Abstract
Exosomes, membrane-bound vesicles having a diameter of 30–150nm, are secreted by most cell types, including tumor cells. These vesicles mediate intercellular communication by transferring bioactive molecules (including a variety of proteins and nucleic acids) from donor to recipient cells. Notably, tumor cells secrete more exosome into microenvironment than nontumoral cells. Tumor-derived exosomes are enriched in molecular and genetic traits of tumor cells that facilitate cancer initiation, progression, and metastasis. Due to their abundance and stability, exosomes are one of the promising diagnostic and prognostic biomarkers for various cancers. Despite promising clinical potential, exosome-based diagnostics remains challenging because of the heterogeneity of exosome and difficulties in the profiling of exosomal contents. Therefore, there is a necessity to develop the sensing platform for molecular fingerprinting of exosomes toward clinical application. In this critical review, we explore the emerging use of nanoplasmonic biosensors to detect exosomal biomarkers and the application of this technology to the diagnosis and monitoring of cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is the leading cause of death worldwide. Early diagnosis and personalized treatments are two of the most significant challenges in the fight against cancer1,2. However, traditional methods for cancer diagnosis are primarily based on tissue biopsies, but limited sampling availability and invasiveness present practical difficulties for patient management3. Cancer biomarkers play important role in cancer diagnosis and therapeutics. Even though cancer biomarkers provide accurate information on the staging and the mechanisms underlying the cancer, there is a large gap between biomarker research and clinical usage due to various challenges, such as the low abundance and poor stability in biofluids4,5.
Exosomes are nanometer-sized vesicles (30–150 nm in a diameter) that are actively secreted by cancer cells6. They are excreted into body fluids (such as blood, saliva, and urine) with high abundance and stability7. Exosomes play vital roles in tumorigenesis, cancer progression and metastasis by transferring bioactive molecules between cancer cells and stromal cells in local and distant microenvironments8. Given their features, exosomes are ideal candidates for use as reliable biomarkers for non-invasive cancer diagnostics9. Numerous guidelines have been developed to provide a framework for exosome-based cancer diagnosis, however, there are substantial barriers to implementing advanced techniques in clinical fields. Therefore, analyzing exosomal biomarkers for the diagnosis and prognosis of cancer has attracted significant attention. Most cancer states start with small changes in cellular processes that become amplified the more prolonged cancer progresses without medical intervention. To improve exosome-based diagnostic efficiency, many techniques have been applied to measure the levels of exosomal biomarker such as enzyme-linked immunosorbent assay (ELISA)10, flow cytometry11 and nanoplasmonic biosensor12. Among these techniques, Surface-enhanced Raman scattering (SERS)-based nanoplasmonic biosensor is a highly sensitive and real-time analysis. This method is particularly attractive for exosome-based diagnostic, as it does not require tedious sample preparations and complicated instrumentation but is also non-destructive and minimally invasive. This review aims to comprehensively describe state of the art in nanoplasmonic sensing of exosomal biomarkers for cancer diagnosis and prognosis.
Biogenesis, Secretion and Molecular Contents of Exosome in Cancer
Exosome biogenesis initiates as an endocytic pathway at the plasma membrane13,14. This starts at an invagination of endosomal membranes, leading to the formation of an endosome. In this process, multivesicular bodies (MVBs) fuse with the plasma membrane, culminating in the release of an exosome (Figure 1). Exosome formation is accompanied by the coordinated efforts of protein networks as summarized in Table 1. In particular, many of these factors not only interact with directly exosomal cargo, but also indicate that vesicle formation is a complex regulatory process that is tightly coupled with substrate sequestration for exosome secretion.
During the biogenesis and before the secretion of exosomes, various molecular contents are loaded into the lumen of exosomes. Exosomes contain various biomolecules13,15. These exosomal contents are heterogenous depending on the origin of the cells, and pathological and physiological status16. For example, exosomal proteins consist of the characteristic proteins that belong to the biogenesis process and secretion17. In addition, exosomes carry genetic biomolecules such as mRNA, long noncoding RNA, microRNA(miRNA), and double-stranded RNA(DNA)18. Furthermore, lipids are an essential component of exosomes. They not only form the bilayer membrane structure but also participate in the homeostasis regulation of recipient cells to maintain their stable state19. Tumor derived exosomes can facilitate communication between tumor and normal cells through the transport of tumor molecular signature20. Meanwhile, tumor cells secrete at least 10-fold more exosomes into microenvironment than normal cells. As a result, tumor derived exosomes change their microenvironment from a normal state to a tumor state, for example tumor growth, invasion, and drug resistance21.
