Abstract
Residency, in particular oncology residency, is a challenging time with extensive academic demands, long working hours, and uncertainty about the future. Our study aimed to evaluate the prevalence and factors associated with burnout, anxiety and depression among oncology residents at a tertiary cancer centre. An anonymised questionnaire-based study was conducted among medical, surgical, paediatric and radiation oncology resident doctors at a tertiary cancer centre in April 2019. We used Copenhagen Burnout Index (CBI) to assess burnout (which includes personal, work-related and patient-related burnout), Patient Health Questionnaire (PHQ9) for depression and Generalised Anxiety Disorder (GAD7) for anxiety. The questionnaire was served to 201 residents. The overall response rate was 70.6%. High personal, work-related and patient-related burnout was identified in 71.1%, 67.6% and 23.2% of the respondents respectively. Medical oncology residents had the highest rate of personal and work-related burnout (95% and 85%) while head and neck oncology residents had the highest rate of patient-related burnout (33.3%). 27.5% of participants were found to have high levels of anxiety on the GAD7 while 14.8% of participants were detected to have a high score on the PHQ9 for depression. High personal burnout and work-related burnout were associated with both high anxiety and depression scores (p < 0.05). There is a high prevalence of burnout, depression and anxiety among oncology residents. With an expected rise in cancer burden in the next decade, psychological issues in caregivers can be expected to increase. Further studies will be needed to determine interventions to reduce psychological distress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Residency is a challenging time in the professional development of a doctor with extensive academic demands, long working hours, lack of autonomy and uncertainty about the future [1]. Oncology residency in particular is even more demanding because of the nature of the disease they are managing. Greenglass defined burnout as “a state of physical, emotional and mental exhaustion that results from long-term involvement in work situations that are emotionally demanding” [2]. Burnout is associated with negative effects on the physician’s physical and mental health and may lead to cardiovascular disease, depression and suicidal ideation [3]. Psychological distress can impact work performance, patient safety and compromise quality of care [4]. Recently, burnout has been included as an “occupational phenomenon” in the International Classification of Diseases-11 (ICD-11) by the World Health Organisation [5]. The prevalence of burnout has been reported between 27 and 75% across all specialties worldwide [3, 6, 7]. In India, a few studies have evaluated the rate of burnout in residents and have found it to be between 52 and 76% [8, 9]. Presently, there is no data published on burnout in oncologists in India. In the background of the poor doctor to patient ratio and strenuous residency programs, we aimed to evaluate the prevalence of burnout, anxiety and depressive disorders and identify perceived causes of psychosocial unrest in oncology residents.
Methods
Participants and Study Design
This cross-sectional survey-based study was carried out at the Tata Memorial Hospital, Mumbai—the largest tertiary referral centre for cancer in India. Medical oncology, paediatric oncology, surgical oncology, head and neck oncology, gynaecologic oncology and radiation oncology were included. Resident doctors were invited by email to participate voluntarily in an anonymous electronic survey in April–May 2019. The survey was open for 3 weeks and a single email was sent after 1 week as a reminder to complete the form. Doctors were defined as either “speciality” residents or “super-speciality” residents based on whether they were pursuing a postgraduate degree or had completed their post-graduation and were pursuing a super-speciality course. Radiation oncology fell under the “speciality” group while the rest formed the “super-speciality” group. Super-speciality residents differ from speciality residents, being at different age groups, stages of learning, family pressures, etc. and were hence grouped separately.
Study Tools
We employed the Copenhagen Burnout Inventory (CBI), Patient Health Questionnaire (PHQ-9) and the Generalised Anxiety Disorder (GAD-7) scale as the tools for this survey. The CBI has scales on personal burnout, work-related burnout and patient-related burnout [10]. All items have five response categories in a Likert scale. Each scale ranges from 0 to 100 points, with high scores indicating higher levels of burnout. Total score on the scale is the average of the scores and a mean score of ≥ 50 is considered a high level of burnout. The PHQ-9 is a diagnostic tool for depression that is quick and easy to complete. The GAD-7 scale was developed as a self-reporting anxiety questionnaire. These scoring tools have been translated and validated in multiple studies [11, 12]. Cut points of 5, 10, 15 and 20 represent none, mild, moderate, moderately severe and severe levels of depression on the PHQ-9. PHQ scores ≥ 10 had a sensitivity of 88% and a specificity of 88% for major depression [12]. Cut points of 5, 10 and 15 represent mild, moderate and severe levels of anxiety on the GAD-7. A sensitivity of 89% and a specificity value of 82% for identifying GAD were reported at a cutoff score of 10 [13]. We included a blank space for free comments at the end of the questionnaire.
