proposed as a new paradigm. According to Sweeney et al. [9], the SMO mutation would be a signature of ameloblastomas of the maxilla, while the BRAF mutation would be the predominant event in tumours of the mandible. This difference in the molecular aetiopathogenesis of mandible and maxillary tumours seems rather improbable. Our data are clearly not consistent with this “new paradigm”. SMO mutations were not observed in any of our 17 ameloblastoma samples, including four from the maxilla. Additionally, in the study by Sweeney and colleagues [9], mutations in SMO occurred simultaneously with other FGFR2-RAS-BRAF mutations. Moreover, in a series of 50 cases reported by Brown and colleagues [7], SMO mutations occurred in isolation only in one case, whereas the other seven cases showed SMO mutations simultaneously with other FGFR2-RAS-BRAF mutations. Our data further strengthen the notion that the BRAF alteration is not a signature of mandibular ameloblastomas but that it is most likely a driver mutation for both mandibular/maxillary tumours. SMO somatic mutations may function as secondary passenger events.
Conclusion
BRAFV600E-activating mutations is a common event in ameloblastomas, occurring regardless of site or histological type. This mutation is also present in some odontogenic carcinomas. The SMOF412E somatic mutation previously reported by others [9] probably represents a secondary genetic event in the ameloblastoma pathogenesis. Our findings support the possibility for personalised, molecular-targeted therapy for ameloblastomas and odontogenic carcinomas harbouring the BRAFV600E mutation.
References
Barnes L, Eveson JW, Reichart P, Sidransky D. (eds.) (2005) World Health Organization classification of tumours. Pathology and genetics of head and neck tumours. IARC Press, Lyon
Hertog D, van der Waal I. Ameloblastoma of the jaws. A critical reappraisal based on a 40-years single institution experience. Oral Oncol. 2010;46(1):61–4.
Hall JM, Weathers DR, Unni KK. Ameloblastic carcinoma: an analysis of 14 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(6):799–807.
Neville B, Damm DD, Allen CM, Bouquot J. Oral and maxillofacial pathology. Philadelphia: WB Saunders; 2009.
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–54.
Mercer KE, Pritchard CA. Raf proteins and cancer: B-Raf is identified as a mutational target. Biochim Biophys Acta. 2003;1653(1):25–40.
Brown NA, Rolland D, McHugh JB, Weigelin HC, Zhao L, Lim MS. Activating FGFR2-RAS-BRAF mutations in ameloblastoma. Clin Cancer Res. 2014;20(21):5517–26.
Kurppa KJ, Catón J, Morgan PR, Ristimäki A, Ruhin B, Kellokoski J, et al. High frequency of BRAF V600E mutations in ameloblastoma. J Pathol. 2014;232(5):492–8.
Sweeney RT, McClary AC, Myers BR, Biscocho J, Neahring L, Kwei KA, et al. Identification of recurrent SMO and BRAF mutations in ameloblastomas. Nat Genet. 2014;46(7):722–5.
Gomes CC, Diniz MG, Gomez RS. Progress towards personalized medicine for ameloblastoma. J Pathol. 2014;232(5):488–91.
Ackerman GL, Altini M, Shear M. The unicystic ameloblastoma: a clinicopathologic study of 57 cases. J Oral Pathol. 1988;17(9–10):541–6.
Marino-Enriquez A, Fletcher CDM. Shouldn’t we care about the biology of benign tumours. Nat Rev Cancer. 2014;14:701–2.
Patton EE, Widlund HR, Kutok JL, Kopani KR, Amatruda JF, Murphey RD, et al. BRAF mutations are sufficient to promote nevi formation and cooperate with p53 in the genesis of melanoma. Curr Biol. 2005;15(3):249–54.
Dankort D, Curley DP, Cartlidge RA, Nelson B, Karnezis AN, Damsky Jr WE, et al. Braf(V600E) cooperates with Pten loss to induce metastatic melanoma. Nat Genet. 2009;41(5):544–52.
Acknowledgments
This work was supported by grants from the National Council for Scientific and Technological Development (CNPq)/Brazil, Coordination for the Improvement of Higher Education Personnel (CAPES)/Brazil and “Fundação de Amparo a Pesquisa do Estado de Minas Gerais” (FAPEMIG)/Brazil. RS Gomez and CC Gomes are research fellows at CNPq/Brazil.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
The correspondent author is the Guarantor of Submission.
Rights and permissions
About this article
Cite this article
Diniz, M.G., Gomes, C.C., Guimarães, B.V.A. et al. Assessment of BRAFV600E and SMOF412E mutations in epithelial odontogenic tumours. Tumor Biol. 36, 5649–5653 (2015). https://doi.org/10.1007/s13277-015-3238-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3238-0