Functions of Exosome in Cancer
Exosomes derived from cancer cells are involved in a variety of cellular functions and participate in pathological as well as physiological events (Figure 2). Since exosomes can distribute throughout all body fluids, exosome transfer oncogenic traits within the tumor microenvironments (TME) to distant tissue sites. To re-program their surroundings to the TME, cancer cells secrete numerous exosomes. In several studies, cancer cells were found to secrete significantly more exosomes than normal cells22. The communication net-work of exosome secretion in the TME is entirely tumor driven. It promotes tumor progression and metastasis by silencing the antitumor immune response, altering the stroma cell response, and supporting new vessel growth to prompt the survival of tumor cells. For example, Peinado et al. demonstrated that exosomes derived from mouse melanoma cells can educate and transform the born marrow environment into a melanoma-promoting milieu23.
Functions of tumor-derived exosome in cancer. Tumor-derived exosomes carry genetic traits into the TME. Genetic components induce tumor progression and metastasis in exosomes. Exosomes permit (a) horizontal transfer of oncogenic traits from the primary tumor to recipient target cells located in distant organs. Furthermore, tumor-derived exosomes contribute to (b) tumor progression via enhanced (c) angiogenesis and (d) metastasis.
In addition, tumor derived exosomes called oncosomes transfer various mRNA and miRNA, which contribute to tumorigenesis by translating into a functional protein. They deliver oncogenic traits to recipient cells, sustain autocrine signaling in tumor cells, and modify stroma cell function in the TME. Therefore, exosomes derived from tumor play a crucial role in oncogenic transformation. As such, exosomes derived from cancer cells are key regulators in cancer development24.
Exosomes as Cancer Biomarker
Tumor-derived exosomes containing molecular and genetic traits representative of the tumor cells are abundant in all body fluid types, including blood, urine and salvia. In particular, these exosomes can mediate cell-cell communication through the horizontal transfer of tumorigenic information to promote tumor progression and metastasis25,26. Furthermore, exosomal phospholipid membranes encapsulate biologically active molecules and protect their contents against degradation in the extracellular environment27. Due to their stability, exosomes represent a promising bio-marker for early cancer diagnosis and disease monitoring28,29. Content analysis of the exosome can be robust and non-invasive for repeated tests. As tumor cells release a large abundance of exosomes, it affords relatively unbiased readouts of the whole tumor burden and is less affected by intra-tumor genetic heterogeneity. Additionally, molecular profiling of tumor-derived exosomes has been demonstrated to correlate with tumor burden, prognosis, even as a treatment30, 31. Despite such promising clinical potential, the analysis of exosomal contents remains a challenging. Conventional biosensors for detecting exosomal biomarkers to diagnose early-stage tumor formation or recurrence have severe limitations, including poor selectivity and low sensitivity. Many approaches reviewed previously have focused on addressing these challenges using nanoplasmonic platforms.
Nanoplasmonic Approaches Toward Exosome Analysis for Clinical Diagnosis
Exosomes attract considerable interest in the fields of diagnosis and prognosis due to the multitude of bio-molecules present that contain information regarding derived parent cells. Although many traditional methods are available for the molecular analysis of exosomes, most require bulk samples, which makes it challenging to differentiate small subpopulations derived from specific cell types (e.g., cancer cells) within a large population derived from other cell types32. Optical biosensors that exploit for light absorption, fluorescence, Raman scattering, and refractive index are powerful analytical tools for the detection, quantification, and analysis of biochemical interactions with fast detection, high sensitivity, and real-time monitoring without any time-consuming steps before the sample pretreatment steps33,34. Among other optical biosensors, nanoplasmonic biosensors could be a representative tool for identifying subtle signal differences based on strong electromagnetic (EM) field enhancement resulting from the localized surface plasmon resonance (LSPR) phenomenon of metallic nanostructures in this context35–40. In particular, we focused on SERS spectroscopy for the exosome analysis for clinical applications.
SERS based Nanoplasmonic Sensor
SERS has emerged as a promising analytical tool for monitoring biological interactions due to its high sensitivity, low background-to-noise ratio, and appropriateness for application in various conditions41–43. Based on the LSPR, Raman signals from biomolecules are significantly increased due to metallic nano-structures that bind analytes44–48 (Figure 3). When nano-sized metallic structures are excited by incident light, the electric field of the incoming light induces polarization of the free electrons, which is called LSPR49–55. This phenomenon results in EM field enhancement, which dramatically amplifies the signal observed from molecules bound to the surface of metallic nanostructures56–60. LSPR is also highly sensitive to changes in the local dielectric environment, meaning that even single molecular level sensitivity using SERS can be achieved as well as enhancement factors (EF) over ~1015. SERS also can provide a characteristic fingerprint Raman peak, which is an abundant source of information for identifying the targets43,61,62. Because of these merits, many SERS techniques have been developed to analyze biological reactions concerning disease pathogenesis in practice. Here, we introduce several SERS techniques for detecting exosomes and exosomal biomarkers for cancer diagnosis and monitoring progression.