Ethical Considerations and Statistical Analysis
The study was submitted to the Institutional Ethics Committee (IEC). It met the criteria for exemption from the review process as defined by the Indian Council of Medical Research and the IEC granted permission to conduct the study. An informed consent form was integrated into the electronic submission form. The questionnaire given to the participants did not have any unique identifiers. Analysis was done using the Statistical Package for the Social Sciences (SPSS) software (version 20) (IBM Corp., Armonk, NY, USA).
Results
From April to May 2019, the questionnaire was served to 201 oncology residents. Of those, 142 residents responded giving us a response rate of 70.6%. The demographic composition, number of years in oncology training and speciality details are summarised in Table 1. Maximum participation was from male surgical oncologists and female radiation oncologists with both groups having 32 participants (22.5%) each. We assessed the questionnaire’s reliability by applying a Cronbach’s alpha for each component and the results were 0.90, 0.90 and 0.89 for personal, work-related and patient-related burnout, respectively, illustrating correlation between all three dimensions. The mean burnout scores for personal and work burnout showed strong correlation (p < 0.001), but similar correlation was not observed for other dimensions.
Rates of Burnout, Depression and Anxiety
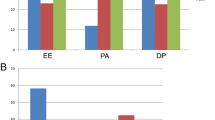
Proportionately, 71.1% of the respondents were identified as having high personal burnout, 67.6% with high work-related burnout and 23.2% with high patient-related burnout. A total of 20.4% of all participants experienced high burnout in all three dimensions. The distribution of different dimensions of burnout in each oncology speciality is illustrated in Fig. 1. Overall, 39 residents (27.5%) reached the cutoff defining moderate and severe anxiety while 21 residents (14.8%) reached the level defining moderately severe and severe depression. Of these residents, 19 (13.4%) had high levels of both depression and anxiety. Table 2 depicts the distribution of scores among all participants.
Factors Related to Burnout, Depression and Anxiety
Gender
While 67.3% of female respondents had a high level of personal burnout, 73.3% male respondents correspondingly had high personal burnout (p = 0.4). About 61.5% of women had high work-related burnout in contrast to 71.1% of men (p = 0.24). High level of patient-related burnout was reported in 25% female doctors against the 22.2% seen in their male counterparts (p = 0.7). Although male participants had higher rates of depression (11.5% vs 16.6%, p = 0.40) and anxiety (25% vs 28.9%, p = 0.86) compared with female participants, it was not statistically different.
Oncology Speciality
Medical oncology residents consistently had the highest median burnout scores across all subscales. A chi-square test run across all departments showed no statistical difference between the number of participants with high personal, work-related and patient-related burnout (p = 0.7, p = 0.058 and p = 0.89, respectively). For super-specialty residents, there was no statistical difference between the burnout faced by medical (medical oncology and paediatric oncology) and surgical oncology (surgical oncology, head and neck oncology and gynaecological oncology) residents in training (p 0.72). There was also no statistical difference in anxiety and depression between surgical and medical departments (p = 0.60 and p = 0.57, respectively). A higher percentage of medical oncology residents were depressed than their counterparts but no statistically significant difference was noted.
Years of Training
While there was a rise in scores in the 2nd year of super-speciality training, there was no significant difference between the 3 years of training (p = 0.77). For radiation oncology residents, the opposite result was seen with a statistically higher burnout in the initial 2 years of training compared with the last 2 years (p = 0.015). In the speciality group and super-specialty groups, candidates in their second year of training formed the highest proportion of respondents with high anxiety levels. Depression was highest in the 2nd year speciality residents and highest in 3rd year super-speciality residents. The distribution across years of training for anxiety and depression is illustrated in Fig. 2. While the prevalence of a high level of anxiety and depression was 33.9% and 10.2% in specialty oncology residents, the prevalence of high anxiety and depression was present in 22.8% and 18.1% of super-speciality residents, respectively (p = 0.343). On univariate analysis, respondents with high burnout were significantly more prone to higher anxiety and depression (p 0.018).