SERS Detection of Exosome and Exosomal Biomarkers
Several exosome analyses using SERS studies have been recently reported. Shin et al. analyzed specific surface protein compositions of exosomes to diagnose/prognose cancer35. In this study, Raman bands of exosomes from nonsmall cell lung cancer cells were correlated well with their several protein markers (CD9, CD81, EpCAM, and EGFR), indicating these results will contribute studies on exosomal surface protein markers for diagnosis of cancer. To effectively detect the target biomarker, many researchers focused on developing SERS substrates, which enhance the signal to noise ratio of the Raman spectra of single molecules. Sivashanmugan et al. fabricated the bimetallic nanoplasmonic gap-mode SERS substrate to investigate exosomes63 (Figure 4a). Ag nanocubes (AgNCs) on an Au nanorods (AuNRs) formed a robust plasmonic cavity effect on the hot-ring (HR) diameter of the AuNR surface. The optimized bimetallic nanoplasmonic gap-mode SERS substrates have shown that the exosomes can be detected at concentrations 104–105 times lower than normal blood samples. In addition, they succeed in distinguishing the SERS spectrum pattern from lung cancer-derived exosomes by comparing lung cancer (PC-9, H1975, and HCC827) and normal (NL-20, BEAS-2B, and L929) cell lines. In addition, the sample requirements of this method are 100–1000 times less than those of Western blot analysis, making it suitable for clinical applications, primarily through liquid biopsy. To diagnose and classify lung cancer, Park et al. combined SERS and principal component analysis (PCA)64 (Figure 4b). Since PCA can maximize the covariance of the SERS spectral data, it could convert coordinate space to classify exosomes. In this study, exosomes from two lung cancer cell lines (H1299 and H522) and one normal (alveolar) cell line were distinguished through PCA by 95.3% sensitivity and 97.3% specificity. The PCA results were induced by 11 different points in SERS spectra from lung cancer cell-derived exosomes. Notably, this method could detect exosomes at a low concentration of 109 particles/mL, which is a 100-fold lower concentration than ELISA. Also, shorter experimental time was necessary since this method was label-free, meaning it did not require a specific sample preparation step For our previous study, we applied head flocked gold nanopillars SERS substrates to detect three exosomal miRNAs (miR-21, miR-222, and miR-200c) for the accurate diagnosis of breast cancer65 (Figure 5). Due to the capillary force under exposure to the solvent, the adjacent nanopillars flocked, resulting in the formation of multiple hotspots. Additionally, locked nucleic acid (LNA) was applied to the SERS sensor, increasing the detection limit of 1 aM. In this system, expression levels of exosomal miRNAs released from three different subtypes of breast cancer cell lines were analyzed. Each subtype has a different miRNA expression pattern, and the sensing results were consistent with qRT-PCR, which means the sensor can be a new platform to classify molecular subtypes of breast cancer.
(a) Schematic diagram of fabricating bimetallic gap-mode substrates (AgNCs on AuNR). AgNCs were self-assembled on an AuNR surface, producing high-density HR area using 1,2-ethanedithiol63. Images reproduced with permission from [63]. (b) Schematic diagram of lung cancer diagnosis through SERS classification of exosome using PCA64. Images reproduced with permission from [64].
Schematic diagram of exosomal miRNA detection using head-flocked nanopillar SERS substrates. LNA capture probes were immobilized on the head-flocked nanopillar SERS substrate followed by capturing target miRNAs. Subsequently, Cy3-LNA detection probes were also bound to the target miRNAs. Hybridization of perfectly matched LNA capture probes-target miR-NAs-LNA detection probes generated strong Cy3 Raman signal by hot spot inside of head-flocked nanopillar structures65. Images reproduced with permission from [65].