Qualitative Findings
We received 30 different responses in the open section at the end of the questionnaire for comments. Many responses indicate stressors in the underpinning hierarchy in the medical education system, particularly among junior resident doctors and senior faculty, and suggest reexamining this hierarchical relationship. The responses also indicate a necessity to stand for each other and create a strong support network. While improving interpersonal relations and support from peers and seniors emerged as some of the significant measures to tackle burnout, addressing daily workloads and working hours surfaced as other important themes. Most residents suggested an urgent need for defined work hours with a fixed day of the week off in addition to better leave flexibility. In the context of this specific research study, many responses suggested the need to improve infrastructural facilities as a measure to reduce work stress. Quality nutrition, reasonable accommodation and improved recreation facilities appeared as crucial interventions that participants felt would help.
Discussion
Residency is an important period in a young doctor’s life and for many doctors in their early career stage, it is the defining period. Burnout begins during the medical student’s life, continues throughout residency and then progressively increases during the daily life of a physician [14, 15]. This survey was carried out in a tertiary care hospital which caters to 72,000 registered outpatients and 27,880 inpatients in 1 year [16]. This is the first study of this nature conducted among oncology residents in India. While the Maslach Burnout Inventory (MBI) remains synonymous with burnout, it has been subject to a number of criticisms, including its exclusive commercial availability and its doubtful applicability to different cultural and workplace contexts [10]. We picked the Copenhagen Burnout Inventory (CBI) scale as it is available free of charge and has been validated in other large studies involving both senior doctors and residents [9, 17].
Burnout in Indian Residents and Oncology Residents Worldwide
A study on 558 resident doctors in India showed the rates of personal and patient-related burnout to be 51.8% and 22.5%, which closely approximates our figures of 71.1% and 23.2%. Work-related burnout in our study was much higher at 67.6% in contrast to 37.2% reported in the other study [9]. Another study in India using a different scale showed 76.6% residents at risk of burnout [8]. Oncology caregivers have satisfying careers but are at a higher risk of burnout due to various occupational factors such as constantly taking life-changing therapeutic decisions, delivering bad news and limited ability to prolong life for many patients [18]. In addition, there is a necessity to constantly stay up to date with oncology advances, dedicate time to research and work with limited resources. Studies which used the MBI found the rates of burnout in oncology residents to be as high as 44–50% although an exact comparison is not always possible due to the difference in the nature of tools used and heterogeneity across studies [19, 20].
Burnout in Oncology Subspecialities
The rate of burnout varies among medical specialties, with comparisons not always available for each speciality. Studies in most Western medical oncology residents have shown a prevalence between 20 and 37%, but one large study from Europe has shown it to be as high as 71% [20,21,22]. A multi-centre study from Brazil found the prevalence to be as high as 88% at the end of 1st year medical oncology fellowship [23]. Our study found a high level of personal and work-related burnout among medical oncology residents, between 85 and 95%. Burnout in radiation oncology residents in Europe has been reported between 35 and 45%, similar to that reported in North America (33.1–45%) [20, 24,25,26]. Studies from France and Australia have reported higher rates of 57% and 84% [27, 28]. In our study, 62.7% of radiation oncology residents had high personal burnout, 61% had high work-related burnout and 25.4% had high burnout attributed to interaction with patients. A study among surgical oncology residents across Europe showed a burnout rate of 25% [29]. This was in stark contrast to the personal and work-related burnout rate of 74% and 77% we found in our surgical oncology residents. Although no data has been directly reported on gynaecologic oncology residents, the rate among practising doctors is 35% in a study among the society of gynaecologic oncology [30]. While our study had very few participants from the department of gynaecologic oncology, the reported rate of burnout for different subscales was between 25 and 75%. A study in paediatric oncologists revealed the level of burnout to be as high as 50% in paediatric oncologists with < 10 year of practice [31]. The rate of burnout in our paediatric oncology residents across different dimensions was 12.5% for patient-related burnout and 75% each for personal and work-related burnout. A comprehensive study among head and neck surgery residents in the USA showed a high level of burnout among 10% of residents while the level of moderate burnout was as high as 76% which is similar to the 33.3–58.3% across different dimensions in our study [32].
Depression and Anxiety
A study from India using the same PHQ-9 tool reported that 14.4% resident doctors had scored ≥ 15, similar to the 18.1% doctors with the same score in our study. An alarming 16.6% of our respondents reported that they had thoughts of being better off dead or hurting themselves in the past week, which mirrored the 16.7% in the aforementioned study [8]. Globally, residents were reported to have a depression rate of between 20.9 and 43.2% with very few studies mentioning the rate among oncology residents [33]. Depression among surgical oncology residents was reported to be 51% in a study in Europe while it was 42% among radiation oncology residents in France [27, 29]. A study from Brazil reported moderate to high depression among 6% of medical oncology residents [23]. A review of literature showed very few studies assessing the prevalence of anxiety in postgraduate students and none in oncology residents. One study reported high anxiety among 36.6% Indian resident doctors [34]. A similar study using the GAD-7 in an American university revealed a 15.9% prevalence of anxiety compared with 27.5% in our study [35]. Other studies globally have reported an anxiety rate of 8–43.6% using different screening tools [36,37,38]. While some studies showed that female residents scored significantly lower than male residents on burnout scales, other studies have shown the opposite [7]. We found no statistical difference across gender and speciality. A systematic review reported no difference in depression rates between men and women as well as between surgical and non-surgical specialities [33].
Analysis of Themes and Subthemes
Relooking the hierarchical relation between senior and junior doctors appeared to be a priority. Along with a strict view against bullying at the workplace, flattening hierarchy was a theme from other studies to reduce stress at the workplace and has been shown to improve patient safety [39, 40]. Although some of the issues will have to be dealt with contextually, there is a definite need to identify and develop a universalised understanding of burnout [41, 42]. There is a need to move away from the notion that instances of burnout represent “weakness” or personal mental ill-health—a view echoed by some doctors in our study [43]. Epstein and Privitera proposed one essential component of intervention is the recognition that this is a real problem for physicians [44]. The social stigma of mental health issues in medical professionals may complicate the matter [45]. For emotional exhaustion, structural institutional changes (including duty hour restrictions) were more effective than individual-level interventions. While participants in our study strongly felt that a restriction in work hours and fixed work timings would improve well-being, it must also be noted that reductions in shift lengths may have unpredictable effects on the quality of care and training [46]. In another review, the individual-level interventions studied (mindfulness-based approaches and small group discussions) were found to be effective [43]. Targeting issues related to infrastructure deficiencies and system flaws which lead to difficulties managing outpatients surfaced as potential factors that could reduce burnout. Similar responses from doctors in New Zealand resonates a need for reciprocating care from the system that enhances well-being of employees through better management of patient services [17]. A crucial response that emerged is the need for psychosocial support and professional help. Easy, affordable access to adequate counselling services is an additional tool that can enhance resident performance and help provide high-quality patient care [7].
Although the study provides some insight into the life of oncology residents in India, it has some inherent drawbacks. Firstly, the study design was cross-sectional and thus precludes causal interpretation between various factors. Secondly, the study consists of data from a self-reported questionnaire which may lead to overestimation of personal effects. And third, it was a single institution study and the findings cannot be generalised to oncology residents across the country. Despite the limitations of the study, it does have many strengths. It is the first study to describe the rates of burnout, anxiety and depression rates among oncology residents in India using validated tools and is probably representative of the scenario in other emerging economies. The appreciable response rate can help draw definitive insights into the problem. It also covered all fields of oncology—medical, surgical and radiation oncology, which allows us to get a comprehensive picture. The free comments section provides a peep into the individual’s perception and the macro themes generated provide some contextual information from which solutions can be sought.
Conclusion
The high level of burnout, anxiety and depression in this study is a cause for concern both due to its implications on the health of young oncologists as well as its potential impact on patient care. Further studies, in the form of in-depth interviews, surveys across a larger number of oncology trainees and follow-up studies to measure the impact of intervention would be required to establish the causes and evaluate solutions to improve the psychosocial well-being of oncology residents.