SERS Tags-based Detection of Exosome and Exosomal Biomarkers
Instead of utilizing SERS substrates, other studies utilized SERS tags for signal enhancement to analyze exosomes. Zong et al. used SERS nanotags having core-shell structure, with gold core-silver shell nanorods (Au@AgNRs) and magnetic nanobeads with two different antibodies specific for two proteins on exosomes, respectively66. In this SERS-based method for protein measurement, the SERS signal was 3.8 times higher for SKBR3 breast cancer cell-derived exosomes than MRC5 normal fibroblasts-derived exosomes with exosomal CD63 and HER2 as the biomarkers. These results demonstrated its potential for breast cancer diagnosis. Wang et al. also used magnetic beads and AuNPs decorated with specific aptamers to identify several exosome types simultaneously67 (Figure 6a). Three types of Raman reporters (DTNB, MMC, and 2NAT) were utilized to form different SERS tags providing unique SERS signals. Each AuNP functionalized with different Raman reporters had different aptamers (DTNB Raman reporter for HER2 aptamer, MMC for CEA aptamer, and 2NAT for PSMA aptamer). These SERS tags allowed detection of several cancerous exosomes simultaneously without spectral overlapping. When target exosomes were captured, they formed an aptaimmunocomplex, decreasing SERS intensity in the supernatant. This approach was successfully tested for the detection in real blood samples, indicating that the SERS-based method is a promising tool for multiple cancer screening systems. In another study, a new analysis strategy was proposed by combining duplex-specific nuclease (DSN) and ARANPs (Au@R6G@AgAu nanoparticles), which have internal nanogap to generate stable SERS signals to enhance the Raman signal for detecting miR-2168 (Figure 6b). Specifically, ARANPs have internal nanogap for creating hot spots to provide stable and reproducible Raman signals. When the target exosomal miRNAs were captured, DSN could cleave the DNA/miRNA duplex, releasing SERS tags. In the meantime, the target exosomal miRNAs remained intact and were involved in the next cycling amplification step. After the cycling step, concentrated SERS tags made strong SERS. As a result, a combination of ARANPs and DSN gave this platform a detection limit of 5 fM. Importantly, miR-21 extracted from the blood samples of patients with recurrent non-small-lung cell cancer was detectable in a small sample volume (5.0µL), which implies that this system could be a powerful potential tool for point-of-care testing. Another study used DSN to develop SERS biosensors for pancreatic cancer diagnosis69 (Figure 6c). As a SERS tag, Au@Ag@DTNB was synthesized for one- step detection of miRNAs. Under the presence of target miRNAs, DSN can sever the double-stranded DNA/ miRNA duplex, releasing SERS tags from Fe3O4@Ag. Releasing SERS tags causes SERS intensity quenching, indicating that target miRNAs were effectively detected. In this system, single-base recognition with a detection limit of 1 aM is achieved by Au@Ag@ DTNB SERS tag in one step.
(a) Schematic diagram of SERS-based multiplex detection of exosomes. Three types of probe were utilized to detect different target exosomes. Decreased Raman signal of specific probes from supernatant means the corresponding target exosome was detected successfully67. Images reproduced with permission from [67]. (b) Schematic diagram of ARANPs synthesis and SERS-based exosomal miRNAs detection strategy. DSN cleaved the DNA/miRNA duplex under existence of target miRNAs, releasing ARANPs. Released ARANPs made stronger Raman signals according to the number of target miRNAs68. Images reproduced with permission from [68]. (c) Schematic diagram of fabricating Fe3O4@Ag-SERS tags and DSN-assisted miRNAs detection process using SERS. Cleaving DNA/miRNAs duplex by DSN caused streptavidin-SERS tag release, inducing Raman intensity quenching69. Images reproduced with permission from [69].
Li et al. developed polydopamine-modified immunocapture substrates and an ultrathin polydopamine-encapsulated antibody-reporter-Ag(shell)-Au(core) multilayer (PEARL) SERS nanotag to detect pancreatic cancer-derived exosomes70 (Figure 4c). By using specific antibodies, chip-exosome-PEARL tag sandwich structure was formed under the presence of target exosomes, and Raman intensity at 1072 cm-1 was measured for quantitative analysis. Furthermore, this strategy could distinguish metastasized tumors from metastasis-free tumors, and P1–2 stages from P3 stage tumors in an ultrasmall volume (2µl) of clinical pancreatic serum samples, which could be achieved through histopathological test.
Schematic diagram of PDA chip-exosome-PEARL SERS tag assay. Target exosomes were captured on the PDA immunocapture substrate followed by PEARL SERS tag binding70. Images reproduced with permission from [70].
Conclusion and Future Perspectives
To date, although conventional biopsies play a crucial role in cancer diagnosis, these methods are invasive and associated with infection complications. Furthermore, intratumor heterogeneity poses a challenge as they provide false-negative results due to sampling bias. Therefore, exosome-based liquid biopsy is growing in popularity because it is non-invasive, easy to use, and involves real-time monitoring of patient status. In this review, we have provided an overview of exosomes as a non-invasive cancer biomarker, as well as the recent developments nanoplasmonic biosensors as exosome-based cancer diagnostic tools. SERS based sensing techniques show ultrahigh sensitivity (fM ~ aM level) and are capable of detecting exosomes at low volumes. These SERS based exosome diagnostics are facilitated by well-established SERS substrates that serve as SERS hotspots with significant SERS EFs. Therefore, it is apparent that SERS-based plasmonic biosensors for exosome analysis are a prospective alternative to traditional techniques, such as Radioimmunoassay (RIA) or ELISA.
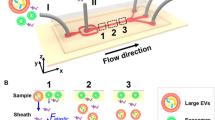
Despite recent success in SERS-based exosome diagnostics, there are still some drawbacks to real world application. First, most of the current studies have only focused on increasing detection specificity and sensitivity. However, the effective detection of exosomal cancer biomarkers is not just a single target detection issue. Relative concentration variants of the target with other proteins should be monitored as well as the absolute concentration of the target. Second, integrated devices that satisfy clinical demands that overcome the gap between the clinical and market needs have not been fully developed yet. For clinical use, novel technologies that can construe multiple or an ensemble of signals are needed. In addition, a commercialized and integrated plasmonic biosensor platform is required. Intensive SERS studies and integrated platform research will assist in solving these problems in the near future. For example, the integration of microfluidic systems and the SERS technique will be a more powerful cancer diagnostic technology through separating and analyzing exosomes in bio-fluids in one chip. Furthermore, to decrease the size and cost of the Raman spectrometers, the development of ultrahigh sensitive, user-friendly, ubiquitous, and low-cost SERS platforms for clinical applications can be achieved.
References
Ginsburg, O., Bray, F., Coleman, M.P., Vanderpuye, V., Eniu, A., Kotha, S.R., Sarker, M., Huong, T.T., Allemani, C., Dvaladze, A., Gralow, J., Yeates, K., Taylor, C., Oomman, N., Krishnan, S., Sullivan, R., Kombe, D., Blas, M.M., Parham, G., Kassami, N., & Conteh, L. The global burden of women’s cancers: a grand challenge in global health. Lancet 389, 847–860 (2017).
Emery, J.D., Shaw, K., Williams, B., Mazza, D., Fallon-Ferguson, J., Varlow, M. & Trevena, L.J. The role of primary care in early detection and follow-up of cancer. Nat. Rev. Clin. Oncol. 11, 38–48 (2014).
Buder, A., Tomuta, C. & Filipits, M. The potential of liquid biopsies. Curr. Opin. Oncol. 28, 130–134 (2016).
Tubiana, M. Radiation risks in perspective: radiation-induced cancer among cancer risks. Radiat. Environ. Bioph. 39, 3–16 (2000).
Ruckert, F., Pilarsky, C. & Grutzmann, R. Serum tumor markers in pancreatic cancer-recent discoveries. Cancers (Basel) 2, 1107–1124 (2010).
Huang, T. & Deng, C.X. Current progresses of exosomes as cancer diagnostic and prognostic biomarkers. Int. J. Biol. Sci. 15, 1–11 (2019).
Wong, C.H. & Chen, Y.C. Clinical significance of exosomes as potential biomarkers in cancer. World J. Clin. Cases 7, 171–190 (2019).
Tian, W.J., Liu, S.S. & Li, B.R. Potential role of exosomes in cancer metastasis. Biomed Res. Int. 2019, 4649705 (2019).
Cappello, F., Logozzi, M., Campanella, C., Bavisotto, C.C., Marcilla, A., Properzi, F. & Fais, S. Exosome levels in human body fluids: A tumor marker by themselves? Eur. J. Pharm. Sci. 96, 93–98 (2017).
Campos-Silva, C., Suarez, H., Jara-Acevedo, R., Linares-Espinos, E., Martinez-Pineiro, L., Yanez-Mo, M. & Vales-Gomez, M. High sensitivity detection of extracellular vesicles immune-captured from urine by conventional flow cytometry. Sci. Rep. 9, 2042 (2019).
Liu, C., Xu, X., Li, B., Situ, B., Pan, W., Hu, Y., An, T., Yao, S. & Zheng, L. Single-exosome-counting immunoassays for cancer diagnostics. Nano Lett. 18, 4226–4232 (2018).
Rojalin, T., Phong, B., Koster, H.J. & Carney, R.P. Nanoplasmonic approaches for sensitive detection and molecular characterization of extracellular vesicles. Front. Chem. 7, 279 (2019).
Ingato, D., Lee, J.U., Sim, S.J. & Kwon, Y.J., Good things come in small packages: Overcoming challenges to harness extracellular vesicles for therapeutic delivery. J. Controlled Release 241, 174–185 (2016).
Mathieu, M., Martin-Jaular, L., Lavieu, G. & Thery, C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell-to-cell communication. Nat. Cell Biol. 21, 9–17 (2019).
Colombo, M., Raposo, G. & Thery, C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu. Rev. Cell Dev. Biol. 30, 255–289 (2014).
Raposo, G. & Stoorvogel, W. Extracellular vesicles: Exosomes, microvesicles, and friends. J. Cell Biol. 200, 373–383 (2013).
Gutierrez-Vazquez, C., Villarroya-Beltri, C., Mittelbrunn, M. & Sanchez-Madrid, F. Transfer of extracellular vesicles during immune cell-cell interactions. Immunol. Rev. 251, 125–142 (2013).
Valadi, H., Ekstrom, K., Bossios, A., Sjostrand, M., Lee, J.J. & Lotvall, J.O. Lotvall, J.O. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 9, 654–659 (2007).
Chu, Z.T., Witte, D.P. & Qi, X.Y. Saposin C-LBPA interaction in late-endosomes/lysosomes. Exp. Cell Res. 303, 300–307 (2005).