References
van Vendeloo SN, Godderis L, Brand PLP, Verheyen K, Rowell SA, Hoekstra H (2018) Resident burnout: evaluating the role of the learning environment. BMC Med Educ 18:54
Schaufeli WB, Greenglass ER (2001) Introduction to special issue on burnout and health. Psychol Health 16:501–510
Elbarazi I, Loney T, Yousef S, Elias A (2017) Prevalence of and factors associated with burnout among health care professionals in Arab countries: a systematic review. BMC Health Serv Res 17:491
Melamed S, Shirom A, Toker S, Berliner S, Shapira I (2006) Burnout and risk of cardiovascular disease: evidence, possible causal paths, and promising research directions. Psychol Bull 132:327–353
WHO | Burn-out an “occupational phenomenon”: International Classification of Diseases. 2019 [cited 31 Jul 2019]. Available: https://www.who.int/mental_health/evidence/burn-out/en/
Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, Mata DA (2018) Prevalence of burnout among physicians: a systematic review. JAMA. 320:1131–1150
Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M et al (2009) Burnout during residency training: a literature review. J Grad Med Educ 1:236–242
Grover S, Sahoo S, Bhalla A, Avasthi A (2018) Psychological problems and burnout among medical professionals of a tertiary care hospital of North India: a cross-sectional study. Indian J Psychiatry 60:175–188
Ratnakaran B, Prabhakaran A, Karunakaran V (2016) Prevalence of burnout and its correlates among residents in a tertiary medical center in Kerala, India: a cross-sectional study. J Postgrad Med 62:157–161
Kristensen T, Borritz M, Villadsen E, Christensen K. (2005) The Copenhagen Burnout Inventory: a new tool for the assessment of burnout
Lowe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W et al (2008) Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care 46:266–274
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16:606–613
Spitzer RL, Kroenke K, Williams, JBW, Löwe B. (2006) A brief measure for assessing Generalized Anxiety Disorder. Archives of Internal Medicine. p. 1092. doi:https://doi.org/10.1001/archinte.166.10.1092
Dyrbye LN, Thomas MR, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, Shanafelt TD (2006) Personal life events and medical student burnout: a multicenter study. Acad Med 81:374–384
Dyrbye LN, Thomas MR, Shanafelt TD (2005) Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc 80:1613–1622
User S. TMC-Annual Report - Tata Memorial Centre. [cited 30 Sep 2019]. Available: https://tmc.gov.in/index.php/tmc-annual-report
Chambers CN, Frampton CM, Barclay M, McKee M (2016) Burnout prevalence in New Zealand’s public hospital senior medical workforce: a cross-sectional mixed methods study. BMJ Open 6:e013947
Shanafelt TD, Gradishar WJ, Kosty M, Satele D, Chew H, Horn L, Clark B, Hanley AE, Chu Q, Pippen J, Sloan J, Raymond M (2014) Burnout and career satisfaction among US oncologists. J Clin Oncol 32:678–686
Bragard I, Etienne A-M, Libert Y, Merckaert I, Liénard A, Meunier J, Delvaux N, Hansez I, Marchal S, Reynaert C, Slachmuylder JL, Razavi D (2010) Predictors and correlates of burnout in residents working with cancer patients. J Cancer Educ 25:120–126
Blanchard P, Truchot D, Albiges-Sauvin L, Dewas S, Pointreau Y, Rodrigues M, Xhaard A, Loriot Y, Giraud P, Soria JC, Kantor G (2010) Prevalence and causes of burnout amongst oncology residents: a comprehensive nationwide cross-sectional study. Eur J Cancer 46:2708–2715
Nguyen TP, Tam VC, Lester RE, Ruiz JC, Bouchard-Fortier A, Card C et al (2014) Burnout among Canadian oncologists and oncology residents. J Clin Orthod 32:6549–6549
Shanafelt TD, Raymond M, Horn L (2014) Oncology fellows’career plans, expectations, and well-being: do fellows know what they are getting into? Journal of Clinical. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4876315/
Cubero DIG, Fumis RRL, de Sá TH, Dettino A (2016. Available: https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s13187-015-0850-z) Burnout in medical oncology fellows: a prospective multicenter cohort study in Brazilian institutions. J Cancer 31:582–587
Ciammella P, De Bari B, Fiorentino A, Franco P, Cavuto S, Alongi F, et al. (2013) The “BUONGIORNO” project: burnout syndrome among young Italian radiation oncologists. Cancer Investigation. pp. 522–528. doi:https://doi.org/10.3109/07357907.2013.830735