Akers, J.C., Gonda, D., Kim, R., Carter, B.S. & Chen, C.C. Biogenesis of extracellular vesicles (EV): exosomes, microvesicles, retrovirus-like vesicles, and apoptotic bodies. J. Neuro-Oncol. 113, 1–11 (2013).
Chiarugi, P. & Cirri, P. Metabolic exchanges within tumor microenvironment. Cancer Lett. 380, 272–280 (2016).
Logozzi, M., De Milito, A., Lugini, L., Borghi, M., Calabro, L., Spada, M., Perdicchio, M., Marino, M. L., Federici, C., Iessi, E., Brambilla, D., Venturi, G., Lozupone, F., Santinami, M., Huber, V., Maio, M., Rivoltini, L. & Fais, S. High levels of exosomes expressing CD63 and caveolin-1 in plasma of melanoma patients. Plos One 4, e5219 (2009).
Peinado, H., Aleckovic, M., Lavotshkin, S., Matei, I., Costa-Silva, B., Moreno-Bueno, G., Hergueta-Redondo, M., Williams, C., Garcia-Santos, G., Ghajar, C.M., Nitadori-Hoshino, A., Hoffman, C., Badal, K., Garcia, B.A., Callahan, M.K., Yuan, J.D., Martins, V.R., Skog, J., Kaplan, R.N., Brady, M.S., Wolchok, J.D., Chapman, P.B., Kang, Y.B., Bromberg, J. & Lyden, D. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat. Med. 18, 883–891 (2012).
Syn, N., Wang, L.Z., Sethi, G., Thiery, J.P. & Goh, B.C. Exosome-mediated metastasis: From epithelial-mesenchymal transition to escape from immunosurveillance. Trends Pharmacol. Sci. 37, 606–617 (2016).
Chen, W.X., Liu, X.M., Lv, M.M., Chen, L., Zhao, J. H., Zhong, S.L., Ji, M.H., Hu, Q., Luo, Z., Wu, J.Z. & Tang, J.H. Exosomes from drug-resistant breast cancer cells transmit chemoresistance by a horizontal transfer of microRNAs. Plos One 9, e95240 (2014).
Wang, B., Tan, Z. & Guan, F. Tumor-derived exosomes mediate the instability of cadherins and promote tumor progression. Int. J. Mol. Sci. 20, 3652 (2019).
Ye, S.B., Li, Z.L., Luo, D.H., Huang, B.J., Chen, Y. S., Zhang, X.S., Cui, J., Zeng, Y.X. & Li, J. Tumor-derived exosomes promote tumor progression and T-cell dysfunction through the regulation of enriched exosomal microRNAs in human nasopharyngeal carcinoma. Oncotarget 5, 5439–5452 (2014).
Revenfeld, A.L., Baek, R., Nielsen, M.H., Stensballe, A., Varming, K. & Jorgensen, M. Diagnostic and prognostic potential of extracellular vesicles in peripheral blood. Clin. Ther. 36, 830–846 (2014).
Jakobsen, K.R., Paulsen, B.S., Baek, R., Varming, K., Sorensen, B.S. & Jorgensen, M.M. Exosomal proteins as potential diagnostic markers in advanced non-small cell lung carcinoma. J. Extracell. Vesicles 4, 26659 (2015).
Li, I. & Nabet, B.Y. Exosomes in the tumor microenvironment as mediators of cancer therapy resistance. Mol. Cancer 18, 32 (2019).
Fu, Q.H., Zhang, Q., Lou, Y., Yang, J.Q., Nie, G., Chen, Q., Chen, Y.W., Zhang, J.Y., Wang, J.X., Wei, T., Qin, H., Dang, X.W., Bai, X.L. & Liang, T.B. Primary tumor-derived exosomes facilitate metastasis by regulating adhesion of circulating tumor cells via SMAD3 in liver cancer. Oncogene 37, 6105–6118 (2018).
Lee, C., Carney, R., Lam, K. & Chan, J.W. SERS analysis of selectively captured exosomes using an integrin-specific peptide ligand. J. Raman Spectrosc. 48, 1771–1776 (2017).
Lee, S.W., Kang, C.D., Yang, D.H., Lee, J.S., Kim, J.M., Ahn, D.J. & Sim, S.J. The development of a generic bioanalytical matrix using polydiacetylenes. Adv. Funct. Mater. 17, 2038–2044 (2007).
Long, F., Zhu, A. & Shi, H. Recent advances in optical biosensors for environmental monitoring and early warning. Sensors (Basel) 13, 13928–13948 (2013).
Shin, H., Jeong, H., Park, J., Hong, S. & Choi, Y. Correlation between cancerous exosomes and protein markers based on surface-enhanced Raman spectroscopy (SERS) and principal component analysis (PCA). ACS Sens. 3, 2637–2643 (2018).
Sherry, L.J., Jin, R.C., Mirkin, C.A., Schatz, G.C. & Van Duyne, R.P. Localized surface plasmon resonance spectroscopy of single silver triangular nanoprisms. Nano Lett. 6, 2060–2065 (2006).
Mayer, K.M., Hao, F., Lee, S., Nordlander, P. & Hafner, J.H. A single molecule immunoassay by localized surface plasmon resonance. Nanotechnology 21, 255503 (2010).
Truong, P.L., Cao, C., Park, S., Kim, M. & Sim, S.J. A new method for non-labeling attomolar detection of diseases based on an individual gold nanorod immunosensor. Lab Chip 11, 2591–2597 (2011).
Petryayeva, E. & Krull, U.J. Localized surface plasmon resonance: Nanostructures, bioassays and biosensing-A review. Anal. Chim. Acta 706, 8–24 (2011).
Truong, P.L., Kim, B.W. & Sim, S.J. Rational aspect ratio and suitable antibody coverage of gold nanorod for ultra-sensitive detection of a cancer biomarker. Lab Chip 12, 1102–1109 (2012).
Shafer-Peltier, K.E., Haynes, C.L., Glucksberg, M. R. & Van Duyne, R.P. Toward a glucose biosensor based on surface-enhanced Raman scattering. J. Am. Chem. Soc. 125, 588–593 (2003).
Wang, Y. & Irudayaraj, J. A SERS DNAzyme biosensor for lead ion detection. Chem. Commun. (Camb) 47, 4394–4396 (2011).
Nguyen, A.H., Lee, J.U. & Sim, S.J. Nanoplasmonic probes of RNA folding and assembly during pre-mRNA splicing. Nanoscale 8, 4599–4607 (2016).
Xu, S., Ji, X., Xu, W., Zhao, B., Dou, X., Bai, Y. & Ozaki, Y. Surface-enhanced Raman scattering studies on immunoassay. J. Biomed. Opt. 10, 031112 (2005).
Qian, X., Peng, X.H., Ansari, D.O., Yin-Goen, Q., Chen, G.Z., Shin, D.M., Yang, L., Young, A.N., Wang, M.D. & Nie, S. In vivo tumor targeting and spectroscopic detection with surface-enhanced Raman nanoparticle tags. Nat. Biotechnol. 26, 83–90 (2008).
Stokes, R.J., McBride, E., Wilson, C.G., Girkin, J.M., Smith, W.E. & Graham, D. Surface-enhanced Raman scattering spectroscopy as a sensitive and selective technique for the detection of folic acid in water and human serum. Appl. Spectrosc. 62, 371–376 (2008).
Douglas, P., Stokes, R.J., Graham, D. & Smith, W.E. Immunoassay for P38 MAPK using surface enhanced resonance Raman spectroscopy (SERRS). Analyst 133, 791–796 (2008).
Das, G., Mecarini, F., Gentile, F., De Angelis, F., Mohan Kumar, H., Candeloro, P., Liberale, C., Cuda, G., Di Fabrizio, E., Nano-patterned SERS substrate: application for protein analysis vs. temperature. Biosens. Bioelectron. 24, 1693–1699 (2009).
Willets, K.A. & Van Duyne, R.P. Localized surface plasmon resonance spectroscopy and sensing. Annu. Rev. Phys. Chem. 58, 267–297 (2007).
Endo, T., Kerman, K., Nagatani, N., Hiepa, H.M., Kim, D.K., Yonezawa, Y., Nakano, K. & Tamiya, E. Multiple label-free detection of antigen-antibody reaction using localized surface plasmon resonance-based core-shell structured nanoparticle layer nanochip. Anal. Chem. 78, 6465–6475 (2006).
Sagle, L.B., Ruvuna, L.K., Ruemmele, J.A. & Van Duyne, R.P. Advances in localized surface plasmon resonance spectroscopy biosensing. Nanomedicine-Uk 6, 1447–1462 (2011).
Truong, P.L., Ma, X. & Sim, S.J. Resonant Rayleigh light scattering of single Au nanoparticles with different sizes and shapes. Nanoscale 6, 2307–2315 (2014).
Nguyen, A.H. & Sim, S.J. Nanoplasmonic biosensor: Detection and amplification of dual bio-signatures of circulating tumor DNA. Biosens. Bioelectron. 67, 443–449 (2015).
Lee, J.U., Nguyen, A.H. & Sim, S.J. A nanoplasmonic biosensor for label-free multiplex detection of cancer biomarkers. Biosens. Bioelectron. 74, 341–346 (2015).
Kim, H., Lee, J.U., Song, S., Kim, S. & Sim, S.J. A shape-code nanoplasmonic biosensor for multiplex detection of Alzheimer’s disease biomarkers. Biosens. Bioelectron. 101, 96–102 (2018).
Kim, S., Jung, J.M., Choi, D.G., Jung, H.T. & Yang, S.M. Patterned arrays of Au rings for localized surface plasmon resonance. Langmuir 22, 7109–7112 (2006).