Ramey SJ, Ahmed AA, Takita C, Wilson LD, Thomas CR Jr, Yechieli R (2017) Burnout evaluation of radiation residents nationwide: results of a survey of United States residents. Int J Radiat Oncol Biol Phys 99:530–538
Dahn H, McGibbon A, Bowes D. (2019) Burnout and resiliency in Canadian oncology residents: a nationwide resident and program director survey. Practical Radiation Oncology. pp. e118–e125. doi:https://doi.org/10.1016/j.prro.2018.08.001
Lazarescu I, Dubray B, Joulakian MB, Blanchard P, Chauvet B, Mahé M-A, Mornex F, Rocher F, Thureau S (2018) Prevalence of burnout, depression and job satisfaction among French senior and resident radiation oncologists. Cancer Radiother 22:784–789
Leung J, Rioseco P (2017) Burnout, stress and satisfaction among Australian and New Zealand radiation oncology trainees. J Med Imaging Radiat Oncol 61:146–155
Mordant P, Deneuve S, Rivera C, Carrabin N, Mieog JS, Malyshev N, van der Vorst J, Audisio RA, French Association of Young Surgical Oncologists (AJCO), European Society of Surgical Oncology Young Surgeons and Alumni Club (EYSAC) (2014) Quality of life of surgical oncology residents and fellows across Europe. J Surg Educ 71:222–228
Rath KS, Huffman LB, Phillips GS, Carpenter KM. Burnout and associated factors among members of the Society of Gynecologic Oncology. American journal of 2015. Available: https://www.sciencedirect.com/science/article/pii/S0002937815007863
Roth M, Morrone K, Moody K, Kim M, Wang D, Moadel A, Levy A (2011) Career burnout among pediatric oncologists. Pediatr Blood Cancer 57:1168–1173
Golub JS, Weiss PS, Ramesh AK, Ossoff RH. Burnout in residents of otolaryngology–head and neck surgery: a national inquiry into the health of residency training. Academic. 2007. Available: https://journals.lww.com/academicmedicine/Fulltext/2007/06000/Burnout_in_Residents_of_Otolaryngology_Head_and.14.aspx
Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E et al (2015) Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 314:2373–2383
Dave S, Parikh M, Vankar G, Valipay SK (2018) Depression, anxiety, and stress among resident doctors of a teaching hospital. Indian J Soc Psychiatry 34:163
Mousa OY, Dhamoon MS, Lander S, Dhamoon AS. (2016) The MD blues: under-recognized depression and anxiety in medical trainees. PLOS ONE. p. e0156554. doi:https://doi.org/10.1371/journal.pone.0156554
Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R (2009) Anxiety and depression in residents-results of a Swiss longitudinal study. Z Psychosom Med Psychother 55:37–50
Talih F, Warakian R, Ajaltouni J, Shehab AAS, Tamim H. (2016) Correlates of depression and burnout among residents in a Lebanese academic medical center: a cross-sectional study. Academic Psychiatry. pp. 38–45. doi:https://doi.org/10.1007/s40596-015-0400-3
Marzouk M, Ouanes-Besbes L, Ouanes I, Hammouda Z, Dachraoui F, Abroug F (2018) Prevalence of anxiety and depressive symptoms among medical residents in Tunisia: a cross-sectional survey. BMJ Open 8:e020655
Rabøl LI, McPhail MA, Østergaard D, Andersen HB, Mogensen T. (2012) Promoters and barriers in hospital team communication. A focus group study. Journal of Communication in Healthcare. pp. 129–139. doi:https://doi.org/10.1179/1753807612y.0000000009
Quine L (1999) Workplace bullying in NHS community trust: staff questionnaire survey. BMJ. 318:228–232
Shannon D. Physician well-being: a powerful way to improve the patient experience. Physician Exec. 2013;39: 6–8, 10, 12
Lyndon A. (2016) Burnout among health professionals and its effect on patient safety. Agency of Healthcare Research and Quality
Krishnan V, Sarkar S (2017) Physician burnout: can we prevent or reduce it? Natl Med J India 30:149–150
Epstein RM, Privitera MR (2016) Doing something about physician burnout. Lancet. 388:2216–2217
Schwenk TL, Davis L, Wimsatt LA (2010) Depression, stigma, and suicidal ideation in medical students. JAMA. 304:1181–1190
Goitein L, Shanafelt TD, Wipf JE, Slatore CG, Back AL. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005;165: 2601–2606
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented as a poster at 40th Congress of European Society of Surgical Oncology 2020.
Rights and permissions
About this article
Cite this article
Noronha, J., Malik, A., Bindhulakshmi, P. et al. Oncology Residency–a Burning Issue, Results of a Questionnaire-Based Survey on Psychological Well-being of Oncology Residents. Indian J Surg Oncol 11, 387–393 (2020). https://doi.org/10.1007/s13193-020-01183-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-020-01183-7