Luther, J.M., Jain, P.K., Ewers, T. & Alivisatos, A.P. Localized surface plasmon resonances arising from free carriers in doped quantum dots. Nat. Mater. 10, 361–366 (2011).
Liu, L.Q., Ouyang, S.X. & Ye, J.H. Gold-nanorodphotosensitized titanium dioxide with wide-range visible-light harvesting based on localized surface plasmon resonance. Angew. Chem. Int. Ed. 52, 6689–6693 (2013).
Zhang, D.M., Lu, Y.L., Jiang, J., Zhang, Q., Yao, Y., Wang, P., Chen, B.L., Cheng, Q.Y., Liu, G.L. & Liu, Q.J. Nanoplasmonic biosensor: Coupling electrochemistry to localized surface plasmon resonance spectroscopy on nanocup arrays. Biosens. Bioelectron. 67, 237–242 (2015).
Ma, X., Song, S., Kim, S., Kwon, M.S., Lee, H., Park, W. & Sim, S.J. Single gold-bridged nanoprobes for identification of single point DNA mutations. Nat. Commun. 10, 836 (2019).
Nguyen, A.H., Lee, J., Choi, H.I., Kwak, H.S. & Sim, S.J. Fabrication of plasmon length-based surface enhanced Raman scattering for multiplex detection on microfluidic device. Biosens. Bioelectron. 70, 358–365 (2015).
Kim, W.H., Lee, J.U., Song, S., Kim, S., Choi, Y.J. & Sim, S.J. A label-free, ultra-highly sensitive and multiplexed SERS nanoplasmonic biosensor for miRNA detection using a head-flocked gold nanopillar. Analyst 144, 1768–1776 (2019).
Sivashanmugan, K., Huang, W.L., Lin, C.H., Liao, J.D., Lin, C.C., Su, W.C. & Wen, T.C. Bimetallic nanoplasmonic gap-mode SERS substrate for lung normal and cancer-derived exosomes detection. J. Taiwan Inst. Chem. Eng. 80, 149–155 (2017).
Park, J., Hwang, M., Choi, B., Jeong, H., Jung, J.H., Kim, H.K., Hong, S., Park, J.H. & Choi, Y. Exosome classification by pattern analysis of surface-enhanced Raman spectroscopy data for lung cancer diagnosis. Anal. Chem. 89, 6695–6701 (2017).
Lee, J.U., Kim, W.H., Lee, H.S., Park, K.H. & Sim, S. J. Quantitative and specific detection of exosomal miRNAs for accurate diagnosis of breast cancer using a surface-enhanced Raman scattering sensor based on plasmonic head-flocked gold nanopillars. Small 15, e1804968 (2019).
Zong, S.F., Wang, L., Chen, C., Lu, J., Zhu, D., Zhang, Y.Z., Wang, Z.Y. & Cui, Y.P. Facile detection of tumor-derived exosomes using magnetic nanobeads and SERS nanoprobes. Anal. Methods-Uk 8, 5001–5008 (2016).
Wang, Z.L., Zong, S.F., Wang, Y.J., Li, N., Li, L., Lu, J., Wang, Z.Y., Chen, B.A. & Cui, Y.P. Screening and multiple detection of cancer exosomes using an SERS-based method. Nanoscale 10, 9053–9062 (2018).
Ma, D., Huang, C., Zheng, J., Tang, J., Li, J., Yang, J. & Yang, R. Quantitative detection of exosomal microRNA extracted from human blood based on surface-enhanced Raman scattering. Biosens. Bioelectron. 101, 167–173 (2018).
Pang, Y., Wang, C., Lu, L., Wang, C., Sun, Z. & Xiao, R. Dual-SERS biosensor for one-step detection of microRNAs in exosome and residual plasma of blood samples for diagnosing pancreatic cancer. Biosens. Bioelectron. 130, 204–213 (2019).
Li, T.D., Zhang, R., Chen, H., Huang, Z.P., Ye, X., Wang, H., Deng, A.M. & Kong, J.L. An ultrasensitive polydopamine bi-functionalized SERS immunoassay for exosome-based diagnosis and classification of pancreatic cancer. Chem. Sci. 9, 5372–5382 (2018).
Acknowledgements
J. U. Lee and S. Kim contributed equally to this work. This study was supported by the grant (No. NRF- 2019R1A2C3009821/2010-0027955) from the National Research Foundation of Korea (NRF) and the grant (No. 2014M1A8A1049278) from the Korea CCS R&D Center (Korea CCS 2020 Project) funded by the Korea government (Ministry of Science and ICT).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Lee, J.U., Kim, S. & Sim, S.J. SERS-based Nanoplasmonic Exosome Analysis: Enabling Liquid Biopsy for Cancer Diagnosis and Monitoring Progression. BioChip J 14, 231–241 (2020). https://doi.org/10.1007/s13206-020-4301-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13206-020-4301-5